Abstract
As age-related changes progress, individuals with long-term mobility disabilities experience more challenges in engaging with everyday activities. This archival analysis identified common activity challenges older adults with long-term mobility disabilities report and the type of strategies they employed to respond to these challenges, using the interview data (n=60) from the ACCESS Study. We discovered that activity challenges come from intrinsic factors (i.e., mobility limitations, strength, health conditions) as well as extrinsic factors (transferring and physical access). With these challenges in mind, we constructed home environment design strategies that could meet the needs of people aging with mobility disabilities.
Keywords: Aging in place, design, everyday activities, housing, home modification, mobility disability
Introduction
Humans’ intrinsic capacities generally decrease as they age, potentially resulting in different types of disabilities. Some individuals are aging into disability, meaning that they experience normal age-related changes that impact one or more bodily functions. On the other hand, some individuals have pre-existing impairments prior to old age and age-related declines, which is referred to as aging with disability (Mitzner et al., 2018). In general, living with disabilities in old age may impact one’s independence. However, the challenges to maintaining independence among these two groups are not the same. People who are aging with disability are facing more challenges and requires more support throughout their lifespan (LaPlante, 2014).
In addition to their primary disability, older adults with long-term physical disabilities face increasing health problems and declining physical functions (Molton & Yorkston, 2016). Such conditions impact their activities of daily living (ADLs), which include using the toilet, eating, ambulating, dressing, bathing, and grooming. Engagement in those activities depends on household behavior, which are more complex than basic sensory, motor, and cognitive functions. Household behavior have many facets of complexity that involve body (personal) and environmental systems (Lawton, 1990). While it is acknowledged that both personal and environmental factors impact household behavior in everyday activities engagement, we have limited knowledge about the specifics of those challenges, especially among people aging with long-term mobility disabilities. Understanding common challenges they encounter when doing various activities at home is essential to inform the design of the built environment for this population.
The goal of this study was to understand the experience of older adults aging in place with long-term mobility disabilities regarding their everyday activity challenges and strategies to maintain their independence. We aimed to identify areas that need more support and propose home design recommendations that fit with their need without taking away their dignity in maintaining autonomy.
Patterns of Disability
Physical disability is the most common disability domain among American adults, accounting for 27.8% of the population (Taylor, 2018). Compared to other physical disabilities, mobility disability is the most prevalent type of disability among American older adults, affecting more than 15% of adults aged 65–74, 26% of adults aged 75–85, and 48% of adults aged 85 and over (Roberts et al., 2018). Mobility or ambulatory disability is defined as “serious difficulty walking or climbing stairs” (Erickson et al., 2020). In 2014, approximately 17.6 million older adults aged 65 and older had difficulty walking or climbing stairs (Taylor, 2018). Moreover, they are five times more likely to use canes, crutches, or walkers than adults between 18 and 64 years old (Taylor, 2018).
People aging with physical disabilities are experiencing systemic health problems at a higher rate than people without disabilities (Molton & Yorkston, 2016). Older adults with long-term mobility disabilities are at risk of having secondary conditions caused by age-related declines, such as vision, hearing, and memory problems, in addition to their primary mobility disabilities (Koon et al., 2020). Thus, older adults with long-term mobility disabilities have added complexity to their everyday lives due to their primary disabilities and other interactive effects of age-related declines.
Challenges in Conducting Everyday Activities
Older adults’ mobility disabilities and age-related decreasing capacity impact their ability to conduct everyday activities. In addition to the aforementioned, ADLs include self-care activities that are important for one’s basic health and survival. There are also the Instrumental Activities of Daily Living (IADLs), which are activities beyond the basic self-care, but necessary to maintain independence for aging in place. Some IADLs examples are doing laundry, shopping, cooking, and housekeeping. Challenges to conduct everyday activities could come from an individual’s functional limitations and the environment wherein they conduct the activities. Identifying where and how individual’s functional limitations coincide with the physical environment’s barriers that create accessibility problems for older adults with long-term mobility disabilities is necessary to develop support for their independence.
Built Environmental Support for Maintaining Independence
The process of maintaining independence is key to aging in place, rather than merely a selection of places of residence (Rogers et al., 2020). Maintaining independence in everyday activities is an important factor of successful aging. Aging in place should be understood as an adaptive process that depends on individual situations (Lee, 2008; Scharlach & Moore, 2016). Hence, older adults should be supported to age in place wherever they are.
Aging in place can take place in different types of residential settings. In the United States, 25.9% of older adults live alone in a household, whereas the rest live with family in a household, live with non-family in a household, or live in group quarters (Roberts et al., 2018). Despite the residential settings, aging in place positively contributes to older adults’ health, wellbeing, sense of independence, security, privacy, and comfort (Sixsmith & Sixsmith, 2008). Although increasing attention has been given to the importance of aging in place, there is a need to identify the appropriate types of support needed for older adults to maintain independence and perform everyday activities, especially for adults aging with long-term disabilities.
Archival Study Purpose
This archival study used the interview data from the Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) interview study (Koon et al., 2020; Remillard et al., 2018). ACCESS provides a comprehensive needs assessment for older adults with long-term vision, hearing, and mobility disabilities. The interview data contain rich information about the unique challenges older adults with long-term disabilities face when conducting various everyday activities. Our analysis herein focused on older adults with long-term mobility disabilities, specifically regarding their daily activities at home. The information will help identify the opportunity to provide adequate support for older adults aging in place with long-term mobility disabilities.
The purpose was to identify the activity challenges that older adults with long-term mobility disabilities face in their home environment and to understand their strategies to deal with such challenges. The study design was guided by the Ecological Theory of Adaptation and Aging model (Nahemow & Lawton, 1973), which illustrates the relationship between human competence and environmental press in older adults’ adaptive behavior, facilitated by the person-environment interaction. The interaction is a dialectic of balance between human autonomy and environmental support (Lawton, 1990). We examined the person-environment interaction between the physical condition of the home environment and older adults’ physical capacity to answer the following research questions:
What are the common activity challenges that older adults with long-term mobility disabilities experience in their home environment?
What types of strategies do older adults with long-term mobility disabilities implement to respond to their activity challenges?
Materials and Methods
Overview of ACCESS
ACCESS is a large-scale study that investigated the needs of older adults aging with disabilities. There were three disability groups; vision, hearing, and mobility, with 60 individuals for each group (Koon et al., 2020; Remillard et al., 2018). The study comprised (1) questionnaires to collect information about participants’ demographics, health, and functional limitation and (2) in-depth interviews to assess the participants’ perception of everyday activities challenges and their strategies to manage them. The study was conducted at the University of Illinois Urbana-Champaign and the Georgia Institute of Technology with IRB approval from each university.
Participants
This archival study focused on the interview data for the older adults with mobility disabilities (N=60). Eligible participants were aged 60–79 years old and had mobility disabilities for at least ten years. Mobility disability was defined as having serious difficulty walking or climbing stairs (Disability Glossary, 2021). Koon et al. (2020) provided a more detailed description of the participants.
In-depth Structured Interview
The interview was conducted either in-person or remotely via telephone for about 1–1.5 hours. During the interview, participants were asked to rate each activity based on the difficulty level of performing the task using a 3-point scale (1= not at all difficult, 2 = a little difficult, 3 = very difficult, or N/A = not applicable). Their difficulty rating was based on how they are currently engaging with the activity including with the help or support from others, if any. Then, for each activity category, the interviewer identified one activity with the highest difficulty rating to follow up with a set of open-ended questions (see Table 1).
Table 1.
Follow up questions for the most difficult activity in each activity category.
| Challenge question |
| Thinking about [most difficult activity], what aspect or part of this creates the most challenges for you? |
| Strategy to the challenge |
| How do you handle this challenge? |
| Do you use any sort of devices, tools, or technologies to help you with [most difficult activity]? |
| Do you use any of your own methods or things you came up with to help you do [most difficult activity]? |
| Do you get help from anyone (for example, services, care providers, family members) to do [most difficult activity]? |
Data Analysis
The Original ACCESS Coding Scheme
The coding scheme was developed deductively by generating categories based on a literature study and inductively through content analysis to identify the emerging themes in the interview scripts (see Koon et al., 2020). The initial development, refinement, reliability testing, and coding of the interview scripts were conducted by four primary members of the ACCESS team. The coding was conducted using MAXQDA©, a software program commonly used to analyze qualitative and mixed-methods data.
Activities Selection
ACCESS covered a range of activities in the domestic and public spaces (Koon et al., 2020). For the present analysis, we selected activities that occur in the home environment; namely, basic daily activities, activities around the home, and managing health activities (see Table 2).
Table 2.
Activities included in the study.
| Activity Category | Activity |
|---|---|
| Basic daily activities | Bathing, showering, grooming |
| Dressing | |
| Eating or feeding self | |
| Moving around the home | |
| Toileting | |
| Transferring | |
| Activities around the home | Doing hobbies at home |
| Housekeeping | |
| Noticing alerts | |
| Repairing and maintaining home | |
| Managing health | Managing diet and nutrition |
| Caring for others |
Codes Selection
This study used the existing coding schemes from ACCESS and selected the codes related to personal and environmental factors based on the Ecological Theory of Adaptation and Aging model (Nahemow & Lawton, 1973). We interpreted human competence as individuals’ ability that is influenced by their primary disability and other age-related changes, whereas environmental press is the barrier in the built environment (see Figure 1). Selections of challenge codes and the definitions are presented in Table 3. For the response strategies, we included all the strategy codes from ACCESS and classified them into three categories: person, environment, and person-environment strategies. Person category consisted of strategies that only involved themselves, whereas environment category involved strategies that changed the built environment. The person-environment category included strategies involving other things outside the individual and the built environment, for instance involving other people for assistance or using tools and technology. Table 4 shows the categorization of strategy codes and their definition. A detailed description of the coding selection process for this archival study is available in Ramadhani and Rogers (2021).
Figure 1.
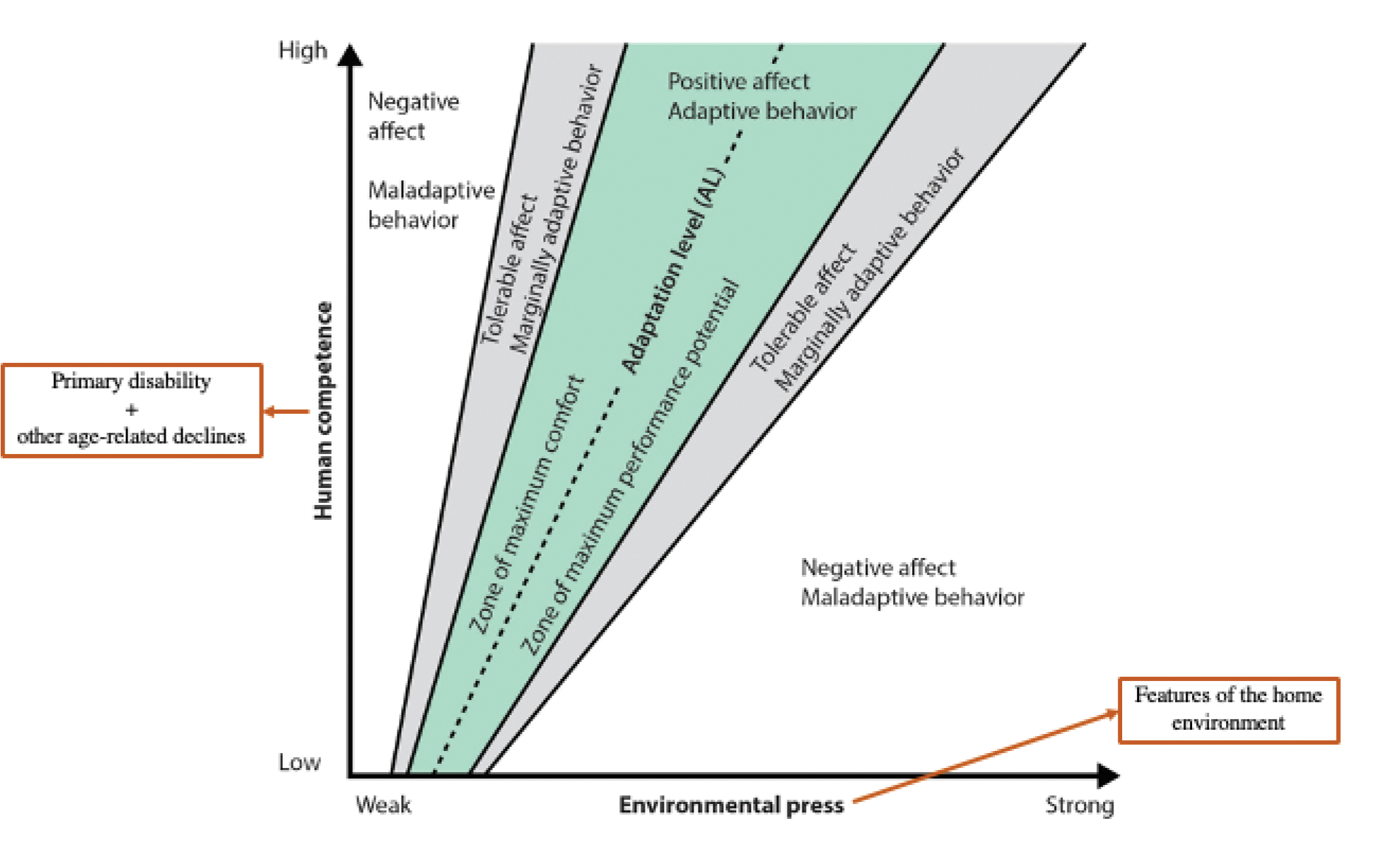
The Ecological Theory of Adaptation and Aging Model (Nahemow & Lawton, 1973).
Table 3.
Selection of codes, counts, and definitions related to the challenges faced by participants.
| Factor | Challenge codes | Definitions |
|---|---|---|
| Person | General health limitations | Constraints caused by health or physical problems that were not specific to motor, visual, or auditory limitations. |
| Mobility limitations | Specific comments related to mobility challenges or mobility abilities/limitations including gross motor movement, fine motor movement, balance. | |
| Physical strength/endurance limitations | The source of the challenge is a lack of strength; objects/tools/bodyweight too heavy/participant not strong enough to complete the task, or struggle with the task because of a lack of physical strength (upper/lower body strength). The source of challenge may also be exhaustion, fatigue, lack of energy, or lack of endurance. | |
| Environment | Physical access | Access to buildings, private or public spaces, the living/built environment, and any other place a person might need or want to go for work, play, education, etc. Physical access includes accessible routes, curb ramps, parking, passenger loading zones, etc. Also, it includes access to things that are physically out of reach (too high, too far). |
| Transferring | The act of transferring: in and out of the shower, on and off the toilet, in and out of bed is the source of the challenge. |
Table 4.
Participant strategy coding scheme.
| Strategies | ACCESS codes | Definitions |
|---|---|---|
| Person | Perseverance | Participant still does the task; it may take more time or effort to complete; displays patience; they persist & do not give up. |
| Prioritizing and planning | Participant plans ahead or prioritizes certain things over others. | |
| Negative emotional response | Mentions an emotional response such as getting impatient, aggressive, frustrated, or depressed. | |
| Reliance on learning and experience | Relies on what is familiar, routines, what they already know. The participant uses organization, keeping things in a certain place. The participant learns something new that they previously did not know. (i.e., Takes a class, researches on the internet. Learns from experience or gains familiarity somehow). | |
| Environment | Home modification | Mentions a structural and permanent change to one’s home |
| Redesign or unconventional use | Participant alters the current design of the residence without bringing in new elements/participant uses an object or something in an unconventional way or a way in which it is not designed to be used. | |
| Person-Environment | Tools or technology | Uses tools or technologies to help with task |
| Assistance from others | Receives help from someone or has someone else do the task (informal or formal help). | |
| Other person’s previous or proposed strategy | Applies other person’s strategy or suggested strategy to the challenge. | |
| New challenge or issues introduced | The response to the challenges creates further or new challenge(s). |
Analytic Approach
First, the unit of analysis was defined by creating segments on participants’ answers to the follow-up questions to the most difficult activity in each category (see Figure 2). There was one follow-up up question regarding the challenges. Participants’ answer to that question was defined as one segment of analysis. Then, four questions covered participants’ general strategies, tools and technologies, methods, and assistance to manage the activity challenges for the strategy follow-up questions. All their answers to this series of questions were defined as one segment of analysis. Next, we extracted the number of times each identified challenge code was mentioned in the challenge segments. The next step was to map the strategies to the three groups: person, environment, and person-environment strategies. Finally, we calculated the number of times the strategy codes were mentioned to get the frequency of strategies of each group. We followed the same process for all the activities across three categories.
Figure 2.
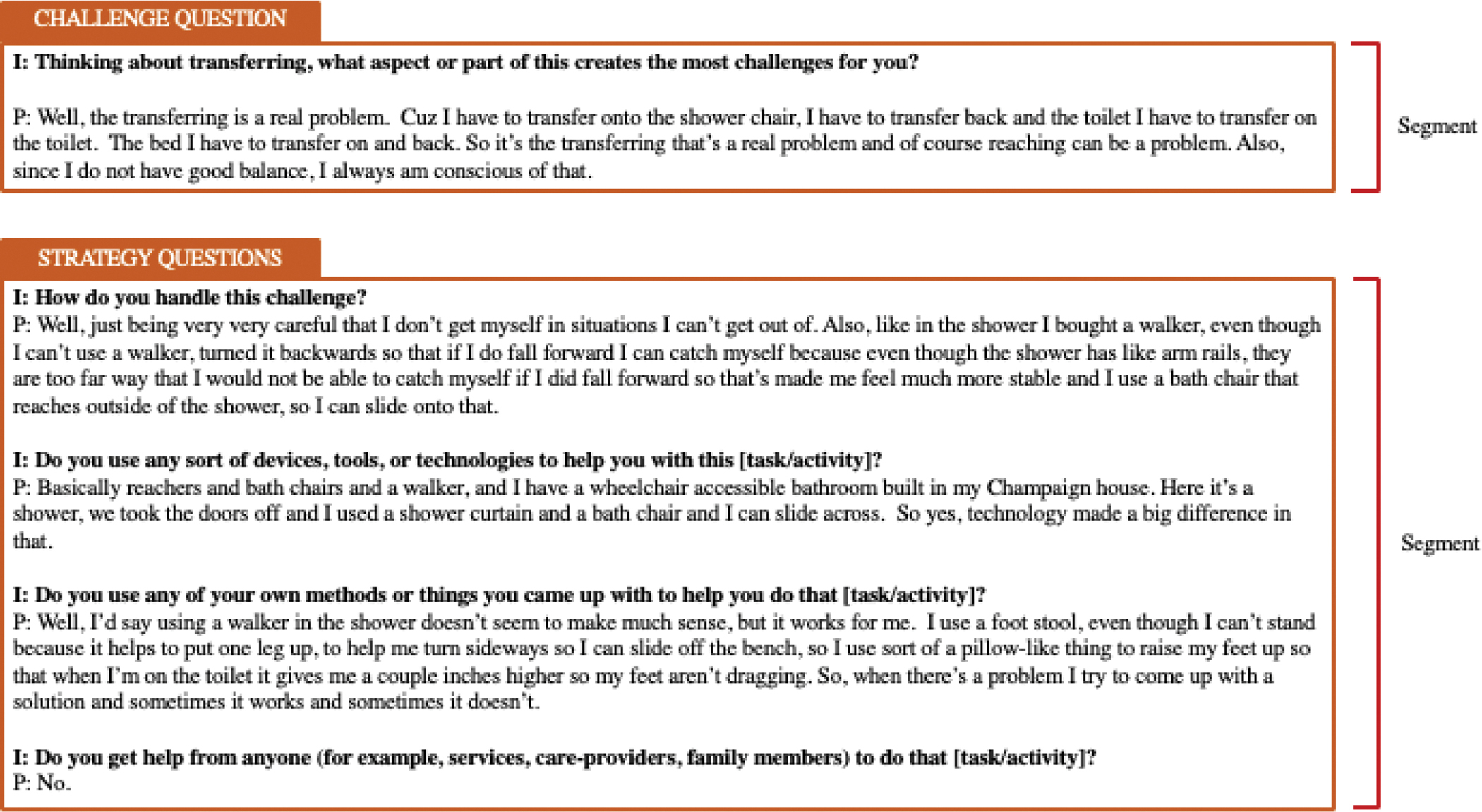
Defining one segment in the ‘challenge and strategy’ follow up questions.
Results
Participant Characteristics
Table 5 provides the details on demographics, housing, and mobility disability characteristics of participants. Participants were aged 60–79 (M = 69, SD = 5.4). Majority of participants were female and had education level of some college/associate degree or higher. Only 12% of participants could walk independently without using a walking aid. Nonetheless, most of them perceived their health as excellent, very good, or good.
Table 5.
Participant demographic and descriptive.
| Variable | Categories | N | % |
|---|---|---|---|
|
| |||
| Sex | Female | 35 | 58.3 |
| Male | 25 | 41.7 | |
|
| |||
| Education | < High school | 2 | 3.3 |
| High school graduate / GED | 6 | 10 | |
| Vocational training | 1 | 1.7 | |
| Some college / Associate degree | 10 | 16.7 | |
| Bachelor’s degree | 11 | 18.3 | |
| Master’s degree | 20 | 33.3 | |
| Doctorate degree | 10 | 16.7 | |
|
| |||
| Race | White/Caucasian | 52 | 86.7 |
| Black/African American | 5 | 8.3 | |
| Other | 2 | 3.3 | |
| No answer | 1 | 1.7 | |
| Do not wish to answer | 4 | 6.7 | |
| Unknown | 1 | 1.7 | |
|
| |||
| Income | <$25,000 | 12 | 20 |
| $25,000–$49,999 | 13 | 21.7 | |
| $50,000–$74,999 | 11 | 18.3 | |
| >$75,000 | 19 | 31.7 | |
| Do not wish to answer | 4 | 6.7 | |
| Do not know for certain | 1 | 1.7 | |
|
| |||
| Marital status | Single | 14 | 23.3 |
| Married | 26 | 43.3 | |
| Separated | 1 | 1.7 | |
| Divorced | 13 | 12.7 | |
| Widowed | 6 | 10 | |
|
| |||
| Type of housing | Single-family home | 34 | 56.7 |
| Apartment or condominium | 21 | 35 | |
| Assisted living facility | 0 | 0 | |
| Nursing home | 3 | 5 | |
| Other | 2 | 3.3 | |
|
| |||
| Housing or community specifically designed for seniors (i.e., 55 and older) | Yes | 19 | 31.7 |
| No | 40 | 66.7 | |
| Not sure | 1 | 1.6 | |
|
| |||
| Perceived health | Poor | 4 | 6.7 |
| Fair | 10 | 16.7 | |
| Good | 32 | 53.3 | |
| Very good | 11 | 18.3 | |
| Excellent | 2 | 3.3 | |
|
| |||
| Cause of mobility disability | Polio | 30 | 50 |
| Neurological condition (e.g., cerebral palsy) | 11 | 18 | |
| Accident or event | 10 | 17 | |
| Congenital condition (e.g., spina bifida) | 4 | 7 | |
| Spinal cord injury | 4 | 7 | |
| Other (e.g., adverse drug reaction) | 1 | 1 | |
|
| |||
| Walk independently without using a walking aid | Yes | 7 | 12 |
| No | 52 | 87 | |
| Missing data | 1 | 2 | |
|
| |||
| Serious difficulty lifting something heavy (∼10 pounds) | Yes | 30 | 50 |
| No | 30 | 50 | |
|
| |||
| Serious difficulty reaching overhead | Yes | 27 | 45 |
| No | 32 | 53 | |
| Missing data | 1 | 2 | |
Basic Daily Activities
The basic daily activities category consisted of (1) bathing, showering, grooming, (2) dressing, (3) eating of feeding self, (4) moving around the home, (5) toileting, and (6) transferring. The most frequently mentioned challenge in this category was transferring (53%), such as transferring in and out of the shower, toilet, bed, and other activities requiring them to change position when moving between objects. A participant said, “Transferring to a higher place. I don’t know if you noticed, but these days hotel beds are higher than they used to be.” Twenty-nine percent of the challenges were due to mobility limitations, which resulted in troubles reaching things up and down. One participant expressed, “I have trouble hooking and unhooking. My arms don’t reach like they used to.” Physical strength was the next challenge (10%). The lack of upper and lower body strength impacted participants’ endurance, for instance, when pushing manual chairs on the carpeting. Finally, the least common challenges were general health (4%) and physical access (4%), which tied to their overall health and the inaccessible routes in the built environment. Figure 3 illustrates the frequency of challenges in the basic daily activities category.
Figure 3.
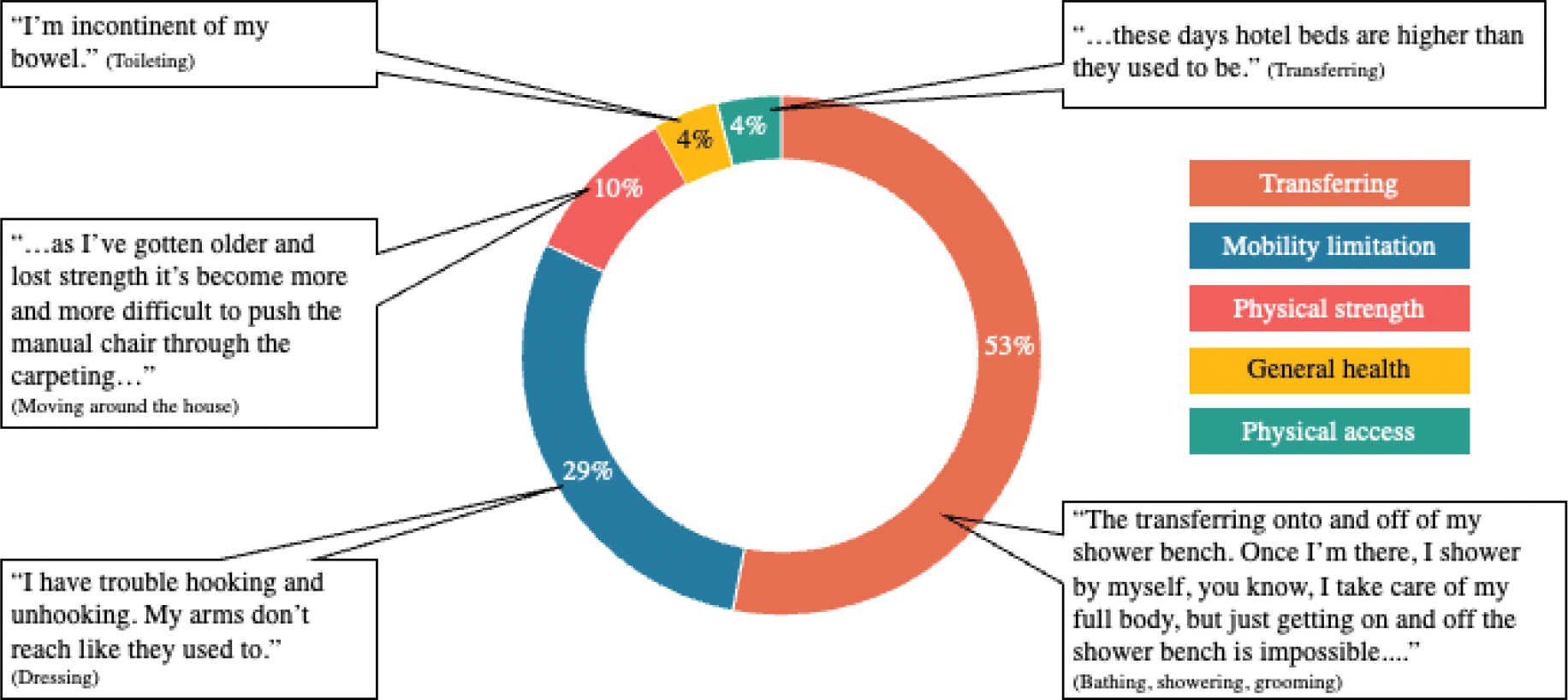
Challenges across basic daily activities.
Participants’ overall strategies to the basic daily activities challenges are presented in Figure 4. We noticed a majority of strategies belonged to the person-environment category (63% overall). Toileting activity had the highest percentage (78%) of person-environment strategies. A participant said, “Basically, I have the bathroom preset set up for handicap accessibility ... [my wife] helps me to pull down my trousers, takes the pedals off, and pushes me up to the toilet, and I sit on it backward.” This participant combined the utilization of handicapped toilet technology and assistance from others, which fell under the person-environment category.
Figure 4.
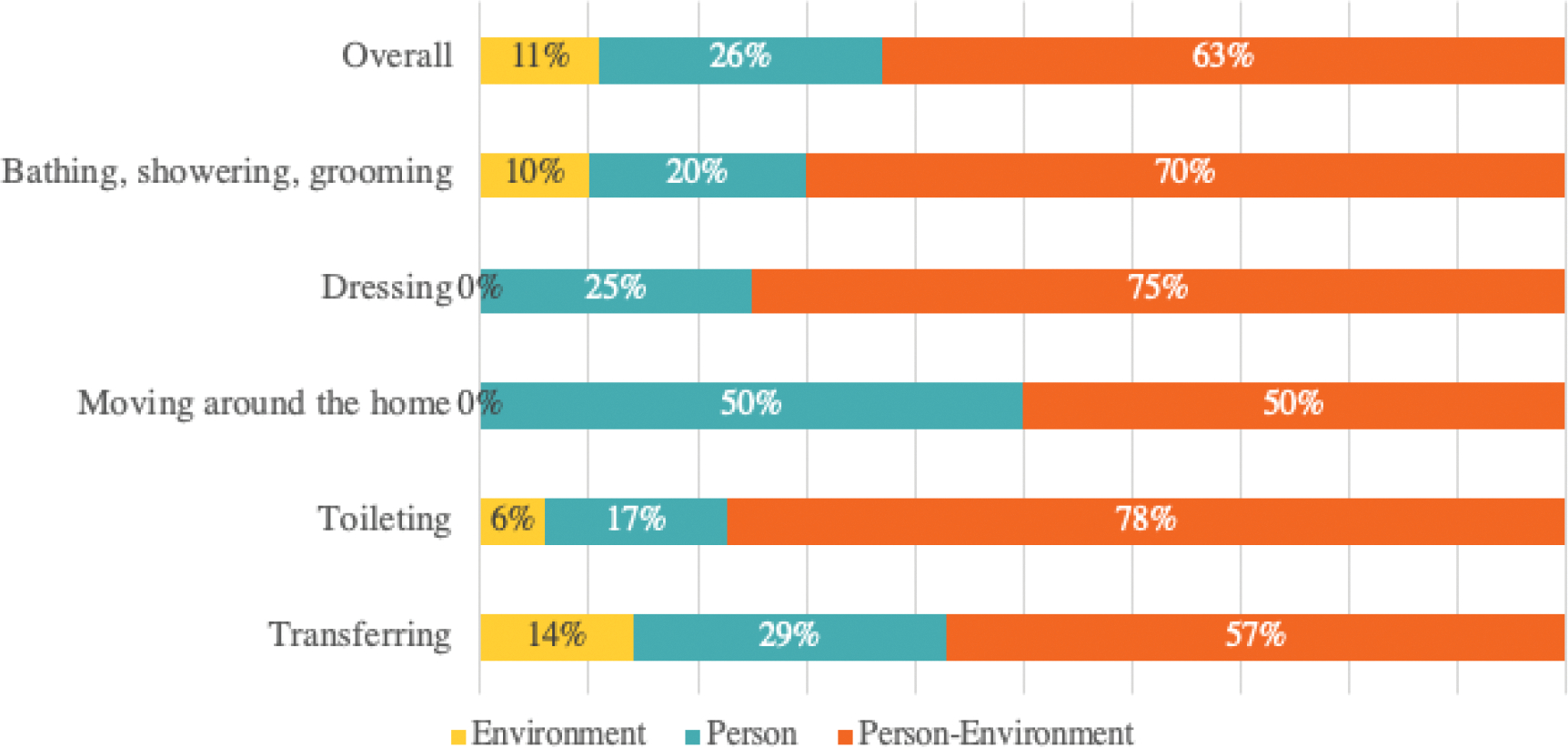
Strategies for basic daily activities.
The person category accounted for 26% of strategies for basic daily activities. Participants’ strategies included reliance on planning, patience, and perseverance. As an illustration, a participant took their time when doing the activities, “I am more cautious, and so I am more apt to go very slow.” Across the activities in this category, moving around the home had the highest percentage of person strategy (50%). A participant highlighted that they “Just pushing harder” to mobilize around their house despite their mobility challenges and the obstacles in their home environment.
We noticed that there was a lack of environment strategies to overcome the basic daily activities challenges. Only 11% of environment strategies, such as home modification and redesign of things were implemented. Two of the activities in this category; dressing and moving around the home had no strategy that involve environment strategies. Although not commonly reported, we had participants who made changes in their home environment to allow easier conduct of activities. To take a case in point, a wheelchair user participant said, “We took the [showers] doors off, and I used a shower curtain and a bath chair, and I can slide across.”
Activities Around the Home
Activities around the home category consisted of: (1) doing hobbies at home, (2) home repair and maintenance, and (3) housekeeping. The most frequently mentioned challenge in this category was mobility limitation (47%). As a result of their mobility limitation, participants had limited endurance to stay standing for a long time when vacuuming or mopping the floor, reaching high when putting detergent into the laundry machine or dusting high places, and using machines to do yard work. One participant expressed, “They have these new front-loading machines that are really high, and I can’t even see where I put the detergent and stuff in from sitting in my wheelchair.” We also discovered that home repair and maintenance activities often required participants to use stairs or ladders, which they could not do.
The second most challenging factor was the physical access in their home (31%). Oftentimes, the location, orientation, and the size of the tools or technology that participants used to do their hobbies, housekeeping, and home maintenance were not accessible. In fact, access to controllers of dishwashers and laundry machines, storage spaces, and windows was either too high, too low, or too far from their reach. The inaccessibility prevented them from conducting the activities successfully. As an illustration, laundry machines with control buttons on the top are difficult for wheelchair users. Similarly, outdoor spaces are also often inaccessible. A participant expressed, “I can’t do yard care in a wheelchair because the chair doesn’t go over grass. It basically gets onto the grass and gets stuck.”
Furthermore, the least common challenges were physical strength (11%) and general health (11%), wherein participants who had lost their strength and dexterity could not do activities that required heavy lifting, bending, or holding their body weight for an extended time. The overall distribution of activities around the home challenges is depicted in Figure 5.
Figure 5.
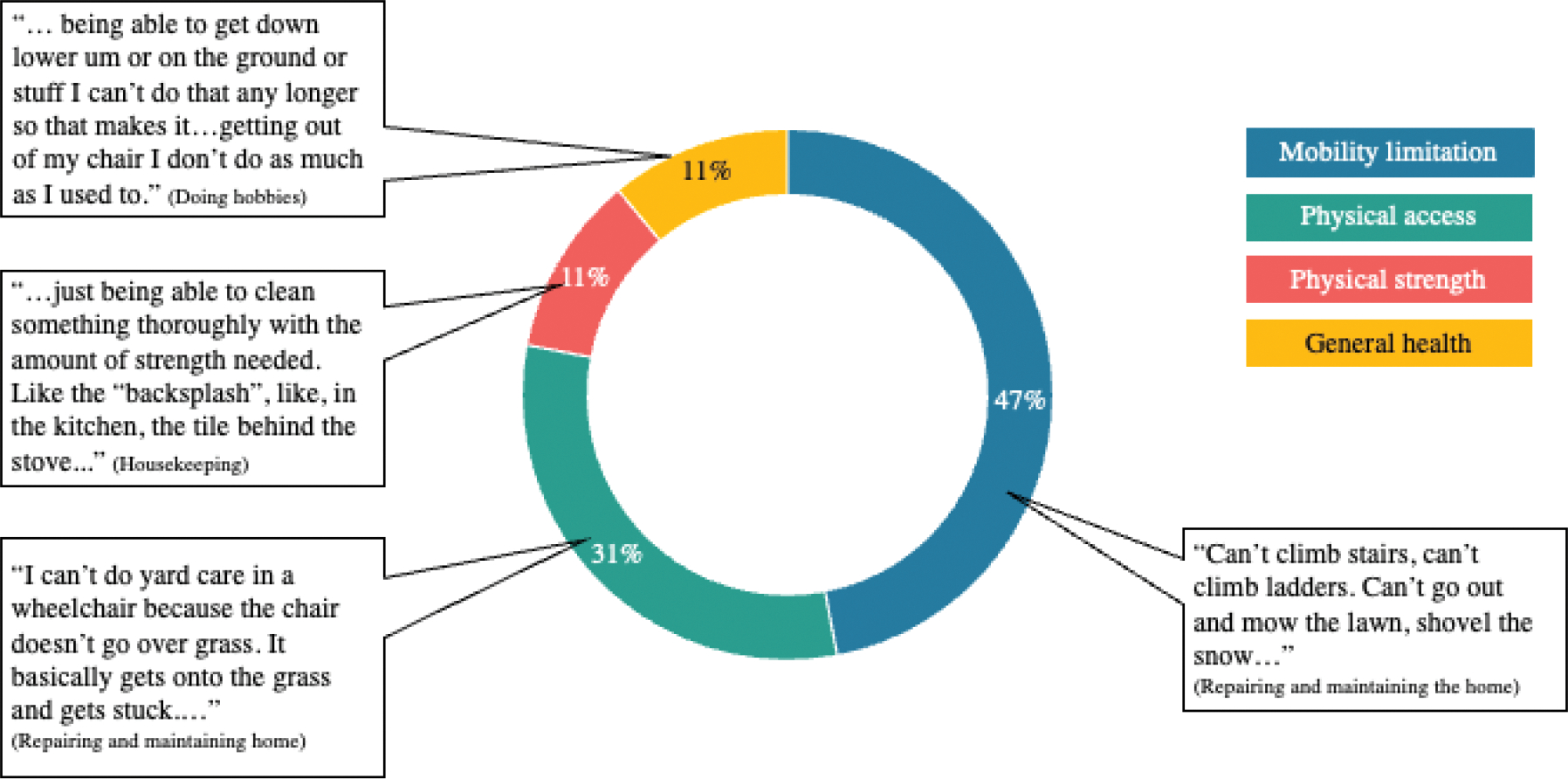
Challenges across activities around the home.
The overall strategies for the activities around the home challenges are presented in Figure 6. We noticed that most responses also involved person-environment strategies. Across the activities in this category, the person-environment category accounted for 65% of participants’ responses. Home repair and maintenance had the highest percentage (68%) of person-environment strategies. Participants’ strategies include hiring gardeners, plumbers, or handypersons to help them do clean, maintain, and repair their house. A participant said, “I have a lawn service that takes care of the lawn, they take care of the snow in the wintertime. I hire a handyman or have neighbors help with some of the routine maintenance requirements. And I hire professional services to take care of any other projects that are more involved, such as any kind of simple plumbing that requires professional help, or something that requires carpentry work.”
Figure 6.
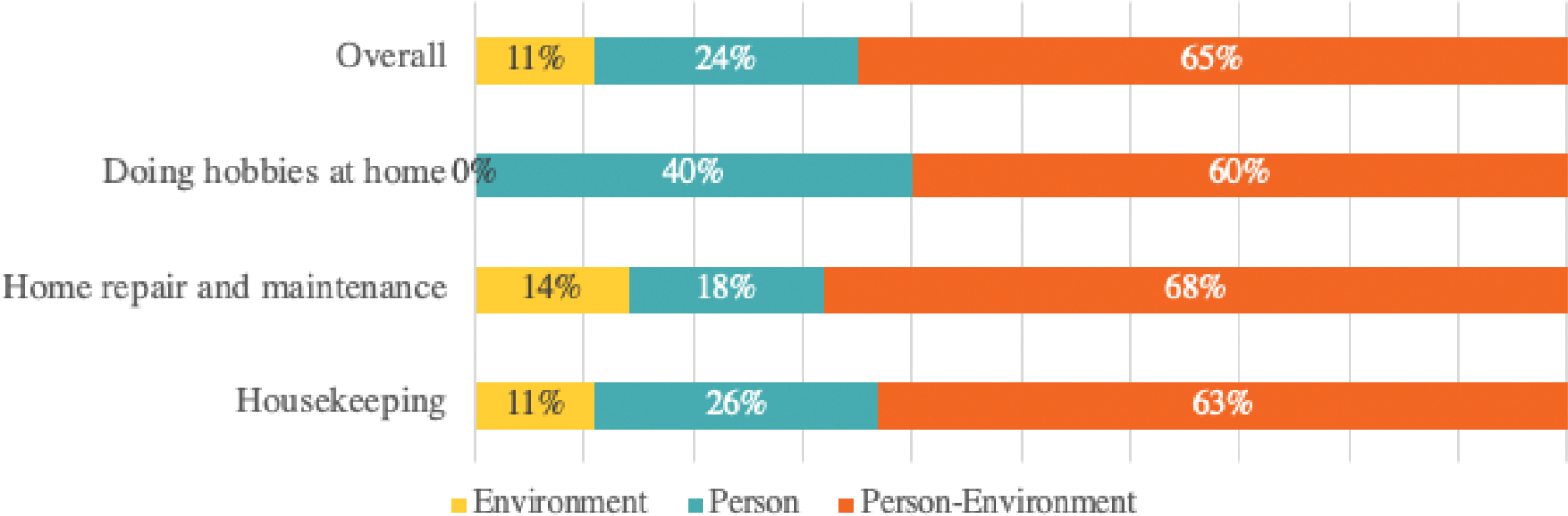
Strategies for activities around the home.
Strategies that were classified into the person category accounted for 24% of strategies for activities around the home overall challenges. Strategies included perseverance, planning, and reliance on previous familiarity and experience to overcome the challenge when doing hobbies, housekeeping, maintaining, and repairing homes. A participant expressed the importance of planning ahead when doing housekeeping, “Just think first. You are always thinking ahead. It is like playing a game; you have got to think at least three or four steps ahead. You do not just get to do stuff. You don’t.”
We discovered a lack of environment strategies, which only accounted for 11% of strategies to overcome activities around the home challenges. Doing hobbies at home had no strategies that involved modification or redesign of the home environment. As a result of less focus on doing the environmental change, they tended to look for assistance from other people to help them do the tasks. Nevertheless, we encountered some interesting redesign strategies. For example, a participant redesigned their wheelchair to help them carry things around, “I came up with something years ago. It’s a, people call it a luggage carrier or a forklift. It’s two little levers that I have mounted just above my feet in the front of the chair. I can flip those down and make a little pairing device there, so if I travel, I put my suitcase there, I can put the dog there in his little travel bag, and I carry things around the house in those little levers that come down.”
Managing Health
Managing health category consisted of: (1) caring for others and (2) managing diet and nutrition. The most frequently mentioned challenge in this category was general health conditions (61%). Participants reported that their general health condition limited their ability to care for others, such as when preparing meals. A participant expressed their inability to help their mother, “I can’t cook, I can’t make a meal…I could not feed her or get her to take her medicine or any of that.” The next most challenging factor was mobility limitations (27%), followed by physical strength (6%) and physical access (6%). Caring for others often needs strength and mobility, such as helping to carry luggage or other heavy things, helping to get out of the bed, toilet, or walking around the home. Participants’ mobility limitations and lack of physical strength became barriers to providing physical help for others. “I wouldn’t be able to physically help somebody, like help them walk, help them to get better, that kind of thing,” said one participant. Lastly, physical access challenges impacted participants’ ability to access important spaces, such as the kitchen, if they wanted to meal prep for themselves and others. The overall distribution of managing health activity challenges is depicted in Figure 7.
Figure 7.
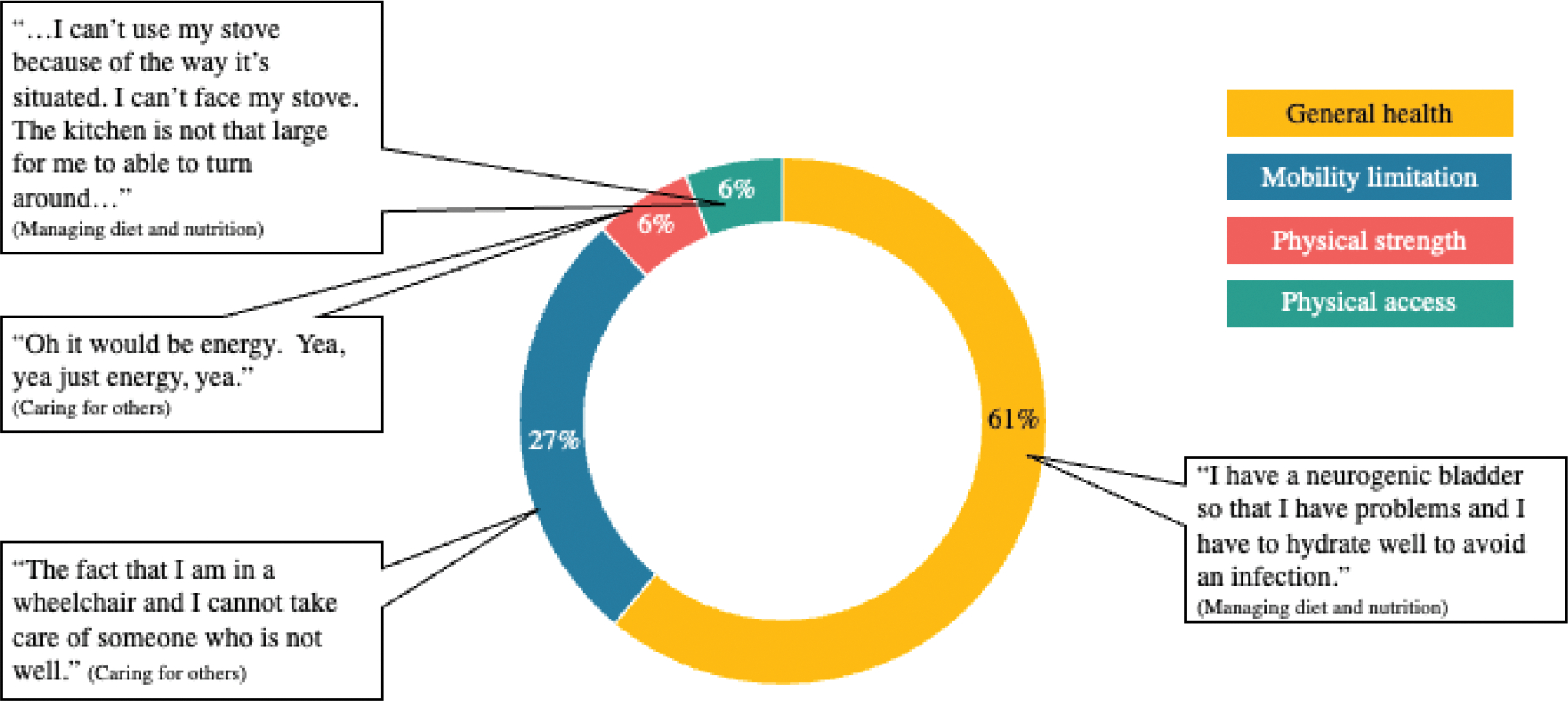
Challenges across managing health activities.
The overall strategies for managing health activities challenges are presented in Figure 8. Most strategies were in the person-environment category (68%). Participants relied a lot on getting assistance from other people, such as family members, friends, or neighbors. A participant said, “None of my family live near me, but I’ve become very friendly with some neighbors. I wouldn’t hesitate to ask one of them to help. And they’d be very happy to do so. You know people are very accommodating for the most part.” Besides, tools and technology were also commonly utilized to care for others. Basket and rolling carts were examples of tools that participants used to carry things for the person they cared for. “…if they’re sick in bed and I have to bring them things, I have a rolling cart here at the house that I put things on, and then I can roll my cart with things on it that they need”, said one of the participants. Interestingly, we also found that participants utilized their mobility devices beyond their personal needs but used them as tools to help others. A participant expressed, “Well, I might use the lifting or standing part of the of my power chair to help me say grab my wife with one arm so I can help her get up...”.
Figure 8.
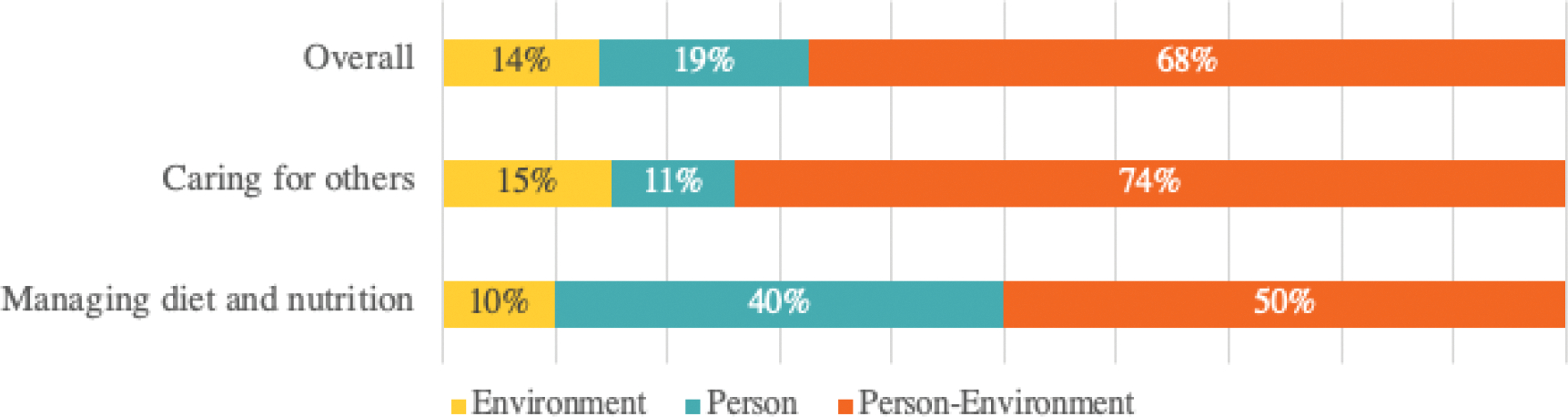
Strategies for managing health activities.
Furthermore, strategies in the person category accounted for 14% of response for managing health activities. Such strategies were reflected in participants’ reliance on learning, familiarity, planning when caring for others and managing diet and nutrition. A participant highlighted the importance of learning from multiple resources to find ways of overcoming their challenges, “I look online, I do a lot of reading, you know. I’ll take a webinar, you know, that kind of thing.” Perseverance was also very important, “…I will try to do the best that I can, which is not always the best, but I try to do the best that I can”, said one of the participants. We also found that participants were aware and familiar with what they can and cannot do, so they would not do things beyond their ability. A participant said, “…I try to stay away from stuff that’s going to be too heavy for me to use, like making sure I’m careful with the pot size and things like that. Because if I can’t handle picking it up and getting it from one area to another, I know not to deal with it. And then sometimes, I just don’t have the energy to make the meal. So, I have plenty of sandwiches and eat frozen food.”
With regard to environment strategies, there were only 14% of strategies to overcome the managing health challenges. Nevertheless, we discovered several interesting redesigns or unconventional uses of things. One participant utilized their wheelchair as a tool to help others, “If someone was limping I could say -Well here hold on to the back of my chair, and I’ll help you-, or if somebody just needed a short little ride I could just -sit on my lap, I’ll get you there-.” Another participant said that their modified wheelchair that help them carry heavy things, “…my little carrying device. I can move actually very large, I move furniture on the front of my chair. I could figure a way and I had to move a small bookcase one time and I didn’t want to unload all the books. I put a rope around and I just kept pulling a little bit a little bit a little bit until I got it where it needed to be. You know, each challenge comes along and you try and figure it out.” Although limited, some of the redesign examples that participants shared illustrated the possibility of environment strategies to be implemented further beyond the modification of mobility devices.
Themes across Activity Categories
The distribution of activity challenges differed across three activity categories (Figure 9), whereas the strategies were quite similar (Figure 10). In the basic daily activities category, transferring was the most frequent challenge. Consider toileting and moving around the home. These activities often require participants to move between two objects with different heights, especially when transferring from a lower to a higher platform. For the next activity category, activities around the home, mobility limitations were the most frequent challenge. Mobility limitations related to gross motor movement, fine motor movement, and balance (Rogers et al., 1998). These limitations often preclude participants when housekeeping, repairing, and maintaining their homes. In the managing health category, we found that participants’ general health conditions, such as chronic disease and other health problems, were the dominating barrier to managing their diet and nutrition or providing care for others. Such varied challenges across activity categories illustrated the wide range of barriers that could prevent successful activity conduct in the home environments.
Figure 9.
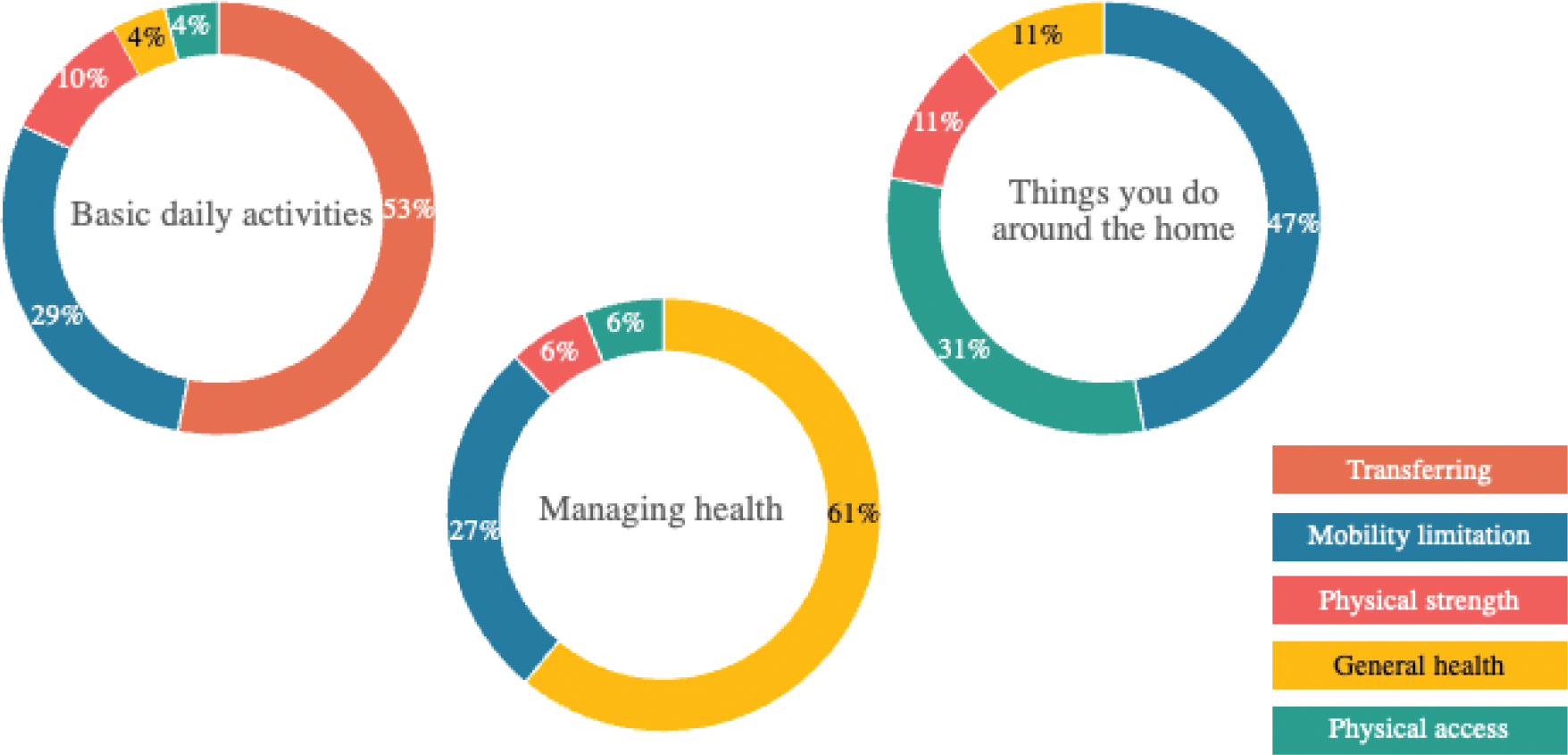
Challenges across categories.
Figure 10.
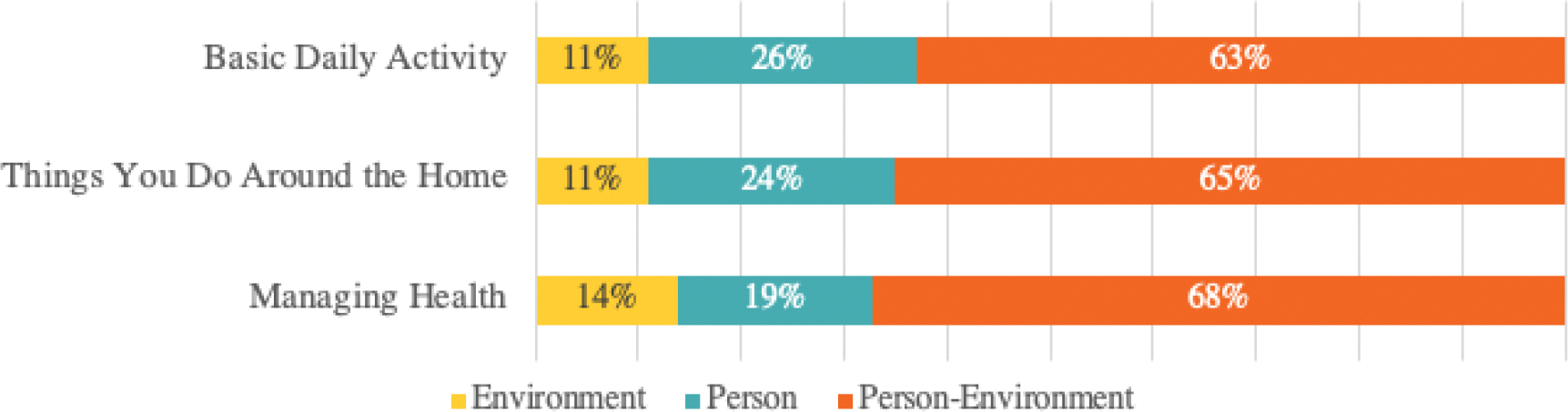
Strategies across categories.
Interestingly, despite the diverse activity challenges, the patterns of participants’ strategies were similar. Strategies to overcome the various activity challenges at home were dominated by the person-environment category. This category included strategies that used tools, technology, and assistance from others. The utilization of tools and technology was quite common to overcome the transferring challenge in the basic daily activity category. For example, participants used transfer boards and grab bars when showering, bathing, or toileting. For the activities around the home, participants frequently got assistance from others. They hired gardeners, plumbers, and handymen to help them with home repair, maintenance, and housekeeping activities. Likewise, in managing health activities, we observed the combination of tools and technology and getting assistance from others to overcome challenges to manage their diet and nutrition and provide care for others.
Overall, there was a lack of focus on environment strategies, especially regarding home modifications. Out of 60 participants in this study, only six participants reported that they conducted home modification in response to their activity challenges. Among then, 67% of them were female and 83% of them had bachelor’s degree or higher. All of participants who modified their home to better support their everyday activities had yearly household income of $50,000 or more. Higher educational background and income may be associated with the likelihood of conducting home modification, due to the financial expense. Across the categories, less than 15% of strategies were tied to the built environmental change. The most common type of modification was the transformation of participants’ bathrooms to be wheelchair accessible. Examples included changing to ADA accessible toilet seat, adding a shower bench, and grab bars to the bathroom.
Discussion and Conclusion
Challenges
We found that the challenges to conducting everyday activities among older adults with long-term mobility disabilities were dominated by their mobility, physical strength, and general health limitations. These findings are expected, considering that participants live with long-term mobility disabilities and possibly age-related diseases. In addition to their internal capacities, the physical access and transferring barriers in the home environment also created activity challenges. In other words, physical limitations and accessibility to places were frequent obstacles to conducting successful activities (Koon et al., 2020). Nahemow and Lawton (1973) illustrated this as the interaction between human competence and environmental press on the Ecological Theory of Adaptation and Aging (see Figure 1). Lack of competence to complete tasks due to primary disability and other age-related challenges and environmental barriers in the home environment resulted in difficulty doing various everyday activities. Such ‘activity limitations’ impact individuals’ affect and adaptive behavior (Nahemow & Lawton, 1973; Sanford, 2012). Similar findings were described by Silverglow and colleagues (2021) who highlighted the interactions between physical features of the home environment and older adults that are mutually affecting each other. To summarize, the challenges to conduct everyday activities are influenced by human competence, the condition of the built environment, and the interaction between the two.
Strategies
The strategies to respond to activity challenges were dominated by the person-environment strategies, which involved things beyond the individuals themselves and the built environment. The second-most-common strategies were person strategies, followed by environment strategies as the least common. Person-environment strategies include reliance on tools and technology, getting assistance from others, or implementing their previous or other person’s strategies. Assistance from others remained in high demand for older adults with long-term mobility disabilities (Koon et al., 2020). The assistance was provided by relatives, friends, neighbors, and even professionals, especially for activities with less privacy, such as housekeeping and yard work. While having someone to rely on can improve older adults’ feeling of safety (Pettersson et al., 2020), one should also consider ways to balance the help and remain to have control of their lives (Silverglow et al., 2021).
Although we discovered that person-environment strategies could facilitate participants in conducting their activities at home successfully, other strategies should be explored to maintain older adults’ independence. We noticed that there were very few strategies tied to the built environment. Nevertheless, the built environment could greatly contribute to minimizing the presence of challenges in the first place, especially when designers are aware of the potential challenges that older adults with mobility disabilities may face in their everyday life. A study by Petersson et al. (2008) showed that people aging with disabilities experienced reduced difficulty and increased safety after they modified their home environments, especially for transferring and self-care activities conducted in the bathroom.
Home Environment Design Recommendations for Maintaining Independence of Older Adults with Long-term Mobility Disabilities
Incorporating the environmental and behavioral assessment to understand the person-environment dynamic of aging in place is important to be the basis of supportive home design for older adults who are aging with disabilities (Mitzner et al., 2018). From participants’ experiences, we learned that some environmental barriers could be eliminated to support their everyday activities. Therefore, we propose the following design considerations that are mapped upon the overarching challenges that we identified in this study:
-
Transferring
Maintaining similar heights of beds/chairs/toilet
Adjustable heights of platforms
Handrails or grab bars in strategic places
Built-in (expandable) transfer board
-
Changing position (laying – sitting – standing)
Bed rails
Chairs with armrests
Sturdy furniture around critical locations
-
Reaching
Storing frequently used things on the easy-to-reach height
Storage spaces that can be movable (up/down) to help bring things up/down
Provide tools (with feasible and accessible storage) that can be used to help reach things
-
Maintaining endurance
Minimizing the use of carpet
Minimizing changes of level
Resting/pause space
-
Controlling
Putting appliances on the easy-to-reach height
Appliances with controls in the front
Allow remote control of appliances
Home modifications positively contribute to aging in place (Hwang et al., 2011). These considerations can be implemented as minor or major home modifications, depending on the needs and abilities of individuals. Modifications can also be anticipated by preparing the structure, spatial configuration, and flexibility of the home when it was initially built. Therefore, when built environmental support is needed to complement other response strategies, it will not require big and costly renovation. In fact, having a home environment that can support people living independently is generally less expensive than residential care (Sixsmith & Sixsmith, 2008).
In conclusion, this study has shown that the home activity challenges that people aging with mobility disabilities encounter are impacted by their internal capacities and the built environmental press. Older adults have managed to find strategies to face the challenges, utilizing the resources within themselves (i.e., perseverance, patience, planning), in the built environment (i.e., redesigning), and getting help from others or using tools and technology. Although the built environment created many challenges, the strategies used to modify the built environment were less frequent. As such, this creates an opportunity for designers to propose home modification strategies to help alleviate the challenges of older adults with long-term mobility disabilities. Awareness about the potential changes and challenges in older adults’ everyday activities engagement at home is critical for architects and interior designers, to ensure new residential settings are designed with flexibility and adaptability that allow minimum and low-cost modifications for accommodating older adults’ changing needs and capacities as they are advancing to old age.
This study focused on identifying activity-specific challenges and the response strategies to address the challenges. We did not collect detailed information on the residential building age, conditions, and modification regulations, as physical environmental condition was not the main goal of ACCESS. Nevertheless, we would expect that residential settings conditions and regulations may impact the possibility of implementing permanent physical modifications in participants’ home environments. The association between socio-demographics characteristics with the ways to deal with the challenges were not explored deeply, but we found that participants who conducted home modification have higher education level and income. We would expect that people with lower income, education, and minority groups would be less likely to have resources to make home modification that can be costly. Future studies should explore why modification of the built environment is less preferred to reduce barriers in their home. Although older adults with long-term mobility disabilities can persevere in facing their disability and health challenges through technology and social support, needs for customizable support through home modifications is an important factor to promoting older adults’ independence at home (Remillard et al., 2019). Architects and interior designers can support older adults to overcome their challenges to age in place through designing home environments that are appropriate and suitable for their changing needs.
Acknowledgements
The authors would like to thank Maurita Harris, Lyndsie Koon, and Elena Remillard for their contributions on the project.
Funding
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research [NIDILRR grant number 90REGE0006–01-00] under the auspices of the Rehabilitation and Engineering Research Center on Technologies to Support Aging-in-Place for People with Long-Term Disabilities (TechSAge; www.TechAgeRERC.org). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS).
Footnotes
Widya Ramadhani is a PhD candidate in architecture at the University of Illinois Urbana-Champaign. Her research focuses on the person-environment transaction to negotiate the decrease of older adult’s physical and cognitive ability, particularly in residential environments. Her dissertation research is on the food-related activities among older women to understand the personal and built environmental adaptation for independence in later life. She received her B.Arch from Universitas Indonesia in 2014, and her M.Arch from the University of Illinois-Urbana Champaign in 2017.
Wendy A. Rogers, Ph.D., is Shahid and Ann Carlson Khan Professor of Applied Health Sciences at the University of Illinois Urbana-Champaign. Her primary appointment is in the Department of Kinesiology and Community Health. She has an appointment in Educational Psychology and is affiliate of the Beckman Institute, Illinois Informatics Institute, Center for Social and Behavioral Science, and the Discovery Partners Institute. She received her B.A. from the University of Massachusetts - Dartmouth, and her M.S. (1989) and Ph.D. (1991) from the Georgia Institute of Technology. She is a Certified Human Factors Professional (BCPE Certificate #1539).
Disclosure statement
The authors report there are no competing interests to declare.
References
- Disability glossary. (2021, November 21). U.S. Census Bureau. https://www.census.gov/topics/health/disability/about/glossary.html#par_textimage_952582087
- Erickson W, Lee C, & von Schrader S (2020). 2018 Disability Statistics Status Report: United States. Cornell University Yang-Tan Institute on Employment and Disability (YTI). https://www.disabilitystatistics.org/ [Google Scholar]
- Hwang E, Cummings L, Sixsmith A, & Sixsmith J (2011). Impacts of Home Modifications on Aging-in-Place. Journal of Housing For the Elderly, 25(3), 246–257. 10.1080/02763893.2011.595611 [DOI] [Google Scholar]
- Koon LM, Remillard ET, Hartley JQ, Harris MT, Mitzner TL, & Rogers WA (2019). Coding scheme for the aging concerns, challenges, and everyday solution strategies (ACCESS) study: Adults aging with mobility or vision disabilities (TechSAge-TR-1902). Rehabilitation Engineering Research Center of Technologies to Support Aging-in-Place for People with Long-Term Disabilities. [Google Scholar]
- Koon LM, Remillard ET, Mitzner TL, & Rogers WA (2020). Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) for adults aging with a long-term mobility disability. Disability and Health Journal, 13(4), 100936. 10.1016/j.dhjo.2020.100936 [DOI] [PubMed] [Google Scholar]
- LaPlante MP (2014). Key goals and indicators for successful aging of adults with early-onset disability. Disability and Health Journal, 7(1), S44–S50. 10.1016/j.dhjo.2013.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP (1990). Aging and Performance of Home Tasks. Human Factors, 32(5), 527–536. 10.1177/001872089003200503 [DOI] [PubMed] [Google Scholar]
- Lee M (2008). Aging in place: A contemporary social phenomenon [Dissertation]. https://ir.library.oregonstate.edu/concern/graduate_thesis_or_dissertations/g158bk98s
- Mitzner TL, Sanford JA, & Rogers WA (2018). Closing the capacity-ability gap: Using technology to support aging with disability. Innovation in Aging, 2(1). 10.1093/geroni/igy008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molton IR, & Yorkston KM (2016). Growing Older With a Physical Disability: A Special Application of the Successful Aging Paradigm: Table 1. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, gbw122. 10.1093/geronb/gbw122 [DOI] [PubMed] [Google Scholar]
- Nahemow L, & Lawton MP (1973). Toward an ecological theory of adaptation and aging. Environmental Design Research, 1, 24–32. [Google Scholar]
- Petersson I, Lilja M, Hammel J, & Kottorp A (2008). Impact of home modification services on ability in everyday life for people ageing with disabilities. Journal of Rehabilitation Medicine, 40(4), 253–260. 10.2340/16501977-0160 [DOI] [PubMed] [Google Scholar]
- Pettersson C, Malmqvist I, Gromark S, & Wijk H (2020). Enablers and Barriers in the Physical Environment of Care for Older People in Ordinary Housing: A Scoping Review. Journal of Aging and Environment, 34(3), 332–350. 10.1080/02763893.2019.1683671 [DOI] [Google Scholar]
- Ramadhani WA, & Rogers WA (2021). Aging in place at home: Understanding personal and environmental activity challenges and response strategies of older adults with long-term mobility disabilities (TechSAge-TR-2105). Rehabilitation Engineering Research Center on Technologies to Support Aging-in-Place for People with Long-Term Disabilities. [Google Scholar]
- Remillard ET, Mitzner TL, Singleton JL, Koon LM, & Rogers WA (2018). Developing the Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) Study [TechSAge-TR-1801]. Rehabilitation Engineering Research Center on Technologies to Support Successful Aging with Disability. [Google Scholar]
- Remillard ET, Fausset CB, & Fain WB (2019). Aging with long-term mobility impairment: Maintaining activities of daily living via selection, optimization, and compensation. The Gerontologist, 59(3), 559–569. 10.1093/geront/gnx186 [DOI] [PubMed] [Google Scholar]
- Roberts AW, Ogunwole SU, Blakeslee L, & Rabe MA (2018). The Population 65 Years and Older in the United States: 2016: American Community Survey Reports (ACS-38; American Community Survey Reports). U.S. Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2018/acs/ACS-38.pdf [Google Scholar]
- Rogers WA, Meyer B, Walker N, & Fisk AD (1998). Functional Limitations to Daily Living Tasks in the Aged: A Focus Group Analysis. Human Factors, 40(1), 111–125. 10.1518/001872098779480613 [DOI] [PubMed] [Google Scholar]
- Rogers WA, Ramadhani WA, & Harris MT (2020). Defining Aging in Place: The Intersectionality of Space, Person, and Time. Innovation in Aging, 4(4), igaa036. 10.1093/geroni/igaa036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford JA (2012). Universal design as a rehabilitation strategy: Design for the ages. Springer Pub. [Google Scholar]
- Scharlach AE, & Moore KD (2016). Aging in Place. In Bengtson VL, Settersten RA, Kennedy BK, Morrow-Howell N, & Smith J (Eds.), Handbook of theories of aging (Third edition, pp. 407–425). Springer Publishing Company, LLC. [Google Scholar]
- Silverglow A, Lidèn E, Berglund H, Johansson L, & Wijk H (2021). What constitutes feeling safe at home? A qualitative interview study with frail older people receiving home care. Nursing Open, 8(1), 191–199. 10.1002/nop2.618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sixsmith A, & Sixsmith J (2008). Ageing in place in the United Kingdom. Ageing International, 32(3), 219–235. 10.1007/s12126-008-9019-y [DOI] [Google Scholar]
- Taylor DM (2018). Americans With Disabilities: 2014 (Current Population Reports, pp. P70–152). U.S. Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2018/demo/p70-152.pdf [Google Scholar]


