Abstract
Introduction
To address the challenges of rapidly changing healthcare, governments and health services are increasingly emphasising healthcare delivery models that are flexible, person centred, cost-effective and integrate hospital services more closely with primary healthcare and social services. In addition, such models increasingly embed consumer codesign, integration of services, and leverage digital technologies such as telehealth and sophisticated medical records systems.
Objectives
This paper provides a study protocol to describe a method to elicit consumer and healthcare provider needs and expectations for the development of innovative care models.
Methods and analysis
A literature review identified six key models of care, supported by a common theme of consumer-focused care, along with the international evidence supporting the efficacy of these models. A mixed-methods study of the needs and expectations of consumer members and health providers who reside or work in the area of a new hospital catchment will be undertaken. They will complete a community-specific and provider-specific, short demographic questionnaire (delivered during the recruitment process) and be assigned to facilitator-coordinated online workshops comprising small focus groups. Follow-up interviews will be offered. Culturally and linguistically diverse members and Aboriginal and Torres Strait Islander Elders and their communities will also be consulted. Data will be analysed thematically (qualitative) and statistically (quantitative), and findings synthesised using a triangulated approach.
Ethics and dissemination
The results will be actively disseminated through peer-reviewed journals, conference presentations and in a report to stakeholders. This study was reviewed and approved by the relevant Ethics Committee in New South Wales, Australia.
Keywords: organisation of health services, organisational development, protocols & guidelines
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The study will be the first of its kind to identify the key evidence-based, innovative models of healthcare, considering the benefits and implementation considerations for each model, as perceived by consumers and healthcare providers.
The study design is developed in collaboration with the local health district where the health facility will be located.
A key strength of the study is the use of mixed-methods and the triangulation of data from multiple sources.
A key limitation of the study is that the structure of workshops focused on specific scenarios which may not be generalisable.
Background
Around the world, the delivery of quality hospital care is transforming in response to the availability of new and enhanced technologies and increasing demand for care.1 Challenges to extant healthcare systems include an increase in the proportion of older adults in the population2–4 that will redirect the focus of health towards long-term and chronic care.3 Increased demand on the healthcare system comes from multiple sources, including higher prevalence of chronic diseases such as obesity, kidney failure5 and cognitive decline.3 The shift to patient-centred healthcare models3 will also have resource implications while aiming for improvements in patient and staff satisfaction and quality of care.6 To address the growing challenges globally, health services and governments are experimenting with more cost-effective care alternatives often delivered outside hospitals walls,7 prioritising greater consumer engagement8 9 and investing in digitised care services.10 Digital services have the potential to support more personalised care, integrated with existing models and delivered remotely (eg, telemedicine). Additionally, advanced technologies such as robotics, artificial intelligence (AI) and big data analytics may provide more seamless and efficient care.4
In 2018, Braithwaite and colleagues identified key trends shaping the health systems of the future: global demographic dynamics, work in creating sustainable health systems, evolving technologies such as genomics and AI, and new models of care. Please insert reference (3) Braithwaite et al. New models of care are emerging to meet new circumstances. For example, the COVID-19 global health pandemic in 2020 acted as a catalyst or trigger for change (eg, rapid adoption of telehealth) that have been called for previously by those who suffer from chronic conditions.11 E-health, telehealth and virtual care models allowed patients to remain socially distant rather than having physical contact with the community and health services, simultaneously reducing the risk of the virus spreading among patients and healthcare providers.12 These innovative models take a novel approach to provide high-quality and safe care in and out of hospital settings.13
In Australia, the New South Wales (NSW) government announced funding for a new health facility at Rouse Hill. The Western Sydney Local Health District (LHD) is planning the new health facility and is seeking innovative ways of delivering care that are more accessible, efficient and effective for healthcare providers, funders and the population. In consultation with our research team, it was believed that there was an opportunity to create a different kind of facility—a modern and digitally enabled capability. Seeking views from consumers and providers will ensure that the way the facility provides services is deeply connected to community needs. These include physical, health and psychosocial needs; rapid access to care for consumers; and adequate resources and infrastructure for providers.
The goal of this project is to provide a research-based approach to develop an innovative health facility and health service; one that delivers a high-quality care solution for the community rather than simply establishing more hospital beds, departments, units and wards. Realising this vision will have far-reaching implications for the design and delivery of health services in the future. But to develop any new model for integrating community and hospital acute care and support services, we need to turn to the community and healthcare providers to understand their expectations and the healthcare needs that may be met by innovative models of care. While we are gaining data to inform the construction and design of a ‘hospital’, we use the term ‘health facility’ to reflect blue sky thinking and avoid being constrained by language that implies a large conglomeration of buildings and beds.
Identifying evidence-based models of care
Before eliciting consumers and providers’ needs and expectations, we needed to assess the evidence to identify candidate models of care. We therefore undertook a grey literature review to identify potential models of care, followed by an academic review of the international evidence supporting the efficacy of these models.
The grey literature review involved an advanced search using Google and included websites such as WHO and the Organisation for Economic Co-operation and Development using search terms such as ‘future hospital’. Two reviewers completed a title and abstract screen and three reviewed the full-text documents. Eighty-five documents were included, comprising 55 reports, 17 online newspaper articles, 10 articles or bulletins from organisation websites, 2 online articles and an opinion piece. From this review, six key themes were deductively determined that were used to group innovative models of healthcare. Consumer-focused care, where during planning, delivery and evaluation, consumers, carers and families are placed at the centre of care, was a common theme that underpinned the other six models, for example, individualised self-management support in early chronic kidney disease transition of care plan from hospital to home involving a multidisciplinary team.5 As such, only six models will be presented, each incorporating consumer-focused care (see table 1). Benefits, drawbacks and past implementation of the models were also identified.
Table 1.
Six evidence-based innovative models of care
| Model | Description | Example |
| Ambulatory care and diagnostic hospitals | Non-admitted services, where patient care does not involve an overnight stay and usually involves diagnosis and treatment on the same day. | Same-day joint arthroplasty21 |
| Digital hospitals | Hospitals that make extensive use of new technologies to provide streamlined care, improve patient safety and care quality and improve overall care cost-effectiveness. | Machine learning algorithm for prediction of post-total hip arthroplasty complications22 |
| Hospital in the home | Some or all of patient care and consultation which is typically delivered in the hospital settings is delivered to patients in their own home. | Early discharge hospital at home care for chronic obstructive airway disease managed by a community service23 |
| Integrated care | Multidimensional needs of the patient are delivered in a coordinated manner by an interdisciplinary team or network of healthcare professionals. | Orthogeriatric fracture service24 |
| Virtual care | Patient care and consultation delivered through telephone or video communication. | Telehealth management in patients with heart failure25 |
| Specialist hospitals and population-specific care units | Specialist hospitals provide selective care services for targeted patient groups. Population-specific care units are pathways within general hospitals dedicated to treatment of specific conditions. | Comprehensive cancer centres26 |
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses was used to guide the academic literature review to extract the evidence-based support for the models of care identified in the grey literature.14 Search strings chosen from prevalence data of the focal community in the context of the models were applied to three academic databases (PsycINFO, Ovid MEDLINE and CINAHL). For example, ‘virtual hospital’ AND ‘cardiac arrest’. Sixteen reviewers (eight pairs) completed a title and abstract screen and subsequently reviewed the full-text documents. Given the large numbers of papers resulting from the searches (ie, over 200 000 results), the researchers confined the searches to review papers only. Sixty-one peer-reviewed English language review studies with human subjects, dated 2016–2021, met the criteria for inclusion. This review will be reported separately.
Methods
Study aim
The study aims to elicit health consumers and healthcare providers’ needs drawn from the local community and expectations of a new health facility, and how these needs may be met through the delivery of innovative models of care.
Study design
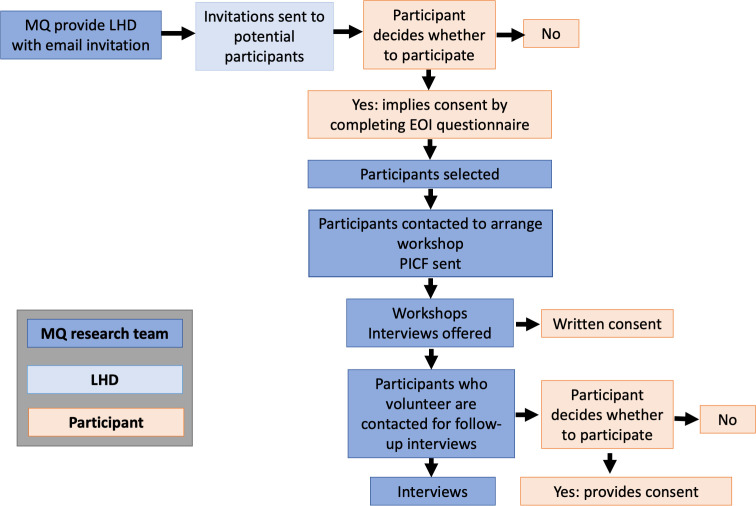
We will conduct a mixed-methods study of consumer and provider needs and expectations in relation to innovative models of care delivery for a new health facility. As illustrated in figure 1, the design comprises collections of consumer and provider data via a short expression of interest (EOI) questionnaire comprising demographic information (as part of the recruitment process), facilitator-coordinated workshops and supplementary interviews. Data collection will occur in a sequential manner, where results from the EOI questionnaire will inform workshop design. In addition, interview design and recruitment will be informed by the learnings from the workshops. Together, these methods of data collection will facilitate a varied and dynamic exploration of community and provider needs and expectations for innovative models of healthcare (see figure 1).
Figure 1.
Data collection points over time for consumer and provider groups.
Study setting
The project will be conducted online and in person. Specifically, the recruitment demographic questionnaire will be hosted and completed online. The face-to-face workshops will be held at public metropolitan hospitals and community centres in NSW, Australia. Participants will be provided with options to attend workshops during or outside of working hours. For face-to-face workshops, we will follow all current COVID-19 guidelines at the time of data collection (eg, social distancing, wearing of masks). In addition, the meeting format will be adjustable to being video enabled to respond to any face-to-face restrictions in place associated with the COVID-19 pandemic. Supplementary interviews with interested participants identified in the workshops will be conducted via an online platform such as Zoom or over the telephone for participant convenience.
The catchment area where a new health facility is currently being planned comprises a land area of almost 500 km2 and a population estimated in 2019 to be 300 000 residents. Between the 2006 and 2016 population censuses, the catchment experienced a population growth rate of 29% and this growth rate was predicted to rise when assessed using the 2021 census data.15 16 The 2016 census reported that adults aged 35–44 years and school-age children aged 5–9 years were the largest age groups, 37% of the population was born outside Australia and 0.9% identified as Aboriginal and/or Torres Strait Islander.17 As such, the workshops will include participants who self-identify with these diverse populations.
Procedures
Recruitment
Consumer members will include residents and patient representatives within the new health facility catchment (49 suburbs) as defined by the LHD’s planning team on 16 July 2021. The participants will be recruited through the LHD’s network and connections via email, postings in local newspapers and through Facebook invitations. For providers, emails will be sent by the LHD to potential participating providers such as healthcare professionals and support staff via their established connections. These connections include, but are not limited to, consumer networks, LHD community newsletters, migrant resources centres, the Primary Health Network and the Youth Advisory Council. To reach potential consumer participants who may not have access to email or the internet, the invitation will also be posted in local newspapers and advertised as flyers at LHD hospitals. For providers, emails will be distributed via the LHD’s broadcast system, the Primary Health Network and from the chief executive officer.
As 37% of the consumers are from culturally and linguistically diverse (CALD) backgrounds, non-English-speaking participants will be invited to participate in the study, aided by bilingual interpreters from the LHD. The research materials comprising the invitation, EOI questionnaire, workshop and interview scripts will be translated into the five most prevalent non-English languages in the community—Hindi, Punjabi, Mandarin, Korean and Arabic.
For those accessing the research invitation electronically (via email or Facebook advertisements), the invitation will include a link to an online EOI questionnaire using REDCap electronic data capture tools.18 The questionnaire will collect demographic data including age, gender, location, ethnicity and contact information. The providers will be asked to indicate their role and specialty, and the consumers will be asked for pertinent health information such as whether they have a chronic health condition (online supplemental file 1). Responses to the questionnaire will be taken as implied consent for collection of the demographic information.
bmjopen-2021-059330supp001.pdf (85.5KB, pdf)
The provided contact information will be used to send the participant details about the location and time of the workshops (either via phone or email—as selected by the participant). For all participants who attend a workshop, we will ask for written informed consent prior to commencement of the workshop. Participants will be sent the participant information and consent form (PICF) prior to the workshop so that they can come prepared with questions for the research team. Once participants sign the consent form, the research staff will photocopy the PICF and provide a copy to each consenting participant. In the event of delivering the workshops online, a link will be sent to the participants for access to the PICF using REDCap tools.18
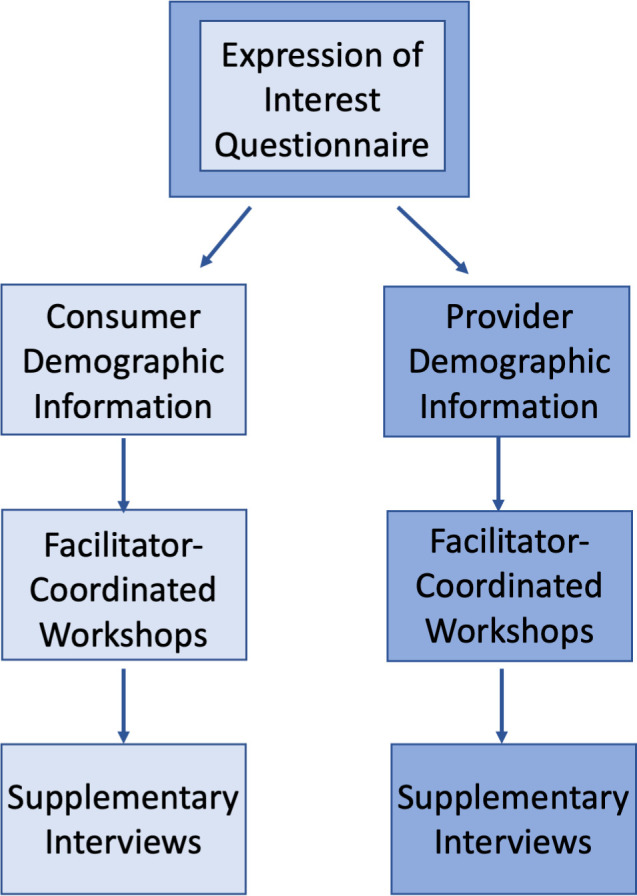
After each workshop, those who express interest in an optional follow-up interview will be contacted to confirm the findings. The PICF for the workshop informs participants that they may be contacted after the workshop to be invited to a follow-up interview. Figure 2 provides a map of the recruitment process for consumers and providers.
Figure 2.
Recruitment process map. MQ, Macquarie University; EOI, expression of interest; LHD, local health district; PICF, participant information and consent form;
Workshops
There will be a total of 12 workshops across two streams of six: one stream for health providers and another for consumer members. Two to four additional workshops will be held for CALD consumers and Aboriginal and Torres Strait Islander consumers. Each workshop has been designed to elicit responses to the seven models of care. To do this, we will divide participants into smaller parallel groups that each will examine three models of care in detail, rather than present all seven models and induce fatigue. The models have been counterbalanced across the eight workshops to ensure that the presentation and order of each model is balanced. There will be up to eight facilitators and scribes at each workshop (a facilitator and scribe per group). Where needed, some groups within the workshops will be supported by bilingual interpreters. The number of participants in each workshop group has been designed based on our collective research experience as an appropriate number for elicitation of the data we are seeking and is consistent with the number of participants in focus groups where people feel relatively comfortable speaking to others.19
The workshops will start with a short explanation by a research team lead, explaining that the purpose of the workshop is to capture the needs of the consumers or providers and their perspectives on innovative models of care delivery. They will then allocate the researchers and participants to the groups. Within each group, the researchers will take notes, facilitate discussion and ask probing questions. Audio-recording devices and researcher notes will be used to capture the content of discussions.
After a brief icebreaker activity, the researchers will then ask questions to probe the participants’ digital literacy (eg, ‘How comfortable are you using a smartphone/smartwatch/computer?’). These questions are included as two of the models of care presented (virtual care and digital hospitals) involve engagement with technology and understanding the level of participant digital literacy will be important for interpreting the findings. Workshop scenarios and questions have been designed around consumer-focused care and the six innovative models of care identified in the literature review in collaboration with a clinical subject matter expert and coauthor (KM) (table 1). The priority conditions used in the scenarios have been identified from the demographic data provided by the LHD as the most common burdens of disease in the new health facility catchment and are listed below:
Cardiac arrest, chest pain, acute myocardial infarction, congestive heart failure.
Fractures, knee replacement, hip replacement, joint replacement, abnormal gait, bone disease, osteoporosis.
Abdominal pain, pelvic pain, gastrointestinal pain.
Pneumonia, asthma, chronic obstructive pulmonary disease.
Postnatal depression.
Dialysis (haemodialysis, etc), kidney disease, end-stage kidney disease.
Scenarios will be presented to participants for each model of care (see table 2). Three of the six models along with the scenarios will be presented in each workshop in counterbalanced order to minimise biases (eg, 1 2 3, 4 5 6; 2 3 1, 5 6 4, etc).
Table 2.
Models of care and scenarios
| Model | Scenario |
| Ambulatory care and diagnostic hospitals | ‘Maria is a 45 year old woman who is able to walk unaided and travels to a centre for treatment 2–3 times per week (eg, renal dialysis in a shopping centre, or chemotherapy).’ |
| Digital hospital | ‘John is a 70-year-old man who has a heart condition that causes dizziness (eg, irregular heartbeat). As this places him at a high risk of falls, he has been admitted to hospital for monitoring. Beside his bed is a digital matt that detects and alerts the staff if he has had a fall.’ |
| Hospital in the home | ‘Jenny is a 35-year-old, single mother of three who developed a breast infection with an abscess following the birth of her baby. She was treated with intravenous antibiotics (on a drip) and a tube was placed into her breast to drain the infected fluid. After 24 hours, she returned home to her children and is provided wound care and support in her home from a visiting nurse.’ |
| Integrated care | ‘Steve is a 50-year-old man with Type II diabetes who is obese and smokes a packet of cigarettes a day. He is having trouble walking so visits his local Emergency Department where he sees a General Practitioner (GP), who has a practice in an office next to the Emergency Department. The GP diagnoses a foot ulcer and identifies that Steve requires a full review of his care. Steve will be looked after in hospital by a multidisciplinary team of healthcare professionals (eg, endocrinologist, ulcer team, nutritionist) using an electronic medical record system for communication.’ |
| Virtual care | ‘Ivy is a 40-year-old woman who developed chest pain along with an irregular heartbeat following a dental procedure. She visited the local Emergency Department where no abnormality was found and was discharged. As she was still concerned about a sudden heart attack, she was fitted with a digital heart monitor with chest leads that talked to an application on her smart watch. Ivy was shown how to indicate an unusual heart event using her watch. Anytime Ivy tagged an event, the information was sent to a healthcare professional at the moment it happened.’ |
| Specialist hospitals and population-specific care units | ‘Harrold is an 82-year-old man with mild dementia, who develops a urinary tract infection. He has been referred to a specialist dementia unit in a geriatric care ward at the local hospital. Harrold and his family are reassured that he will receive the highest level of evidence-based care for dementia from a specialised team of health professionals.’ |
Following the presentation of each scenario, we will ask general questions about the model’s strengths and weaknesses, usability and safety for themselves and people in their care. To understand patient needs, questions will be asked about how each model would work, with participants thinking about their own care, as well as the safety and risks. For providers, we will ask them about barriers and enablers from their own and their patients’ perspectives, for each model of care, and their anticipated needs when providing care in the new hospital. At the end of each workshop, the participants will be asked to indicate their preferred model of care via a poll. Example facilitator scripts for the consumer and provider groups are provided in online supplemental file 2.
bmjopen-2021-059330supp002.pdf (191.3KB, pdf)
Each workshop will be planned for a 2-hour duration with a 5 min break after the first hour. Each participant will be invited to participate in one workshop but will be offered a series of dates to choose from. Participants will not be paid for their participation but those who attend in person will be provided with refreshments.
Participants
The consumer workshops will include residents of the new health facility catchment area. Provider workshops will comprise health providers that provide care or are likely to provide care and stakeholders who make decisions about the provision of care such as LHD executives and administrators, for the catchment population. In the first wave of data collection, we will recruit 15–30 participants for each of the workshops (this estimation takes into consideration participant loss to follow-up). Six workshops will result in approximately 120 health providers and 120 consumer member participants (240 participants in total). However, the number of participants invited to each workshop may be influenced by government-mandated COVID-19 restrictions at the time of data collection. In a second wave, up to 40 non-English-speaking, CALD participants will be recruited with the support of the LHD’s Multicultural Health Team.
In parallel, there will be a third, but separate and aligned, wave of data collection to include consultation with Aboriginal and Torres Strait Islander Elders. Consultation with these community members will involve a formal process of consultation with Aboriginal liaison officers in the LHD to develop an Aboriginal Health Impact Statement and associated ethics proposal. This consultation will be conducted in person to ensure this is delivered in a culturally respectful manner as directed by the Aboriginal liaison officers in the LHD.
Inclusion criteria
All participants will be 18 or older and will either have English language competence (written and spoken) or interpreter-assisted non-English language (written and spoken), sufficient to provide verbal informed consent. The study is open to all community members, but we will also specifically seek to recruit participants representative of the six specific health conditions/services by targeting the recruitment of condition networks associated with these health conditions.
Those who currently provide care to those residing in the catchment for the new health facility, or who make decisions about the provision of care for those residing in the catchment, are eligible to participate. This will include general practitioners and other health providers such as community nurses and services, allied healthcare professionals, aged care facilities, community care organisations, the Primary Health Network, community care providers, the ambulance service and other identified stakeholders. The inclusion criteria are broad enough to capture any health provider in the LHD or new health facility catchment, but we will also target participants whose work relates to patients in the six specific listed conditions or services.
Interviews
Supplementary to the workshop, we will invite those participants who are key stakeholders but were unable to participate in the workshop, or those who indicate interest during the workshops to participate in semistructured interviews. The purpose of these interviews is to expand on areas of interest and verify the findings from the workshop data. The focus of the interviews will be driven by those who volunteer. For example, if a consumer has experience with a model (eg, hospital in the home for renal dialysis), one-on-one interviews will allow us to probe further into the specific barriers and enablers of the model while maintaining participant privacy. Interviews will be audio recorded and are expected to last approximately 45 min. The interview script commences with ‘For Model X, can you please elaborate on what you think is meant by the strengths/barriers/enablers/safety issues…’, and is deliberately open ended to allow the participants to freely express their views. The interview script is provided in online supplemental file 3.
bmjopen-2021-059330supp003.pdf (36.9KB, pdf)
Data collection
Participants’ demographic information (eg, age, gender) and health-relevant data will be collected through the EOI questionnaire. Consumers will be asked about their experiences using acute, chronic and outpatient services, their ethnicity, language spoken at home and residential postcode. Consumers will be allocated a workshop group based on their experiences with healthcare services. Where possible, consumers with common experiences (eg, chronic conditions) will be allocated to the same group. Additionally, CALD participants will be allocated to a group and presented with models which are perceived to be of increased relevance for this population (eg, virtual care, digital hospital). Aboriginal and Torres Strait Islander people will be presented with all six models. Providers will be asked to indicate their role, clinical specialty, whether they are employed by the LHD and work postcode. Where possible, providers with similar roles (eg, nurses, general practitioners) will be allocated to the same group. In the case of workshops being delivered online, participants will be sent their information and consent forms to sign before attending.
The workshops and supplementary interviews will be run by a team of experienced health services researchers and will explore the experiences and views of participants concerning innovative models of care. Responses will be audio recorded. Key themes and different points of view will be identified and recorded for qualitative analysis. Each group within a workshop will provide their written notes and observations to the workshop facilitator who will collate the data. The data will then be aggregated across all the workshops for analysis, separately for consumers and providers.
Planned data analyses
The quantitative data that include demographic and health-related data from the EOI questionnaire will be analysed using SPSS V.22.020 and weighted against the Australian Bureau of Statistics data for the catchment, to assess the representativeness of the sample. Consumer and provider workshop and interview data for each model will be merged into two aggregated, narrative summaries: one for consumers and one for providers. All participants will be deidentified, and any identifiable features of the experiences or personal details shared in the group will be changed (eg, if a unique service or practitioner is mentioned; or features of the disease that identifies the patient). Data collected in the workshops and interviews will only be used for this research project. Aggregated data sets will be analysed separately for consumers and providers.
Qualitative data (ie, facilitator notes and key elements of the workshop recordings) will be thematically analysed independently using an open coding process by two members of the research team, who will work together to resolve discrepancies. Themes will be extracted that characterise the expectations and needs of the consumers and health providers in terms of the new health facility catchment. Any variation in response, or conflicting views, will be reported. Data collection and analysis will occur iteratively; questions used for workshops and guides for observations will be refined and expanded as new findings emerge.
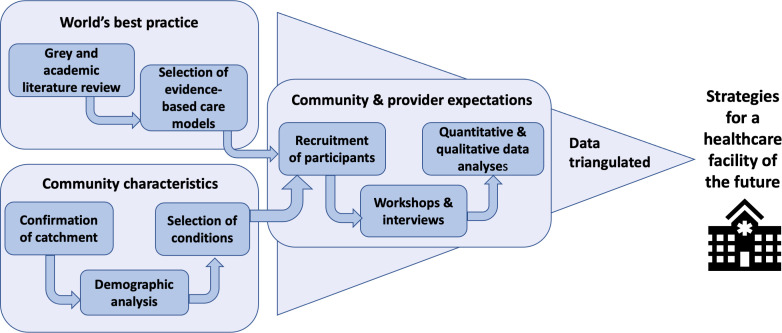
Synthesising and integrating results
Data will be synthesised using a triangulated approach, whereby literature review findings, community characteristics and findings from the focus groups and interviews will be integrated to arrive at a set of evidence-based community-supported and provider-supported strategies for delivering care to those in the healthcare catchment. Figure 3 illustrates the data collection, analysis and synthesis strategy for the project. Triangulated findings will be used to inform planning options and the feasibility of implementation of the options for the development of the new health facility.
Figure 3.
Recruitment process and data plan for the project.
Patient and public involvement
No patient was involved. No patient data are reported in this paper.
Discussion
This study seeks to examine consumer and provider needs and expectations for the development of an innovative care model for a health facility, specifically about six evidence-based models of care, and the consumer-focused care that underpins them, and the health conditions that form major burdens of disease found in a diverse catchment area in metropolitan NSW, Australia. The study investigates community perspectives on each model of care in detail, each presented within a purpose-designed, contextualised health scenario. Healthcare delivery is changing due to the introduction of new and enhanced technologies, the increasing social and economic burdens of ageing populations and the prevalence of chronic disease, among other factors. Therefore, it is important that we use these findings to guide the development of new healthcare facilities to ensure that both consumer and provider needs are met. These findings may be used to inform policies on how to design new healthcare facilities in consideration of consumer and provider needs.
The limitations of this study may include the following factors: due to the scope of the project, we cannot include an exhaustive list of health conditions. We have used a data-driven approach to stratify the main diseases reported in the new catchment as defined by the LHD. In addition, this study is limited to the LHD under investigation and the specific needs of the consumers and providers in that district, and the catchment area could change as the LHD redefines its boundaries. Finally, low rates of participant enrolment are a potential limitation. To address this, we have ensured that our recruitment strategy is designed so that the study is advertised widely across several different mediums and locations to increase the likelihood of snowballing. In the case of low recruitment numbers, we will readvertise the study.
Expected outcomes
Adopting an evidence-based approach, we will elicit opinions from consumers and providers within the catchment of a new healthcare facility about the barriers and enablers associated with consumer-focused care and six innovative care models. Findings will be available to provide guidance in designing care models for future health facility development in Australia and globally. Ultimately, the outcomes will help ease the burdens that many health facilities face such as the increasing social and economic burdens of ageing populations and the prevalence of chronic disease.
Ethics and dissemination
There are no known health or safety risks associated with participation in any aspect of the described study. Ethics approval for conducting the study was obtained from the Local Health District Human Research Ethics Committee (2021/PID01000). The results will be actively disseminated through peer-reviewed journals, conference presentations and reports to stakeholders.
Supplementary Material
Acknowledgments
The authors wish to thank Natasia Seo, Anita Calderan and Chrissan Segaram for their advice and assistance in obtaining the demographic data for the health facility catchment area. The authors also wish to thank Monika Latanik and the local health district’s multicultural unit for assisting with the planning for CALD recruitment and interpretation services.
Footnotes
Twitter: @annjcar, @RClaywilliams, @zeyadmahmoud, @HealthDataProf, @YvonneZurynski, @JanetCLong
Contributors: GL, JB, RC-W and PDH conceptualised the study. AC, NR, CP, ZM, RC-W, PDH, KM, RM, YZ, JCL, FR, GA and JB contributed to the design of the study. AC drafted the initial manuscript, assisted by NR, CP, ZM, RC-W, PDH and JB. All authors contributed to the refinement of the paper and approved the final manuscript.
Funding: The study was funded by Health Infrastructure (NSW, Australia) as an independent consultancy to support a larger project developing and implementing a new health facility in Sydney, Australia (grant number: HI20314).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Braithwaite J, Mannion R, Matsuyama Y, et al. Healthcare systems: future predictions for global care. Boca Raton, Florida: CRC Press, 2018. [Google Scholar]
- 2.Amalberti R, Nicklin W, Braithwaite J. Preparing National health systems to cope with the impending tsunami of ageing and its associated complexities: towards more sustainable health care. Int J Qual Health Care 2016;28:412–4. 10.1093/intqhc/mzw021 [DOI] [PubMed] [Google Scholar]
- 3.Braithwaite J, Mannion R, Matsuyama Y, et al. The future of health systems to 2030: a roadmap for global progress and sustainability. Int J Qual Health Care 2018;30:823–31. 10.1093/intqhc/mzy242 [DOI] [PubMed] [Google Scholar]
- 4.Penno E, Gauld R. Change, connectivity, and challenge: exploring the role of health technology in shaping health care for aging populations in Asia Pacific. Health Syst Reform 2017;3:224–35. 10.1080/23288604.2017.1340927 [DOI] [PubMed] [Google Scholar]
- 5.Havas K, Douglas C, Bonner A. Meeting patients where they are: improving outcomes in early chronic kidney disease with tailored self-management support (the CKD-SMS study). BMC Nephrol 2018;19:279. 10.1186/s12882-018-1075-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joseph A, Kirk Hamilton D. The Pebble projects: coordinated evidence-based case studies. Build Res Inf 2008;36:129–45. 10.1080/09613210701652344 [DOI] [Google Scholar]
- 7.Conley J, O'Brien CW, Leff BA, et al. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med 2016;176:1693–702. 10.1001/jamainternmed.2016.5974 [DOI] [PubMed] [Google Scholar]
- 8.Chewning B, Bylund CL, Shah B, et al. Patient preferences for shared decisions: a systematic review. Patient Educ Couns 2012;86:9–18. 10.1016/j.pec.2011.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frist WH. Connected health and the rise of the patient-consumer. Health Aff 2014;33:191–3. 10.1377/hlthaff.2013.1464 [DOI] [PubMed] [Google Scholar]
- 10.Khan A, Mir MS. Digital hospitals. Scholarly Journal of Biological Science 2021;10:104–6. [Google Scholar]
- 11.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020;26:309–13. 10.1177/1357633X20916567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duffy S, Lee TH. In-Person health care as option B. N Engl J Med 2018;378:104–6. 10.1056/NEJMp1710735 [DOI] [PubMed] [Google Scholar]
- 13.Länsisalmi H, Kivimäki M, Aalto P, et al. Innovation in healthcare: a systematic review of recent research. Nurs Sci Q 2006;19:66–72. 10.1177/0894318405284129 [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Australian Bureau of Statistics . Australian statistical geography standard (ASGS), 2021. Available: https://www.abs.gov.au/websitedbs/d3310114.nsf/home/australian+statistical+geography+standard+(asgs) [Accessed 01 May 2021].
- 16.Australian Bureau of Statistics . 2016 census. Available: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2916.0main+features252016 [Accessed 01 May 2021].
- 17.Epidemiology and Health Analytics, Western Sydney Local Health District . Epidemiological Profile - Rouse Hill Catchment Area (RHCA) Residents. 2021. Sydney: Western Sydney Local Health District, 2021. [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bloor M. Focus groups in social research. London: UK: SAGE Publications, 2001. [Google Scholar]
- 20.IMB C . IBM SPSS statistics for windows, version 22.0. Armonk, NY: IBM Corp, 2013. [Google Scholar]
- 21.Carey K, Morgan JR, Lin M-Y, et al. Patient Outcomes Following Total Joint Replacement Surgery: A Comparison of Hospitals and Ambulatory Surgery Centers. J Arthroplasty 2020;35:7–11. 10.1016/j.arth.2019.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah AA, Devana SK, Lee C, et al. Development of a novel, potentially universal machine learning algorithm for prediction of complications after total hip arthroplasty. J Arthroplasty 2021;36:1655–62. 10.1016/j.arth.2020.12.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bal Özkaptan B, Kapucu S. Home nursing care with the self-care model improves self-efficacy of patients with chronic obstructive pulmonary disease. Jpn J Nurs Sci 2016;13:365–77. 10.1111/jjns.12118 [DOI] [PubMed] [Google Scholar]
- 24.Naranjo A, Fernández-Conde S, Ojeda S, et al. Preventing future fractures: effectiveness of an orthogeriatric fracture liaison service compared to an outpatient fracture liaison service and the standard management in patients with hip fracture. Arch Osteoporos 2017;12:112. 10.1007/s11657-017-0373-9 [DOI] [PubMed] [Google Scholar]
- 25.JAd O, Cordeiro RG, Rocha RG, et al. Impact of telephone monitoring on patients with heart failure: a randomized clinical trial. ACTA Paul Enferm 2017;30:333–42. [Google Scholar]
- 26.Grant SJ, Marthick M, Lacey J. Establishing an integrative oncology service in the Australian healthcare setting-the Chris O'Brien Lifehouse Hospital experience. Support Care Cancer 2019;27:2069–76. 10.1007/s00520-018-4460-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059330supp001.pdf (85.5KB, pdf)
bmjopen-2021-059330supp002.pdf (191.3KB, pdf)
bmjopen-2021-059330supp003.pdf (36.9KB, pdf)