INTRODUCTION
The anatomical foot-ankle complex provides essential functions that are necessary for standing and walking performance in able-bodied individuals. Specifically, the foot-ankle complex must support balance during standing yet maintain an appropriate rocker geometry as the body advances over the stance limb and provide push-off work during the pre-swing phase of gait. Perry1 described how four rockers of the foot and ankle act in series to facilitate forward advancement throughout mid-stance. Hansen et al.2 expanded this concept further by describing the integrated effect of these rockers to produce a smooth roll-over shape during stance phase of walking. Although the anatomical ankle joint range of motion of the plantarflexion/dorsiflexion angle during stance phase is only on average 25 degrees, this motion is critical for load acceptance at limb collision and subsequent forward progression.3 Importantly, able-bodied persons adapt their ankle joint stiffness for standing4 and with walking speed5 to meet the specific demands of those tasks.
Lower-limb prosthesis users have a fixed prosthetic foot-ankle stiffness profile that is dependent on the mechanical characteristics of the components incorporated into the prosthesis by their prosthetist.6,7 Furthermore, they are generally less efficient ambulators8,9 and their gait stability is compromised, attributable in part to deficiencies in the function of their prostheses.10,11 Some important functions for walking are absent or diminished during prosthetic gait due to a reduction or absence of ankle motion, such as plantarflexion for stable foot-flat position following initial contact10 and adequate dorsiflexion for tibial progression through stance.12 Consequently, fitting lower-limb prosthesis users with prosthetic foot-ankle mechanisms that attempt to replicate corresponding anatomical functions is desirable.5,13 It has been demonstrated that the gait of lower-limb prosthesis users can be improved by providing motion at an articulated prosthetic ankle,14 but the increased motion may adversely affect standing balance given the role of ankle impedance to postural control.15 Therefore, it is important to consider how prosthetic ankle stiffness affects the ability of transtibial prosthesis users to ambulate and stand upright, since the prescribed stiffness likely influences the user’s performance during both activities. However, the means to identify a prosthetic foot-ankle stiffness profile that is capable of providing benefits for both standing and walking has not yet been reported but is clinically important.16 Ultimately, compliant foot-ankle mechanisms that allow for a normal range of ankle joint motion during walking will likely improve gait performance,14,17–24 but decrease standing balance. Conversely, a rigid ankle combination will likely maximize standing balance,13,14,25 but diminish gait performance. Therefore, some sort of compromise in prosthetic foot-ankle joint stiffness would seem necessary to enable both efficient standing and walking performance.
Standing balance has been defined as the ability to maintain the body’s center of mass (COM) over its base of support, with minimal body sway often considered a reflection of better postural control.26 During upright standing, COM motion in the medial-lateral and anterior-posterior directions is primarily controlled by the hip and ankle joints, respectively.27 Specific to postural control, the anatomical ankle joint regulates COM location by alternating between dorsiflexion and plantarflexion moments. While ankle impedance can be volitionally modulated in intact individuals, lower-limb prosthesis users rely on the elastic joint resistance of the prosthetic foot-ankle mechanism to control COM position through restorative forces. Buckley et al.28 analyzed sway during quiet standing in six unilateral prosthesis users—three transtibial and three transfemoral—and compared their data with able-bodied controls. Center of pressure (COP) excursions during standing were significantly greater in the prosthesis user group, suggesting that they have greater difficulty controlling and maintaining balance. These results are consistent with other studies that report greater standing sway in prosthesis users compared with able-bodied controls.29–32 Moreover, Nederhand et al.15 studied dynamic balance control of lower-limb prosthesis users and described a correlation between ankle stiffness and balance control.
Gait of unilateral prosthesis users is typically asymmetric, which may reflect the limitations imposed by altered anatomical structures and the functional shortcomings of the prosthesis. Consequently, certain aspects of gait function can be improved through optimization in prosthetic component designs.7 Previous studies3,33–40 provide good documentation on the effects of different prosthetic feet on gait biomechanics, but there is only a small amount of information about correlating isolated mechanical properties and their ultimate influence on human gait.12 However, passive prosthetic devices are set up to provide the most advantages at the user’s customary walking speed, which could diminish user performance at slower or faster walking speeds.33 We believe that transtibial prosthesis users’ gait may reasonably be improved at any walking speed by appropriately tuning the prosthetic ankle dorsiflexion stiffness. Specifically, variation of stiffness could reduce step length asymmetry, modulate gait biomechanics, and reproduce a radius of the foot-ankle roll-over shape close to able-bodied individuals, which is desirable to improve gait.13,41 However, little is still known on what prosthetic foot-ankle stiffness would best accommodate users of lower-limb prostheses, or how the characteristics of their gait are modified with changes in prosthetic ankle dorsiflexion stiffness and walking speed. Although a passive-mechanical prosthetic foot-ankle component may not fully restore the function of the anatomical ankle, it is worthwhile to consider how prosthetic foot-ankle stiffness could be tuned to improve standing balance while not compromising walking ability.
The purpose of this study was to determine how systematically varying the prosthetic foot-ankle stiffness affects standing and walking performance in persons with unilateral, transtibial amputation. Specifically, this study focused on the isolated changes in ankle dorsiflexion stiffness given its dominant role in forward progression and anterior movement of the COM as it interacts with the keel lever arm. We hypothesized that participants would have better standing balance performance when fitted with a stiffer prosthetic ankle dorsiflexion component as it would act against anterior COM motion. Furthermore, we hypothesized that a softer dorsiflexion stiffness would improve gait biomechanics and this effect would also depend on walking speed. This study will contribute to a better understanding of how prosthetic foot-ankle stiffness affects both standing and walking performance, emphasizing the importance of optimizing prosthetic foot-ankle stiffness through clinical fitting procedures that satisfy the objectives for both activities.
METHODS
This study was reviewed and approved by the Jesse Brown VA Medical Center (VAMC) Institutional Review Board (IRB). Written informed consent was obtained from prospective participants prior to their enrollment in the study.
PARTICIPANTS
A convenience sample was recruited through the following inclusion criteria: age from 18–80 years; residual limb length classified as medium to long; prosthesis user for at least one year; good skin integrity upon visual inspection; does not require the use of assistive devices to walk; clinically presents with good standing balance and recovery; can walk continuously for a minimum of one hour and for a distance of at least eight city blocks without an assistive device (self-reported).
EXPERIMENTAL PROTOCOL
After providing informed consent, participants were fitted with a Venture foot (College Park Industries, Warren, MI) (Figure 1). The Venture foot is a prosthetic foot with a modular component that enables specific elements affecting foot-ankle stiffness to be interchanged. For the present study, the dorsiflexion bumper of the articulated ankle joint was varied using three different levels of stiffness to serve as three experimental conditions: Soft, Medium, and Firm. Linear stiffness (KLin) of each individual bumper was obtained by dividing the difference of the applied force from initial load (Fstart=100N) to final load (Fend=3000 N) by the linear displacement (Ldisp) of the isolated ankle mechanism (KLin= [Fend-Fstart]/ Ldisp). The final load was calculated by using the weight limit of the Venture foot (275 lbs. according to the manufacturer) in late stance and then calculating the force applied on the bumper using the ratio of lever arms. The result was an approximate force of 3000N. The ankle joint rotational (KRot) stiffness was calculated by multiplying the linear stiffness and the moment arm squared from the applied force to the center of rotation (KRot=KLin*moment_arm2). The modular design of the Venture foot also gives the alternative to interchange footplates with different stiffness. The stiffness for the footplate was calculated using a similar method as the one described for the dorsiflexion bumper stiffness. For each size, the manufacturer offers between 3 to 5 different footplate stiffness; in the present study the footplate with a medium value of stiffness was used for every experimental session. The values of linear stiffness and rotational stiffness of each individual bumper and footplate used are presented on Table 1.
Figure 1 -. College Park Venture foot:

without the foot shell. (To note, the foot shell was worn during human subject testing.)
Table 1 -.
Linear Stiffness and Rotational Stiffness for each individual bumper
| Stiffness Bumper | Linear Stiffness (N/mm) | Rotational Stiffness (Nm/rad) |
|---|---|---|
| Soft | 594.8 | 1209.2 |
| Medium | 946.5 | 1919.8 |
| Firm | 1155.0 | 2341.3 |
The testing protocol required a total of three visits, starting with a fitting session and two experimental sessions. During the fitting session, the Venture foot was fitted to the participants’ customary socket by a certified prosthetist. The dorsiflexion bumper was initially selected according to the manufacturer’s recommendations based upon the participant’s weight and activity level. After an accommodation period of at least one week, the participant visited the laboratory for the first of two experimental sessions. Two stiffness conditions were tested during the first session, and the third stiffness condition was tested in the second session (order randomized). Each experimental session consisted of standing balance and gait data collection trials. For all the trials, data were collected using a modified Helen Hayes full-body marker set.42 Kinematic data were collected using a 12-camera motion measurement system (Motion Analysis Corp. (MAC), Santa Rosa, CA) with a sampling rate of 120 Hz and kinetic data were acquired using six floor-embedded force platforms (AMTI, Watertown, MA) with sampling rate of 960 Hz. For the three standing balance trials, participants quietly stood with their feet on two separate force platforms for 30 seconds. While standing, participants were asked to look straight ahead and maintain a comfortable but still position. Standing balance was collected for both an eyes open and closed (blindfold) condition and participants’ feet position was maintained across all balance trials and conditions. During the gait trials, participants were asked to walk at three self-selected speeds (normal, slow, and fast). The order for each speed condition were pre-established starting with normal speed, followed by slow speed, and ended with fast walking speed. Normal speed was defined as the usual comfortable speed that the participants walk; slow speed was defined as when strolling while window shopping; and fast speed defined as when trying to catch the bus without running. Participants performed repeated trials until five clean force plate strikes (one foot within the force plate borders) were collected for each leg.
DATA ANALYSIS
All data were treated with a 4th order, bidirectional, 6.0Hz low pass Butterworth filter using CORTEX® (MAC, Santa Rosa, CA). Standing balance data were analyzed using custom software in MATLAB® (MathWorks, Natick, MA) and included the root-mean-square (RMS) distances of plantar center of pressure displacement (COPrms)(mm)43 and the asymmetry of vertical ground reaction force (GRF) magnitudes (V-GRFa). V-GRFa was determined by subtracting the prosthetic limb vertical GRF from the sound limb vertical GRF, dividing the quantity by the sum of both forces, and multiplying the result by 100. Gait parameters from spatiotemporal, kinetic, and kinematic data were calculated using Orthotrack®6.6.4 (MAC, Santa Rosa, CA) and subsequently analyzed using MATLAB®. The spatiotemporal gait characteristics included walking speed (m/s), stride length (m), and step length asymmetry (%). Step length asymmetry was determined by subtracting the prosthetic limb step length from the sound limb step length and dividing it by the stride length and multiplying the result by 100. Kinematic parameters included prosthetic side instantaneous dorsiflexion-plantarflexion angle (DPAngle)(°), and ankle-foot roll-over shape radii (R-ROS)(%) values according to Hansen et al.,44 using MATLAB® and the positions of the ankle joint center, knee joint center, heel, toe, and center of pressure. All R-ROS values are presented as a percentage of body height. Kinetic data included instantaneous vertical ground reaction forces (V-GRF) (N/Kg) for both limb sides, and prosthetic side ankle flexion-extension moment (Nm/Kg) and power (W/Kg).
STATISTICAL ANALYSIS
To address the first hypothesis, a two-way repeated-measures ANOVA was conducted on the standing balance outcomes (COPrms and V-GRFa) to assess the main and interaction effects of stiffness and the eyes-open/eyes-closed (i.e., vision) conditions. For gait data, a one-dimension Statistical Parametric Mapping analysis (SPM)45 was used to identify regional differences in instantaneous kinetic and kinematic data between the three stiffness conditions (Firm, Medium, and Soft) across the entire gait cycle for each walking speed separately. The critical threshold for the SPM comparison was determined to be 5% (α=0.05). These results would give us the details on how the stiffness is affecting the geometry and forces present on gait. To address the second hypothesis, a two-way repeated-measures ANOVA was conducted on step length asymmetry and R-ROS to assess the main and interaction effects of stiffness and walking speed. It is desirable to have a foot-ankle component that emulates anatomical structures like a R-ROS close to able-bodied individuals. Additionally, reducing asymmetry is advantageous since an increase in asymmetry could reflect an increased effort on the sound side which in turn may produce comorbidities after long-term prosthesis use. A Bonferroni correction was used to account for the familywise type-I error rate associated with each hypothesis, reducing critical α to 0.025.
RESULTS
PARTICIPANTS
Ten participants with unilateral transtibial amputation were enrolled in the study and all completed the testing protocol. Participant information is listed in Table 2; all confirmed as minimum K3 by the research prosthetist considering self-reporting activities and based on the definition found in Lower Limb Workgroup Consensus Document.46
Table 2 -.
Participants’ Data
| Participant Number | Prosthetic Side | Gender | Age | Mass (Kg) | Height (cm) | Prosthetic Foot Size | Years since Amputation | Linear Stiffness (N/mm) | Rotational Stiffness (Nm/rad) |
|---|---|---|---|---|---|---|---|---|---|
| 01 | R | M | 61 | 111.7 | 186.0 | 28 | 40 | 62.4 | 860.4 |
| 02 | L | F | 42 | 80.5 | 155.0 | 24 | 5 | 70.7 | 727.3 |
| 03 | L | M | 59 | 75.9 | 165.5 | 26 | 19 | 58.8 | 693 |
| 04 | L | F | 42 | 57.0 | 171.0 | 24 | 15 | 70.7 | 727.3 |
| 05 | L | F | 59 | 83.9 | 165.0 | 24 | 14 | 70.7 | 727.3 |
| 06 | R | M | 26 | 68.9 | 173.0 | 26 | 10 | 62.4 | 721.3 |
| 07 | R | F | 58 | 60.4 | 169.0 | 25 | 22 | 69.9 | 691.8 |
| 08 | R | F | 23 | 62.7 | 165.0 | 25 | 20 | 69.9 | 691.8 |
| 09 | L | M | 56 | 103.0 | 187.5 | 28 | 34 | 56.5 | 780.4 |
| 10 | R | M | 69 | 81.5 | 170.0 | 28 | 54 | 62.4 | 860.4 |
| Average (St Dev) | 50 (14) | 78.6 (17.0) | 170.7 (9.3) | 65.4 (5.5) | 748.1 (64.7) |
QUIET STANDING DATA
There was a significant main effect of stiffness [F(2,58)=6.51, p=0.003] and vision [F(1,29)=21.43, p<0.001] conditions on COPrms (Figure 2.A) and no interaction effect [F(2,58)=1.65, p=0.201]. The post-hoc pairwise comparisons indicated a significant difference between Firm and Soft bumpers (4.88 vs 5.64, p=0.004) and between eyes-closed and eyes-open conditions (5.60 vs 4.74, p<0.001). No significant differences were observed for V-GRFa between stiffness [F(2,58)=2.45, p=0.095] or vision [F(1,29)=1.64, p=0.210] conditions, and there was no significant interaction effect [F(2,58)=1.40, p=0.256] (Figure 2.B).
Figure 2 -. Mean Results of Quiet Standing Evaluations:

at different stiffness and testing conditions. A) COPrms(mm) B) V-GRFa (%). (Error bars: 95% CI) (COPrms: root-mean-square distances of center of pressure displacement, V-GRFa: asymmetry of vertical ground reaction force magnitudes).
SPATIOTEMPORAL DATA
Table 3 presents a summary of the results of the spatiotemporal data main and interaction effects. There was an interaction effect for stiffness*speed on walking speed and stride length; the simple main effect of stiffness is presented in Table 4 at each speed level. These results were used to confirm if the instructions of walking at different speeds were effective and to determine the interaction effect with stiffness. Step length asymmetry data summary is presented in Figure 3 and results from the multiple comparison post-hoc analyses are presented in Table 5.
Table 3 -. Spatiotemporal Results:
main and interaction effects from the two-way repeated measures ANOVA
| Dependent Variable | Effect Source | df | F | p value | Correction |
|---|---|---|---|---|---|
| Walking Speed (m/s) | Stiffness | 2,198 | 4.39 | 0.140 | N A |
| Speed | 1.118,166.75 | 751.63 | *0.000 | Greenhouse-Geisser | |
| Stiffness* Speed | 3.45,341.93 | 8.06 | *0.000 | Greenhouse-Geisser | |
| Stride (m) | Stiffness | 2,198 | 12.24 | *0.000 | N A |
| Speed | 1.24,122.33 | 505.15 | *0.000 | Greenhouse-Geisser | |
| Stiffness*Speed | 4,396 | 6.92 | *0.000 | N A | |
| Step Length Asymmetry (%) | Stiffness | 2,198 | 19.15 | *0.000 | N A |
| Speed | 1.81,179.33 | 1.40 | 0.250 | Greenhouse-Geisser | |
| Stiffness* Speed | 4,396 | 1.30 | 0.268 | N A |
df: degrees of freedom, N A: not applicable
statistical significance
Table 4 -.
Simple main effects of stiffness on walking speed and stride at each speed level
| Dependent Variable | Speed Level | df | F | p value |
|---|---|---|---|---|
| Walking Speed (m/s) | Slow | 2,98 | 344.17 | *0.000 |
| Medium | 2,98 | 436.37 | *0.000 | |
| Fast | 2,98 | 300.97 | *0.000 | |
| Stride (m) | Slow | 2,98 | 11.21 | *0.000 |
| Medium | 2,98 | 1.09 | 0.339 | |
| Fast | 2,98 | 9.42 | *0.000 |
df: degrees of freedom
statistical significance
Figure 3 -. Mean Step Length Asymmetry (%):

results by condition and walking speeds. (Error bars: 95% CI).
Table 5 -.
Post hoc analysis results on step length asymmetry (%)
| Condition 1 | Firm | Firm | Medium | Medium | Soft | Soft |
|---|---|---|---|---|---|---|
| Condition 2 | Medium | Soft | Firm | Soft | Firm | Medium |
| Mean 1 | 4.44 | 4.44 | 5.07 | 5.07 | 5.70 | 5.70 |
| Mean 2 | 5.07 | 5.70 | 4.44 | 5.70 | 4.44 | 5.07 |
| p value | *0.004 | *0.000 | *0.004 | *0.007 | *0.000 | *0.007 |
statistical significance
KINETIC AND KINEMATIC DATA
The results of SPM analyses are presented in Figures 4 through 9. At every walking speed level, there were significant (p<0.001) differences in dorsiflexion angle (Figures 4 through 6 A–B) between 40% to 60% of the gait cycle (terminal stance – pre-swing). The Soft condition showed the larger dorsiflexion angle compared to Medium and Firm. Ankle moment (Figures 4 through 6 C–D) demonstrated significant difference (p<0.001) between 30% to 40% (terminal stance) at fast and normal walking speeds. Ankle moments during this period of the gait cycle were smaller for the Soft bumper compared to the other two stiffness conditions. Finally, despite changes in ankle range-of-motion and moments there were no significant differences in ankle power at any walking speed between the three stiffness conditions across the gait cycle (Figures 4 through 6 E–F). There were also no significant main effects at any walking speeds for V-GRF (Figures 7 through 9).
Figure 4 -. SPM Results for Spatiotemporal Data for Fast Walking Speeds.

A) Ankle angle evolution B) SPM F-value for ankle angle C) Ankle moment evolution D) SPM F-value for ankle moment E) Ankle power evolution F) SPM F-value for ankle power (For A, C and E dotted line(…)=soft stiffness, dashed line(- -)=medium stiffness, and continuous line(_)=firm stiffness) (For B, D and F dashed line represents p-value=0.01) (SPM: Statistical Parametric Mapping).
Figure 9. SPM Results for V-GRF at slow walking speeds.

A) V-GRF on the prosthetic side evolution B) SPM F-value for V-GRF on the sound side C) V-GRF on the sound side evolution D) SPM F-value for V-GRF on the sound side (For A and C dotted line(…)=soft stiffness, dashed line(- -)=medium stiffness and continuous line(__)=firm stiffness) (For B and D dashed line represents p-value=0.01) (SPM: Statistical Parametric Mapping, V-GRF: vertical ground reaction force).
Figure 6. SPM Results for Spatiotemporal Data for Slow Walking Speeds.
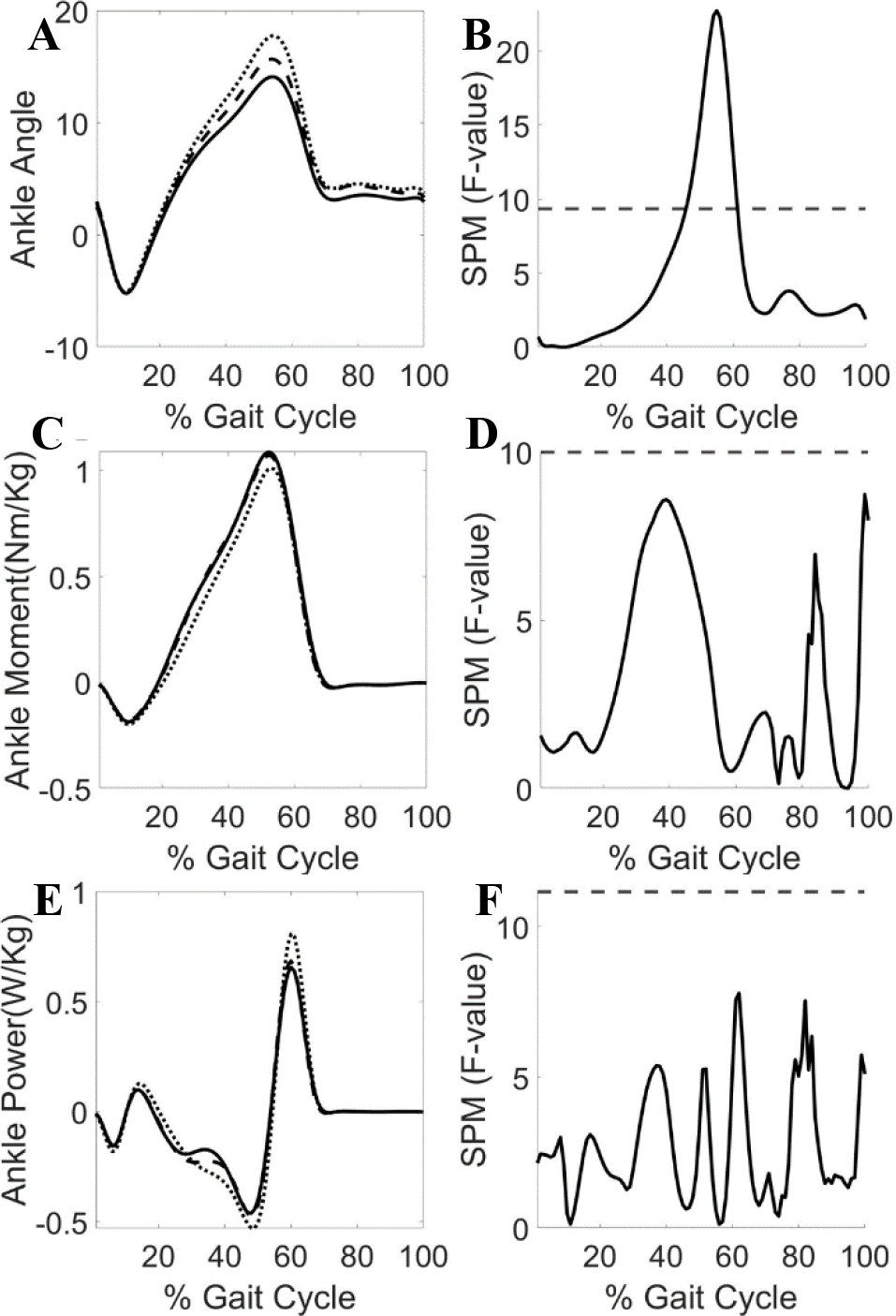
A) Ankle angle evolution B) SPM F-value for ankle angle C) Ankle moment evolution D) SPM F-value for ankle moment E) Ankle power evolution F) SPM F-value for ankle power (For A, C and E dotted line(…)=soft stiffness, dashed line(- -)=medium stiffness and continuous line(__)=firm stiffness) (For B, D and F dashed line represents p-value=0.01) (SPM: Statistical Parametric Mapping).
Figure 7. SPM Results for V-GRF at fast walking speeds.

A) V-GRF on the prosthetic side evolution B) SPM F-value for V-GRF on the sound side C) V-GRF on the sound side evolution D) SPM F-value for V-GRF on the sound side (For A and C dotted line(…)=soft stiffness, dashed line(- -)=medium stiffness and continuous line(__)=firm stiffness) (For B and D dashed line represents p-value=0.01) (SPM: Statistical Parametric Mapping, V-GRF: vertical ground reaction force).
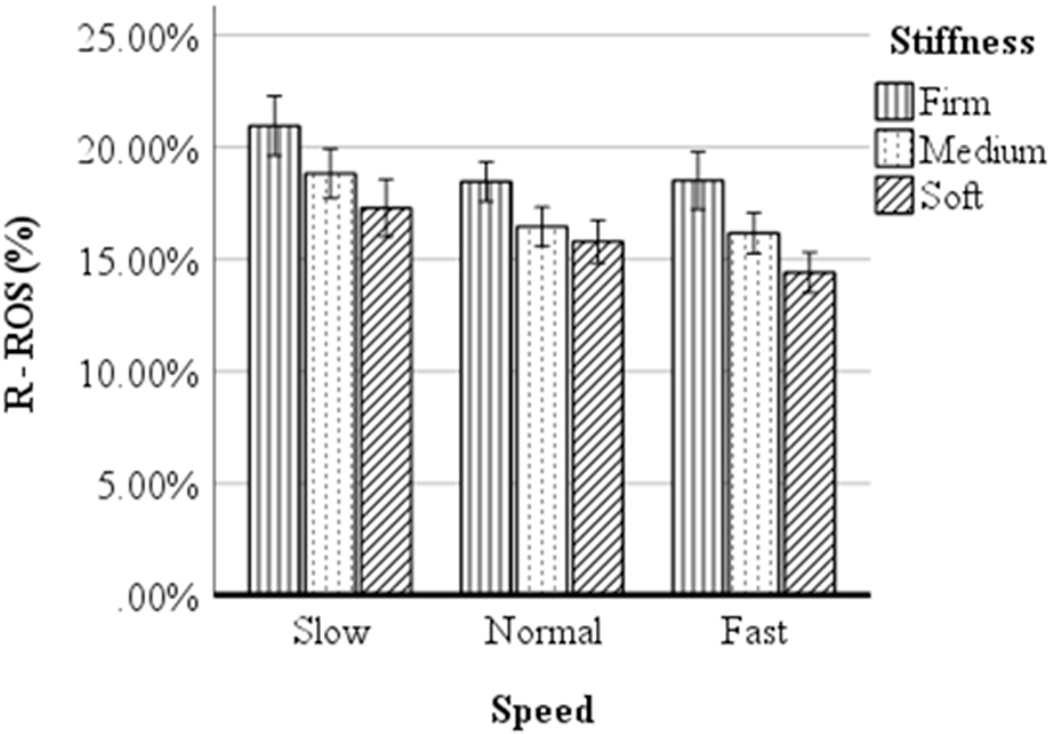
R-ROS
The main effects of stiffness condition [F(2,98)=38.62, p<0.001] and walking speed [F(2,98)=24.52, p<0.001] on R-ROS (Figure 10) were significant. The interaction effect between speed and stiffness was not significant [F(4,196)=0.957, p=0.432]. Pairwise comparisons indicated significant differences between all three levels of stiffness (Firm, Medium, and Soft: 19.32 vs 17.16 vs 15.84, p<0.001), between slow and fast walking speeds (16.37 vs 19.03, p<0.001) and between normal and fast walking speeds (16.91 vs 19.03, p<0.001). Figures 11A and B illustrate the ROS average trajectories for each walking speed (A) and stiffness conditions (B) for participant 3.
Figure 10. Mean R-ROS (%):
results by condition and walking speeds, normalized as a percentage of body height. (Error bars: 95% CI) (R-ROS: roll-over shape radii).
Figure 11. ROS for Participant 3.-.
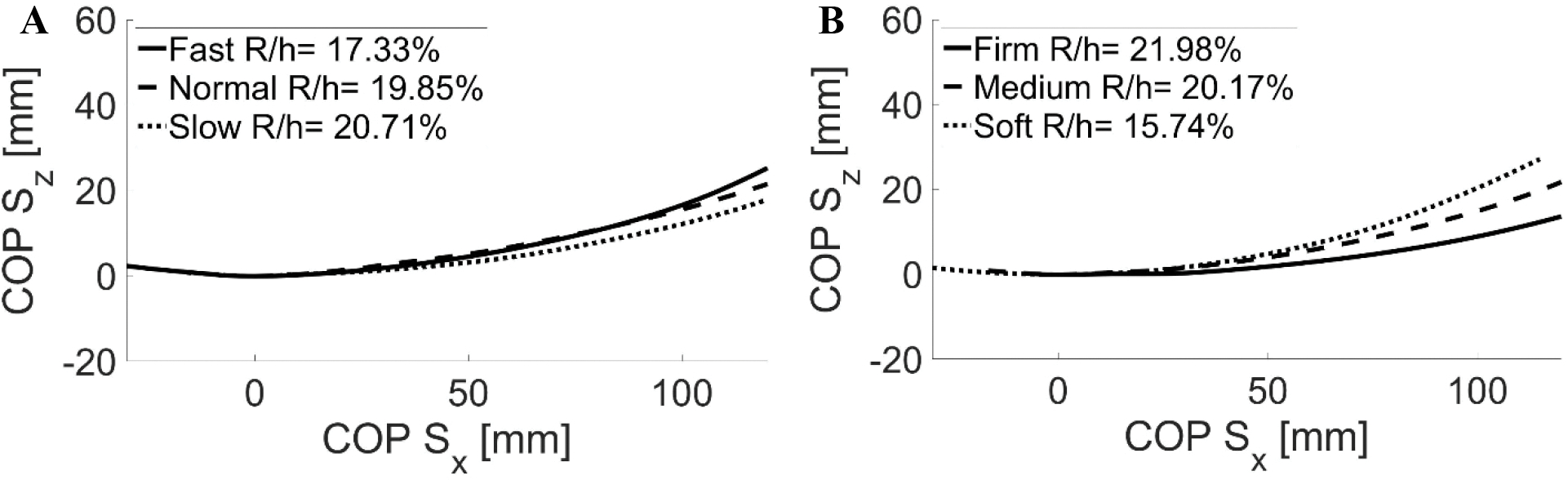
This is the average trajectory of ROS of each condition for participant 3 A) different speed levels; B) different stiffness conditions (ROS: roll-over shape, COP Sx: x coordinate of center of pressure on shank-based coordinate system, COP Sz: z coordinate of center of pressure on shank-based coordinate system)
DISCUSSION
The purpose of this study was to determine the effect of prosthetic ankle dorsiflexion stiffness on measures of standing and walking performance in unilateral transtibial prosthesis users. Our first hypothesis—participants would have better standing balance performance when fitted with a stiffer ankle dorsiflexion component—was partially supported. The quiet standing evaluations showed a distinction between Soft and Firm conditions. The smaller COPrms for the Firm condition indicates less sway of the COP due to the higher stiffness of the prosthetic foot-ankle component. Some of the participants reportedly felt more stable during the Firm condition, but there was no evidence that they relied more on the prosthetic side for body weight support under that test condition. Standing balance results indicated that participants achieved better balance performance while using higher stiffness prosthetic configurations. Consequently, the Firm stiffness was the most advantageous condition from among those tested.
The second hypothesis—a softer dorsiflexion stiffness will improve gait biomechanics and this effect would also depend on walking speed—was partially supported and offered an interesting insight about the influence of ankle dorsiflexion stiffness on gait. The systematic variation of prosthetic ankle dorsiflexion stiffness showed a significant effect on stride length and step length asymmetry during walking. For step length asymmetry, only the main effect of stiffness was significant, of which there was a difference between the Firm stiffness condition and the other two conditions (Figure 3). Several studies have presented information about the importance of symmetry for prosthesis users47–49 and the Firm condition was able to improve spatial symmetry. This improvement may represent the participant’s increased forward progression during stance phase of walking on the prosthetic side resulting in a longer sound step length. However, this change in symmetry does not match the ground reaction force result that showed no change on the force applied on each side under different conditions. As suggested in a previous study,2 this apparent contradiction between step length symmetry and V-GRF could be a kinetic invariance that maintains the same forces on each leg in spite of improved forward progression on the prosthetic side. Furthermore, this effect of stiffness on step length symmetry was not influenced by walking speed. In other words, at any walking speed, the geometry of the foot-ankle complex will be influenced by the stiffer ankle stiffness ultimately increasing forward progression.
Prosthetic ankle dorsiflexion stiffness also had an effect on ankle joint kinematics and kinetics. Specifically, the prosthetic ankle dorsiflexion stiffness was inversely correlated with the prosthetic ankle dorsiflexion angle between 45–60% of gait (late stance), and it directly correlated with the prosthetic ankle moment between 30–40% (midstance). This inverse relationship between prosthetic ankle dorsiflexion angle and stiffness was expected since a higher stiffness will rotate the ankle joint less for a given moment. This result also confirms that the adjustments to dorsiflexion stiffness had the intended effect on the mechanical response of the prosthetic ankle-foot. In the case of the prosthetic ankle moment, the progression of the center of pressure (COP) under the plantar surface of the foot relates directly to the rotational stiffness; a higher prosthetic ankle stiffness enables the COP to progress further anteriorly during stance than lower stiffness conditions.
The R-ROS results indicate an influence of walking speed (Figure 5.A) and ankle dorsiflexion stiffness (Figure 5.B). The effect of walking speed is related to the passive prosthesis attributes. A passive prosthetic device does not have the same biological and mechanical characteristics as the human foot, which is capable of adapting the stiffness properties to maintain the R-ROS invariant with speed.5 However, the stiffness of a passive prosthetic mechanism remains constant at every walking speed and the applied ground reaction force increases directly with walking speed, resulting in a larger radius for slow walking speeds and a smaller one for fast speeds, which has been demonstrated in bench test characterization of prosthetic feet.6 The pairwise comparisons indicate a significant difference of R-ROS between slow and fast speeds. Furthermore, there is the influence of stiffness on R-ROS similar to the results reported by Major et al.12 The condition that most closely approximated the able-bodied R-ROS value of 19% of height13 was the Firm condition, which is the same condition that improved symmetry and increased ankle moment at each self-selected walking speed. These outcomes were related since the improvement in step length symmetry could have been caused by the geometry of ROS provided by Firm condition (close to 19%) and the greater anterior progression of the COP, resulting in an increased forward progression on the prosthetic side. Contrary to our first hypothesis, the condition that was able to improve gait biomechanics was the Firm stiffness condition.
Figure 5. SPM Results for Spatiotemporal Data for Normal Walking Speeds.
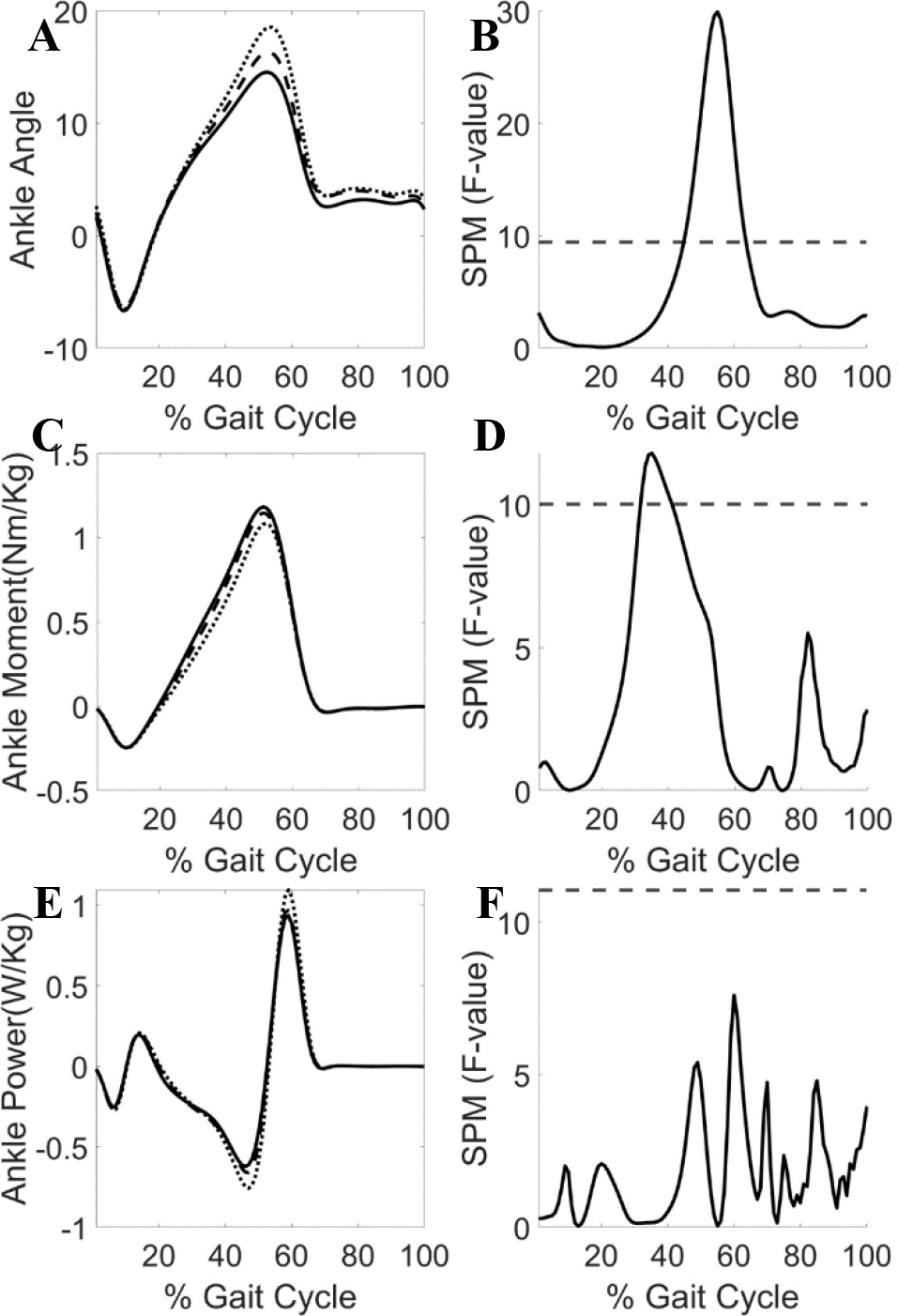
A) Ankle angle evolution B) SPM F-value for ankle angle C) Ankle moment evolution D) SPM F-value for ankle moment E) Ankle power evolution F) SPM F-value for ankle power (For A, C and E dotted line(…)=soft stiffness, dashed line(- -)=medium stiffness and continuous line(__)=firm stiffness) (For B, D and F dashed line represents p-value=0.01) (SPM: Statistical Parametric Mapping).
After considering the data obtained from both the quiet standing and gait analyses, there was a single prosthetic foot-ankle stiffness that provided the best performance and could be identified as the most desirable configuration from among those stiffness conditions tested. However, due to the limitations in the testing protocol, we cannot conclude with certainty that this particular stiffness was the optimal one from among all possibilities. To make this determination, the effects produced by configurations with stiffness values greater than Firm also need to be analyzed as well additional metrics of relevance to standing balance and gait performance. The better performance for standing balance favored the Firm stiffness condition given reductions in body sway to suggest improved postural control. Additionally, during the walking portion of the study, the R-ROS provided by the Firm condition was the closest approximation to able-bodied R-ROS and produced better step length symmetry compared to the other stiffness configurations. Taking into consideration the results from both sets of analyses, the Firm stiffness could be considered the most desirable for both standing and walking from among the conditions and outcomes that were evaluated.
LIMITATIONS
There are several study limitations that need to be considered to aid with results interpretation. First, the ages and levels of activity of the participants were diverse and could have influenced our results. For example, participant 6 was able to control the Venture foot behavior despite the different stiffness conditions. His walking biomechanics and balance results alone did not reflect any observable change regardless of which condition he used. Second, Soft and Firm conditions were the minimum and maximum stiffness levels of the tested conditions, and a greater range of stiffness would provide a more complete profile of user walking or standing balance response. Another aspect to consider was the recurring comment from the participants about disliking the testing conditions that they perceived as being the most different from their own customary prosthetic foot and this response could have entered participant-specific bias into the results. Apart from this, there was a relatively short accommodation period for each testing condition. Even though participants were able to accommodate for a period of one week to the Venture foot, specifically to the manufacturer recommended stiffness, the stiffness conditions were changed at every testing session and prevented a longer accommodation period for each specific condition, which could have influenced our results. Finally, the stiffness of the prosthetic foot-ankle components was not necessarily proportional to the participant’s body weight. Instead, smaller participants tested the same ankle dorsiflexion stiffness values as larger participants. Additionally, the Venture’s footplate stiffness varied with the size and side of the prosthetic foot (Table 2). In other words, the footplate stiffness affected the combined dorsiflexion stiffness for the Venture foot and ultimately influenced the participant’s gait outcomes. There are a couple of recommendations for future studies that could improve our understanding of this effect of stiffness. A first future study design might normalize the combined prosthetic foot-ankle stiffness as a function of body weight so that all participants test three stiffness conditions proportional to the load they apply to the prosthesis. The next future design might select different combinations of footplate and ankle stiffness while identifying those combinations that have an equivalent combined stiffness. These data could help us to better understand the individual effect of each component (i.e., footplate and dorsiflexion bumper), and identify if there is a difference in conditions when the components have different individual stiffnesses, but the combined stiffness is similar. Nonetheless, despite these limitations, the results provide clinically relevant information on how prosthetic foot-ankle stiffness influences gait and standing balance while highlighting areas for further investigation.
CONCLUSIONS
The results of the current study improved our understanding about how prosthetic foot-ankle stiffness influences standing and walking in unilateral transtibial prosthesis users. It informs how variation of ankle dorsiflexion stiffness can influence key aspects of balance and gait. During quiet standing, we observed that stiffer prosthetic foot-ankle conditions reduced sway. During walking, the Firm stiffness was able to improve symmetry and best replicate the able-bodied individuals’ R-ROS, providing the most advantages. Further, walking speed had a profound influence on the R-ROS of a passive prosthetic foot-ankle mechanism during gait. Contrary to what is observed during able-bodied gait, passive prosthetic components are not capable of maintaining a constant ROS geometry at different speeds, particularly when the forces applied are directly proportional to the walking speed. Considering that passive prosthetic components are set up for customary walking speeds and there is an effect of those speeds, it is imperative to continue to pursue additional studies to examine how walking speed affects prosthetic foot performance and how to improve passive prosthetic designs that could present the same gait characteristics over a larger range of walking speeds. In general, prosthetists should consider the performance of patients during both the standing and walking to help determine the individual prosthetic stiffness for each prosthesis user.
Figure 8. SPM Results for V-GRF at normal walking speeds.

A) V-GRF on the prosthetic side evolution B) SPM F-value for V-GRF on the sound side C) V-GRF on the sound side evolution D) SPM F-value for V-GRF on the sound side (For A and C dotted line(…)=soft stiffness, dashed line(- -)=medium stiffness and continuous line(__)=firm stiffness) (For B and D dashed line represents p-value=0.01) (SPM: Statistical Parametric Mapping, V-GRF: vertical ground reaction force).
ACKNOWLEDGMENT
This work was supported by Merit Review Award # RX002107 from the United States (U.S.) Department of Veterans Affairs Rehabilitation Research and Development Service. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. The authors acknowledge the use of the Jesse Brown VA Medical Center Motion Analysis Research Laboratory, Chicago, IL.
Footnotes
Conflict of Interest:
Steven A. Gard is the Editor-in-Chief for the Journal of Prosthetics and Orthotics (JPO), and Matty J. Major is a JPO Editorial Board member. This article was submitted and reviewed according to the journal’s standard, double-blinded peer review process.
REFERENCES
- 1.Perry J, Burnfield JM. Gait analysis. Normal and pathological function 2nd ed. California: Slack. 2010. [Google Scholar]
- 2.Hansen AH, Meier MR, Sessoms PH, Childress DS. The effects of prosthetic foot roll-over shape arc length on the gait of trans-tibial prosthesis users. Prosthet Orthot Int. Dec 2006;30(3):286–299. doi: 10.1080/03093640600816982. [DOI] [PubMed] [Google Scholar]
- 3.Perry J, Boyd LA, Rao SS, Mulroy SJ. Prosthetic weight acceptance mechanics in transtibial amputees wearing the Single Axis, Seattle Lite, and Flex Foot. IEEE Trans Rehabil Eng. Dec 1997;5(4):283–289. doi: 10.1109/86.650279. [DOI] [PubMed] [Google Scholar]
- 4.Hansen AH, Wang CC. Effective rocker shapes used by able-bodied persons for walking and fore-aft swaying: implications for design of ankle-foot prostheses. Gait Posture. Jun 2010;32(2):181–184. doi: 10.1016/j.gaitpost.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansen AH, Childress DS, Knox EH. Roll-over shapes of human locomotor systems: effects of walking speed. Clin Biomech (Bristol, Avon). May 2004;19(4):407–414. doi: 10.1016/j.clinbiomech.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Major MJ, Twiste M, Kenney LP, Howard D. Amputee Independent Prosthesis Properties--a new model for description and measurement. J Biomech Sep 23 2011;44(14):2572–2575. doi: 10.1016/j.jbiomech.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 7.Major MJ, Fey NP. Considering passive mechanical properties and patient user motor performance in lower limb prosthesis design optimization to enhance rehabilitation outcomes. Phys Ther Rev Jul 17 2017;22(3–4):1–15. doi: 10.1080/10833196.2017.1346033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Genin JJ, Bastien GJ, Franck B, Detrembleur C, Willems PA. Effect of speed on the energy cost of walking in unilateral traumatic lower limb amputees. Eur J Appl Physiol. Aug 2008;103(6):655–663. doi: 10.1007/s00421-008-0764-0. [DOI] [PubMed] [Google Scholar]
- 9.Waters RL, Perry J, Antonelli D, Hislop H. Energy cost of walking of amputees: the influence of level of amputation. J Bone Joint Surg Am Jan 1976;58(1):42–46. https://www.ncbi.nlm.nih.gov/pubmed/1249111. [PubMed] [Google Scholar]
- 10.Major MJ, Twiste M, Kenney LP, Howard D. The effects of prosthetic ankle stiffness on stability of gait in people with transtibial amputation. J Rehabil Res Dev. 2016;53(6):839–852. doi: 10.1682/JRRD.2015.08.0148. [DOI] [PubMed] [Google Scholar]
- 11.Gard SA, Fatone S. Biomechanics of Lower Limb Function and Gait. Report of a Consensus Conference on the Orthotic Management of Stroke Patients; 2004; Copenhagen, Denmark,. [Google Scholar]
- 12.Major MJ, Twiste M, Kenney LP, Howard D. The effects of prosthetic ankle stiffness on ankle and knee kinematics, prosthetic limb loading, and net metabolic cost of trans-tibial amputee gait. Clin Biomech (Bristol, Avon). Jan 2014;29(1):98–104. doi: 10.1016/j.clinbiomech.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Hansen AH, Childress DS. Investigations of roll-over shape: implications for design, alignment, and evaluation of ankle-foot prostheses and orthoses. Disabil Rehabil. 2010;32(26):2201–2209. doi: 10.3109/09638288.2010.502586. [DOI] [PubMed] [Google Scholar]
- 14.Su PF, Gard SA, Lipschutz RD, Kuiken TA. The effects of increased prosthetic ankle motions on the gait of persons with bilateral transtibial amputations. Am J Phys Med Rehabil. Jan 2010;89(1):34–47. doi: 10.1097/PHM.0b013e3181c55ad4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nederhand MJ, Van Asseldonk EH, van der Kooij H, Rietman HS. Dynamic Balance Control (DBC) in lower leg amputee subjects; contribution of the regulatory activity of the prosthesis side. Clin Biomech (Bristol, Avon). Jan 2012;27(1):40–45. doi: 10.1016/j.clinbiomech.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Hafner BJ. Clinical Prescription and Use of Prosthetic Foot and Ankle Mechanisms: A Review of the Literature. JPO: Journal of Prosthetics and Orthotics. 2005;17(4):S5–S11. https://journals.lww.com/jpojournal/Fulltext/2005/10001/Clinical_Prescription_and_Use_of_Prosthetic_Foot.4.aspx. [Google Scholar]
- 17.Adamczyk PG, Roland M, Hahn ME. Sensitivity of biomechanical outcomes to independent variations of hindfoot and forefoot stiffness in foot prostheses. Hum Mov Sci. Aug 2017;54:154–171. doi: 10.1016/j.humov.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Asha AR, Munjal R, Kulkarni J, Buckley JG. Impact on the biomechanics of overground gait of using an ‘Echelon’ hydraulic ankle-foot device in unilateral trans-tibial and trans-femoral amputees. Clin Biomech (Bristol, Avon). Aug 2014;29(7):728–734. doi: 10.1016/j.clinbiomech.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Fey NP, Klute GK, Neptune RR. The influence of energy storage and return foot stiffness on walking mechanics and muscle activity in below-knee amputees. Clin Biomech (Bristol, Avon). Dec 2011;26(10):1025–1032. doi: 10.1016/j.clinbiomech.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Koehler-McNicholas SR, Nickel EA, Barrons K, et al. Mechanical and dynamic characterization of prosthetic feet for high activity users during weighted and unweighted walking. PLoS One. 2018;13(9):e0202884. doi: 10.1371/journal.pone.0202884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raschke SU, Orendurff MS, Mattie JL, et al. Biomechanical characteristics, patient preference and activity level with different prosthetic feet: a randomized double blind trial with laboratory and community testing. J Biomech Jan 2 2015;48(1):146–152. doi: 10.1016/j.jbiomech.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Schnall BL, Dearth CL, Elrod JM, et al. A more compliant prosthetic foot better accommodates added load while walking among Servicemembers with transtibial limb loss. J Biomech Jan 2 2020;98:109395. doi: 10.1016/j.jbiomech.2019.109395. [DOI] [PubMed] [Google Scholar]
- 23.Stefanyshyn DJ, Engsberg JR, Tedford KG, Harder JA. A pilot study to test the influence of specific prosthetic features in preventing trans-tibial amputees from walking like able-bodied subjects. Prosthet Orthot Int. Dec 1994;18(3):180–190. doi: 10.3109/03093649409164403. [DOI] [PubMed] [Google Scholar]
- 24.Zelik KE, Collins SH, Adamczyk PG, et al. Systematic variation of prosthetic foot spring affects center-of-mass mechanics and metabolic cost during walking. IEEE Trans Neural Syst Rehabil Eng. Aug 2011;19(4):411–419. doi: 10.1109/tnsre.2011.2159018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nederhand MJ, Van Asseldonk EHF, der Kooij Hv, Rietman HS. Dynamic Balance Control (DBC) in lower leg amputee subjects; contribution of the regulatory activity of the prosthesis side. Clin Biomech. 2012;27(1):40–45. doi: 10.1016/j.clinbiomech.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 26.Shumway-Cook A, Anson D, Haller S. Postural sway biofeedback: its effect on reestablishing stance stability in hemiplegic patients. Arch Phys Med Rehabil. Jun 1988;69(6):395–400. https://www.ncbi.nlm.nih.gov/pubmed/3377664. [PubMed] [Google Scholar]
- 27.Winter DA, Patla AE, Prince F, Ishac M, Gielo-Perczak K. Stiffness control of balance in quiet standing. J Neurophysiol Sep 1998;80(3):1211–1221. doi: 10.1152/jn.1998.80.3.1211. [DOI] [PubMed] [Google Scholar]
- 28.Buckley JG, O’Driscoll D, Bennett SJ. Postural sway and active balance performance in highly active lower-limb amputees. Am J Phys Med Rehabil Jan 2002;81(1):13–20. doi: 10.1097/00002060-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Fernie GR, Holliday PJ. Postural sway in amputees and normal subjects. J Bone Joint Surg Am Oct 1978;60(7):895–898. https://www.ncbi.nlm.nih.gov/pubmed/701337. [PubMed] [Google Scholar]
- 30.Geurts AC, Mulder TW, Nienhuis B, Rijken RA. Postural reorganization following lower limb amputation. Possible motor and sensory determinants of recovery. Scand J Rehabil Med. 1992;24(2):83–90. https://www.ncbi.nlm.nih.gov/pubmed/1604266. [PubMed] [Google Scholar]
- 31.Rusaw DF. Adaptations from the prosthetic and intact limb during standing on a sway-referenced support surface for transtibial prosthesis users. Disabil Rehabil Assist Technol. Oct 2019;14(7):682–691. doi: 10.1080/17483107.2018.1498925. [DOI] [PubMed] [Google Scholar]
- 32.Toumi A, Simoneau-Buessinger E, Bassement J, et al. Standing posture and balance modalities in unilateral transfemoral and transtibial amputees. J Bodyw Mov Ther. Jul 2021;27:634–639. doi: 10.1016/j.jbmt.2021.05.009. [DOI] [PubMed] [Google Scholar]
- 33.De Asha AR, Munjal R, Kulkarni J, Buckley JG. Walking speed related joint kinetic alterations in trans-tibial amputees: impact of hydraulic ‘ankle’ damping. J Neuroeng Rehabil. Oct 17 2013;10:107. doi: 10.1186/1743-0003-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gitter A, Czerniecki JM, DeGroot DM. Biomechanical analysis of the influence of prosthetic feet on below-knee amputee walking. Am J Phys Med Rehabil Jun 1991;70(3):142–148. doi: 10.1097/00002060-199106000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Hermodsson Y, Ekdahl C, Persson BM, Roxendal G. Gait in male trans-tibial amputees: a comparative study with healthy subjects in relation to walking speed. Prosthet Orthot Int. Aug 1994;18(2):68–77. doi: 10.3109/03093649409164387. [DOI] [PubMed] [Google Scholar]
- 36.Hofstad C, Linde H, Limbeek J, Postema K. Prescription of prosthetic ankle-foot mechanisms after lower limb amputation. Cochrane Database Syst Rev. 2004(1):CD003978. doi: 10.1002/14651858.CD003978.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson L, De Asha AR, Munjal R, Kulkarni J, Buckley JG. Toe clearance when walking in people with unilateral transtibial amputation: effects of passive hydraulic ankle. J Rehabil Res Dev. 2014;51(3):429–437. doi: 10.1682/JRRD.2013.05.0126. [DOI] [PubMed] [Google Scholar]
- 38.Moore R Patient Evaluation of a Novel Prosthetic Foot with Hydraulic Ankle Aimed at Persons with Amputation with Lower Activity Levels. Journal of Prosthetics and Orthotics. November/01 2016;29:1. doi: 10.1097/JPO.0000000000000120. [DOI] [Google Scholar]
- 39.Moore R Effect on Stance Phase Timing Asymmetry in Individuals with Amputation Using Hydraulic Ankle Units. JPO: Journal of Prosthetics and Orthotics. 2016;28(1):44–48. doi: 10.1097/jpo.0000000000000083. [DOI] [Google Scholar]
- 40.Wirta RW, Mason R, Calvo K, Golbranson FL. Effect on gait using various prosthetic ankle-foot devices. J Rehabil Res Dev. Spring 1991;28(2):13–24. doi: 10.1682/jrrd.1991.04.0013. [DOI] [PubMed] [Google Scholar]
- 41.Houdijk H, Wezenberg D, Hak L, Cutti AG. Energy storing and return prosthetic feet improve step length symmetry while preserving margins of stability in persons with transtibial amputation. J Neuroeng Rehabil. Sep 5 2018;15(Suppl 1):76. doi: 10.1186/s12984-018-0404-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. May 1990;8(3):383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 43.Prieto TE, Myklebust JB, Hoffmann RG, Lovett EG, Myklebust BM. Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Trans Biomed Eng. Sep 1996;43(9):956–966. doi: 10.1109/10.532130. [DOI] [PubMed] [Google Scholar]
- 44.Hansen A, Gard S, Childress D. The determination of foot/ankle roll-over shape: clinical and research applications. Paper presented at: Pediatric Gait: A New Millennium in Clinical Care and Motion Analysis Technology; 22–22 July 2000, 2000. doi: 10.1109/PG.2000.858888. [Google Scholar]
- 45.Pickle NT, Silverman AK, Wilken JM, Fey NP. Statistical analysis of timeseries data reveals changes in 3D segmental coordination of balance in response to prosthetic ankle power on ramps. Sci Rep Feb 4 2019;9(1):1272. doi: 10.1038/s41598-018-37581-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Medicare & Medicaid Services. Lower Limb Prosthetic Wrokgroup Concensus Document. website. https://www.cms.gov/Medicare/Coverage/DeterminationProcess/downloads/LLP_Consensus_Document.pdf. Published 2017, 2022.
- 47.Hurwitz DE, Sumner DR, Block JA. Bone density, dynamic joint loading and joint degeneration. A review. Cells Tissues Organs. 2001;169(3):201–209. doi: 10.1159/000047883. [DOI] [PubMed] [Google Scholar]
- 48.Nolan L, Wit A, Dudzinski K, Lees A, Lake M, Wychowanski M. Adjustments in gait symmetry with walking speed in trans-femoral and trans-tibial amputees. Gait Posture. Apr 2003;17(2):142–151. doi: 10.1016/s0966-6362(02)00066-8. [DOI] [PubMed] [Google Scholar]
- 49.Radin EL, Parker HG, Pugh JW, Steinberg RS, Paul IL, Rose RM. Response of joints to impact loading. 3. Relationship between trabecular microfractures and cartilage degeneration. J Biomech. Jan 1973;6(1):51–57. doi: 10.1016/0021-9290(73)90037-7. [DOI] [PubMed] [Google Scholar]