We read with intereste paper by Kobo et al.1 evaluating the impact of multisite artery disease on clinical outcomes after percutaneous coronary intervention. They enroled 37 198 patients in an observational registry, stratifying the population according to the presence or absence of known prior vascular disease; (1) not known prior vascular disease (62.3%), (2) known single territory (32.6%), and (3) known 2–3 territories (5.1%). After inverse propensity score weighting, they found that all-cause death at 1 year incrementally increased with the number of diseased vascular beds (2.22, 3.28, and 5.29%).
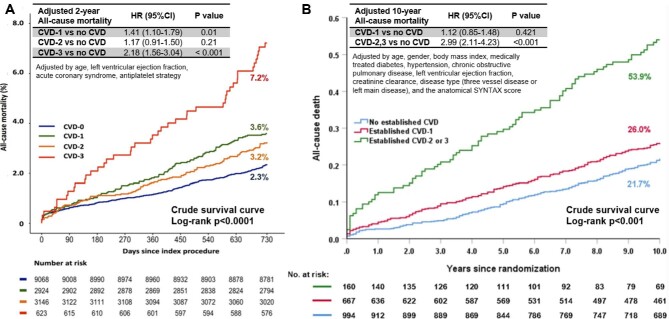
In the GLOBAL LEADERS, a randomized, superiority, all-comers trial (n = 15 761 patients) comparing 1-month dual antiplatelet therapy with ticagrelor monotherapy, Garg et al. previously (in 2019) compared the hazard ratio for 2-year all-cause mortality of patients with one or multiple territories of established cardiovascular disease (CVD) to those without CVD in unadjusted and adjusted models (Figure 1A).2,3
Figure 1.
(A) The unadjusted Kaplan–Meier survival curves show significantly higher mortality in patients having PCI with established vascular disease in three territories compared with those without (P < 0.001). When comparing patients without CVD to those with one or three territories of CVD, the hazard ratio for 2-year all-cause mortality increased in adjusted models in the GLOBAL LEADERS trial (cited from the previously published manuscript and modified; Garg S, et al. Impact of established cardiovascular disease on outcomes in the randomized global leaders trial. Catheter Cardiovasc Interv. 2020 ;96:1369–1378). (B) Crude 10-year survival curves according to the extent of established CVD and hazard ratio for 10-year mortality with one or multiple established CVD compare with no CVD in the SYNTAXES trial (whole population) (cited from the previously published manuscript and modified; Wang R et al. Impact of established cardiovascular disease on 10-year death after coronary revascularization for complex coronary artery disease. Clin Res Cardiol. 2021 ;110:1680–1691). Abbreviations: CVD, cerebrovascular disease; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft.
In 2021, Wang et al. demonstrated that the presence of CVD involving more than one territory was associated with a significantly increased risk of 10-year all-cause death in the SYNTAXES study (Figure 1B).4,5
The data of Kobo et al. are largely confirmatory of these previous publications, though conspicuously not mentioned in their references.
Contributor Information
Shigetaka Kageyama, Department of Cardiology, National University of Ireland, Galway (NUIG), Galway, Ireland.
Patrick W Serruys, Department of Cardiology, National University of Ireland, Galway (NUIG), Galway, Ireland.
Yoshinobu Onuma, Department of Cardiology, National University of Ireland, Galway (NUIG), Galway, Ireland.
Scot Garg, Department of Cardiology, Royal Blackburn Hospital, Blackburn, UK.
Conflict of interest:
Dr. Serruys reports personal consultation fees from Philips/Volcano, SMT, Novartis, Xeltis, Merillife, outside the submitted work. Other authors have nothing to declare.
References
- 1. Kobo O, Saada M, von Birgelen C, Tonino PAL, Íñiguez-Romo A, Fröbert Oet al. Impact of multisite artery disease on clinical outcomes after percutaneous coronary intervention: an analysis from the e-Ultimaster Registry. Eur Heart J.––Qual Care Clin Outcomes. 2022:qcac043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vranckx P, Valgimigli M, Jüni P, Hamm C, Steg PG, Heg Det al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: a multicentre, open-label, randomised superiority trial. Lancet. 2018;392:940–949. [DOI] [PubMed] [Google Scholar]
- 3. Garg S, Chichareon P, Kogame N, Takahashi K, Modolo R, Chang CCet al. Impact of established cardiovascular disease on outcomes in the randomized global leaders trial. Catheter Cardiovasc Interv. 2020;96:1369–1378. [DOI] [PubMed] [Google Scholar]
- 4. Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJet al. SYNTAX Extended Survival Investigators . Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet North Am Ed. 2019;394:1325–1334. [DOI] [PubMed] [Google Scholar]
- 5. Wang R, Garg S, Gao, C, Kawashima H, Ono M, Hara Het al. Impact of established cardiovascular disease on 10-year death after coronary revascularization for complex coronary artery disease. Clin Res Cardiol. 2021;110:1680–1691. [DOI] [PMC free article] [PubMed] [Google Scholar]