Abstract
Stress management interventions (SMIs) can alleviate the psychosocial stress often experienced by women with heart failure. The purpose of this meta-analysis was to summarize women’s participation rates, and predictors of participation, in SMIs for the management of psychosocial distress in women with chronic HF. Studies were retrieved from bibliographic databases, reference sections of relevant papers, and research registries. Included studies (a) evaluated a SMI approach for the management of chronic HF, (b) sampled chronic HF patients, and (c) used a randomized controlled trial (RCT) design. Independent coders extracted the relevant data. Thirty-five RCTs met inclusion criteria (N = 3,649; mean age = 63.5±7.0 years). All studies sampled both men and women; the mean proportion of women who participated in the trials was 38.8% (95% confidence interval [CI]=34.5–43.4; I2 = 82.4, 95% CI=81.0–83.6). Women’s participation rates were higher in studies sampling more HF patients with hypertension (B = 1.01, SE = 0.45, P = .046) but fewer HF patients prescribed beta blockers (B = −1.10, SE = 0.33, P = .006), F (2,12) = 6.27, P = 0.014, adjusted R2 = 61%. SMIs may offer women a complementary or integrative approach to standard treatment to help manage the psychological distress associated with HF. Future research should explore the potential benefits of offering stress management approaches to women as part of comprehensive HF care.
Keywords: chronic heart failure, women, stress management interventions, meta-analysis
INTRODUCTION
Heart failure (HF) is a chronic condition affecting 26 million adults globally (Ponikowski et al., 2014). The global prevalence of HF is increasing worldwide but most notably in Asia where HF prevalence is 1.2 to 6.7% of the population (Ponikowski et al., 2014). HF affects 6.2 million U.S. adults (2.2% of the population) and is expected to increase 46% by 2030 (Virani et al., 2020). The increasing prevalence can be attributed to improvements in survival following a HF diagnosis but long-term prognosis for HF patients remains poor with high rates of hospitalization, hospital readmissions, and mortality (Dharmarajan & Rich, 2017). The burden on the healthcare system is substantial, costing the U.S. healthcare system an estimated $11 billion in 2014 (Jackson et al., 2018).
The prevalence of HF is similar among men and women and increases with age, but the clinical presentation, prognosis, and etiology of HF varies by sex (Levinsson et al., 2018). Women with HF tend to be diagnosed at an older age, present with multiple comorbidities (e.g., obesity, hypertension, chronic kidney disease), and report worse symptoms than men (Dewan, Rorth, Jhund, et al., 2019; Dewan, Rorth, Raparelli, et al., 2019; Pepine et al., 2020). Women with HF are also more likely than men to report greater psychological distress (e.g., depression, anxiety), increased fatigue, and lower quality of life (Chobufo et al., 2020; Lesman-Leegte et al., 2009; Piepenburg et al., 2019). Cardiovascular death, especially sudden death, however, is lower in women compared to men (Dewan, Rorth, Raparelli, et al., 2019; Pepine et al., 2020). Consequently, women tend to live longer with HF but experience greater symptom burden (Dewan, Rorth, Jhund, et al., 2019; Dewan, Rorth, Raparelli, et al., 2019). Therefore, secondary prevention efforts are necessary to improve outcomes especially among women with HF.
Cardiac rehabilitation (CR) programs offer supervised exercise programs integrated with education and counseling to promote the secondary prevention of HF. Participation in CR is associated with decreased morbidity and mortality (Morris & Chen, 2019). Compared to men, women’s participation in CR is associated with similar or greater improvements in mortality, cardiorespiratory fitness, psychological functions, and quality of life (Galati et al., 2018). Women, however, are less likely to be referred to CR and are also less likely to complete CR even when referred and enrolled relative to men (Colella et al., 2015; Oosenbrug et al., 2016).
Women are less likely to enroll in or complete CR due to multiple concerns, including concerns that aerobic exercise may place an undue strain on the heart, lack of motivation, and elevated depressive symptoms (Resurreccion et al., 2017). Stress management interventions (SMIs) provide stress management training with or without gentle physical exercise and stretching that may be an acceptable, complementary or integrative health (CIH) approach to help women not only manage the psychological distress but also the symptoms of, and treatment for, HF (Baum et al., 1995). Few exercise-based CR programs offer these additional interventions but prior reviews show the potential benefits of SMIs (e.g., cognitive-behavioral therapy, mindfulness, tai chi, yoga) as a CIH approach to CR to reduce psychological distress and increase quality of life among patients with cardiac disease (Blumenthal et al., 2016; Liu et al., 2018). Furthermore, emerging evidence shows that some SMIs such as tai chi and yoga can improve cardiorespiratory endurance among HF patients relative to controls (Gathright et al., 2020). Patient enrolled in CR who experience a reduction in psychosocial distress (e.g., depression) also had a lower mortality rate (Milani & Lavie, 2007; Milani et al., 2011).
Women represent 52% of patients living with HF but are often underrepresented in randomized controlled trials (RCTs) of recommended exercise-based CR for the management of chronic HF (Samayoa et al., 2014; Virani et al., 2020). SMIs can address the psychological and physical concerns that often prevent women from participating in CR but do women with HF participate in SMIs? To our knowledge, women’s participation rates in SMIs for chronic HF has not been documented. Therefore, the purpose of this meta-analysis was to investigate women’s participation rates in RCTs of SMIs for chronic HF and to assess possible predictors of women’s participation (i.e., patient characteristics such as age, race, HF stage, comorbidities, and medications, geographical location, and type of SMI).
METHODS
The Preferred Reported Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in the conduct and preparation of this meta-analysis (Moher et al., 2009). The PRISMA checklist can be found in the Electronic Supplemental Materials (Supplemental Table 1).
Eligibility Criteria
Published studies were included in the meta-analysis if the study (a) evaluated a SMI; (b) sampled chronic HF patients; and (c) used an RCT design. For this meta-analysis, SMIs were operationalized as interventions that included cognitive approaches (e.g., cognitive behavioral stress management, cognitive therapy, or coping skills interventions), relaxation techniques (e.g., mindfulness meditation, biofeedback, progressive muscle relaxation), and exercise-based practices (e.g., tai chi, yoga). Interventions that included aerobic exercise training were excluded because these interventions are provided as part of standard CR.
Information Sources and Search Strategy
Studies were identified using four information sources: (1) electronic bibliographic database (PubMed, PsycINFO, Embase, ProQuest Dissertations & Theses Global, CINAHL, Cochrane Library, ERIC, Global Health, SocIndex, and Web of Science) searches were conducted using a Boolean search string [((“complementary and alternative medicine”) OR (autogenic training) OR (biofeedback) OR (“cognitive restructuring”) OR (“cognitive behavioral stress management”) OR (“deep breathing”) OR (“emotional freedom technique”) OR (guided imagery) OR (“mindfulness-based stress reduction”) OR (mindfulness) OR (meditation) OR (“problem-solving training”) OR (“progressive muscle relaxation”) OR (“relaxation techniques”) OR (self-disclosure) OR (self-hypnosis) OR (tai chi) OR (“transcendental meditation”) OR (yoga) OR (“stress management”)) AND (“heart failure” OR (heart failure))] with no language or geographical restrictions applied; (2) reviewing reference sections of relevant manuscripts; (3) review of electronic tables of contents of related journals; and (4) electronic searches of online databases of funded research (e.g., NIH RePORTER) and clinical trials (ClinicalTrials.gov). Database searches were conducted in August 2017 and repeated annually with the last search conducted in April 2020 to ensure the inclusion of all records published through March 2020.
Study Selection
All records retrieved from the electronic bibliographic database searches were initially screened for inclusion based on title and abstract. The full-text manuscripts of potentially relevant records were retrieved and reviewed for inclusion by the study authors and verified by the PI (LAJSS). If the research was reported in multiple records, the records were linked in the database and represented as a single unit. The record reporting the most complete data was selected as the primary study, additional study records were considered relevant supplemental materials. Relevant research identified from reference sections, journals, and databases of funded research and clinical trials were cross-referenced with the electronic bibliographic database records and were added to the database as additional records as needed.
Data Extraction
Two raters independently coded study information, sample and intervention characteristics, and methodological features of the studies using a coding form with predefined codes. The quality of the studies was assessed using a 17-item methodological quality (MQ) rating form adapted from published checklists (Downs & Black, 1998; Fowkes & Fulton, 1991; Miller et al., 1995); the total possible score is 25 with higher values indicating stronger study quality. Coding discrepancies were reviewed, discussed, and resolved. The interrater reliability was high with 91% agreement between coders for the categorical variables (mean Cohen’s κ = 0.79) and the mean inter-class correlation coefficient for the continuous variables was 0.92 (median = 1.00).
Statistical Analyses
The proportion of women included in each sample (calculated based on the number of women who consented to participate in the study divided by the total number of participants in the sample) was used as the effect size (ES) estimate. Consistent with meta-analytic recommendations, the observed proportions were then converted to logits and used in the analyses (Lipsey & Wilson, 2001). The mean logit and the corresponding 95% confidence intervals (CIs) were calculated using a random-effects model with the between-study variance estimated using restricted maximum likelihood (Lipsey & Wilson, 2001). Results of the analyses (using logits) were converted back to proportions (and corresponding CIs) for ease of interpretation of study findings. The distribution of the ESs surrounding the mean logit ES was assessed using the homogeneity statistic, Q; a significant Q indicates a lack of homogeneity and an inference of heterogeneity. To assess heterogeneity, the I2 index and its corresponding 95% CIs were calculated consistent with a random-effects model (Higgins & Thompson, 2002; Huedo-Medina et al., 2006).
To explain variability in the proportion of women included in the samples, moderator analyses were conducted using meta-regression (following random-effects assumptions with a Knapp-Hartung adjustment) with weights equivalent to the inverse of the variance for the mean logit ESs (Hedges, 1994; Lipsey & Wilson, 2001) These analyses examined a priori selected predictors of women’s participation in SMIs. Patient characteristics (age, race, HF stage, comorbidities, medications), geographical location, and type of SMI (cognitive, relaxation, and exercise-based) were examined as potential moderators of women’s participation. Meta-regression was also used to assess the impact of methodological quality on the proportion of women included in the samples.
Publication bias was assessed by visually inspecting the funnel plot and conducting statistical tests (i.e., Egger’s regression test, Begg’s rank correlation test) (Begg & Mazumdar, 1994; Egger et al., 1997; Sterne & Egger, 2001) Trim-and-fill methods were used to statistically detect and adjust for the possibility of missing studies (Duval & Tweedie, 2000) All statistical analyses were conducted in Stata 16 (LLC, 2020)
RESULTS
Study, Sample, and Intervention Characteristics
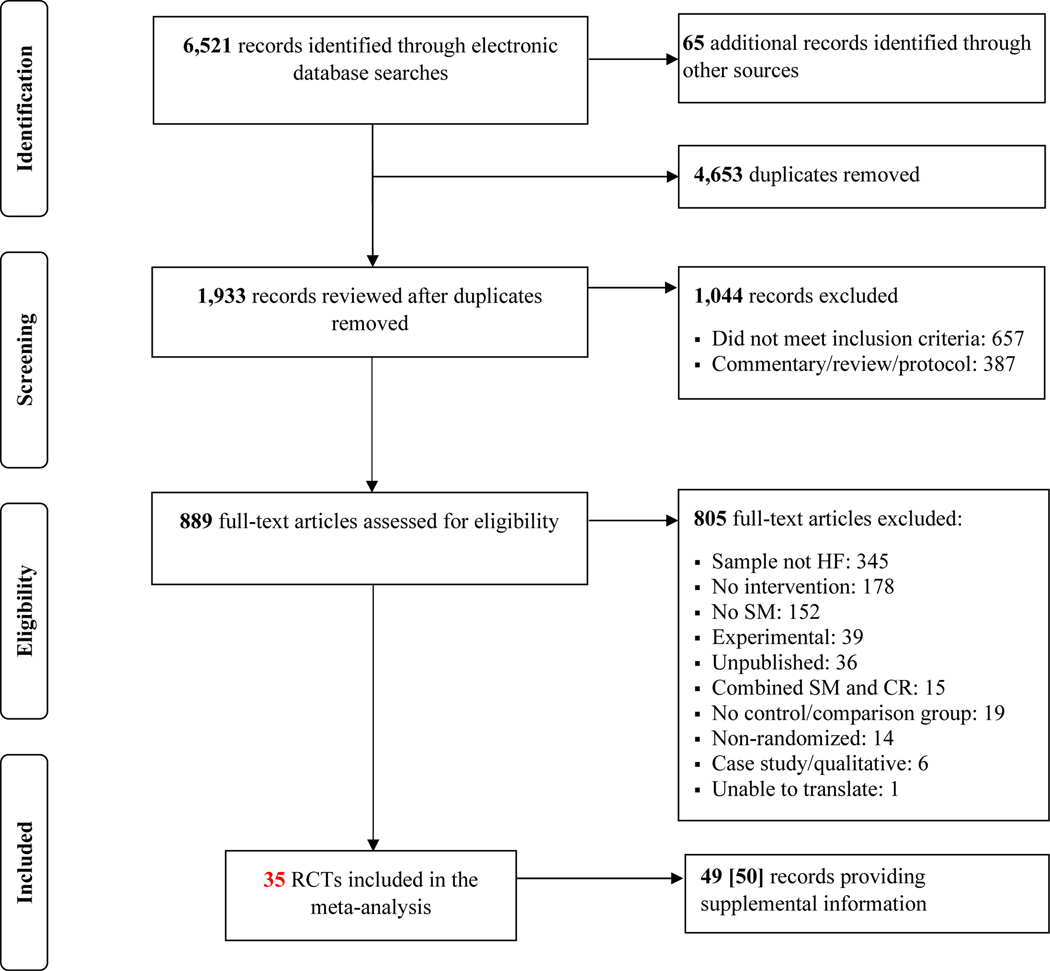
Comprehensive searches revealed 1,933 unique studies; 35 RCTs met inclusion criteria (see Figure 1 for details). Characteristics of the included RCTs are provided in Table 1. Studies were published between 1997 and 2019 with data collection occurring between 1992 and 2018 (mean lag time = 4.11 years, SD = 2.30; range = 1–9 years). The studies were conducted in the United States (43%), China (31%), Sweden (6%), Brazil (3%), Germany (3%), India (3%), Iran (3%), Philippines (3%), Taiwan (3%), and England (3%). Financial support was reported in 20 (57%) of the studies; 15 studies (43%) did not report receiving research funding.
Figure 1.
Search and Selection Procedures. Note. A discrepancy in the total number of studies providing supplemental information is due to the inclusion of Pullen(Pullen et al., 2008) as both a primary study and a linked pilot study for Pullen.(Pullen et al., 2010) HF, heart failure; SM, stress management; CR, cardiac rehabilitation.
Table 1.
Study and Sample Characteristics of the 34 Randomized Controlled Trials Included in the Meta-Analysis.
| Citation | Location | Data Year | N | % F | Age | % NW | % NYHA Class | LVEF I/C | % HTN | % Beta-Blockers | Intervention | Control | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | ||||||||||||
| Aghamohammadi (2019) | Iran | 2019 | 90 | 44 | 69 | NR | 0 | NR | NR | 0 | NR | NR | NR | SM | HE |
| Barrow (2007) | England | 2004 | 69 | 18 | 68 | NR | 0 | NR | NR | 0 | NR | 0 | NR | Tai Chi | UC |
| Bose (2016) | Sweden | 2011 | 103 | 31 | 71 | NR | 0 | 84 | 16 | 0 | NR | 58 | 98 | CET | UC |
| Cajanding (2016) | Philippines | 2013 | 123 | 33 | 56 | NR | 12 | 43 | 40 | 5 | NR | 37 | NR | CBT | UC |
| Chang (2005) * | USA | 2000 | 63 | 1 | 67 | 16 | 0 | 51 | 49 | 0 | 31/30 | NR | 76 | RR | UC |
| Curiati (2005) | Brazil | 2000 | 19 | 74 | 75 | NR | 84 | 16 | 0 | 0 | 57/72 | 95 | 84 | Meditation | HE |
| Dekker (2012) | USA | 2009 | 42 | 45 | 66 | 10 | 0 | 19 | 74 | 7 | 41/38 | 88 | 86 | CBT | UC |
| Freedland (2015) | USA | 2010 | 158 | 46 | 56 | 37 | NR | NR | 42 | 0 | 40/38 | 72 | 92 | CBT | HE |
| Gary (2010) * | USA | 2004 | 36 | 58 | 66 | 28 | 0 | 43 | 57 | 0 | NR | 81 | NR | CBT | UC |
| Hagglund (2018) | Sweden | 2010 | 45 | 22 | 75 | NR | 0 | NR | NR | 0 | NR | NR | NR | Tai Chi | UC |
| Huang (2016) | Taiwan | 2008 | 60 | 33 | 60 | 100 | NR | NR | NR | NR | 49/41 | NR | NR | BFAR | UC |
| Jayadevappa (2007) | USA | 2003 | 31 | 61 | 64 | 100 | 0 | NR | NR | 0 | 27 | NR | NR | TM | HE |
| Krishna (2014) | India | 2011 | 130 | 30 | 50 | NR | 29 | 71 | 0 | 0 | 39/40 | 79 | 78 | Yoga | UC |
| Kristen (2010) | Germany | 2003 | 17 | 35 | 60 | NR | 0 | 82 | 18 | 0 | 29/31 | NR | 100 | Acupuncture | Placebo |
| Li (2012) | China | 2010 | 40 | 53 | 67 | 100 | 0 | 0 | NR | NR | NR | NR | NR | Acupuncture | UC |
| Li (2003) | China | 2010 | 40 | 53 | 67 | 100 | 0 | 0 | NR | NR | NR | 20 | NR | Acupuncture | UC |
| Moser (1997) | USA | 1992 | 43 | 38 | 55 | NR | 0 | 0 | NR | NR | 22/21 | NR | NR | BFAR | AC |
| Pen (2016) | China | 2013 | 61 | 43 | 67 | 100 | 0 | NR | NR | 0 | 32/33 | NR | NR | Tai Chi | UC |
| Powell (2010) | USA | 2001 | 902 | 47 | 64 | 40 | 0 | 68 | 32 | 0 | NR | 75 | 71 | SMC | HE |
| Pullen (2008) | USA | 2006 | 19 | 53 | 51 | 82 | 37 | 26 | 37 | 0 | 28/23 | 89 | 95 | Yoga | UC |
| Pullen (2010) | USA | 2008 | 40 | 43 | 54 | 98 | 28 | 40 | 33 | 0 | 31/27 | 95 | 97 | Yoga | UC |
| Redwine (2019) | USA | 2010 | 48 | 10 | 65 | 40 | NR | NR | NR | NR | 46 | NR | NR | Tai Chi | UC |
| Sang (2015a) | China | 2013 | 60 | 42 | 66 | 100 | 0 | NR | NR | 0 | 35/37 | NR | NR | Tai Chi | UC |
| Sang (2015b) | China | 2013 | 100 | 43 | 71 | 100 | 0 | NR | NR | 0 | 36/37 | 0 | NR | Tai Chi | UC |
| Seo (2016) | USA | 2011 | 73 | 31 | 66 | 0 | 0 | 51 | 46 | 3 | 35/39 | NR | 89 | DBR | HE |
| Sherwood (2017) | USA | 2009 | 199 | 27 | 58 | 0 | 0 | NR | NR | 0 | 32/28 | 74 | 97 | CST | HE |
| Swanson (2009) | USA | 2007 | 35 | 21 | 55 | 20 | NR | NR | NR | 0 | 30/29 | 7 | 100 | Biofeedback | Placebo |
| Wang (2018) | China | 2016 | 60 | 43 | 69 | 100 | 0 | 38 | 62 | 0 | NR | NR | 8 | MBSR | UC |
| Wang (2014) | China | 2009 | 142 | 58 | 62 | NR | 8 | 62 | 17 | 13 | NR | 59 | NR | Biofeedback | UC |
| Yao (2010) | China | 2008 | 150 | 41 | 52 | 100 | 0 | 100 | 0 | 0 | 31/30 | 16 | 48 | Tai Chi | UC |
| Yeh (2011) | USA | 2002 | 30 | 37 | 64 | 43 | 17 | 50 | 27 | 7 | 28/30 | 70 | 90 | Tai Chi | HE |
| Yeh (2004) | USA | 2005 | 100 | 36 | 67 | 14 | 20 | 63 | 17 | 0 | 24/22 | 67 | 86 | Tai Chi | UC |
| Yu (2007) * | Hong Kong | 2002 | 121 | 50 | 75 | 100 | 4 | 56 | 38 | 3 | NR | 68 | 22 | PMRT | HE |
| Zhao (2019) | China | 2017 | 86 | 45 | 61 | 100 | 0 | 46 | 37 | 17 | 41/43 | NR | NR | MBCT | UC |
| Zhao (2018) | China | 2015 | 148 | 49 | 70 | 100 | NR | NR | NR | NR | NR | NR | NR | MBSR | HE |
Sample participating in a non-SMI was excluded: Chang et al. (2005) (Education, n = 32); Gary et al. (2010) (Exercise, n = 20; Exercise/CBT, n = 18); Yu et al. (2007) (Exercise Training, n = 32).
NW, nonwhite; NYHA, New York Heart Association; LVEF, left ventricular ejection fraction; I/C, intervention/control; HTN, hypertension; AC. Attention Control; BFAR, Biofeedback-Assisted Relaxation; CBT, Cognitive Behavioral Therapy; CET, Coping Effectiveness Training; CST, Coping Skills Training; DBR, Diaphragmatic Breathing Retraining; EDUC, Education; HE, Health Education; MBSR, Mindfulness-Based Stress Reduction; MBCT, Mindfulness-Based Cognitive Therapy; PMRT, Progression Muscle Relaxation Therapy; RR, Relaxation Response; SM, Self-Management; SMC, Self-Management Counseling; TM, Transcendental Meditation; UC, Usual Care; NR, Not Reported.
The samples included a total of 3,649 patients who consented to participate in the studies and 3,402 participants were included in the studies’ analyses. All studies recruited patients from clinical settings and included both women and men in the samples. The mean age of the participants was 63.5±7.0 years. In addition, 18 studies reported the age range of the study sample; ages ranged from 18 and 94 years with 67% of the study samples including participants ≥80 years of age. Race of the samples was fully or partially reported in most studies (26 out of 35); 69±36% (range = 6 to 100%) of participants were nonwhite. Less than half of the studies (17 out of 35) assessed baseline depressive symptoms using validated measures (e.g., Beck’s Depression Inventory (Beck et al., 1996), Hamilton Depression Rating Scale (Hamilton, 1960), Hospital Anxiety and Depression Scale(Zigmond & Snaith, 1983)); three studies recruited patients with elevated depressive symptoms (Dekker et al., 2012; Freedland et al., 2015; Gary et al., 2010)
Participants’ clinical characteristics were incompletely described in most studies. Thirty-three studies reported full or partial data on New York Heart Association Classification (NYHA) with 45% of the studies sampling patients classified as NYHA Class II or III. In the studies reporting NYHA Class of the study samples, 11±24% (k = 30) of patients were Class I, 46±28% (k = 22) were Class II, 30±21% (k = 21) were Class III, and 2±4% (k = 30) were Class IV. Twenty-one studies characterized patients’ cardiac functioning using left ventricular ejection fraction (LVEF). The average LVEF was 33±8% (range = 22–46; k = 13); with 35±8% (range = 22–57; k = 20) and 34±11% (range = 21–72; k = 20) for the intervention and control groups, respectively. Comorbidities were common among patients, with 57±32% (k = 20) reporting hypertension, 31±10% (k = 15) reporting diabetes, and 32±9% (k = 10) reporting coronary heart disease. Nineteen studies provided full or partial information on patients’ pharmacotherapy: 79±27% beta-blockers (k = 18), 66±24% angiotensin-converting enzyme inhibitors (k = 18), 69±27% diuretics (k = 15), 53±25% antiplatelets (k = 6), and 63±10% statins (k = 6).
SMIs included tai chi (k = 9), cognitive-behavioral therapy approaches (k = 6), biofeedback (4), yoga (k = 3), acupuncture (k = 3), self-management education/counseling (k = 2), mindfulness-based stress reduction (k = 2), mindfulness-based cognitive therapy (k = 1), progressive muscle relaxation therapy (k = 1), diaphragmatic breathing (k = 1), meditation (k = 1), relaxation, (k = 1), and transcendental meditation (k = 1). Control groups consisted of usual care (k = 22), health-related education/advice (k = 10), placebo (k = 2), and no treatment (assessment only, k = 1).
Prevalence and Predictors of Women’s Participation in SMIs
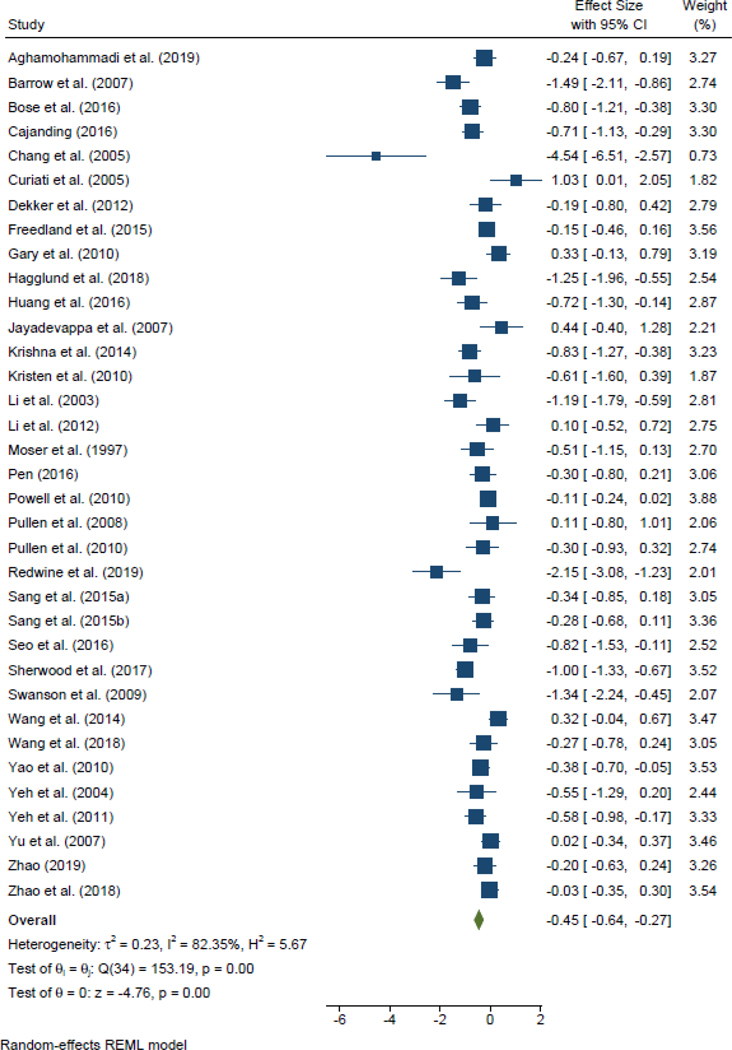
The mean proportion of women who participated in the trials was 38.8% (95% CI=34.9–43.4; I2 = 82.4, 95% CI=81.0–83.6; k = 35; Figure 2). Participation rates did not differ based on age, race, NYHA class, LVEF, comorbidities (i.e., diabetes), geographical location, or type of SMI (Table 2). The proportion of women participants was higher in studies sampling HF patients with hypertension (p =.021) and lower in studies sampling HF patients prescribed with beta-blockers (p = .081). A multiple meta-regression test showed that hypertension and beta-blockers predicted women’s participation in RCTs of SMIs. The model was significant (F [2, 12] = 6.27, p = .014, I2 residual = 62.5%) and accounted for 61% (adjusted R2) of the between-study variance in the mean proportion of women who participated with limited variance remaining (τ2 = .064). Adjusting for multiple testing using the permutation test (20000 permutations) showed that the proportion of women participating in SMIs was associated with lower beta-blocker use (adjusted p-value = .007) but not hypertension (adjusted p-value = .079).
Figure 2.
Forest Plot of the Effect Sizes (and 95% Confidence Intervals) of Women’s Participation Rates in SMIs. Note. Proportions were converted to logits and used in all analyses.
Table 2.
Predictors of Women’s Participation in Randomized Controlled Trials of SMIs for Heart Failure*
| k | Coefficient | SE | p-value | |
|---|---|---|---|---|
| Sample Characteristics | ||||
| Age, mean (SD) | 35 | .009 | .017 | .585 |
| Nonwhite, % | 26 | .559 | .363 | .137 |
| NYHA Class, % | ||||
| I | 30 | −.043 | .530 | .935 |
| II | 22 | −.349 | .504 | .497 |
| III | 21 | .884 | .595 | .154 |
| IV | 30 | 1.364 | 2.840 | .635 |
| LVEF, mean (SD) | 22 | .012 | .018 | .526 |
| Medications, % | ||||
| Beta-blockers | 18 | −.905 | .486 | .081 |
| ACE-inhibitors | 18 | −.557 | .640 | .397 |
| Diuretics | 15 | −.078 | .7567 | .919 |
| Statins | 6 | −2.821 | 1.595 | .152 |
| Antiplatelet | 6 | .059 | .930 | .952 |
| Comorbidities, % | ||||
| Hypertension | 20 | .938 | .372 | .021 |
| Diabetes | 15 | −.149 | 1.419 | .918 |
| CHD | 10 | −1.670 | 2.272 | .483 |
| Study Characteristics | ||||
| United States | ||||
| Yes | 15 | −.116 | .234 | .622 |
| No (Ref) | 20 | |||
| Type of SMI | ||||
| Cognitive | 7 | .273 | .301 | .371 |
| Relaxation | 16 | .321 | .259 | .224 |
| Exercise-based (Ref) | 12 |
k, number of studies; SE, standard error; NYHA, New York Heart Association; LVEF, left ventricular ejection fraction; ACE, angiotensin converting enzyme; CHD, coronary heart disease; SMI, stress management intervention; Ref, reference category.
Unstandardized regression coefficients and the standard errors from each moderator test are presented. Continuous variables (age, non-white, NYHA class, LVEF, medications, and comorbidities) were mean centered; categorical variables were dummy coded (United States: 1 = yes, 0 = no; type of SMI: 1 = Cognitive, 2 = Relaxation, 3 = Exercise-Based). SMIs were categorized as cognitive (e.g., cognitive behavioral therapy, coping skills training), relaxation (e.g., mindfulness-based stress reduction, progressive muscle relaxation), or exercise-based (e.g., tai chi, yoga). Bold variables are significant at the p<.10 level.
The methodological quality of the studies was moderate to high (mean = 70±9%; range = 52–88%); study quality was not associated with women’s participation rate (β = −1.34, SE = 1.12, p = .232). Visual inspection of the funnel plot did not reveal any asymmetries that would indicate publication bias (see Supplemental Figure 1); statistical tests revealed discrepant results (Egger: bias coefficient = −2.23, SE = 0.76, P =.003; Begg: Δx-y = −131.00, z = 1.85, P = 0.065) but trim-and-fill methods indicated that no studies were omitted (estimated ES = 38.8%, 95% CI = 34.5–43.4%).
DISCUSSION
The current study shows that 38.8% of women participated in RCTs of SMIs which is substantially higher than the 19–30% of women who participated in meta-analyses of exercise-based CR for patients with HF (Lewinter et al., 2015; Taylor et al., 2019). Our findings suggest that offering stress management training may be an important consideration for women with HF. Psychosocial stress (e.g., depression, anxiety) has a profound impact on cardiovascular health,(Das & O’Keefe, 2008) and women with HF are more likely to experience higher levels of depressive symptoms, greater anxiety, and worse quality of life compared to men (Moser et al., 2010; Riedinger et al., 2001; Rutledge et al., 2006). While counseling to reduce stress is a recommended component for all patients enrolled in exercise-based CR, stress management training (e.g., cognitive-behavioral stress management, progressive muscle relaxation, meditation, yoga) is not routinely included as a component of traditional CR programs. CR may be an ideal setting to implement stress management training given the improved psychosocial and clinical benefits of enhanced CR + stress management training compared to standard exercise-based CR alone (Blumenthal et al., 2016).
Women’s participation in SMIs was higher in studies sampling women with hypertension and lower in studies enrolling participants using beta blockers. These findings are consistent with the large body of research showing significant sex-differences in the clinical presentation and treatment of HF. Comorbid cardiovascular-related conditions, except for hypertension, are less likely to be diagnosed in women with HF compared to men (Dewan, Rorth, Jhund, et al., 2019). Hypertension is more common among older adults (≥65 years of age) (Ahmad & Oparil, 2017), and women tend to develop HF at an older age, which may explain the sex differences in rates of hypertension among women and men with HF (Bozkurt & Khalaf, 2017). Consistent with these sex-disparities, our moderator analyses showed that samples with higher proportions of hypertensive patients significantly predicted higher rates of women’s participation. In our analyses, age was not a significant predictor of women’s participation, but this may have been a result of a restricted range of ages given that inclusion criteria reported in many of the individual studies restricted participation to patients within a specified age range. Similar to the differences in clinical presentation, women are undertreated relative to men with HF (Dewan, Rorth, Jhund, et al., 2019; Levinsson et al., 2018). Beta blocker therapy tends to be delayed or reduced in women with HF (Baumhakel et al., 2009) even though the efficacy of beta blockers is similar in both women and men.(Kotecha et al., 2016) Furthermore, most studies sampled HF patients with reduced ejection fraction (i.e., patients with LVEF ≤40%) for which beta-blockers are first-line pharmacological therapy. Understanding these sex differences in the clinical presentation and treatment of HF will be important in developing appropriate stress management approaches for women.
The proportion of women enrolled in RCTs of SMIs for HF in the current meta-analysis differ markedly from the proportion of women in the general population of HF patients (38.8% vs. 51.6%). Furthermore, none of the included studies targeted women or reported using strategies to increase women’s participation in the trials. Women are often underrepresented in HF clinical trials (Tahhan et al., 2018), and receive suboptimal HF treatment compared with men (Dewan, Rorth, Jhund, et al., 2019). Future RCTs should enroll a representative sample of the HF population to more completely understand the benefits of SMIs for all HF patients. This could be accomplished by not only specifying inclusion criteria that required equal numbers of women to be enrolled in the trial but also by developing targeted recruitment strategies, educating physicians and other healthcare workers who may refer patients to these trials about the value of stress management, and offering flexible hours, days, and delivery methods for SMIs.
Limitations
There are several limitations of the current meta-analysis that must be considered when interpreting our findings. First, by specifying that the included studies be published RCTs of SMIs for HF, our findings may not be representative of all SMIs for HF. It is well-known that that studies with significant findings are more likely to be published than studies with non-significant findings (i.e., publication bias) and it is also possible that the samples included in published studies may be systematically different from that of unpublished studies. Only published RCTs of SMIs for HF were included as a measure to increase the quality of the included studies and to obtain more reliable results. Second, our findings indicated significant between-study heterogeneity among the 35 included studies with an I2 of 82%. Meta-regression tests were conducted to identify possible sources of heterogeneity, but heterogeneity was only moderately reduced in the final model (I2 = 63%) suggesting at least some between-study heterogeneity could not be explained by the selected moderators. Finally, our moderator tests were limited by the number or completeness of studies reporting on predictors of interest (e.g., race/ethnicity, HF status, comorbidities, medications). More complete reporting of patient demographic and health characteristics is needed for all RCTs of SMIs for HF.
Conclusion
The current study shows that 38.8% of women participated in RCTs of SMIs which is higher than the 19–30% reported in recent meta-analyses of exercise-based CR for patients with HF (Lewinter et al., 2015; Taylor et al., 2019). Future research should explore the potential benefits of offering stress management training to women as part of comprehensive HF care to minimize sex-related gaps in engagement in care.
Supplementary Material
Acknowledgements:
We are grateful to the Systematic Review and Meta-Analysis Research Methods (SMART) Team, especially Julie DeCosta, Marissa L. Donahue, Melissa M. Feulner, and Brittany L. Balletto, for their assistance with data collection.
DECLARATIONS
Funding. This work was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under award number 5R01AT008815 to Lori A. J. Scott-Sheldon, PhD. Emily C. Gathright, PhD was supported by 1K23AG061214 from the National Institute on Aging. Elena Salmoirago-Blotcher is supported by grant 5R01HL149672 from the National Heart, Lung and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure. The authors declare that they have no conflicts of interest.
Availability of data and material. This data used in this meta-analytic review were extracted from published randomized controlled trials of stress management interventions for heart failure patients. The database used to conduct the analyses is available upon request to the first author.
Code availability. The commands used to conduct the meta-analysis are available in Stata 16.0.
References
- Aghamohammadi T, Khaleghipour M, Shahboulaghi F, Dalvandi A, & Maddah S (2019). Effect of self-management program on health status of elderly patients with heart failure: a single-blind, randomized clinical trial [Journal: Article]. Journal of acute disease, 8(5), 179–184. 10.4103/2221-6189.268405 [DOI] [Google Scholar]
- Ahmad A, & Oparil S (2017, Jul). Hypertension in Women: Recent Advances and Lingering Questions. Hypertension, 70(1), 19–26. 10.1161/HYPERTENSIONAHA.117.08317 [DOI] [PubMed] [Google Scholar]
- Barrow DE, Bedford A, Ives G, O’Toole L, & Channer KS (2007). An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: A randomised controlled pilot study. Postgraduate Medical Journal, 83(985), 717–721. 10.1136/pgmj.2007.061267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum A, Herberman H, & Cohen L (1995, Dec). Managing stress and managing illness: Survival and quality of life in chronic disease. J Clin Psychol Med Settings, 2(4), 309–333. 10.1007/BF01991680 [DOI] [PubMed] [Google Scholar]
- Baumhakel M, Muller U, & Bohm M (2009, Mar). Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. European Journal of Heart Failure, 11(3), 299–303. 10.1093/eurjhf/hfn041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II (BDI-II) (Vol. 78). The Psychological Corporation. 10.1037/t00742-000 [DOI] [Google Scholar]
- Begg CB, & Mazumdar M (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 1088–1101. 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Sherwood A, Smith PJ, Watkins L, Mabe S, Kraus WE, Ingle K, Miller P, & Hinderliter A (2016, Apr 5). Enhancing Cardiac Rehabilitation With Stress Management Training: A Randomized, Clinical Efficacy Trial. Circulation, 133(14), 1341–1350. 10.1161/CIRCULATIONAHA.115.018926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bose C, Persson H, Björling G, Ljunggren G, Elfström ML, & Saboonchi F (2016). Evaluation of a coping effectiveness training intervention in patients with chronic heart failure–A randomized controlled trial. European Journal of Cardiovascular Nursing, 15, 537–548. 10.1177/1474515115625033 [DOI] [PubMed] [Google Scholar]
- Bozkurt B, & Khalaf S (2017, Oct-Dec). Heart Failure in Women. Methodist Debakey Cardiovasc J, 13(4), 216–223. 10.14797/mdcj-13-4-216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cajanding RJ (2016). The Effectiveness of a nurse-led cognitive-behavioral therapy on the quality of life, self-esteem and mood among Filipino patients living with heart failure: A randomized controlled trial. Applied Nursing Research, 31, 86–93. 10.1016/j.apnr.2016.01.002 [DOI] [PubMed] [Google Scholar]
- Chang BH, Hendricks A, Zhao Y, Rothendler JA, LoCastro JS, & Slawsky MT (2005). A relaxation response randomized trial on patients with chronic heart failure. Journal of Cardiopulmonary Rehabilitation, 25, 149–157. 10.1097/00008483-200505000-00005 [DOI] [PubMed] [Google Scholar]
- Chobufo MD, Khan S, Agbor VN, Rahman E, Foryoung JB, Jolayemi A, Jonnadula S, Patel N, Enoru S, Dufresne A, & Nfor T (2020, Feb 15). 10-Year trend in the prevalence and predictors of depression among patients with heart failure in the USA from 2007–2016. International Journal of Cardiology, 301, 123–126. 10.1016/j.ijcard.2019.09.028 [DOI] [PubMed] [Google Scholar]
- Colella TJ, Gravely S, Marzolini S, Grace SL, Francis JA, Oh P, & Scott LB (2015, Apr). Sex bias in referral of women to outpatient cardiac rehabilitation? A meta-analysis. European Journal of Preventive Cardiology, 22(4), 423–441. 10.1177/2047487314520783 [DOI] [PubMed] [Google Scholar]
- Curiati JA, Bocchi E, Freire JO, Arantes AC, Braga M, Garcia Y, Guimaraes G, & Fo WJ (2005). Meditation reduces sympathetic activation and improves the quality of life in elderly patients with optimally treated heart failure: A prospective randomized study. Journal of Alternative and Complementary Medicine, 11, 465–472. 10.1089/acm.2005.11.465 [DOI] [PubMed] [Google Scholar]
- Das S, & O’Keefe JH (2008, Oct). Behavioral cardiology: recognizing and addressing the profound impact of psychosocial stress on cardiovascular health. Curr Hypertens Rep, 10(5), 374–381. 10.1007/s11906-008-0070-6 [DOI] [PubMed] [Google Scholar]
- Dekker RL, Moser DK, Peden AR, & Lennie TA (2012). Cognitive therapy improves three-month outcomes in hospitalized patients with heart failure. Journal of Cardiac Failure, 18, 10–20. 10.1016/j.cardfail.2011.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewan P, Rorth R, Jhund PS, Shen L, Raparelli V, Petrie MC, Abraham WT, Desai AS, Dickstein K, Kober L, Mogensen UM, Packer M, Rouleau JL, Solomon SD, Swedberg K, Zile MR, & McMurray JJV (2019, Jan 8). Differential Impact of Heart Failure With Reduced Ejection Fraction on Men and Women. J Am Coll Cardiol, 73(1), 29–40. 10.1016/j.jacc.2018.09.081 [DOI] [PubMed] [Google Scholar]
- Dewan P, Rorth R, Raparelli V, Campbell RT, Shen L, Jhund PS, Petrie MC, Anand IS, Carson PE, Desai AS, Granger CB, Kober L, Komajda M, McKelvie RS, O’Meara E, Pfeffer MA, Pitt B, Solomon SD, Swedberg K, Zile MR, & McMurray JJV (2019, Dec). Sex-Related Differences in Heart Failure With Preserved Ejection Fraction. Circ Heart Fail, 12(12), e006539. 10.1161/circheartfailure.119.006539 [DOI] [PubMed] [Google Scholar]
- Dharmarajan K, & Rich MW (2017, Jul). Epidemiology, Pathophysiology, and Prognosis of Heart Failure in Older Adults. Heart Fail Clin, 13(3), 417–426. 10.1016/j.hfc.2017.02.001 [DOI] [PubMed] [Google Scholar]
- Downs SH, & Black N (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology & Community Health, 52(6), 377–384. 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. 10.1111/j.0006-341x.2000.00455.x [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowkes F, & Fulton P (1991). Critical appraisal of published research: introductory guidelines. British Medical Journal, 302(6785), 1136–1140. 10.1136/bmj.302.6785.1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedland KE, Carney RM, Rich MW, Steinmeyer BC, & Rubin EH (2015). Cognitive behavior therapy for depression and self-care in heart failure patients: A randomized clinical trial. JAMA Internal Medicine, 175, 1773–1782. 10.1001/jamainternmed.2015.5220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galati A, Piccoli M, Tourkmani N, Sgorbini L, Rossetti A, Cugusi L, Bellotto F, Mercuro G, Abreu A, D’Ascenzi F, & Working Group on Cardiac Rehabilitation of the Italian Society of, C. (2018, Dec). Cardiac rehabilitation in women: state of the art and strategies to overcome the current barriers. J Cardiovasc Med (Hagerstown), 19(12), 689–697. 10.2459/JCM.0000000000000730 [DOI] [PubMed] [Google Scholar]
- Gary RA, Dunbar SB, Higgins MK, Musselman DL, & Smith AL (2010). Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. Journal of Psychosomatic Research, 69, 119–131. 10.1016/j.jpsychores.2010.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gathright EC, Salmoirago-Blotcher E, DeCosta J, Donahue ML, Feulner MM, Cruess DG, Wing RR, Carey MP, & Scott-Sheldon LAJ (2020). Stress management interventions for adults living with heart failure: A systematic review and meta-analysis. The Miriam Hospital. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagglund L, Boman K, & Brannstrom M (2018, Apr). A mixed methods study of Tai Chi exercise for patients with chronic heart failure aged 70 years and older. Nursing Open, 5(2), 176–185. 10.1002/nop2.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62. 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges LV (1994). Fixed effects models. In Cooper H & Hedges LV (Eds.), The Handbook of Research Synthesis (pp. 285–299). Russell Sage Foundation. [Google Scholar]
- Higgins JP, & Thompson SG (2002, Jun 15). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- Huang T-Y, Moser DK, & Hwang S-L (2016). The short-term and long-term effects of biofeedback-assisted relaxation therapy in patients with heart failure: A randomized control study. SAGE Open Nursing, Jan-Dec, 1–8. 10.1177/2377960816680825 [DOI] [Google Scholar]
- Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, & Botella J (2006, Jun). Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods, 11(2), 193–206. https://doi.org/2006-07641-005 [pii] 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, & Ritchey MD (2018, Dec). National Burden of Heart Failure Events in the United States, 2006 to 2014. Circ Heart Fail, 11(12), e004873. 10.1161/circheartfailure.117.004873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayadevappa R, Johnson JC, Bloom BS, Nidich S, Desai S, & Chhatre S (2007). Effectiveness of transcendental meditation on functional capacity and quality of life of African Americans with congestive heart failure: A randomized control study. Ethnicity & Disease, 17(1), 72–77. [PMC free article] [PubMed] [Google Scholar]
- Kotecha D, Manzano L, Krum H, Rosano G, Holmes J, Altman DG, Collins PD, Packer M, Wikstrand J, Coats AJ, Cleland JG, Kirchhof P, von Lueder TG, Rigby AS, Andersson B, Lip GY, van Veldhuisen DJ, Shibata MC, Wedel H, Bohm M, Flather MD, & Beta-Blockers in Heart Failure Collaborative, G. (2016, Apr 20). Effect of age and sex on efficacy and tolerability of beta blockers in patients with heart failure with reduced ejection fraction: individual patient data meta-analysis. British Medical Journal, 353, i1855. 10.1136/bmj.i1855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishna BH, Pal P, Pal GK, Balachander J, Jayasettiaseelon E, Sreekanth Y, Sridhar MG, & Gaur GS (2014). A randomized controlled trial to study the effect of yoga therapy on cardiac function and n terminal pro BNP in heart failure. Integrative Medicine Insights(9), 1–6. 10.4137/IMI.S13939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristen AV, Schuhmacher B, Strych K, Lossnitzer D, Friederich H-C, Hilbel T, Haass M, Katus HA, Schneider A, & Streitberger KM (2010). Acupuncture improves exercise tolerance of patients with heart failure: a placebo-controlled pilot study. Heart, 96, 1396–1400. [DOI] [PubMed] [Google Scholar]
- Lesman-Leegte I, Jaarsma T, Coyne JC, Hillege HL, Van Veldhuisen DJ, & Sanderman R (2009, Feb). Quality of life and depressive symptoms in the elderly: a comparison between patients with heart failure and age- and gender-matched community controls. Journal of Cardiac Failure, 15(1), 17–23. 10.1016/j.cardfail.2008.09.006 [DOI] [PubMed] [Google Scholar]
- Levinsson A, Dube MP, Tardif JC, & de Denus S (2018, Oct). Sex, drugs, and heart failure: A sex-sensitive review of the evidence base behind current heart failure clinical guidelines. ESC Heart Fail, 5(5), 745–754. 10.1002/ehf2.12307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinter C, Doherty P, Gale CP, Crouch S, Stirk L, Lewin RJ, LeWinter MM, Ades PA, Kober L, & Bland JM (2015, Dec). Exercise-based cardiac rehabilitation in patients with heart failure: a meta-analysis of randomised controlled trials between 1999 and 2013. European Journal of Preventive Cardiology, 22(12), 1504–1512. 10.1177/2047487314559853 [DOI] [PubMed] [Google Scholar]
- Li JZ, Yan; Li Jie. (2003). Clinical Research on the Effects of Acupuncture on the Left Ventricular Contraction Function in Symptomless Cardiac Failure Patients. World Journal of Acupuncture-Moxibustion, 13(2), 16–19. [Google Scholar]
- Li Z. y., Lao M. x., & Pan Q. j. (2012). Effect of acupuncture on hemodynamics and cardiac function in patients with chronic heart failure. Shanghai J Acu-mox, 31(7), 480–482. [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical Meta-Analysis. Sage. [Google Scholar]
- Liu T, Chan AW, Liu YH, & Taylor-Piliae RE (2018, Apr). Effects of Tai Chi-based cardiac rehabilitation on aerobic endurance, psychosocial well-being, and cardiovascular risk reduction among patients with coronary heart disease: A systematic review and meta-analysis. European Journal of Cardiovascular Nursing, 17(4), 368–383. 10.1177/1474515117749592 [DOI] [PubMed] [Google Scholar]
- LLC S (2020). Stata/SE 16.1 for Windows. In [Google Scholar]
- Milani RV, & Lavie CJ (2007, Sep). Impact of cardiac rehabilitation on depression and its associated mortality. The American Journal of Medicine, 120(9), 799–806. 10.1016/j.amjmed.2007.03.026 [DOI] [PubMed] [Google Scholar]
- Milani RV, Lavie CJ, Mehra MR, & Ventura HO (2011, Jan). Impact of exercise training and depression on survival in heart failure due to coronary heart disease. The American Journal of Cardiology, 107(1), 64–68. 10.1016/j.amjcard.2010.08.047 [DOI] [PubMed] [Google Scholar]
- Miller W, Brown J, & Simpson T (1995). What works? A methodological analysis of the alcohol treatment outcome literature. In Miller W, Brown J, Simpson T, Handmaker N, Thomas B, Luckie L, Montgomery H, Hester R, & Tonigan J (Eds.), Handbook of Alcoholism Treatment Approaches: Effective Alternatives (2nd ed., pp. 12–44). Alynn & Bacon. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- Morris JH, & Chen L (2019, Feb). Exercise Training and Heart Failure: A Review of the Literature. Card Fail Rev, 5(1), 57–61. 10.15420/cfr.2018.31.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser D, Dracup K, Woo M, & Stevenson L (1997). Voluntary control of vascular tone by using skin-temperature biofeedback-relaxation in patients with advanced heart failure [Clinical Trial; Comparative Study; Randomized Controlled Trial; Research Support, Non-U.S. Gov’t; Research Support, U.S. Gov’t, P.H.S.]. Alternative Therapies in Health and Medicine, 3(1), 51–59. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/814/CN-00135814/frame.html [PubMed] [Google Scholar]
- Moser DK, Dracup K, Evangelista LS, Zambroski CH, Lennie TA, Chung ML, Doering LV, Westlake C, & Heo S (2010, Sep-Oct). Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart Lung, 39(5), 378–385. 10.1016/j.hrtlng.2009.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosenbrug E, Marinho RP, Zhang J, Marzolini S, Colella TJ, Pakosh M, & Grace SL (2016, Nov). Sex Differences in Cardiac Rehabilitation Adherence: A Meta-analysis. Can J Cardiol, 32(11), 1316–1324. 10.1016/j.cjca.2016.01.036 [DOI] [PubMed] [Google Scholar]
- Pen XF (2016). Effect of Taijiquan exercise on cardiac function and quality of life in patients with chronic heart failure Chinese Journal of Physical Medicine and Rehabilitation, 38, 51–53. [Google Scholar]
- Pepine CJ, Merz CNB, El Hajj S, Ferdinand KC, Hamilton MA, Lindley KJ, Nelson MD, Quesada O, Wenger NK, & Fleg JL (2020, Apr 1). Heart failure with preserved ejection fraction: Similarities and differences between women and men. International Journal of Cardiology, 304, 101–108. 10.1016/j.ijcard.2020.01.003 [DOI] [PubMed] [Google Scholar]
- Piepenburg SM, Faller H, Stork S, Ertl G, & Angermann CE (2019, Mar). Symptom patterns and clinical outcomes in women versus men with systolic heart failure and depression. Clin Res Cardiol, 108(3), 244–253. 10.1007/s00392-018-1348-6 [DOI] [PubMed] [Google Scholar]
- Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, Jaarsma T, Krum H, Rastogi V, & Rohde LE (2014). Heart failure: preventing disease and death worldwide. ESC Heart Failure, 1(1), 4–25. 10.1002/ehf2.12005 [DOI] [PubMed] [Google Scholar]
- Powell LH, Calvin JE Jr, Richardson D, Janssen I, Mendes De Leon CF, Flynn KJ, Grady KL, Rucker-Whitaker CS, Eaton C, & Avery E (2010). Self-management counseling in patients with heart failure: The heart failure adherence and retention randomized behavioral trial. Journal of the American Medical Association, 304(12), 1331–1338. 10.1001/jama.2010.1362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullen P, Thompson W, Benardot D, Brandon L, Mehta P, Rifai L, Vadnais D, Parrott J, & Khan B (2010). Benefits of yoga for African American heart failure patients. Medicine and Science in Sports and Exercise, 42(4), 651–657. 10.1249/MSS.0b013e3181bf24c4 [DOI] [PubMed] [Google Scholar]
- Pullen PR, Nagamia SH, Mehta PK, Thompson WR, Benardot D, Hammoud R, Parrott JM, Sola S, & Khan BV (2008). Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. Journal of Cardiac Failure, 14(5), 407–413. 10.1016/j.cardfail.2007.12.007 [DOI] [PubMed] [Google Scholar]
- Redwine LS, Wilson K, Pung MA, Chinh K, Rutledge T, Mills PJ, & Smith B (2019). A Randomized Study Examining the Effects of Mild-to-Moderate Group Exercises on Cardiovascular, Physical, and Psychological Well-being in Patients With Heart Failure. Journal of Cardiopulmonary Rehabilitation and Prevention, 39(6), 403–408. 10.1097/HCR.0000000000000430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resurreccion DM, Motrico E, Rigabert A, Rubio-Valera M, Conejo-Ceron S, Pastor L, & Moreno-Peral P (2017, Aug). Barriers for Nonparticipation and Dropout of Women in Cardiac Rehabilitation Programs: A Systematic Review. J Womens Health (Larchmt), 26(8), 849–859. 10.1089/jwh.2016.6249 [DOI] [PubMed] [Google Scholar]
- Riedinger MS, Dracup KA, Brecht ML, Padilla G, Sarna L, & Ganz PA (2001, Mar-Apr). Quality of life in patients with heart failure: do gender differences exist? Heart Lung, 30(2), 105–116. 10.1067/mhl.2001.114140 [DOI] [PubMed] [Google Scholar]
- Rutledge T, Reis VA, Linke SE, Greenberg BH, & Mills PJ (2006, Oct 17). Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol, 48(8), 1527–1537. 10.1016/j.jacc.2006.06.055 [DOI] [PubMed] [Google Scholar]
- Samayoa L, Grace SL, Gravely S, Scott LB, Marzolini S, & Colella TJ (2014, Jul). Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can J Cardiol, 30(7), 793–800. 10.1016/j.cjca.2013.11.007 [DOI] [PubMed] [Google Scholar]
- Sang Lin L, Lang F, & Tian Y (2015a). Influence of “tai chi kangfu cao” on angiotensin II and brain natriuretic peptide in plasma of elderlypatients with chronic heart failure of coronary heart disease. Chinese Journal of Gerontology, 16, 4599–4600. [Google Scholar]
- Sang Lin L, Lang F, & Tian Y (2015b). Influence of “tai chi kangfu cao” on cardiac function and quality of life in elderly patients with chronic heart failure of coronary heart disease. Chinese Journal of Gerontology, 14, 3957–3958. [Google Scholar]
- Seo Y, Yates B, LaFramboise L, Pozehl B, Norman JF, & Hertzog M (2016). A home-based diaphragmatic breathing retraining in rural patients with heart failure. Western Journal of Nursing Research, 38(3), 270–291. 10.1177/0193945915584201 [DOI] [PubMed] [Google Scholar]
- Sherwood A, Blumenthal JA, Koch GG, Hoffman BM, Watkins LL, Smith PJ, O’Connor CM, Adams KF, Rogers JG, & Sueta C (2017). Effects of Coping Skills Training on Quality of Life, Disease Biomarkers, and Clinical Outcomes in Patients With Heart Failure: A Randomized Clinical Trial. Circulation: Heart failure, 10(1), e003410. 10.1161/CIRCHEARTFAILURE.116.003410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JA, & Egger M (2001). Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. Journal of Clinical Epidemiology, 54(10), 1046–1055. 10.1016/s0895-4356(01)00377-8 [DOI] [PubMed] [Google Scholar]
- Swanson KS, Gevirtz RN, Brown M, Spira J, Guarneri E, & Stoletniy L (2009). The Effect of Biofeedback on Function in Patients with Heart Failure. Applied Psychophysiology and Biofeedback, 34(2), 71–91. 10.1007/s10484-009-9077-2 [DOI] [PubMed] [Google Scholar]
- Tahhan AS, Vaduganathan M, Greene SJ, Fonarow GC, Fiuzat M, Jessup M, Lindenfeld J, O’Connor CM, & Butler J (2018, Oct 1). Enrollment of Older Patients, Women, and Racial and Ethnic Minorities in Contemporary Heart Failure Clinical Trials: A Systematic Review. JAMA Cardiol, 3(10), 1011–1019. 10.1001/jamacardio.2018.2559 [DOI] [PubMed] [Google Scholar]
- Taylor RS, Long L, Mordi IR, Madsen MT, Davies EJ, Dalal H, Rees K, Singh SJ, Gluud C, & Zwisler AD (2019, Aug). Exercise-Based Rehabilitation for Heart Failure: Cochrane Systematic Review, Meta-Analysis, and Trial Sequential Analysis. JACC Heart Fail, 7(8), 691–705. 10.1016/j.jchf.2019.04.023 [DOI] [PubMed] [Google Scholar]
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW, American Heart Association Council on, E., Prevention Statistics, C., & Stroke Statistics, S. (2020, Mar 3). Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation, 141(9), e139–e596. 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- Wang F, Shen G, & Feng J (2018). Influences of mindfulness - based stress reduction on self - perceived burden and medication compliance of patients with chronic heart failure. Anhui Medical Journal, 39(9). 10.3969/j. [DOI] [Google Scholar]
- Wang L-N, Tao H, Zhao Y, Zhou Y-Q, & Jiang X-R (2014). Optimal timing for initiation of biofeedback-assisted relaxation training in hospitalized coronary heart disease patients with sleep disturbances. The Journal of Cardiovascular Nursing, 29(4), 367–376. 10.1097/jcn.0b013e318297c41b [DOI] [PubMed] [Google Scholar]
- Yao C, Li F, & Ma Y (2010). Effects of shadow boxing on rehabilitation in patients with chronic heart failure. Chinese Journal of Cardiovascular Rehabilitation Medicine, 19, 364–367. [Google Scholar]
- Yeh GY, McCarthy EP, Wayne PM, Stevenson LW, Wood MJ, Forman D, Davis RB, & Phillips RS (2011). Tai Chi Exercise in Patients With Chronic Heart Failure A Randomized Clinical Trial. Archives of Internal Medicine, 171(8), 750–757. 10.1016/j.cardfail.2010.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, Goldberger AL, Davis RB, & Phillips RS (2004). Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. American Journal of Medicine, 117(8), 541–548. 10.1016/j.amjmed.2004.04.016 [DOI] [PubMed] [Google Scholar]
- Yu DS, Lee DT, & Woo J (2007). Effects of relaxation therapy on psychologic distress and symptom status in older Chinese patients with heart failure. Journal of Psychosomatic Research, 62(4), 427–437. 10.1016/j.jpsychores.2006.10.012 [DOI] [PubMed] [Google Scholar]
- Zhao H, Yuan Y, & Chen C (2018). Effects of mindfulness-based stress reduction training on negative emotions in elderly patients with chronic heart failure. Chinese Journal of Modern Nursing, 19, 2315–2318. [Google Scholar]
- Zhao M (2019). Effect of mindfulness—-based cognitive therapy on psychological status and quality of life in patients with chronic heart failure. Tianjin Journal of Nursing, 27(5). [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.