Abstract
Study objective
To evaluate whether an Intensive Cardiac Rehabilitation (ICR) program improves depression and cardiac self-efficacy among patients with a qualifying cardiac diagnosis.
Design
Prospective, longitudinal cohort design.
Setting
Single-center, tertiary referral, outpatient cardiac rehabilitation center.
Participants
Patients with a qualifying diagnosis for ICR.
Interventions
Outpatient ICR.
Main outcome measure(s)
Mental health, as assessed using the Patient Health Questionnaire-9 (PHQ-9) and cardiac self-efficacy using the Cardiac Self-Efficacy (CSE) scale.
Results
Of the 268 patients included (median age 69 y, 73% men), 70% had no depressive symptoms at baseline (PHQ-9 score <5). PHQ-9 scores improved in the overall sample (p < 0.0001), with greater improvements among patients with mild depressive symptoms at baseline (−4 points, p < 0.001) and those with moderate to severe depressive symptoms at baseline (−5.5 points, p < 0.001). Cardiac self-efficacy improved overall, and the two subsections of the cardiac self-efficacy questionnaire titled, “maintain function” and “control symptoms” improved (all p < 0.001).
Conclusions
Participation in an outpatient ICR program is associated with fewer depressive symptoms and greater cardiac self-efficacy among patients with CVD who qualify for ICR. The improvement in depression was greatest for those with moderate to severe depressive symptoms.
Keywords: Depression, Cardiovascular disease, Intensive Cardiac Rehabilitation, Cardiac self-efficacy
1. Introduction
It is estimated that one in four patients with cardiovascular disease (CVD) also concurrently suffers from depression [1]. In addition, patients with CVD frequently report low self-efficacy, which reflects an impaired confidence in their ability to “overcome a difficult situation or accomplish a certain behavioral goal” [2]. Self-efficacy is inversely related to both depression and anxiety [2]. Poor self-efficacy not only negatively affects quality of life but also feeds forward and negatively affects behaviors (such as medication adherence), which may worsen quality of life [3], [4]. Importantly, depression and reduced cardiac self-efficacy are associated with higher mortality rates following major cardiac events [3]. Given that CVD and depression are common, chronic, and debilitating conditions that frequently overlap and negatively impact health outcomes, research on effective treatments for concurrent diagnoses is warranted. Traditional cardiac rehabilitation (CR) programs involve 36 sessions of exercise in a monitored outpatient healthcare setting. It has been demonstrated that participation in traditional CR results in reductions in depressive symptoms and the associated excess mortality [5]. Intensive Cardiac Rehabilitation (ICR) has the same Medicare indications for patient referral as traditional CR; however, ICR is comprised of up to 36 sessions of education classes in addition to a maximum of 36 sessions of exercise. There are three ICR programs approved by the Centers for Medicare & Medicaid Services. Participation in a residential ICR program has been demonstrated to lower CVD risk factors, [6], [7], but effects on cardiac self-efficacy are unknown. Moreover, the effect that participation in outpatient ICR confers on depressive symptoms and cardiac self-efficacy remains unknown. Thus, we sought to test the hypothesis that participation in an outpatient ICR program will be associated with a reduction in depressive symptoms. Our secondary goal was to determine the effect of ICR on cardiac self-efficacy because self-efficacy is associated with greater well-being and physical functioning [8], [9], [10]. To address these hypotheses, we performed a prospective, longitudinal, observational cohort study.
2. Materials and methods
2.1. Design
This was a single group study design with participants completing the Patient Health Questionnaire 9 (PHQ-9) and Cardiac Self-Efficacy (CSE) scale at their initial and 24th visits. This study was approved by the Washington University in St. Louis Institutional Review Board. All patients provided written informed consent.
2.2. Sample
Patients were referred to outpatient ICR by their healthcare provider according to eligibility based on Medicare guidelines. The eligibility criteria include at least one of the following cardiac index events: acute myocardial infarction (MI), coronary artery bypass graft surgery (CABG), stable angina pectoris, heart valve repair or replacement, percutaneous transluminal coronary angioplasty or coronary stenting (PCI), heart or heart-lung transplant, or heart failure (HF) with reduced ejection fraction (i.e., left ventricular ejection fraction ≤ 35%) with no documented HF hospitalizations or procedures within the preceding 6 weeks. Subjects had to be referred by a physician for ICR. Exclusion criteria for this study included inability to give informed consent, patients who knew a priori that they would not participate in at least 24 visits, and lack of PHQ-9 data. Thus, all patients had to have completed pre-ICR and post 24 visits of ICR PHQ9 questionnaires to be included in this analysis.
2.3. Intensive Cardiac Rehabilitation program
The ICR program was comprised of a series of 36 education sessions that address eating healthfully, exercising regularly, and having a healthy mindset in addition to the exercise sessions that are included in traditional CR. The ICR program consists of a maximum of 36 visits, with 2 sessions per visit. Patients were scheduled to attend ~2–3 visits per week; each visit was comprised of one session of supervised monitored exercise and one session of cardiac health education on topics ranging from heart-healthy cooking classes to videos about heart-healthy lifestyle change. This education curriculum includes videos such as “Healthy Minds, Bodies, and Hearts”, “How Our Thoughts Can Heal Our Hearts”, and workshops such as “Stress and Health Workshop”, “Taking Charge of Stress”, “New Thoughts, New Behaviors”, “Managing Moods and Relationships”, and “Mindful Eating”.
The follow-up timepoint of 24 visits was prospectively chosen to balance considerations of study retention and effect of ICR. Most patients at the Washington University School of Medicine/Barnes-Jewish Hospital Heart Care Institute ICR complete at least 24 visits; fewer complete 36 visits.
2.4. Outcome variables and measures
The PHQ-9 was used to assess depressive symptoms [11]. Each question asks patients to rate whether they have experienced symptoms in the last 2 weeks on a Likert scale of 0 to 3 for each of the 9 cardinal symptoms of major depression. A score of 0 indicates that the patient experienced the symptom “not at all”, 1 indicates “several days”, 2 indicates “more than half the days”, and 3 indicates “nearly every day”. The PHQ-9 has 9 questions, with a score range of 0 to 27. A score of 0–4 indicates no depression, scores 5–9 indicate mild depression, 10–14 indicates moderate depression, 15–19 indicates moderately severe depression, and 20 or above indicates severe depression. If a patient scored above the mild depression range (>9 on the PHQ-9), their primary care doctor was notified, and their PHQ-9 form was faxed to their office; patients were not directly referred to a mental health professional. All patients had equal time with the ICR team and did not receive additional services or treatment based on their baseline PHQ-9.
The CSE questionnaire was used to assess patients' belief in their ability to manage the challenges posed by CVD [12]. Each question asks the patient to rate their level of confidence that they can manage their CVD using a five-point Likert scale. A score of 0 indicates “not at all”, 1 “somewhat confident”, 2 “moderately confident”, 3 “very confident”, and 4 “completely confident”. The cardiac self-efficacy questionnaire has 16 items and the total score range is 0 to 64 points, with higher scores indicating greater self-efficacy. The cardiac self-efficacy is comprised of 2 subscores: “control symptoms” refers to a patient's belief in their ability to regulate the symptoms of their CVD and is comprised of eight questions, while the “maintain function” subsection refers to a patient's belief in their ability to maintain physical functionality and is comprised of five questions. Three questions are not included in either subscore. Each subscore is quantified by taking the mean value of the corresponding subset of questions, on a scale of 0 to 4. Patients completed the PHQ-9 and CSE questionnaires during their initial appointment at baseline and again during the follow-up visit.
2.5. Data analysis
Study data were collected and managed using REDCap electronic data capture tools hosted at Washington University in St. Louis, Missouri [13], [14]. Categorical variables are reported as number (%). Continuous variables are reported as mean ± standard deviation for normally distributed variables and median and interquartile range [IQR] when non-normally distributed. Changes in depression severity and cardiac self-efficacy were assessed using a paired, nonparametric Wilcoxon test. A post-hoc analysis excluding those patients who started antidepressant medications during the study was also performed. Correlation between the improvement in 6 min walk test and PHQ-9/CSE scores was assessed using Spearman correlation coefficients. Baseline and follow-up antidepressants use was compared using McNemar test. The analyses were performed using R statistical software version 4.0.2 (R Core Team (2021) R Foundation for Statistical Computing, Vienna, Austria).
3. Results
The baseline characteristics of enrolled intensive cardiac rehabilitation (ICR) patients (N = 268) are listed in Table 1. On average, patients were in their 7th decade, and were majority white and male. Nearly half were never smokers, nearly a quarter had a diagnosis of diabetes, and over two-thirds had a diagnosis of hypertension. Prior to enrollment, patients had experienced one or more cardiac index events. The most common referral diagnosis was a percutaneous coronary intervention (PCI), with over half of patients having undergone angioplasty with or without stent placement or other PCI. Several patients had more than one qualifying diagnoses (e.g., myocardial infarction and PCI). The average patient at baseline had a body mass index (BMI) in the overweight category. The median waist circumference in both men and women would qualify as one of the diagnostic criteria for metabolic syndrome. At baseline, on average, patients had normal cholesterol concentrations, likely due in part to more than 80% of patients being on statin therapy (Table 2). Baseline hemodynamics, on average, were also in the normal range, but the median six-minute walk distance (495 m) was lower than the 50th percentile reported in the literature for healthy adults aged 60–69 years old [15]. The median time (and interquartile range [IQR]) for the time between the pre-ICR evaluation and the post-ICR evaluation was 70 days [IQR 61, 84 days]. BMI, waist circumference, blood pressure, resting heart rate, and total cholesterol all significantly decreased, while six-minute walk distance and handgrip strength improved from pre-ICR to post-24 visits of ICR (see Supplemental Table 1).
Table 1.
Baseline characteristics of study population (n = 268).
| Characteristics | n (%), median [IQR], or mean ± SD |
|---|---|
| Demographics/cardiac risk factors | |
| Age (years) | 69 [62, 75] |
| Race (White) | 250 (93.3) |
| Biological sex, male | 195 (72.8) |
| Smoking | |
| Never | 121 (46.5) |
| Past | 131 (50.4) |
| Current | 8 (3.1) |
| Body mass index (kg/m2) | 29.0 [26.4, 33.2] |
| Waist circumference in women (cm) | 96.5 [87.6, 110.2] |
| Waist circumference in men (cm) | 105.4 [96.5, 115.6] |
| History of hypertension | 184 (68.7) |
| History of diabetes | 60 (22.4) |
| Total cholesterol (mg/dL) | 133 [113, 154] |
| LDL-cholesterol (mg/dL) | 59 [45, 76] |
| HDL-cholesterol (mg/dL) | 43 [36, 52] |
| Cardiac index eventsaN (%) | |
| Acute myocardial infarction | 91 (34.0) |
| Acute ST elevation myocardial infarction | 39 (43.8) |
| Coronary artery bypass graft | 57 (21.3) |
| Stable angina pectoris | 16 (6.0) |
| Valve replacement/repair | 53 (19.8) |
| Percutaneous coronary intervention procedures | 155 (57.8) |
| Angioplasty | 34 (12.7) |
| Stent | 136 (50.7) |
| Other | 1 (0.4) |
| Heart transplant | 3 (1.1) |
| Heart failure | 67 (25.0) |
| Left ventricular assist device | 1 (0.4) |
| Exercise performance and hemodynamics | |
| 6 minute walk distance (m) | 495 [410, 555] |
| Right hand grip (kg) | 32 [25, 40] |
| Left hand grip (kg) | 31 [23, 39] |
| Resting heart rate (bpm) | 74.5 ± 12.0 |
| Resting systolic blood pressure (mm Hg) | 126 [114, 140] |
| Resting diastolic blood pressure (mm Hg) | 72 [64, 80] |
Abbreviations: HDL = high-density lipoprotein; LDL = low-density lipoprotein.
Patients may have had more than one cardiac index event and more than one PCI procedure.
Table 2.
Baseline medication use of study population (n = 268).
| Medication | n (%) |
|---|---|
| Cardiac medications | 267 (99.6) |
| ACE inhibitor/ARB | 140 (52.4) |
| Aldosterone antagonist | 24 (9.0) |
| ARB + sacubitril | 4 (1.5) |
| Aspirin | 237 (88.8) |
| Beta-adrenergic blocker | 222 (83.1) |
| Anticoagulantsa | 181 (67.8) |
| Diuretics | 79 (29.6) |
| Statins | 237 (88.8) |
| SGLT2 inhibitors | 13 (4.9) |
| Psychotropic medications | 50 (19.0) |
| SSRIs | 22 (8.2) |
| Other antidepressants | 23 (8.6) |
| Benzodiazepines | 17 (6.3) |
| Other anxiolytics | 1 (0.4) |
| Antipsychotic agents | 2 (0.8) |
Abbreviations: ACE = angiotensin-converting enzyme; ARB = angiotensin receptor blocker; SGLT2 = sodium glucose cotransporter 2; SSRI = selective serotonin reuptake inhibitor.
Including antiplatelet agents and direct oral anticoagulants.
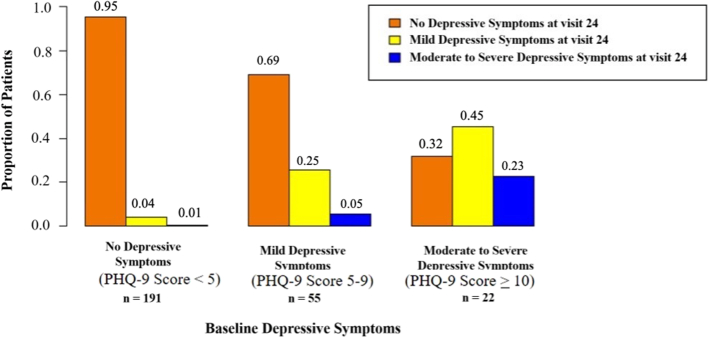
Regarding depression, 38 patients (14%) had a clinical diagnosis of depression prior to beginning ICR, per their medical record. At baseline, antidepressant medications were taken by 45 patients (17%), 20 of whom had a clinical diagnosis of depression. A summary of baseline medication use is shown in Table 2. The baseline median PHQ-9 score was 2.0 (IQR: 1.0, 5.0) points, highlighting the fact that most patients did not have significant depressive symptoms. Of the 268 patients enrolled, 191 (70%) did not have depressive symptoms at baseline (PHQ-9 score <5), 55 patients (21%) had mild depressive symptoms (PHQ-9 score 5–9), while 22 patients (8%) had moderate to severe depressive symptoms (PHQ-9 score ≥10).
Overall, patients who participated in the ICR program exhibited a significant improvement in depressive symptoms, as reflected by a decrease in median PHQ-9 score of 1.0 point (IQR: 0, 2.3; p < 0.0001) at follow-up. Fig. 1 shows the median changes in PHQ-9 scores for each category of baseline depressive symptoms (i.e., no depressive symptoms, mild depressive symptoms, moderate to severe depressive symptoms). Of the 191 patients who did not exhibit depressive symptoms at baseline, the vast majority (79.6%) had no change or improved their scores at follow-up. Among patients with mild depressive symptoms at baseline, PHQ-9 scores improved in 84%, while 5% did not experience a change, and 11% displayed a worsening (i.e., increase) in depressive symptoms at follow-up. In patients with moderate or severe depression at baseline, 91% improved their scores, while 5% had no change, and 5% had worse scores. There was no relationship between 6-minute walk improvement (median 150 m) and PHQ-9 score improvement.
Fig. 1.

Change in the PHQ-9 score from pre-ICR to after 24 ICR visits as grouped by baseline PHQ-9 score. Interquartile range (IQR) and median is indicated by the box, whiskers indicate the 95% confidence intervals. A decrease in PHQ-9 indicates fewer/less severe depressive symptoms. Outliers are marked with hollow circles.
Fig. 2 displays the proportion of patients in each depression category who changed, and those who did not change, clinical category from baseline to follow-up. Of the patients with no baseline depressive symptoms, 95% still had no depressive symptoms at the 24th visit, and only 5% had depressive symptoms. Of the patients with mild baseline depressive symptoms, nearly 70% improved their clinical category and had no depressive symptoms by follow-up; while one quarter had no change, and only 5% had moderate to severe depressive symptoms at follow-up. Of the patients with moderate to severe baseline depressive symptoms, 77% showed an improvement at follow-up. For the two patients (of a total of 191) who had a PHQ-9 score of <5 at baseline who had a follow-up score of >10, one of them had severe lower extremity pain with walking that was attributed to statin use by his cardiologist; the other one patient had no obvious cause for the change in PHQ-9 score in the medical record.
Fig. 2.
Proportion of patients who changed their depression category after 24 visits of ICR for each baseline depression category. Orange bars represent the proportion of patients with no depressive symptoms at visit 24 (PHQ-9 score < 5). Yellow bars represent the proportion of patients with mild depressive symptoms at visit 24 (i.e., PHQ-9 scores 5–9). Blue bars represent the proportion of patients with moderate to severe depressive symptoms at visit 24 (i.e., PHQ-9 score ≥ 10).
In this real-world study in a clinical setting, 17% of patients were taking antidepressant medication at baseline. After starting the ICR program, 30 patients began antidepressant medications, while seven discontinued antidepressant medication (p = 0.0003 follow-up vs. baseline antidepressant use). Using a post-hoc sensitivity analysis that excluded patients who began antidepressant medications during the study, there was still a significant improvement in PHQ-9 score (p < 0.001).
The median total CSE score for 233 patients who completed this questionnaire at baseline was 36.0 [30.0, 44.0] out of 64 maximum points. The median (IQR) subscale scores were 3.2 [2.6, 3.6] points for the “control symptoms” category and 3.0 [2.0, 4.0] for the “maintain function” category (of 4 maximum points for each).
Overall, patients who participated in the ICR program exhibited improvements in cardiac self-efficacy, as reflected by increases in the CSE total score and the factor scores for “maintain function” and “control symptoms” (all p < 0.001), as shown in Fig. 3. Overall, CSE scores stayed the same or improved in 74.9%, and the “maintain function” and “control symptoms” subscores improved or stayed the same in 82.2% and 79.3%, respectively. After excluding patients who started antidepressant medications during the study, there was still a significant improvement (p < 0.001) in overall cardiac self-efficacy and the subsection factor scores.
Fig. 3.
Change in cardiac self-efficacy (CSE) questionnaire scores from pre-ICR to after 24 ICR visits for a) total CSE score, b) the “maintain function” subsection, and c) the “control symptoms” subsection. Interquartile range (IQR) and median is indicated by the box, whiskers indicate the 95% confidence intervals. Increase in CSE score indicates greater cardiac self-efficacy. Outliers are marked with hollow circles.
4. Discussion
Results of this observational cohort study show that outpatient ICR is associated with improvements in depression and cardiac self-efficacy in patients with CVD. Improvements in depression were particularly notable among patients with moderate to severe depression at baseline. Not only did the majority of depressed patients have improvements in depression overall, but their scores also changed enough to decrease its clinical severity, for example from moderate/severe depression to mild or no depression. Patients also demonstrated significant improvements in overall cardiac self-efficacy, as well as the cardiac self-efficacy categories of “maintaining function” and “controlling symptoms”. Together, these findings suggest that outpatient ICR may be an effective treatment to improve mental well-being and self-efficacy in patients with CVD in a real-world, outpatient clinical setting.
Patients who were at least mildly depressed at baseline demonstrated significant improvements in depression. The greatest improvements were made by patients with moderate to severe depression, whose PHQ-9 scores improved by a median of 5.5 points. This is a clinically significant improvement, similar to the effect of successful antidepressant medication therapy [16], suggesting that ICR programs meaningfully improve depressive symptoms in patients with concurrent CVD. Patients with mild depression also improved by a median of 4 points on the PHQ-9, which was a significant enough improvement that many of these patients no longer qualified as having clinical depression. These findings of improved depression and cardiac self-efficacy remained after excluding patients who had started on antidepressant medications during the study. Unsurprisingly, those who were not clinically depressed at baseline had no significant change in PHQ-9 score.
These findings in outpatient ICR are congruent with those in previous studies that demonstrated the positive effects of exercise on mental health, including improvements in overall well-being, alleviation of depressive symptoms, and enhancements in brain plasticity and function [17], [18], [19]. For example, Milani and Lavie showed in their retrospective evaluation of traditional CR in patients with heart failure with reduced ejection fraction that CR was associated with improvements in depression scores using the Kellner Symptom questionnaire [5]. The results from that study and others that show benefits of exercise on mental health raise the possibility that the benefit from ICR might be solely attributed to the exercise sessions rather than the education and mental health intervention sessions [5]. However, we did not find a significant correlation between the improvement in 6 min walk and the PHQ-9 score change. At first glance, our finding appear to contradict the previous study by Milani and Lavie, who showed that the patients who had an improvement in peak oxygen consumption (VO2peak) demonstrated an improvement in depression scores (and mortality) [5]. In their study they showed that even mild improvements in VO2peak were associated with improvements in depression. It may be that there is not a linear relationship between exercise performance improvement and benefit of ICR (or CR). We speculate that some of the improvements in ICR may also result from the education/healthy mind interventions that are a part of ICR (but not CR). Mindfulness and stress management have been shown to have distinct benefits on cognition in older adults [20] and in patients with CVD [21]. Thus, our study lays the groundwork for a future randomized trial between ICR and CR investigating the relationship with mental health. Given that approximately 30% of patients in our study had clinically significant depression at baseline, efforts to improve depression during CR/ICR are of high public health importance.
It should be noted that the number of patients on antidepressant medications increased from baseline to the follow-up visit. This is likely due to increased patient contact with ICR staff and communication of baseline PHQ-9 scores between staff and the patient's primary care physician if the score was >9, which may have increased antidepressant prescriptions. This is also a benefit of our ICR program: increased screening for depression and informing physicians when evidence of depression is identified on the initial PHQ-9 questionnaire. Nevertheless, in our post-hoc analysis, after excluding the subjects who started taking antidepressants, the improved depression and CSE scores persisted. This would suggest that there is a significant effect of ICR itself for the improvement of depression and cardiac self-efficacy in patients with CVD.
In addition to depression, cardiac self-efficacy improved significantly following ICR participation. The improvement in overall cardiac self-efficacy indicates a greater level of confidence in patients' abilities to manage their cardiovascular health successfully [9]. Improvements in the cardiac self-efficacy factors maintain function and control symptoms reflect enhanced confidence in the ability to control CVD symptoms and to maintain their current level of functioning. Prior studies demonstrated that greater CSE scores are correlated with less negative affect and greater life satisfaction [8]. Higher CSE scores also correlate with better physical and social function after controlling for baseline health and anxiety levels [9] and decreased frailty [10].
The present study has limitations. Though it is a large and prospective observational study, it was conducted at a single center. Given that the insurance coverage for ICR is limited to patients who have experienced Medicare-specified eligibility criteria including the cardiac diagnoses previously listed, the results from our study cannot be extrapolated to patients who do not fit our entry criteria. Results may also differ in a more heterogeneous patient population. Additionally, this study did not compare results to a traditional cardiac rehabilitation or no-rehabilitation control group.
Continued work is also necessary to better understand the interaction between depression and CVD. A comprehensive meta-analysis found that there is no definitive proof that treating depression improves cardiovascular health and reduces mortality [22]; however, secondary analyses showed that among CVD patients whose treatment for depression was successful, the prognosis was improved. Further work to determine the mechanisms connecting depression and CVD are needed to better devise effective treatments for both conditions. Additionally, it is not yet known how long the benefits of ICR endure following program completion. Follow-up data are needed to determine whether the beneficial effects of ICR are maintained or diminish over time.
5. Conclusions
This is the first study to demonstrate the improvements in depression and cardiac self-efficacy that are associated with outpatient ICR. Given the improvements in depressive symptoms associated with participation in the ICR program and the strong relationship between depression following major cardiac events and increased mortality, clinical providers should consider recommending ICR as a viable treatment for patients with CVD. Moreover, given that patients with more significant depression and CVD appear to reap the greatest mental health benefit, providers should highlight the potential mental health benefits of attending ICR to their patients who have CVD and concurrent depression.
The following are the supplementary data related to this article.
Changes in anthropomorphic, hemodynamic, and exercise performance Pre-ICR and Post-24 visits of ICR.
Grant support
This work was supported by grants from the National Institutes of Health (R01AG060499; R21HL145217), Bethesda, Maryland and the Foundation for Barnes-Jewish Hospital, St. Louis, Missouri.
CRediT authorship contribution statement
Kristin M. McKenzie: Conceptualization, Data curation, Investigation, Validation, Writing – Original draft, Writing – Review and editing.
Lauren K. Park: Data curation, Investigation, Validation, Writing – Review and editing.
Eric J. Lenze: Conceptualization, Writing – Review and editing, Supervision.
Kristin Montgomery: Data curation, Investigation, Validation, Writing – Review and editing.
Serene Rashdi: Data curation, Investigation, Validation, Writing – Review and editing.
Elena Deych: Data curation, Formal analysis, Writing – Review and editing, Visualization.
Natalie A. Stranczcek: Data curation, Investigation, Validation, Writing – Review and editing.
Erin J. McKenzie: Data curation, Investigation, Validation, Writing – Review and editing.
Michael W. Rich: Conceptualization, Investigation, Validation, Resources, Writing – Review and editing, Supervision, Project administration, Funding acquisition.
Valene Garr Barry: Data curation, Investigation, Validation, Writing – Review and editing.
Jennifer Jonagan: Investigation, Validation, Data curation, Writing – Review and editing.
Nidhi Talpade: Data curation, Investigation, Validation, Writing – Review and editing.
Dotti Durbin: Investigation, Validation, Data curation, Writing – Review and editing.
Tessa Carson: Data curation, Investigation, Validation, Writing – Review and editing.
Linda R. Peterson: Conceptualization, Investigation, Validation, Resources, Writing – Review and editing, Supervision, Project administration, Funding acquisition.
Susan B. Racette: Conceptualization, Investigation, Validation, Resources, Writing – Review and editing, Supervision, Project administration, Funding acquisition.
Lisa de las Fuentes: Conceptualization, Investigation, Validation, Resources, Writing – Review and editing, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Michael W. Rich and Linda R. Peterson report financial support was provided by Foundation for Barnes-Jewish Hospital. Linda R. Peterson, Eric Lenze, Michael W. Rich, Susan Racette, and Lisa de las Fuentes report financial support was provided by National Institutes of Health.
References
- 1.Bradley S.M., Rumsfeld J.S. Depression and cardiovascular disease. Trends Cardiovasc. Med. 2015;25:614–622. doi: 10.1016/j.tcm.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Liu N., Liu S., Yu N., Peng Y., Wen Y., Tang J., Kong L. Correlations among psychological resilience, self-efficacy, and negative emotion in acute myocardial infarction patients after percutaneous coronary intervention. Front. Psychiatry. 2018;9:1. doi: 10.3389/fpsyt.2018.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarkar U., Ali S., Whooley M.A. Self-efficacy as a marker of cardiac function and predictor of heart failure hospitalization and mortality in patients with stable coronary heart disease: findings from the heart and soul study. Health Psychol. 2009;28:166–173. doi: 10.1037/a0013146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okuboyejo S., Mbarika V., Omoregbe N. The effect of self-efficacy and outcome expectation on medication adherence behavior. J. Public Health Afr. 2018;9:826. doi: 10.4081/jphia.2018.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.R.V. Milani, C.J. Lavie, Impact of cardiac rehabilitation on depression and its associated mortality, 120 Am. J. Med. 799-806. doi:10.1016/j.amjmed.2007.03.026. [DOI] [PubMed]
- 6.Barnard R.J., DiLauro S.C., Inkeles S.B. Effects of intensive diet and exercise intervention in patients taking cholesterol-lowering drugs. Am. J. Cardiol. 1997;79:1112–1114. doi: 10.1016/s0002-9149(97)00058-1. https://doi/10.1016/s0002-9149(97)00058-1 [DOI] [PubMed] [Google Scholar]
- 7.Sullivan S., Samuel S. Effect of short-term pritikin diet therapy on the metabolic syndrome. J. Cardiometab. Syndr. 2006;1:308–312. doi: 10.1111/j.1559-4564.2006.05732.x. [DOI] [PubMed] [Google Scholar]
- 8.Caprara M., Di Giunta L., Bermúdez J., Caprara G.V. How self-efficacy beliefs in dealing with negative emotions are associated to negative affect and to life satisfaction across gender and age. PLoS One. 2020;15 doi: 10.1371/journal.pone.0242326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sullivan M.D., LaCroix A.Z., Russo J., Katon W.J. Self-efficacy and self-reported functional status in coronary heart disease: a six-month prospective study. Psychosom. Med. 1998;60:473–478. doi: 10.1097/00006842-199807000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Hladek M.D., Gill J., Bandeen-Roche K., Walston J., Allen J., Hinkle J.L., Lorig K., Szanton S.L. High coping self-efficacy associated with lower odds of pre-frailty/frailty in older adults with chronic disease. Aging Ment.Health. 2020;24:1956–1962. doi: 10.1080/13607863.2019.1639136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fors A., Ulin K., Cliffordson C., Ekman I., I, Brink E. The Cardiac Self-Efficacy Scale, a useful tool with potential to evaluate person-centred care. Eur. J. Cardiovasc. Nurs. 2015;14:536–543. doi: 10.1177/1474515114548622. [DOI] [PubMed] [Google Scholar]
- 13.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L.McLeod, L., Delacqua G., Delacqua F., Kirby J., Duda S.N. REDCap Consortium, The REDCap consortium: Building an international community of software partners. J. Biomed. Inform. 2019 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Casanova C., Celli B.R., Barria P., Casas A., Cote C., de Torres J.P., Jardim J., Lopez M.V., Marin J.M., Montes de Oca M., Pinto-Plata V., Aguirre-Jaime A. Six minute walk distance project ALAT. The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur. Respir. J. 2011;37:150–156. doi: 10.1183/09031936.00194909. [DOI] [PubMed] [Google Scholar]
- 16.Löwe B., Unützer J., Callahan C.M., Perkins A.J., Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med. Care. 2004;42:1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Abdelbasset W.K., Alqahtani B.A., Elshehawy A.A., Tantawy S.A., Elnegamy T.E., Kamel D.M. Examining the impacts of 12 weeks of low to moderate-intensity aerobic exercise on depression status in patients with systolic congestive heart failure - a randomized controlled study. Clinics (Sao Paulo) 2019;74 doi: 10.6061/clinics/2019/e1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lavie C.J., Milani R.V., Artham S.M., Gilliland Y. Psychological factors and cardiac risk and impact of exercise training programs-a review of Ochsner studies. Ochsner J. 2007;7:167–172. [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao J.L., Jiang W.T., Wang X., Cai Z.D., Liu Z.H., Liu G.R. Exercise, brain plasticity, and depression. CNS Neurosci. Ther. 2020;26:885–895. doi: 10.1111/cns.13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brooks H., Oughli H.A., Kamel L., Subramanian S., Morgan G., Blumberger D.M., Kloeckner J., Kumar S., Mulsant B.H., Lenze E.J., Rajji T.K. Enhancing cognition in older persons with depression or anxiety with a combination of mindfulness-based stress reduction (MBSR) and transcranial direct current stimulation (tDCS): results of a pilot randomized clinical trial. Mindfulness (N Y) 2021:1–13. doi: 10.1007/s12671-021-01764-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marino F., Failla C., Carrozza C., Ciminata M., Chilà P., Minutoli R., Genovese S., Puglisi A., Arnao A.A., Tartarisco G., Corpina F., Gangemi S., Ruta L., Cerasa A., Vagni D., Pioggia G. Mindfulness-based interventions for physical and psychological wellbeing in cardiovascular diseases: a systematic review and meta-analysis. Brain Sci. 2021;11:727. doi: 10.3390/brainsci11060727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carney R.M., Freedland K.E. Depression and coronary heart disease. Nat. Rev. Cardiol. 2017;14:145–155. doi: 10.1038/nrcardio.2016.181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Changes in anthropomorphic, hemodynamic, and exercise performance Pre-ICR and Post-24 visits of ICR.