Dear Editor,
As the COVID-19 pandemic has progressed, long-COVID has emerged as a major problem that poses a significant challenge for attending physicians and health care policy makers. Therefore, we read with much interest the recently published unicentre study in the Journal of Infection by Righi et al.,1 carried out on 465 adult COVID-19 patients (235 [50.5%] hospital-admitted) followed-up during nine months, concluding that those with advanced age, intensive care unit (ICU) admission, and multiple symptoms at onset were more likely to have long-term COVID-19 symptoms, with negative impact on physical and mental wellbeing. Other studies have found that female gender, age, longer hospital stay, pre-existing hypertension, cardiovascular disease, diabetes, chronic obstructive pulmonary disease, smoking, obesity, and chronic alcoholism increase the likelihood of long-COVID.2 , 3 It is known that SARS-CoV-2 RNAemia is a predictor of COVID-19 severity and in-hospital complications.4 , 5 However, to the best of our knowledge, only two studies have assessed, up to one or three months after the acute COVID-19 onset, whether SARS-CoV-2 RNAemia may have an impact on long-COVID,6 , 7 both finding that RNAemia at presentation might predict the persistence of symptoms. However, these studies did not provide information regarding long-COVID symptoms nor the association with SARS-CoV-2 RNAemia beyond three months, and could not differentiate between “true” long-COVID and the convalescence phase of the SARS-CoV-2 infection.
In this regard, we conducted a prospective multicentre cohort study in adult COVID-19 patients to determine, at six months (± two months) after hospital admission, the impact of SARS-CoV-2 RNAemia and other risk factors on the development of long-COVID and worsened quality of life. The present research was nested in a prospective observational multicentre cohort study of consecutive hospitalized adult patients with microbiologically confirmed COVID-19, approved by the Ethics Committee of the coordinating institution (C.I. 0771-N-20). Clinical data and samples were collected within 24 h of admission (for detailed information on sampling and viral load quantification, see the supplementary methods). Patients hospitalized at five Spanish centres from March 23 to June 12, 2020 were contacted at six months (± two months) from hospital admission and, after obtaining their informed consent, they answered a telephone questionnaire (Telephone Interview for Cognitive Status, TICS-30,8 supplementary materials) which evaluated persistent symptoms, including neurocognitive impairment, and its impact on quality of life. Long-COVID was considered when patients reported at least one persistent or new onset symptom six months after hospital admission, that worsened quality of life and could not be explained by an alternative diagnosis. Descriptive analyses, chi-square test with correction of Yates, box plots, and linear mixed and logistic regression models adjusted for patient age were performed (supplementary methods).
The mean (±SD) age of the 129 hospitalized COVID-19 participants was 59.8±11.8 years, and 78.3% were men. Overall, 110 patients (90.2%) had pneumonia, the median length of hospital stay was seven days (5 to 11.2 days), 25.9% of patients received high-flow oxygen therapy, 19.2% had acute respiratory distress syndrome (ARDS), and 18% developed other untoward events (supplementary Table 1).
At six months (± two months) after hospital admission, only 22 (17.7%) patients were completely free of any COVID-19 related symptoms, whereas 102 (82.3%) had long-COVID (supplementaries Fig. 1 and Table 2). Sixty-four (49.6%) patients reported worsened quality of life. Symptoms reported were dyspnea (40.6%), fatigue (38%), headache (28.7%), joint pain (37.2%), myalgia (36.4%), concentration difficulty (37.2%), and poor memory performance (46.5%). Most patients had mild (49.6%) or moderate (20.9%) cognitive impairment. The mean TICS-30 test score was 20.6 ± 4.4 points.
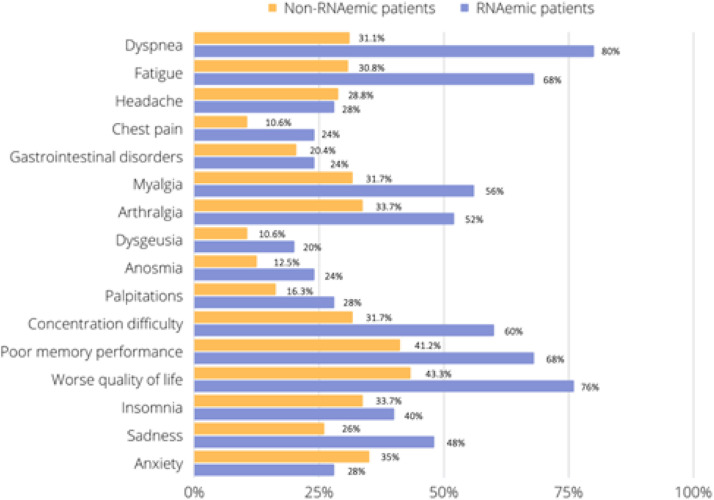
Twenty-five (19.4%) out of 129 participants had SARS-CoV-2 RNAemia at hospital admission, with a mean viral load of 2.62±0.58 log10 copies/ml. Twenty-four (96%) out of these patients presented long-COVID, with dyspnea (80%), fatigue (68%), poor memory performance (68%), and concentration difficulty (60%) being the most common symptoms. Worsened quality of life was perceived by 76% and 43.3% of patients with and without RNAemia (P = 0.006; supplementary Table S2). The mean in the TICS-30 test was 20.2 ± 4.82 points and 76% of these RNAemia-positive patients presented cognitive impairment, wihout differences with non-RNAemia patients. The comparison of long-COVID manifestations between patients with and without RNAemia are detailed in Fig. 1 . Patients with vs. without RNAemia presented higher frequency of ≥4 symptoms (80% vs. 52.8%; P = 0.02). The long-COVID characteristics, according to the presence or absence of RNAemia are detailed in the supplementary Figs. 2–7. No association was found between patients’ blood viral load and quality of life or any long-COVID symptoms.
Fig. 1.
Comparison between long-COVID manifestations in patients with and without SARS-CoV-2 RNAemia.
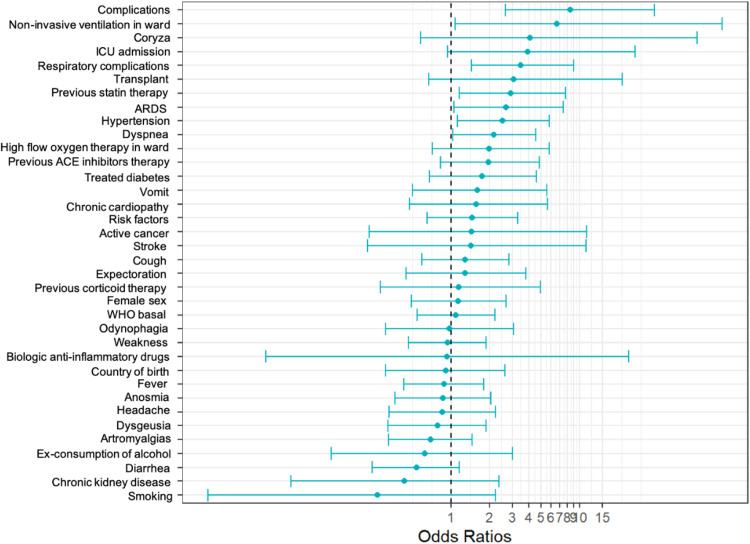
Factors independently associated with long-term worsened quality of life compared to one-year before hospitalization for COVID (age adjusted) were prior statin therapy (OR 2.89; 95% CI, 1.15–7.77), hypertension (OR 2.50; 95% CI, 1.12–5.79), ARDS (OR 2.68; 95% CI, 1.05–7.44), and non-invasive ventilation (OR 6.63; 95% CI, 1.08–127.61) (Fig. 2 ). These findings coincide with those from other studies, which identified preexisting hypertension3 and acute COVID-19 severity as risk factors for long-COVID.9 However, it must be noted that long-COVID may be difficult to differentiate from post-intensive care syndrome.10 Finally, no association was found between inflammatory biomarkers at hospital admission and long-COVID, except for a lower leukocyte count (supplementary Fig. 11).
Fig. 2.
Risk factors associated with worsened quality of life compared to one-year before hospitalization for COVID-19 (age-adjusted). ICU: intensive care unit; ARDS: acute respiratory distress syndrome; ACE: angiotensin-converting enzyme; WHO: Severity rating according to the WHO Clinical Progression Scale, ranged from 0 (not infected) to 10 (dead), doi: 10.1016/S1473-3099(20)30483-7.
Our study has some limitations. Firstly, the information from the patients was obtained by a telephone questionnaire. However, during the study period the policy of most centres was to restrict face-to-face visits as much as possible. Secondly, as we focused on hospitalized patients, our findings cannot be extrapolated to outpatients. Thirdly, the number of patients with RNAemia was small. Therefore, our results regarding the impact of RNAemia in long COVID should be interpreted with caution and explored in further studies with larger samples.
In summary, this study shows that SARS-CoV-2 RNAemia is associated with worse quality of life and the presence of more long-COVID symptoms at six months after hospital admission. The risk factors for long-COVID defined in our study may help identify patients who should undergo a close follow-up after discharge.
Declaration of Competing Interest
None of the study authors have conflicts of interest to declare.
Acknowledgement and funding
A.R. has received a predoctoral research grant from the Instituto de Salud Carlos III, Spanish Ministry of Science, Innovation and Universities, (PFIS grant FI18/00183). G.A.A. reports a predoctoral research grant from the 201808-10 project, funded by La Marató de TV3. This study was supported by the Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, the Spanish Network for Research in Infectious Diseases (REIPI, RD16/0016/0001, RD16/0016/0005, RD16/0016/0009, RD16/0016/0013)-co-financed by the European Development Regional Fund, A way to achieve Europe, Operative program Intelligent Growth 2014-2020, and the Centro de Investigación Biomédica en Red de Enfermedades Infecciosas (CIBERINFEC) [CB21/13/00009; CB21/13/00006], Madrid, Spain. J.S.C. and E.C. received grants from the Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación, Proyectos de Investigación sobre el SARS-CoV-2 y la enfermedad COVID-19 (COV20/00580; COV20/00370). J.S.C. is a researcher belonging to the program “Nicolás Monardes” (C-0059–2018), Servicio Andaluz de Salud, Junta de Andalucía, Spain. Samples and data from patients included in this study from the Hospital Universitario Cruces (Bizkaia, Spain) were provided by the Basque Biobank (www.biobancovasco.org) and were processed following standard operation procedures with appropriate approval of the Ethical and Scientific Committees.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2022.11.009.
Appendix. Supplementary materials
References
- 1.Righi E., Mirandola M., Mazzaferri F., Dossi G., Razzaboni E., Zaffagnini A., et al. Determinants of persistence of symptoms and impact on physical and mental wellbeing in Long COVID: A prospective cohort study. J Infect. 2022;84(4):566–572. doi: 10.1016/j.jinf.2022.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sudre C.H., Murray B., Varsavsky T., Graham M.S., Penfold R.S., Bowyer R.C., et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tleyjeh I.M., Saddik B., AlSwaidan N., AlAnazi A., Ramakrishnan R.K., Alhazmi D., et al. Prevalence and predictors of Post-Acute COVID-19 Syndrome (PACS) after hospital discharge: a cohort study with 4 months median follow-up. PLoS One. 2021;16(12) doi: 10.1371/journal.pone.0260568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ram-Mohan N., Kim D., Zudock E.J., Hashemi M.M., Tjandra K.C., Rogers A.J., et al. SARS-CoV-2 RNAemia predicts clinical deterioration and extrapulmonary complications from COVID-19. Clin Infect Dis. 2022;74(2):218–226. doi: 10.1093/cid/ciab394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hogan C.A., Stevens B.A., Sahoo M.K., Huang C., Garamani N., Gombar S., et al. High frequency of SARS-CoV-2 RNAemia and association with severe disease. Clin Infect Dis. 2021;72(9):e291–e295. doi: 10.1093/cid/ciaa1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Su Y., Yuan D., Yuan D., Chen D.G., Ng R.H., Wang K., et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185(5):881–895. doi: 10.1016/j.cell.2022.01.014. .e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ram-Mohan N., Kim D., Rogers A.J., Blish C.A., Nadeau K.C., Blomkalns A.L., et al. Association between SARS-CoV-2 RNAemia and postacute sequelae of COVID-19. Open Forum Infect Dis. 2021;9(2):ofab646. doi: 10.1093/ofid/ofab646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Castanho T.C., Amorim L., Zihl J., Palha J.A., Sousa N., Santos N.C. Telephone-based screening tools for mild cognitive impairment and dementia in aging studies: a review of validated instruments. Front Aging Neurosci. 2014;6:16. doi: 10.3389/fnagi.2014.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taboada M., Cariñena A., Moreno E., Rodríguez N., Domínguez M.J., Casal A., et al. Post-COVID-19 functional status six-months after hospitalization. J Infect. 2021;82(4):e31–e33. doi: 10.1016/j.jinf.2020.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inoue S., Hatakeyama J., Kondo Y., Hifumi T., Sakuramoto H., Kawasaki T., et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6(3):233–246. doi: 10.1002/ams2.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.