Abstract
Purpose
The aim of this updated version of the systematic review and meta-analysis was to assess the association of PD with lipid profile.
Methods
A comprehensive literature search was done in electronic databases including PubMed, Web of Science, and Scopus until August 2021. Cross-sectional, case-control, and cohort studies investigating the relationship between PD and lipid profile were included. Screening, data extraction, and quality assessment were performed independently by two investigators. A random-effect model was used to pool the effect size. Odds ratio (OR) was used as effect size for the association of PD with Hyperlipidemia, and SMD was used for the association of PD with the mean level of lipid profile.
Results
Overall, 34 documents met the inclusion criteria for this systematic review, and 31 were included for the meta-analysis. Sixteen studies were cross-sectional, 16 case-control, and two cohorts. Results of the random effect model showed that PD increased the odds of dyslipidemia by 15% (OR: 1.15, 95% CI: 1.04, 1.26). The Association of PD with low HDL, high LDL, hypertriglyceridemia, and hypercholesteremia was not statistically significant (P > 0.05). The mean level of HDL in patients with PD was significantly lower than in subjects without PD (SMD: -0.69, 95% CI: -1.11, -0.26). Moreover, the mean level of LDL, TC, TG in patients with PD was significantly higher than in subjects without PD (P < 0.05).
Conclusions
This meta-analysis suggests that periodontitis is associated with an increased odds of dyslipidemia. Therefore, treating periodontitis may improve dyslipidemia, particularly HDL and triglyceride levels.
Keywords: Dyslipidemia; Periodontist disease; Lipid profile, systematic review, Meta-analysis
Introduction
Periodontitis is a chronic infectious disease that involves interactions between bacterial products and inflammatory mediators [1]. Also, it can associate with a number of systemic conditions. The researchers found that Periodontitis often did not exist independently and that its occurrence and development were often related to other systemic diseases in the body that could not be ignored [2]. Periodontal disease has affected more than 50% of the adult population, and it is probably the most common disease in humans [3]. Based on the global burden of disease study in 2019, the global prevalence and disability-adjusted life years (DALYs) of Periodontitis has almost doubled from 1990 to 2019. Also, South and East Asia had the highest increase in prevalence and DALY. It has been identified that population growth and aging are two important factors to increase this prevalence [4]. Studying and knowing about periodontal disease, in addition to information such as the severity and prevalence of the disease, can be effective in identifying preventive, causative, and prognostic factors [3].
Profile lipid is a pattern of lipids in the blood. Profile lipid includes the levels of total cholesterol (TC), low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglyceride, which is important for most cells [5]. According to World Health Organization (WHO), the overall prevalence of raised cholesterol is estimated 39% that in females is more than in males (40% vs. 37%), and 29.7 million DALYS (2% of total DALYs) is attributed to Raised cholesterol [6]. Elevated LDL can lead to the accumulation of cholesterol plaques and increase the risk of atherosclerosis. HDL leads to removing cholesterol from the body, and elevated HDL more than 60 mg/dl can reduce the risk of atherosclerosis [7]. Also, eating habits, gender, smoking, and exercise can contribute to cardiovascular disease [8].
periodontitis and hyperlipidemia may be caused by bacteria and their metabolites. Inflammation and products of the immune cells affect each other. Bacteria-induced endotoxin (LPS) can cause tissue-destroying inflammation by the immune system. Many researchers have done clinical studies on the relationship between the two, but the results are not the same [9–12].
When superficial receptors of leukocytes such as macrophages and PMNs interfere with elevated intravascular lipids, pro-inflammatory cytokines increase, and growth factor production decrease. Thus, these changes can be the cause of the pathogenesis of Periodontitis [12–14]. As mentioned, Periodontitis and Hyperlipidemia have a bilateral effect on each other, and periodontal treatment can decrease the lipid profile [15]. There are some previous systematic reviews in this regard that had some limitations. One of them just indicated an association between Periodontitis and the mean level of lipid profiles [16]. The others had not included all available evidence with a comprehensive search strategy [17, 18]. Therefore, this updated systematic review and meta-analysis has been done to assess the relationship of Periodontitis with lipid profiles.
Materials and methods
We used Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to conduct this systematic review and meta-analysis.
Search strategy
A comprehensive literature search was done in electronic databases including MEDLINE/PubMed, Web of Science, and Scopus for eligible studies on the association between Periodontitis and lipid profile until August 2021. All database was searched using “HDL” OR “High-Density Lipoprotein” OR “LDL” OR “Low-Density Lipoprotein” OR “Triglycerides” OR “Total Cholesterol” OR “Dyslipidemia” OR “Hyperlipidemia” OR “Hypertriglyceridemia” OR “Hypercholesterolemia” OR “Lipids” OR “lipid profile “AND “Periodontal Disease” OR “Periodontitis” keywords and all related terms included according to search strategy of each database (supplementary Table 1). One investigator performed a search strategy and was approved by the second investigator.
Eligibility criteria and selection study
All observational studies (cross-sectional, case-control, and cohort) that investigated the association of Periodontitis with lipid profiles were included. Also, the studies in the clinical diagnostic criterion of lipid profile and Periodontitis were not clearly defined or not reported were excluded. Periodontitis was defined as CAL > 1, PD > 2, and CPI > 2 [19, 20]. In the case of studies with multiple publications, the most recent were considered.
After removing duplicate studies, two investigators independently examined the title, abstract, and full text for related studies, respectively, based on eligibility criteria. Disagreement was first discussed by two investigators; otherwise, the final decision was made by the third investigator.
Data extraction
Two investigators independently performed the data extraction using an electronic data extraction form. The following characteristics were extracted. First author, year of publication, country, study design, sample size, age (mean or range), percent of male, the definition of lipid profile and Periodontitis, effect size (odds ratio (OR), Relative risk (RR)), and standardized mean difference (SMD) with 95% confidence intervals, and confounders variables adjusted in statistical analysis. Disagreement was first discussed by two investigators; otherwise, the final decision was made by the third investigator.
Quality assessment
The Newcastle-Ottawa Scale was used to assess the quality of included studies. This scale consists of three components, including selection, comparability, and outcome by eight items. The scale is available separately for cohort and case-control studies. The total score ranged from 0 to 9, with a higher score indicating a low risk of bias. The categorized risk of bias is considered as follows: 0–4 for low quality, 5–6 for moderate quality, and 7–9 for high quality. Disagreement was first discussed by two investigators; otherwise, the final decision was made by the third investigator.
Statistical analysis
The heterogeneity among studies was examined using a chi-square-based Q test and I-square statistics. I-squared values, 0%, 25%, and 75%, showed low, moderate, and high heterogeneity, respectively. Random-effect meta-analysis model (using the Der-Simonian and Laird method) was used If heterogeneity was statistically significant (P-value < 0.1) [21]. For the meta-analysis, the Odds ratio (OR) was used as the effect size for the association of periodontitis with hyperlipidemia, and standardized mean difference (SMD) was used for the association of periodontitis with the mean level of lipid profile. We calculated 95% confidence intervals for each effect estimate. Since the number of studies with the prospective design was limited, meta-analysis was performed only for case-control and cross-sectional studies. Subgroup analyses were done with regard to quality assessment, type of lipid profile, periodontal indices (probing depth (PD), clinical attachment loss (CAL, Community Periodontal Index (CPI), and Bleeding on probing (BOP)), and study population (healthy and unhealthy study subjects). Publication bias was estimated by Egger’s test, and P-value < 0.1was considered to be statistically significant. Publication bias was presented visually using a funnel plot. All analyses were conducted using Stata (version 11; Stata Corp, College Station, Texas).
Results
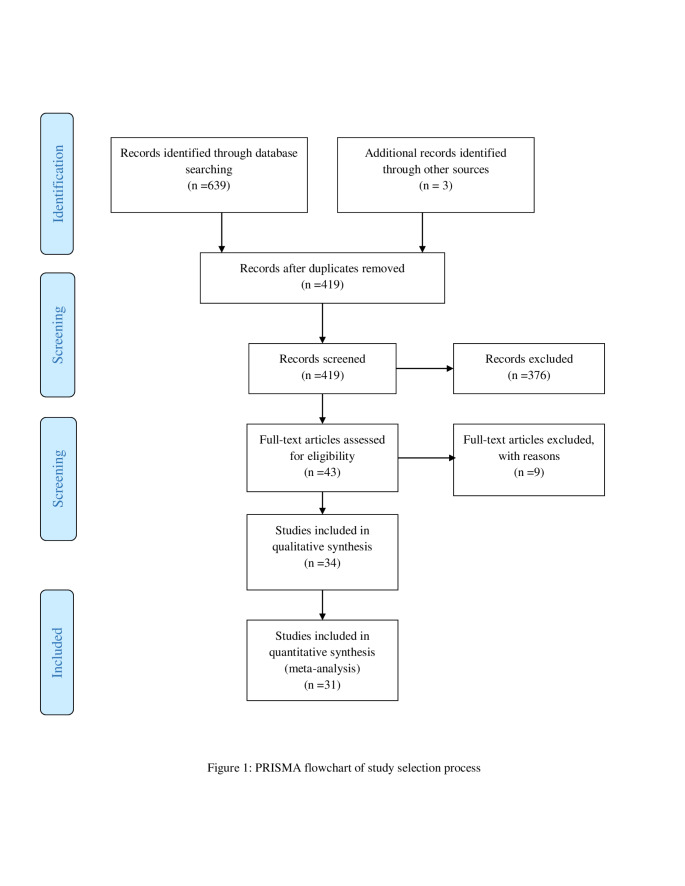
The initial literature search provided 642 documents. Six hundred eight were excluded because 223 were duplicates, and 376 were irrelevant in the title, abstract, and full text. Finally, 34 met the inclusion criteria for systematic review and 31 were included for meta-analysis (Fig. 1).
Fig. 1.
PRISMA flowchart of the study selection process
Qualitative synthesis
The main characteristics of included studies have been shown in Table 1. Sixteen studies were cross-sectional, 16 case-control and two cohorts. Nineteen studies reported dichotomous data, and 13 reported mean and standard deviation. Also, two studies reported linear regression (beta and standard error) and were excluded from the meta-analysis. Most studies were performed in India (six studies) and fewest in France, Finland, Taiwan, Austria, Germany, and Colombia (one study). The studies were published between 2000 and 2020 years. Of 34 studies, two studies were carried out on women only. The sample size of included studies in the systematic review was 103,468 (51.35% male), ranging from 30 to 65,078 participants, and in the meta-analysis was 38,143. The most commonly adjusted confounding factors were age, gender, and smoking status. According to the Lipid profile, HDL was measured in 34 studies, TG in 34 studies, LDL in 18 studies, and TC in 14 studies. According to periodontal indices, PD was measured in 14 studies, CAL in eight studies, PD/CAL in 10 studies, CPI (Community Periodontal Index), and PD/BOP in nine studies. In case-control and cross-sectional studies, OR (95% CI) ranged between 0.15 (0.01, 1.51) [22] and 7.13 (3.30–15.40) [23]. The relative risk was reported in one study [24].
Table 1.
Characteristics of included studies
| No of study | Author, year, and country | Age Mean ± SD/ range |
Study design | Sample | Male% | Definition of lipid profile | Definition of periodontal | Effect size (95% CI) | Confounders | Quality scores (9) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Song, Korea, 2020 [48] | 55.4 ± 7.30 | Cohort | 65,078 | 62.80 | TC | CPI ≥ 1 |
Beta: -0.0013 Standard error: 0.0042 p-value: 0.762 |
Sex, age, household income, smoking, alcohol, exercise, BMI, hypertension, diabetes mellitus, chronic kidney disease, aspartate aminotransferase level, alanine aminotransferase level, baseline lipid level, time from the baseline examination, markers for oral health status, and oral hygiene care |
8 | |
| LDL |
Beta: -0.0047 Standard error: 0.0047 p-value: 0.315 |
||||||||||
| HDL |
Beta: -0.0066 Standard error: 0.0026 p-value:0.013 |
||||||||||
| TG |
Beta: 0.0074 Standard error: 0.0046 p-value:0.110 |
||||||||||
| 2 | Cury, Brazil, 2017 [49] | 47.3 ± 7.9 | Case-control | 80 | 72.85 | TG > 200 mg/dl ( Mean ± SD) | PD and CAL ≥ 4 mm with BOP or CAL ≥ 5 mm with BOP |
Case: 195.5 ± 5.1 Control: 185.9 ± 6.0 |
Gender and age | 5 | |
| TC > 200 mg/dl |
Case: 195.5 ± 5.1 Control: 185.9 ± 6.0 |
||||||||||
| HDL < 60 mg/dl |
Case: 195.5 ± 5.1 Control: 185.9 ± 6.0 |
||||||||||
| LDL > 30 mg/dl |
Case: 195.5 ± 5.1 Control:185.9 ± 6.0 |
||||||||||
| 3 | Jaramillo, 2016, Colombia [50] | 28–69 | Case-control | 651 | 36% | TG > 150 | CAL > 6 and PD ≥ 5 | OR: 1.30 (0.91–1.86) | Age, sex and Smoking | 6 | |
| HDL ≤ 50 mg/dL women | OR: 0.89 (0.64–1.27) | ||||||||||
| 4 | Shinjo, 2019, USA [51] | 64.4 ± 6.9 | Cross-sectional | 170 | 86% | TC | CAL ≥ 6 mm OR PD ≥ 5 mm |
Case: 166.50 ± 40.30 Control: 171.7 ± 36.30 |
7 | ||
| LDL |
Case: 83.70 ± 25.50 Control: 85.20 ± 24.70 |
||||||||||
| HDL |
Case:65.50 ± 27.40 Control:70.30 ± 21.70 |
||||||||||
| TG |
Case:82.00 ± 43.00 Control: 75.40 ± 37.90 |
||||||||||
| 5 | Lee, 2017, Korea, [52] | > 20 | Cross-sectional | 6,905 | Men | TC ≥ 200 | CPI > 2 | OR: 1.09 (0.85–1.40) | Area, education, BMI, alcohol intake, menopausal status (in women), and smoking status | 8 | |
| LDL ≥ 160 | OR: 0.88 (0.44–1.76) | ||||||||||
| HDL ≥ 40 | OR: 1.27 (0.86–1.88) | ||||||||||
| TG ≥ 150 | OR: 1.61 (0.89–1.52) | ||||||||||
| Women | TC ≥ 200 | OR: 1.63 (1.03–1.78) | |||||||||
| LDL ≥ 160 | OR: 1.38 (1.01–5.60) | ||||||||||
| HDL ≥ 40 | OR: 1.37 (1.02–1.84) | ||||||||||
| TG ≥ 150 | OR: 0.57 (0.48–1.17) | ||||||||||
| 6 | Fentoglu, Turkey, 2009 [23] | 48.40 ± 7.14 | Case-control | 98 | 43.87% |
TG > 200 mg/dl HDL-C < 35 mg/dl LDL-C > 130 mg/dl, |
PI | OR: 2.74 (1.31–5.71) | Age, gender, BMI, hypertension, number of missing teeth, and daily brushing habit | 6 | |
| CAL | OR: 4.93 (2.32–10.40) | ||||||||||
| PD | OR:7.13 (3.30–15.40) | ||||||||||
| 7 | Aditi Sangwan, India ,2013 [53] | 43.26 ± 10.03 | cross-sectional | 140 | 54.28% |
TG: >200 mg/dL TC: >200 mg/d; LDL-C: >130 mg/d; HDL-C: <35 mg/dL |
PD | OR: 2.87(1.4–5.51) | Smoking, residual confounding effect of smoking can lead to biased estimates | 6 | |
| CAL | OR: 2.13( 1.12–4.08) | ||||||||||
| 8 | Shimazaki, Japan, 2007 [34] | 55.7 ± 18.8 | Cross-sectional | 584 | 0% | TG > 150 mg/dL | PD ≥ 2 mm | OR: 1.50 (0.90–2.60) | Age, smoking status, lipid-lowering medication, and total cholesterol | 9 | |
| HDL < 50 mg/dL | PD ≥ 2 mm | OR: 2.20 (1.40–3.60) | |||||||||
| HDL < 50 mg/dL | CAL ≥ 3 mm | OR: 2.80 (1.40–5.60) | |||||||||
| TG > 150 mg/dL | CAL ≥ 3 mm | OR: 2.0 (1.0-4.20) | |||||||||
| 9 | Khader, Jordan, 2008 [33] |
patients with MeS48.3 ± 13.0 persons without MeS46.1 ± 10.9 |
Cross-sectional | 156 | 35.9% |
HDL < 40 mg/dl (men) HDL < 50 mg/dl (women) |
CAL > 3 mm |
β = 9.5, SE = 3.5 p-value = 0.007 |
Adjusted means of periodontal parameters between one group and the reference group | 8 | |
| TG > 150 mg/dl | CAL > 3 mm |
β = 9.6, SE = 3.8 p-value = 0.013 |
|||||||||
|
HDL < 40 mg/dl (men) HDL <50 mg/dl (women) |
PD > 3 mm |
β = 4.1, SE = 3.6 p-value = 0.253 |
|||||||||
| TG ≥ 150 mg/dl | PD > 3 mm |
β = 20.3, SE = 3.9 p-value < 0.005 |
|||||||||
| 10 | Kushiyama, Japan, 2009 [32] | 40–70 | Cross-sectional | 1,070 | 26.7% |
HDL < 40 mg/dl (men) HDL <50 mg/dl (women) |
CPI ≥ 3 | OR: 1.50 (1.02–2.21) | Age, gender, and smoking habits | 8 | |
| TG ≥ 150 mg/dl | CPI ≥ 3 | OR: 1.14 (0.79–1.66) | |||||||||
| 11 | Benguigui, France, 2010 [38] | 35–74 | Cross-sectional | 255 | 54.9% | TG ≥1.7mmol/l (150 mg/dl) | CAL ≥ 6 and/or PD ≥ 5 mm. | OR: 2.32 (0.72–7.44) | Age, gender, educational level, smoking habits, alcohol consumption, CRP, and dental plaque | 9 | |
|
HDL 1mmol/l (40 mg/dl) in men 1.3mmol/l (50 mg/dl) in women |
OR: 0.24 (0.06–1.02) | ||||||||||
| 12 | Kwon, Korea ,2011 [31] |
No periodontitis37.79 periodontitis 55.00 |
Cross-sectional | 7,178 | 37.5% |
HDL < 40 mg/dl (men) HDL <50 mg/dl (women) |
CPI ≥ 3(3.5 mm > pocket) | OR: 1.34 (1.14–1.56) | Age, smoking habits, alcohol intake, toothbrushing frequency, and a present number of teeth. | 9 | |
| TG ≥150 mg/dl | CPI ≥ 3(3.5 mm > pocket) | OR: 1.38 (1.17–1.62) | |||||||||
| 13 | Minagawa, Japan ,2015 [36] | 80 | Cross-sectional | 234 | 47.4% | TG ≥ 150 mg/dL and/or HDL < 40 mg/dL and/or the current use of anti-dyslipidemia medications | PD ≥ 5 mm | OR: 1.61 (0.88–2.96) | Gender, income, education, smoking status, the pattern of visits to a dentist, brushing frequency, exercise habits, and dietary energy and food intake | 9 | |
| 14 | Timonen, ,Finland ,2010 [54] | 30 to 64 | Cross-sectional | 2,050 | 39.2% | TG > 2.0 mmol/L or HDLcholesterol < 40 mg/dl | PD ≥ 6 mm | OR: 1.03(0.70–1.52) | Gender, age, education, plaque level, toothbrushing frequency, dental attendance pattern, and alcohol | 8 | |
| 15 | Sora, USA, 2013 [37] | 55.27 ± 10.65 | Cross-sectional | 283 | 24.0% | Serum HDL cholesterol < 40 mg/dl | CAL > 6 mm | OR: 0.98 (0.55–1.75) | Age, total teeth, smoking status, HbA1c and gender | 6 | |
| PD ≥ 5 mm | OR: 0.85(0.51–1.42) | ||||||||||
| Triglyceride level ≥ 150 mg/dl | CAL > 6 mm | OR: 1.25 (0.52–2.99) | |||||||||
| PD ≥ 5 mm | OR: 1.71 (0.85–3.41) | ||||||||||
| 16 | Thanakun, Taiwan ,2014 [22] | 47.0 (35 to 76) | Cross-sectional | 125 | 42.4% | HDL-levels (< 40 mg/dL in males and < 50 mg/dL in females) | CAL > 4 mm | OR: 0.55(0.15, 2.01) | Age, sex, alcohol consumption, education level, and frequency of tooth brushing. | 8 | |
| TG levels < 150 mg/dL) | CAL > 4 mm | OR: 2.43 (0.54, 10.90) | |||||||||
| HDL-levels (< 40 mg/dL in males and < 50 mg/dL in females) | PD > 4 mm and BOP > 10% | OR: 0.15 (0.01, 1.51) | |||||||||
| TG levels < 150 mg/dL) | PD > 4 mm and BOP > 10% | OR: 1.04 (0.10, 10.51) | |||||||||
| 17 | Alhabashneh, Jordan ,2015 [30] | 53.8 ± 9.6 (21–80) | Cross-sectional | 280 | 50.7% | HDL cholesterol: <40 mg/dL (1.03 mmol/L) | PD ≥ 3 mm and CAL ≥ 3 mm | OR: 1.99 (1.15, 3.46) | Age, family income, residency area, smoking, teeth brushing, and number of missing teeth | 9 | |
| TG level: ≥150 mg/dL (1.7 mmol/L | OR: 1.41 (0.77, 2.60) | ||||||||||
| 18 | Masanori Iwasaki, japan, 2015 [24] | 75 | Cohort | 125 | 89.55% | TG ≥150 mg/dL | CAL ≥ 3 mm | RR: 1.20 (0.52, 2.77) | Gender, income, education, smoking status, number of the teeth | 6 | |
| HDL-C levels < 40 mg/dL in men and < 50 mg/dL in women | CAL ≥ 3 mm | RR: 2.11 (0.96, 4.64) | |||||||||
| 19 | D´Aiuto, USA ,2008 [55] |
Severe periodontitis 52.3 Moderate periodontitis 54.2 Mild or no periodontitis 38.7 |
Cross-sectional | 13,677 | 62.0% | Low HDL cholesterol,(40 mg/dl for men and 50 for women) |
CAL > 6 mm, PD > 4 mm |
OR: 1.35 (0.87, 2.09) | Age, sex, years of education, poverty to income ratio, ethnicity, general conditions, and smoking | 9 | |
| TG > 150 mg/dL |
CAL > 6 mm PD > 4 mm |
OR: 0.96 (0.61, 1.51) | |||||||||
| 20 | Morita, Japan, 2009 [56] | 43.3 | Cross-sectional | 2,478 | 81.8% | TG > 150 mg/dL | CPI > 3 mm | OR: 1.3 (1.0, 1.7) | Age, gender, and smoking habit.CI, confidence interval | 8 | |
| HDL < 40 mg/dL | CPI > 3 mm | OR: 1.6 (1.0, 2.6) | |||||||||
| 21 | LaMonte, USA ,2014 [57] | 32.3 ± 1.2 (50–79) | Cross-sectional | 657 | 0% | Low HDL-C(< 50 mg/dL) | CAL < 6 mm with PD < 5 mm | OR: 1.08 (0.71, 1.64) | Age, smoking, hormone therapy use, history of diagnosed heart disease, tooth brushing, dental visits, recreational physical activity | 8 | |
| TG > 150 mg/dL | CAL < 6 mm, with PD < 5 mm | OR: 1.04 (0.70, 1.55) | |||||||||
| 22 | Moeintaghavi, Iran, 2005 [35] | 32.3 ± 1.2 | Case -control | 40 | 60% | TG > 200 mg/dl |
CPI 3,4 ,PD > 4 mm |
OR: 2.74 (1.22, 6.18) | Age and sex | 6 | |
| LDL > 200 mg/dl |
CPI 3,4, PD > 4 mm |
OR: 2.28 (1.02, 5.11) | |||||||||
| TC > 200 mg/dl |
CPI 3,4, PD > 4 mm |
OR: 1.10 (0.49, 2.45) | |||||||||
| HDL < 29 mg/dl |
CPI 3,4, PD > 4 mm |
OR: 1.40 (0.62, 3.12) | |||||||||
| 23 | Akalin, 2008, Turkey [58] | 49.04 ± 8.97 | Case-control | 34 | 50% | Healthy participate | HDL | PD ≥ 5 |
Case: 45.18 ± 11.84 Control: 53.18 ± 10.32 |
6 | |
| LDL |
Case: 108.31 ± 32.84 Control:99.5 ± 22.00 |
||||||||||
| TG |
Case:118.65 ± 115.38 Control: 90.53 ± 89.30 |
||||||||||
| TC |
Case:176.47 ± 41.68 Control: 169.12 ± 28.90 |
||||||||||
| Diabetic participate | HDL |
Case: 47.82 ± 10.66 Control: 53.18 ± 10.32 |
|||||||||
| LDL |
Case: 125.91 ± 32.91 Control: 99.5 ± 22.00 |
||||||||||
| TG |
Case: 237.82 ± 115.38 Control: 90.53 ± 89.30 |
||||||||||
| TC |
Case:212.12 ± 41.99 Control: 169.12 ± 28.90 |
||||||||||
| 24 | Andrukhov, 2013, Austria [59] | 39.3 ± 4.8 | Case-control | 143 | 54.5% | HDL | PD ≥ 5 |
Case: 56.3 ± 1.60 Control: 53.90 ± 1.90 |
4 | ||
| LDL |
Case: 139.90 ± 3.60 Control: 127.00 ± 5.40 |
||||||||||
| TC |
Case: 219.00 ± 4.00 Control: 205.60 ± 6.10 |
||||||||||
| TG |
Case: 113.40 ± 7.50 Control: 96.30 ± 7.90 |
||||||||||
| 25 | Duzagac, 2015, Turkey [60] | 40.36 ± 5.53 | Case-control | 30 | HDL |
PD ≥ 4 and BOP, CAL ≥ 2 |
Case: 51.90 ± 10.70 Control: 54.50 ± 8.90 |
7 | |||
| LDL |
Case: 108.04 ± 47.31 Control: 104.81 ± 34.06 |
||||||||||
| TG |
Case: 77.90 ± 33.40 Control: 74.00 ± 25.00 |
||||||||||
| 26 | Golpasandhagh, 2014, Iran [61] | 34.74 ± 4.71 | Case-control | 90 | 43.3% |
TC > 220 mg/ dL |
PD ≥ 4 | OR: 4.04 (1.54, 11.00) | Age, gender and BMI | 7 | |
| TG > 200 mg/dL | OR: 5.20 (1.83, 14.73) | ||||||||||
| LDL > 178 mg/dL | OR: 0.65 (0.10, 4.10) | ||||||||||
| HDL < 29 mg/dL | OR: 0.65 (0.10, 4.10) | ||||||||||
| 27 | Joseph, 2011, India [62] | 33.73 | Case-control | 176 | 35.80% | TC |
PD ≥ 5 CAL ≥ 4 |
Case: 163.93 ± 27.61 Control: 167.73 ± 28.81 |
Age, sex | 5 | |
| TG |
Case: 41.97 ± 23.33 Control: 49.03 ± 44.19 |
||||||||||
| HDL |
Case:41.56 ± 7.95 Control: 40.62 ± 6.63 |
||||||||||
| LDL |
Case:104.04 ± 26.25 Control: 105.66 ± 27.14 |
||||||||||
| 28 | Kumar, 2014, India [63] | NR | Case-control | 50 | NR | LDL | CAL ≥ 4 |
Case: 110.22 ± 25.75 Control: 83.44 ± 37.56 |
6 | ||
| HDL |
Case: 37.39 ± 9.35 Control: 38.66 ± 9.35 |
||||||||||
| TG |
Case: 190.60 ± 137.52 Control: 167.72 ± 80.08 |
||||||||||
| 29 | losche, 2000, Germany [64] | 55.10 | Case- control | 79 | 41.77% | TC > 230 | PD ≥ 4 |
Case: 243.00 ± 37.30 Control: 224.80 ± 39.10 |
Age and sex | 6 | |
| LDL > 160 |
Case: 187.30 ± 37.30 Control: 165.50 ± 35.90 |
||||||||||
| HDL > 45 |
Case: 52.20 ± 11.70 Control: 55.80 ± 17.80 |
||||||||||
| TG > 200 |
Case: 175.60 ± 115.50 Control: 126.20 ± 53.10 |
||||||||||
| 30 | Monteiro, 2009, brazil [65] | 45.00 | Case-control | 80 | 42.50% | TC > 200 mg/dl | PD ≥ 5 |
Case: 202.41 ± 45.77 Control: 192.35 ± 27.69 |
Age, BMI, FBS, Sex | 7 | |
| HDL < 40 mg/dl |
Case:47.48 ± 7.97 Control: 53.62 ± 10.68 |
||||||||||
| LDL > 130 mg/dl |
Case:131.32 ± 40.87 Control: 120.26 ± 22.81 |
||||||||||
| TG > 150 mg/dl |
Case:144.48 ± 104.78 Control: 99.25 ± 41.24 |
||||||||||
| 31 | Penumarthy, 2013, India [66] | 33.92 | Case- control | 60 | 78.33% | TG |
PD ≥ 6 CAL ≥ 3 |
Case: 160.00 ± 60.90 Control: 107.07 ± 24.89 |
Age and sex | 6 | |
| TC |
Case: 208.30 ± 52.82 Control: 167.70 ± 22.46 |
||||||||||
| HDL |
Case: 33.27 ± 5.82 Control: 46.03 ± 8.99 |
||||||||||
| LDL |
Case: 142.80 ± 44.94 Control: 104.80 ± 20.51 |
||||||||||
| 32 | Pushparani, 2014, India [67] | 38.56 | Case-control | 300 | 46.5% | TC |
PD ≥ 5 CAL ≥ 3 |
Case: 180.70 ± 45.22 Control: 185.00 ± 31.67 |
Age and sex | 6 | |
| TG |
Case: 152.80 ± 55.60 Control: 150.60 ± 52.69 |
||||||||||
| HDL |
Case: 26.85 ± 7.84 Control: 38.68 ± 7.05 |
||||||||||
| LDL |
Case: 140.10 ± 41.50 Control: 130.60 ± 27.04 |
||||||||||
| 33 | Sridhar, 2009, India [68] | 44.77 | Case- control | 60 | 44.77% | HDL |
PD ≥ 5 CAL ≥ 3 |
Case: 39.20 ± 7.29 Control: 41.07 ± 9.52 |
Age, sex, number teeth | 4 | |
| TG |
Case: 100.57 ± 35.05 Control: 90.30 ± 32.70 |
||||||||||
| 34 | Taleghani, 2010, Iran [69] | 46.5 | Case-control | 52 | 34.62% | TC > 250 | PD ≥ 4 |
Case: 207.30 ± 42.10 Control: 192.30 ± 34.60 |
Age and weight ranges, sex, and diet, without periodontal treatment | 6 | |
| TG > 200 |
Case: 165.20 ± 83.70 Control: 128.40 ± 71.10 |
||||||||||
| LDL > 180 |
Case: 122.70 ± 35.10 Control: 116.40 ± 29.00 |
||||||||||
| HDL < 30 |
Case: 48.80 ± 12.60 Control: 48.80 ± 12.60 |
||||||||||
| TC = total cholesterol; TG = triglyceride; LDL = low-density lipoprotein; HDL = high-density lipoprotein; PI = plaque index; PD = probing depth; CAL = clinical attachment level; BOP = bleeding on probing, Body mass index (BMI) | |||||||||||
Quantitative synthesis
The pooled association of deriodontitis and dyslipidemias is shown in Table 2. Moderate significant heterogeneity was seen among the included studies for the overall association of periodontitis with dyslipidemia (I-squared = 28.70%, P = 0.024). The random effect meta-analysis model showed that periodontitis increased the odds of dyslipidemia by 15% (OR: 1.15, 95% CI: 1.04, 1.26)). The association of periodontitis with low HDL, high LDL, hypertriglyceridemia, and hypercholestromia was not statistically significant (P > 0.05). In the subgroup meta-analysis, there was not a significant association between periodontitis indices with the type of lipid profile except for the association between PD and low HDL (OR: 1.32, 95% CI: 1.17, 1.47)). Moreover, there was a significant positive association between periodontitis indices and lipid profile in studies with healthy (OR: 1.15, 95% CI: 1.04, 1.26) and unhealthy study populations (OR: 1.15, 95% CI: 1.05, 1.26). Also, according to the quality assessment, the association of periodontitis and dyslipidemia only in high-quality studies was statistically significant (OR: 1.16, 95% CI: 1.02, 1.30).
Table 2.
Meta-analysis of the association between periodontitis with dyslipidemia in included studies
| No studies | Sample size | Pooled OR (95% CI) | Heterogeneity assessment | |||
|---|---|---|---|---|---|---|
| I-squared % | Q test | P-value | ||||
| Lipid profile | ||||||
| Low HDL | 13 | 34,273 | 1.11 (0.91, 1.32) | 55.70 | 42.90 | 0.001 |
| High TG | 13 | 33,203 | 1.17 (1.00, 1.34) | 26.90 | 23.25 | 0.141 |
| High LDL | 3 | 7,035 | 1.01 (0.49, 1.54) | 0.00 | 1.87 | 0.760 |
| High TC | 3 | 7,305 | 1.29 (0.93, 1.66) | 40.90 | 6.77 | 0.149 |
| Dyslipidemia | 13 | 34,273 | 1.15 (1.04, 1.26) | 28.70 | 79.90 | 0.024 |
| Lipid profile-dental indices | ||||||
| High TG | ||||||
| PD | 7 | 17,558 | 1.18 (0.88, 1.49) | 63.30 | 19.07 | 0.008 |
| CAL | 3 | 992 | 1.56 (0.79, 2.34) | 0.00 | 0.93 | 0.819 |
| PD-CAL | 5 | 15,520 | 1.12 (0.87, 1.37) | 0.00 | 2.05 | 0.727 |
| Low HDL | ||||||
| PD | 8 | 18,628 | 1.32 (1.17, 1.47) | 0.00 | 5.82 | 0.757 |
| CAL | 4 | 992 | 0.88 (0.41, 1.35) | 19.10 | 3.71 | 0.295 |
| PD-CAL | 10 | 14,520 | 0.98 (0.55, 1.40) | 70.00 | 13.35 | 0.010 |
| Population | ||||||
| Healthy subjects | 16 | 36.232 | 1.15 (1.04, 1.26) | 33.50 | 73.72 | 0.013 |
| Unhealthy subjects | 2 | 563 | 1.15 (1.05, 1.26) | 0.00 | 4.96 | 0.420 |
TC = total cholesterol; TG = triglyceride; LDL = low-density lipoprotein; HDL = high-density lipoprotein; PI = plaque index; PD = probing depth; CAL = clinical attachment level
The association of Periodontitis with mean lipid levels is presented in Table 3. Significant severe heterogeneity was reported among the included studies (I-squared = 94.60%, P < 0.001). By random effect model, the result showed that in patients with periodontitis, the mean level of lipid profile was higher than in patients without Periodontitis (SMD: 0.32, 95% CI: 0.05, 0.58)). Associations of periodontitis with TG (SMD: 0.57, 95% CI: 0.20, 0.93)), TC (SMD: 0.68,95% CI: 0.14, 1.22)), LDL (SMD: 0.87, 95% CI: 0.30, 1.35)) was statistically positive and with HDL (SMD: -0.69, 95% CI: -1.11, -0.26) was statistically negative. In the subgroup meta-analysis, according to the study population, there was a significant positive association between periodontitis with mean lipid profile in studies with the unhealthy population (SMD: 0.54, 95% CI: 0.03, 1.05). According to quality assessment, only in studies with moderate quality the association of Periodontitis and mean lipid profile was statistically significant (SMD: 0.28, 95% CI: 0.009, 0.55)).
Table 3.
Meta-analysis of the association between periodontitis with mean lipid levels in included studies
| Overall | No studies | Sample size | SMD (95% CI) | Heterogeneity assessment | ||
|---|---|---|---|---|---|---|
| I-squared % | Q test | P-value | ||||
| Lipid profile | ||||||
| HDL | 13 | 1,314 |
-0.69 (-1.11, -0.26) |
91.40 | 150.41 | < 0.001 |
| TG | 13 | 1,314 |
0.57 (0.20, 0.93) |
88.80 | 116.24 | < 0.001 |
| LDL | 12 | 1,254 |
0.87 (0.30, 1.35) |
94.00 | 199.92 | < 0.001 |
| TC | 10 | 1,111 |
0.68 (0.14, 1.22) |
94.10 | 169.03 | < 0.001 |
| Lipid profile-dental indices | ||||||
| TG | ||||||
| PD | 5 | 388 |
0.93 (0.27, 1.60) |
89.00 | 48.27 | < 0.001 |
| PD-CAL | 7 | 876 |
0.29 (-0.02, 0.62) |
75.00 | 24.92 | < 0.001 |
| HDL | ||||||
| PD | 5 | 388 |
-0.26 (-0.1.23, -0.08) |
86.80 | 37.90 | < 0.001 |
| PD-CAL | 7 | 876 |
-0.80 (-1.49, -0.10) |
94.40 | 106.75 | < 0.001 |
| LDL | ||||||
| PD | 5 | 388 |
0.89 (-0.01, 1.79) |
94.30 | 87.58 | < 0.001 |
| PD-CAL | 6 | 816 |
0.75 (0.01, 1.50) |
94.60 | 93.17 | < 0.001 |
| TC | ||||||
| PD | 5 | 388 |
0.87 (0.01, 1.74) |
93.92 | 79.94 | < 0.001 |
| PD-CAL | 5 | 786 |
0.43 (-0.18, 1.06) |
92.70 | 54.53 | < 0.001 |
| Population | ||||||
| Healthy subjects | 12 | 1,264 |
0.28 (0.00, 0.57) |
77.30 | 26.43 | < 0.001 |
| Unhealthy subjects | 2 | 84 |
0.54 (0.03, 1.05) |
95.20 | 918.82 | < 0.001 |
TC = total cholesterol; TG = triglyceride; LDL = low-density lipoprotein; HDL = high-density lipoprotein; PI = plaque index; PD = probing depth; CAL = clinical attachment level
Quality assessment
The frequency of studies with high, middle, and low quality were 18, 14, and 2 studies, respectively.
Publication Bias
No evidence of publication bias was observed in association of lipid profile and periodontitis in included studies (coefficient = 0.021, p-value = 0.949) (Fig. 2).
Fig. 2.
Funnel plot association of lipid profile and periodontitis in cross-sectional and case-control studies for dichotomous data
Discussion
In this systematic review and meta-analysis, we reviewed the documents regarding the relationship between periodontitis and lipid profile. Periodontitis was significantly associated with dyslipidemia in cross-sectional and case-control studies in a way that periodontitis increased the odds of dyslipidemia by 15% and the likelihood of low HDL by 32%. According to continuous data, there were significant positive associations between periodontitis indices with mean TG, LDL, and TC, while a significant negative association existed with HDL; therefore, periodontitis indices were increased by increasing the lipid profile, except for HDL, which had a protective effect on Periodontitis.
Periodontal disease is an infection of the gum generated by poor brushing and flossing habits that allow plaque to build up on the teeth and harden. In severe stages, periodontal disease can lead to sore, bleeding gums, painful chewing problems, and even tooth loss [11, 25]. Moreover, patients with periodontal disease may experience alterations in their lipid profile[15, 26]. Furthermore, there were significant positive associations between periodontitis and TG, LDL, and TC while a significant negative association with HDL. Also, some evidence showed an association between periodontitis and blood lipid levels [13, 14, 27, 28]. Periodontal disease is one of the infectious and inflammatory diseases. Inflammation caused by oral microorganisms in this disease can affect the role of periodontal disease in the formation of atheroma and, consequently atherosclerosis. Bacteria associated with periodontal disease can colonize atheromatic plaques and cause localized inflammation and the spread of this inflammation, leading to the formation and development of atheroma and eventually rupture. Systemic inflammation can be caused by bacteria in the blood; it may also be the result of cytokines produced in the periodontal lesion that has entered the bloodstream [29]. Results are somewhat different according to the types of blood lipids. In some of them, the prevalence of periodontal disease was associated with increased levels of lipid profile [30–35], while others did not find any significant association between periodontal disease and dyslipidemia [36–38]. Different species of bacteria in infected gums secrete various pro-inflammatory toxins and metabolites [39, 40]. These metabolites could affect health status via different mechanisms in our body [41–44]. The oral cavity contains around 700 bacterial species; some of them are known as periodontopathic bacteria. Porphyromonasgingivalis (P. gingivalis) has been identified as a major etiological pathogen in periodontitis, due to virulence factors including fimbriae, lipopolysaccharides, capsule, and proteases [45]. Gingipains which is a cysteine protease produced by P. gingivalis and assumed as the main causative agent in periodontal disease that results in tissue damage of periodontium [40, 46]. These bacteria could contribute to damage and structural losses. It has been shown that other species of bacteria which could play a role in the alteration of lipid profile and lipid metabolism change the level of lactate, acetone, isopropanol, glycerol, and methanol in comparison to commensal microbiota in a healthy mouth [47]. It seems that prevention and treatment of periodontal diseases can be an effective approach to controlling lipid disorders and cardiovascular complications.
This study has some strengths and limitations. Due to the low number of eligible articles, we could not perform a meta-regression to find the source of heterogeneity. We could not prevent the possibility of residual confounding as more studies were needed. The included studies had different limitations, including insufficient data and missed information such as the number of remaining teeth, previous periodontal treatment, or the use of antibiotics. Therefore, limitations should be considered while interpreting these results. Regardless of these limitations, it is worth emphasizing some strengths of this study, while we invested a great deal of effort in limiting possible sources of bias. Although there are some previous systematic reviews on the association between periodontist and lipid profiles, they had inadequate analyses, insufficient included studies, and incomplete search strategies. We tried to have the most comprehensive systematic review and meta-analyses in this regard by considering lipid profiles as both quantitative and qualitative variables.
Conclusions
This meta-analysis suggests that periodontitis is associated with an increased odds of dyslipidemia. Therefore, treating periodontitis may improve dyslipidemia, particularly HDL and triglyceride levels.
Statements and Declarations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Funding:
This study was funded by Alborz University of Medical Sciences.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40200-022-01071-7.
References
- 1.Cardoso EM, Reis C, Manzanares-Céspedes MC. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad Med. 2018;130(1):98–104. doi: 10.1080/00325481.2018.1396876. [DOI] [PubMed] [Google Scholar]
- 2.Macri E, Lifshitz F, Ramos C, Orzuza R, Costa O, Zago V, et al. Atherogenic cholesterol-rich diet and periodontal disease. Arch Oral Biol. 2014;59(7):679–86. doi: 10.1016/j.archoralbio.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Raitapuro-Murray T, Molleson T, Hughes F. The prevalence of periodontal disease in a Romano-British population c. 200–400 AD. Br Dent J. 2014;217(8):459–66. doi: 10.1038/sj.bdj.2014.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu L, Zhang SQ, Zhao L, Ren ZH, Hu CY. Global, regional, and national burden of periodontitis from 1990 to 2019: results from the Global Burden of Disease study 2019. J Periodontol. 2022. [DOI] [PubMed]
- 5.Nordestgaard BG. A test in context: lipid profile, fasting versus nonfasting. J Am Coll Cardiol. 2017;70(13):1637–46. doi: 10.1016/j.jacc.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Indicator Metadata Registry List Raised cholesterol 2008 [Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3236.
- 7.Cooney M, Dudina A, De Bacquer D, Wilhelmsen L, Sans S, Menotti A, et al. HDL cholesterol protects against cardiovascular disease in both genders, at all ages and at all levels of risk. Atherosclerosis. 2009;206(2):611–6. doi: 10.1016/j.atherosclerosis.2009.02.041. [DOI] [PubMed] [Google Scholar]
- 8.Bäck M, Hansson GK. Leukotriene receptors in atherosclerosis. Ann Med. 2006;38(7):493–502. doi: 10.1080/07853890600982737. [DOI] [PubMed] [Google Scholar]
- 9.Zhou X, Zhang W, Liu X, Zhang W, Li Y. Interrelationship between diabetes and periodontitis: role of hyperlipidemia. Arch Oral Biol. 2015;60(4):667–74. doi: 10.1016/j.archoralbio.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Chen S, Lin G, You X, Lei L, Li Y, Lin M, et al. Hyperlipidemia causes changes in inflammatory responses to periodontal pathogen challenge: implications in acute and chronic infections. Arch Oral Biol. 2014;59(10):1075–84. doi: 10.1016/j.archoralbio.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol. 2005;43(11):5721–32. doi: 10.1128/JCM.43.11.5721-5732.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papapanou P. Epidemiology of periodontal diseases: an update. J Int Acad Periodontol. 1999;1(4):110–6. [PubMed] [Google Scholar]
- 13.Hajishengallis G, Chavakis T, Lambris JD. Current understanding of periodontal disease pathogenesis and targets for host-modulation therapy. Periodontol 2000. 2020;84(1):14–34. doi: 10.1111/prd.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stapleton PA, Goodwill AG, James ME, Brock RW, Frisbee JC. Hypercholesterolemia and microvascular dysfunction: interventional strategies. J Inflamm. 2010;7(1):1–10. doi: 10.1186/1476-9255-7-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fu Y-W, Li X-X, Xu H-Z, Gong Y-Q, Yang Y. Effects of periodontal therapy on serum lipid profile and proinflammatory cytokines in patients with hyperlipidemia: a randomized controlled trial. Clin Oral Investig. 2016;20(6):1263–9. doi: 10.1007/s00784-015-1621-2. [DOI] [PubMed] [Google Scholar]
- 16.Lianhui Y, Meifei L, Zhongyue H, Yunzhi F. Association between chronic periodontitis and hyperlipidemia: a Meta-analysis based on observational studies. Hua Xi Kou Qiang Yi Xue Za Zhi. 2017;35(4):419–26. doi: 10.7518/hxkq.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nepomuceno R, Pigossi SC, Finoti LS, Orrico SR, Cirelli JA, Barros SP, et al. Serum lipid levels in patients with periodontal disease: A meta-analysis and meta‐regression. J Clin Periodontol. 2017;44(12):1192–207. doi: 10.1111/jcpe.12792. [DOI] [PubMed] [Google Scholar]
- 18.Xu J, Duan X. Association between periodontitis and hyperlipidaemia: A systematic review and meta-analysis. Clin Exp Pharmacol Physiol. 2020;47(11):1861–73. doi: 10.1111/1440-1681.13372. [DOI] [PubMed] [Google Scholar]
- 19.Ainamo J. Relationship between malalignment of the teeth and periodontal disease. Scand J Dent Res. 1972;80(2):104–10. doi: 10.1111/j.1600-0722.1972.tb00270.x. [DOI] [PubMed] [Google Scholar]
- 20.Carranza F. Newman And Carranza’s Clinical Periodontology. China: WB Saunders Elsevier; 2019. [Google Scholar]
- 21.Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed.). 2003;327:557–60. [DOI] [PMC free article] [PubMed]
- 22.Thanakun S, Watanabe H, Thaweboon S, Izumi Y. Association of untreated metabolic syndrome with moderate to severe periodontitis in Thai population. J Periodontol. 2014;85(11):1502–14. doi: 10.1902/jop.2014.140105. [DOI] [PubMed] [Google Scholar]
- 23.Fentoğlu Ö, Öz G, Taşdelen P, Uskun E, Aykaç Y, Bozkurt FY. Periodontal status in subjects with hyperlipidemia. J J Periodontol. 2009;80(2):267–73. doi: 10.1902/jop.2009.080104. [DOI] [PubMed] [Google Scholar]
- 24.Iwasaki M, Sato M, Minagawa K, Manz MC, Yoshihara A, Miyazaki H. Longitudinal relationship between metabolic syndrome and periodontal disease among Japanese adults aged ≥ 70 years: the Niigata Study. J Periodontol. 2015;86(4):491–8. doi: 10.1902/jop.2015.140398. [DOI] [PubMed] [Google Scholar]
- 25.Könönen E, Gursoy M, Gursoy UK, Periodontitis A multifaceted disease of tooth-supporting tissues. J Clin Med. 2019;8(8):1135. doi: 10.3390/jcm8081135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bresolin AC, Pronsatti MM, Pasqualotto LN, Nassar PO, Jorge AS, da Silva EAA, et al. Lipid profiles and inflammatory markers after periodontal treatment in children with congenital heart disease and at risk for atherosclerosis. Vasc Health Risk Manag. 2013;9:703. doi: 10.2147/VHRM.S52187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dahlen G, Basic A, Bylund J. Importance of virulence factors for the persistence of oral bacteria in the inflamed gingival crevice and in the pathogenesis of periodontal disease. J Clin Med. 2019;8(9):1339. doi: 10.3390/jcm8091339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 2000. 2014;64(1):57–80. doi: 10.1111/prd.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.How KY, Song KP, Chan KG. Porphyromonas gingivalis: an overview of periodontopathic pathogen below the gum line. Front Microbiol. 2016;7:53. doi: 10.3389/fmicb.2016.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alhabashneh R, Khader Y, Asa’ad F. The association between periodontal disease and metabolic syndrome among outpatients with diabetes in Jordan. Diabetes Metab Disord. 2015;14(1):1–7. doi: 10.1186/s40200-015-0192-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwon YE, Ha JE, Paik DI, Jin BH, Bae KH. The relationship between periodontitis and metabolic syndrome among a Korean nationally representative sample of adults. J Clin Periodontol. 2011;38(9):781–6. doi: 10.1111/j.1600-051X.2011.01756.x. [DOI] [PubMed] [Google Scholar]
- 32.Kushiyama M, Shimazaki Y, Yamashita Y. Relationship between metabolic syndrome and periodontal disease in Japanese adults. J Periodontol. 2009;80(10):1610–5. doi: 10.1902/jop.2009.090218. [DOI] [PubMed] [Google Scholar]
- 33.Khader Y, Khassawneh B, Obeidat B, Hammad M, El-Salem K, Bawadi H, et al. Periodontal status of patients with metabolic syndrome compared to those without metabolic syndrome. J Periodontol. 2008;79(11):2048–53. doi: 10.1902/jop.2008.080022. [DOI] [PubMed] [Google Scholar]
- 34.Shimazaki Y, Saito T, Yonemoto K, Kiyohara Y, Iida M, Yamashita Y. Relationship of metabolic syndrome to periodontal disease in Japanese women: the Hisayama Study. J Dent Res. 2007;86(3):271–5. doi: 10.1177/154405910708600314. [DOI] [PubMed] [Google Scholar]
- 35.Moeintaghavi A, Haerian-Ardakani A, Talebi-Ardakani M, Tabatabaie I. Hyperlipidemia in patients with periodontitis. J Contemp Dent Pract. 2005;6(3):78–85. [PubMed] [Google Scholar]
- 36.Minagawa K, Iwasaki M, Ogawa H, Yoshihara A, Miyazaki H. Relationship between metabolic syndrome and periodontitis in 80-year‐old Japanese subjects. J Periodontal Res. 2015;50(2):173–9. doi: 10.1111/jre.12190. [DOI] [PubMed] [Google Scholar]
- 37.Sora ND, Marlow NM, Bandyopadhyay D, Leite RS, Slate EH, Fernandes JK. Metabolic syndrome and periodontitis in Gullah African Americans with type 2 diabetes mellitus. J Clin Periodontol. 2013;40(6):599–606. doi: 10.1111/jcpe.12104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Benguigui C, Bongard V, Ruidavets JB, Chamontin B, Sixou M, Ferrières J, et al. Metabolic syndrome, insulin resistance, and periodontitis: a cross-sectional study in a middle‐aged French population. J Clin Periodontol. 2010;37(7):601–8. doi: 10.1111/j.1600-051X.2010.01571.x. [DOI] [PubMed] [Google Scholar]
- 39.Yamada M, Takahashi N, Matsuda Y, Sato K, Yokoji M, Sulijaya B, et al. A bacterial metabolite ameliorates periodontal pathogen-induced gingival epithelial barrier disruption via GPR40 signaling. Sci Rep. 2018;8(1):1–12. doi: 10.1038/s41598-018-27408-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Genco CA, Potempa J, Mikolajczyk-Pawlinska J, Travis J. Role of gingipains R in the pathogenesis of Porphyromonas gingivalis-mediated periodontal disease. Clin Infect Dis. 1999;28(3):456–65. doi: 10.1086/515156. [DOI] [PubMed] [Google Scholar]
- 41.Hajishengallis G, Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021:1–15. [DOI] [PMC free article] [PubMed]
- 42.Scotti E, Boué S, Sasso GL, Zanetti F, Belcastro V, Poussin C, et al. Exploring the microbiome in health and disease: Implications for toxicology. Toxicol Res Appl. 2017;1:2397847317741884. [Google Scholar]
- 43.Griffiths R, Barbour S. Lipoproteins and lipoprotein metabolism in periodontal disease. Clin Lipidol. 2010;5(3):397–411. doi: 10.2217/clp.10.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Macfarlane GT, Steed H, Macfarlane S. Bacterial metabolism and health-related effects of galacto‐oligosaccharides and other prebiotics. J Appl Microbiol. 2008;104(2):305–44. doi: 10.1111/j.1365-2672.2007.03520.x. [DOI] [PubMed] [Google Scholar]
- 45.Paster BJ, Olsen I, Aas JA, Dewhirst FE. The breadth of bacterial diversity in the human periodontal pocket and other oral sites. Periodontol 2000. 2006;42(1):80–7. doi: 10.1111/j.1600-0757.2006.00174.x. [DOI] [PubMed] [Google Scholar]
- 46.Hočevar K, Potempa J, Turk B. Host cell-surface proteins as substrates of gingipains, the main proteases of Porphyromonas gingivalis. Biol Chem. 2018;399(12):1353–61. doi: 10.1515/hsz-2018-0215. [DOI] [PubMed] [Google Scholar]
- 47.Banjoko IO, Adeyanju MM, Ademuyiwa O, Adebawo OO, Olalere RA, Kolawole MO, et al. Hypolipidemic effects of lactic acid bacteria fermented cereal in rats. Lipids Health Dis. 2012;11(1):1–11. doi: 10.1186/1476-511X-11-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Song TJ, Kim JW, Kim J. Oral health and changes in lipid profile: A nationwide cohort study. J Clin Periodontol. 2020;47(12):1437–45. doi: 10.1111/jcpe.13373. [DOI] [PubMed] [Google Scholar]
- 49.Cury EZ, Santos VR, da Silva Maciel S, Gonçalves TED, Zimmermann GS, Mota RMS, et al. Lipid parameters in obese and normal weight patients with or without chronic periodontitis. Clin Oral Investig. 2018;22(1):161–7. doi: 10.1007/s00784-017-2095-1. [DOI] [PubMed] [Google Scholar]
- 50.Jaramillo A, Contreras A, Lafaurie GI, Duque A, Ardila CM, Duarte S, et al. Association of metabolic syndrome and chronic periodontitis in Colombians. Clin Oral Investig. 2017;21(5):1537–44. doi: 10.1007/s00784-016-1942-9. [DOI] [PubMed] [Google Scholar]
- 51.Shinjo T, Ishikado A, Hasturk H, Pober DM, Paniagua SM, Shah H, et al. Characterization of periodontitis in people with type 1 diabetes of 50 years or longer duration. J Periodontol. 2019;90(6):565–75. doi: 10.1002/JPER.18-0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee S, Im A, Burm E, Ha M. Association between periodontitis and blood lipid levels in a Korean population. J Periodontol. 2018;89(1):28–35. doi: 10.1902/jop.2017.170111. [DOI] [PubMed] [Google Scholar]
- 53.Sangwan A, Tewari S, Singh H, Sharma RK, Narula SC. Periodontal status and hyperlipidemia: Statin users versus non-users. J Periodontol. 2013;84(1):3–12. doi: 10.1902/jop.2012.110756. [DOI] [PubMed] [Google Scholar]
- 54.Timonen P, Niskanen M, Suominen-Taipale L, Jula A, Knuuttila M, Ylöstalo P. Metabolic syndrome, periodontal infection, and dental caries. J Dent Res. 2010;89(10):1068–73. doi: 10.1177/0022034510376542. [DOI] [PubMed] [Google Scholar]
- 55.D’Aiuto F, Sabbah W, Netuveli G, Donos N, Hingorani AD, Deanfield J, et al. Association of the metabolic syndrome with severe periodontitis in a large US population-based survey. J Clin Endocrinol Metab. 2008;93(10):3989–94. doi: 10.1210/jc.2007-2522. [DOI] [PubMed] [Google Scholar]
- 56.Morita T, Ogawa Y, Takada K, Nishinoue N, Sasaki Y, Motohashi M, et al. Association between periodontal disease and metabolic syndrome. J Public Health Dent. 2009;69(4):248–53. doi: 10.1111/j.1752-7325.2009.00130.x. [DOI] [PubMed] [Google Scholar]
- 57.LaMonte MJ, Williams AM, Genco RJ, Andrews CA, Hovey KM, Millen AE, et al. Association between metabolic syndrome and periodontal disease measures in postmenopausal women: the Buffalo OsteoPerio study. J Periodontol. 2014;85(11):1489–501. doi: 10.1902/jop.2014.140185. [DOI] [PubMed] [Google Scholar]
- 58.Akalın FA, Işıksal E, Baltacıoğlu E, Renda N, Karabulut E. Superoxide dismutase activity in gingiva in type-2 diabetes mellitus patients with chronic periodontitis. Arch Oral Biol. 2008;53(1):44–52. doi: 10.1016/j.archoralbio.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 59.Andrukhov O, Haririan H, Bertl K, Rausch WD, Bantleon HP, Moritz A, et al. Nitric oxide production, systemic inflammation and lipid metabolism in periodontitis patients: possible gender aspect. J Clin Periodontol. 2013;40(10):916–23. doi: 10.1111/jcpe.12145. [DOI] [PubMed] [Google Scholar]
- 60.Duzagac E, Cifcibasi E, Erdem M, Karabey V, Kasali K, Badur S, et al. Is obesity associated with healing after non-surgical periodontal therapy? A local vs. systemic evaluation. J Periodontal Res. 2016;51(5):604–12. doi: 10.1111/jre.12340. [DOI] [PubMed] [Google Scholar]
- 61.Hagh LG, Zakavi F, Hajizadeh F, Saleki M. The association between hyperlipidemia and periodontal infection. Iranian Red Crescent Medical Journal. 2014;16(12). [DOI] [PMC free article] [PubMed]
- 62.Joseph R, Nath SG, Joseraj M. Elevated plasma homocysteine levels in chronic periodontitis: A hospital-based case‐control study. J Periodontol. 2011;82(3):439–44. doi: 10.1902/jop.2010.100271. [DOI] [PubMed] [Google Scholar]
- 63.Kumar K, Ranganath V, Naik R, Banu S, Nichani A. Assessment of high-sensitivity C‐reactive protein and lipid levels in healthy adults and patients with coronary artery disease, with and without periodontitis–a cross‐sectional study. J Periodontal Res. 2014;49(6):836–44. doi: 10.1111/jre.12172. [DOI] [PubMed] [Google Scholar]
- 64.Lösche W, Karapetow F, Pohl A, Pohl C, Kocher T. Plasma lipid and blood glucose levels in patients with destructive periodontal disease. J Clin Periodontol. 2000;27(8):537–41. doi: 10.1034/j.1600-051x.2000.027008537.x. [DOI] [PubMed] [Google Scholar]
- 65.Monteiro AM, Jardini MA, Alves S, Giampaoli V, Aubin EC, Figueiredo Neto AM, et al. Cardiovascular disease parameters in periodontitis. J Periodontol. 2009;80(3):378–88. doi: 10.1902/jop.2009.080431. [DOI] [PubMed] [Google Scholar]
- 66.Penumarthy S, Penmetsa GS, Mannem S. Assessment of serum levels of triglycerides, total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol in periodontitis patients. J Indian Soc Periodontol. 2013;17(1):30. doi: 10.4103/0972-124X.107471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pushparani D, Anandan SN, Theagarayan P. Serum zinc and magnesium concentrations in type 2 diabetes mellitus with periodontitis. J Indian Soc Periodontol. 2014;18(2):187. doi: 10.4103/0972-124X.131322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sridhar R, Byakod G, Pudakalkatti P, Patil R. A study to evaluate the relationship between periodontitis, cardiovascular disease and serum lipid levels. Int J Dent Hyg. 2009;7(2):144–50. doi: 10.1111/j.1601-5037.2008.00318.x. [DOI] [PubMed] [Google Scholar]
- 69.Taleghani F, Shamaei M, Shamaei M. Association between chronic periodontitis and serum lipid levels. 2010. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.