Abstract
Objectives
Diabetic Peripheral Neuropathy (DPN) is the commonest complication in individuals with type 2 diabetes mellitus affecting 50% of total diabetic population. The ankle mobility is seen to be significantly reduced along with alteration in plantar pressure distribution. Neural mobilization is a neoteric technique that is being used to treat various conditions of neural involvement. It is hypothesized that the application of neural mobilization will improve ankle mobility and plantar pressure distribution in individuals with DPN by restoring the mechanical and neurophysiological functions of the tibial and common peroneal nerves.
Methods
A single group pre-post, quasi experimental, same subject design will be used. Participants with prior diagnosis of DPN will be selected according to eligibility criteria. The ankle ranges of motion (Both Active & Passive) and plantar pressure distribution at six foot regions will be taken as the outcome measures. All the participants will receive neural mobilization of tibial & common peroneal nerves (3 sets of 30 repetitions in 2 min with 1 min break in between) for 3 times/ week for 4 weeks. Outcome measurements will be taken at the baseline and after completion of the intervention.
Conclusion
This study will be investigating the possible advantageous effects of neural mobilization in improving ankle joint ranges of motion and plantar pressure distribution in patients with DPN and will help the clinicians and researchers develop preventive measures to reduce the burden of diabetic ulcers.
CTRI/2022/04/042187 [Registered on: 27/04/2022].
Keywords: Ankle, Ankle ROM, Diabetic peripheral neuropathy, Neural mobilization, Plantar pressure
Introduction
Diabetes mellitus is a clump of diversified metabolic diseases characterized by marked hyperglycemia and the individuals with diabetes are vulnerable to numerous serious complications like retinopathy, nephropathy and neuropathies [1, 2]. India is being known as a “diabetes capital” of the world, with an estimated 65 + million diabetic patients aged 20–79 years in 2013, and substantial further increase is anticipated [1]. International diabetes federation suggested a prevalence of 425 million people world-wide in 2017, expecting a rise up to 628 million by 2045 [3]. Diabetic peripheral neuropathy is one of the most prevalent chronic complications of diabetes mellitus affecting almost 50% of the total diabetic population and further increase in prevalence with the duration of diabetes [4, 5]. It can be focal or diffuse, proximal or distal, affecting both peripheral and autonomic system[2] occurring as a common consequence of type 1 and type 2 diabetes mellitus and chronic hyperglycemia. Individuals with diabetes often presents with alterations in gait biomechanics,such as reduced gait speed, decreased ankle joint range of motion and altered plantar pressure distribution patterns that increases the risk of developing planter ulcers.
In DPN patients, ankle Range of Motion (ROM) is known to be reduced significantly; mainly restricting the plantar flexion at ankle joint. Limited ankle joint movement has several clinical manifestations, including reduced shock absorption and altered plantar pressure distribution [4]. The rear foot(R) and forefoot(F) pressures are elevated in the diabetic peripheral neuropathic foot, but the F/R ratio is only seen increased in severe diabetic peripheral neuropathy. Also the Sensory impairment, foot deformities, limited joint mobility, reduced plantar tissue thickness, all these are interrelated to cause high forefoot plantar pressure. [5] Neural mobilization techniques are used to reinstate the dynamic balance between the mechanical interfaces and the relative movement of neural tissues, reducing the intrinsic pressure on the neural tissues and therefore promoting the superlative physiologic function of the nerves [6]. A previous study showed the effects of tibial nerve mobilization given for 3 weeks for improving the nerve conduction velocity in patients with diabetic peripheral neuropathy and thus reducing the neuropathic symptoms [7]. The effects of tibial nerve mobilization are also proved to improve the hip and ankle ranges of motion in healthy individuals. Evidence of the positive effects of neurodynamic mobilization along with manual therapy in common peroneal nerve palsy is also present where the proximal and distal sliders are given as 3 sets for 4 min with 1 min break in between each application [8]. This study will aim to investigate the effectiveness of neural mobilization in improving ankle ranges of motion and plantar pressure distribution in individuals with diabetic peripheral neuropathy.
Methods
Study design
This single group pre-post quasi experimental study will be conducted at the physiotherapy department of a tertiary care superspeciality hospital. The participants will be selected according to purposive sampling method. Prior to the participation, all details of the study will be explained and written informed consent will be taken from the subjects. The baseline and post treatment data for ankle ROM (active and passive) & plantar pressure distribution will be recorded using universal goniometer and Podia scan Software (Diabetik Foot Care India Pvt Limited) respectively.
The study has been approved by Institutional Research Ethics Committee (IEC/MMU/2021/1933) of Maharishi Markandeshwar (Deemed to be University), Mullana-Ambala, and Haryana, India. The trial is prospectively registered with trial registration number (CTRI/2022/04/042187). The data will be collected from Outpatient Department of Neurological Physiotherapy, Maharishi Markandeshwar Institute of physiotherapy & Rehabilitation.
Subjects & sample size
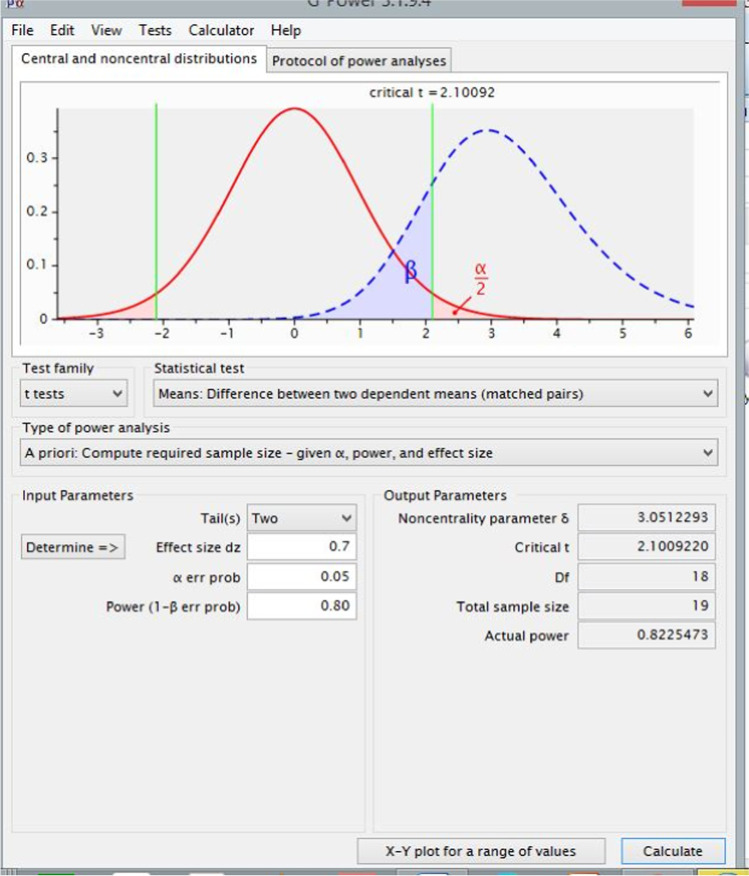
A sample of 23 subjects within age group of 35–70 years who will be referred by the physician as type 2 DM induced DPN will be included in the study. The exclusion of the patients will be done on the basis of presence of any other systemic disease rather than diabetes, diabetic ulcer in either foot, any history of amputation, fracture, strain, history of trauma leading to nerve injuries in last one year, any significant neurological dysfunction, patients with rheumatoid arthritis, fixed ankle contracture/ charcot joint or any recent vascular complications.. The sample size is calculated by statistical G Power 3.9.1.4 software [9]. The anticipated effect size is taken as 0.7 with level of significance (LOS) taken as 0.05 and power of study is set to be at 80% (β = 0.84). After the calculation sample size is found to be 23 with 20% [9] (Fig. 1).
Fig. 1.
Sample Size Calculation
Outcome measurements
Demographic & Anthropometric measurements (weight, height, BMI, limb length) will be done. Baseline measurements of ankle ROM (active & passive) and plantar pressure distribution will be taken prior to an intervention. Determination of baseline characteristics of every patient would be done by the therapist through the standardized assessment form. The plantar pressure measurements will be taken by using Harris mat [10] (Diabetik foot care India Pvt Limited) and will be analyzed using the Podia Scan Software [11].(Fig. 2) Both Active ROM and Passive ROM of Ankle joint (plantar flexion to dorsiflexion) will be measured using the Universal Goniometer, which has good reliability and validity [12]. During the treatment period all the participants will be allowed to follow their medical treatment protocol; if there is any alteration the participant will be excluded from the further analysis and the data will be considered for analysis using intention to treat analysis (Fig. 3).
Fig. 2.
Plantar Pressure Distribution using Podia Scan Software
Fig. 3.
Flow Chart of Neural Mobilization Techniques
Intervention
After the evaluation of all the assessments and determining the baseline measures, interventions would be given. Each participant will receive 30 min of session, conducting 3 times/ week for 4 consecutive weeks. The intervention includes both the neural sliders and tensioners for Tibial and Common Peroneal nerves (Figs. 4 and 5). The intervention procedure will include neural mobilization of tibial and common peroneal nerves that will proceed according to the steps given in the flow chart (Fig. 3). In the remote sequences, the hip joint will be kept in fixed position, and the remote joints i.e. knee and ankle will be moved. As the pain will subside, we will proceed to standard sequence. In standard sequence the hip and ankle joint will be moved keeping the knee in fixed position.
Fig. 4.
Sliders of Tibial nerve (a-c) and Common Peroneal Nerve (d-f)
Fig. 5.
Tensioners of Tibial nerve (a) and Common Peroneal Nerve (b)
Neural mobilization techniques:
For Tibial nerve
Remote Sliders: The therapist will do the dorsiflexion & eversion at the ankle joint and then passively move the hip in flexion and look for the onset of symptoms/pain. The therapist will lower the hip to few degrees in symptom free position. The knee will be moved into flexion (unloads the tibial nerve) with ankle DF & Eversion (loads the tibial nerve) and then released in knee extension (loading) with plantarflexion (unloading).
Local Sliders: The therapist will do the dorsiflexion & eversion at ankle joint and then passively move the hip in flexion and maintaining the knee in extension and look for the onset of symptoms/ pain. The therapist will lower the hip to a few degrees in symptom free position and then the hip will be moved in flexion (unloading of tibial nerve) with ankle DF & eversion (loading of tibial nerve) and then released in hip extension (loading) with plantarflexion (unloading).
Tensioners: The therapist will passively lift the patient’s leg off the table maintaining hip in flexion and knee in extension (stretch position of all non-moving joints). Then the ankle will be moved in DF & eversion (loading) and released into plantarflexion (unloading) [13].
For Common peroneal nerve
Remote sliders: The therapist will do the plantarflexion & inversion at the ankle joint and then passively move the hip in flexion and look for the onset of symptoms/pain. The therapist will lower the hip to few degrees in symptom free position. The knee will be moved into flexion (unloads the peroneal nerve) with ankle PF & inversion (loads the peroneal nerve) and then released in knee extension (loading) with Dorsiflexion (unloading).
Local Sliders: The therapist will do the Plantarflexion & Inversion at ankle joint and then passively move the hip in flexion and maintaining knee in extension and look for the onset of symptoms/pain. The therapist will keep the hip and knee in symptom free position and then the hip will be moved in flexion (unloading of peroneal nerve) with ankle PF & inversion (loading of peroneal nerve) and then released in hip extension (loading) with dorsiflexion (unloading).
Tensioners: The therapist will passively lift the patient’s leg off the table maintaining hip in flexion and knee in extension (stretch position of all non-moving joints). Then the ankle will be moved in PF& inversion (loading) and released into dorsiflexion(unloading) [13].
Gentle oscillations will be repeated for 3 sets (30 repetitions in 2 min) with 1 min rest in between. The amplitude of the oscillations will be increased gradually for each patient in accordance to his/her tolerance and reaction.
Statistical analysis
The data collected will be analyzed by the primary investigator. Descriptive statistics will be used to evaluate the baseline characteristics of the eligible participants. Depending on the distribution, which will be evaluated by the Shapiro–Wilk test, either the Wilcoxon Signed Rank test or a paired t-test will be used to compare the pre & post intervention results within the group [14]. Data will be analyzed using the statistical software (SPSS version 20. SPSS Inc. Chicago, II, USA) Level of significance will be set as 0.50.
Data confidentiality will be maintained throughout the course. Data assessment forms will be kept in specific folders only the researcher holding the key to it. Adverse effects occurring in the study may call out for interim analysis.
Result
Results will be reported after assessing variables on outcome measures for ankle ROM (active & passive) and plantar pressure distribution in individuals with DPN.
Discussion
The protocol involves the intervention including the neural mobilization techniques for improving the ankle mobility and plantar pressure distribution in individuals with diabetic peripheral neuropathy. This is the first study which will be evaluating the effectiveness of neural mobilization in this condition by upgrading the physiologic functions of the nerve due to its neural ‘’flossing’’ effect causing the restoration of normal mobility and axonal transport in compromised neural structures. Some previous studies showed the effects of neural mobilization in patients with nerve related disorders and most of them observed statistically significant improvements in pre and post intervention measurements. After neural mobilization, tissue mobility, blood circulation, and axonal transport, all of which are necessary for a neuron’s usefulness and mechanical integrity, will be increased. The present study will focus on improving the mobility at ankle joint by improving the Neuro-physiologic function of tibial and common peroneal nerves and modify the motor symptoms of diabetic neuropathy and will cause marked decrease in developing the risk of diabetic foot ulcers. The evidence of short term effectiveness of NM techniques (neural sliders and tensioners) on knee extension angle is available in which healthy individuals are taken and the intervention is compared with static hamstring stretching for improving knee extension angle [8]. A research report published in 2017 for the effectiveness of neural mobilization in treating the Neuro musculoskeletal conditions which shows the positive effects of NM on chronic low back pain, carpal tunnel syndrome, lateral epicondylalgia and plantar heel pain. Their findings also revealed that tensioning techniques are very effective in chronic nerve related back pain and plantar heel pain although sliders techniques are more adopted as they impart a less strain and greater mobilization of the nervous system. [3]
The neural mobilization can be done in active and passive ways; both are used effectively according to the choice of the therapist for different conditions. The active neural mobilization exercises can also be integrated in home exercises protocol of individuals with DPN.
Conclusion
This study will provide an insight to a potential rehabilitation measure which will be easy to use and can increase level of independence in individuals with diabetic peripheral neuropathy which may also improve their quality of life and decrease incidence of diabetic ulcers in future.
Abbreviations
- ROM
Range Of Motion
- DF
Dorsi Flexion
- PF
Plantar Flexion
- DPN
Diabetic Peripheral Neuropathy
Author’s contribution
MG is the principal investigator and drafted the manuscript. AS and MG are the supervisory team who participated in the review and approval of the intervention protocol. All authors were involved in the revision and editing of the manuscript. The final manuscript was read and approved by all authors.
Declarations
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Madhu Goyat, Email: madhugoyat813@gmail.com.
Akanksha Saxena, Email: akankshasaxena623@mmumullana.org, Email: akankshasaxena623@gmail.com.
Manu Goyal, Email: manu.goyal@mmumullana.org.
References
- 1.Wells JCK, Pomeroy E, Walimbe SR, Popkin BM, Yajnik CS. The Elevated Susceptibility to Diabetes in India: An Evolutionary Perspective. Front Public Heal. 2016;4:145. doi: 10.3389/fpubh.2016.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vinik A, Ullal J, Parson HK, Casellini CM. Diabetic neuropathies: Clinical manifestations and current treatment options. Nat Clin Pract Endocrinol Metab. 2006;2:269–281. doi: 10.1038/ncpendmet0142. [DOI] [PubMed] [Google Scholar]
- 3.Nathan MD. Long-Term Complications of Diabetes Mellitus. N Engl J Med. 1993;328:1676–1685. doi: 10.1056/NEJM199306103282306. [DOI] [PubMed] [Google Scholar]
- 4.Yavuz M, Erdemir A, Botek G, Hirschman GB, Bardsley L, Davis BL. Peak Plantar Pressure and Shear Locations. Diabetes Care. 2007;30:2643–5 . doi: 10.2337/dc07-0862. [DOI] [PubMed] [Google Scholar]
- 5.Caselli A, Pham H, Giurini JM, Armstrong DG, Veves A. The forefoot-to-rearfoot plantar pressure ratio is increased in severe diabetic neuropathy and can predict foot ulceration. Diabetes Care. 2002;25:1066–1071. doi: 10.2337/diacare.25.6.1066. [DOI] [PubMed] [Google Scholar]
- 6.Shacklock M. Neural mobilization: A systematic review of randomized controlled trials with an analysis of therapeutic efficacy. J Man Manip Ther. 2008;16:23–24. doi: 10.1179/106698108790818594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doshi MK, Singarvelan RM. Effect of Tibial Nerve Mobilization on Nerve Conduction Velocity in Diabetic Neuropathy Patient. Int J Heal Sci Res. 2019;9:218–224. [Google Scholar]
- 8.Villafañe JH, Pillastrini P, Borboni A. Manual therapy and neurodynamic mobilization in a patient with peroneal nerve paralysis : a case report. J Chiropr Med Nat Univ Health Sci. 2013;12:176–81. doi: 10.1016/j.jcm.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang H. Sample size determination and power analysis using the G * Power software. 2021;1–12. [DOI] [PMC free article] [PubMed]
- 10.Cisneros LL, Fonseca THS, Abreu VC. Inter- and intra-examiner reliability of footprint pattern analysis obtained from diabetics using the Harris Mat. Rev Bras Fisioter. 2010;14:200–205. doi: 10.1590/S1413-35552010000300011. [DOI] [PubMed] [Google Scholar]
- 11.Ramamoorthy V. Physiatrist ’ s Assessment and Management of Diabetic Foot. Int J Heal Sci Res. 2019;9:219–223. [Google Scholar]
- 12.Suman VJ. Reliability of Goniometric Measurements and Visual Estimates of Ankle Joint Active Range of Motion Obtained in a Clinical Setting. Arch Phys Med Rehabil. 1993;74:1113–1118. doi: 10.1016/0003-9993(93)90071-H. [DOI] [PubMed] [Google Scholar]
- 13.Butler DS. The Neurodynamic Techniques; A difinitive guide fromthenoigroup. Noigroup Publications for NOI Australasia; 2005.
- 14.Mishra P, Pandey CM, Singh U, Gupta A, Sahu C, Keshri A. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth. 2019;22:67–72. doi: 10.4103/aca.ACA_157_18. [DOI] [PMC free article] [PubMed] [Google Scholar]