Abstract
Periprosthetic joint infection remains a major complication in arthroplasty. We present the first description of a case of periprosthetic joint infection with Actinomyces radingae, microorganism that is mostly found on the skin of the upper body and might cause particular challenges as it is difficult to culture and specify. Furthermore, a thorough microbiologic workup may indicate the source of infection. In this case, it is possible that perspiration from the surgeon was the source of intraoperative contamination. Intraoperative contamination through perspiration may be important and should be avoided by all means.
Keywords: Periprosthetic joint infection, PJI, Total hip arthroplasty, THA, Actinomyces radingae
Introduction
Total hip arthroplasty (THA) is a very successful treatment for various pathologies of the hip joint [1]. Nevertheless, there are major complications. Among these, periprosthetic joint infection (PJI) has a lifetime incidence of approximately 1% after THA [2,3]. Coagulase-negative staphylococci, Staphylococcus aureus, and Streptococcus spp. account for the vast majority of the detected organisms in hip PJI cases [[4], [5], [6]]. Anaerobic bacteria make up 3%-6% of the causative microorganisms [7].
We present a case of PJI with a rare species of Actinomyces. This report represents the first case description with Actinomyces radingae as the causative microorganism for PJI, to the best of our knowledge. It also demonstrates that detailed interpretation of the findings might help identify a specific and easily neglected source of contamination.
Case history
Six years prior to initial consultation of a 51-year-old male patient, internal fixation of the proximal femur had been performed with a cephalomedullary nail due to a nondisplaced intertrochanteric fracture. As the patient felt pain around the greater trochanter, possibly caused by the nail, it had been removed 1 year later as the fracture had consolidated in an anatomic position. Apart from suffering from chronic low back pain and being a smoker, the patient was otherwise healthy, taking only analgesics like paracetamol and nonsteroidal anti-inflammatory drugs. He then had been asymptomatic until groin pain developed about 1 year prior to consultation. Osteoarthritis had then been diagnosed and THA had been performed (Fig. 1). Early recovery had been uneventful. After 3 months, the patient presented good hip function but complained of persistent groin pain. The symptoms worsened, and cup loosening was identified 1 month later (Fig. 1). While white blood cell count was normal and c-reactive protein was only slightly elevated (9 mg/l), joint aspiration yielded a cell count suspicious of infection (3546 leucocytes/μl with 81% polymorphonuclear granulocytes), and A. radingae was identified in 2 separate samples taken at repeated aspiration. Further testing showed that the bacterium was sensitive to beta-lactam antibiotics but resistant to clindamycin.
Figure 1.
Zone of interest of the conventional radiographs of the pelvis showing the right hip of the 51-year-old patient described. (a) Situation prior to THA. Note the postoperative and posttraumatic alterations of the proximal femur, after internal fixation (black arrows). Osteoarthritis was mainly posteroinferior. (b) postoperative control after THA. The cup is seated slightly too medially, the medial border crossing the ilioischial line (black arrowheads), and cranially. Leg length and femoral offset were reconstructed properly. (c) Radiograph after 4 months. Note loosening of the cup and shortening of the leg consecutive to migration of the cup. (d) After revision with debridement, exchange of the cup and implantation of vancomycin-loaded calcium sulphate beads (asterisk). Note restoration of an anatomic centre of rotation, with the cup not protruding anymore medially to the ilioischial line (black arrowheads). (e) Eighteen months after revision, showing no signs of loosening. Particularly, the residual sclerotic bone of the acetabulum resorbed, indicating proper integration of the cup. The calcium sulphate beads dissolved within months.
Despite the delay of 22 weeks since the index operation, debridement with retention of the stem but revision of the loose cup was performed through the anterior approach used for the primary THA. This choice was made in agreement with in-house infectious diseases specialists, since the stem was well integrated, and the biofilm development by the identified microorganism was not considered to require any extension of the antibiotic treatment nor any additional biofilm-active drug. Systemic antibiotic treatment was enhanced by local application of antibiotic-loaded calcium sulfate beads (50-ml Osteoset; Wright Medical Technologies, Arlington, TN) with 4 g of vancomycin (Vancomycin Labatec; Labatec Pharma, Geneva, Switzerland). Intraoperative microbiological sampling identified A. radingae in all 5 biopsies, as well as Staphylococcus epidermidis in 2 tissue biopsies. Furthermore, Peptoniphilus lacrimalis as well as the aforementioned bacteria were identified in the sonicate of the retrievals. Initially, amoxicillin and daptomycin were administered intravenously for 2 weeks [8,9], followed by oral levofloxacin and rifampicin, for a total duration of 3 months. Even though Staphylococcus epidermidis was identified, a decision was made against secondary revision of the stem, as vancomycin was applicated locally in biofilm-active doses [10,11].
More than 2 years after the discontinuation of the antibiotics, the patient shows good function of the hip with a free range of motion without any signs of persistent infection. Nevertheless, he complains of persistent groin pain as well as lower back pain radiating to the hip and thigh. Blood testing and joint aspiration were repeated without pathologic findings (white blood cell 5.42 G/l, c-reactive protein < 1 mg/l; 650 leucocytes/μl with 21% polymorphonuclear granulocytes), as it also was the case at a second institution. Arthritis of the iliosacral joint was postulated, and infiltration with steroids was performed. This relieved the pain for more or less 6 months, and pain remains under control with basic analgesics like paracetamol and nonsteroidal anti-inflammatory drugs. Furthermore, bilateral inguinal hernias have been diagnosed as one possible cause for the persisting groin pain.
The patient provided written informed consent for publication of anonymized data.
Biofilm culture and imaging
A. radingae biofilms were grown on medical-grade titanium-aluminum-niobium discs in Brain Heart Infusion broth (BHI broth; Oxoid AG, Pratteln, Switzerland). The deep-frozen clinical strain was subcultured and adjusted to optical density of 1.0 at 600 nm, and 1 mL of this inoculum was added to a sterile container with 20 mL of BHI per single titanium-aluminum-niobium disc. The culture was incubated at 100 rpm at 37°C for 48 hours. Then, the discs were transferred into 10 ml of sterile phosphate-buffered saline solution. Biofilm was quantified by sonication of the disc for 5 minutes in an ultrasound water bath (Bandelin Sonorex Super 10P; Bandelin, Berlin, Germany) followed by vortexing for 30 seconds and subsequent serial dilution onto Mueller-Hinton-Agar plates. Plates were incubated at 37°C, and colony forming units were counted after 24 hours.
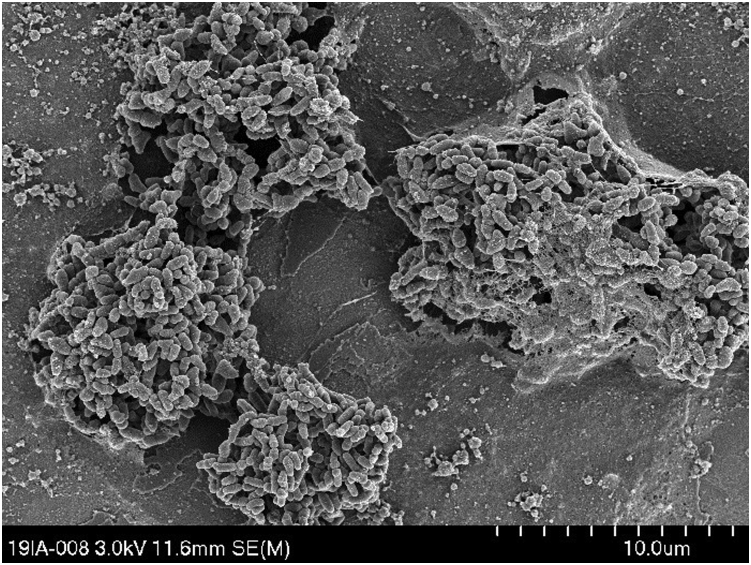
One additional disc was examined after 48 hours of incubation by scanning electron microscopy. The sample was dehydrated through a series of steps with ethanol at increasing concentration (70%, 80%, 90%, 96%, and 100%). Discs were then air-dried overnight and sputter-coated with 10-nm gold and palladium, using a BAL-TEC MED 020 sputter coater connected to a BAL-TEC MCS 010 and a BAL-TEC QSG 060 (BAL-TEC, Principality of Liechtenstein). Images of the surface (Fig. 2) were acquired using an S-4700 field emission scanning electron microscope and Quartz PCI image management system (Hitachi, Chiyoda, Japan), set at an accelerating voltage of 3 kV, a current of 40 μA, and a working distance of 12 mm.
Figure 2.
Scanning electron micrograph of Actinomyces radingae biofilm. Biofilm was grown over 48 hours on medical-grade titanium-aluminum-niobium disc and showed numerous clusters of cells, suggestive of microcolony or biofilm formation. Additionally, note the extracellular polymeric substances appearing to cover partially the cluster on the right-hand side. Biofilms were fixed with ethanol, sputter-coated with gold and palladium, and imaged using a Hitachi S-4700 field emission scanning electron microscope. We counted how many cells were within the biofilm, and it was approximately 100,000 per disc. This is less than we would expect from a staphylococcal biofilm by about 20- to 50-fold.
Discussion
The genus Actinomyces encompasses many groups of gram-positive rods that are either facultative anaerobic or microaerophilic [12]. Numerous species of this genus are part of the human commensal flora of the skin and oral cavity [13]. Actinomyces are among the dominant species in dental plaque. Furthermore, A. radingae is known to be found especially on the skin of the upper body [14]. The true incidence of infections due to this genus remains unclear due to several reasons. One reason is that these bacteria are difficult to culture and specify phenotypically [15]. Furthermore, they are rarely isolated alone and were, therefore, often considered as contaminants [15]. This changed during the 1980s and 1990s, as new biochemical methods were able to specify and separate the group of so-called nondiptheria Corynebacterium [16]. With growing awareness, Actinomyces spp. were found more frequently to be pathogenic, for example, in genital pathologies, urinary tract infections, skin-related infections, appendicitis, cholecystitis, or ear-nose-throat infections. In a series of 294 infections with Actinomyces-like organisms, Actinomyces spp. were isolated alone in only 84 cases (29%), with the spectrum of concomitant flora including both anaerobic and aerobic bacteria [15]. To the best of our knowledge, this is the first case describing A. radingae in PJI. A. radingae is also able to form biofilms (Fig. 2). However, this is not known to be particularly problematic regarding antibiotic treatment, as it is for other microorganisms [[17], [18], [19]].
As only A. radingae had been identified in the joint aspiration by the time of revision and as biofilm formation of this pathogen is not considered to be problematic regarding antibiotic treatment, as it would be for Staphylococcus spp., Pseudomonas spp., or fungi, a major partial revision was chosen, even though such procedures are known to be unfavorable in terms of re-revision rates [20]. Despite a longer delay, success rates of implant-retaining procedures remain high, if associated with adequate, biofilm-active antibiotic treatment [[21], [22], [23], [24]]. Despite the later identification of the concomitant presence of Staphylococcus spp., the treatment remained successful regarding cure of infection. The European standard treatment scheme with 2 weeks of intravenous treatment followed by 10 weeks of oral treatment with biofilm-active drugs with high bioavailability had been applied [8,9]. Enhancing the systemic antibiotic treatment with local vancomycin-loaded calcium sulphate beads might be another explanation, as this treatment is able to reach antibiotic concentrations above the levels necessary for eradication of mature biofilms [10,11,25]. Actinomyces spp. may be considered as being sensitive to vancomycin [26,27]. However, when joint aspiration reveals Actinomyces spp., one must take into consideration the presence of a polymicrobial infection [15].
PJI is one of the major complications after THA, with a life-long incidence of 1% in large register-based studies [2,3,28]. In the case reported here, PJI most probably developed secondary to intraoperative contamination, considering that multiple bacterial strains were identified. Hematogenous contamination is very unlikely in a polymicrobial infection. All 3 (A. radingae, S. epidermidis, and P. lacrimalis) are skin commensals, A. radingae in particular as it is a commensal especially present on the skin of the upper body [14]. Therefore, contamination of the surgical site by perspiration of the operating room personnel has to be considered as a likely cause of infection. As A. radingae is rare among all Actinomyces spp., identification of this species on the surgeon’s forehead would have proven the hypothesis, but he refused sampling. Furthermore, the use of surgical helmets might have prevented the contamination in this particular case. Due to a variety of complex mechanisms, these devices are however not able to reduce overall PJI rates and may not be recommended in general [29].
Summary
Rare microorganisms must be taken into consideration as a causative in cases of PJI. To the best of our knowledge, this is the first report of A. radingae causing PJI. While Actinomyces spp. are common skin commensals, the species radingae identified in this case, as well as the other bacteria identified, point towards contamination of the surgical site by perspiration from the surgeon. Despite biofilm formation in chronic PJI, implant removal may not be necessary in case of infection with such microorganisms.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.08.023.
Informed patient consent
The authors confirm that written informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report.
Author contributions
Conceptualization: H.K., S.P., and P.W.; methodology: H.K., S.P., T.F.M., and P.W.; investigations: H.K., T.F.M., and P.W.; writing – original draft: H.K. and P.W.; writing – review and editing: S.P., T.F.M., and C.M.; visualization: H.K. and T.F.M.; supervision: P.W.; resources: C.M. and P.W.; project administration: P.W.
Appendix A. Supplementary Data
References
- 1.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Gundtoft P.H., Overgaard S., Schønheyder H.C., Møller J.K., Kjærsgaard-Andersen P., Pedersen A.B. The “true” incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties. Acta Orthop. 2015;86:326–334. doi: 10.3109/17453674.2015.1011983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huotari K., Peltola M., Jämsen E. The incidence of late prosthetic joint infections. Acta Orthop. 2015;86:321–325. doi: 10.3109/17453674.2015.1035173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holleyman R.J., Baker P.N., Charlett A., Gould K., Deehan D.J. Analysis of causative microorganism in 248 primary hip arthroplasties revised for infection: a study using the NJR dataset. Hip Int. 2016;26:82–89. doi: 10.5301/hipint.5000313. [DOI] [PubMed] [Google Scholar]
- 5.Geipel U. Pathogenic organisms in hip joint infections. Int J Med Sci. 2009;6:234–240. doi: 10.7150/ijms.6.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rafiq I., Gambhir A.K., Wroblewski B.M., Kay P.R. The microbiology of infected hip arthroplasty. Int Orthop. 2006;30:532–535. doi: 10.1007/s00264-006-0125-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah N.B., Tande A.J., Patel R., Berbari E.F. Anaerobic prosthetic joint infection. Anaerobe. 2015;36:1–8. doi: 10.1016/j.anaerobe.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Zimmerli W., Trampuz A., Ochsner P.E. Prosthetic-joint infections. N Engl J Med. 2004;351:1645–1654. doi: 10.1056/NEJMra040181. [DOI] [PubMed] [Google Scholar]
- 9.Osmon D.R., Berbari E.F., Berendt A.R., Lew D., Zimmerli W., Steckelberg J.M., et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1–e25. doi: 10.1093/cid/cis803. [DOI] [PubMed] [Google Scholar]
- 10.Wahl P., Guidi M., Benninger E., Rönn K., Gautier E., Buclin T., et al. The levels of vancomycin in the blood and the wound after the local treatment of bone and soft-tissue infection with antibiotic-loaded calcium sulphate as carrier material. Bone Joint J. 2017;99-B:1537–1544. doi: 10.1302/0301-620X.99B11.BJJ-2016-0298.R3. [DOI] [PubMed] [Google Scholar]
- 11.Post V., Wahl P., Richards R.G., Moriarty T.F. Vancomycin displays time-dependent eradication of mature Staphylococcus aureus biofilms. J Orthop Res. 2017;35:381–388. doi: 10.1002/jor.23291. [DOI] [PubMed] [Google Scholar]
- 12.Garrity G., Brenner D.J., Krieg N.R., Staley J.T. In: Bergey’s Manual® of systematic bacteriology volume two: the proteobacteria (Part C) Brenner D., editor. Springer US; New York, NY: 2005. [Google Scholar]
- 13.Sarkonen N., Könönen E., Summanen P., Könönen M., Jousimies-Somer H. Phenotypic identification of Actinomyces and related species isolated from human sources. J Clin Microbiol. 2001;39:3955–3961. doi: 10.1128/JCM.39.11.3955-3961.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hama Attar K., Waghorn D., Lyons M., Bs B.M., Cunnick G. Rare species of Actinomyces as causative pathogens in breast abscess. Breast J. 2007;13:501–505. doi: 10.1111/j.1524-4741.2007.00472.x. [DOI] [PubMed] [Google Scholar]
- 15.Sabbe L.J.M., Van De Merwe D., Schouls L., Bergmans A., Vaneechoutte M., Vandamme P. Clinical spectrum of infections due to the newly described Actinomyces species A. turicensis, A. radingae, and A. europaeus. J Clin Microbiol. 1999;37:8–13. doi: 10.1128/jcm.37.1.8-13.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coyle M.B., Lipsky B.A. Coryneform bacteria in infectious diseases: clinical and laboratory aspects. Clin Microbiol Rev. 1990;3:227–246. doi: 10.1128/CMR.3.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aslam S. Effect of antibacterials on biofilms. Am J Infect Control. 2008;36:S175.e9–S175.e11. doi: 10.1016/j.ajic.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Bjarnsholt T., Jensen P.Ø., Fiandaca M.J., Pedersen J., Hansen C.R., Andersen C.B., et al. Pseudomonas aeruginosa biofilms in the respiratory tract of cystic fibrosis patients. Pediatr Pulmonol. 2009;44:547–558. doi: 10.1002/ppul.21011. [DOI] [PubMed] [Google Scholar]
- 19.Baeza J., Cury M.B., Fleischman A., Ferrando A., Fuertes M., Goswami K., et al. General assembly, prevention, local antimicrobials: proceedings of international consensus on orthopedic infections. J Arthroplasty. 2019;34:S75–S84. doi: 10.1016/j.arth.2018.09.056. [DOI] [PubMed] [Google Scholar]
- 20.Engesæter L.B., Dale H., Schrama J.C., Hallan G., Lie S.A. Surgical procedures in the treatment of 784 infected THAs reported to the Norwegian Arthroplasty Register. Acta Orthop. 2011;82:530–537. doi: 10.3109/17453674.2011.623572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker S.J.M., Grammatopoulos G., Davies O.L.I., Lynch K., Pollard T.C.B., Andrade A.J. Outcomes of hip arthroplasty after failed hip arthroscopy: a case-control study. J Arthroplasty. 2017;32:3082–3087.e2. doi: 10.1016/j.arth.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 22.Martínez-Pastor J.C., Vilchez F., Pitart C., Sierra J.M., Soriano A. Antibiotic resistance in orthopaedic surgery: acute knee prosthetic joint infections due to extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae. Eur J Clin Microbiol Infect Dis. 2010;29:1039–1041. doi: 10.1007/s10096-010-0950-y. [DOI] [PubMed] [Google Scholar]
- 23.Shohat N., Goswami K., Tan T.L., Yayac M., Soriano A., Sousa R., et al. Frank Stinchfield Award: identifying who will fail following irrigation and debridement for prosthetic joint infection. Bone Joint J. 2020;102-B:11–19. doi: 10.1302/0301-620X.102B7.BJJ-2019-1628.R1. [DOI] [PubMed] [Google Scholar]
- 24.Barberán J., Aguilar L., Carroquino G., Giménez M.-J., Sánchez B., Martínez D., et al. Conservative treatment of staphylococcal prosthetic joint infections in elderly patients. Am J Med. 2006;119:993.e7–993.e10. doi: 10.1016/j.amjmed.2006.03.036. [DOI] [PubMed] [Google Scholar]
- 25.Gramlich Y., Johnson T., Kemmerer M., Walter G., Hoffmann R., Klug A. Salvage procedure for chronic periprosthetic knee infection: the application of DAIR results in better remission rates and infection-free survivorship when used with topical degradable calcium-based antibiotics. Knee Surg Sports Traumatol Arthrosc. 2020;28:2823–2834. doi: 10.1007/s00167-019-05627-8. [DOI] [PubMed] [Google Scholar]
- 26.Steininger C., Willinger B. Resistance patterns in clinical isolates of pathogenic Actinomyces species. J Antimicrob Chemother. 2016;71:422–427. doi: 10.1093/jac/dkv347. [DOI] [PubMed] [Google Scholar]
- 27.Barberis C., Budia M., Palombarani S., Rodriguez C.H., Ramírez M.S., Arias B., et al. Antimicrobial susceptibility of clinical isolates of Actinomyces and related genera reveals an unusual clindamycin resistance among Actinomyces urogenitalis strains. J Glob Antimicrob Resist. 2017;8:115–120. doi: 10.1016/j.jgar.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 28.Fowler T.J., Sayers A., Whitehouse M.R. Two-stage revision surgery for periprosthetic joint infection following total hip arthroplasty. Ann Transl Med. 2019;7:S261. doi: 10.21037/atm.2019.12.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Young S.W., Zhu M., Shirley O.C., Wu Q., Spangehl M.J. Do “surgical helmet systems” or “body exhaust suits” affect contamination and deep infection rates in arthroplasty? A systematic Review. J Arthroplasty. 2016;31:225–233. doi: 10.1016/j.arth.2015.07.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.