Abstract
The promise of COVID-19 vaccines in ending the pandemic can only be achieved by overcoming the challenge of vaccine refusal. Healthcare workers (HCWs) are the trusted advisors of vaccination decisions. Recommendations for vaccinating children against COVID-19 are recently gaining more public health attention due to the role of children in disease transmission and associated morbidities. Vaccination is one of the first medical decisions parents or guardians make on behalf of their children. To investigate the determinants associated with vaccine acceptability among the general population through a direct interview questionnaire and assess guardians’ views towards childhood COVID-19 vaccinations. This cross-sectional study included 2919 participants A pre-designed structured questionnaire about COVID-19 vaccination acceptability was completed by trained interviewers and interviewing the participants or their guardians (for those below 18 years old). Nearly two-thirds of participants (66.5%) accepted vaccination, 20.2% were refusing and 13.3% were hesitant. Most participants who were guardians of children below 12 years and from 13 to 17 years reported that they would accept vaccination of their children (72.5% and 70.5%, respectively). The acceptance rate among HCWs was 58.2%. The main reasons beyond vaccine refusal were mistrust of vaccine efficacy (39.5%) and having concerns regarding vaccine safety (38.8%). In a multivariable regression model, being male (OR 1.362, 95% CI 1.082–1.714, p = 0.008) resident in rural area (OR 1.796, 95% CI 1.435–2.247, p = 0.000), and lower education (OR 1.245, 95% CI 1.018–1.523, p = 0.033) were associated with an increased acceptance to be vaccinated. The acceptance rate for vaccinating children reported among their guardians was higher than adults for themselves. Extremes of age showed higher vaccine acceptance compared to young adults. Upper Egypt governorates (Faiyum and Giza) were outpacing Lower Egypt governorates in vaccination acceptance rates.
Subject terms: Health care, Medical research
Introduction
Vaccination reduced the mortality rates of major communicable diseases over decades. Correspondingly, mass coronavirus disease-2019 (COVID-19) vaccination ultimately might end the COVID-19 pandemic by obtaining herd-immunity level coverage, enabling communities to return to their pre-COVID-19 state1.
The World Health Organization (WHO) reported COVID-19 vaccine delivery challenges due to the significant roadblock, vaccine acceptance2. It is defined as “the degree to which individual question, accept, or refuse vaccination.” It is an essential indicator for vaccine uptake rate (vaccination uptake = access + acceptance), and consequently, vaccine distribution success3.
Attitude toward the vaccines is dynamic and considerably changes over time as it is affected by complex personal factors, complacency (do not perceive a need for a vaccine, do not value vaccination), convenience (access to vaccines), effectiveness, side effects, novel techniques of vaccines and risk of COVID-19 exposure4. Healthcare workers (HCWs) are strong advocates for better dissemination of vaccine knowledge and boosting vaccine acceptance among the general population5.
Acceptance of COVID-19 vaccines among samples of the adult Egyptian population and HCWs was investigated in certain governorates through online surveys6–9. Despite the easiness of performing these online surveys (especially during the COVID-19 pandemic), they are known to have accessibility issues and selection bias compared to the interview questionnaire due to the under-representation of some population sectors such as children, the elderly, and illiterates10. This highlights the importance of investigating vaccine acceptance determinants via interview questionnaire across different governorates of Egypt. Moreover, to the best of our knowledge, there is scarce information on the Egyptian parents’ or guardians’ acceptability of COVID-19 vaccines to their children (below 18 years). The success of the future COVID-19 vaccination program for children will depend on guardians’ views towards childhood vaccinations. Exploring the acceptance rate and their predictors would support establishing new policies to promote vaccine uptake.
A global vaccine survey across several countries recognized insufficient knowledge about the vaccines, misinformation from social media, little efficacy and serious adverse effects causing death, manufacturers do not disclose adverse effects of vaccines, and political affiliation as the perceived barriers for accepting of COVID-19 vaccination11–13.
The aim of the present study was to determine the rate of vaccine acceptance and shed light on its predictors among the Egyptian population for themselves or their children across different governorates and among HCWs by direct interview questionnaire.
Methods
A cross-sectional survey-based study was conducted between January and June 2021. This period coincided with the second and third waves of the COVID-19 pandemic in Egypt. According to the Egyptian Ministry of Health and Population, the second pandemic wave of COVID-19 had stricken Egypt from November 2020 till January 2021, and the third wave started from March 2021. At that time, vaccines for COVID-19 were reserved primarily for HCWs and high-risk groups of the general population. Only two vaccine types were available, namely, Sinopharm BBIBP and Oxford/AstraZeneca COVID-19 vaccine (AZD1222).
Study population
This study was a part of a project which enrolled 2919 participants (2276 participants from the community and 643 HCWs from 39 hospitals across Egypt). The study was performed across ten Egyptian governorates, eight from Lower Egypt (Alexandria, Monufia, Cairo, Suez, Qalyubia, Dakahlia, Beheria, Kafr Elsheikh), and two from Upper Egypt (Faiyum and Giza). All governorates, settings and study participants were selected randomly. The sampling techniques were described elsewhere14.
Data collection
A pre-designed structured questionnaire was completed by trained interviewers interviewing the participants or their guardians (for those below 18 years old). The study questionnaire was comprehensive but easy to understand. It comprised multiple sections with 90 items; one section included all general demographic information; age, sex, residence, occupation, education, lifestyle behaviors, and anthropometric data. The height and weight of all participants were measured to calculate their Body Mass Index (BMI). Standard adult BMI groupings were applied: underweight (BMI < 18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), and obese (BMI ≥ 30). Children's BMI classification was as follows; underweight (< 5th percentile), normal weight (5th to < 85th percentile), and overweight/ Obese (> 85th percentile). Associated comorbidities were recorded. Another section of the questionnaire comprised questions about contact with COVID-19 patients, history of COVID-19 infection, nature, and severity of symptoms. Some work setting data of HCWs were included in the questionnaire sheet, such as job category (physicians, nurses, pharmacist, etc.) type of hospital (COVID-19 isolation hospital or not). Departments of HCWs were categorized as being high-risk departments; intensive care units, emergency room, internal medicine wards, radiology, laboratory, or outpatient clinics) versus low-risk departments (others).
Subsequently, participants were asked about their acceptance to receive a potential COVID-19 vaccine by the following questions: “Do you agree to receive COVID-19 vaccine?” Answer options included “Yes,” “No,” and “Not sure.”, and if the answer was “no”, an open question was asked to assess the reasons for vaccine rejection “what is the cause of refusal?” The general acceptance of COVID-19 vaccine was the primary outcome variable of the study. It was categorized as accepting (Yes), refusing (No), and hesitant (Not sure).
To delineate spatial pattern of vaccine acceptance in the study area, the collected data were mapped using ArcGIS (ver. 10.8) (ESRI 2020) and two thematic maps were produced representing the vaccine acceptance and vaccine hesitancy in different governorates. Such mapping can highlight spatial variations in vaccine acceptance in the study area, which can be further justified by prevailing socioeconomic and cultural factors15.
Statistical analysis
Data were fed to statistical software IBM SPSS version 22 (SPSS, Inc. Chicago, IL). Quantitative variables were expressed by the mean (X̅) and standard deviation (SD), while categorical variables by absolute and relative frequency. Descriptive analysis based on frequency and percent distribution was done for all categorical variables, including socio-demographic and behavioral data. Cross-tabulation and Chi-squared (χ2) test were used to analyze the associations between accepting the vaccine and the characteristics of participants. All statistical analyses were done using two-tailed tests. A P-value less than 0.05 was considered statistically significant. All questionnaire data was assessed in univariate analysis. Multiple logistic regression analysis was conducted to assess the significant independent predictors of COVID-19 vaccines’ acceptability with 95% confidence intervals (95% CI). For handling the missing data (where “not applicable” is the response), the model was conducted only on adult sample (n = 2352) and occupation related variables (e.g., type of the hospital, working hours) were removed from the model. The dependent variable was set as a dichotomous variable coded as “1” if the participant accept to take the vaccine, and “zero” otherwise (Refuse or hesitant).
Ethics approval
The study was conducted in compliance with the Helsinki Declaration and was approved by the Institutional Review Board (IRB) Committee, Faculty of Medicine, Alexandria University; IRB number: 00012098—FWA number: 00018699, serial number: 0305136. Anonymity and confidentiality of participants were confirmed and written informed consent was obtained from each participant. For young participant less than 18 years, informed consent from a parent and/or legal guardian for study participation was obtained.
Consent to participate
Written informed consent was obtained from all participants.
Results
A total of 2919 participants completed the study questionnaire. Their age ranged from 2 to 90 years (mean = 37.07, SD 17.944 years). Most of them were in the age group of 25–39 years (820; 28.1%), followed by those aged from 40 to 49 years (533; 18.3%), and a minority of them were in the age group of 70–90 years (79; 2.7%). 567 (19.4%) were below 18 years. The majority of participants were women (1675; 57.4%), urban residents (2029; 69.5%), and married (76.5%). Most study participants reported having a university degree or higher (44.4%). Only 823 (28.2%) of participants had associated comorbidities. 43.1% of HCWs were physicians, 17.9% were nurses, and the remaining were technicians, pharmacists, and others.
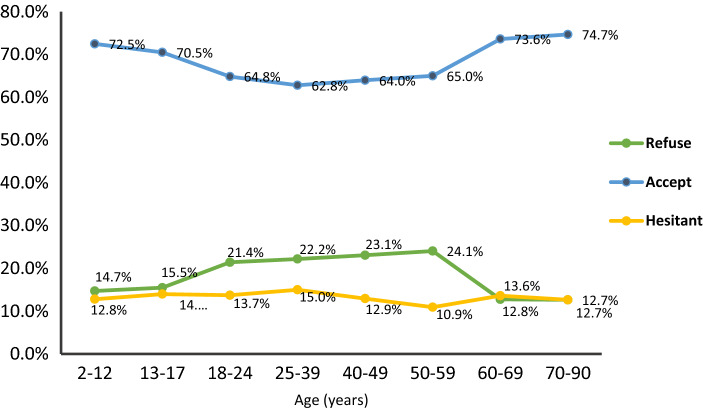
Participants demonstrated an overall 66.5% (1940/2919) acceptance rate to get a COVID-19 vaccine for themselves. Most participants who were guardians of children below 12 years and from 13 to 17 years reported that they would accept vaccination of their children (72.5% and 70.5%, respectively). The highest acceptability rate was among elderly group (70–90 years) (74.7%) (p = 0.001) (Fig. 1).
Figure 1.
Vaccine acceptance in different age groups.
Males represented a higher percentage among the vaccine acceptance group compared to those who refused (45.1% vs. 38.5%, p = 0.001). Also, rural residence had significantly a higher frequency among the acceptance group compared the refusal one (35.6% vs. 18.3%, p = 0.000). Neither pre-existing comorbidities nor history of travel during the last six months or body weight were statistically associated with vaccine acceptability. Smokers constituted a higher proportion among the acceptance group compared to the refusal group (28.6% vs. 13.2%; p = 0.003) (Table 1).
Table 1.
Factors associated with COVID-19 vaccine acceptance (n = 2919).
| Willing to receive COVID-19 vaccine | p-value | ||||||
|---|---|---|---|---|---|---|---|
| No (refuse) (n = 590) |
Yes (accept) (n = 1940) |
Not sure (hesitant) (n = 389) | |||||
| No | % | No | % | No | % | ||
| Gender | 0.001* | ||||||
| Male | 227 | 38.5% | 874 | 45.1% | 143 | 36.8% | |
| Female | 363 | 61.5% | 1066 | 54.9% | 246 | 63.2% | |
| Residence | 0.000* | ||||||
| Urban | 482 | 81.7% | 1249 | 64.4% | 298 | 76.6% | |
| Rural | 108 | 18.3% | 691 | 35.6% | 91 | 23.4% | |
| Comorbidities | 0.633 | ||||||
| No | 424 | 71.9% | 1385 | 71.4% | 287 | 73.8% | |
| Yes | 166 | 28.1% | 555 | 28.6% | 102 | 26.2% | |
| BMI | 0.210 | ||||||
| Normal weight | 154 | 26.1% | 504 | 26.0% | 96 | 24.7% | |
| Underweight | 11 | 1.9% | 24 | 1.2% | 11 | 2.8% | |
| Overweight/ obese | 425 | 72.0% | 1412 | 72.8% | 282 | 72.5% | |
| Smoking status | 0.003* | ||||||
| No | 512 | 86.8% | 1385 | 71.4% | 287 | 73.8% | |
| Yes | 78 | 13.2% | 555 | 28.6% | 102 | 26.2% | |
| Exercise | 0.096 | ||||||
| No | 104 | 17.6% | 297 | 15.3% | 75 | 19.3% | |
| Yes | 486 | 82.4% | 1643 | 84.7% | 314 | 80.7% | |
| History of travel abroad within the last six months | 0.676 | ||||||
| No | 587 | 99.5% | 1923 | 99.1% | 386 | 99.2% | |
| Yes | 3 | 0.5% | 17 | 0.9% | 3 | 0.8% | |
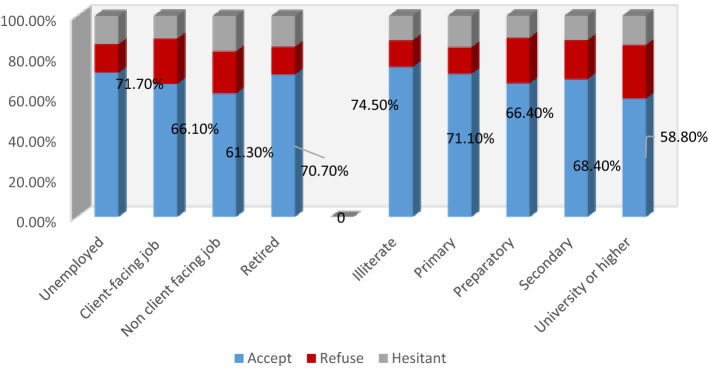
Surprisingly, a significantly higher percentage of illiterates were accepting COVID-19 vaccination (74.5%; p = 0.000), followed by primary education (71.1%) and secondary education (68.4%). Regarding occupation, the highest acceptability was among unemployed (71.7%) and retired participants (70.7%), followed by those working at client-facing jobs (66.1%) (p = 0.000) (Fig. 2).
Figure 2.
The acceptance of COVID-19 vaccines concerning occupation status and educational level.
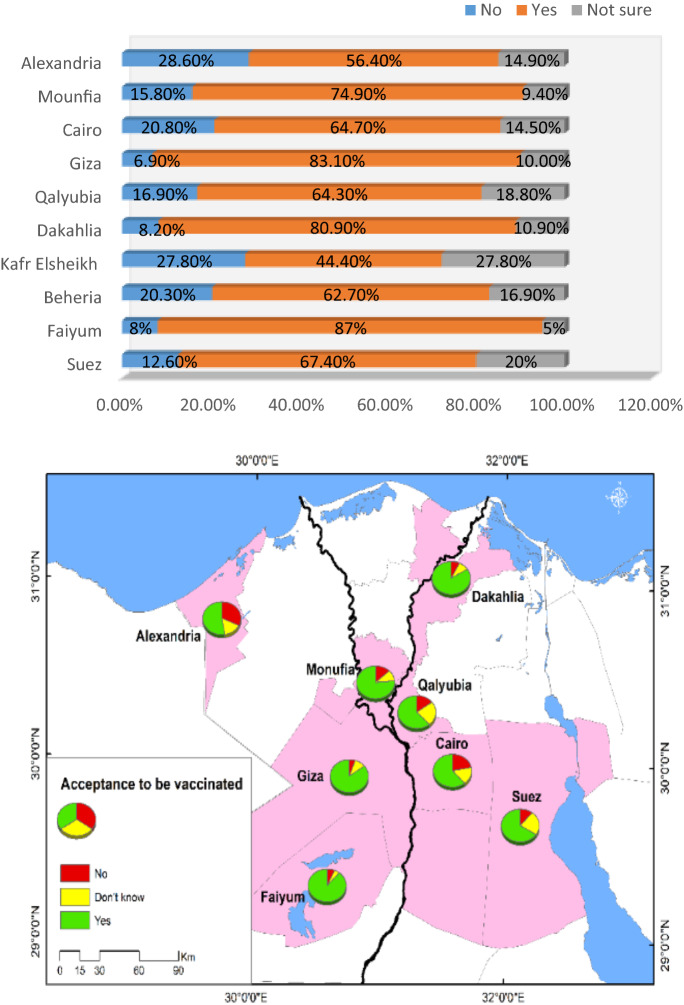
As regards geographical distribution, residents of Faiyum Governorate were the most accepting of COVID-19 vaccination (87%), while those from Kafr Elsheikh Governorate were the least (44.4%) (Fig. 3).
Figure 3.
Vaccine acceptance in different Egyptian governorates.
Table 2 illustrates the acceptability of COVID-19 vaccines among participants according to COVID-19 associated factors. Out of all participants, 373 (12.8%) reported a previous history of COVID-19 infection. Their contribution to the refusal rate was higher than that to the acceptance rate (16.4% vs. 11.4%; p = 0.004). Those who reported having more than five symptoms of COVID-19 infection were less accepting to be vaccinated than those with no one or two symptoms (p = 0.004). Almost two-thirds (66.4%) of those who accepted to receive the vaccine did not report a history of contact with COVID-19 patients compared to approximately half (50.8%) of those who refused (p = 0.000).
Table 2.
Relation between vaccine acceptance and COVID-19 associated factors (n = 2919).
| Willing to receive COVID-19 vaccine | P-value | ||||||
|---|---|---|---|---|---|---|---|
| No (refused) (n = 590) |
Yes (accept) (n = 1940) |
Not sure (hesitant) (n = 389) |
|||||
| No | % | No | % | No | % | ||
| Contact with COVID-19 patient | 0.000* | ||||||
| No | 300 | 50.8% | 1288 | 66.4% | 242 | 62.2% | |
| Yes | 290 | 49.2% | 652 | 33.6% | 147 | 37.8% | |
| History of COVID-19 infection | 0.004* | ||||||
| Never | 493 | 83.6% | 1719 | 88.6% | 334 | 85.9% | |
| Yes (once or more) | 97 | 16.4% | 221 | 11.4% | 55 | 14.1% | |
| Number of reported COVID symptoms | 0.004* | ||||||
| 0 | 172 | 29.2% | 690 | 35.6% | 142 | 36.5% | |
| 1–2 | 160 | 27.1% | 562 | 29.0% | 110 | 28.3% | |
| 3–4 | 121 | 20.5% | 369 | 19.0% | 71 | 18.3% | |
| 5+ | 137 | 23.2% | 319 | 16.4% | 66 | 17.0% | |
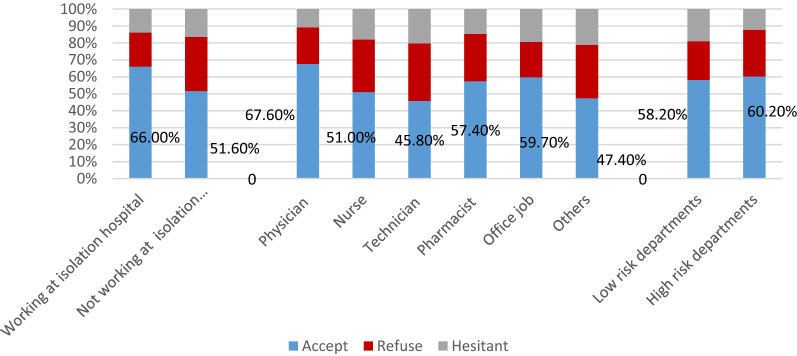
Among HCWs, the acceptance rate was 58.2%. Physicians were the most accepting group (67.6%), whereas technicians were the least (45.8%) (p = 0.062). Higher acceptability was among those working in COVID-19 isolation hospitals (66% vs 51.6%; p = 0.001), and at high-risk departments (60.2% vs 58.2%; p = 0.069) (Fig. 4).
Figure 4.
The acceptance of COVID-19 vaccines among HCWs according to job task, type of hospital and department.
Analysis of the predictors of vaccine acceptance among adults is shown in Table 3. Results of multivariate analysis showed that significant independent predictors of vaccine acceptance were being male (OR 1.362, 95% CI 1.082–1.714, p = 0.008), rural residents (OR 1.796, 95% CI 1.435–2.247, p = 0.000), lower education (below university) (OR 1.245, 95% CI 1.018–1.523, p = 0.033), not working (OR 2.101, 95% CI 1.344–3.284, p = 0.001), working in client facing jobs (OR 1.560, 95% CI 1.028–2.368, p = 0.037), and practicing exercise (OR 1.278, 95% CI 1.011–1.617, p = 0.041).
Table 3.
Predictors of vaccine acceptance among adult Egyptian participants (n = 2352).
| Crude OR (LL-UL) | P-value | Adjusted OR (LL-UL) | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 1.454 (1.221–1.732) | 0.000* | 1.362 (1.082–1.714) | .008* | ||||
| Female (Ref.) | ||||||||
| Age (years) | ||||||||
| 18–59 (Ref.) | ||||||||
| ≥ 60 | 1.603 (1.227–2.094) | 0.001* | 1.264 (0.930–1.717) | 0.134 | ||||
| Residence | ||||||||
| Urban (Ref.) | ||||||||
| Rural | 2.106 (1.712–2.592) | 0.000* | 1.796 (1.435–2.247) | 0.000* | ||||
| Crowding index | ||||||||
| < 1 (Ref.) | ||||||||
| 1- > 2 | 1.191 (1.002–1.416) | 0.047* | 1.130 (0.939–1.360) | 0.195 | ||||
| 2 + | 0.979 (0.577–1.660) | 0.937 | 0.955 (0.551–1.655) | 0.869 | ||||
| Educational level | ||||||||
| Below university level | 1.669 (1.407–1.980) | 0.000* | 1.245 (1.018–1.523) | 0.033* | ||||
| University graduate or above (Ref.) | ||||||||
| Marital status | ||||||||
| Not married (Ref.) | ||||||||
| Married | 1.202 (0.988–1.462) | 0.066 | 1.044 (0.847–1.289) | 0.685 | ||||
| Comorbidities** | ||||||||
| No comorbidities (Ref.) | ||||||||
| Any comorbidities | 1.172 (0.979–1.405) | 0.085 | 1.131 (0.930–1.375) | 0.217 | ||||
| Occupation | ||||||||
| Not working | 1.642 (1.090–2.472) | 0.018* | 2.101 (1.344–3.284) | 0.001* | ||||
| Client facing job*** | 1.108 (0.749–1.637) | 0.608 | 1.560 (1.028–2.368) | 0.037* | ||||
| Non-client facing job (Ref.) | ||||||||
| Smoking status | ||||||||
| No (Ref.) | ||||||||
| Yes | 1.586 (1.258–2.000) | 0.000* | 1.259 (0.948–1.673) | 0.112 | ||||
| Exercise | ||||||||
| No (Ref.) | ||||||||
| Yes | 1.166 (0.935–1.455) | 0.173 | 1.278 (1.011–1.617) | 0.041* | ||||
| History of COVID-19 infection | ||||||||
| Never | 1.312 (1.044–1.650) | 0.020* | 1.091 (0.852–1.397) | 0.490 | ||||
| Yes (Ref.) | ||||||||
| Contact with COVID-19 patient | ||||||||
| No | 1.494 (1.259–1.772) | 0.000* | 1.043 (0.844–1.289) | 0.698 | ||||
| Yes (Ref.) | ||||||||
| Applying (Practice) COVID protective measures*** | ||||||||
| Not done (0) | 1.253 (0.759–2.068) | 0.378 | 1.165 (0.689–1.968) | 0.569 | ||||
| Partially done(1–4) | 1.110 (0.687–1.795) | 0.669 | 1.010 (0.612–1.665) | 0.970 | ||||
| Completely done (5) (Ref.) | ||||||||
| History of travel abroad within the last six months | ||||||||
| No (Ref.) | ||||||||
| Yes | 1.826 (0.671–4.966) | 0.238 | 2.583 (0.916–7.282) | 0.073 | ||||
| BMI | ||||||||
| Normal (Ref.) | ||||||||
| Underweight | 0.525 (0.187–1.472) | 0.221 | 0.494 (0.166–1.470) | 0.205 | ||||
| Overweight/obese | 1.166 (0.947–1.436) | 0.149 | 1.173 (0.938–1.467) | 0.163 | ||||
**Chronic morbidities include cardiac diseases, hypertension, diabetes mellitus, chronic renal and liver diseases.
***HCWs were included in the client facing jobs.
****Wear mask, wash hand, use soap for hand wash, use disinfectant, social distancing [each variable was binary(yes/no)].
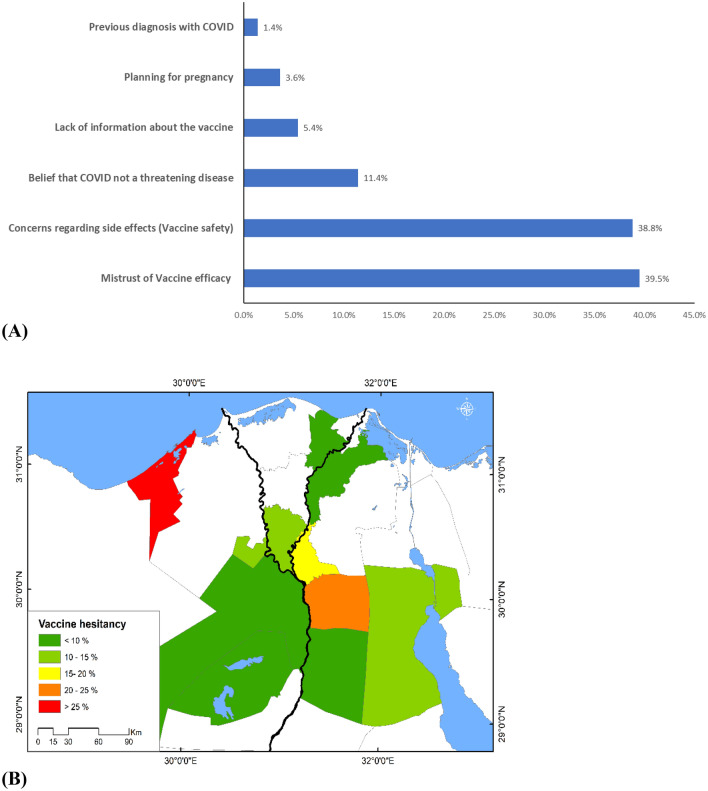
The commonest justifications of vaccine refusal were the mistrust of vaccine efficiency (39.5%), and concerns about the possible side effects (38.8%). In addition, a minority of participants argued that planning for pregnancy (3.6%) and previous diagnosis with COVID-19 infections (1.4%) were their causes of refusal (Fig. 5).
Figure 5.
(A) Causes of vaccine refusal (B) Proportion of individuals who refused to receive COVID-19 vaccination across different governorates.
Discussion
Egypt began its vaccination program in January 2021. Despite the tentative effectiveness and safety of the Chinese Sinopharm BIBP COVID-19 vaccine, the Egyptian Drug Authority (EDA), as in most Arab nations, had approved it for quarantine hospitals medical staff, followed by other medical teams, then high‐risk groups of the general population16. Hence, during this period, the vaccine acceptance rates might have been affected, where it reached only 8% among the general population6. As a part of the COVID‐19 Vaccines Global Access (COVAX) facility, a batch of Oxford/AstraZeneca (AZD1222) was obtained late in January 202117. By the end of 2021, 70 million doses of different types of vaccines were delivered by UNICEF18. The availability of this wide variety of vaccines with different techniques might help raise vaccine acceptance rates. From April–May (2021), Elgendey and Abdelrahim reported an 88% acceptance rate among the general population through an online survey19. A lower percentage was recorded in the present study (66.5%), which can be considered a more representative result as it was delivered by interview questionnaires which are known to minimize the bias associated with online surveys such as multiple responses from participants and inaccurate self-reported demographic or characteristics information as well as selection bias. The acceptance rate was comparable at the regional level to a study among Saudi participants (64.7%)20. Much lower acceptance rate (25%) was recorded through survey that included four Arab countries (Jordan, Saudi Arabia, Lebanon, and Iraq)21.
The extraordinary rapid development of COVID-19 vaccines had put pressure on HCWs to practice their advisory role and transmit confidence to the public, as they are the most trusted source of information on vaccination. Individuals whose physicians recommend vaccination were more likely to be vaccinated22. Unfortunately, lower acceptance rates among HCWs were encountered in the current study (58.2%). The result agreed with the pooled acceptance rate of COVID-19 vaccine among HCWs around the world (55%)23. This observation might be attributed to that, just as the case with the general population, HCWs may have some misinformation about the vaccines, and that they were not feeling well informed about the techniques of the new vaccines, which might have led to concerns and mistrust of vaccine safety. The hopeful prospects are that HCWs' acceptance rate was higher than previous Egyptian studies (21–26%)8,9 and that the assessment of the HCWs intention was during the period of vaccines development and testing. Moreover, doctors, whom the community might have faith in, had the highest acceptance rate among other categories of HCWs. Therefore, HCWs' stance towards vaccines might change as more information on how COVID-19 vaccines are developed and tested becomes available. It should be noted that higher pooled acceptance rate (78%) among HCWs in China was reported which was explained by the availability of comprehensive scientific evidence and tremendous information related to COVID-19 and COVID-19 vaccines at an unprecedented pace which drive HCWs to become more aware of safety and effectiveness of different vaccines24.
Evidence suggests the importance of building the trust of guardians in COVID‐19 vaccines to be able to achieve children vaccination. According to WHO, an increasing number of vaccines had been authorized for emergency use for adolescent age group (12–17 years old) in some countries (messenger RNA (mRNA) vaccines; Pfizer-BioNTech (BNT162b2) and Moderna mRNA-1273). In November 2021, Pfizer-BioNTech (BNT162b2) had been approved for use in children aged 5–11 years, and Egypt's government announced to use it for vaccinating 12–15 years old children25,26. Sinopharm COVID-19 BBIBP and Sinovac-CoronaVac had been tried in children as young as age 3 years and the Chinese authorities approved them for the age of 3–17 years. Both mRNA vaccines' efficacy, immunogenicity, and safety were similar or higher compared to adults. In October 2021, the Global Advisory Committee on Vaccine Safety (GACVS) concluded that in all age groups, the benefits of mRNA COVID-19 vaccines outweigh the risks. Outbreaks of COVID-19 infections had been identified in secondary schools, summer camps and day-care centres. Children usually have fewer and milder symptoms compared to adults; however, they shed the virus through the respiratory tract and faeces to older and more vulnerable individuals. In addition, the indirect impact related to school closures and disruption of the educational services mandates children's vaccination25.
Limited literature had explored guardians’ perception towards vaccination of their children. Th acceptance rates of guardians were 64.0%, 72.6%, and 92.9% in low and middle income countries27. In the present study, most guardians of children below 12 years and from 13 to 17 years had a positive attitude towards vaccination for their children (72.5% and 70.5%, respectively). These findings correspond well with a study conducted in The United Arab Emirates, where the acceptance of the respondents to vaccinate their children reached 75.1%28. Also, similar result was recorded in England where 48.2% of participants accepted, and 40.9% were unsure but leaning towards vaccinating their children29. Therefore, information on the safety of vaccines for children must be communicated clearly to alleviate guardians’ concerns.
Several studies had reported the previous history of COVID-19 infection as a determinant of vaccine acceptance30–32. On the contrary, in the current study, the refusal rate among those with previous infection was higher than acceptance rate (16.4% vs. 11.4%; p = 0.004). This may be explained by their belief in protection. This conclusion was also arrived at by Alqudeimat et al., from Kuwait, where a lower acceptance rate was observed in those who believed that natural protective immunity had developed after natural infection33.
Almost two-thirds (66.4%) of those who accepted to receive the vaccine did not report a history of contact with COVID-19 patients compared to approximately half (50.8%) of those who refused (66.4% vs. 50.8%; p = 0.000) indicating risk perception of contracting COVID-19 infection and their confidence in the immunity conferred by COVID-19 vaccines. Physicians, especially those working at high-risk departments, were more accepting vaccination. However, acceptability was not statistically associated with the frequency of exposure to suspected cases/day. On the contrary, Fares et al. from Egypt outlined that those directly dealing with COVID-19 patients had 3 times higher odds of vaccine acceptance8.
Certain demographic and social determinants of vaccine acceptance should be considered to prevent disparities in vaccine uptake. Prior findings correspond well with the present study, where males represented a higher percentage among the vaccine acceptance group compared to those who refused34,35, which may be attributed to females’ panic of unanticipated side effects of vaccines on menstruation, pregnancy, and future pregnancy generations. On the contrary, Mohamed et al. from Malaysia recorded a higher acceptance rate among females36. Similar to the present study, acceptance of vaccination was reported to increase with age, which may be due to associated disabilities in older age groups31,35; however, a conflicting finding among younger age groups was reported in the United States, which may be due to different perceptions and beliefs of populations across countries30.
Unemployed and retired participants reported higher COVID-19 vaccine acceptance rates. A contradicting observation was recorded by Alqudeimat et al., where the retired group was the least accepting group33. Lower acceptability of COVID-19 vaccine was recorded among those with a university education or higher (58.8%) than other education levels. Nevertheless, national public health strategies should target college students and young adults who can transmit the infection to elderly risky groups owing to the sense of invulnerability. On the other hand, Patwary et al. from Bangladesh delineated that the highest acceptance rate was among those with a bachelor’s degree37. It should be noted that the direct interview questionnaire used in the present study facilitated the assessment of vaccine acceptance among illiterates (74.5%) by more engagement of the respondents who are not familiar with internet use and a better understanding of the questions, which improves data quality. To the best of our knowledge, all previously published similar studies were carried out using online surveys, highlighting our study's importance. High acceptance rate among low educated may be attributed to that highly educated persons may have more concerns about vaccine safety and long-term adverse reactions. They may use social media to search information on COVID-19 vaccination which had a significant impact on spreading fear and panic of vaccination. This finding agreed with those reported by Jabessa and Bekele from Ethiopia where low education was associated with greater willingness to take the COVID-19 vaccine38.
Health-related variables, such as long-standing comorbidities were not statistically associated with vaccine acceptance. Despite the growing evidence that COVID-19 vaccines exhibit short-term vaccination efficacy among obese subjects compared to those with normal body weight39, in our study, acceptance rate among obese was slightly higher than their refusal which was in accordance with a study from Kuwait33. That might be attributed to their fear of more grave complications related to COVID-19 in case they get infected. On the other hand, a study in Canada showed that obese people were more ambivalent about COVID-19 vaccination40.
Misconception about the protective effect of smoking against COVID-19 infection might indicate that the vaccine offers little protection41. Several studies reported that current smokers were less likely to accept the COVID-19 vaccine33,37. In the current study, smokers constituted a higher proportion among the acceptance group compared to the refusal group.
In the current study, Upper Egypt governorates (Faiyum and Giza) were outpacing Lower Egypt governorates in vaccination acceptance rates. Nevertheless, the present study enrolled more urban residents (69.5%), a lagging-behind acceptance rate was encountered in urban residents (61.6% vs. 77.6%), which was in line with studies conducted by Omar and Hani and Elsayed et al. from Egypt7,42. The possible explanation is that, according to the Central Agency for Public Mobilization and Statistics (CAPMAS.), Upper Egypt governorates had the highest rates of illiteracy among Egyptian governorates, reaching 34% in Faiyum and 15.9% in Cairo and Giza. Individuals who obtained higher levels of education are more concerned about COVID-19 vaccine safety and potential side effects and have more tendency to refuse vaccination43.
Reluctance toward vaccination was associated with leading causes of refusal which had been delineated in previous studies, such as mistrust of vaccine safety due to ubiquity of negative and false information on vaccines on the internet, lack of information on different vaccines techniques, and possible side effects where reports of myocarditis and pericarditis were recorded in male adolescents and young adults after receiving Pfizer-BioNTech (BNT162b2) and Moderna mRNA-1273). In addition, reports of thrombosis and Guillain-Barré syndrome were recorded after Johnson & Johnson’s Janssen and Oxford/AstraZeneca COVID-19 vaccine (AZD1222)44,45.
Conclusion
High vaccine acceptance was reported among children's guardians and elderly compared to young adults. Lower acceptance rate among HCWs was recorded. Some predictors of vaccine acceptance were male gender, rural residence, illiteracy, negative history of COVID-19 infection or contact with COVID-19 patients. Being underweight had lower odds of vaccine acceptance compared to those with normal weight. Mistrust of vaccine safety and concerns about the possible side effects were the main causes of vaccine refusal. Direct interview questionnaire allowed assessing vaccine acceptance among illiterates and elderly.
Author contributions
Conceptualization, E.M.E.; Data curation, E.M.E., A.A., E.A.O., M.A.H.; Formal analysis, A.A., M.A.H.; Funding acquisition, E.M.E.; Investigation, E.M.E., A.A., N.F.A.E.-M.A., E.A.O.; Methodology, E.M.E.; Project administration, E.M.E., A.G.F.; Resources, E.M.E.; Supervision, E.M.E. and A.G.F.; Validation, A.G.F.; Visualization, E.A.O.; Writing—original draft, N.F.A.E.-M.A.; Writing—review & editing, E.M.E., E.A.O., A.G. F. All authors consented for publication.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This work was supported financially by the Science and Technology Development Fund (STDF), Egypt; Project No. 43834.
Data availability
The corresponding author would make the data available upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Muhajarine N, et al. COVID-19 vaccine hesitancy and refusal and associated factors in an adult population in Saskatchewan, Canada: Evidence from predictive modeling. PLoS ONE. 2021;16(11):e0259513. doi: 10.1371/journal.pone.0259513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Ten Threats to Global Health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. [Accessed 10 Jan 2021].
- 3.Thomson A, Robinson K, Vallee-Tourangeau G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34(8):1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 4.Moola S, et al. A rapid review of evidence on the determinants of and strategies for COVID-19 vaccine acceptance in low- and middle-income countries. J. Glob. Health. 2021;11:05027. doi: 10.7189/jogh.11.05027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malik A, Malik J, Ishaq U. Acceptance of COVID-19 vaccine in Pakistan among health care workers. PLoS ONE. 2021;16(9):e0257237. doi: 10.1371/journal.pone.0257237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qunaibi EA, Helmy M, Basheti I, Sultan I. A high rate of COVID-19 vaccine hesitancy in a large-scale survey on Arabs. eLife. 2021 doi: 10.7554/eLife.6803897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omar DI, Hani BM. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J. Infect. Public Health. 2021;14(10):1481–1488. doi: 10.1016/j.jiph.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 Vaccination perception and attitude among healthcare workers in Egypt. J. Prim. Care Community Health. 2021;12:21501327211013303. doi: 10.1177/21501327211013303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El-Sokkary RH, et al. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: A cross-sectional study. BMC Infect. Dis. 2021;21:762. doi: 10.1186/s12879-021-06392-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrade C. The limitations of online surveys. Indian J. Psychol. Med. 2020;42(6):575–576. doi: 10.1177/0253717620957496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Le CN, Nguyen UTT, Do DTH. Predictors of COVID-19 vaccine acceptability among health professions students in Vietnam. BMC Public Health. 2022;22(1):854. doi: 10.1186/s12889-022-13236-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dubov A, et al. Predictors of COVID-19 vaccine Acceptance and hesitancy among healthcare workers in Southern California: Not Just "Anti" vs "Pro" vaccine. Vaccines. 2021;9(12):1428. doi: 10.3390/vaccines9121428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazarus JV, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Ghitany EM, Farag S, Farghaly AG, Hashish MH, Hassaan MA, Omran EA. A pre-vaccine exploratory survey of SARS-CoV-2 humoral immunity among Egyptian general population. Trop. Med. Health. 2022;50(1):53. doi: 10.1186/s41182-022-00448-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ESRI. E. S. R. I. ArcGIS Desktop: Release 10. 8 (Environmental Systems Research Institute, 2020).
- 16.Cyranoski D. Arab nations first to approve Chinese COVID vaccine: Despite lack of public data. Nature. 2020;588:548. doi: 10.1038/d41586-020-03563-z. [DOI] [PubMed] [Google Scholar]
- 17.WHO (EMRO). News: Media centre. http://www.emro.who.int/media/news/glimmer-of-hope-covid-19-vaccines-roll-out-incountries-of-the-eastern-mediterranean-region.html. [Accessed on 18–1–2022].
- 18.A day at a Vaccine Center in New Cairo. https://www.unicef.org/egypt/stories/day-vaccine-center-new-cairo.
- 19.Elgendy MO, Abdelrahim MEA. Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. J. Med. Virol. 2021;93(12):6535–6543. doi: 10.1002/jmv.27199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Padhi BK, Almohaithef MA. Determinants of covid-19 vaccine acceptance in Saudi Arabia: A web-based national survey. J. Multidiscip. Healthc. 2020;13:1657–1663. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abu-Farha R, et al. Willingness of Middle Eastern public to receive COVID-19 vaccines. Saudi Pharm. J. 2021;29(7):734–739. doi: 10.1016/j.jsps.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu PJ, et al. Association of provider recommendation and offer and influenza vaccination among adults aged > =18 years—United States. Vaccine. 2018;36:890–898. doi: 10.1016/j.vaccine.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 23.Luo C, et al. Intention to COVID-19 vaccination and associated factors among health care workers: A systematic review and meta-analysis of cross-sectional studies. Am. J. Infect. Control. 2021;49(10):1295–1304. doi: 10.1016/j.ajic.2021.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shui X, Wang F, Li L, Liang Q. COVID-19 vaccine acceptance among healthcare workers in China: A systematic review and meta-analysis. PLoS ONE. 2022;17(8):e0273112. doi: 10.1371/journal.pone.0273112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization. Interim Statement on COVID-19 Vaccination for Children and Adolescents. https://www.who.int/news/item/24-11-2021-interim-statement-on-covid-19-vaccination-for-children-and-adolescents
- 26.Egypt to vaccinate 12–15 years old children against coronavirus: Cabinet https://english.ahram.org.eg/NewsContent/1/1236/443448/Egypt/Health/Egypt-to-vaccinate---years-old-children-against-co.aspx
- 27.Bono SA, et al. Adults' acceptance of COVID-19 vaccine for children in selected lower- and middle-income countries. Vaccines. 2021;10(1):11. doi: 10.3390/vaccines10010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.AlKetbi LMB, et al. Parents' views on the acceptability of a COVID-19 vaccine for their children: A cross-sectional study in Abu Dhabi-United Arab Emirates. Vaccine. 2022 doi: 10.1016/j.vaccine.2022.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine. 2020;38(49):7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reiter PL, Pennell ML, Katz ML. Acceptability of COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-COV-2 vaccine: A survey of U.S. adults. Ann. Intern. Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dror AA, et al. Vaccine hesitancy: The next challenge in the fight against covid-19. Eur. J. Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alqudeimat Y, et al. Acceptance of a COVID-19 Vaccine and its related determinants among the general adult population in Kuwait. Med. Princ. Pract. 2021;30(3):262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. E Clin. Med. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Che Isahak CI. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLoS ONE. 2021;16(8):e0256110. doi: 10.1371/journal.pone.0256110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patwary MM, et al. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the health belief model and the theory of planned behavior model. Vaccines. 2021;9:1393. doi: 10.3390/vaccines9121393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jabessa D, Bekele F. Willingness to receive the COVID-19 vaccine and associated factors among residents of Southwestern Ethiopia: A cross-sectional study. Patient Prefer. Adher. 2022;16:1177–1185. doi: 10.2147/PPA.S362264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Townsend MJ, Kyle TK, Stanford FC. COVID-19 vaccination and obesity: Optimism and challenges. Obesity. 2021;29:634–635. doi: 10.1002/oby.23131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vallis M, Glazer S. Protecting individuals living with overweight and obesity: Attitudes and concerns towards COVID-19 vaccination in Canada. Obesity. 2021;29:1128–1137. doi: 10.1002/oby.23182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jackson SE, Paul E, Brown J, Steptoe A, Fancourt D. Negative vaccine attitudes and intentions to vaccinate against Covid-19 in relation to smoking Status: A population survey of UK adults. Nicotine Tob. Res. 2021;23:1623–1628. doi: 10.1093/ntr/ntab039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elsayed M, et al. Factors influencing decision making regarding the acceptance of the COVID-19 vaccination in Egypt: A Cross-sectional study in an Urban, well-educated sample. Vaccines. 2022;10(1):20. doi: 10.3390/vaccines10010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.More than 25% of Egypt’s population ‘illiterate’ https://egyptianstreets.com/2014/09/09/more-than-25-of-egypts-population-illiterate/#
- 44.Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A. Myocarditis and pericarditis after vaccination for COVID-19. JAMA. 2021;326(12):1210–1212. doi: 10.1001/jama.2021.13443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagalli S, Shankar KN. Sub-acute onset of Guillain-Barré syndrome post-mRNA-1273 vaccination: A case report. SN Compr. Clin. Med. 2022;4(1):41. doi: 10.1007/s42399-022-01124-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The corresponding author would make the data available upon reasonable request.