Abstract
PURPOSE
The purpose of this study is to evaluate translucency and masking ability of translucent zirconia compared to conventional zirconia and lithium disilicate materials.
MATERIALS AND METHODS
Three types of zirconia blocks with different yttria contents (3Y, 4Y, 5.5Y) and LS blocks (Rosetta SM) were used. Ten specimens for each group were fabricated with 10 mm diameter, with both 0.8 mm and 1.5 mm thicknesses (± 0.02 mm). All groups of zirconia specimens were sintered and polished according to the manufacturer’s instructions. To calculate the translucency parameter (TP), CIELAB value was measured with a spectrophotometer on black and white backgrounds. To investigate the color masking abilities, background shades of A2, normal dentin, discolored dentin, and titanium were used. The color difference (ΔE) was calculated with the CIELAB values of A2 shade background as a reference compared with the values in the various backgrounds. One-way ANOVA and Bonferroni tests were conducted (P < .05).
RESULTS
The TP values of zirconia specimens increased as the yttria content increased. All materials used in the study were able to adequately mask normal dentin shade (ΔE < 5.5), but were incapable of masking severely discolored dentin (ΔE > 5.5). On the titanium background, all materials of 1.5 mm thickness were able to mask the background shade, but with a thickness of 0.8 mm, only 3Y-TZP and 4Y-PSZ were able to mask titanium background.
CONCLUSION
All zirconia materials and lithium disilicate specimens used in this study were unable to adequately mask the shade of severely discolored dentin. It is recommended to use 3Y-TZP or 4Y-PSZ with a sufficient thickness of 0.8 mm or more to mask titanium.
Keywords: Translucent zirconia, Masking ability, Translucency parameters, Conventional zirconia
INTRODUCTION
Zirconia has been used in the dental field for more than 15 years owing to its excellent esthetics, high corrosion resistance, biocompatibility and low thermal conductivity.1,2,3 The optical properties of zirconia are affected by chemical composition, microstructural defects, phase distribution and crystal size. Although they have been continuously advancing since its introduction, their optical properties still have space for improvement.4
Tetragonal partially stabilized zirconia containing 3 mol% yttria (3Y-TZP) is also known as conventional zirconia or 1st generation zirconia.5 Because of its high refractive index and small crystal structure, which causes a lot of light scattering at the grain boundaries, it is considered to be opaque. To achieve aesthetic outcomes of restoration, the optical properties of dental materials need to be similar to the enamel translucency of the natural teeth. In order to increase the translucency of zirconia, various sintering conditions were experimented, and the number and size of alumina particles were reduced and repositioned in the zirconia structure. This has led to the development of 2nd generation zirconia with higher light transmittance and higher strength.6,7 However, even with improved qualities, it still lacked translucency compared to glass ceramics. For more translucency, 3rd generation zirconia (cubic/tetragonal fully stabilized zirconia) with cubic phase of 53% was developed by increasing yttria content to 5 mol% (9.3 wt %). With the development of 3rd generation translucent zirconia, it became possible to use monolithic zirconia restorations in esthetic areas.1 However, contrary to the boost in optical properties, some mechanical properties were compromised due to the alteration of contents. It is reported that the fracture strength is lower than that of conventional zirconia materials.8 To overcome this shortcoming, translucent zirconia without a significant decrease in strength have been introduced recently, satisfying the needs of the clinicians and patients.9
There are certain circumstances, in which the improved translucency may act as a disadvantage, such as in the cases of discolored teeth, metallic cores, and implant titanium abutments. In such cases, the dark color of the substructure may affect the color of the translucent final prostheses, and clinicians are required to select appropriate materials capable of masking the substructure.10,11 The color of dental ceramics differs with their backgrounds’ masking ability, and therefore evaluating the degree of translucency is an important factor of color measurement and aesthetics. Ceramic translucency is usually evaluated with translucency parameter (TP). The TP is defined as the color difference (ΔE) between a uniform thickness of a material over a white and a black background. Higher TP value means the material is opaquer.12
Since the development of the 3rd generation zirconia, there have been many studies investigating the mechanical and optical properties of conventional zirconia and translucent zirconia.13,14,15,16,17,18 However, few studies have investigated the optical effect and translucency of yttria content in translucent zirconia along with its masking ability in various backgrounds such as discolored teeth and implant titanium abutments. Most of previous studies conducted experiments at a single thickness in order to compare the difference in the translucency of the materials themselves; usually between the most commonly used translucent zirconia 5Y-PSZ with conventional zirconia 3Y-TZP.15,19 In addition, there are only few studies involving relatively recently introduced 4Y-PSZ or measuring the degree of translucency and masking ability in various thickness of the material considering clinical situations of cervical and incisal areas.
The purpose of this study is to compare the translucency of conventional zirconia (3Y-TZP), two translucent zirconia (4Y-PSZ, 5.5Y-PSZ) and lithium disilicate (LS) materials at two thicknesses (0.8 and 1.5 mm), and to compare the masking ability of these materials on various backgrounds such as normal dentin, discolored dentin, and implant titanium abutment. The null hypotheses of this study are as the following: first, there are no differences in translucency among the tested materials. Second, there are no significant differences in masking ability of these materials when placed on various background and material types.
MATERIALS AND METHODS
Monolithic CAD-CAM ceramic materials, including 3 different types of zirconia with different yttria contents from one manufacturer (Rainbow Shade Block A2: 3Y-TZP, Rainbow Shine T Block A2: 4Y-PSZ, Rainbow High Shine Block A2:5.5Y-PSZ; Genoss, Suwon, Gyeonggi-do, Korea), and a lithium disilicate block (Rosetta SM® A2; HASS Corp, Gangneung, Korea) were tested in 2 thicknesses (n = 10 for each thickness tested). Disk-shaped test specimens with a diameter of 10 mm, and thickness of 0.8 mm and 1.5 mm were fabricated. 0.8 mm represents cervical thickness and 1.5 mm represents the thickness of the middle and incisal part of the crown (Table 1).20
Table 1. Materials used in this study.
| Materials | Composition (wt%) (Phase ratio) | ||
|---|---|---|---|
| Zirconia | |||
| 3Y-TZP | Rainbow Shade | ZrO2 83-96%, Y2O3 4-7%, HfO2 ≤ 5%, Al2O3 ≤ 1%, Other oxides (80% tetragonal, 20% cubic phase) | |
| 4Y-PSZ | Rainbow Shine T | ZrO2 81-94%, Y2O3 6-9%, HfO2 ≤ 5%, Al2O3 ≤ 1%, Other oxides (50% tetragonal, 50% cubic phase) | |
| 5.5Y-PSZ | Rainbow High Shine | ZrO2 79-92%, Y2O3 8-11%, HfO2 ≤ 5%, Al2O3 ≤ 1%, Other oxides (35% tetragonal, 65% cubic phase) | |
| Lithium disilicate | |||
| LS | Rosetta SM | SiO2 ≤ 85%, Li2O ≤ 13%, Other oxides | |
3Y-TZP (3 mol% yttria tetragonal zirconia polycrystals), 4Y-PSZ (4 mol% yttria partially stabilized zirconia), 5.5Y-PSZ (5.5 mol% yttria partially stabilized zirconia), LS (lithium disilicate).
The zirconia specimens were designed with a CAD software (Meshmixer; Autodesk Inc., San Rafael, CA, USA) and fabricated with a milling system (IDC MIKRO 5X; Evolve Dentistry, UK). The specimens were sintered according to the manufacturer’s instructions. Zirconia specimens were polished on one side by a single operator using a lab handpiece (STRONG 102L; Saeshin, Daegu, Korea) with an adjustment/polishing kit (Luster; Meisinger, Centennial, CO, USA) at a constant speed of 10,000 rpm following manufacturer’s instructions. The intended thicknesses (± 0.02 mm) were confirmed with a digital caliper (0604CAL6++ LDC Digital Caliper; Electronix Express, Rahway, NJ, USA). Lithium disilicate specimens were fabricated using the Cerec system (Cerec inLab MC XL; Dentsply Sirona, York, PA, USA) and polished with a polishing kit (Luster; Meisinger, Centennial, CO, USA) to obtain the planned thickness (0.8 ± 0.02 mm, 1.5 ± 0.02 mm). All specimens were not glazed in this experiment.
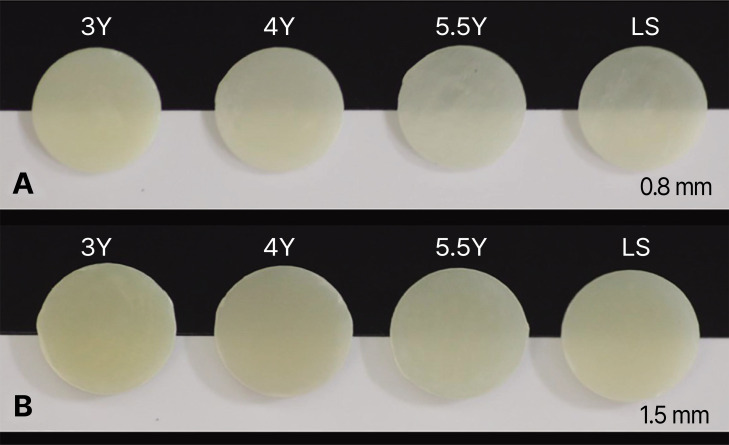
For translucency evaluation, color measurement was conducted by one examiner with a handy spectrophotometer (SpectroShade Micro; MHT Optic Research AG, Niederhasli, Switzerland) equipped with a digital camera connected to LED illuminants. Two polarized, telecentric, monochromatic (λ = 410-680 nm) illuminants are placed in two sides at a 45° angle of the camera. Color measurements were conducted under the same condition to avoid errors that can affect the measured value.21 To exclude external light, a polyvinyl siloxane putty material (Silagum putty soft; DMG, Hamburg, Germany) was molded to the spectrophotometer and acted as a jig for the specimens. No external light interfered in the measurement. The Commission Internationale de I’Eclairage (CIELAB) values of the specimens were measured on black and white backgrounds (Fig. 1).
Fig. 1. Specimens of zirconias and lithium disilicate on black and white backgrounds. (A) 0.8 mm thickness specimens, (B) 1.5 mm thickness specimens. 3Y (3 mol% yttria tetragonal zirconia polycrystals), 4Y (4 mol% yttria partially stabilized zirconia), 5.5Y (5.5 mol% yttria partially stabilized zirconia), LS (lithium disilicate).
Translucencies of zirconia and lithium disilicate blocks were evaluated by calculating translucency parameters. TP value is interpreted as the color difference between the same specimens in contact with black and white background. They were calculated from the following formula:22
| TP = [(L*B - L*W)2 + (a*B - a*W)2 + (b*B - b*W)2]1/2. |
L*: brightness, a*: redness to greenness, b*: yellowness to blueness, B: black background, W: white background.
For masking ability test, A2 shade composite resin specimen (FiltekZ350 A2 Dentin; 3M ESPE, St. Paul, MN, USA) was used as a reference background. Two different shades (ND3 and ND9) of tooth-colored resin substrates (IPS Natural Die Material; Ivoclar Vivadent, Schaan, Liechtenstein) were used to imitate standard dentin (ND3) and severely discolored dentin (ND9).23 They were prepared to be 10 mm in diameter and 5 mm thick by using putty molds.
A titanium background disk with a diameter of 10 mm and a height of 5 mm was designed using a CAD software (Meshmixer; Autodesk Inc., San Rafael, CA, USA), and Ti-6Al-4V alloy was milled with a milling machine (XD-20H; Hanwha, Seoul, Korea). The same digital caliper was used to confirm the thickness of background materials (5.0 ± 0.02 mm).
Color measurement was performed in the same manner as in the translucency test. The ceramic specimens were placed on the background without any intermediate. To examine the masking abilities of zirconia blocks and lithium disilicate blocks, CIELAB values were measured on all four backgrounds. The A2 shade background was selected as the reference.
Masking ability was evaluated by the color difference (ΔE) between the specimens on the A2 shade background and the same specimen on the other backgrounds. ΔE values were calculated using the following formula11:
| ΔE*ab = [(L*2 - L*1)2 + (a*2 - a*1)2 + (b*2 - b*1)2]1/2 |
The ΔE values were compared with the acceptability (ΔE = 5.5) and perceptibility thresholds (ΔE = 2.6), and the masking abilities were assessed.24
Statistical analysis of the data was conducted using a statistical software (IBM SPSS Statistics v25; IBM Corp., Armonk, NY, USA). Normal distribution of each TP value and ΔE value was verified with Shapiro-Wilk test and Q-Q plot. One-way ANOVA and Bonferroni methods were used to compare the TP values of different materials with the same thicknesses. To evaluate the statistical difference of masking ability of the tested materials, ΔE values were analyzed using one-way ANOVA and Bonferroni post hoc tests conducted for multiple pairwise comparison. The level of significance is set at 0.05.
RESULTS
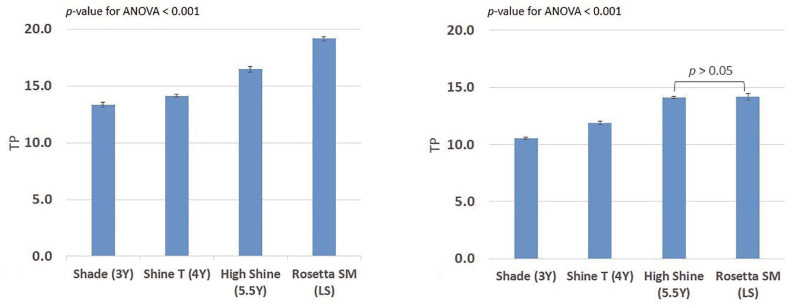
The means and standard deviations of TP values are shown in Table 2. For the 0.8 mm thickness groups, statistically significant differences were observed among the TP values of various ceramic materials (P < .001). Multiple pairwise tests showed that the mean TP values of all materials were significantly different from each other. High Shine (5.5Y-PSZ) was significantly more translucent than Shine T (4Y-PSZ). Shade (3Y-TZP) was less translucent than the two translucent zirconia blocks (4Y-PSZ and 5.5Y-PSZ) and Rosetta SM (LS) was significantly more translucent than all the zirconia blocks (P < .001).
Table 2. Average translucency parameter(TP) values and standard deviations for each specimen.
| Zirconia | Lithium disilicate | |||
|---|---|---|---|---|
| Thickness (mm) | Shade (3Y) | Shine T (4Y) | High Shine (5.5Y) | Rosetta SM (LS) |
| 0.8 | 13.32 ± 0.32 a | 14.12 ± 0.18 b | 16.47 ± 0.39 c | 19.17 ± 0.29 d |
| 1.5 | 10.55 ± 0.14 a | 11.89 ± 0.26 b | 14.13 ± 0.12 c | 14.20 ± 0.32 c |
*Letters a,b,c,d mean statistically significant differences between groups (P < .05 ).
**3Y (3 mol% yttria tetragonal zirconia polycrystals), 4Y (4 mol% yttria partially stabilized zirconia), 5.5Y (5.5 mol% yttria partially stabilized zirconia), LS (lithium disilicate)
There were also significantly different TP values for the 1.5 mm thickness groups. The multiple pairwise comparison test indicated that while High Shine and Rosetta SM were not significantly different, they both were more translucent than Shine T and Shade. With higher yttria contents, the average TP values were higher for both 0.8 mm and 1.5 mm thickness groups (Fig. 2).
Fig. 2. Graphs showing the mean translucency parameter (TP) values. (A) 0.8 mm thickness specimens, (B) 1.5 mm thickness specimens.
3Y (3 mol% yttria tetragonal zirconia polycrystals), 4Y (4 mol% yttria partially stabilized zirconia), 5.5Y (5.5 mol% yttria partially stabilized zirconia), LS (lithium disilicate).
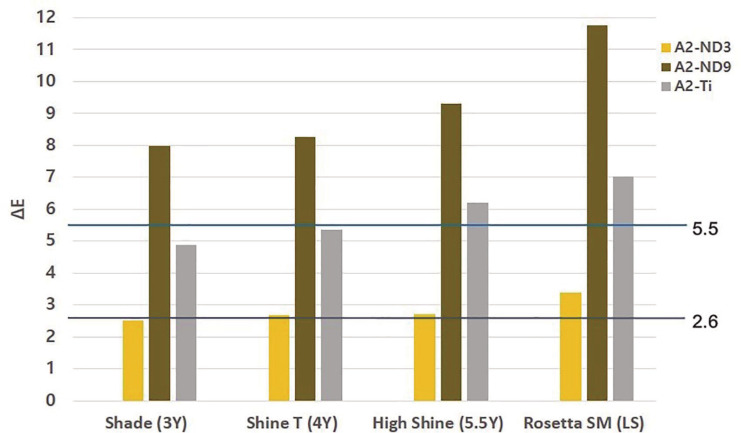
The means and standard deviations of ΔE values for each background are shown in Table 3. For the 0.8 mm thickness groups, the ΔE values did not show statistical differences among zirconia blocks on ND3 background. On the ND9 background, the ΔE value showed differences among all groups except between Shade and Shine T. Significant differences were observed among groups on the titanium background. Overall, in zirconia groups, the ΔE value increased with the yttria content. The highest ΔE value was observed in Rosetta SM. Figure 3. shows the mean ΔE values of each materials and the acceptability and perceptibility thresholds. In all specimens, the mean ΔE values were smaller than the acceptability threshold (ΔE = 5.5) on ND3 and significantly higher than the acceptability threshold on ND9. On the titanium background, the ΔE value of 3Y-TZP and 4Y-PSZ were smaller than 5.5, but the ΔE values of 5.5Y-PSZ and LS were larger than 5.5.
Table 3. Mean ΔE values and standard deviations for each specimen.
| Zirconia | Lithium disilicate | |||||
|---|---|---|---|---|---|---|
| Background | Thickness (mm) | Shade (3Y) | Shine T (4Y) | High shine (5.5Y) | Rosetta SM (LS) | P-value for ANOVA |
| ND3 | 0.8 | 2.52 ± 0.14 a | 2.68 ± 0.12 a | 2.72 ± 0.31 a | 3.39 ± 0.25 b | < .001 |
| ND9 | 0.8 | 7.98 ± 0.06 a | 8.25 ± 0.32 a | 9.28 ± 0.32 b | 11.75 ± 0.28 c | < .001 |
| Ti | 0.8 | 4.88 ± 0.11 a | 5.36 ± 0.11 b | 6.21 ± 0.26 c | 7.01 ± 0.29 d | < .001 |
| ND3 | 1.5 | 2.37 ± 0.41 a | 2.61 ± 0.21 a | 2.69 ± 0.25 a | 2.36 ± 0.14 a | .02 |
| ND9 | 1.5 | 6.05 ± 0.36 a | 6.57 ± 0.29 b | 7.61 ± 0.17 c | 7.9 ± 0.31 c | < .001 |
| Ti | 1.5 | 4.09 ± 0.64 a | 4.33 ± 0.29 a | 5.11 ± 0.18 b | 4.71 ± 0.14 b | < .001 |
*Under the same conditions, the same superscription indicates that there is no statistical difference in the mean value (P > .05).
**Letters a,b,c,d mean statistically significant differences between groups (P < .05).
***3Y (3 mol% yttria tetragonal zirconia polycrystals), 4Y (4 mol% yttria partially stabilized zirconia), 5.5Y (5.5 mol% yttria partially stabilized zirconia), LS (lithium disilicate).
****ND3 and ND9 of tooth-colored resin substrates to imitate standard dentin (ND3) and severely discolored dentin (ND9), Ti (milled Ti-6Al-4V alloy to imitate titanium abutment).
Fig. 3. The mean ΔE values of 0.8 mm specimens on each backgrounds. Acceptability threshold (5.5) and perceptibility threshold (2.6) are shown on the graph.
ΔE - color difference between the specimens on the A2 shade background and the same specimen on the other backgrounds.
3Y (3 mol% yttria tetragonal zirconia polycrystals), 4Y (4 mol% yttria partially stabilized zirconia), 5.5Y (5.5 mol% yttria partially stabilized zirconia), LS (lithium disilicate).
A2 - A2 shade composite resin , ND3 and ND9-tooth-colored resin substrates to imitate standard dentin (ND3) and severely discolored dentin (ND9), Ti -milled Ti-6Al-4V alloy to imitate titanium abutment.
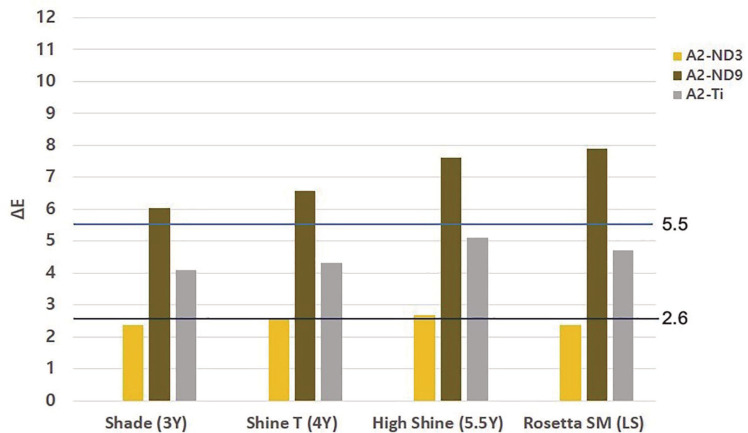
For the 1.5 mm thickness groups, there were no significant differences among all groups on the ND3. On the ND9, the ΔE value increased with increasing yttria content, while High Shine and Rosetta SM showed similar values. In the titanium background, the mean ΔE values of Shade and Shine T were similar, and High Shine and Rosetta SM were similar. As with the results in the 0.8 mm specimens, the ΔE value increased as the yttria content of the zirconia block increased. The mean ΔE values of 1.5 mm specimens are compared with the acceptability and perceptibility thresholds as shown in Figure 4. In all specimens, the mean ΔE values were less than the acceptability threshold (ΔE = 5.5) in ND3 and titanium backgrounds, while they were greater than 5.5 in ND9.
Fig. 4. The mean ΔE values of 1.5 mm specimens on each backgrounds. Acceptability threshold (5.5) and perceptibility threshold (2.6) are shown on the graph.
DISCUSSION
In this study, the difference in translucency among conventional zirconia, translucent cubic phase-containing zirconia, and lithium disilicate were compared. Also, the masking ability of each material was compared by color differences in various background materials. The null hypotheses were rejected because there were differences in translucency and masking abilities among tested materials.
In conventional zirconia, 3 mol% yttria was added to stabilize the tetragonal phase of zirconia crystals at room temperature. These stabilizing dopants stabilize the tetragonal and cubic phases at room temperature, and the amount of dopant can be adjusted to make partially or fully stabilized zirconia.18 When the yttria content is increased from 3 to 5 mol%, the translucency can be increased by increasing the cubic phase proportion.25 Zhang26 stated that Y-TZP containing 5.18 wt% (3 mol%) yttria contains more than 90% tetragonal phase, and to produce translucent zirconia, the yttria concentration should be increased to 7 wt% (4 mol%) or higher. The newly developed translucent zirconia 5Y-PSZ contains 5 mol% yttria and is predominantly occupied by cubic phase (>50%).27 The size of cubic crystals is larger than tetragonal crystals, which makes light scatter less at the grain boundaries. In addition, it is more isotropic, which leads to light spreading more uniformly. The translucent zirconia blocks (4Y-PSZ, 5.5Y-PSZ) used in this study also has increased the yttria content for improved translucency and showed improved results compared to the conventional zirconia (3Y-TZP).
There are previous studies comparing the translucency of conventional zirconia and translucent zirconia with higher yttria contents. Kwon et al.15 reported that 1 mm thick Katana UTML (5Y-PSZ) has a higher TP value than Katana HT (3Y-TZP), and Zhang et al.19 reported that 0.5 mm thick Zpex Smile (5Y-PSZ) shows a higher TP value than Zpex (3Y-TZP). In this study, the TP value was higher in zirconia with increased yttria contents, which is in agreement with previous studies. When comparing 5.5Y-PSZ and LS, LS showed significantly higher TP value in 0.8 mm but did not show statistically significant difference in 1.5 mm. In all ceramics, the translucency increases as thickness decreases, but the amount of change in value varies.28 In the case of LS, it is expected that the degree of translucency becomes greater as the thickness decreases compared to 5.5-PSZ.
In the study by Yan et al.29 using 1 mm thick specimens, Zpex Smile (5Y-PSZ) showed lower TP values than IPS e.max CAD (LS), but showed higher TP value compared to Zpex (3Y-TZP) and Zpex 4 (4Y-PSZ). In Yan’s study, there was no significant difference in the TP values of 3Y-TZP and 4Y-PSZ, but in this study, the TP value of 4Y-PSZ was significantly higher than that of 3Y-TZP. Further research would be needed to find out whether 4Y-PSZ has sufficiently improved translucency compared to conventional zirconia.
Yu et al.30 reported that the TP value of 1 mm-thick human dentin was 16.4 and that of enamel is 18.1, which is similar to that of glass ceramics (14.9-19.6). In this study, the mean TP value of 0.8 mm-thick specimens were 14.12 for 4Y-PSZ and 16.47 for 5.5-PSZ, indicating that they are less translucent than that of 1 mm-thick dentin or enamel. Therefore, even with improved optical properties of zirconia, in order to reproduce translucent nature of teeth, more improvement is necessary.
In the second part of the study, masking ability of each specimen was compared. To achieve ideal masking, the minimum thickness of zirconia depends on the background. According to the manufacturer, for monolithic zirconia crowns, a thickness of 0.8 mm or more in the cervical region and 1.5 mm or more in the incisal area is required.31 For lithium disilicate materials, it is possible to use a minimum of 0.4 mm thickness for a veneer, but it is recommended to use a thickness of at least 1.0 mm for a crown. Therefore, in this study, 0.8 mm represents the cervical thickness while 1.5 mm represents the incisal and middle thickness of crown restorations. All test specimens were made in A2 shade, and the CIELAB values measured on the A2 background were used as a reference to calculate the color change due to various backgrounds. In order to reproduce clinical situations, normal sound dentin without any discolorations, discolored teeth due to root canal treatment or medications, and titanium, which is most often used as an implant abutment, were selected as the backgrounds. In this study, to evaluate masking abilities of each materials, thresholds for acceptability (ΔE = 5.5) and perceptibility (ΔE = 2.6) were assumed.24 All specimens could effectively mask normal dentin shade but could not mask severely discolored dentin shade (ΔE > 5.5). In the clinical situation, the degree and area of discoloration in one tooth are varied.32 The ND9 shade used in this study represents severe discoloration, and if the discoloration is less severe than this, the use of zirconia material may be considered. The use of materials other than tested would be recommended to mask severe discoloration equal or superior to ND9.
In 5.5Y-PSZ, the ΔE value of 0.8 mm thickness groups exceeded the acceptability threshold value when placed on the titanium background, while it was smaller than the acceptability threshold value in the 1.5 mm-thick groups. Therefore, it is recommended to use 3Y-TZP or 4Y-PSZ on a titanium background and 5.5Y-PSZ should only be used with sufficient thickness at cervical area to mask titanium. This recommendation should be applied with some caution because in this study, all zirconia specimens were fabricated from zirconia blocks of single manufacturer. Sulaiman et al.33 reported that there was a statistically significant difference when comparing translucency between the brands.
As a result of this study, there should be no problem in reproducing the desired color with all materials on normal dentin, but additional considerations may be required for titanium abutments and discolored teeth. When fabricating a prosthesis with translucent zirconia on the titanium substrate, it is necessary to form a deep chamfer margin much thicker than 0.8 mm to obtain an appropriate masking effect. It is also necessary to select an appropriate material according to the degree of discoloration of the teeth and to plan proper margin thickness in order to effectively mask discolored teeth.
While highly translucent zirconia, containing a large amount of cubic phase, has improved optical properties, it has decreased flexural strength.15 The zirconia used in these studies, according to the manufacturer, have flexural strength values of 1100 - 1200 Mpa for 3Y-TZP and 4Y-PSZ, 800 MPa for 5-5Y-TZP, and 440 MPa for LS. According to ISO 6872,34 dental ceramic materials can be used for single-unit anterior or posterior prostheses and anterior three-unit prostheses when the flexural strength is 500 MPa or higher, and can be used for fixed partial dentures with four or more units when their flexural strength is 800 MPa or higher. Therefore, it could be concluded that 5.5Y-PSZ used in this study can be successfully used up to a 3-unit prosthesis in the anterior region, while it is recommended to use 4Y-PSZ or 3Y-TZP for long span restorations.
There are some limitations of this in vitro study as it may differ somewhat from the clinical situation. The CIELAB value was measured using a disk-shaped specimen and not in a crown shape. The shade of background materials may be different from that of natural teeth, which can potentially act as a different background due to its translucent and opalescent characteristics and which varies from patient to patient. In the case of discolored teeth, the degree and area of discoloration are also various, making it difficult to define them as one color. Another limitation of this study is that CIELAB formula is used to evaluate the color difference. CIELAB formula is simple and acceptable method to draw the conclusion that translucency and masking ability is affected by the yttria content of zirconia.35 However, since CIEDE2000 (ΔE00) is currently recommended by the Commission Internationale de l’Éclairage (CIE), this formula needs to be considered in further studies. In addition, although external light was excluded in the experiment, various factors affecting optical properties of zirconia, such as metamerism in different light sources, glazing, type of cement, thickness of cement, the effect of moisture in the mouth and soft tissue, were not considered. Further research is needed to supplement these limitations.
CONCLUSION
Within the limitations of this study, the following conclusions can be drawn: in both 0.8 mm and 1.5 mm thick zirconia specimens, the TP value increased significantly as the yttria content increased from 3 mol% to 4 mol% and 5.5 mol%. All zirconia and lithium disilicate specimens tested could not perfectly mask ND9 shade regardless of its thickness. 0.8 mm thickness specimens of 5.5Y-PSZ and lithium disilicate could not mask titanium shade, but 1.5 mm thickness was sufficient to mask titanium shade for all materials tested. It is recommended to use 3Y-TZP or 4Y-PSZ which contains lower yttria content with a thickness above 0.8 mm to mask titanium.
References
- 1.Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int. 2017;48:369–380. doi: 10.3290/j.qi.a38057. [DOI] [PubMed] [Google Scholar]
- 2.Christensen GJ. Choosing an all-ceramic restorative material: porcelain-fused-to-metal or zirconia-based? J Am Dent Assoc. 2007;138:662–665. doi: 10.14219/jada.archive.2007.0239. [DOI] [PubMed] [Google Scholar]
- 3.Vagkopoulou T, Koutayas SO, Koidis P, Strub JR. Zirconia in dentistry: Part 1. Discovering the nature of an upcoming bioceramic. Eur J Esthet Dent. 2009;4:130–151. [PubMed] [Google Scholar]
- 4.Shahmiri R, Standard OC, Hart JN, Sorrell CC. Optical properties of zirconia ceramics for esthetic dental restorations: A systematic review. J Prosthet Dent. 2018;119:36–46. doi: 10.1016/j.prosdent.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008;24:299–307. doi: 10.1016/j.dental.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Stawarczyk B, Frevert K, Ender A, Roos M, Sener B, Wimmer T. Comparison of four monolithic zirconia materials with conventional ones: Contrast ratio, grain size, four-point flexural strength and two-body wear. J Mech Behav Biomed Mater. 2016;59:128–138. doi: 10.1016/j.jmbbm.2015.11.040. [DOI] [PubMed] [Google Scholar]
- 7.Stawarczyk B, Emslander A, Roos M, Sener B, Noack F, Keul C. Zirconia ceramics, their contrast ratio and grain size depending on sintering parameters. Dent Mater J. 2014;33:591–598. doi: 10.4012/dmj.2014-056. [DOI] [PubMed] [Google Scholar]
- 8.Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Three generations of zirconia: From veneered to monolithic. Part II. Quintessence Int. 2017;48:441–450. doi: 10.3290/j.qi.a38157. [DOI] [PubMed] [Google Scholar]
- 9.Church TD, Jessup JP, Guillory VL, Vandewalle KS. Translucency and strength of high-translucency monolithic zirconium oxide materials. Gen Dent. 2017;65:48–52. [PubMed] [Google Scholar]
- 10.Suputtamongkol K, Tulapornchai C, Mamani J, Kamchatphai W, Thongpun N. Effect of the shades of background substructures on the overall color of zirconia-based all-ceramic crowns. J Adv Prosthodont. 2013;5:319–325. doi: 10.4047/jap.2013.5.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vichi A, Louca C, Corciolani G, Ferrari M. Color related to ceramic and zirconia restorations: a review. Dent Mater. 2011;27:97–108. doi: 10.1016/j.dental.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 12.Della Bona A, Nogueira AD, Pecho OE. Optical properties of CAD-CAM ceramic systems. J Dent. 2014;42:1202–1209. doi: 10.1016/j.jdent.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Bayindir F, Koseoglu M. The effect of restoration thickness and resin cement shade on the color and translucency of a high-translucency monolithic zirconia. J Prosthet Dent. 2020;123:149–154. doi: 10.1016/j.prosdent.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Huh YH, Yang EC, Park CJ, Cho LR. In vitro evaluation of the polishing effect and optical properties of monolithic zirconia. J Prosthet Dent. 2018;119:994–999. doi: 10.1016/j.prosdent.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 15.Kwon SJ, Lawson NC, McLaren EE, Nejat AH, Burgess JO. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018;120:132–137. doi: 10.1016/j.prosdent.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Elsayed A, Meyer G, Wille S, Kern M. Influence of the yttrium content on the fracture strength of monolithic zirconia crowns after artificial aging. Quintessence Int. 2019;50:344–348. doi: 10.3290/j.qi.a42097. [DOI] [PubMed] [Google Scholar]
- 17.Carrabba M, Keeling AJ, Aziz A, Vichi A, Fabian Fonzar R, Wood D, Ferrari M. Translucent zirconia in the ceramic scenario for monolithic restorations: A flexural strength and translucency comparison test. J Dent. 2017;60:70–76. doi: 10.1016/j.jdent.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Patel N. Effect of Different Implant Abutment Materials on Optical Properties of Translucent Monolithic Zirconia Crowns. Marquette University; Master of Science (MS); 2019. [Google Scholar]
- 19.Zhang F, Inokoshi M, Batuk M, Hadermann J, Naert I, Van Meerbeek B, Vleugels J. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater. 2016;32:e327–e337. doi: 10.1016/j.dental.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 20.Arif R, Yilmaz B, Johnston WM. In vitro color stainability and relative translucency of CAD-CAM restorative materials used for laminate veneers and complete crowns. J Prosthet Dent. 2019;122:160–166. doi: 10.1016/j.prosdent.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Lee YK. Criteria for clinical translucency evaluation of direct esthetic restorative materials. Restor Dent Endod. 2016;41:159–166. doi: 10.5395/rde.2016.41.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnston WM, Ma T, Kienle BH. Translucency parameter of colorants for maxillofacial prostheses. Int J Prosthodont. 1995;8:79–86. [PubMed] [Google Scholar]
- 23.Chaiyabutr Y, Kois JC, Lebeau D, Nunokawa G. Effect of abutment tooth color, cement color, and ceramic thickness on the resulting optical color of a CAD/CAM glass-ceramic lithium disilicate-reinforced crown. J Prosthet Dent. 2011;105:83–90. doi: 10.1016/S0022-3913(11)60004-8. [DOI] [PubMed] [Google Scholar]
- 24.Douglas RD, Steinhauer TJ, Wee AG. Intraoral determination of the tolerance of dentists for perceptibility and acceptability of shade mismatch. J Prosthet Dent. 2007;97:200–208. doi: 10.1016/j.prosdent.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 25.Jiang L, Liao Y, Wan Q, Li W. Effects of sintering temperature and particle size on the translucency of zirconium dioxide dental ceramic. J Mater Sci Mater Med. 2011;22:2429–2435. doi: 10.1007/s10856-011-4438-9. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y. Making yttria-stabilized tetragonal zirconia translucent. Dent Mater. 2014;30:1195–1203. doi: 10.1016/j.dental.2014.08.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alraheam IA, Donovan T, Boushell L, Cook R, Ritter AV, Sulaiman TA. Fracture load of two thicknesses of different zirconia types after fatiguing and thermocycling. J Prosthet Dent. 2020;123:635–640. doi: 10.1016/j.prosdent.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Wang F, Takahashi H, Iwasaki N. Translucency of dental ceramics with different thicknesses. J Prosthet Dent. 2013;110:14–20. doi: 10.1016/S0022-3913(13)60333-9. [DOI] [PubMed] [Google Scholar]
- 29.Yan J, Kaizer MR, Zhang Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 2018;88:170–175. doi: 10.1016/j.jmbbm.2018.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu B, Ahn JS, Lee YK. Measurement of translucency of tooth enamel and dentin. Acta Odontol Scand. 2009;67:57–64. doi: 10.1080/00016350802577818. [DOI] [PubMed] [Google Scholar]
- 31.Sun T, Zhou S, Lai R, Liu R, Ma S, Zhou Z, Longquan S. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J Mech Behav Biomed Mater. 2014;35:93–101. doi: 10.1016/j.jmbbm.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Fabbri G, Mancini R, Marinelli V, Ban G. Anterior discolored teeth restored with Procera all-ceramic restorations: a clinical evaluation of the esthetic outcome based on the thickness of the core selected. Eur J Esthet Dent. 2011;6:76–86. [PubMed] [Google Scholar]
- 33.Sulaiman TA, Abdulmajeed AA, Donovan TE, Ritter AV, Vallittu PK, Närhi TO, Lassila LV. Optical Properties and light irradiance of monolithic zirconia at variable thicknesses. Dent Mater. 2015;31:1180–1187. doi: 10.1016/j.dental.2015.06.016. [DOI] [PubMed] [Google Scholar]
- 34.ISO 6872. Dentistry-Ceramic materials. Geneva; Switzerland: International Standard Organization (ISO); 2008. [Google Scholar]
- 35.Gómez-Polo C, Montero J, Gómez-Polo M, Martin Casado A. Comparison of the CIELab and CIEDE 2000 Color Difference Formulas on Gingival Color Space. J Prosthodont. 2020;29:401–408. doi: 10.1111/jopr.12717. [DOI] [PubMed] [Google Scholar]