Abstract
Purpose:
To evaluate the functional and anatomical outcomes for autologous retinal autograft with Finesse™ Flex Loop for failed macular holes.
Methods:
This is a retrospective study analyzing medical records of consecutive patients with refractory macular hole (at least 1 prior surgery) and eyes with retinal detachment with coexisting macular holes (MH). Optical coherence tomography (OCT) of the macula was performed before and after surgery. The primary study outcome evaluated were the functional and anatomic macular hole closure, and secondary outcomes were improvement in visual acuity and restoration of the outer retinal bands, external limiting membrane, and ellipsoid zone in eyes with acquisition of autologous retinal transplant using Finesse Loop.
Results:
The study included eight eyes of eight patients; retinal autograft was performed in six (75.0%) and autologous retinal transplantation (ART) with rhegmatogenous retinal detachment (RRD) was performed in two (25.0%) eyes. The average MH basal diameter in the study was 1310.88 ± 138.63 µm. The successful hole closure rate was observed to be 75% (6 eyes) and 100% retinal reattachment was observed in ART with RRD. Statistically significant (P = 0.001) improvement was noted for preop and postop visual acuity gain for ART acquisition and postop macular hole closure. The restoration of the external limiting membrane (ELM) and ellipsoid zone (EZ) was observed in 37.5% (3 eyes) of patients.
Conclusion:
Finesse™ Flex Loop can be used to harvest retinal tissue and it provides good anatomical and functional outcomes for failed macular hole.
Keywords: Finesse loop, macular hole, refractory macular hole, retinal detachment
With modern vitreoretinal surgical techniques for managing macular holes (MH) with pars plana vitrectomy (PPV) and internal limiting membrane (ILM) peeling with gas tamponade, primary MH closure rates have exceeded 90%. However, with refractory MH subjected to prior ILM peeling, the anatomic and functional success rarely exceeds70%.[1]
Since the development of autologous retinal transplantation (ART) in 2016 as a surgical technique by DS Grewal et al.,[2] the technique has been performed and perfected for better outcomes around the world, with modifications including combined neurosensory retina—retinal pigment epithelium—choroid grafts, subretinal placement of the graft, and even as a primary treatment for managing large chronic macular holes.[3] Grafting procedures, such as ART and amniotic membrane grafts, have allowed surgeons to treat macular holes using a tissue scaffold to promote centripetal migration of macular hole edges in the case of an amniotic membrane and the addition of tissue in the ART.[3] The role of blood products as adjuvants has been studied in literature which show good adherence of the transplant to the foveal graft site.[4] In this study, we present the use of Finesse™ Flex Loop for the acquisition of ART and evaluate the functional and anatomical outcomes in managing refractory macular holes with and without rhegmatogenous retinal detachment (RRD).
Methods
This is a retrospective analysis of medical records of patients with refractory MH (at least one prior surgery) and eyes with retinal detachment with coexisting MH who underwent surgical repair with an ART free flap in a tertiary eye hospital in India. The study protocol was approved by the Institutional Review Board for Human Subjects and the study adheres to the tenets set forth in the Declaration of Helsinki. Surgical informed consent was obtained from all the participants.
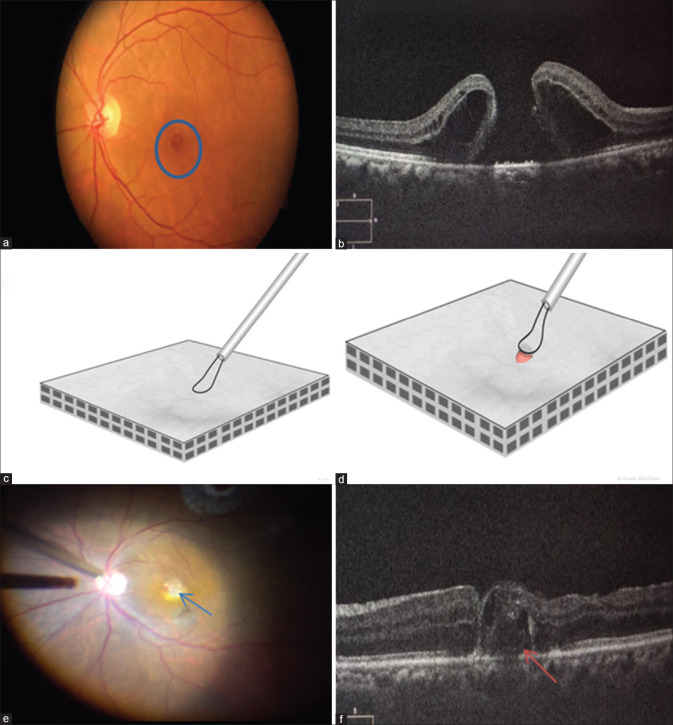
All patients had more than 6 months of postoperative follow up. Exclusion criteria were patients who had any ocular history of diabetic retinopathy, vascular occlusion, retinal neovascularization, inflammatory disease, or trauma. Inclusion criteria were patients with refractory full-thickness MHs [Fig. 1a] after at least one prior surgery with removal of the ILM and an intraocular tamponade, and eyes with RRD with coexisting macular hole. Optical coherence tomography (OCT) [Fig. 1b] was performed before and after surgery in all eyes using a commercially available spectral-domain OCT device (Cirrus 500).
Figure 1.
(a) Fundus image of the left eye with a refractory macular hole (blue circle); (b) Preoperative OCT of the MH. (c) Animation with the Finesse Loop above the retinal surface; (d) Loops help in lifting the retinal harvest tissue; (e) Intraoperative ART in situ of MH (blue arrow); (f) Postoperative radial OCT of the ART filling the MH with restoration of ELM and EZ (orange arrow)
The primary study outcome evaluated the functional and anatomic MH closure after the retinal free flap on OCT. Secondary outcomes were visual acuity (VA) improvement, restoration of the outer retinal bands—external limiting membrane (ELM) and ellipsoid zone (EZ)—which were measured using OCT and comparison of outcomes in eyes with acquisition of ART using Finesse Loop.
Surgical technique
A three-port, 23-gauge PPV (Constellation; Alcon, Fort Worth, TX) was performed after giving peribulbar anesthesia using monitored anesthesia care by a single surgeon. In all eyes, any residual peripheral vitreous was removed with the assistance of scleral depression. A neurosensory retina harvest site was selected in the mid-periphery, typically superior to the supero-temporal or nasal arcade. The size of the harvest was calibrated according to the size of the MH intraoperatively. Endodiathermy was performed in a concentric manner around the site of harvest and was followed by endolaser barrage of 2–3 rows around the cauterized retinal tissue [Video 1].
ART was harvested using a membrane loop (FINESSE Flex loop, Alcon, Fort Worth, TX, USA). It was used to gently lift the retinal flap [Fig. 1c] from its bed after doing endodiathermy and a localized laser barrage. The area of diathermy makes the retina friable and easier to lift up using the loop. Full thickness of the graft was assured by visualizing a clear choroidal bed underneath [Fig. 1d]. An intraocular forceps was used to hold the edge of the autologous retinal graft (ARG) which assisted in peeling the autologous tissue. The graft was then transferred to MH and tucked in the MH filling the gap [Fig. 1e]. The eye wherein ART was taken in RRD, the nasal retina was attached and was chosen as the harvest site with the Finesse Flex loop. The patients were prescribed routine topical medications and were advised two weeks of prone position. They were initially seen at one week, three weeks, and six weeks. The surgical success was determined at the 6th week [Fig. 1f]. The OCT was repeated at six weeks postoperatively. Thereafter, they were followed up on three-monthly basis, depending on the operating surgeon’s judgement. Silicone oil removal was done three months after the surgery.
Statistical analysis
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences) for Windows (version 24.0). Categorical variables were described as frequency (percentage), and mean ± standard deviation was used for continuous parameters. All the data were entered on Microsoft Excel and it is a combination of qualitative and quantitative variables. Descriptive statistics were performed for continuous variables and frequency distribution was used for qualitative variables. Wilcoxon signed-rank test was used to test the pre- and post-VA value. The Chi-squared test for independence was used to test the association between the two qualitative variables. All statistical tests were performed using SPSS 24 and any statistical test with a P value less than 0.05 was considered as statistically significant.
Results
The study included eight eyes of eight patients: three males (37.5%) and five females (62.5%) [Table 1]. The age ranged from 24 to 65 years. The ART was done in six eyes (75.0%) and ART with RRD was performed in two eyes (25.0%). The average MH basal diameter in the study was 1310.88 ± 138.63 µm with a range 1069–1529 µm. The intraoperative tamponading agent used in surgery was perfluoropropane (14%) in six eyes (75.0%), and silicone oil was used in two eyes (25.0%). The eyes with ART with RRD had 100% retinal reattachment which was maintained after silicone oil removal. The successful hole closure rate was observed to be six eyes (75.0%) in our study. The demographic details are given in Table 2.
Table 1.
Patients pre- and post-operative demographic data
| Patient | Age | Gender | Preop Vision (logMar) | Postop Vision (logMar) | Basal Hole Diameter (µm) | Complication |
|---|---|---|---|---|---|---|
| 1 | 55 | Female | 1 | 0.60 | 1286 | Nil |
| 2 | 46 | Male | 1.4 | 0.60 | 1334 | Nil |
| 3 | 65 | Female | 0.6 | 0.50 | 1529 | Nil |
| 4 | 59 | Male | 1.1 | 0.80 | 1280 | Nil |
| 5 | 53 | Female | 1.4 | 1 | 1389 | Graft shrinkage |
| 6 | 50 | Female | 0.8 | 0.40 | 1069 | Graft shrinkage |
| 7 | 52 | Female | 1.3 | 0.80 | 1200 | Nil |
| 8 | 24 | Male | 1.3 | 1 | 1400 | Nil |
Table 2.
Demography of the patients in the study
| Frequency (n=8) | |
|---|---|
| Age groups (years) | |
| ≤40 | 1 (12.5%) |
| 41-60 | 6 (75.0%) |
| >60 | 1 (12.5%) |
| Mean±SD | 50.5±12.15 |
| Gender | |
| Male | 3 (37.5%) |
| Female | 5 (62.5%) |
| Operated Eye | |
| Right | 5 (62.5%) |
| Left | 3 (37.5%) |
| Type of Surgery | |
| ART | 6 (75.0%) |
| ART + RRD | 2 (25.0%) |
| RD Clock Hours | |
| Time to previous surgery | 2.75±5.09 |
| Mean±SD (months) | |
| Macular hole basal diameter (µm) | 1310.88±138.63 |
| Lens Status | |
| Phakic | 4 (50.0%) |
| Pseudophakic | 3 (37.5%) |
| Cataract Combined | |
| Cataractous | |
| Aphakic | 1 (12.5%) |
| Tamponade | |
| Gas | 6 (75.0%) |
| Silicon Oil | 2 (25.0%) |
| Auto-graft site | |
| SNQ | 5 (62.5%) |
| STQ | 3 (37.5%) |
In comparing the preop and postop visual acuity gain with ART acquisition and postop macular hole closure, the postoperative visual recovery at six weeks was statistically significant (P = 0.001) [Table 3]. In the study, improvement in visual acuity was observed in 75% (six eyes), over a follow-up period of six months.
Table 3.
The comparison of pre- op and post op visual acuity
| Vision | Mean±SD | Mean Difference (95% C.I (Lower-Upper)) | P |
|---|---|---|---|
| Loop | |||
| Preop | 1.113±0.295 | 0.4±0.2 | 0.001 |
| Postop | 0.713±0.223 |
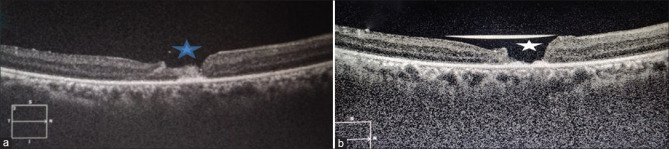
While analyzing the outcomes for restoration of ELM and EZ in the postoperative period, the restoration was noted in three eyes (37.5%). No statistically significant outcomes (P = 0.174) with respect to complete restoration of ELM and EZ were observed. The postoperative complications with ART were of graft shrinkage in two eyes (25.0%) which were observed at six weeks of postoperative follow up [Fig. 2].
Figure 2.
(a) Postoperative radial OCT of the ART filling the MH gap (blue star) at 1 week postoperatively; (b) Postoperative radial OCT of the ART shrinkage (white star) at 6 weeks postoperatively
Discussion
Surgical techniques for the repair of macular holes have undergone a stepwise evolution since the initial reports of vitrectomy and gas tamponade in the early 1990s.[5]
A macular hole that fails to close in the first attempt despite adequate ILM peeling poses a challenge. Large chronic holes or those in high myopic eyes are more prone to failure.[6] The inverted flap technique, advocated by Michalewska et al.,[7] was seen to be more successful in closing such holes. The success rate of ILM peeling alone was seen to vary from 78% to 81% versus 89% with inverted ILM flap in large MH >800 µm in size.[8,9]
The advent of ART has generated new and interesting clinical questions with regard to successful anatomical and functional outcomes. In comparison with the anatomical outcomes as observed for refractory macular holes, we observed a 75% (six eyes) successful macular hole closure with respect to 89% anatomical closure rate as reviewed in literature with ART.[3,4] With regard to the functional closure for restoration of ELM and EZ on OCT, the global consortium noted a success rate of 67% which is lesser than our study of 37.5% due to smaller sample size in our study.[3]
On comparing the outcomes for combined macular hole and RRD, we observed a 100% (two eyes) anatomical closure rate of MH and 100% retinal reattachment rate with silicone oil as an internal tamponade, respectively. In comparison to the results obtained by the global consortium,[3] the retinal reattachment rate after the first surgery was 79% and MH closure was 95%, which is in comparison to our study. Similar results have been noted by Dilraj Grewal et al.[2] for MH associated with RRD and similar results have been reported by Singh A et al.[10] in managing MH with RRD. With regard to the restoration of ELM and EZ in MH with RRD eyes, in our study, we observed only one (50%) eye at six months of follow-up period whereas in literature, five cases demonstrated reconstitution of the ELM (29%) at a mean of 1.9 ± 0.60 months and four cases conveyed reconstitution of the EZ band (24%) at a mean of 1.5 ± 0.29 months in the global consortium.[3] With regard to postoperative visual improvement, ART obtained with Finesse Loop showed statistically significant visual outcomes. In our study, improvement in visual acuity was observed in 75% of patients in comparison to Dilraj Grewal et al.[1] wherein they observed postoperative improvement in 52.3%, and vision was stable in 33.3%. In the outcomes obtained in the global consortium, they observed that patients with MH, whether primary or refractory, were more likely to have better final visual acuity than patients with MH-RRD.[3] In our study, we found no significant difference in anatomical outcomes with regard to the use of internal tamponade of silicone oil versus perfluoropropane gas (P = 0.06). Similarly in literature, no significant difference between tamponade agent and MH closure rate and visual acuity was observed.[3]
The Finesse™ Flex Loop’s nitinol (nickel/titanium) loop is designed for consistency and for excellent visibility to the contact area, and the concave-shaped tines are designed to help avoid unnecessary penetration during procedures. The tines have been postulated that they do not penetrate any deeper than 85% of the ILM,[9] but herein we use the loop for acquisition of ART as it allows smoother and well-defined and complete harvest of the retinal tissue with minimal retinal tissue distortion and minimal chances of choroidal/retinal bleeding, and limits the use of bimanual instrumentation for harvesting ART.
Our study has several limitations due to its retrospective nature, limited number of patients, and a shorter follow up of six months. To understand the efficacy and safety of ART relative to other surgical techniques of MH closure (e.g., vitrectomy with ILM peel or flap, amniotic membrane graft, etc.), a national, multicenter, randomized, single-masked, prospective clinical trial could be designed, including standardized ancillary testing with OCT, OCTA, autofluorescence, microperimetry, multifocal ERG, and adaptive optics.
Conclusion
In conclusion, our technique of harvesting ART using the Finesse™ Flex Loop provides good anatomic and functional outcomes for failed macular holes and even in eyes with MH with RRD with minimal complication rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on: www.ijo.in
References
- 1.Grewal DS, Charles S, Parolini B, Kadonosono K, Mahmoud TH. Autologous retinal transplant for refractory macular holes:Multicenter international collaborative study group. Ophthalmology. 2019;126:1399–408. doi: 10.1016/j.ophtha.2019.01.027. [DOI] [PubMed] [Google Scholar]
- 2.Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134:229–30. doi: 10.1001/jamaophthalmol.2015.5237. [DOI] [PubMed] [Google Scholar]
- 3.Moysidis SN, Koulisis N, Adrean SD, Charles S, Chetty N, Chhablani JK, et al. Autologous retinal transplantation for primary and refractory macular holes and macular hole retinal detachments:The global consortium. Ophthalmology. 2021;128:672–85. doi: 10.1016/j.ophtha.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Wu A-L, Chuang L-H, Wang N-K, Chen K-J, Liu L, Yeung L, et al. Refractory macular hole repaired by autologous retinal graft and blood clot. BMC Ophthalmol. 2018;18:213. doi: 10.1186/s12886-018-0898-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wendel RT, Patel AC, Kelly NE, Salzano TC, Wells JW, Novack GD. Vitreous surgery for macular holes. Ophthalmology. 1993;100:1671–6. doi: 10.1016/s0161-6420(93)31419-3. [DOI] [PubMed] [Google Scholar]
- 6.Steel DH, Donachie PHJ, Aylward GW, Laidlaw DA, Williamson TH, Yorston D, et al. Factors affecting anatomical and visual outcome after macular hole surgery:Findings from a large prospective UK cohort. Eye (Lond) 2021;35:316–25. doi: 10.1038/s41433-020-0844-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Nawrocki J. Inverted internal limiting membrane flap technique for surgical repair of myopic macular holes. Retina. 2014;34:664–9. doi: 10.1097/IAE.0000000000000042. [DOI] [PubMed] [Google Scholar]
- 8.Narayanan R, Singh SR, Taylor S, Berrocal MH, Chhablani J, Tyagi M, et al. Surgical outcomes after inverted internal limiting membrane flap versus conventional peeling for very large macular holes. Retina. 2019;39:1465–9. doi: 10.1097/IAE.0000000000002186. [DOI] [PubMed] [Google Scholar]
- 9.Kubota M, Watanabe T, Hayashi T, Watanabe A, Nakano T. Novel use of finesse flex loop for macular hole retinal detachment. Am J Ophthalmol Case Rep. 2020;18:100703. doi: 10.1016/j.ajoc.2020.100703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh A, Dogra M, Singh SR, Moharana B, Tigari B, Singh R. Microscope-integrated optical coherence tomography-guided autologous full-thickness neurosensory retinal autograft for large macular hole-related total retinal detachment. Retina (Philadelphia, Pa.) 2020 doi: 10.1097/IAE.0000000000002729. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.