Abstract
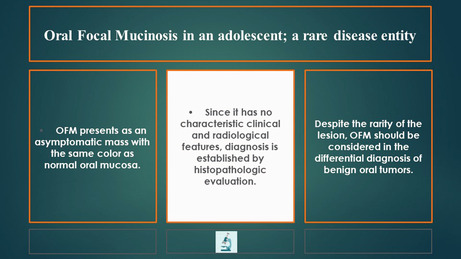
Oral focal mucinosis (OFM) is an extremely rare benign lesion of the oral cavity with unknown etiology, considered the oral counterpart of cutaneous focal mucinosis. It occurs mainly in women in the fourth and fifth decades of life. It has no characteristic features, and diagnosis depends on histological evaluation. Its pathogenesis is related to the excessive production of hyaluronic acid by fibroblasts during collagen production, which leads to focal myxoid degeneration. To date, ten documented cases have been reported in the literature in adolescents. This paper reports a rare case of OFM with a narrative review of the available literature.
Keywords: connective tissue disease, myxomatous lesion, Oral focal mucinosis
Oral focal mucinosis presents as an asymptomatic mass with the same color as normal oral mucosa. Since it has no characteristic clinical and radiological features, diagnosis is established by histopathologic evaluation. Despite the rarity of the lesion, OFM should be considered in the differential diagnosis of benign oral tumors.
1. INTRODUCTION
Oral focal mucinosis (OFM) is a rare lesion in the oral cavity that is considered a counterpart of cutaneous focal mucinosis. Its exact etiology is unknown but increased hyaluronic acid and myxoid fibro collagenous tissue production are thought to be the cause. It is an asymptomatic and benign lesion with a predilection for keratinized tissue such as gingiva or hard palate. It is more common in women than men, with an approximate ratio of 3:1. It often occurs in the fourth and fifth decades of life, and it has also been reported rarely in children and adolescents. 1 Since the first report by Tomich et al. in 1974, 100 cases of OFM have been reported in the English‐language literature. 2 , 3 Histologically, the lesion appears as a well‐circumscribed and uniform area of myxomatous connective tissue and contains no mast cells and often no reticulin network. 4 This myxomatous tissue is positive for alcian blue staining, which may resemble other oral myxoid lesions such as soft‐tissue myxoma, fibrous hyperplasia with myxoid degeneration, nerve sheath myxoma (NSM), myxoid neurofibroma, and mucocele. 3
The mucinous site is much less vascular than the adjacent connective tissue. Perivascular infiltration of T‐cell lymphocytes at the periphery is evident. 5
It is a histopathological diagnosis, as OFM remains clinically similar to other more common oral lesions. In a review study by Gonzaga et al., among the 14,204 oral lesion biopsies over 42 years, only 11 cases were histopathologically diagnosed as OFM. The primary clinical diagnoses of these lesions were oral traumatic fibroma, followed by peripheral giant cell granuloma. 6
2. CASE PRESENTATION
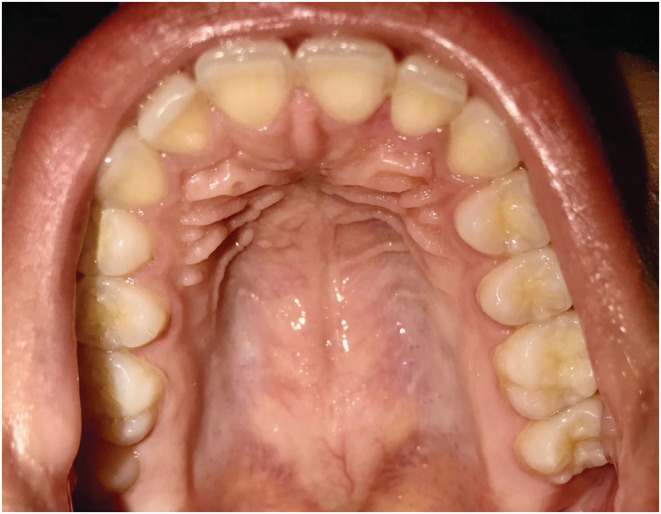
A 17‐year‐old female patient presented to the Department of Oral Medicine, Tehran University of Medical Science, with a chief complaint of a gingival mass. A pedunculated exophytic nodule of 5*5 mm was present palatally between her UL1 and UL2 (Figure 1), and the patient reported that this lesion had been present for over a year and remained asymptomatic. The lesion had a homogenous texture and firm consistency with normal and non‐ulcerated overlying mucosa. A periapical radiograph confirmed no root resorption or alveolar crestal bone loss (Figure 2). There was no history of trauma, no pathological mobility of the teeth was noted, and oral hygiene was good. The patient did not take any medication and had no systemic disease. The differential clinical diagnosis of fibroma and peripheral ossifying fibroma was made, and the excisional biopsy was performed under a local anesthetic.
FIGURE 1.

Preoperative intraoral view of the lesion.
FIGURE 2.

Periapical radiograph showing no root resorption and bone loss.
A periodontal dressing packing material was placed (COE‐PAK) due to the impossibility of suturing in the surgical area. The surgical wound healed satisfactorily without complications and with no signs of recurrence after 12 weeks. The patient has routinely followed up with no signs of discomfort or recurrence (Figure 3).
FIGURE 3.
Postoperative intraoral view after 3 months.
Written informed consent was obtained from the patient and her parents to publish this case report and any accompanying images.
3. MICROSCOPIC EVALUATION
Histopathologic analysis showed an encapsulated nodular lesion composed of a proliferation of bland‐looking spindle cells in the prominent myxoid stroma and fine collagen bundles (Figure 4). Parakeratotic stratified squamous epithelial of the oral mucosa covered the lesion. In the IHC study, S‐100 was negative, ruling out other myxomatous lesions of neural origin (Figure 5). Special staining showed PAS negative, and reticulin was positive in surrounding fibers (Figure 6).
FIGURE 4.
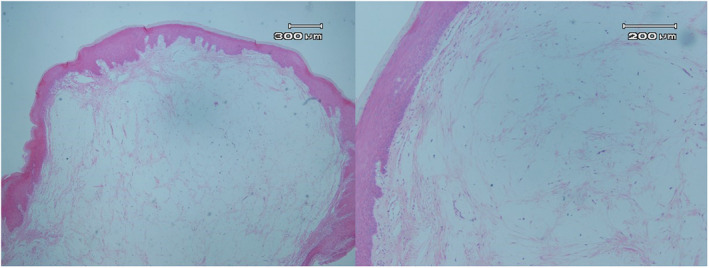
H&E section showing proliferation of bland‐looking spindle cells in a myxoid stroma ( 40×, 100× magnification).
FIGURE 5.
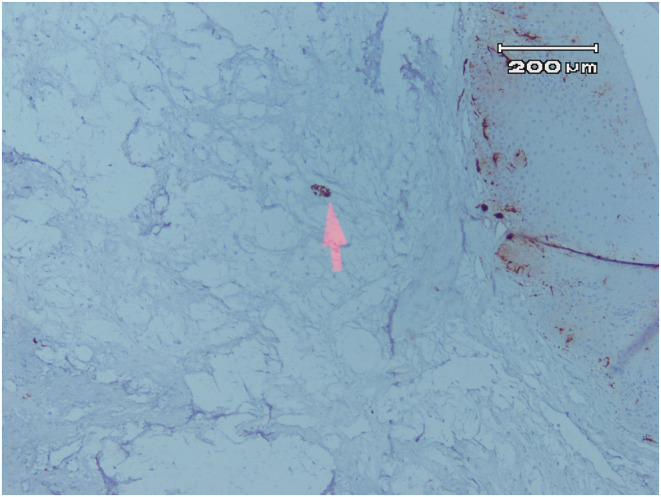
S‐100 staining of the tumor was negative, ruling out a myxomatous lesion of neural origin; the nerve bundle showed internal positive control (100× magnification).
FIGURE 6.
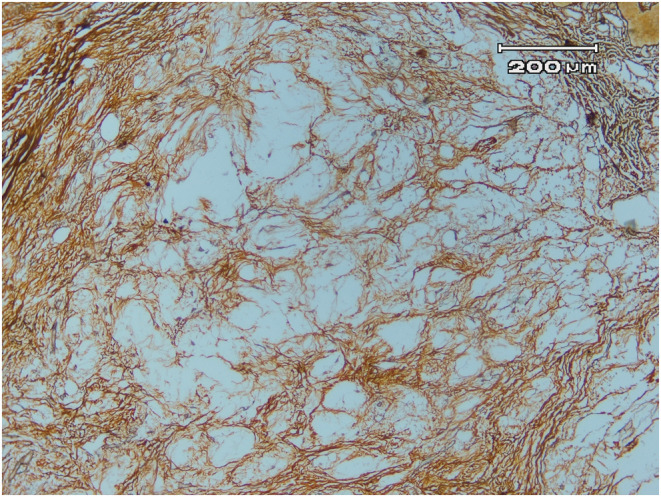
Immunohistochemical staining showing positivity for Reticulin (100× magnification).
4. DISCUSSION
In 1966, Johnson and Helwig described an asymptomatic dome‐shaped skin nodule, frequently on the face and trunk, termed cutaneous facial mucinosis. The oral counterpart of this lesion was described by Tomich. 2 Clinically, OFM is seen as a painless sessile, firm nodule the same color as the surrounding mucosa. The most common intraoral sites are gingiva, palate, and alveolar ridge mucosa. The review of the available literature shows that it is most diagnosed as irritation fibroma or epulis and the clinical diagnosis of OFM is impossible. However, there are no characteristic clinical and radiological features; accidental findings during dental treatment have been reported. 3 The pathophysiology of OFM is unclear, but the local accumulation of mucin in connective tissue due to the increased production of hyaluronic acid by fibroblasts is considered to be the cause of this lesion. 9 Neto et al. 15 suggested that a predisposing factor for OFM could be traumatic stimuli. JOSHI et al. 16 also described trauma as an influential factor in increasing the size of these lesions. Pathological examination, including immunostaining, is essential for the definitive diagnosis of OFM. Histopathological findings include a lack of encapsulation of the neoplastic tissue mass, a myxomatous stroma, and sometimes localized fibrous connective tissue. 9 Myxoid tumors of the oral cavity include diverse lesions with a wide range of biological behaviors. In the classification Bajpai et al. 17 presented for myxoid tumors of the oral cavity, these tumors were divided into seven general groups, including adipose, neural, fibroblastic, chondroblastic, muscle, odontogenic and miscellaneous tumors, in terms of myxoid degeneration in histopathology. The primary histological differential diagnoses of OFM are soft‐tissue myxoma, nerve sheath myxoma, inflammatory fibroepithelial hyperplasia with myxoid degeneration, and odontogenic myxoma. 15 Soft‐tissue myxomas are extremely rare tumors composed of very loose cellular connective tissue containing little collagen and large amounts of an intercellular substance rich in acid mucopolysaccharide. 18 Unlike tumors, OFM comprises a localized area of relatively thick myxomatous tissue surrounded by collagen fibers. This histological feature is necessary to differentiate OFM and other lesions. 19 The helpful morphological findings that differentiate OFM from myxoma include non‐infiltrative growth patterns, superficial location, and the presence of fragmented and randomly arranged collagen fibers. 6 Unlike OFM, soft‐tissue myxoma shows abundant formation of reticular fibers, evidenced by silver staining. 20
Nerve sheath myxoma, a variant of neurofibroma, is included in the differential diagnoses of OFM. Still, their difference is that nerve sheath myxoma has fibrous septa between multiple myxoid nodules, and more plump stromal cells are evident. 5
As mentioned earlier, OFM is common in women in the fourth and fifth decades of life and is rare in children and adolescents. However, there are reports of OFM in children even at the age of two. 11 To the best of our knowledge, ten reported cases of oral focal mucinosis in patients under 18 years old (Table 1).
TABLE 1.
Cases of oral focal mucinosis in adolescents reported to date.
| Author | Age | Sex | Location | Duration | Symptoms | Clinical differential | Treatment |
|---|---|---|---|---|---|---|---|
| Tomich 1974 2 | 16 | Male | Gingiva | Not available | Asymptomatic | Irritation Fibroma | Surgical excision |
| Gnepp 1989 7 | 4 | Female | Hard palate | Not available | Asymptomatic | Not available | Not available |
| Buchner 1990 8 | 16 | Female | Gingiva | Not available | Not available | Not available | Not available |
| Aldred 2003 9 | 16 | Female | Gingiva | 4 months | Asymptomatic | Fibrous hyperplasia | Surgical excision |
| Lee 2012 10 | 17 | Female | Gingiva | Not available | Not available | Not available | Not available |
| Woo 2015 11 | 2 | Female | Palate | 3 months | Asymptomatic | Palatal exostosis, lymphoma, Pleomorphic adenoma | Surgical excision |
| Yanaguizawa 2018 12 | 14 | Female | Buccal mucosa | Not available | Asymptomatic | Fibroma | Surgical excision |
| Cho 2019 13 | 13 | Female | Gingiva | 4 months | Asymptomatic | Fibroma, peripheral ossifying fibroma | Surgical excision |
| Cameron 2020 14 | 14 | Female | Gingiva | Not available | Asymptomatic | Epulis, fibroma | Surgical excision |
| Cunha Silva 2021 3 | 8 | Male | Gingiva | 36 months | Asymptomatic | Pyogenic granuloma | Surgical excision |
Oral focal mucinosis presents as a localized gingival mass, with irritation fibroma, pyogenic granuloma peripheral ossifying fibroma (POF), and peripheral giant cell granuloma (PGCG) as the appropriate differential diagnosis. Irritation fibroma is a form of fibrous reactive hyperplasia that occurs on the gingiva at any age with a predilection for young adults. It should be treated by local excision, including the periodontal ligament and any etiologic agent, such as calculus. 21 Myxoid degeneration can be present at irritation fibroma, making it more difficult to distinguish these two entities. The main histological parameter to differentiate these entities must be the extension of the myxoid areas, which are more extensive in OFM but focal in irritation fibroma. 6
Peripheral ossifying fibroma is a fibro‐osseous reactive lesion that occurs exclusively on the gingiva, and clinically, it is a slow‐growing nodular mass with a smooth surface and the same color as the normal mucosa. POF is more common in women in the second decade of life, with a high chance of recurrence. 22 PG may represent a red‐purple nodule, with or without ulceration, sessile or pedunculated. It is known to involve the gingiva commonly with the highest incidence in the second and fifth decades, and females are slightly more affected than males. The distinguishing feature of this lesion from OFM is its tendency to bleed. 23 PGCG also occurs exclusively on the gingiva or edentulous alveolar ridge and is a relatively common tumorlike growth of the oral cavity. The clinical appearance is similar to the pyogenic granuloma of the gingiva, but PGCG often is more blue‐purple. Although PGCG develops within soft tissue, cupping resorption of the underlying alveolar bone sometimes is seen. 22 This aspect is not found in OFM. 24
Mesenchymal tumors such as Schwannoma and Neurofibroma can also be added to the differential diagnosis. Schwannoma is a benign neoplasm derived from a proliferation of Schwan cells of the nerve sheath, occurring mainly in the 4th decade of life with no gender predominance. It represents an asymptomatic lump at any oral cavity site, but the tongue is the favored location. 25 Neurofibroma may appear as solitary or multiple lesions as part of the neurofibromatosis syndrome. Solitary neurofibroma presents at any age as an asymptomatic submucosal mass. The tongue and the buccal mucosa are the most frequently involved sites in the oral cavity, but other areas, such as the palate, lip, and gingiva, have also been reported. 26
So far, surgical excision has been a treatment for all reported cases of OFM. Of all these reported cases, there has been only one recurrence due to incomplete resection. 27 However, regular follow‐up observations may be necessary in most cases.
Here, we presented a case of OFM in an adolescent, a rare entity. Although OFM is difficult to diagnose clinically, this lesion should be considered in the differential diagnosis of benign oral tumors.
5. CONCLUSION
Oral focal mucinosis is a rare benign disorder often clinically misdiagnosed as reactive lesions or delicate proliferative processes. Clinicians should consider OFM in the differential diagnosis of soft‐tissue lesions in the oral cavity, mainly in the gingiva.
AUTHOR CONTRIBUTIONS
AT and KHM were involved in the diagnosis and management of the patient and have been responsible for the clinical part of the manuscript. SD reported the histopathological evaluation. AT and KHM did the literature review and drafted the manuscript. KHM was responsible for final editing of the manuscript. All authors have read and approved the final manuscript.
CONFLICT OF INTEREST
The authors declare that the research was conducted without any commercial or financial relationships construed as a potential conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy. The patient and her parent are aware of this report and signed the informed consent.
ACKNOWLEDGEMENT
The authors would like to thank the patient for giving consent for the publication of the case.
Tonkaboni A, Hafezi Motlagh K, Derakhshan S. Oral focal mucinosis in an adolescent: A rare entity. Clin Case Rep. 2022;10:e06594. doi: 10.1002/ccr3.6594
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1. de Lima AAS, Machado MÂN, Martins WD, et al. Oral focal mucinosis. Quintessence Int. 2008;39:7. [PubMed] [Google Scholar]
- 2. Tomich CE. Oral focal mucinosis: a clinicopathologic and histochemical study of eight cases. Oral Surg Oral Med Oral Pathol. 1974;38(5):714‐724. [DOI] [PubMed] [Google Scholar]
- 3. Silva Cunha JL, Leite AA, de Castro Abrantes T, et al. Oral focal mucinosis: a multi‐institutional study and literature review. J Cutan Pathol. 2021;48(1):24‐33. [DOI] [PubMed] [Google Scholar]
- 4. Gonzaga AK, de Oliveira DH, Lopes ML, Queiroz LM, Dantas da Silveira EJ. Clinicopathological study of oral focal mucinosis: a retrospective case series. Med Oral Patol Oral Cir Bucal. 2018;23(4):e401‐e405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ena S, Manjari N, Anirban C, Ramesh A. Oral focal mucinosis: a rare case report of two cases. Ethiop J Health Sci. 2013;23(2):178‐182. [PMC free article] [PubMed] [Google Scholar]
- 6. Gonzaga AK, de Oliveira DH, Lopes ML, Filho TJ, Queiroz LM, da Silveira ÉJ. Clinicopathological study of oral focal mucinosis: a retrospective case series. Med Oral Patol Oral Cir Bucal. 2018;23(4):e401‐e405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gnepp DR, Vogler C, Sotelo‐Avila C, Kielmovitch IH. Focal mucinosis of the upper aerodigestive tract in children. Hum Pathol. 1990;21(8):856‐858. [DOI] [PubMed] [Google Scholar]
- 8. Buchner A, Merrell PW, Leider AS, Hansen LS. Oral focal mucinosis. Int J Oral Maxillofac Surg. 1990;19(6):337‐340. [DOI] [PubMed] [Google Scholar]
- 9. Aldred MJ, Talacko AA, Ruljancich K, et al. Oral focal mucinosis: report of 15 cases and review of the literature. Pathology. 2003;35(5):393‐396. [DOI] [PubMed] [Google Scholar]
- 10. Lee JG, Allen G, Moore L, Gue S. Oral focal mucinosis in an adolescent: a case report. Aust Dent J. 2012;57(1):90‐92. [DOI] [PubMed] [Google Scholar]
- 11. Woo J, Cheung WS. Bilateral oral focal mucinosis on the palate of a 2‐year‐old child: a case report. Int J Paediatr Dent. 2015;25(1):70‐72. [DOI] [PubMed] [Google Scholar]
- 12. Yanaguizawa WH, Costa SAP, Sanches GT, et al. Unusual clinical presentations of Oral focal mucinosis: two case reports. Oral Surg, Oral Med, Oral Pathol Oral Radiol. 2018;126(3):e83. [Google Scholar]
- 13. Cho JJ, Shupak RP, Michaels C. Oral focal mucinosis of the mandible in an adolescent patient. BMJ Case Rep. 2019;12(12):e232671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cameron A, Webster JEN, Wicks CE, Colbert SD. Oral focal mucinosis of the palate: a rare disease entity. BMJ Case Rep. 2020;13(3):e230233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Neto JR, Sendyk M, Uchida LM, Nunes FD, de Paiva JB. Oral focal mucinosis associated with surgically assisted rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2014;145(4):534‐538. [DOI] [PubMed] [Google Scholar]
- 16. Joshi CP, Dani NH, Mahale SA, Patel NR. A case of oral focal mucinosis of gingiva: lesion in disguise. J Indian Soc Periodontol. 2015;19(5):586‐588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bajpai M, Pardhe N. A simplified working classification proposed for myxoid tumors of Oral cavity. Iran J Pathol. 2017;12(4):413‐414. [PMC free article] [PubMed] [Google Scholar]
- 18. Shenoy VS, Rao RA, Prasad V, Kamath PM, Rao KS. Soft tissue myxoma–a rare differential diagnosis of localized oral cavity lesions. J Clin Diagn Res. 2014;8(12):Kd01‐Kd02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nilesh K, Kothi HS, Patil R, Pramod RC. Oral focal mucinosis of posterior maxilla. J Oral Maxillofac Pathol. 2017;21(2):273‐276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gabay E, Akrish S, Machtei EE. Oral focal mucinosis associated with cervical external root resorption: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(4):e75‐e78. [DOI] [PubMed] [Google Scholar]
- 21. Shetty P, Padmanabhan V, Kavitha PR, Thomas H. Peripheral fibroma obstructing the eruption pathway. Indian J Dent Res. 2012;23(5):677‐679. [DOI] [PubMed] [Google Scholar]
- 22. Salum FG, Yurgel LS, Cherubini K, De Figueiredo MA, Medeiros IC, Nicola FS. Pyogenic granuloma, peripheral giant cell granuloma and peripheral ossifying fibroma: retrospective analysis of 138 cases. Minerva Stomatol. 2008;57(5):227‐232. [PubMed] [Google Scholar]
- 23. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16(1):79‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bharti V, Singh J. Oral focal mucinosis of palatal mucosa: a rare case report. Contemp Clin Dent. 2012;3(Suppl 2):S214‐S218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moreno‐García C, Pons‐García MA, González‐García R, Monje‐Gil F. Schwannoma of tongue. J Maxillofac Oral Surg. 2014;13(2):217‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bharath TS, Krishna YR, Nalabolu GR, Pasupuleti S, Surapaneni S, Ganta SB. Neurofibroma of the palate. Case Rep Dent. 2014;2014:898505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sowmya G, Manjunatha BS, Nahar P, Aggarwal H. Oral focal mucinosis: a rare case with literature review. Case Reports. 2015;2015:bcr2014208321. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


