Abstract
Background
Telemedicine is an expanding and feasible approach to improve medical care for patients with long-term conditions. However, there is a poor understanding of patients’ acceptability of this technology and their rate of uptake.
Objective
The aim of this study was to systematically review the current evidence on telemonitoring in the management of patients with long-term conditions and evaluate the patients’ uptake and acceptability of this technology.
Methods
MEDLINE, Scopus, and CENTRAL (the Cochrane Central Register of Controlled Trials) were searched from the date of inception to February 5, 2021, with no language restrictions. Studies were eligible for inclusion if they reported any of the following outcomes: intervention uptake and adherence; study retention; patient acceptability, satisfaction, and experience using the intervention; changes in physiological values; all-cause and cardiovascular-related hospitalization; all-cause and disease-specific mortality; patient-reported outcome measures; and quality of life. In total, 2 reviewers independently assessed the articles for eligibility.
Results
A total of 96 studies were included, and 58 (60%) were pooled for the meta-analyses. Meta-analyses showed a reduction in mortality (risk ratio=0.71, 95% CI 0.56-0.89; P=.003; I2=0%) and improvements in blood pressure (mean difference [MD]=−3.85 mm Hg, 95% CI −7.03 to −0.68; P=.02; I2=100%) and glycated hemoglobin (MD=−0.33, 95% CI −0.57 to −0.09; P=.008; I2=99%) but no significant improvements in quality of life (MD=1.45, 95% CI −0.10 to 3; P=.07; I2=80%) and an increased risk of hospitalization (risk ratio=1.02, 95% CI 0.85-1.23; P=.81; I2=79%) with telemonitoring compared with usual care. A total of 12% (12/96) of the studies reported adherence outcomes, and 9% (9/96) reported on satisfaction and acceptance outcomes; however, heterogeneity in the assessment methods meant that a meta-analysis could not be performed.
Conclusions
Telemonitoring is a valid alternative to usual care, reducing mortality and improving self-management of the disease, with patients reporting good satisfaction and adherence. Further studies are required to address some potential concerns regarding higher hospitalization rates and a lack of positive impact on patients’ quality of life.
Trial Registration
PROSPERO CRD42021236291; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=236291
Keywords: chronic condition, telemonitoring, telemedicine, eHealth, self-monitoring, systematic review, meta-analysis
Introduction
Background
In the United Kingdom, 15 million people live with at least one long-term condition [1], with their care accounting for 70% of the National Health Service budget [1]. Those with long-term conditions have significantly reduced quality of life (QoL) as well as an increased risk of morbidity and mortality [2,3]. Cardiovascular disease, diabetes mellitus, and chronic obstructive pulmonary disease (COPD) are the most common chronic conditions worldwide [4]. Lack of care coordination [5,6] and care planning consultation [5,6] are among the common barriers that patients with long-term conditions face. In addition, the restrictions induced by the COVID-19 pandemic have amplified the challenges that people living with chronic diseases experience in terms of managing their health and accessing health care [7].
Advances in technology have the potential to support patients with long-term conditions in managing their health at home, making the provision of remote health care more accessible and efficient [8]. Web-based health care and telemedicine include the remote delivery of care using communication technology (eg, videoconference software, web-based applications, and home-based health measurement) to enable consultations between patients and their care team, providing continuous monitoring of relevant health parameters. This allows health care professionals to promptly respond to changes in patient health status and adapt their clinical management in real time [9].
Objectives
Recent evidence has deemed telemedicine feasible for patients with long-term conditions and effective in terms of improving medical care [10]. As telemedicine is a rapidly expanding and changing field, recent umbrella reviews [10,11] that consider older primary studies have potentially made conclusions based on noncontemporary data. Therefore, the aim of this systematic review was to update and expand the current literature on telemonitoring by better defining the interventions included to encompass the role that interactive, 2-way communication devices play in improving the care of patients with long-term conditions, as well as evaluate patient uptake and acceptability of this technology.
Methods
Overview
This systematic review was registered on PROSPERO (International Prospective Register of Systematic Reviews; CRD42021236291) and conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [12].
This review aimed to address the following research questions: (1) What is the rate of uptake, patient retention, and patient satisfaction when using 2-way (patient-health care provider) remote patient monitoring devices to manage chronic health conditions? (2) What factors are associated with patient retention and satisfaction when using 2-way (patient-health care provider) remote patient monitoring devices to manage chronic health conditions? (3) Does the use of 2-way (patient-health care provider) remote patient monitoring devices for the management of chronic health conditions affect patient outcomes (eg, changes in physiological measurements, QoL, all-cause and cardiovascular-related hospitalizations, and all-cause and disease-specific mortality)?
Criteria for Considering Studies to Include in the Review
Studies carried out in any setting aiming to evaluate telemonitoring interventions for participants with at least one chronic condition among the following—cardiovascular disease, COPD, or diabetes mellitus—were eligible for inclusion. All randomized controlled trials (RCTs) and nonrandomized trials, before-and-after (pre-post) studies, and interrupted time series were considered for inclusion. Cross-sectional studies and case reports were excluded. Qualitative studies were included to assess participant satisfaction. Ongoing studies (if any) were also considered and presented in a dedicated table.
Participants
Adult participants (aged ≥18 years) were eligible for inclusion in this review if they reported one or more of the following chronic health conditions: cardiovascular diseases (eg, coronary artery disease, atrial fibrillation, stroke, heart failure, and hypertension), COPD, or diabetes mellitus.
Intervention
Interventions designed to remotely collect health information from patients using digital technologies and electronically transfer the information to health care professionals for monitoring and assessment were eligible for inclusion. Only interventions where the participant received a digital device for remote patient monitoring and the participant or their caregiver took physiological measurements and either input the information into the device or the device automatically uploaded the data were included. Health devices suitable for inclusion had to transmit data to the participant’s health care team, and the participant’s health care team had to monitor the information received, assessing it and making appropriate changes to the participant’s treatment accordingly. A 2-way exchange of information was required for a study to be included.
Comparator
Studies in which usual care or a different intervention was used as control or comparator were also considered as eligible for inclusion, as were studies that did not have a control group.
Outcomes
The primary outcomes of interest were (1) intervention uptake (number of people willing to participate in the intervention) and adherence (level of commitment of the patient to the prescribed intervention); (2) study retention (number of people who completed the intervention); and (3) patient acceptability (level of acceptance of the intervention by the participants), satisfaction (number of participants pleased with the intervention), and experience using the intervention. Secondary outcomes included (1) changes in physiological measurements (eg, oxygen saturation, blood pressure [BP], and blood glucose level); (2) all-cause and cardiovascular-related hospitalizations; (3) all-cause and disease-specific mortality; (4) patient-reported outcome measures (eg, mental well-being, depression, and anxiety questionnaires); and (5) QoL, quality-adjusted life years, and any other health economic outcomes reported in the studies. All the studies that reported one or more of these outcomes were considered eligible for inclusion.
Search Strategy
The search strategy was developed by the review team, which agreed on the key terms. Medical Subject Headings terms and synonyms for the different terms, such as “telemedicine,” “digital monitoring,” and “e-health” (Table S1 in Multimedia Appendix 1 [13-163]), were used and combined with Boolean operators, proximity operators, truncations, and wildcards. MEDLINE, Scopus, and CENTRAL (the Cochrane Central Register of Controlled Trials) were searched from the date of inception to February 5, 2021, for relevant studies. There were no language restrictions, but the availability of the full text was a requirement for inclusion. Search results were managed using EndNote (version X9.3.3; Clarivate Analytics).
Study Selection
Two reviewers (MC and DGL) independently screened the titles and abstracts of the studies retrieved from the databases against the search criteria. Additional screening of the preliminary results was independently undertaken by 3 other reviewers (BB, SH, and MI). The full texts of all potentially relevant articles were retrieved and independently assessed by the reviewers in duplicate. Any disagreement was resolved through discussion with the senior author (DL).
Data Extraction
Data extraction was conducted independently by 2 reviewers (DGL and MC). The following information was extracted: (1) authors, year, country, and reference; (2) study aim; (3) study characteristics (study design and sample size); (4) participant characteristics (age, sex, and ethnicity); (5) health condition; (6) intervention (type of telemedicine device, input of the data [manual or automated], delivery of the intervention, staff involved, duration and frequency of the intervention, and follow-up points); (7) comparators (usual care, different intervention, or no intervention); and (8) outcomes (primary and secondary, as reported in the study).
Risk of Bias Assessment
Six authors (DGL, MC, BB, SH, MI, and DL) independently assessed the individual studies for risk of bias in duplicate, and any discrepancies were resolved via discussion or referral to a third reviewer, as required. For RCTs, the Cochrane Risk of Bias version 2 tool [164] was used. For nonrandomized studies, the Risk Of Bias In Non-randomized Studies of Interventions [165] was used.
Data Synthesis
Meta-analyses were conducted on comparable studies. Primary and secondary outcome effect measures with 95% CIs were pooled using the RevMan software (The Cochrane Collaboration) [166]. The results are presented visually using forest plots. Where continuous data were not homogeneous, an estimate of the standardized mean difference (MD) with 95% CIs was calculated. For studies in which quantitative data were too few or too heterogeneous, a narrative synthesis approach was used.
Dichotomous analyses were conducted using the number of events and total sample size as reported in the included studies. The results of the selected studies were combined using the Mantel-Haenszel method. Effect sizes are expressed as relative risk and 95% CIs. Random effect models were applied to all meta-analyses owing to heterogeneity in study characteristics and populations. Heterogeneity was quantitatively assessed using the Higgins index (I2).
For the analysis of QoL, the postintervention scores, as reported in the included studies, were used. Where the SD was not reported, it was calculated using the calculator function available in RevMan. For analysis of changes in physiological parameters (BP and glycated hemoglobin [HbA1c]) and QoL, the results of the selected studies were combined using the generic inverse variance method. Effect sizes are expressed as the MD and SD.
Findings from the included qualitative studies will be synthesized elsewhere using a meta-aggregative approach to data synthesis.
Results
Overview
The database searches identified 10,401 papers. After independent screening of titles and abstracts by 2 study authors, 98.77% (10,273/10,401) of papers were determined to be duplicates or not eligible. After screening against the inclusion and exclusion criteria, of the remaining 128 papers, 96 (75%) were included. No ongoing studies were found (Figure 1). A full list of the excluded studies with reasons for exclusion is provided in Table S2 in Multimedia Appendix 1. Full texts of all 96 included papers [13-109] were retrieved.
Figure 1.
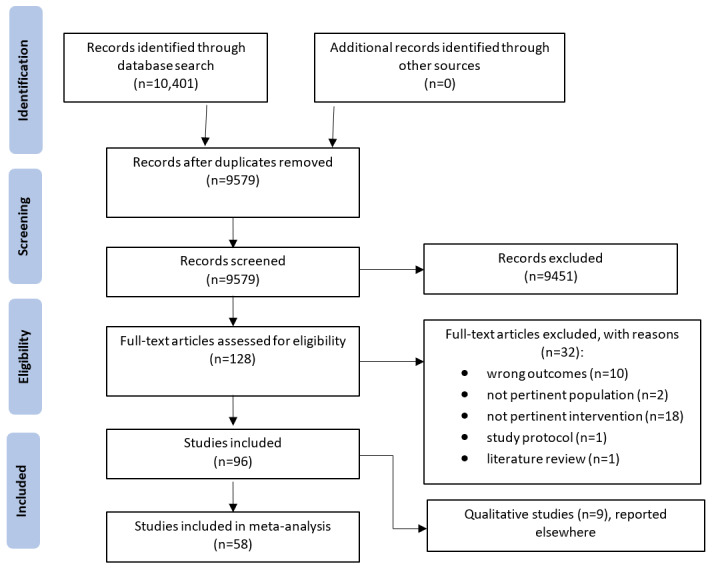
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram depicting the screening and study selection process.
No study reporting outcomes related to intervention uptake, study retention, and patient acceptability were identified in our search and, therefore, these outcomes could not be analyzed. The following analyses and results concern only patient adherence and satisfaction as well as clinical and patient-reported outcomes.
Characteristics of the Included Studies
The included studies were published between 1998 and 2020, with sample sizes ranging from 20 [36,99] to 3562 [102] participants and a total sample of 26,167 participants. The mean age ranged from 44 [22] to 78 [107] years, and the proportion of men varied from 25% [51] to 76% [91]. Most of the included studies were conducted in the United Kingdom (21/96, 22%) and the United States (29/96, 30%), with additional studies conducted in Belgium (2/96, 2%), Canada (4/96, 4%), Denmark (5/96, 5%), Poland (2/96, 2%), Singapore (2/96, 2%), South Korea (2/96, 2%), Spain (9/96, 9%), Germany (4/96, 4%), and Italy (6/96, 6%; Multimedia Appendix 2 [13-109,136]). In addition, the following countries had 1% (1/96) of the studies each: Australia [37], China [99], Finland [106], Greece [49], Hong Kong [28], Israel [14], Japan [66], Malaysia [67], the Netherlands [25], and Taiwan [29] (Multimedia Appendix 2).
Populations in the included studies comprised patients with diabetes (27/96, 28% of the studies), cardiovascular disease (stroke, atrial fibrillation, hypertension, and heart failure; 52/96, 54% of the studies), COPD (12/96, 12% of the studies), and mixed chronic conditions (diabetes, hypertension, and COPD; 5/96, 5% of the studies; Multimedia Appendix 2).
Types of Interventions
The studies varied in their design, type of telemonitoring system used, and method of delivery (Multimedia Appendix 2). Most (64/96, 67%) were RCTs, with 4% (4/96) being nonrandomized controlled studies, 2% (2/96) being cluster randomized studies, 10% (10/96) being longitudinal studies, 4% (4/96) being retrospective analyses, 3% (3/96) being pre-post analyses, and 9% (9/96) having a mixed methods or qualitative design. Most studies (88/96, 92%) used telemonitoring systems that collected patient information via computers, tablets, or dedicated devices (eg, modem) and transferred these data to a web-based server. Some studies collected patient data via SMS text message (3/96, 3%) or by telephone (4/96, 4%). A total of 4% (4/96) of the studies provided educational videos to increase the patients’ knowledge of the disease. The length of the intervention was highly variable, with 5% (5/96) of the studies assessing it over a short period (7-45 days), 21% (20/96) assessing it over a 2- to 4-month period, and most interventions (76/96, 79%) lasting 6 to 12 months. The follow-up periods were inconsistent among the studies and, where present, ranged from 3 to 18 months.
Types of Comparators
Most studies (79/96, 82%) compared the intervention with usual care, which consisted of routine visits (outpatient clinics) and in-person consultations with general practitioners or the hospital care team (Multimedia Appendix 2). A total of 10% (10/96) of the studies did not have a control group. A total of 1% (1/96) of the studies asked the control group to manually record their data in a diary. In total, 2% (2/96) of the studies used educational videos in the control group to improve patients’ knowledge of the disease, another 2% (2/96) compared the intervention with another telemonitoring device, and 1% (1/96) compared the intervention (telemonitoring device) with telephone communication. A total of 1% (1/96) of the studies used a similar intervention as the control group comparing patients with and without heart failure.
Types of Outcomes
In total, 12 studies reported adherence to the intervention, including 9 (75%) in patients with cardiovascular disease, 2 (17%) in patients with diabetes, and 1 (8%) in patients with COPD (Multimedia Appendix 2). Patient satisfaction with the intervention was assessed in 9% (9/96) of the studies (2/9, 22% in patients with cardiovascular disease; 3/9, 33% in patients with diabetes; 2/9, 22% in patients with COPD; and 2/9, 22% in a mixed population; Multimedia Appendix 2).
Most studies (31/96, 32%) reported changes in physiological parameters, which varied depending on the population observed, with 39% (12/31) of these studies reporting BP values for patients with cardiovascular disease, 55% (17/31) reporting HbA1c values for patients with diabetes, and 6% (2/31) reporting multiple physiological values in mixed populations (Multimedia Appendix 2).
Hospital admission during the intervention was recorded in 29% (28/96) of the studies (21/28, 75% in patients with cardiovascular disease; 4/28, 14% in patients with COPD; and 3/28, 11% in a mixed sample), and death was noted in 18% (17/96) of the studies (14/17, 82% in patients with cardiovascular disease; 2/17, 12% in patients with COPD; and 1/17, 6% in a mixed population; Multimedia Appendix 2).
QoL before and after the intervention was recorded in 22% (21/96) of the studies (11/21, 52% in patients with cardiovascular disease; 2/21, 10% in patients with diabetes; 6/21, 29% in patients with COPD; and 2/21, 10% in a mixed population; Multimedia Appendix 2).
Excluded Studies
A total of 25% (32/128) of the studies assessed for eligibility [110-141] were excluded. A summary of these studies can be found in Table S2 in Multimedia Appendix 1. Most (18/32, 56%) were excluded as they were not related to a telemonitoring intervention, 6% (2/32) included disease populations not covered in this review, 31% (10/32) reported outcomes outside the scope of this review, 3% (1/32) were literature reviews, and 3% (1/32) were study protocols.
Risk of Bias Assessment
A summary of the risk of bias assessment of the included studies can be found in Tables S3-S5 in Multimedia Appendix 1. Overall, most RCTs (48/66, 73%) and non-RCTs (17/20, 85%) included in this review showed either some concerns or a high risk of bias. Most RCT studies (45/66, 68%) showed either some concerns or a high risk of bias in the randomization process as well as in the selection of the reported results. Some RCTs (18/66, 27%) showed either some concerns or a high risk of bias in missing outcome data. Few RCTs (17/66, 26%) showed either some concerns or a high risk of bias in the measurement of the outcomes.
Most of the non-RCTs (18/20, 90%) showed either some concerns or a high risk of bias in the bias due to confounding category. A total of 50% (10/20) of the studies showed either some concerns or a high risk of bias in the bias in measurement of outcomes category. Few of the non-RCTs (9/20, 45%) showed either some concerns or a high risk of bias in the bias due to missing data category as well as in the bias due to deviations from the intended intervention category.
The studies included in the meta-analyses were assessed for publication bias. Funnel plots and Egger tests were performed only where ≥10 studies were available [167].
Funnel plots for the outcomes of systolic BP (SBP), HbA1c, and mortality can be found in Figures S1-S6 in Multimedia Appendix 1. The Egger test results revealed no evidence of publication bias for SBP, HbA1c, or mortality.
Ongoing Studies
The database search did not return any protocols for ongoing studies. Searches on ClinicalTrials.gov (updated to February 5, 2021) identified 22 ongoing studies [142-163] (n=14, 64% on patients with cardiovascular disease; n=4, 18% on patients with diabetes; and n=4, 18% on patients with COPD), which are reported in detail in Table S6 in Multimedia Appendix 1.
Primary Outcomes
Adherence
Adherence was assessed in 12 studies at different time points: 1 month (n=3, 25%) [51,66,84], 6 weeks (n=2, 17%) [58,103], 2 months (n=1, 8%) [13], 3 months (n=1, 8%) [30], 6 months (n=4, 33%) [42,48,59,92], and 12 months (n=1, 8%) [36]. Of the 12 studies, 7 (58%) [13,36,42,48,58,59,92] demonstrated a benefit of telemonitoring on patient adherence when compared with a comparator, whereas 4 (33%) [30,51,66,84] showed no difference when compared with a comparator. A total of 8% (1/12) of the studies [103] compared 2 telemonitoring systems and showed that educational support combined with telemonitoring positively influenced adherence compared with telemonitoring alone. Owing to variations in how adherence was defined in the studies, a meta-analysis was not performed. A summary of these studies is presented in Table 1.
Table 1.
Studies examining the impact of telemonitoring interventions versus comparator on adherence (N=12).
| Study type and authors, year, and country | Study population, N | Condition | Intervention type, number of participants, age (years), men (n [%]) | Comparator, number of participants, age (years), mean (n [%]) | Outcomes | Follow-up | Impact of telemonitoring | ||||||
| Randomized controlled trials | |||||||||||||
|
|
Ong et al [84], 2016, United States | 1437 | CHFa | Automated upload of data on dedicated device or software, 715, mean 73 (SD not reported), men: 382 (53.4); women: 333 (46.6) | Usual care, 722, mean 73 (SD not reported), men: 382 (53.4); women: 333 (46.6) | Adherence electronically recorded; 82.7% | 1 month | =b | |||||
|
|
Gallagher et al [51], 2017, United States | 40 | HFc | Manual upload of data on dedicated device or software, 20, median 68 (IQR 49-79), men: 15 (75); women: 5 (25) | Usual care, 20, median 62 (IQR 52-75), men: 15 (75); women: 5 (25) | Adherence recorded electronically; 81% in both groups | 1 month | = | |||||
|
|
Kotooka et al [66], 2018, Japan | 183 | CHF | Automated upload of data on dedicated device or software, 93, mean 67.1 (SD 12.8), men: 51 (56); women: 39 (44) | Usual care, 91, mean 65.4 (SD 15.6), men: 56 (61); women: 35 (39) | Adherence recorded electronically; 90% at 12 months | 12 months | = | |||||
|
|
Varon et al [103], 2015, United Kingdom | 534 | HF | Docobo system (telemonitoring only), 135, mean 69.1 (SD 12.6), not reported | Motiva system (telemonitoring+ educational videos), 399, mean 69.1 (SD 12.6), not reported | Adherence assessed by the amount of missing data during the telemonitoring period | 6 weeks | −d | |||||
|
|
Kardas et al [58], 2016, Poland | 60 | Type 2 diabetes | Automated upload of data on dedicated device or software, 30, mean 59.9 (SD 5.31), men: 17 (57); women: 13 (43) | Usual care, 30, mean 59 (SD 8.9), men: 19 (63); women: 11 (47) | Adherence expressed as medication taken vs medication prescribed; 92.9% | 6 weeks | +e | |||||
|
|
Cho et al [30], 2009, South Korea | 69 | Type 2 diabetes | Mobile app, 35, mean 51.1 (SD 13.1), 26 men; 74 womenf | Web-based telemonitoring system, 34, mean 51.1 (SD 13.1), 26 men; 74 womenf | Adherence, self-reported; >70% in both groups | 3 months | = | |||||
|
|
Seto et al [92], 2012, Canada | 100 | CHF | Automated upload of data on dedicated device or software, 50, mean 55.1 (SD 13.7), men: 41 (82); women: 9 (18) | Usual care, 50, mean 52.3 (SD 13.7), men: 38 (76); women: 12 (24) | Adherence registered electronically; 80% | 6 months | + | |||||
|
|
Evans et al [48], 2016, United States | 441 | HF and healthy | Disease group: automated upload of data on dedicated device or software, 421, mean 71.8 (SD 8.8), 46 men; 54 womenf | Healthy group: automated upload of data on dedicated device or software, 20, mean 72.2 (SD 4.3), 50 men; 50 womenf | Adherence checking the amount of data against the participants’ time spent in the study; between 71% and 81% | 6 months | + | |||||
| Nonrandomized studies | |||||||||||||
|
|
Agboola et al [13], 2013, United States | 30 | Hypertension | Web-based device, 15, mean 61.9 (SD not reported), 20 men; 80 womenf | Mobile blood pressure device, 15, mean 61.6 (SD not reported), 20 men; 80 womenf | Adherence recorded electronically based on frequency of data transmission | 2 months | + | |||||
|
|
Domingo et al [42], 2012, Spain | 97 | HF | Automated upload of data on dedicated device or software, 46, mean 66.5 (SD 11.5), men: 14 (30); women: 32 (70) | Usual care, 51, mean 66.5 (SD 11.5), men: 15 (30); women: 36 (70) | Adherence based on the number of educational videos watched; between 67% and 85% | 6 months | + | |||||
|
|
Karg et al [59], 2012, Germany | 36 | COPDg | Automated upload of data on dedicated device or software, 36, mean 67.9 (SD 6.9), men: 27 (75); women: 9 (25) | N/Ah | Adherence: use of the device for at least two-thirds of working days; full compliance | 6 months | + | |||||
|
|
De Lusignan et al [36], 2001, United Kingdom | 20 | CHF | Manual upload of data on dedicated device or software, 10, mean 75.2 (SD not reported), not reported | Usual care, 10, mean 75.2 (SD not reported), not reported | Adherence based on the frequency of the uploaded data; 90% | 12 months | + | |||||
aCHF: congestive heart failure.
bNo differences between telemonitoring and usual care.
cHF: heart failure.
dNegative impact of telemonitoring over comparator.
ePositive impact of telemonitoring over comparator.
fAbsolute value not reported in the paper.
gCOPD: chronic obstructive pulmonary disease.
hN/A: not applicable.
Satisfaction
Patient satisfaction with the intervention was assessed in 9 studies (n=2, 22% in patients with cardiovascular disease; n=3, 33% in patients with diabetes; n=2, 22% in patients with COPD; and n=2, 22% in a mixed population; Table 2). A total of 56% (5/9) of the studies [22,28,42,78,91] demonstrated a benefit of telemonitoring on patient satisfaction when compared with a comparator, whereas 44% (4/9) [30,43,44,95] showed no difference when compared with a comparator. Owing to variations in how satisfaction was defined in the studies, a meta-analysis was not performed. A summary of these studies is provided in Table 2.
Table 2.
Studies examining the impact of telemonitoring interventions versus comparator on satisfaction (N=9).
| Study type and authors, year, and country | Study population, N | Condition | Intervention type, number of participants, age (years), mean (n [%]) | Comparator, number of participants, age (years), mean (n [%]) | Outcomes | Follow-up | Impact of telemonitoring | |
| Randomized controlled trials | ||||||||
|
|
Bergenstal et al [22], 2005, United States | 47 | Type 2 diabetes | Automated data transmitted via modem, 24, mean 44 (SD 17), 37 men; 63 womena | Data transmitted via telephone, 23, mean 45 (SD 13), 39 men; 61 womena | Satisfaction: 5-point questionnaire; 4.30 in the phone group and 4.52 in the modem group | 4 weeks | =b |
|
|
Chau et al [28], 2012, Hong Kong | 40 | COPDc | Manual upload of data on dedicated device or software, 22, mean 73.5 (SD 6), men: 21 (95); women: 1 (5) | Usual care, 18, mean 72.2 (SD 6), men: 18 (100); women: 0 (0) | Satisfaction: 10-item questionnaire based on a 5-point system; 91% | 2 months | +d |
|
|
Edmonds et al [44], 1998, Canada | 35 | Type 2 diabetes | Mobile phone data transmission, 16, not reported, not reported | Usual care, 19, not reported, not reported | Satisfaction: patient questionnaire | 3 months | Further studies required |
|
|
Cho et al [30], 2009, South Korea | 69 | Type 2 diabetes | Mobile app, 35, mean 51.1 (SD 13.1), 26 men; 74 womena | Web-based telemonitoring system, 34, mean 51.1 (SD 13.1), 26 men; 74 womena | Satisfaction: questionnaire, internet vs phone; 81% vs 79%, respectively | 3 months | = |
|
|
Sicotte et al [95], 2011, Canada | 46 | COPD | Manual upload of data on dedicated device or software, 23, mean 73.7 (SD 9.6), men: 13 (56); women: 10 (44) | Usual care, 23, mean 75.4 (SD 9.7), men: 13 (56); women: 10 (44) | Satisfaction: 5-point questionnaire; 4.50 score | 3 months | = |
|
|
Domingo et al [42], 2012, Spain | 97 | HFe | Automated upload of data on dedicated device or software, 46, mean 66.5 (SD 11.5), men: 14 (30); women: 32 (70) | Usual care, 51, mean 66.5 (SD 11.5), men: 15 (30); women: 36 (70) | Satisfaction: 10-point questionnaire; 8.4 score | 6 months | + |
| Nonrandomized studies | ||||||||
|
|
Schoenfeld et al [91], 2004, United States | 59 | CHFf | Manual upload of data on dedicated device or software, 59, mean 64 (SD 14), men: 45 (76); women: 14 (24) | N/Ag | Satisfaction: 3-point questionnaire; 98.1% indicating ease of use of the device | 7 days | + |
|
|
Donate-Martinez et al [43], 2016, Spain | 74 | Chronic conditions (COPD, type 2 diabetes, and HF) | Manual upload of data on dedicated device or software, 74, mean 67.95 (SD 11.14), men: 49 (66); women: 25 (44) | N/A | Satisfaction: 11-item questionnaire with 10-point score; 8.63 score overall | 12 months | = |
|
|
Mira-Solves et al [77], 2014, Spain | 410 | Chronic conditions (type 2 diabetes, hypertension, CHF, and COPD) | Automated upload of data on dedicated device or software, 410, not reported, 64 men; 36 womena | N/A | Satisfaction: questionnaire, 89.4% were satisfied with the ease of use. | 24 months | + |
aAbsolute value not reported in the paper.
bNo differences between telemonitoring and usual care.
cCOPD: chronic obstructive pulmonary disease.
dPositive impact of telemonitoring over comparator.
eHF: heart failure.
fCHF: congestive HF.
gN/A: not applicable.
Secondary Outcomes
QoL Measurement
Studies included in the meta-analyses were pooled by comparable scales (eg, the Short Form 36 Health Survey Questionnaire) and end points (eg, 6 or 12 months), with 8% (8/96) of the studies [16,31,33,35,47,96,101,104] included in the meta-analyses.
A total of 50% (4/8) of these studies [16,31,35,104] reported the Short Form 36 Health Survey Questionnaire scores (mental and physical) at comparable end points (12 months) and were included in the meta-analyses (Figure 2 [15,31,35,47,96,101,104,136], subgroups 1.9.3 and 1.9.4). From the meta-analysis, telemonitoring showed greater improvements compared with usual care on physical component scores (weighted MD=3.72, 95% CI 1.73-5.70; P<.001; I2=51%; Figure 2) compared with the comparator but no difference in mental component scores (weighted MD=1.06, 95% CI −0.12 to 2.25; P=.08; I2=0%; Figure 3 [15,39,40,50,60,64,84,96,101,105,107]).
Figure 2.
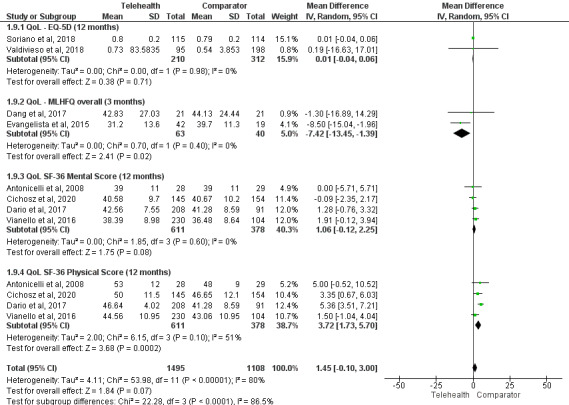
Impact of telemonitoring versus comparator on quality of life (QoL). 1.9.1: EQ-5D; 1.9.2: Minnesota Living with Heart Failure Questionnaire (MLHFQ); 1.9.3: SF-36 mental score; and 1.9.4: SF-36 physical component [15,31,35,47,96,101,104,136].
Figure 3.
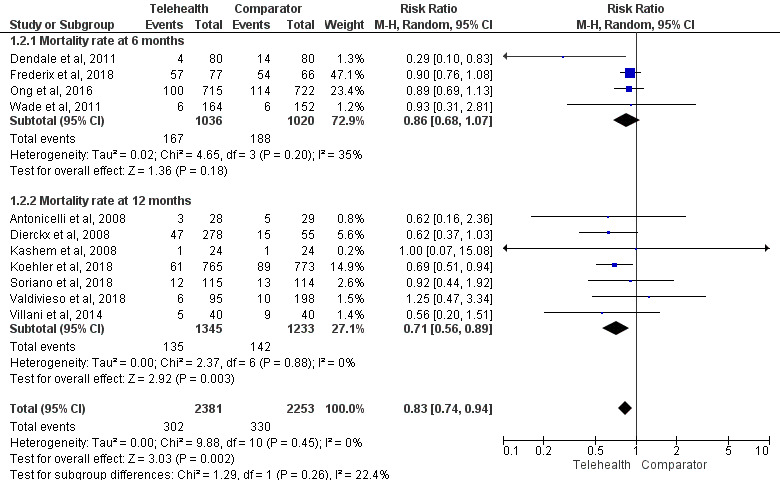
Impact of telemonitoring versus comparator on the mortality rate at 6 and 12 months. The study by Mortara et al [80] was not included in the mortality meta-analyses because of the use of a composite outcome of mortality and hospitalization where absolute mortality results were not available. The study by Seto et al [92] was not included in the mortality meta-analyses because of 0 events in the control group [15,39,40,50,60,64,84,96,101,105,107].
In total, 25% (2/8) of the studies [96,101] reported EQ-5D scores at comparable end points (12 months) and were included in the meta-analysis (Figure 2, subgroup 1.9.1). There was no difference in QoL between the groups (weighted MD=0.01, 95% CI −0.04 to 0.06; P=.71; I2=0%)
A total of 25% (2/8) of the studies [33,47] using the Minnesota Living with Heart Failure Questionnaire overall scores at 3 months were included in the meta-analysis (Figure 2, subgroup 1.9.2), demonstrating that the telemonitoring group showed greater improvements in QoL (weighted MD=−7.42, 95% CI −13.45 to −1.39; P=.02; I2=0%) compared with the comparator.
A total of 14% (13/96) of the studies [20,23,36,43,58,62,65,70,92,100,103,107,108] could not be included in the meta-analysis because they reported different time points and used different questionnaires to assess QoL. Of these 13 studies, 4 (31%) reported a significant improvement in QoL in the telemonitoring group compared with usual care at 6 weeks [58], 6 months [92,100], and 12 months [43] measured using a variety of questionnaires (Minnesota Living with Heart Failure Questionnaire [92], EQ-5D [43,58], and 15D [100]), whereas 9 (69%) reported no difference in QoL between telemonitoring and usual care at 4 weeks [70], 6 weeks [65,103], 7 weeks [70], 3 months [36], 6 months [23,62,107], 9 months [108], and 12 months [36]. A total of 8% (1/13) of the studies [20] reported significant improvement in QoL in the usual care group compared with telemonitoring at 2 and 6 months using the St George’s Respiratory Questionnaire.
Mortality
Meta-analyses for mortality were conducted at the 6- and 12-month follow-up (Figure 3). Sensitivity analyses were conducted at the 6- and 12-month follow-up excluding studies at high risk of bias and at 12 months excluding non-RCTs (Figure S1 in Multimedia Appendix 1). A sensitivity analysis with the exclusion of non-RCTs at 6 months was not conducted as all the studies included were RCTs.
A total of 11 studies contributed to the all-cause mortality meta-analysis: 4 (36%) [39,50,84,107] (N=2056) provided data at 6 months, and 7 (64%) [16,40,61,64,96,101,105] (N=2578) provided data at 12 months. There was no significant difference in all-cause mortality between telemonitoring and the comparator at 6 months (risk ratio [RR]=0.86, 95% CI 0.68-1.07; P=.18; I2=35%; Figure 3). This finding was consistent when studies evaluated as having a high risk of bias were excluded (Figure S1 in Multimedia Appendix 1). There was a significantly lower risk of all-cause mortality with telemonitoring than with the comparator at 12 months (RR=0.71, 95% CI 0.56-0.89; P=.003; I2=0%; Figure 3). This finding was consistent following the exclusion of non-RCTs and studies evaluated as having a high risk of bias (Figure S1 in Multimedia Appendix 1).
Hospitalization
Meta-analyses for hospitalization at the 6- and 12-month follow-up were conducted (Figure 4 [23,25,34,52,80,83]), with sensitivity analyses excluding studies classified as having a high risk of bias (Figure S2 in Multimedia Appendix 1) and a subgroup analysis including only studies on patients with heart failure (12/96, 12%). Subgroup analyses for studies on patients with COPD and multiple chronic conditions were not possible because of a lack of absolute values or comparator [29,85].
Figure 4.
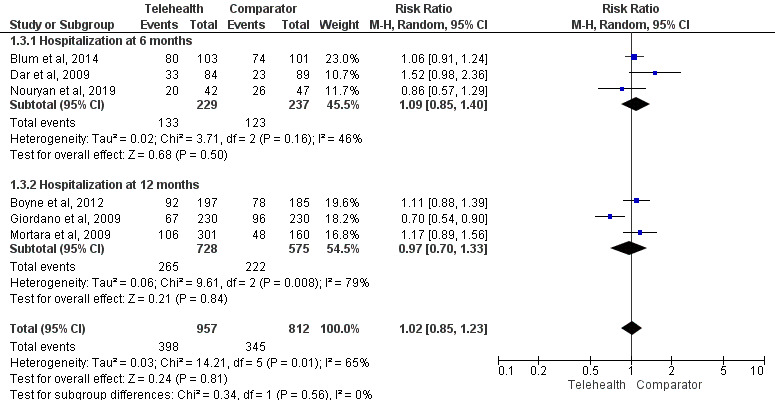
Impact of telemonitoring versus comparator on hospitalization at 6 and 12 months [23,25,34,52,80,83].
A total of 8 studies contributed to the all-cause hospitalization meta-analyses: 3 (38%) [23,34,83] (n=466) provided data at 6 months, and 5 (62%) [25,52,80,96,101] (n=1825) provided data at 12 months. There was no significant difference in the risk of all-cause hospitalization between the groups at 6 months (RR=1.09, 95% CI 0.85-1.40; P=.50; I2=46%) or 12 months (RR=0.97, 95% CI 0.70-1.33; P=.84; I2=79%; Figure 4). This result was also consistent after the exclusion of studies evaluated as having a high risk of bias (Figure S2 in Multimedia Appendix 1). The meta-analysis that included only patients with heart failure showed no difference in the risk of hospitalization between the telemonitoring and comparator groups (RR=0.99, 95% CI 0.81-1.22; P=.94; I2=69%; Figure S2 in Multimedia Appendix 1).
Changes in BP
A total of 10% (10/96) of the studies [16,17,24,38,45,62,72,75,77] reporting on the change in SBP and 8% (8/96) of the studies [15,17,24,45,62,72,75,77,90] reporting on the change in diastolic BP (DBP) between a telemonitoring intervention and usual care were included in the meta-analyses. Further details on the analyses of BP are provided in Multimedia Appendix 1.
Changes in SBP
SBP was significantly reduced in the telemonitoring group (n=1477) compared with that in the usual care group (n=1484; weighted MD=−5.34 mm Hg, 95% CI −7.81 to −2.86; P<.001; I2=100%; Figure 5 [15,17,24,38,45,62,72,75,77,90]). In the subgroup analysis according to study time points, similar results were observed for SBP at 6 months (weighted MD=−3.85 mm Hg, 95% CI −7.03 to −0.68; P=.02; I2=100%; Figure 5) and 12 months (weighted MD=−3.85 mm Hg, 95% CI −7.03 to −0.68; P=.02; I2=100%; Figure S3 in Multimedia Appendix 1) in favor of telemonitoring.
Figure 5.
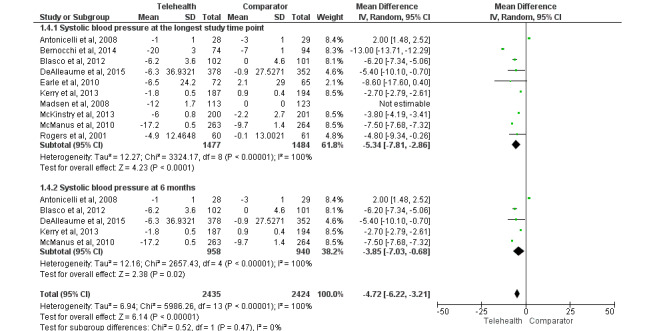
Impact of telemonitoring versus usual care on changes in systolic blood pressure (mean difference) at the longest study time point and at 6 months [15,17,24,38,45,62,72,75,77,90].
The sensitivity analysis, excluding studies where the SD was not reported directly [38,45,90], did not materially change the results (weighted MD=−5.19 mm Hg, 95% CI −8.01 to −2.37; P<.001; I2=100%; Figure S3 in Multimedia Appendix 1). The sensitivity analysis was also performed excluding studies with a high risk of bias (Figure S3 in Multimedia Appendix 1); the results remained in favor of telemonitoring (weighted MD=–2.84 mm Hg, 95% CI −4.22 to −1.46; P<.001; I2=98%).
Changes in DBP
A meta-analysis including the longest time point demonstrated a significant reduction in DBP in favor of telemonitoring (n=1218) compared with the comparator (n=1255; weighted MD=−2.83 mm Hg, 95% CI −3.98 to −1.68; P<.001; I2=99%; Figure S4 in Multimedia Appendix 1). In the subgroup analysis, a similar result was observed for DBP reduction at 6 months (weighted MD=−5.44 mm Hg, 95% CI −9.00 to −1.87; P=.003; I2=100%; Figure S4 in Multimedia Appendix 1) in favor of telemonitoring but not for DBP at 12 months (weighted MD=−1.09 mm Hg, 95% CI −4.76 to 2.57; P=.56; I2=97%; Figure S4 in Multimedia Appendix 1). Sensitivity analyses at the longest time point excluding studies with high risk of bias (Figure S4 in Multimedia Appendix 1) showed no significant reduction in DBP in the telemonitoring group (weighted MD=−1.07 mm Hg, 95% CI −2.58 to 0.44; P=.16; I2=98%) compared with usual care.
Changes in HbA1c
A total of 19% (18/96) of the studies reported on HbA1c, and all the studies (18/18, 100%) compared telemonitoring with usual care, with 61% (11/18; n=3277) included in the meta-analysis [27,30,35,46,49,58,63,87,89,94,109]. Further details on the excluded studies for the meta-analysis are provided in Multimedia Appendix 1.
The duration of the interval before and after varied, with 18% (2/11) of these studies reporting a 6-week assessment [58,87], 45% (5/11) [27,30,46,49,63] reporting 3-month assessments, 9% (1/11) reporting 9-month assessments [109], and 27% (3/11) [35,89] reporting 12-month assessments. A sensitivity analysis was performed excluding studies with a high risk of bias [58,94].
The overall mean change in HbA1c is shown in Figure S5 in Multimedia Appendix 1. The pooled estimate showed a reduction in the mean change in HbA1c in the telemonitoring group (n=1703; weighted MD=−0.33, 95% CI −0.57 to −0.09; P=.008; I2=99%; Figure S5 in Multimedia Appendix 1). The results did not materially change after the sensitivity analysis excluding studies at high risk of bias [58,87] (Figure S5 in Multimedia Appendix 1). Subgroup analyses according to study time points showed no significant difference in the change in HbA1c values between telemonitoring and the comparator (Figure S5 in Multimedia Appendix 1).
Discussion
Principal Findings
Our results suggest that telemonitoring interventions are associated with good patient adherence and satisfaction. Although this review did not demonstrate improvements in QoL with telemonitoring, there was evidence to suggest reductions in all-cause mortality and improvements in BP and blood glucose control. Conversely, there was evidence to suggest that telemonitoring interventions may be associated with a higher rate of hospitalizations, which could be interpreted as a positive role of telemonitoring in detecting patients’ health issues more than usual care.
Comparison With Prior Work
Our review showed improvements in physiological parameters (BP and blood glucose) in patients receiving telemonitoring interventions. These findings demonstrate the positive role of telemonitoring in improving patients’ self-management of their conditions. This is in line with other reviews that have shown similar improvements in hypertension [168] and type 2 diabetes self-management [169] after telemonitoring interventions.
The studies included in this review consistently showed that patients receiving telemonitoring interventions had lower all-cause mortality compared with patients receiving usual care. A recent umbrella review [170] examining the effects of telemonitoring on mortality in several clinical populations (cardiovascular, COPD, and neurological) reported similar findings for the cardiovascular population, where the mortality rate was either reduced in the telemedicine users or remained unchanged compared with usual care. The same review [170] did not find any difference in mortality between telemonitoring and usual care in patients with COPD. The impact on death is an important outcome when considering the administration of remote interventions over in-person visits, and the reduced mortality rate with telemonitoring reported in our review suggests the effectiveness of telemonitoring for patients with chronic conditions.
Surprisingly, the overall results of our review showed a higher risk of hospitalization among patients undergoing telemonitoring interventions. There is inconsistency in the previous literature on the role that telemonitoring plays in reducing the risk of rehospitalization, with some studies reporting no differences compared with usual care [171] and others concluding that telemonitoring is an effective tool to reduce all-cause hospitalization in adults with heart failure [172]. Thurmond et al [173] noted the importance that the type of telemonitoring intervention has on its acceptability by patients and, consequently, their adherence to it, which, when poor, may influence the rate of rehospitalization. This would suggest the need to identify common characteristics of effective telemonitoring interventions (or “active ingredients”) that facilitate patient acceptability. It may also be possible that increased hospitalizations with telemonitoring is a positive finding (ie, reasons for hospitalization may be identified earlier by telemonitoring, and hospitalization may be initiated earlier than with usual care, averting serious outcomes and death). Hypothetically, this could have contributed to the reduced mortality at 12 months; however, future research is needed to substantiate this.
The results of this review are in line with those of previous systematic reviews assessing patient satisfaction with telemonitoring interventions [174,175]. From qualitative reports, the convenience of decreased travel time and costs and the reassurance of being monitored are the most likely reasons for patients preferring telemonitoring over usual care [176]. It is important to note that patient satisfaction may differ with the type of telemonitoring device used; indeed, available evidence suggests that higher patient satisfaction is reported for videoconferences and devices that allow for automated data transmission [174].
The included studies did not report significant improvements in the QoL of patients receiving a telemonitoring intervention compared with usual care. Our findings confirm previous reviews [177,178] while expanding the results to populations outside care homes [178] and including study designs other than RCTs [177]. Although telemonitoring does not seem to improve QoL compared with usual care, previous findings [178] have shown important benefits of telemonitoring in improving patients’ confidence in accessing health care services.
Strengths and Limitations
This review used a strict definition of telemonitoring, only including studies that used a device to collect health measures and facilitated 2-way communication or action between the patient and health care team. Despite the inclusion of studies with low methodological quality, sensitivity analyses were conducted where appropriate, reducing the potential for bias to affect the results of this review. The studies included in this review presented a wide range of telemonitoring interventions that differed in the personnel involved, administration of the intervention, and technology used and that were examined in a variety of populations with different long-term conditions, thus making the results highly generalizable. A robust methodology was used, with independent screening and data extraction by 2 reviewers and risk of bias assessment in duplicate.
Several limitations are noteworthy. First, despite our initial plans to investigate uptake, patient retention and satisfaction, and associated factors when using 2-way (patient-health care provider) remote patient monitoring devices to manage chronic health conditions, no studies reported uptake and retention outcomes and, therefore, these outcomes could not be reported in this review. Most of the included studies assessed similar outcomes but used different measurement tools, thus making comparison difficult, particularly in studies investigating patient adherence [13,30,36,42,48,51,58,59,66,84,92,103] and satisfaction [22,28,30,42-44,78,91,95] with the intervention. Second, despite our efforts to define the best search strategy to identify all relevant articles for our review, the possible omission of papers because of the heterogeneity in the key terms used by the authors cannot be ruled out. We did not conduct any searches for gray literature. Third, most outcomes analyzed in this review have been infrequently investigated in the literature (eg, mortality was reported only in 17/96, 18% of the included studies; adherence was reported in only 12/96, 12% of the studies; and satisfaction was reported in only 9/96, 9% of the studies), and further research is required to properly assess the effects of telemonitoring on these outcomes. Moreover, some conditions (eg, COPD) were underrepresented as few studies investigating the effects of telemonitoring interventions on these populations were available; thus, we could not conduct a separate meta-analysis for each condition. The type and quality of usual care also varied throughout the included studies, which may have influenced the results in favor of or against telemonitoring.
Conclusions
Telemonitoring is a promising tool to manage long-term conditions, with the potential to reduce the associated costs and alleviate patient difficulties in accessing primary health care. Patient satisfaction and adherence to telemonitoring appear, overall, to be promising. Although telemonitoring resulted in improvement in physiological parameters and reduced all-cause mortality compared with usual care, there was no improvement in QoL and an increased risk of hospitalization with telemonitoring. Although the latter may be a positive finding indicating earlier detection of health issues and action (resulting in hospitalization), this result warrants further investigation. Telemonitoring is expanding rapidly, more so since the COVID-19 pandemic, and has been shown to be a viable alternative to usual care for the management of patients with long-term health conditions.
Acknowledgments
The authors would like to thank all the Telehealth and Artificial Intelligence for Older People (TAILOR) investigators: Dr Asan Akpan, Dr Girvan Burnside (University of Liverpool), Mr Robert Halhead, Mr Stephen Hope, Mr Peter Levene, Mr Geoff Hayllar (Docobo Ltd, Leatherhead, United Kingdom), Mr Peter Almond (Mersey Care National Health Service Trust), Ms Sarah Dyas (Clinical Research Network, North West Coast), and Ms Lindsay Sharples (Innovation Agency). The authors would also like to thank Dr Marie Held (University of Liverpool) for her help in translating some of the included papers from German to English. This project has received funding from the Liverpool Clinical Commissioning Group, Research Capability Funding (LCCG_RCF20-21_01).
Abbreviations
- BP
blood pressure
- COPD
chronic obstructive pulmonary disease
- DBP
diastolic blood pressure
- HbA1c
glycated hemoglobin
- MD
mean difference
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO
International Prospective Register of Systematic Reviews
- QoL
quality of life
- RCT
randomized controlled trial
- RR
risk ratio
- SBP
systolic blood pressure
Supplementary figures and tables that were not included in the main manuscript.
Summary of the included studies (N=96).
Footnotes
Conflicts of Interest: BJRB has received research funding from the Bristol Myers Squibb (BMS)-Pfizer Alliance. SLH has received an investigator-initiated grant from BMS. GYHL has been a consultant and speaker for the BMS-Pfizer Alliance, Boehringer Ingelheim, and Daiichi-Sankyo. No fees were received personally. DJW has been a consultant and speaker for Medtronic and Boston Scientific. DAL has received investigator-initiated educational grants from BMS; been a speaker for Boehringer Ingelheim, Bayer, and the BMS-Pfizer Alliance; and consulted for Boehringer Ingelheim, Bayer, and the BMS-Pfizer Alliance, all outside the submitted work.
References
- 1.Goodwin N, Sonola L, Thiel V, Kodner D. Co-ordinated care for people with complex chronic conditions: key lessons and markers for success. The King's Fund. 2013. [2021-10-01]. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/co-ordinated-care-for-people-with-complex-chronic-conditions-kingsfund-oct13.pdf .
- 2.Masnoon N, Kalisch Ellett L, Shakib S, Caughey GE. Predictors of mortality in the older population: the role of polypharmacy and other medication and chronic disease-related factors. Drugs Aging. 2020 Oct;37(10):767–76. doi: 10.1007/s40266-020-00794-7.10.1007/s40266-020-00794-7 [DOI] [PubMed] [Google Scholar]
- 3.Tyack Z, Frakes KA, Barnett A, Cornwell P, Kuys S, McPhail S. Predictors of health-related quality of life in people with a complex chronic disease including multimorbidity: a longitudinal cohort study. Qual Life Res. 2016 Oct;25(10):2579–92. doi: 10.1007/s11136-016-1282-x.10.1007/s11136-016-1282-x [DOI] [PubMed] [Google Scholar]
- 4.Noncommunicable diseases. World Health Organization. 2021. Apr 13, [2022-04-01]. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases .
- 5.Coulter A, Roberts S, Dixon A. Delivering better services for people with long-term conditions: building the house of care. The King's Fund. 2013. Oct, [2021-10-01]. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf .
- 6.How to deliver high-quality, patient-centred, cost-effective care: consensus solutions from the voluntary sector. The King's Fund. 2010. [2021-10-01]. https://www.kingsfund.org.uk/sites/default/files/how-to-deliver-high-quality-patient-centred-cost-effective-care-16-september-2010-kings-fund.pdf .
- 7.Topriceanu CC, Wong A, Moon JC, Hughes AD, Bann D, Chaturvedi N, Patalay P, Conti G, Captur G. Evaluating access to health and care services during lockdown by the COVID-19 survey in five UK national longitudinal studies. BMJ Open. 2021 Mar 18;11(3):e045813. doi: 10.1136/bmjopen-2020-045813. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33737441 .bmjopen-2020-045813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salisbury C, Thomas C, O'Cathain A, Rogers A, Pope C, Yardley L, Hollinghurst S, Fahey T, Lewis G, Large S, Edwards L, Rowsell A, Segar J, Brownsell S, Montgomery AA. TElehealth in CHronic disease: mixed-methods study to develop the TECH conceptual model for intervention design and evaluation. BMJ Open. 2015 Feb 06;5(2):e006448. doi: 10.1136/bmjopen-2014-006448. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=25659890 .bmjopen-2014-006448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvarez P, Sianis A, Brown J, Ali A, Briasoulis A. Chronic disease management in heart failure: focus on telemedicine and remote monitoring. Rev Cardiovasc Med. 2021 Jun 30;22(2):403–13. doi: 10.31083/j.rcm2202046. https://www.imrpress.com/journal/RCM/22/2/10.31083/j.rcm2202046 .1625013559951-898126196 [DOI] [PubMed] [Google Scholar]
- 10.Eze ND, Mateus C, Cravo Oliveira Hashiguchi T. Telemedicine in the OECD: an umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One. 2020 Aug 13;15(8):e0237585. doi: 10.1371/journal.pone.0237585. https://dx.plos.org/10.1371/journal.pone.0237585 .PONE-D-20-02481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Snoswell CL, Chelberg G, De Guzman KR, Haydon HH, Thomas EE, Caffery LJ, Smith AC. The clinical effectiveness of telehealth: a systematic review of meta-analyses from 2010 to 2019. J Telemed Telecare (forthcoming) 2021 Jun 29;:1357633X211022907. doi: 10.1177/1357633X211022907. [DOI] [PubMed] [Google Scholar]
- 12.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agboola S, Havasy R, Myint-U K, Kvedar J, Jethwani K. The impact of using mobile-enabled devices on patient engagement in remote monitoring programs. J Diabetes Sci Technol. 2013 May 01;7(3):623–9. doi: 10.1177/193229681300700306. https://europepmc.org/abstract/MED/23759394 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amir O, Ben-Gal T, Weinstein JM, Schliamser J, Burkhoff D, Abbo A, Abraham WT. Evaluation of remote dielectric sensing (ReDS) technology-guided therapy for decreasing heart failure re-hospitalizations. Int J Cardiol. 2017 Aug 01;240:279–84. doi: 10.1016/j.ijcard.2017.02.120. https://linkinghub.elsevier.com/retrieve/pii/S0167-5273(16)32225-2 .S0167-5273(16)32225-2 [DOI] [PubMed] [Google Scholar]
- 15.Antonicelli R, Testarmata P, Spazzafumo L, Gagliardi C, Bilo G, Valentini M, Olivieri F, Parati G. Impact of telemonitoring at home on the management of elderly patients with congestive heart failure. J Telemed Telecare. 2008;14(6):300–5. doi: 10.1258/jtt.2008.071213.14/6/300 [DOI] [PubMed] [Google Scholar]
- 16.Antonicelli R, Mazzanti I, Abbatecola AM, Parati G. Impact of home patient telemonitoring on use of β-blockers in congestive heart failure. Drugs Aging. 2010 Oct 01;27(10):801–5. doi: 10.2165/11538210-000000000-00000.3 [DOI] [PubMed] [Google Scholar]
- 17.Bernocchi P, Scalvini S, Bertacchini F, Rivadossi F, Muiesan ML. Home based telemedicine intervention for patients with uncontrolled hypertension--a real life non-randomized study. BMC Med Inform Decis Mak. 2014 Jun 12;14:52. doi: 10.1186/1472-6947-14-52. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-14-52 .1472-6947-14-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baron JS, Hirani S, Newman SP. A randomised, controlled trial of the effects of a mobile telehealth intervention on clinical and patient-reported outcomes in people with poorly controlled diabetes. J Telemed Telecare. 2017 Feb;23(2):207–16. doi: 10.1177/1357633X16631628.1357633X16631628 [DOI] [PubMed] [Google Scholar]
- 19.Baron JS, Hirani SP, Newman SP. Investigating the behavioural effects of a mobile-phone based home telehealth intervention in people with insulin-requiring diabetes: results of a randomized controlled trial with patient interviews. J Telemed Telecare. 2017 Jun;23(5):503–12. doi: 10.1177/1357633X16655911.1357633X16655911 [DOI] [PubMed] [Google Scholar]
- 20.Bentley CL, Mountain GA, Thompson J, Fitzsimmons DA, Lowrie K, Parker SG, Hawley MS. A pilot randomised controlled trial of a Telehealth intervention in patients with chronic obstructive pulmonary disease: challenges of clinician-led data collection. Trials. 2014 Aug 06;15:313. doi: 10.1186/1745-6215-15-313. https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-15-313 .1745-6215-15-313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beran M, Asche SE, Bergdall AR, Crabtree B, Green BB, Groen SE, Klotzle KJ, Michels RD, Nyboer RA, O'Connor PJ, Pawloski PA, Rehrauer DJ, Sperl-Hillen JM, Trower NK, Margolis KL. Key components of success in a randomized trial of blood pressure telemonitoring with medication therapy management pharmacists. J Am Pharm Assoc (2003) 2018;58(6):614–21. doi: 10.1016/j.japh.2018.07.001. https://europepmc.org/abstract/MED/30077564 .S1544-3191(18)30337-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergenstal RM, Anderson RL, Bina DM, Johnson ML, Davidson JL, Solarz-Johnson B, Kendall DM. Impact of modem-transferred blood glucose data on clinician work efficiency and patient glycemic control. Diabetes Technol Ther. 2005 Apr;7(2):241–7. doi: 10.1089/dia.2005.7.241. [DOI] [PubMed] [Google Scholar]
- 23.Blum K, Gottlieb SS. The effect of a randomized trial of home telemonitoring on medical costs, 30-day readmissions, mortality, and health-related quality of life in a cohort of community-dwelling heart failure patients. J Card Fail. 2014 Jul;20(7):513–21. doi: 10.1016/j.cardfail.2014.04.016.S1071-9164(14)00176-6 [DOI] [PubMed] [Google Scholar]
- 24.Blasco A, Carmona M, Fernández-Lozano I, Salvador CH, Pascual M, Sagredo PG, Somolinos R, Muñoz A, García-López F, Escudier JM, Mingo S, Toquero J, Moñivas V, González MA, Fragua JA, López-Rodríguez F, Monteagudo JL, Alonso-Pulpón L. Evaluation of a telemedicine service for the secondary prevention of coronary artery disease. J Cardiopulm Rehabil Prev. 2012;32(1):25–31. doi: 10.1097/HCR.0b013e3182343aa7. [DOI] [PubMed] [Google Scholar]
- 25.Boyne JJ, Vrijhoef HJ, Crijns HJ, De Weerd G, Kragten J, Gorgels AP, TEHAF investigators Tailored telemonitoring in patients with heart failure: results of a multicentre randomized controlled trial. Eur J Heart Fail. 2012 Jul;14(7):791–801. doi: 10.1093/eurjhf/hfs058. doi: 10.1093/eurjhf/hfs058.hfs058 [DOI] [PubMed] [Google Scholar]
- 26.Buis LR, Roberson DN, Kadri R, Rockey NG, Plegue MA, Danak SU, Guetterman TC, Johnson MG, Choe HM, Richardson CR. Understanding the feasibility, acceptability, and efficacy of a clinical pharmacist-led mobile approach (BPTrack) to hypertension management: mixed methods pilot study. J Med Internet Res. 2020 Aug 11;22(8):e19882. doi: 10.2196/19882. https://www.jmir.org/2020/8/e19882/ v22i8e19882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bujnowska-Fedak MM, Puchała E, Steciwko A. The impact of telehome care on health status and quality of life among patients with diabetes in a primary care setting in Poland. Telemed J E Health. 2011 Apr;17(3):153–63. doi: 10.1089/tmj.2010.0113. [DOI] [PubMed] [Google Scholar]
- 28.Chau JP, Lee DT, Yu DS, Chow AY, Yu WC, Chair SY, Lai AS, Chick YL. A feasibility study to investigate the acceptability and potential effectiveness of a telecare service for older people with chronic obstructive pulmonary disease. Int J Med Inform. 2012 Oct;81(10):674–82. doi: 10.1016/j.ijmedinf.2012.06.003.S1386-5056(12)00116-5 [DOI] [PubMed] [Google Scholar]
- 29.Chen YH, Lin YH, Hung CS, Huang CC, Yeih DF, Chuang PY, Ho YL, Chen MF. Clinical outcome and cost-effectiveness of a synchronous telehealth service for seniors and nonseniors with cardiovascular diseases: quasi-experimental study. J Med Internet Res. 2013 Apr 24;15(4):e87. doi: 10.2196/jmir.2091. https://www.jmir.org/2013/4/e87/ v15i4e87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communication using a mobile phone with a glucometer for glucose control in type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. J Telemed Telecare. 2009;15(2):77–82. doi: 10.1258/jtt.2008.080412.15/2/77 [DOI] [PubMed] [Google Scholar]
- 31.Cichosz SL, Udsen FW, Hejlesen O. The impact of telehealth care on health-related quality of life of patients with heart failure: results from the Danish TeleCare North heart failure trial. J Telemed Telecare. 2020;26(7-8):452–61. doi: 10.1177/1357633X19832713. [DOI] [PubMed] [Google Scholar]
- 32.Cleland JG, Louis AA, Rigby AS, Janssens U, Balk AH, TEN-HMS Investigators Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) study. J Am Coll Cardiol. 2005 May 17;45(10):1654–64. doi: 10.1016/j.jacc.2005.01.050. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(05)00484-5 .S0735-1097(05)00484-5 [DOI] [PubMed] [Google Scholar]
- 33.Dang S, Dimmick S, Kelkar G. Evaluating the evidence base for the use of home telehealth remote monitoring in elderly with heart failure. Telemed J E Health. 2009 Oct;15(8):783–96. doi: 10.1089/tmj.2009.0028. [DOI] [PubMed] [Google Scholar]
- 34.Dar O, Riley J, Chapman C, Dubrey SW, Morris S, Rosen SD, Roughton M, Cowie MR. A randomized trial of home telemonitoring in a typical elderly heart failure population in North West London: results of the Home-HF study. Eur J Heart Fail. 2009 Mar;11(3):319–25. doi: 10.1093/eurjhf/hfn050. doi: 10.1093/eurjhf/hfn050.hfn050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dario C, Toffanin R, Calcaterra F, Saccavini C, Stafylas P, Mancin S, Vio E. Telemonitoring of type 2 diabetes mellitus in Italy. Telemed J E Health. 2017 Feb;23(2):143–52. doi: 10.1089/tmj.2015.0224. [DOI] [PubMed] [Google Scholar]
- 36.de Lusignan S, Wells S, Johnson P, Meredith K, Leatham E. Compliance and effectiveness of 1 year's home telemonitoring. The report of a pilot study of patients with chronic heart failure. Eur J Heart Fail. 2001 Dec;3(6):723–30. doi: 10.1016/s1388-9842(01)00190-8. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1388-9842&date=2001&volume=3&issue=6&spage=723 .S1388-9842(01)00190-8 [DOI] [PubMed] [Google Scholar]
- 37.De San Miguel K, Smith J, Lewin G. Telehealth remote monitoring for community-dwelling older adults with chronic obstructive pulmonary disease. Telemed J E Health. 2013 Sep;19(9):652–7. doi: 10.1089/tmj.2012.0244. [DOI] [PubMed] [Google Scholar]
- 38.DeAlleaume L, Parnes B, Zittleman L, Sutter C, Chavez R, Bernstein J, LeBlanc W, Dickinson M, Westfall JM. Success in the achieving cardiovascular excellence in Colorado (A CARE) home blood pressure monitoring program: a report from the shared networks of Colorado Ambulatory Practices and Partners (SNOCAP) J Am Board Fam Med. 2015;28(5):548–55. doi: 10.3122/jabfm.2015.05.150024. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=26355126 .28/5/548 [DOI] [PubMed] [Google Scholar]
- 39.Dendale P, De Keulenaer G, Troisfontaines P, Weytjens C, Mullens W, Elegeert I, Ector B, Houbrechts M, Willekens K, Hansen D. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail. 2012 Mar;14(3):333–40. doi: 10.1093/eurjhf/hfr144. doi: 10.1093/eurjhf/hfr144.hfr144 [DOI] [PubMed] [Google Scholar]
- 40.Dierckx R, Cleland JG, Pellicori P, Zhang J, Goode K, Putzu P, Boyalla V, Clark AL. If home telemonitoring reduces mortality in heart failure, is this just due to better guideline-based treatment? J Telemed Telecare. 2015 Sep;21(6):331–9. doi: 10.1177/1357633X15574947.1357633X15574947 [DOI] [PubMed] [Google Scholar]
- 41.Dinesen B, Haesum LK, Soerensen N, Nielsen C, Grann O, Hejlesen O, Toft E, Ehlers L. Using preventive home monitoring to reduce hospital admission rates and reduce costs: a case study of telehealth among chronic obstructive pulmonary disease patients. J Telemed Telecare. 2012 Jun;18(4):221–5. doi: 10.1258/jtt.2012.110704.jtt.2012.110704 [DOI] [PubMed] [Google Scholar]
- 42.Domingo M, Lupón J, González B, Crespo E, López R, Ramos A, Urrutia A, Pera G, Verdú JM, Bayes-Genis A. Evaluation of a telemedicine system for heart failure patients: feasibility, acceptance rate, satisfaction and changes in patient behavior: results from the CARME (CAtalan Remote Management Evaluation) study. Eur J Cardiovasc Nurs. 2012 Dec;11(4):410–8. doi: 10.1016/j.ejcnurse.2011.02.003.S1474-5151(11)00033-8 [DOI] [PubMed] [Google Scholar]
- 43.Doñate-Martínez A, Ródenas F, Garcés J. Impact of a primary-based telemonitoring programme in HRQOL, satisfaction and usefulness in a sample of older adults with chronic diseases in Valencia (Spain) Arch Gerontol Geriatr. 2016;62:169–75. doi: 10.1016/j.archger.2015.09.008.S0167-4943(15)30060-1 [DOI] [PubMed] [Google Scholar]
- 44.Edmonds M, Bauer M, Osborn S, Lutfiyya H, Mahon J, Doig G, Grundy P, Gittens C, Molenkamp G, Fenlon D. Using the Vista 350 telephone to communicate the results of home monitoring of diabetes mellitus to a central database and to provide feedback. Int J Med Inform. 1998;51(2-3):117–25. doi: 10.1016/s1386-5056(98)00109-9.S1386-5056(98)00109-9 [DOI] [PubMed] [Google Scholar]
- 45.Earle KA, Istepanian RS, Zitouni K, Sungoor A, Tang B. Mobile telemonitoring for achieving tighter targets of blood pressure control in patients with complicated diabetes: a pilot study. Diabetes Technol Ther. 2010 Jul;12(7):575–9. doi: 10.1089/dia.2009.0090. [DOI] [PubMed] [Google Scholar]
- 46.Egede LE, Williams JS, Voronca DC, Knapp RG, Fernandes JK. Randomized controlled trial of technology-assisted case management in low income adults with type 2 diabetes. Diabetes Technol Ther. 2017 Aug;19(8):476–82. doi: 10.1089/dia.2017.0006. [DOI] [PubMed] [Google Scholar]
- 47.Evangelista LS, Lee JA, Moore AA, Motie M, Ghasemzadeh H, Sarrafzadeh M, Mangione CM. Examining the effects of remote monitoring systems on activation, self-care, and quality of life in older patients with chronic heart failure. J Cardiovasc Nurs. 2015;30(1):51–7. doi: 10.1097/JCN.0000000000000110. https://europepmc.org/abstract/MED/24365871 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Evans J, Papadopoulos A, Silvers CT, Charness N, Boot WR, Schlachta-Fairchild L, Crump C, Martinez M, Ent CB. Remote health monitoring for older adults and those with heart failure: adherence and system usability. Telemed J E Health. 2016 Jun;22(6):480–8. doi: 10.1089/tmj.2015.0140. https://europepmc.org/abstract/MED/26540369 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fountoulakis S, Papanastasiou L, Gryparis A, Markou A, Piaditis G. Impact and duration effect of telemonitoring on ΗbA1c, BMI and cost in insulin-treated diabetes mellitus patients with inadequate glycemic control: a randomized controlled study. Hormones (Athens) 2015;14(4):632–43. doi: 10.14310/horm.2002.1603. http://hormones.gr/preview.php?c_id=8577 . [DOI] [PubMed] [Google Scholar]
- 50.Frederix I, Vanderlinden L, Verboven AS, Welten M, Wouters D, De Keulenaer G, Ector B, Elegeert I, Troisfontaines P, Weytjens C, Mullens W, Dendale P. Long-term impact of a six-month telemedical care programme on mortality, heart failure readmissions and healthcare costs in patients with chronic heart failure. J Telemed Telecare. 2019 Jun;25(5):286–93. doi: 10.1177/1357633X18774632. [DOI] [PubMed] [Google Scholar]
- 51.Gallagher BD, Moise N, Haerizadeh M, Ye S, Medina V, Kronish IM. Telemonitoring adherence to medications in heart failure patients (TEAM-HF): a pilot randomized clinical trial. J Card Fail. 2017 Apr;23(4):345–9. doi: 10.1016/j.cardfail.2016.11.001. https://europepmc.org/abstract/MED/27818309 .S1071-9164(16)31209-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Giordano A, Scalvini S, Zanelli E, Corrà U, Longobardi GL, Ricci VA, Baiardi P, Glisenti F. Multicenter randomised trial on home-based telemanagement to prevent hospital readmission of patients with chronic heart failure. Int J Cardiol. 2009 Jan 09;131(2):192–9. doi: 10.1016/j.ijcard.2007.10.027.S0167-5273(07)01959-6 [DOI] [PubMed] [Google Scholar]
- 53.Grady M, Cameron H, Levy BL, Katz LB. Remote health consultations supported by a diabetes management Web application with a new glucose meter demonstrates improved glycemic control. J Diabetes Sci Technol. 2016 May;10(3):737–43. doi: 10.1177/1932296815622646. https://europepmc.org/abstract/MED/26685995 .1932296815622646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grant S, Hodgkinson J, Schwartz C, Bradburn P, Franssen M, Hobbs FR, Jowett S, McManus RJ, Greenfield S. Using mHealth for the management of hypertension in UK primary care: an embedded qualitative study of the TASMINH4 randomised controlled trial. Br J Gen Pract. 2019 Sep;69(686):e612–20. doi: 10.3399/bjgp19X704585. https://bjgp.org/cgi/pmidlookup?view=long&pmid=31262847 .bjgp19X704585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Greenwood DA, Blozis SA, Young HM, Nesbitt TS, Quinn CC. Overcoming clinical inertia: a randomized clinical trial of a telehealth remote monitoring intervention using paired glucose testing in adults with type 2 diabetes. J Med Internet Res. 2015 Jul 21;17(7):e178. doi: 10.2196/jmir.4112. https://www.jmir.org/2015/7/e178/ v17i7e178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hanley J, Fairbrother P, McCloughan L, Pagliari C, Paterson M, Pinnock H, Sheikh A, Wild S, McKinstry B. Qualitative study of telemonitoring of blood glucose and blood pressure in type 2 diabetes. BMJ Open. 2015 Dec 23;5(12):e008896. doi: 10.1136/bmjopen-2015-008896. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=26700275 .bmjopen-2015-008896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, Earle KA. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare. 2009;15(3):125–8. doi: 10.1258/jtt.2009.003006.15/3/125 [DOI] [PubMed] [Google Scholar]
- 58.Kardas P, Lewandowski K, Bromuri S. Type 2 diabetes patients benefit from the COMODITY12 mHealth system: results of a randomised trial. J Med Syst. 2016 Dec;40(12):259. doi: 10.1007/s10916-016-0619-x.10.1007/s10916-016-0619-x [DOI] [PubMed] [Google Scholar]
- 59.Karg O, Weber M, Bubulj C, Esche B, Weber N, Geiseler J, Bachl C, Schellhorn H. Akzeptanz einer telemedizinischen Intervention bei Patienten mit chronisch-obstruktiver Lungenerkrankung. Dtsch Med Wochenschr. 2012 Mar;137(12):574–9. doi: 10.1055/s-0031-1299033. [DOI] [PubMed] [Google Scholar]
- 60.Kashem A, Droogan MT, Santamore WP, Wald JW, Bove AA. Managing heart failure care using an internet-based telemedicine system. J Card Fail. 2008 Mar;14(2):121–6. doi: 10.1016/j.cardfail.2007.10.014.S1071-9164(07)01091-3 [DOI] [PubMed] [Google Scholar]
- 61.Kashem A, Droogan MT, Santamore WP, Wald JW, Marble JF, Cross RC, Bove AA. Web-based Internet telemedicine management of patients with heart failure. Telemed J E Health. 2006 Aug;12(4):439–47. doi: 10.1089/tmj.2006.12.439. [DOI] [PubMed] [Google Scholar]
- 62.Kerry SM, Markus HS, Khong TK, Cloud GC, Tulloch J, Coster D, Ibison J, Oakeshott P. Home blood pressure monitoring with nurse-led telephone support among patients with hypertension and a history of stroke: a community-based randomized controlled trial. CMAJ. 2013 Jan 08;185(1):23–31. doi: 10.1503/cmaj.120832. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=23128283 .cmaj.120832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform. 2008 Jun;77(6):399–404. doi: 10.1016/j.ijmedinf.2007.07.006.S1386-5056(07)00139-6 [DOI] [PubMed] [Google Scholar]
- 64.Koehler F, Koehler K, Deckwart O, Prescher S, Wegscheider K, Kirwan BA, Winkler S, Vettorazzi E, Bruch L, Oeff M, Zugck C, Doerr G, Naegele H, Störk S, Butter C, Sechtem U, Angermann C, Gola G, Prondzinsky R, Edelmann F, Spethmann S, Schellong SM, Schulze PC, Bauersachs J, Wellge B, Schoebel C, Tajsic M, Dreger H, Anker SD, Stangl K. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018 Sep 22;392(10152):1047–57. doi: 10.1016/S0140-6736(18)31880-4.S0140-6736(18)31880-4 [DOI] [PubMed] [Google Scholar]
- 65.Konstam V, Gregory D, Chen J, Weintraub A, Patel A, Levine D, Venesy D, Perry K, Delano C, Konstam MA. Health-related quality of life in a multicenter randomized controlled comparison of telephonic disease management and automated home monitoring in patients recently hospitalized with heart failure: SPAN-CHF II trial. J Card Fail. 2011 Feb;17(2):151–7. doi: 10.1016/j.cardfail.2010.08.012.S1071-9164(10)01091-2 [DOI] [PubMed] [Google Scholar]
- 66.Kotooka N, Kitakaze M, Nagashima K, Asaka M, Kinugasa Y, Nochioka K, Mizuno A, Nagatomo D, Mine D, Yamada Y, Kuratomi A, Okada N, Fujimatsu D, Kuwahata S, Toyoda S, Hirotani S, Komori T, Eguchi K, Kario K, Inomata T, Sugi K, Yamamoto K, Tsutsui H, Masuyama T, Shimokawa H, Momomura S, Seino Y, Sato Y, Inoue T, Node K, HOMES-HF study investigators The first multicenter, randomized, controlled trial of home telemonitoring for Japanese patients with heart failure: home telemonitoring study for patients with heart failure (HOMES-HF) Heart Vessels. 2018 Aug;33(8):866–76. doi: 10.1007/s00380-018-1133-5.10.1007/s00380-018-1133-5 [DOI] [PubMed] [Google Scholar]
- 67.Lee JY, Chan CK, Chua SS, Paraidathathu T, Lee KK, Tan CS, Nasir N, Lee SW. Using telemedicine to support care for people with type 2 diabetes mellitus: a qualitative analysis of patients' perspectives. BMJ Open. 2019 Oct 22;9(10):e026575. doi: 10.1136/bmjopen-2018-026575. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=31640990 .bmjopen-2018-026575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee PA, Greenfield G, Pappas Y. Patients' perception of using telehealth for type 2 diabetes management: a phenomenological study. BMC Health Serv Res. 2018 Jul 13;18(1):549. doi: 10.1186/s12913-018-3353-x. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3353-x .10.1186/s12913-018-3353-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Leng Chow W, Aung CY, Tong SC, Goh GS, Lee S, MacDonald MR, Ng AN, Cao Y, Ahmad AE, Yap MF, Leong G, Bruege A, Tesanovic A, Riistama J, Pang SY, Erazo F. Effectiveness of telemonitoring-enhanced support over structured telephone support in reducing heart failure-related healthcare utilization in a multi-ethnic Asian setting. J Telemed Telecare. 2020 Jul;26(6):332–40. doi: 10.1177/1357633X18825164. [DOI] [PubMed] [Google Scholar]
- 70.Lewis KE, Annandale JA, Warm DL, Hurlin C, Lewis MJ, Lewis L. Home telemonitoring and quality of life in stable, optimised chronic obstructive pulmonary disease. J Telemed Telecare. 2010;16(5):253–9. doi: 10.1258/jtt.2009.090907.jtt.2009.090907 [DOI] [PubMed] [Google Scholar]
- 71.Madigan E, Schmotzer BJ, Struk CJ, DiCarlo CM, Kikano G, Piña IL, Boxer RS. Home health care with telemonitoring improves health status for older adults with heart failure. Home Health Care Serv Q. 2013;32(1):57–74. doi: 10.1080/01621424.2012.755144. https://europepmc.org/abstract/MED/23438509 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Madsen LB, Kirkegaard P, Pedersen EB. Blood pressure control during telemonitoring of home blood pressure. A randomized controlled trial during 6 months. Blood Press. 2008;17(2):78–86. doi: 10.1080/08037050801915468.791848828 [DOI] [PubMed] [Google Scholar]
- 73.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O'Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013 Jul 03;310(1):46–56. doi: 10.1001/jama.2013.6549. https://europepmc.org/abstract/MED/23821088 .1707720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Margolis KL, Asche SE, Dehmer SP, Bergdall AR, Green BB, Sperl-Hillen JM, Nyboer RA, Pawloski PA, Maciosek MV, Trower NK, O'Connor PJ. Long-term outcomes of the effects of home blood pressure telemonitoring and pharmacist management on blood pressure among adults with uncontrolled hypertension: follow-up of a cluster randomized clinical trial. JAMA Netw Open. 2018 Sep 07;1(5):e181617. doi: 10.1001/jamanetworkopen.2018.1617. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2018.1617 .2701733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McKinstry B, Hanley J, Wild S, Pagliari C, Paterson M, Lewis S, Sheikh A, Krishan A, Stoddart A, Padfield P. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ. 2013 May 24;346:f3030. doi: 10.1136/bmj.f3030. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=23709583 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Michaud TL, Siahpush M, Schwab RJ, Eiland LA, DeVany M, Hansen G, Slachetka TS, Boilesen E, Tak HJ, Wilson FA, Wang H, Pagán JA, Su D. Remote patient monitoring and clinical outcomes for postdischarge patients with type 2 diabetes. Popul Health Manag. 2018 Oct;21(5):387–94. doi: 10.1089/pop.2017.0175. [DOI] [PubMed] [Google Scholar]
- 77.McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, Kaambwa B, Banting M, Bryan S, Little P, Williams B, Hobbs FR. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010 Jul 17;376(9736):163–72. doi: 10.1016/S0140-6736(10)60964-6.S0140-6736(10)60964-6 [DOI] [PubMed] [Google Scholar]
- 78.Mira-Solves JJ, Orozco-Beltrán D, Sánchez-Molla M, Sánchez García JJ, en nombre de los investigadores del programa ValCrònic Evaluación de la satisfacción de los pacientes crónicos con los dispositivos de telemedicina y con el resultado de la atención recibida. Programa ValCrònic. Aten Primaria. 2014 Jun;46 Suppl 3:16–23. doi: 10.1016/S0212-6567(14)70061-7. https://linkinghub.elsevier.com/retrieve/pii/S0212-6567(14)70061-7 .S0212-6567(14)70061-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moon EW, Tan NC, Allen JC, Jafar TH. The use of wireless, smartphone app-assisted home blood pressure monitoring among hypertensive patients in Singapore: pilot randomized controlled trial. JMIR Mhealth Uhealth. 2019 May 28;7(5):e13153. doi: 10.2196/13153. https://mhealth.jmir.org/2019/5/e13153/ v7i5e13153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mortara A, Pinna GD, Johnson P, Maestri R, Capomolla S, La Rovere MT, Ponikowski P, Tavazzi L, Sleight P, HHH Investigators Home telemonitoring in heart failure patients: the HHH study (Home or Hospital in Heart Failure) Eur J Heart Fail. 2009 Mar;11(3):312–8. doi: 10.1093/eurjhf/hfp022. doi: 10.1093/eurjhf/hfp022.hfp022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Neumann CL, Menne J, Rieken EM, Fischer N, Weber MH, Haller H, Schulz EG. Blood pressure telemonitoring is useful to achieve blood pressure control in inadequately treated patients with arterial hypertension. J Hum Hypertens. 2011 Dec;25(12):732–8. doi: 10.1038/jhh.2010.119.jhh2010119 [DOI] [PubMed] [Google Scholar]
- 82.Nissen L, Lindhardt T. A qualitative study of COPD-patients' experience of a telemedicine intervention. Int J Med Inform. 2017 Nov;107:11–7. doi: 10.1016/j.ijmedinf.2017.08.004.S1386-5056(17)30203-4 [DOI] [PubMed] [Google Scholar]
- 83.Nouryan CN, Morahan S, Pecinka K, Akerman M, Lesser M, Chaikin D, Castillo S, Zhang M, Pekmezaris R. Home telemonitoring of community-dwelling heart failure patients after home care discharge. Telemed J E Health. 2019 Jun;25(6):447–54. doi: 10.1089/tmj.2018.0099. [DOI] [PubMed] [Google Scholar]
- 84.Ong MK, Romano PS, Edgington S, Aronow HU, Auerbach AD, Black JT, De Marco T, Escarce JJ, Evangelista LS, Hanna B, Ganiats TG, Greenberg BH, Greenfield S, Kaplan SH, Kimchi A, Liu H, Lombardo D, Mangione CM, Sadeghi B, Sadeghi B, Sarrafzadeh M, Tong K, Fonarow GC, Better Effectiveness After Transition–Heart Failure (BEAT-HF) Research Group Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: the better effectiveness after transition -- heart failure (BEAT-HF) randomized clinical trial. JAMA Intern Med. 2016 Mar;176(3):310–8. doi: 10.1001/jamainternmed.2015.7712. https://europepmc.org/abstract/MED/26857383 .2488923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Orozco-Beltran D, Sánchez-Molla M, Sanchez JJ, Mira JJ, ValCrònic Research Group Telemedicine in primary care for patients with chronic conditions: the ValCrònic quasi-experimental study. J Med Internet Res. 2017 Dec 15;19(12):e400. doi: 10.2196/jmir.7677. https://www.jmir.org/2017/12/e400/ v19i12e400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pekmezaris R, Williams MS, Pascarelli B, Finuf KD, Harris YT, Myers AK, Taylor T, Kline M, Patel VH, Murray LM, McFarlane SI, Pappas K, Lesser ML, Makaryus AN, Martinez S, Kozikowski A, Polo J, Guzman J, Zeltser R, Marino J, Pena M, DiClemente RJ, Granville D. Adapting a home telemonitoring intervention for underserved Hispanic/Latino patients with type 2 diabetes: an acceptability and feasibility study. BMC Med Inform Decis Mak. 2020 Dec 07;20(1):324. doi: 10.1186/s12911-020-01346-0. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-020-01346-0 .10.1186/s12911-020-01346-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pressman AR, Kinoshita L, Kirk S, Barbosa GM, Chou C, Minkoff J. A novel telemonitoring device for improving diabetes control: protocol and results from a randomized clinical trial. Telemed J E Health. 2014 Feb;20(2):109–14. doi: 10.1089/tmj.2013.0157. [DOI] [PubMed] [Google Scholar]
- 88.Ralston JD, Cook AJ, Anderson ML, Catz SL, Fishman PA, Carlson J, Johnson R, Green BB. Home blood pressure monitoring, secure electronic messaging and medication intensification for improving hypertension control: a mediation analysis. Appl Clin Inform. 2014 Mar 12;5(1):232–48. doi: 10.4338/ACI-2013-10-RA-0079. https://europepmc.org/abstract/MED/24734136 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rodríguez-Idígoras MI, Sepúlveda-Muñoz J, Sánchez-Garrido-Escudero R, Martínez-González JL, Escolar-Castelló JL, Paniagua-Gómez IM, Bernal-López R, Fuentes-Simón MV, Garófano-Serrano D. Telemedicine influence on the follow-up of type 2 diabetes patients. Diabetes Technol Ther. 2009 Jul;11(7):431–7. doi: 10.1089/dia.2008.0114. [DOI] [PubMed] [Google Scholar]
- 90.Rogers MA, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, Husovsky HL. Home monitoring service improves mean arterial pressure in patients with essential hypertension. A randomized, controlled trial. Ann Intern Med. 2001 Jun 05;134(11):1024–32. doi: 10.7326/0003-4819-134-11-200106050-00008.200106050-00008 [DOI] [PubMed] [Google Scholar]
- 91.Schoenfeld MH, Compton SJ, Mead RH, Weiss DN, Sherfesee L, Englund J, Mongeon LR. Remote monitoring of implantable cardioverter defibrillators: a prospective analysis. Pacing Clin Electrophysiol. 2004 Jun;27(6 Pt 1):757–63. doi: 10.1111/j.1540-8159.2004.00524.x.PACE524 [DOI] [PubMed] [Google Scholar]
- 92.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J Med Internet Res. 2012 Feb 16;14(1):e31. doi: 10.2196/jmir.1909. https://www.jmir.org/2012/1/e31/ v14i1e31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shea S, Weinstock RS, Starren J, Teresi J, Palmas W, Field L, Morin P, Goland R, Izquierdo RE, Wolff LT, Ashraf M, Hilliman C, Silver S, Meyer S, Holmes D, Petkova E, Capps L, Lantigua RA. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. J Am Med Inform Assoc. 2006;13(1):40–51. doi: 10.1197/jamia.M1917. https://europepmc.org/abstract/MED/16221935 .M1917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, Lai AM, Field L, Morin PC, Goland R, Izquierdo RE, Ebner S, Silver S, Petkova E, Kong J, Eimicke JP, IDEATel Consortium A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446–56. doi: 10.1197/jamia.M3157. https://europepmc.org/abstract/MED/19390093 .M3157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sicotte C, Paré G, Morin S, Potvin J, Moreault MP. Effects of home telemonitoring to support improved care for chronic obstructive pulmonary diseases. Telemed J E Health. 2011 Mar;17(2):95–103. doi: 10.1089/tmj.2010.0142. [DOI] [PubMed] [Google Scholar]
- 96.Soriano JB, García-Río F, Vázquez-Espinosa E, Conforto JI, Hernando-Sanz A, López-Yepes L, Galera-Martínez R, Peces-Barba G, Gotera-Rivera CM, Pérez-Warnisher MT, Segrelles-Calvo G, Zamarro C, González-Ponce P, Ramos MI, Jafri S, Ancochea J. A multicentre, randomized controlled trial of telehealth for the management of COPD. Respir Med. 2018 Nov;144:74–81. doi: 10.1016/j.rmed.2018.10.008. https://linkinghub.elsevier.com/retrieve/pii/S0954-6111(18)30314-7 .S0954-6111(18)30314-7 [DOI] [PubMed] [Google Scholar]
- 97.Stuckey M, Fulkerson R, Read E, Russell-Minda E, Munoz C, Kleinstiver P, Petrella R. Remote monitoring technologies for the prevention of metabolic syndrome: the Diabetes and Technology for Increased Activity (DaTA) study. J Diabetes Sci Technol. 2011 Jul 01;5(4):936–44. doi: 10.1177/193229681100500417. https://europepmc.org/abstract/MED/21880237 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Trudel M, Cafazzo JA, Hamill M, Igharas W, Tallevi K, Picton P, Lam J, Rossos PG, Easty AC, Logan A. A mobile phone based remote patient monitoring system for chronic disease management. Stud Health Technol Inform. 2007;129(Pt 1):167–71. [PubMed] [Google Scholar]
- 99.Tsang MW, Mok M, Kam G, Jung M, Tang A, Chan U, Chu CM, Li I, Chan J. Improvement in diabetes control with a monitoring system based on a hand-held, touch-screen electronic diary. J Telemed Telecare. 2001;7(1):47–50. doi: 10.1258/1357633011936138. [DOI] [PubMed] [Google Scholar]
- 100.Tupper OD, Gregersen TL, Ringbaek T, Brøndum E, Frausing E, Green A, Ulrik C. Effect of tele-health care on quality of life in patients with severe COPD: a randomized clinical trial. Int J Chron Obstruct Pulmon Dis. 2018 Aug 29;13:2657–62. doi: 10.2147/COPD.S164121. doi: 10.2147/COPD.S164121.copd-13-2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Valdivieso B, García-Sempere A, Sanfélix-Gimeno G, Faubel R, Librero J, Soriano E, Peiró S, GeChronic Group The effect of telehealth, telephone support or usual care on quality of life, mortality and healthcare utilization in elderly high-risk patients with multiple chronic conditions. A prospective study. Med Clin (Barc) 2018 Oct 23;151(8):308–14. doi: 10.1016/j.medcli.2018.03.013.S0025-7753(18)30213-6 [DOI] [PubMed] [Google Scholar]
- 102.van Berkel C, Almond P, Hughes C, Smith M, Horsfield D, Duckworth H. Retrospective observational study of the impact on emergency admission of telehealth at scale delivered in community care in Liverpool, UK. BMJ Open. 2019 Jul 31;9(7):e028981. doi: 10.1136/bmjopen-2019-028981. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=31371293 .bmjopen-2019-028981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Varon C, Alao M, Minter J, Stapleton M, Thomson S, Jaecques S, Rocca HB, Huffel SV. Telehealth on heart failure: results of the Recap project. J Telemed Telecare. 2015 Sep;21(6):340–7. doi: 10.1177/1357633X15577310.1357633X15577310 [DOI] [PubMed] [Google Scholar]
- 104.Vianello A, Fusello M, Gubian L, Rinaldo C, Dario C, Concas A, Saccavini C, Battistella L, Pellizzon G, Zanardi G, Mancin S. Home telemonitoring for patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulm Med. 2016 Nov 22;16(1):157. doi: 10.1186/s12890-016-0321-2. https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-016-0321-2 .10.1186/s12890-016-0321-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Villani A, Malfatto G, Compare A, Della Rosa F, Bellardita L, Branzi G, Molinari E, Parati G. Clinical and psychological telemonitoring and telecare of high risk heart failure patients. J Telemed Telecare. 2014 Dec;20(8):468–75. doi: 10.1177/1357633X14555644.1357633X14555644 [DOI] [PubMed] [Google Scholar]
- 106.Vuorinen AL, Leppänen J, Kaijanranta H, Kulju M, Heliö T, van Gils M, Lähteenmäki J. Use of home telemonitoring to support multidisciplinary care of heart failure patients in Finland: randomized controlled trial. J Med Internet Res. 2014 Dec 11;16(12):e282. doi: 10.2196/jmir.3651. https://www.jmir.org/2014/12/e282/ v16i12e282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wade MJ, Desai AS, Spettell CM, Snyder AD, McGowan-Stackewicz V, Kummer PJ, Maccoy MC, Krakauer RS. Telemonitoring with case management for seniors with heart failure. Am J Manag Care. 2011 Mar 01;17(3):e71–9. https://www.ajmc.com/pubMed.php?pii=47949 .47949 [PubMed] [Google Scholar]
- 108.Walker PP, Pompilio PP, Zanaboni P, Bergmo TS, Prikk K, Malinovschi A, Montserrat JM, Middlemass J, Šonc S, Munaro G, Marušič D, Sepper R, Rosso R, Siriwardena AN, Janson C, Farré R, Calverley PM, Dellaca' RL. Telemonitoring in chronic obstructive pulmonary disease (CHROMED). A randomized clinical trial. Am J Respir Crit Care Med. 2018 Sep 01;198(5):620–8. doi: 10.1164/rccm.201712-2404OC. [DOI] [PubMed] [Google Scholar]
- 109.Wild SH, Hanley J, Lewis SC, McKnight JA, McCloughan LB, Padfield PL, Parker RA, Paterson M, Pinnock H, Sheikh A, McKinstry B. Supported telemonitoring and glycemic control in people with type 2 diabetes: the telescot diabetes pragmatic multicenter randomized controlled trial. PLoS Med. 2016 Jul;13(7):e1002098. doi: 10.1371/journal.pmed.1002098. https://dx.plos.org/10.1371/journal.pmed.1002098 .PMEDICINE-D-16-00161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Aberger EW, Migliozzi D, Follick MJ, Malick T, Ahern DK. Enhancing patient engagement and blood pressure management for renal transplant recipients via home electronic monitoring and Web-enabled collaborative care. Telemed J E Health. 2014 Sep;20(9):850–4. doi: 10.1089/tmj.2013.0317. https://europepmc.org/abstract/MED/25046403 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Abraham WT. Disease management: remote monitoring in heart failure patients with implantable defibrillators, resynchronization devices, and haemodynamic monitors. Europace. 2013 Jun;15 Suppl 1:i40–6. doi: 10.1093/europace/eut105.eut105 [DOI] [PubMed] [Google Scholar]
- 112.Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, Strickland W, Neelagaru S, Raval N, Krueger S, Weiner S, Shavelle D, Jeffries B, Yadav JS, CHAMPION Trial Study Group Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011 Feb 19;377(9766):658–66. doi: 10.1016/S0140-6736(11)60101-3.S0140-6736(11)60101-3 [DOI] [PubMed] [Google Scholar]
- 113.Abraham WT, Perl L. Implantable hemodynamic monitoring for heart failure patients. J Am Coll Cardiol. 2017 Jul 18;70(3):389–98. doi: 10.1016/j.jacc.2017.05.052. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(17)37594-0 .S0735-1097(17)37594-0 [DOI] [PubMed] [Google Scholar]
- 114.Adamson PB, Abraham WT, Bourge RC, Costanzo MR, Hasan A, Yadav C, Henderson J, Cowart P, Stevenson LW. Wireless pulmonary artery pressure monitoring guides management to reduce decompensation in heart failure with preserved ejection fraction. Circ Heart Fail. 2014 Nov;7(6):935–44. doi: 10.1161/CIRCHEARTFAILURE.113.001229.CIRCHEARTFAILURE.113.001229 [DOI] [PubMed] [Google Scholar]
- 115.Adamson PB, Abraham WT, Stevenson LW, Desai AS, Lindenfeld J, Bourge RC, Bauman J. Pulmonary artery pressure-guided heart failure management reduces 30-day readmissions. Circ Heart Fail. 2016 Jun;9(6):e002600. doi: 10.1161/CIRCHEARTFAILURE.115.002600.CIRCHEARTFAILURE.115.002600 [DOI] [PubMed] [Google Scholar]
- 116.Ades PA, Pashkow FJ, Fletcher G, Pina IL, Zohman LR, Nestor JR. A controlled trial of cardiac rehabilitation in the home setting using electrocardiographic and voice transtelephonic monitoring. Am Heart J. 2000 Mar;139(3):543–8. doi: 10.1016/s0002-8703(00)90100-5.S0002-8703(00)90100-5 [DOI] [PubMed] [Google Scholar]
- 117.Ahring KK, Ahring JP, Joyce C, Farid NR. Telephone modem access improves diabetes control in those with insulin-requiring diabetes. Diabetes Care. 1992 Aug;15(8):971–5. doi: 10.2337/diacare.15.8.971. [DOI] [PubMed] [Google Scholar]
- 118.Ajay VS, Jindal D, Roy A, Venugopal V, Sharma R, Pawar A, Kinra S, Tandon N, Prabhakaran D. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: the mPower heart project. J Am Heart Assoc. 2016 Dec 21;5(12):e004343. doi: 10.1161/JAHA.116.004343. https://www.ahajournals.org/doi/10.1161/JAHA.116.004343?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .JAHA.116.004343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Al-Khatib SM, Piccini JP, Knight D, Stewart M, Clapp-Channing N, Sanders GD. Remote monitoring of implantable cardioverter defibrillators versus quarterly device interrogations in clinic: results from a randomized pilot clinical trial. J Cardiovasc Electrophysiol. 2010 May;21(5):545–50. doi: 10.1111/j.1540-8167.2009.01659.x.JCE1659 [DOI] [PubMed] [Google Scholar]
- 120.Amara W, Montagnier C, Cheggour S, Boursier M, Barnay C, Georger F, Deplagne A, Fromentin S, Mlotek M, Taïeb J. Early detection and treatment of supraventricular arrhythmia by remote monitoring prevents its progression in pacemaker patients: the randomized, multicenter SETAM trial. Europace. 2015 Mar;17(5):iii8. doi: 10.1093/europace/euv151. [DOI] [Google Scholar]
- 121.Ando K, Koyama J, Abe Y, Sato T, Shoda M, Soga Y, Nobuyoshi M, Honda T, Nakao K, Terata K, Kadowaki K, Maeda A, Ogawa S, Manaka T, Hagiwara N, Doi K. Feasibility evaluation of a remote monitoring system for implantable cardiac devices in Japan. Int Heart J. 2011;52(1):39–43. doi: 10.1536/ihj.52.39. http://japanlinkcenter.org/JST.JSTAGE/ihj/52.39?from=PubMed .JST.JSTAGE/ihj/52.39 [DOI] [PubMed] [Google Scholar]
- 122.Bastyr 3rd EJ, Zhang S, Mou J, Hackett AP, Raymond SA, Chang AM. Performance of an electronic diary system for intensive insulin management in global diabetes clinical trials. Diabetes Technol Ther. 2015 Aug;17(8):571–9. doi: 10.1089/dia.2014.0407. https://europepmc.org/abstract/MED/25826466 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Batalik L, Dosbaba F, Hartman M, Batalikova K, Spinar J. Benefits and effectiveness of using a wrist heart rate monitor as a telerehabilitation device in cardiac patients: a randomized controlled trial. Medicine (Baltimore) 2020 Mar;99(11):e19556. doi: 10.1097/MD.0000000000019556. doi: 10.1097/MD.0000000000019556.00005792-202003130-00090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bekelman DB, Plomondon ME, Carey EP, Sullivan MD, Nelson KM, Hattler B, McBryde CF, Lehmann KG, Gianola K, Heidenreich PA, Rumsfeld JS. Primary results of the patient-centered disease management (PCDM) for heart failure study: a randomized clinical trial. JAMA Intern Med. 2015 May;175(5):725–32. doi: 10.1001/jamainternmed.2015.0315.2210885 [DOI] [PubMed] [Google Scholar]
- 125.Benhamou PY, Melki V, Boizel R, Perreal F, Quesada JL, Bessieres-Lacombe S, Bosson JL, Halimi S, Hanaire H. One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes Metab. 2007 Jun;33(3):220–6. doi: 10.1016/j.diabet.2007.01.002.S1262-3636(07)00058-4 [DOI] [PubMed] [Google Scholar]
- 126.Bernocchi P, Vitacca M, La Rovere MT, Volterrani M, Galli T, Baratti D, Paneroni M, Campolongo G, Sposato B, Scalvini S. Home-based telerehabilitation in older patients with chronic obstructive pulmonary disease and heart failure: a randomised controlled trial. Age Ageing. 2018 Jan 01;47(1):82–8. doi: 10.1093/ageing/afx146.4097568 [DOI] [PubMed] [Google Scholar]
- 127.Bhavnani SP, Sola S, Adams D, Venkateshvaran A, Dash PK, Sengupta PP, ASEF-VALUES Investigators A randomized trial of pocket-echocardiography integrated mobile health device assessments in modern structural heart disease clinics. JACC Cardiovasc Imaging. 2018 Apr;11(4):546–57. doi: 10.1016/j.jcmg.2017.06.019. https://linkinghub.elsevier.com/retrieve/pii/S1936-878X(17)30721-0 .S1936-878X(17)30721-0 [DOI] [PubMed] [Google Scholar]
- 128.Biermann E, Dietrich W, Standl E. Telecare of diabetic patients with intensified insulin therapy. A randomized clinical trial. Stud Health Technol Inform. 2000;77:327–32. [PubMed] [Google Scholar]
- 129.Billiard A, Rohmer V, Roques MA, Joseph MG, Suraniti S, Giraud P, Limal JM, Fressinaud P, Marre M. Telematic transmission of computerized blood glucose profiles for IDDM patients. Diabetes Care. 1991 Feb;14(2):130–4. doi: 10.2337/diacare.14.2.130. [DOI] [PubMed] [Google Scholar]
- 130.Böhm M, Drexler H, Oswald H, Rybak K, Bosch R, Butter C, Klein G, Gerritse B, Monteiro J, Israel C, Bimmel D, Käab S, Huegl B, Brachmann J, OptiLink HF Study Investigators Fluid status telemedicine alerts for heart failure: a randomized controlled trial. Eur Heart J. 2016 Nov 01;37(41):3154–63. doi: 10.1093/eurheartj/ehw099.ehw099 [DOI] [PubMed] [Google Scholar]
- 131.Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, Gentry PW, Rose C, Van Houtven C, Wang V, Goldstein MK, Oddone EZ. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. 2011 Jul 11;171(13):1173–80. doi: 10.1001/archinternmed.2011.276.171/13/1173 [DOI] [PubMed] [Google Scholar]
- 132.Boyne JJ, Vrijhoef HJ, Spreeuwenberg M, De Weerd G, Kragten J, Gorgels AP, TEHAF investigators Effects of tailored telemonitoring on heart failure patients' knowledge, self-care, self-efficacy and adherence: a randomized controlled trial. Eur J Cardiovasc Nurs. 2014 Jun;13(3):243–52. doi: 10.1177/1474515113487464.1474515113487464 [DOI] [PubMed] [Google Scholar]
- 133.Bray EP, Jones MI, Banting M, Greenfield S, Hobbs FD, Little P, Williams B, Mcmanus RJ. Performance and persistence of a blood pressure self-management intervention: telemonitoring and self-management in hypertension (TASMINH2) trial. J Hum Hypertens. 2015 Jul;29(7):436–41. doi: 10.1038/jhh.2014.108.jhh2014108 [DOI] [PubMed] [Google Scholar]
- 134.Chan WM, Woo J, Hui E, Lau WW, Lai JC, Lee D. A community model for care of elderly people with diabetes via telemedicine. Appl Nurs Res. 2005 May;18(2):77–81. doi: 10.1016/j.apnr.2004.11.002.S0897189705000145 [DOI] [PubMed] [Google Scholar]
- 135.Chase HP, Pearson JA, Wightman C, Roberts MD, Oderberg AD, Garg SK. Modem transmission of glucose values reduces the costs and need for clinic visits. Diabetes Care. 2003 May;26(5):1475–9. doi: 10.2337/diacare.26.5.1475. [DOI] [PubMed] [Google Scholar]
- 136.Dang S, Karanam C, Gómez-Marín O. Outcomes of a mobile phone intervention for heart failure in a minority county hospital population. Telemed J E Health. 2017 Jun;23(6):473–84. doi: 10.1089/tmj.2016.0211. [DOI] [PubMed] [Google Scholar]
- 137.Desai AS. Home monitoring heart failure care does not improve patient outcomes: looking beyond telephone-based disease management. Circulation. 2012 Feb 14;125(6):828–36. doi: 10.1161/CIRCULATIONAHA.111.031179.125/6/828 [DOI] [PubMed] [Google Scholar]
- 138.Ding H, Jayasena R, Maiorana A, Dowling A, Chen SH, Karunanithi M, Layland J, Edwards I. Innovative Telemonitoring Enhanced Care Programme for Chronic Heart Failure (ITEC-CHF) to improve guideline compliance and collaborative care: protocol of a multicentre randomised controlled trial. BMJ Open. 2017 Oct 08;7(10):e017550. doi: 10.1136/bmjopen-2017-017550. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=28993389 .bmjopen-2017-017550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schwarz KA, Mion LC, Hudock D, Litman G. Telemonitoring of heart failure patients and their caregivers: a pilot randomized controlled trial. Prog Cardiovasc Nurs. 2008;23(1):18–26. doi: 10.1111/j.1751-7117.2008.06611.x. [DOI] [PubMed] [Google Scholar]
- 140.Trief PM, Teresi JA, Eimicke JP, Shea S, Weinstock RS. Improvement in diabetes self-efficacy and glycaemic control using telemedicine in a sample of older, ethnically diverse individuals who have diabetes: the IDEATel project. Age Ageing. 2009 Mar;38(2):219–25. doi: 10.1093/ageing/afn299.afn299 [DOI] [PubMed] [Google Scholar]
- 141.Zakeri R, Morgan JM, Phillips P, Kitt S, Ng GA, McComb JM, Williams S, Wright DJ, Gill JS, Seed A, Witte KK, Cowie MR, REM-HF Investigators Impact of remote monitoring on clinical outcomes for patients with heart failure and atrial fibrillation: results from the REM-HF trial. Eur J Heart Fail. 2020 Mar;22(3):543–53. doi: 10.1002/ejhf.1709. doi: 10.1002/ejhf.1709. [DOI] [PubMed] [Google Scholar]
- 142.Ancker J. Comparative Effectiveness of Telemedicine in Primary Care. Clinical Trials. 2020. Dec 28, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04684836;
- 143.Bessonov IS. Telemedicine Follow-up for Post-ACS Patients. Clinical Trials. 2020. Jul 24, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04485754;
- 144.Colet JC. Heart Failure Events Reduction With Remote Monitoring and eHealth Support Investigator Initiated Trial (HERMeS) Clinical Trials. 2018. Sep 10, [2021-10-01]. https://ClinicalTrials.gov/show/NCT03663907;
- 145.Dominguez H. Brazilian Heart Insufficiency With Telemedicine (BRAHIT) Clinical Trials. 2020. Jul 10, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04466852;
- 146.Esteban C. Impact of the Artificial Intelligence in a Telemonitoring Programme of COPD Patients With Multiple Hospitalizations. Clinical Trials. 2021. Jul 27, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04978922;
- 147.Hoffman J. Influence of Telemonitoring on the Management of LVAD-patients. Clinical Trials. 2020. Nov 3, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04613401;
- 148.Iversen MM. Telemedicine Follow-up in Primary Health Care for Diabetes-related Foot Ulcers (DiaFOTo) Clinical Trials. 2012. Oct 19, [2021-10-01]. https://ClinicalTrials.gov/show/NCT01710774;
- 149.Krzowski B. Mobile App and Digital System for Patients After Myocardial Infarction (afterAMI) Clinical Trials. 2021. Mar 11, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04793425;
- 150.Mahler SA. Enhancing Rural Health Via Cardiovascular Telehealth for Rural Patients Implementation (E-VICTORS) Clinical Trials. 2020. Nov 5, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04617834;
- 151.Marinello R. Telemonitoring of Patients Admitted in Hospital at Home With Acute Decompensated Heart Failure - Pilot Study (MONTEROSA) Clinical Trials. 2020. May 27, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04403659;
- 152.Martin S. TeLIPro Health Program - Active With Diabetes (TeLIPro) Clinical Trials. 2018. Sep 18, [2021-10-01]. https://ClinicalTrials.gov/show/NCT03675919;
- 153.Naqvi IA. Telehealth After Stroke Care: Integrated Multidisciplinary Access to Post-stroke Care (TASC) Clinical Trials. 2020. Nov 23, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04640519;
- 154.Noruzbaeva A. Effects of Remote Monitoring of Patients With Heart Failure Based on Smartphone Application (ERICA-HF) Clinical Trials. 2020. Oct 19, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04591964;
- 155.Nouira S. The Impact of Telemonitoring in the Management of Hypertension (HOROSCOPE) Clinical Trials. 2020. Oct 29, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04607239;
- 156.Omboni S. Telemonitoring of Blood Pressure in Local Pharmacies (TEMPLAR) Clinical Trials. 2018. Dec 19, [2021-10-01]. https://ClinicalTrials.gov/show/NCT03781401;
- 157.Pekmezaris R. Diabetes Management Program for Hispanic/Latino. Clinical Trials. 2019. May 23, [2021-10-01]. https://ClinicalTrials.gov/show/NCT03960424;
- 158.Prigent A. Study Evaluating Telemonitoring and Experimentation in Telemedicine for the Improvement of Healthcare Pathways (ETAPES Program) Compared to Standard of Care in Patients With Chronic Respiratory Failure Receiving Non-invasive Home Ventilation (e-VENT) Clinical Trials. 2020. Nov 4, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04615078;
- 159.Schwartz J, Ssinabulya I. mHealth for Self-care of Heart Failure in Uganda. Clinical Trials. 2020. Jun 11, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04426630;
- 160.Siriwardena AN. Use of MonitorMe in COPD. Clinical Trials. 2019. Sep 27, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04108143;
- 161.Skanes AC. Virtual for Care Atrial Fibrillation Patients Using VIRTUES. Clinical Trials. 2020. Oct 22, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04599114;
- 162.Sun L, Zhu Y, Sun X, Jiang J. Integrative Management of Patients With Atrial Fibrillation Via Hospital-Community-Family-Based Telemedicine (HCFT-AF) Program. Clinical Trials. 2019. Oct 16, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04127799; [DOI] [PMC free article] [PubMed]
- 163.Yin W. COVID-19 Lockdown Related Telemedicine for Type 2 Diabetes. Clinical Trials. 2021. Jan 25, [2021-10-01]. https://ClinicalTrials.gov/show/NCT04723550;
- 164.Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JP. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019 Aug 28;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 165.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016 Oct 12;355:i4919. doi: 10.1136/bmj.i4919. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=27733354 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Review Manager (RevMan). 5.3. Copenhagen, Denmark: The Cochrane Collaboration; 2014. [2021-10-01]. https://training.cochrane.org/online-learning/core-software/revman/revman-5-download . [Google Scholar]
- 167.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. London, UK: The Cochrane Collaboration; 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Shahaj O, Denneny D, Schwappach A, Pearce G, Epiphaniou E, Parke H, Taylor SJ, Pinnock H. Supporting self-management for people with hypertension: a meta-review of quantitative and qualitative systematic reviews. J Hypertens. 2019 Feb;37(2):264–79. doi: 10.1097/HJH.0000000000001867. [DOI] [PubMed] [Google Scholar]
- 169.So CF, Chung JW. Telehealth for diabetes self-management in primary healthcare: a systematic review and meta-analysis. J Telemed Telecare. 2018 Jun;24(5):356–64. doi: 10.1177/1357633X17700552. [DOI] [PubMed] [Google Scholar]
- 170.Snoswell CL, Stringer H, Taylor ML, Caffery LJ, Smith AC. An overview of the effect of telehealth on mortality: a systematic review of meta-analyses. J Telemed Telecare (forthcoming) 2021 Jun 29;:1357633X211023700. doi: 10.1177/1357633X211023700. [DOI] [PubMed] [Google Scholar]
- 171.Kalankesh LR, Pourasghar F, Nicholson L, Ahmadi S, Hosseini M. Effect of telehealth interventions on hospitalization indicators: a systematic review. Perspect Health Inf Manag. 2016 Oct 1;13(Fall):1h. https://europepmc.org/abstract/MED/27843425 . [PMC free article] [PubMed] [Google Scholar]
- 172.Zhu Y, Gu X, Xu C. Effectiveness of telemedicine systems for adults with heart failure: a meta-analysis of randomized controlled trials. Heart Fail Rev. 2020 Mar;25(2):231–43. doi: 10.1007/s10741-019-09801-5. https://europepmc.org/abstract/MED/31197564 .10.1007/s10741-019-09801-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Thurmond VA, Boyle DK. An integrative review of patients' perceptions regarding telehealth used in their health care. Online J Knowl Synth Nurs. 2002 Apr 16;9:2.090002 [PubMed] [Google Scholar]
- 174.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017 Aug 03;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=28775188 .bmjopen-2017-016242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ramaswamy A, Yu M, Drangsholt S, Ng E, Culligan PJ, Schlegel PN, Hu JC. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020 Sep 09;22(9):e20786. doi: 10.2196/20786. https://www.jmir.org/2020/9/e20786/ v22i9e20786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nguyen M, Waller M, Pandya A, Portnoy J. A review of patient and provider satisfaction with telemedicine. Curr Allergy Asthma Rep. 2020 Sep 22;20(11):72. doi: 10.1007/s11882-020-00969-7. https://europepmc.org/abstract/MED/32959158 .10.1007/s11882-020-00969-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hanlon P, Daines L, Campbell C, McKinstry B, Weller D, Pinnock H. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. 2017 May 17;19(5):e172. doi: 10.2196/jmir.6688. https://www.jmir.org/2017/5/e172/ v19i5e172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.McFarland S, Coufopolous A, Lycett D. The effect of telehealth versus usual care for home-care patients with long-term conditions: a systematic review, meta-analysis and qualitative synthesis. J Telemed Telecare. 2021 Feb;27(2):69–87. doi: 10.1177/1357633X19862956. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures and tables that were not included in the main manuscript.
Summary of the included studies (N=96).


