Abstract
This cross-sectional study analyzes patterns in the rates of routine screening and diagnosis for breast, cervical, and colorectal cancer before and after the COVID-19 pandemic.
The COVID-19 pandemic triggered substantial disruptions to health care delivery in the US due to stay-at-home orders and patient fears about visiting health care facilities.1,2 Thus, many forms of health care use, including cancer screenings, sharply decreased in early 2020.3,4,5,6 Although the temporary pause in preventive screening was clinically reasonable and situationally appropriate, long-term delays or avoidance will have adverse implications for population-level cancer-related morbidity and mortality. Studies suggest that cancer screening rebounded through summer 2020; however, more than 2 years after the start of the pandemic, long-term consequences for preventive cancer screening and diagnosis are unknown.3,4,5,6
The aim of this study was to examine patterns in breast, cervical, and colorectal cancer screening and diagnosis before and after the pandemic.
Methods
This cross-sectional study used the Trilliant Health all-payer claims and encounters database, which includes inpatient, outpatient, and prescription drug claims from all 50 states and the District of Columbia. We analyzed calendar year quarterly medical claims from January 2017 to December 2021. Patients aged 21 to 85 years were included (guideline-concordant target populations for the included screening procedures). For breast and cervical cancer, only women were included. Using Current Procedural Terminology codes, we calculated the quarterly number of individuals, per 100 000 eligible beneficiaries, who received screening for breast cancer (mammography), cervical cancer (Papanicolaou test and human papillomavirus screening), and colorectal cancer (colonoscopy, stool testing, stool DNA, computed tomography colonography, or sigmoidoscopy).5 As a secondary outcome, we assessed the annual prevalence rate for each cancer type. Percentage changes in screening tests and diagnoses were compared. In accordance with the National Human Research Protections Advisory Committee Guidelines, this study was exempt from review and informed consent because the data were deidentified. We followed the STROBE reporting guideline.
Results
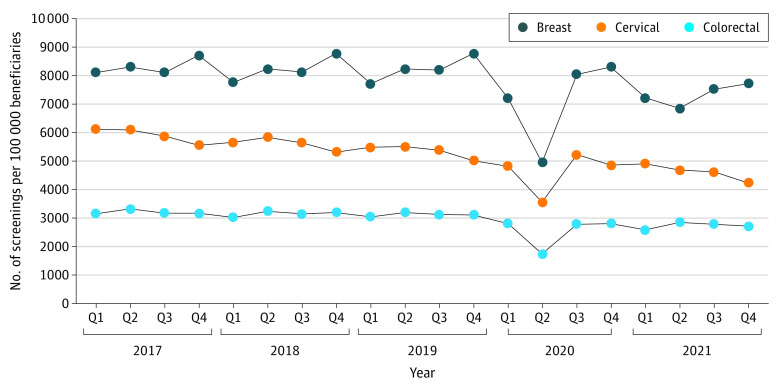
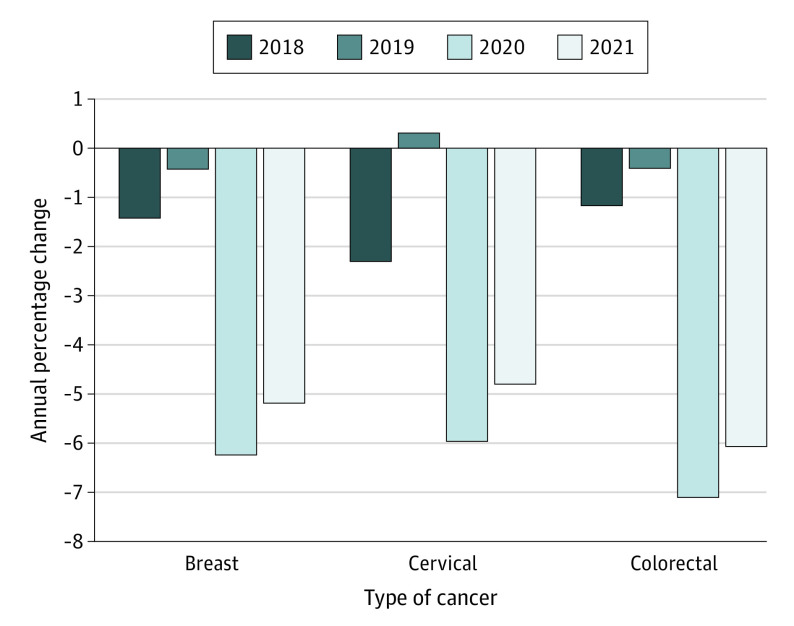
The analysis included 306 million unique individuals with a mean (SD) age of 51.5 (17.2) years; 167 558 961 were female (54.6%) and 139 438 790 were male (45.4%) individuals, and the mean (SD) Charlson Comorbidity Index score was 0.7 (1.7) (0 indicates no comorbid conditions). For breast cancer, the median (IQR) quarterly rate of prepandemic screening mammography was 8216 (8116-8407) per 100 000 beneficiaries, which declined to 4951 in quarter (Q) 2 of 2020—a 40% decrease (Figure 1). Screening mammography rebounded to prepandemic levels by Q3 and Q4 of 2020 but declined to a median (IQR) rate of 7374 (7127-7577) per 100 000 beneficiaries in 2021, with quarterly deficits ranging from 6% to 17%. For cervical cancer, the median (IQR) quarterly rate of prepandemic screening was 5602 (5462-5851) per 100 000 beneficiaries. The rate of cervical cancer screening fell to 3563 in Q2 of 2020—a 36% decline. By Q3 of 2020, cervical cancer screening rebounded toward the prepandemic median, then progressively declined from 4853 in Q4 of 2020 to 4246 in Q4 of 2021. Colorectal cancer screening decreased from a prepandemic median (IQR) of 3162 (3126-3202) per 100 000 beneficiaries to 1746 in Q2 of 2020—a 45% difference. From Q3 of 2020 to Q4 of 2021, quarterly colorectal cancer screening ranged from 2590 to 2861 per 100 000 beneficiaries, 82% to 90% of the prepandemic median. Consistent with the reported reductions in cancer screening, prevalence rates declined by 6.0% to 7.1% between 2019 and 2020 and an additional 4.8% to 6.1% between 2020 and 2021 (Figure 2).
Figure 1. Breast Cancer, Cervical Cancer, and Colorectal Cancer Screening Rates by Quarter (Q) From 2017 to 2021.
Figure 2. Annual Percentage Change in Breast Cancer, Cervical Cancer, and Colorectal Cancer Prevalence Rates.
Discussion
In this cross-sectional study, population-based screening and diagnosis remained below prepandemic levels for the 3 cancer types. The findings suggest that screening quickly rebounded after the initial stages of the pandemic; however, the longer follow-up time reveals that gaps in preventive cancer screening returned and worsened.3,4,5,6 A strength of the study was using a nationally representative, all-payer data set. A limitation of the study was that the reason for each test was not examined (eg, screening vs problem or diagnostic reason). The pattern we found suggests a substantial proportion of forgone care through 2021. To mitigate long-term consequences, multiple stakeholders will need to consider novel strategies and dedicate appropriate resources to increase guideline-concordant cancer screening.
References
- 1.Czeisler ME, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns: United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250-1257. doi: 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Unger JM. Cancer care during COVID-19—a shock to the system. JAMA Netw Open. 2022;5(4):e228864. doi: 10.1001/jamanetworkopen.2022.8864 [DOI] [PubMed] [Google Scholar]
- 3.McBain RK, Cantor JH, Jena AB, Pera MF, Bravata DM, Whaley CM. Decline and rebound in routine cancer screening rates during the COVID-19 pandemic. J Gen Intern Med. 2021;36(6):1829-1831. doi: 10.1007/s11606-021-06660-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh QD. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. 2021;7(3):458-460. doi: 10.1001/jamaoncol.2020.7600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fedewa SA, Star J, Bandi P, et al. Changes in cancer screening in the US during the COVID-19 pandemic. JAMA Netw Open. 2022;5(6):e2215490. doi: 10.1001/jamanetworkopen.2022.15490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878-884. doi: 10.1001/jamaoncol.2021.0884 [DOI] [PMC free article] [PubMed] [Google Scholar]