Abstract
Various U.S. states and municipalities raised their mandated minimum wages between 2017 and 2019. In some areas, minimum wages became high enough to bind for more professional workers, such as lower paid staff at nursing facilities. We add to the small prior literature on the effects of minimum wages on nursing facility staffing using novel establishment-level data on daily hours worked; these data allow us to examine changes in staffing hours along margins previously unexplored in the minimum wage literature. We find no evidence that minimum wage increases reduced hours worked among lower-paid nurses in nursing facilities. In contrast, we find that increases in state and local minimum wages increased hours worked per resident day by nursing assistants; increases occurred for the average of all days throughout the month and on weekend days. We also find that a higher minimum wage increased the share of days in the month that facilities meet at least 75% of the minimum recommended levels of staffing for nursing assistants. These results lessen concerns that minimum wage hikes may reduce the quality of resident care at nursing facilities.
Keywords: Minimum wage, Nursing, Hours, Employment, Nursing facility
Introduction
Recent changes to state and municipal laws make the U.S. a promising context for the study of employment effects of the minimum wage. Although the U.S. federal minimum wage has been $7.25 per hour since 2009, most states have higher minimum wages, and between 2017 and 2019, about half of all states raised their minimum wage rates (Vaghul and Zipperer 2019). In addition, localities are increasingly likely to set minimum wages above the federal level. Prior to 2012, five localities had minimum wage ordinances; by 2019, more than 40 counties and cities had such laws (UC-Berkeley Center for Labor Research 2019). Recent legislative activity has raised minimum wages considerably in some areas. States including California, Illinois, Maryland, Massachusetts, and New Jersey are in the process of raising minimum wages to $15 per hour. Maine and Colorado implemented increases of $2/hour and $1.80/hour between 2017 and 2019, bringing minimum wages close to $11/hour in these states. By the end of 2019, some cities had hourly minimum wages as high as $12.50 (Portland, OR), $13 (Chicago, IL), and $15 (New York City).
Because minimum wages in the U.S. have been fairly low historically, most prior research has focused on their impacts on “casual” employment, that is, on the employment of teenage, retail, and restaurant workers. Yet, recent legislation has set minimum wages high enough to have potential impacts on lower-paid professional workers, such as childcare and early education professionals, and even some university employees. Little is known about the employment effects of minimum wages that bind to professional workers. More empirical research in this area is needed since economic theory offers differing predictions. If the labor market is competitive, theory suggests that minimum wages reduce the quantity of labor demanded; if market imperfections (e.g., monopsony labor markets, search costs, asymmetric information) exist, employment could increase in response to a minimum wage. For example, in a model with search costs, higher minimum wages may lead workers with higher reservation wages to enter the labor market, and employment may increase as these workers are hired.
Larger minimum wage hikes may affect the employment of some healthcare professionals, such as nursing assistants or even some licensed practical nurses (LPNs). Nursing assistants help patients with activities of daily living (e.g., bathing, toileting, eating, etc.) and by monitoring patients’ health concerns and vital signs, while LPNs provide basic medical care. Nursing facilities are the single largest employer of both types of workers in the U.S., employing 37% of nursing assistants and 38% of LPNs (U.S. Bureau of Labor Statistics 2021a, b). Table 1 reports 2017–2019 wage data from the Current Population Survey for workers in these occupations employed in the nursing facility industry. One-tenth of nursing assistants earned less than $10 per hour and 25% earned less than $11 per hour. Additionally, the wages of some LPNs are low enough to be impacted by minimum wage increases, with 7% paid wages below 120% of their state’s minimum wage, and 17% paid less than 150% of their state minimum wage.1 In contrast, median hourly wages are much higher for RNs and very small percentages of registered nurses (RNs) employed at nursing facilities had wages below these thresholds.
Table 1.
Wage distributions of nursing occupations employed in nursing and residential care facilities, January 2017-December 2019
| Sample size | 10th percentile wage ($) |
25th percentile wage ($) |
Median wage ($) |
Share with wages < 120% of state minimum wage | Share with wages < 150% of state minimum wage | |
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Nurse aides | 1,420 | 10 | 11 | 12.9 | 0.14 | 0.50 |
| LPNs | 370 | 11 | 14 | 19 | 0.07 | 0.17 |
| RNs | 567 | 15.6 | 21.6 | 27.9 | 0.01 | 0.06 |
Source: Authors’ calculations from the pooled 2017–2019 Current Population Survey, Outgoing Rotation Groups (Earner Study), from IPUMS (Flood et al. 2020). Observations are weighted using EARNWT. Nurse aides include nursing, psychiatric, and home health aides (occ2010 = 3600), LPNs include licensed practical and licensed vocational nurses (occ2010 = 3500), and RNs include registered nurses (occ2010 = 3130). Nursing and residential care facilities defined as industry codes 8270 and 8290
Potential changes to staffing at nursing facilities are of particular interest to policy makers given the association between nurse staffing and the quality of resident care (e.g., Bostick et al. 2006; Konetzka et al. 2008; Castle 2008; Walsh et al. 2014; Dellefield et al. 2015) and in light of persistent deficiencies in the quality of care (e.g., IOM 1986, 1996; Mor et al. 2009; U.S. GAO 2018). This evidence has spurred various federal and state efforts to increase nurse staffing, such as regulations, payment-based incentives, and workforce development programs. Despite this important policy context, few prior studies have studied the effects of minimum wages on nursing facility employment. Studying national minimum wage increases that took place in the U.K. in 2015-16, Vadean and Allan (2021) found no evidence of a decline in the number of workers employed at care homes, but found that weekly hours worked fell in some residential care facilities. In contrast, in a study of U.S. state and local minimum wage increases between 1992 and 2017, Ruffini (2021) found no evidence that nursing assistant hours per resident day fell at nursing facilities, and some evidence that the number of nursing assistants employed increased.
In this study, we add to the small literature on the effects of minimum wages on nursing facility staffing. Like Ruffini (2021), we focus on the U.S. context, but our work differs in two primary ways. First, we focus on state and local minimum wage changes that took place between 2017 and 2019. As noted earlier, many of the recent increases were much larger, and resulted in much higher, and therefore more binding, minimum wages than their historical precedents. For example, in 2012, only one state (Washington) had a minimum wage higher than the 10th percentile in the national distribution of nursing assistant wages, while in 2019, 10 states did.2 For this reason, the null effects on nursing assistant hours worked documented in prior time periods may not extend to these recent wage policies. As we subsequently show, the bite of the minimum wage, as measured by the ratio of the minimum wage to the local median wage for nursing assistants, was relatively high for large shares of facilities and localities in our data.
Second, we use a new data source -- the Payroll-Based Journal (PBJ) data collected by the Centers for Medicare and Medicaid Services (CMS) under the Affordable Care Act. These data consist of staffing reports for each day of the year made by nearly all U.S. nursing facilities. In comparison, Ruffini (2021) uses facility-year level data on nurse staffing sourced from OSCAR/CASPER and quarterly county-level data on employment in the nursing facility industry. By using PBJ data, we are able to examine facility-level measures at a higher frequency, which avoids certain measurement errors that may arise when using OSCAR/CASPER data to look at minimum wage changes. That is, the OSCAR/CASPER measure period is two weeks, and most analyses apply that two-week measure to the entire calendar year, while in contrast minimum wage increases can occur in the midst of the calendar year. Moreover, we use the PBJ data to examine changes in margins of employment that cannot be examined in the OSCAR/CASPER data, such a weekend staffing and staffing levels in comparison to minimum recommended staffing guidelines.
To preview our results, we find no evidence that increases in the minimum wage reduce hours worked by lower-paid nurses in nursing facilities. In contrast, we find that state and local minimum wages increase the hours per resident day by nursing assistants, both throughout the month and on weekend days. We also find that a higher minimum wage increases the share of days in the month that facilities meet at least three-quarters of the minimum recommended levels of staffing for nursing assistants. These results add to prior evidence from Ruffini (2021) by demonstrating that the larger minimum wages established by recent legislation have positive and significant effects on nursing assistant hours per resident day at nursing facilities, and they contrast with findings from the UK that suggest minimum wages reduce hours worked at some residential care facilities.
This paper is structured as follows: in the second section, we describe the prior literature on minimum wages in more detail. In the third section, we describe our methods and data. We present and discuss our results in the fourth and fifth sections and offer our main conclusion in the sixth section.
Prior Literature
Much of the extant empirical minimum wage literature has examined teen employment or employment in specific industries with large numbers of low-wage workers, namely fast food, restaurant, and retail workers. This extensive literature, reviewed in numerous other papers, has produced estimates of the elasticity of employment with respect to the minimum wage that vary in sign and size. For example, Neumark et al. (2014a, b) report negative and statistically significant elasticities for teens and restaurant workers. In contrast, Dube et al. (2010), Allegretto et al. (2010), and Allegretto et al. (2017) find no significant effects of the minimum wage on teen employment, while some case studies of minimum wage increases report positive and significant effects on fast food employment (e.g., Katz and Krueger 1992; Card and Krueger 1994). Methodological differences contribute to these mixed empirical findings.3 Null employment effects may arise when the minimum wage does not bind due to existing high market wages (e.g., Cengiz et al. 2019).
Economic theory can explain both negative and positive minimum wage elasticities. Negative elasticities are explained by the standard prediction that higher wages reduce the quantity of labor demanded in competitive labor markets. Positive estimates from the literature could be explained by a number of market frictions. For example, in a model with search costs, higher minimum wages can lead workers with higher reservation wages to enter the market, and employment would increase as these workers are newly hired by firms. Alternatively, in a model where firms lack information about worker quality and workers lack knowledge of firm-specific wage offers, a higher minimum wage can lead higher-quality workers to enter the labor market. Guiliano (2013) finds some evidence consistent with both of these explanations using detailed data on workers in one retail chain: higher minimum wages increased the share of new hires who were teens, and increased the employment of teens who were “higher quality” workers. Positive minimum wage elasticities can also arise in labor markets characterized by monopsony power. A monopsony firm paying the same wage to all workers faces a relatively high marginal cost of increasing employment: to recruit an additional worker it needs to raise the wage rate to all its workers. Within a moderate range of wages, a minimum wage reduces this hiring cost at the margin because the firm does not need to raise all its workers’ wages to increase employment. Consistent with this, Azar et al. (2019) use novel data on job postings to measure labor market concentration and find that minimum wages increase employment in the most highly concentrated markets.
A small number of prior studies have examined effects of the minimum wage on healthcare professionals. Three such studies examine the effects of minimum wage policies in the U.K. on employment in the long-term care sector. Machin et al. (2003) and Machin and Wilson (2004) found evidence of modest declines in long-term care facility employment in response to wage increases. More recently, Vadean and Allan (2021) found that national minimum wage increases in 2015-16 led to a temporary reduction in long-term care facility employment, but a large and more persistent reduction in hours worked, a difference the authors attribute to regulations that discourage firms from reducing the number of workers employed.
In the U.S., some prior studies have examined the link between average wages and hours worked in the nursing facility industry using the state minimum wage as an instrument for state-level wages. The first stage results from both Cawley et al. (2006) and Grabowski et al. (2011) show that nursing home worker average wages increased with the minimum wage. Both studies find evidence of factor substitution (between labor and materials in the form of prescription drugs); neither aims to quantify the direct effect of minimum wages on nursing facility employment.
Ruffini (2021), which also focuses on the nursing facility employment effects of minimum wage increases in the U.S., is closest to our study. Focusing on state and local minimum wages from 1992 to 2017, Ruffini (2021) finds no significant effects on county-level employment of female high school graduates in the nursing facility sector (a proxy for nursing assistant employment). This study also modeled minimum wage effects on facility-level employment, using facility-year data from OSCAR/CASPER, which measures staffing prior to facilities’ state inspections. Results provided no evidence that nursing assistant hours per resident day fell and some evidence that the number of nursing assistants employed increased in response to the minimum wage.
We add to this prior literature in two ways. First, as noted earlier, we focus on U.S. minimum wage increases in 2017–2019, during a time when minimum wages were relatively high. Second, we use a new source of facility-level data on nurse hours that offers some advantages relative to OSCAR/CASPER data. OSCAR/CASPER measures nurse staffing from a survey that asks facilities to report staffing in the two-week period prior to a state inspection. Since inspections occur every 9 to 15 months, these measures are often used to provide annual staffing measures; however, this may create some measurement error when aligning hours with the relevant minimum wage when wages change. This is because actual staffing may fluctuate throughout the year and because minimum wage increases often go into effect during the calendar year (i.e., not always on January 1). In contrast, the PBJ data provide daily records of nurse hours worked throughout the year. We aggregate these to monthly averages and are able to align staffing measures with minimum wage changes more precisely.
We also use the daily records to construct measures of hours worked that allow us to examine changes in nurse employment on margins previously unexamined in the minimum wage literature. One such margin is nurse hours worked on weekend days, as opposed to weekdays. Prior research has shown that facilities report considerably lower staffing levels on weekend days as compared to weekdays (Geng et al. 2019). Weekend time per resident day was 17% less than weekday time for LPNs, and 9% less for nursing assistants (Geng et al. 2019, p. 1097). Another margin of employment is the tendency for facilities to meet minimum recommended staffing guidelines. Though not federally mandated, CMS (2001) suggests that facilities have at least 2.8 hours of Certified Nursing Assistants (CNAs) on staff per resident day. Prior studies have not examined the effects of minimum wages on these margins of employment. We describe these measures, and other features of our empirical approach, in more detail below.
Empirical Methods
Data
We obtain data on recent minimum wage hikes occurring at the state and local levels using data from two sources. First, we use the Vaghul and Zipperer (2016, 2019) data, which are intended to include all state and municipal minimum wage legislation enacted through December 31, 2019. We then compared these to data from the UC-Berkeley Center for Labor Research and Education (2019). This comparison identified a few additional local minimum wage increases in our time period, which we added to our analysis.
Tables 6 and 7 of the Appendix list the areas affected by these laws in the period we study (January 2017 - December 2019). As shown in Table 6, 24 states (counting the District of Columbia as a state) in our sample experienced minimum wage increases. The mean increase was $1.015, and the largest increase was $2.50 (D.C.). Seven additional states increased their minimum wages by more than $1 (California, Colorado, Maine, Maryland, New Jersey, New York, and Oregon). By the last month of our study period, the minimum wage was at least $10 per hour in 14 states.
Table 6.
States (including D.C.) with minimum wage increases, 2017–2019
| State | January 2017 minimum wage | December 2019 minimum wage | Increase |
|---|---|---|---|
| Alaska | 9.80 | 9.89 | 0.09 |
| Arizona | 10 | 11 | 1 |
| Arkansas | 8.50 | 9.25 | 0.75 |
| California | 10.5 | 12 | 1.50 |
| Colorado | 9.30 | 11.10 | 1.80 |
| Delaware | 8.25 | 9.25 | 1 |
| District of Columbia | 11.50 | 14 | 2.50 |
| Florida | 8.10 | 8.46 | 0.36 |
| Hawaii | 9.25 | 10.1 | 0.85 |
| Maine | 9 | 11 | 2.00 |
| Maryland | 8.75 | 10.10 | 1.35 |
| Massachusetts | 11 | 12 | 1.00 |
| Michigan | 8.90 | 9.45 | 0.55 |
| Minnesota | 9.50 | 9.86 | 0.36 |
| Missouri | 7.70 | 8.60 | 0.90 |
| Montana | 8.15 | 8.50 | 0.35 |
| New Jersey | 8.44 | 10 | 1.56 |
| New York | 9.70 | 11.12 | 1.42 |
| Ohio | 8.15 | 8.55 | 0.40 |
| Oregon | 9.75 | 11.25 | 1.50 |
| Rhode Island | 9.60 | 10.50 | 0.90 |
| South Dakota | 8.65 | 9.10 | 0.45 |
| Vermont | 10 | 10.78 | 0.78 |
| Washington | 11 | 12 | 1 |
| Mean [Max] Increase | 1.015 [2.5] |
Source: Authors’ calculations using Vaghul and Zipperer (2019), Updated Minimum Wage Data Set [available at https://github.com/benzipperer/historicalminwage, accessed on June 4, 2019]
Table 7.
Sub-state areas with minimum wage increases, 2017–2019
| State | Locality | January 2017 minimum wage |
December 2019 minimum wage |
Increase | |
|---|---|---|---|---|---|
| Arizona | Flagstaff | 10 | 12 | 2 | |
| California | Alameda | 10.5 | 13.5 | 3 | |
| Belmont | 10.5 | 13.5 | 3 | ||
| Berkeley | 12.53 | 15 | 2.47 | ||
| Cupertino | 12 | 15 | 3 | ||
| Fremont | 10.5 | 13.5 | 3 | ||
| Los Altos | 12 | 15 | 3 | ||
| Los Angeles | 10.5 | 14.25 | 3.75 | ||
| Los Angeles County | 10.5 | 14.25 | 3.75 | ||
| Milpitas | 10.5 | 12 | 1.5 | ||
| Mountain View | 13 | 15.65 | 2.65 | ||
| Oakland | 12.86 | 13.8 | 0.94 | ||
| Palo Alto | 12 | 15 | 3 | ||
| Pasadena | 10.5 | 14.25 | 3.75 | ||
| Redwood City | 10.5 | 13.5 | 3 | ||
| Richmond | 12.3 | 15 | 2.7 | ||
| San Diego | 11.5 | 12 | 0.5 | ||
| San Francisco | 13 | 15.59 | 2.59 | ||
| San Jose | 10.5 | 15 | 4.5 | ||
| San Leandro | 10.5 | 14 | 3.5 | ||
| San Mateo | 12 | 13.5 | 1.5 | ||
| Santa Clara | 11.1 | 15 | 3.9 | ||
| Santa Monica | 10.5 | 14.25 | 3.75 | ||
| Sunnyvale | 13 | 15.65 | 2.65 | ||
| Iowa | Johnson County | 10.1 | 7.25 | -2.85 | |
| Linn County | 8.25 | 7.25 | -1 | ||
| Wapello County | 8.2 | 7.25 | − 0.95 | ||
| Illinois | Chicago | 10.5 | 13 | 2.5 | |
| Cook County | 8.25 | 12 | 3.75 | ||
| Maine | Bangor | 9 | 11 | 2 | |
| Portland | 10.68 | 11 | 0.32 | ||
| Maryland | Montgomery County | 10.75 | 13 | 2.25 | |
| Prince George’s County | 10.75 | 11.5 | 0.75 | ||
| Minnesota | Minneapolis | 9.5 | 11 | 1.5 | |
| New Mexico | Albuquerque | 8.8 | 9.2 | 0.4 | |
| Bernalillo County | 8.7 | 9.05 | 0.35 | ||
| Las Cruces | 9.2 | 10.1 | 0.9 | ||
| Santa Fe | 10.91 | 11.8 | 0.89 | ||
| New York | New York City | 11 | 15 | 4 | |
| Long Island & Westchester | 10 | 12.03 | 2.03 | ||
| Oregon | Nonurban counties | 9.5 | 11 | 1.5 | |
| Portland | 9.75 | 12.5 | 2.75 | ||
| Washington | Seattle | 13 | 15 | 2 | |
| Tacoma | 11.15 | 12.35 | 1.2 | ||
| Mean [Max] Increase | 2.36 [4.5] | ||||
Source: Authors’ calculations using Vaghul and Zipperer (2019), Updated Minimum Wage Data Set [available at https://github.com/benzipperer/historicalminwage, accessed on June 4, 2019], and UC Berkeley Center for Labor Research and Education (2019), Inventory of Local Minimum Wage Ordinances (Cities and Counties). In Oregon, the nonurban rate applies to employers located within the following counties: Baker, Klamath, Coos, Lake, Crook, Malheur, Curry, Morrow, Douglas, Sherman, Gilliam, Umatilla, Grant, Union, Harney, Wallowa, Jefferson, and Wheeler
Table 7 shows that 40 sub-state areas in our sample had minimum wage increases; 23 are California localities. The average increase in the sub-state minimum wage was $2.36 per hour and the largest increase was $4.50 per hour (San Jose, CA). Most increases (32) were $1 or more, and in 27 localities the wage increased by $2 or more. By the last month of our study period, the minimum wage was at least $10 per hour in 38 localities and at least $12 in 32 localities. The local minimum wage fell in three Iowa counties after the State of Iowa prohibited Iowa municipalities from setting minimum wage levels in March 2017.
We obtain nurse employment from publicly available Payroll Based Journal (PBJ) data on average daily nurse staffing hours. The PBJ data are collected under Sect. 6106 of the Affordable Care Act (ACA), which requires all nursing facilities, as of 2017, to electronically submit daily staffing hours for individual categories of nursing staff. Facilities report hours that staff are paid to deliver services; these reports do not include break times, leave time or absences. The public data include daily hours separately by occupation and the daily census of facility residents for approximately 15,800 facilities nationwide. We exclude in-hospital and government-run nursing facilities (identified with 2017 NHC data) given the different business models these facilities may follow. Of the total of 15,765 unique facilities in our data at the start of our time period of study, 614 were in-hospital facilities and another 772 were government owned facilities, leading us to exclude 8.8% of facilities. We use the PBJ data from January 1, 2017 (the first month the data are available) through December 31, 2019 (which pre-dates the outbreak of coronavirus in the U.S. and its impacts on nursing homes). We aggregate the daily records to monthly-level data to construct the outcomes of interest for each facility in our dataset.
Our primary outcome is nursing assistant hours per resident day (HPRD), defined as the average of daily staff hours worked across all days in the month divided by the average of daily resident census across all days in the month.4 The wage data presented earlier suggest that nursing assistants are most exposed to minimum wage increases. To measure nursing assistant hours worked, we combine PBJ data on hours by certified nursing assistants (CNAs), nurse aides in training, and medication aides. Nurse aides in training are in their first four months of employment and working toward state certification (CMS 2018), while medication aides are CNAs with additional experience and/or training to dispense medication under the supervision of a licensed nurse (LPN or RN). Given the wage distributions in Table 1, some LPNs may also be affected by minimum wages increases, so we also define a measure of LPN HPRD. Although RN wages are unlikely to be affected directly, we use a measure of RN HPRD to test for spillovers from minimum wage increases to RN employment, given prior evidence that RN labor may serve as a substitute for less skilled nursing labor (e.g., Hyer et al. 2009). For both LPN and RN hours, we include hours for nurses with and without administrative duties, and for RNs we also include hours by RN directors of nursing. For all occupations, we include hours by agency and contract staff as well as by direct employees of the facility.
We use the rich detail provided by the daily PBJ data to construct additional outcomes, and we use these measures to test for changes in nursing assistant hours along margins that may be obscured by average hours per resident day. To test whether weekend staffing is more sensitive to minimum wage changes, we calculate weekend hours per resident day as the average of daily staff hours across Saturdays and Sundays in the month, divided by the average of daily resident census across Saturdays and Sundays in the month. To test whether minimum wage increases affect facility staffing levels in relation to minimum recommended levels, we construct the share of days in the month that a facility meets the minimum threshold. Because facilities meet this threshold infrequently, the mean of this variable is quite low. As an alternate measure, we also construct the share of days in the month that a facility meets 75% of the minimum threshold. This is admittedly arbitrary, but it provides an opportunity to capture variation in the outcome that the former measure does not. We define both of these measures separately for all days in the month and weekend days. As the threshold, we use 2.8 hours of Certified Nursing Assistants (CNAs) per resident day from CMS (2001). To measure CNA hours per resident day, we combine hours for CNAs and medication aides (CNAs with additional qualifications) from the PBJ. In a sensitivity test, we check that we obtain similar results using CNA hours alone.
We assign minimum wages to facility-month observations using monthly minimum wage data from 2017 to 2019 obtained from Vaghul and Zipperer (2019) and the UC Berkeley Center for Research and Education (2019). Prior to merging state laws, we examine each ordinance to determine the applicability of the law to nursing homes, since laws in some areas specify exceptions or alternative minimums based on the number of employees at the establishment or whether the establishment is a non-profit. In those municipalities, we assign minimum wage levels appropriate for the specific facility given its size or ownership type. For example, in Seattle, in some months of our period, a $16/hour wage applies only to establishments with 500 or more employees; since nursing facilities employ fewer than 500 workers, we therefore assign the lower $15/hour wage to Seattle facilities in those months. Similarly, in Minneapolis, where the minimum wage applies to businesses with 100 or fewer employees, we use estimated facility size when assigning the minimum wage.5
To further illustrate the potential for recent minimum wages to affect nursing assistant employment, we obtained 2016 median wages for nursing assistants (occupation code 31-1014 in that year) for each minimum wage area in our sample (all states, and local labor markets with minimum wage increases) from the U.S. Bureau of Labor Statistics (2022). We matched these data to January 2017 minimum wage levels by state/locality to calculate a Kaitz index (the ratio of the minimum wage to the median nursing assistant wage) for each location in our data in the first quarter of our period. Figure 1A and B report the distribution of this Kaitz index across facilities and areas in our dataset, and show that large shares of facilities and areas have index values that are relatively high. For example, 83% of facilities and 82% of areas have Kaitz index values of 0.6 or higher; 22% of facilities and 35% of areas have Kaitz index values of 0.7 or higher. For comparison, in Cengiz et al. (2019) which found no employment effects, the maximum Kaitz index value for all wage earners was 0.59 in localities with minimum wage increases.
Fig. 1.
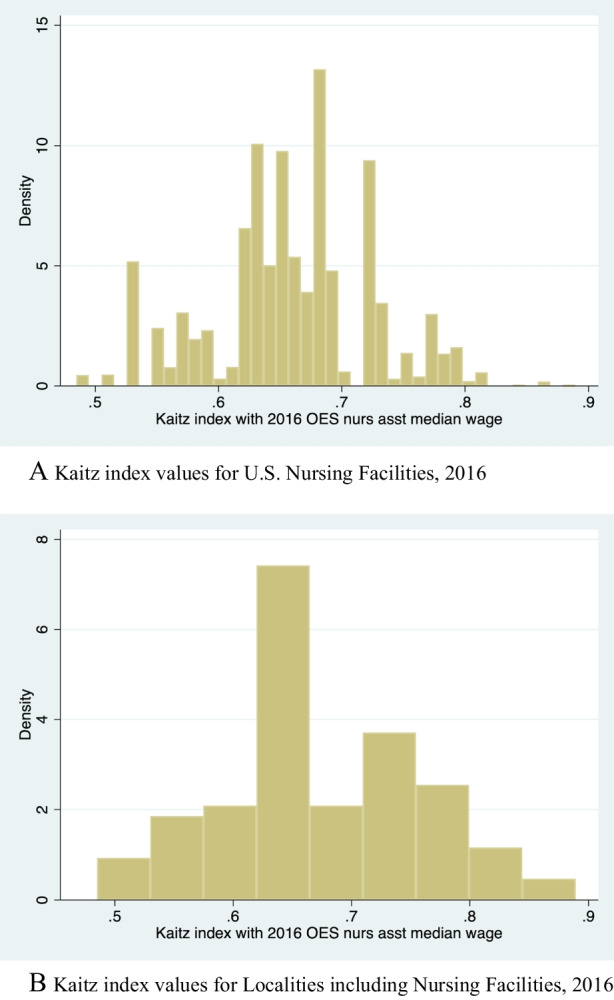
Ratio of state/local minimum wage to median nursing assistant wages, 2016. A Kaitz index values for U.S. Nursing Facilities, 2016. B Kaitz index values for Localities including Nursing Facilities, 2016. Notes: Each figure reports the distribution of a Kaitz index for facilities/localities in our sample in the first quarter of 2017. We define the Kaitz Index as the ratio of the minimum wage in effect in the state (or locality if the local minimum wage exceeds the state minimum wage) in January 2017 to the median wage for nursing assistants in the state/locality in 2016. Median wage data are sourced from the U.S. Bureau of Labor Statistics (2022) for occupation code 31-1014
Estimation
To identify the causal effects of the minimum wage on occupation-specific measures of hours worked, we estimate a generalized difference-in-differences model using our facility-month data, as shown in Eq. (1):
| 1 |
The dependent variable is one of several outcome measures defined above: the log of average HPRD in the month, the log of average HPRD for weekend days in the month, or the share of days (or weekend days) in the month the facility meets a threshold of minimum recommended staffing. Outcomes are specific to a given occupation of workers (nursing assistants, LPNs, or RNs) at facility i in state or locality j, in month t, where t is equal to 1 for the 1st month in our dataset, 2 for the 2nd, and so on, for the 36 months in the sample.
The key explanatory variable is the log of the minimum wage currently in effect in state or locality j in month t. We control for the unemployment rate in the county (c) in which the facility is located and the month, and we include facility fixed effects in λi to capture time-invariant facility traits associated with employment levels (e.g., the facility’s mix of rehabilitation and skilled nursing care, and because facilities do not change location, any time invariant factors associated with the locality). We include month fixed effects in τt to capture national trends in employment. We include state-by-fiscal year effects in θsy to capture state-specific factors that vary over time (e.g., other state policies that could affect nursing facility employment, such as state minimum staffing requirements). Standard errors are adjusted for clustering at the state/locality level (j). The identifying assumption is that in the absence of the minimum wage change, nursing hours would follow a similar trend in localities that raised the minimum wage and those that did not.
A potential concern in a difference-in-differences identification strategy like ours is that minimum wage increases might be more likely in places that were already experiencing staffing trends. Evidence of pre-trends in staffing would suggest that correlations with minimum wages are incidental and may not accurately reflect the causal effect of minimum wage policies on staffing. To investigate whether pre-trends arise in our context, we examine coefficients {δk} from the estimation of Eq. (2):
| 2 |
where Δ is the first-difference operator. The estimates of {δk} represent cumulative policy effects at different horizons (Freyaldenhoven et al. 2021). For example, the estimate of the δ coefficient associated with t = 3 represents the sum of minimum wage effects during the month of the policy change and the next three months. We assume in these specifications that the minimum wage is not related directly to outcomes (i.e., staffing hours) more than 7 months earlier or later. Estimates of δ coefficients before t=-1 (which is normalized to zero) indicate whether there are staffing differences in locations that later experienced different minimum wage policies (i.e., pre-trends).
Results
Table 2 reports the means of the occupation-specific outcomes of interest across facility-months in our estimation sample, which consists of 474,133 facility-month observations. Mean HPRD is greatest for nursing assistants at 2.289, followed by LPNs at 0.874 and RNs at 0.634. Nursing assistant HPRD are somewhat lower on the weekends than weekdays. On average, facilities meet the recommended CNA staffing threshold (2.8 CNA HPRD) 11.4% of days overall and only 7.5% of weekend days. Facilities on average attain 75% of the recommended CNA staffing threshold (2.1 CNA HPRD) 51.5% of days overall and 41.8% of weekend days.
Table 2.
Descriptive statistics for staffing hours measures, 2017–2019
| All facility-month observations | |||
|---|---|---|---|
| Obs | Mean | Std. Dev | |
| Nursing Assistant HPRD, daily average, n = 474,133 | 474,133 | 2.289 | 0.522 |
| LPN HPRD, daily average | 474,133 | 0.873 | 0.343 |
| RN HPRD, daily average | 474,133 | 0.634 | 0.411 |
| Nursing Assistant HPRD, weekend day average | 474,133 | 2.147 | 0.515 |
| % days in month meeting min. rec. staffing for CNAs | 474,133 | 0.114 | 0.253 |
| % weekend days in month meeting min. rec. staffing for CNAs | 473,567 | 0.075 | 0.219 |
| % days in month meeting 75% min. rec. staffing for CNAs | 474,133 | 0.515 | 0.404 |
| % weekend days in month meeting 75% of min. rec. staffing for CNAs | 473,567 | 0.418 | 0.424 |
Source: Authors’ calculations from the Payroll-Based Journal data, January 2017-December 2019. Facilities reported the number of staffing hours across all workers in a given occupational category each day. HPRD = Hours per resident day
We present our main results in Table 3, which reports the coefficient estimates of γ from regressions of the log of average daily HPRD by occupation following Eq. (1). In panel A, we find no evidence that lower-paid nursing hours decrease in response to the minimum wage. For nursing assistant HPRD, the estimated minimum wage elasticity is positive and significant. The magnitude suggests that a 10% increase in the minimum wage increases nursing assistant hours by 0.65%, or 0.015 HPRD, evaluated at the mean. For a facility with 100 residents on a given day, this is equivalent to 1.5 additional nursing assistant hours per day or 45 hours per month. For both LPNs and RNs, the estimated minimum wage elasticities are statistically insignificant.
Table 3.
Effects of state/local minimum wages on facility staffing HPRD
| log (Nursing assistant HPRD) | log (LPN HPRD) |
log (RN HPRD) |
|
|---|---|---|---|
| (1) | (2) | (3) | |
| Panel A: Full Sample | |||
| log (min wage) | 0.065*** | 0.049 | 0.053 |
| (0.023) | (0.042) | (0.046) | |
| Dep var mean (level) | 2.29 | 0.876 | 0.635 |
| No. of facilities | 14,143 | 14,122 | 14,146 |
| No. of observations | 474,033 | 472,291 | 473,910 |
| Panel B: Facilities not constrained by Direct Care staffing requirements | |||
| log (min wage) | 0.054 | -0.057 | -0.002 |
| (0.035) | (0.038) | (0.071) | |
| Dep var mean (level) | 2.31 | 0.883 | 0.644 |
| No. of facilities | 11,619 | 11,603 | 11,619 |
| No. of observations | 396,403 | 394,926 | 396,287 |
| Panel C: Facilities in areas with high Kaitz index for nursing assistants (> January 2017 median) | |||
| log (min wage) | 0.050 | 0.117* | -0.020 |
| (0.039) | (0.060) | (0.083) | |
| Dep var mean (level) | 2.34 | 0.889 | 0.614 |
| No. of facilities | 6,279 | 6,269 | 6,279 |
| No. of observations | 216,781 | 216,086 | 216,682 |
| Panel D: Facilities in areas with high Kaitz index for nursing assistants (> 0.6) | |||
| log (min wage) | 0.057*** | 0.041 | -0.012 |
| (0.021) | (0.043) | (0.051) | |
| Dep var mean (level) | 2.29 | 0.888 | 0.611 |
| No. of facilities | 10,371 | 10,359 | 10,371 |
| No. of observations | 358,214 | 357,207 | 358,100 |
Observations are facility-months. HPRD = hours per resident day, measured as the average of daily total occupation-specific hours divided by daily resident census, across all days in the month. Robust standard errors (clustered by locality) are reported in parentheses. Statistical significance is indicated by *** p < 0.01, ** p < 0.05, * p < 0.1. All models also include the monthly county unemployment rate, facility fixed effects, year-by-month fixed effects, state fixed effects, and state-by-fiscal year fixed effects
It is possible that state minimum staffing regulations constrain facilities from reducing hours worked. To test this, we estimated our models on a sample of nursing facilities unlikely to be constrained by minimum staffing requirements. For this test, we include all facilities in the 18 states that do not have direct care staffing requirements according to the National Consumer Voice for Quality Long-Term Care (2022) as well as facilities with direct care staffing in excess of the state’s minimum by a high enough margin so that even with a large employment reduction the facility would continue to meet state mandated minimum staffing requirements.6 Panel B of Table 3 reports the results. Among facilities not constrained by direct care staffing requirements, we do not find any evidence of reductions in hours in response to the minimum wage. The point estimate for the minimum wage elasticity remains positive for nursing assistant HPRD but is not precisely estimated.
In another test for possible evidence of negative minimum wage elasticities, we focused on facilities in areas where median wages for nursing assistants relative to the minimum wage were relatively high, and where the minimum wage may have more “bite.” We obtained data on median wages for nursing assistants for all areas in our analysis from the U.S. Bureau of Labor Statistics (2022) for 2016, the year before our sample begins, and we constructed a Kaitz index for nursing assistant wages (the ratio of the January 2017 minimum wage to the 2016 median wage for each area). We then selected facilities in areas that were in the top half of the distribution of the Kaitz index (index values greater than 0.63) and for which minimum wage increases may be more binding, and we estimated our models on this group. The results are reported in Panel C of Table 3. Among facilities in areas with high Kaitz index values, we again do not find any evidence of reductions in hours in response to the minimum wage. The point estimate for the minimum wage elasticity remains positive for nursing assistants but is not precisely estimated. The point estimate for the minimum wage elasticity for LPNs is also positive, but this is not robust to other cutoffs in the Kaitz index distribution (as shown in Panel D, which uses a cutoff based on the maximum Kaitz index defined in Cengiz et al. 2019).
To test for evidence of pre-trends in nursing assistant hours, Fig. 2 plots estimates of {δk} from the estimation of Eq. (2). The vertical bars bounded by the horizontal lines represent pointwise 95% confidence intervals. The shaded portion of the vertical bars represents the uniform, sup-t confidence band, which represents the precision of the entire event-time path (Freyaldenhoven et al. 2021). The value of δ− 1 is normalized to zero to facilitate comparisons with the month immediately prior to the minimum wage change. The results are supportive of our identifying assumption in that we obtain pre-period estimates of {δk} that are not statistically different from zero. In months immediately following the minimum wage change, we observe statistically significant increases in nursing assistant HPRD, consistent with the results shown in Table 3.
Fig. 2.
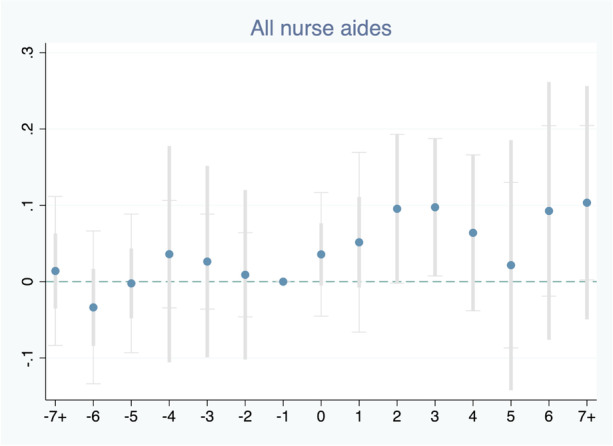
Tests for pre-trends in nursing assistant HPRD. Notes: Figure 2 reports the results from the estimation of Eq. (2) in the text, where the dependent variable is the log of nursing assistant hours per resident day (HPRD). The dots represent the estimated δ coefficients for each period and the vertical bars bounded by the horizontal lines represent pointwise 95% confidence intervals. Each interval is a function of the standard error of the estimate of its associated period-specific effect. The shaded portion of the vertical bars represents the uniform, sup-t confidence band, which represents the precision of the entire event-time path, as in Freyaldenhoven et al. (2021).
In Table 4, we report results from robustness checks of the nursing assistant HPRD models. First we consider the possibility that if minimum wages had a negative effect on average resident days per month, our main results might obscure a decrease in total nursing assistant staff hours. To test for this possibility, we estimated a version of Eq. (1) where the dependent variable is average resident days throughout the month, also obtained from the PBJ data. Column (1) of Table 4 reports the results. It shows that an increase in the minimum wage increased average resident days, ruling out the possibility that decreases hide reductions in total staffing hours.7 In column (2), we obtain similar positive and significant estimates of the minimum wage elasticity using a balanced panel of facilities. In column (3), we obtain similar results when we focus on facilities with a high share of residents whose stays are covered by Medicaid, which is a means-tested public insurance program that covers the cost of 6 in 10 nursing home residents (KFF 2017). Because Medicaid payments to providers are low compared to other payers, facilities that have higher shares of Medicaid residents are more resource constrained, which may lessen their ability to maintain staffing when wages increase. Nonetheless, findings from column (3) show that increases in the minimum wage have a significant positive effect on nursing assistant HPRD at facilities where at least 75% of residents are covered by Medicaid.8 In columns (4) and (5) we examine whether the positive effect on nursing assistant hours per resident day is more common in rural areas than urban areas. Since rural markets are more likely to be dominated by a single facility, evidence that the positive wage elasticity is driven by rural facilities might suggest that the positive hours response to the minimum wage is a result of monopsony power (at least when measured with a traditional concentration-based measure of monopsony). The results, in contrast, suggest that urban facilities are driving the positive minimum wage elasticity.
Table 4.
Robustness of minimum wage effects on nursing assistant HPRD
| Dep Var is log (Resident Days) | Dep Var is log (Nursing Assistant HPRD) | ||||
|---|---|---|---|---|---|
| Full sample |
Balanced panel of facilities | Facilities with high Medicaid resident share | Facilities in rural areas only | Facilities in non-rural areas only | |
| (1) | (2) | (3) | (4) | (5) | |
| log (min wage) | 0.043*** | 0.081*** | 0.090** | 0.013 | 0.066*** |
| (0.015) | (0.023) | (0.040) | (0.067) | (0.022) | |
| Dep var mean (level) | 87.82 | 2.28 | 2.15 | 2.27 | 2.30 |
| No. of facilities | 14,146 | 9,429 | 3,774 | 3,641 | 10,502 |
| No. of observations | 474,133 | 339,444 | 126,321 | 122,299 | 351,734 |
Observations are facility-months. HPRD = hours per resident day, measured as the average of daily total nursing assistant hours divided by daily resident census, across all days in the month. High Medicaid share facilities are those where at least 75% of residents are covered by Medicaid. Robust standard errors (clustered by locality) are reported in parentheses. Statistical significance is indicated by *** p < 0.01, ** p < 0.05, * p < 0.1. All models also include the monthly county unemployment rate, facility fixed effects, year-by-month fixed effects, state fixed effects, and state-by-fiscal year fixed effects
We next examine whether the use of monthly average HPRD obscures other changes in nursing assistant hours on other margins. Table 5 examines average HPRD on weekend days, and results are largely similar to those reported in Table 3: we find positive and statistically significant minimum wage elasticities for nursing assistant hours per resident day. Columns (2)-(5) report results from models of outcomes based on recommended CNA hours. We find no evidence that the minimum wage reduces the share of days in a month that a facility meets minimum recommended hours for CNAs, either for all days or weekend days. However, consistent with our prior findings, the minimum wage has a positive and statistically significant effect on the share of all days in a month that facilities meet 75% of the minimum recommended staffing levels for CNAs. As noted earlier, we include medication aide hours in the construction of the share of days a facility meets these thresholds; in a sensitivity test, we obtain similar results when we omit medication aide hours.
Table 5.
Effects of state/local minimum wages on alternate margins of nursing assistant hours
| log (Nurse assistant weekend HPRD) | % days in month meeting min. rec. staffing for CNAs | % weekend days in month meeting min. rec. staffing for CNAs | % days in month meeting 75% min. rec. staffing for CNAs | % weekend days in month meeting 75% of min. rec. staffing for CNAs | |
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| log (min wage) | 0.056** | 0.010 | -0.022 | 0.088* | 0.074 |
| (0.028) | (0.024) | (0.020) | (0.050) | (0.054) | |
| Dep var mean (level) | 2.15 | 0.144 | 0.097 | 0.578 | 0.472 |
| No. of facilities | 14,141 | 14,146 | 14,143 | 14,146 | 14,143 |
| No. of observations | 473,489 | 474,133 | 473,567 | 474,133 | 473,567 |
Observations are facility-months. HPRD = hours per resident day, measured as the average of total nursing assistant hours divided by daily resident census, across all weekend days in the month. We defined minimum recommended staffing hours for CNAs as 2.8 HPRD. Robust standard errors (clustered by locality) are reported in parentheses. Statistical significance is indicated by *** p < 0.01, ** p < 0.05, * p < 0.1. All models also include the monthly county unemployment rate, facility fixed effects, year-by-month fixed effects, and state-by-fiscal year fixed effects
Discussion
The nursing facility industry is a particularly important context for studying employment effects of the minimum wage given the industry’s reliance on lower-wage healthcare professionals. One-third of all workers in nursing facilities across the U.S. are nursing assistants, who earned a median hourly wage of $13.23 in 2019 (U.S. Bureau of Labor Statistics 2021c). Compared to RNs and LPNs, nursing assistants have more contact with residents, as they routinely assist with bathing, dressing, eating and other daily activities. Given persistent deficiencies in nursing facility quality and the established link between quality and nurse staffing, it is important to examine whether minimum wage increases have the unintended consequence of reducing nursing assistant staffing hours.
We contribute to the small prior literature on this topic by using a novel data source to examine the effects of minimum wages on hours worked by nursing assistants between 2017 and 2019, when 24 states and dozens of localities increased their minimum wages. Because the PBJ data we use are subject to audit, they represent an improvement over unaudited facility-reported nurse staffing from OSCAR/CASPER. Comparing each facility’s reported staffing for the same 2-week period measured in the raw OSCAR/CASPER data, Geng et al. (2019) found that reported staffing hours were higher on average in OSCAR/CASPER than in the PBJ, and that the differences varied by facility ownership. In addition, our monthly averages of daily PBJ data allow us to align staffing measures with the timing of minimum wage changes more accurately than is possible with the nurse staffing data based on OSCAR/CASPER reports (e.g., the Nursing Home Compare data used in Ruffini 2021).
That said, the PBJ data have some limitations. First, since the data are self-reported, nursing facilities could misreport hours worked, even though the PBJ data are subject to audit. Second, facilities are advised to report paid hours; thus, the data do not capture cases where a salaried staff member, paid to work 8 h per day, works more hours without additional payment corresponding to the additional time. This second issue is unlikely to affect lower-paid healthcare professionals like nursing assistants, who are less likely to be salaried compared to RNs and LPNs, and since only 20% of RNs and LPNs are salaried (Geng et al. 2019). Finally, the public PBJ data that we use do not allow us to examine outcomes such as the number of staff employed and turnover.9
In contrast to the predictions of standard economic theory with frictionless competitive labor markets, we find no evidence that state and local minimum wage increases between 2017 and 2019 reduced hours per resident day for nursing assistants. Instead, we find minimum wages increased nursing assistant hours worked per resident day, both throughout the month and on weekends, and increased the share of days in the month that facilities were at or above 75% of the minimum recommended CNA hours per resident day. Our findings differ from studies of nursing facilities in the U.K., which have documented declines in employment or hours worked (Machin et al. 2003; Machin and Wilson 2004; Vadean and Allen 2021). Such findings were short-lived in some cases or limited to certain types of facilities (e.g., private facilities, residential care only facilities). Even though we examine recent larger minimum wage increases, our findings are comparable to those of Ruffini (2021) which found that minimum wage increases between 1992 and 2017 led to small increases in the number of nursing assistant staff at nursing facilities. While that study found no effect on nursing assistant hours per resident day, we observe increases; in particular, we find that nursing assistant hours per resident day increased on weekend days, days that other studies have found to be marked by lower staffing.
The positive minimum wage elasticity we find for U.S. nursing assistants may be explained by the presence of labor market power or frictions. If the labor market is highly concentrated, for example, firms may pay wages below workers’ marginal product of labor, and minimum wage increases in these settings may lead to higher employment. While our findings are not explained by a traditional measure of monopsony power (i.e., the positive employment effects we observe are not driven by rural areas where markets are more concentrated), standard monopsony measures (like counts of the number of firms or a basic Herfindahl-Hirschman Index (HHI)) may not accurately quantify the market power that firms have with regard to wage setting (Manning 2003; Card 2022). Some prior studies in the minimum wage literature provide evidence of these frictions using novel data. For example, Azar et al. (2019) measured firm market power with an occupation-specific HHI defined from job postings by actively searching firms, and found that minimum wages had positive employment effects in more concentrated labor markets. Additionally, Guiliano (2013) used personnel records to identify new labor market entrants whose reservation wage may have been met or exceeded by the minimum wage hike and to measure changes in worker quality. Alternatively, in the presence of barriers to labor force participation by workers (such as childcare costs), higher minimum wages have been found to increase employment, an effect attributed to increases in labor supply (Godoy et al. 2019).
In this study, we lack the same types of novel data to conduct added tests of monopsony and other such market frictions. Focusing on an earlier time period than our study, Ruffini (2021) reports that minimum wages increased stable hires and reduced separations of low-wage female workers at nursing home facilities, which is consistent with dynamic monopsony. Studying the source and presence of these types of frictions in the market for lower-paid healthcare professionals is therefore a promising area for future research, and one that complements the emerging labor economics research on monopsonistic wage setting by firms (Card 2022).
Conclusion
As states and localities have raised minimum wages to levels of $10 and in some cases $15 per hour, it is worth considering the employment consequences in a broader range of settings outside of teenage, retail, and restaurant employment, the settings typically examined in the minimum wage literature. This study examines hours worked by nursing assistants at nursing facilities, and provides evidence that recent relatively large minimum wage increases have not decreased nursing assistant HPRD and instead led to short-lived increases. Especially given the larger minimum wage increases in our study period, our findings lessen concerns about the unintended consequences of these state and local policies.
Acknowledgements
We are grateful for thoughtful comments from Alan Manning, Brian Phelan, and seminar participants at the 2020 EALE/SOLE/ASSLE World Conference and DePaul University. We thank Rishya Suresh and Renee Garrow for valuable research assistance. The project received financial support from the Schroeder Center for Health Policy at William & Mary.
Appendix 1 Additional Tables
Data Availability
Additional results and copies of the computer programs used to generate the results presented in the article are available from the corresponding author at pmchenry@wm.edu.
Declarations
Competing Interests
The authors have no competing interests to declare that are relevant to the content of this article.
Footnotes
Authors’ analysis of the Current Population Survey (CPS) Outgoing Rotation Groups, Earner Study available from IPUMS (Flood et al. 2020). We pooled 2017 to 2019 data, and selected workers employed in the nursing and residential care facility sector who were either (1) nurse aides, defined as nursing, psychiatric, and home health aides; (2) LPNs (licensed practical and licensed vocational nurses); or (3) RNs (registered nurses). We measured wages using the hourly wage reported on the survey or -- for workers that are not paid by the hour -- by dividing weekly earnings by usual hours worked per week. While most workers in our sample were paid on an hourly basis, the percentage of RNs paid hourly is less than that of the other types of workers.
Authors’ calculations from Vaghul and Zipperer (2016, 2019) and Bureau of Labor Statistics (2021c).
One group of studies employs panel data for all U.S. states over time and controls for state (and time period) fixed effects; studies using this generalized difference-in-difference approach generally yield negative estimates of the minimum wage elasticity. To account for regional heterogeneity, several studies use a border discontinuity approach (also called a generalized case study approach). This method focuses on the various local areas across the country comprised of pairs of contiguous border counties, and controls for trends in employment common to the border pair. This group of studies produces minimum wage elasticities that are smaller and in some cases indistinguishable from zero (e.g., Dube et al. 2010, 2016). Finally, case study approaches such as Card and Krueger (1994) provide evidence that minimum wage increases can increase employment in some settings, although different case studies find negative effects (e.g., Sabia et al. 2012).
Before we compute average daily HPRD for the month, we exclude a small number of daily hours measures that we flag as outliers using documentation from NHC. Specifically, we exclude two types of daily records. The first type is days characterized by “highly improbable” staffing levels (unbelievably high or low), according to the CMS’ definition of highly improbable hours per resident day from Nursing Home Compare documentation (CMS 2020). The second includes days with zero residents, since this would prevent us from defining hours per resident day. Overall, these exclusions had a trivial effect on our calculations of facility-month observations. Of the more than 16 million daily records of staffing hours, 0.63% had improbable staffing values and 0.04% had zero values for residents.
In order to match firm-size-specific minimum wage laws to facilities, we estimate the number of employees at a facility as the number of daily staffing hours divided by 8. This is a rough approximation, and we prefer to use overall staffing hours (rather than estimated employees) as the dependent variable in our main specifications.
Only 6 of the 18 states without direct care staffing regulations had minimum wage increases in our period, and the average increase in the minimum wage in those 6 states was substantially smaller relative to all states with minimum wage increases. We considered a facility with nursing assistant HPRD of more than 0.17 above the state’s minimum staffing threshold as having enough flexibility to cut staffing in response to a minimum wage increase. This assumes a large elasticity of employment with respect to the minimum wage (-0.3, from Neumark et al. 2014a) and a large increase in the minimum wage (25%, or the 95th percentile of January 2017 to December 2019 changes across facilities in our sample), which imply a reduction of staffing hours by 7.5%. The average nursing assistant HPRD in our sample is 2.289, so a 7.5% reduction would reduce HPRD by 0.171675.
While not the main focus of our paper, this effect may arise if changes in the minimum wage increase the opportunity cost of informal care and thereby increase demand for formal types of long-term care.
We define the Medicaid coverage rate for each facility as its proportion of residents whose primary support is Medicaid as reported in the 2017 LTCFocus (n.d.) data set, which draws its information from OSCAR/CASPER. LTCFocus (n.d.) is sponsored by the National Institute on Aging (1P01AG027296) through a cooperative agreement with the Brown University School of Public Health.
Some researchers have obtained raw PBJ records from CMS and used the data to construct measures such as employment and turnover (McGarry et al. 2021; Gandhi et al. 2021). However, CMS does not provide an avenue for obtaining these records to the wider research community.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Allegretto SA, Dube, Reich M. Do minimum wages really reduce teen employment? Accounting for heterogeneity and selectivity in state panel data. Ind Relat. 2010;50(2):205–240. doi: 10.1111/j.1468-232X.2011.00634.x. [DOI] [Google Scholar]
- Allegretto S, Dube A, Reich M, Zipperer B. Credible research designs for minimum wage studies: A response to Neumark, Salas, and Wascher. Ind Labor Relat Rev. 2017;70(3):559–592. doi: 10.1177/0019793917692788. [DOI] [Google Scholar]
- Azar J, Huet-Vaughn E, Marinescu I, Taska B, von Wachter T (2019) Minimum wage employment effects and labor market concentration. National Bureau of Economic Research. 10.3386/w26101
- Bostick JE, Ranktz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. J Am Med Dir Assoc. 2006;7:366–376. doi: 10.1016/j.jamda.2006.01.024. [DOI] [PubMed] [Google Scholar]
- Card D. Who sets your wage? Am Econ Rev. 2022;112(4):1075–1090. doi: 10.1257/aer.112.4.1075. [DOI] [Google Scholar]
- Card D, Krueger AB. Minimum wages and employment: A case study of the fast-food industry in New Jersey and Pennsylvania. Am Econ Rev. 1994;84(4):772–793. [Google Scholar]
- Castle N. Nursing home caregiver staffing levels and quality of care: A literature review. J Appl Gerontol. 2008;27(4):375–405. doi: 10.1177/0733464808321596. [DOI] [Google Scholar]
- Cawley J, Grabowski DC, Hirth RA. Factor substitution in nursing homes. J Health Econ. 2006;25:234–247. doi: 10.1016/j.jhealeco.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Cengiz D, Dube A, Lindner A, Zipperer B. The effect of minimum wages on low wage jobs. Quart J Econ. 2019;134(3):1405–1454. doi: 10.1093/qje/qjz014. [DOI] [Google Scholar]
- CMS (Centers for Medicare and Medicaid Services) Appropriateness of minimum nurse staffing ratios in nursing homes. report to congress: Phase II final. Volumes I–III. Baltimore: CMS; 2001. [Google Scholar]
- CMS (Centers for Medicare and Medicaid Services) (2018) Electronic staffing data submission payroll-based journal: Long-term care facility policy manual. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/PBJ-Policy-Manual-Final-V25-11-19-2018.pdf. Accessed 15 Feb 2021
- CMS (Centers for Medicare and Medicaid Services) (2020) Design for nursing home compare five-star quality rating system: Technical users’ guide October 2020. Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/FSQRS. Accessed 4 Jan 2021
- Dellefield ME, Castle NG, McGilton KS, Spilsbury K. The relationship between registered nurses and nursing home quality: An integrative review (2008–2014) Nurs Econ. 2015;33(2):95–108. [PubMed] [Google Scholar]
- Dube A, Lester TW, Reich M. Minimum wage effects across state borders: Estimate using contiguous counties. Rev Econ Stat. 2010;92(4):945–964. doi: 10.1162/REST_a_00039. [DOI] [Google Scholar]
- Dube A, Lester TW, Reich M. Minimum wage shocks, employment flows, and labor market frictions. J Labor Econ. 2016;34(3):663–704. doi: 10.1086/685449. [DOI] [Google Scholar]
- Flood S, King M, Rodgers R, Ruggles S, Warren JR (2020) Integrated public use microdata series, current population survey: Version 8.0 [dataset]. IPUMS, Minneapolis. 10.18128/D030.V8.0
- Freyaldenhoven S, Hansen C, Perez Perez J, Shapiro JM(2021) Visualization, identification, and estimation in the linear panel event-study design. NBER working paper 29170
- Gandhi A, Yu H, Grabowski D. High nursing staff turnover in nursing homes offers important quality information. Health Aff. 2021;40(3):384–391. doi: 10.1377/hlthaff.2020.00957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geng F, Stevenson D, Grabowski D. Daily nursing home staffing levels highly variable, often below CMS expectations. Health Aff. 2019;38(7):1095–1100. doi: 10.1377/hlthaff.2018.05322. [DOI] [PubMed] [Google Scholar]
- Giuliano L. Minimum wage effects on employment, substitution, and the teenage labor supply: Evidence from personnel data. J Labor Econ. 2013;31(1):155–194. doi: 10.1086/666921. [DOI] [Google Scholar]
- Godoy A, Reich M, Allegretto SA(2019) Parental labor supply: Evidence from minimum wage changes. Institute for Research on Labor and Employment Working Paper No. 103–19
- Grabowski DC, Bowblis JR, Lucas JA, Crystal S. Labor prices and the treatment of nursing home residents with dementia. Int J Econ Bus. 2011;18(2):273–292. doi: 10.1080/13571516.2011.584431. [DOI] [Google Scholar]
- Hyer K, Temple A, Johnson CE. Florida’s efforts to improve quality of nursing home care through nurse staffing standards, regulation, and medicaid reimbursement. J Aging Soc Policy. 2009;21(4):318–337. doi: 10.1080/08959420903166910. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine). Committee on Nursing Home Regulation . Improving the quality of care in nursing homes. Washington, DC: National Academy Press; 1986. [Google Scholar]
- IOM (Institute of Medicine) Committee on the Adequacy of Nursing Staff in Hospitals and Nursing Homes . Nursing staff in hospitals and nursing homes: Is it adequate? Washington, DC: National Academy Press; 1996. [Google Scholar]
- Katz LF, Krueger AB. The effect of the minimum wage on the fast food industry. Ind Labor Relat Rev. 1992;46(1):6–21. doi: 10.1177/001979399204600102. [DOI] [Google Scholar]
- KFF (Kaiser Family Foundation) (2017) Medicaid’s role in nursing home care. Available at: https://www.kff.org/wp-content/uploads/2017/06/infographic-medicaid_s-role-in-nursing-home-care-thumbnail.png. Accessed 8 Oct 2021
- Konetzka RT, Stearns SC, Park J. The staffing–outcomes relationship in nursing homes. Health Serv Res. 2008;43(3):1025–1042. doi: 10.1111/j.1475-6773.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LTCFocus (n.d.) Public Use Data sponsored by the National Institute on Aging (P 01 AG027296) through a cooperative agreement with the Brown University School of Public Health. Available at www.ltcfocus.org, 10.26300/h9a2-2c26. Accessed 9 Dec 2019
- Machin S, Manning A, Rahman L. Where the minimum wage bites hard: Introduction of minimum wages to a low wage sector. J Eur Econ Assoc. 2003;1(1):154–180. doi: 10.1162/154247603322256792. [DOI] [Google Scholar]
- Machin S, Wilson J. Minimum wages in a low-wage labour market: Care homes in the UK. Econ J. 2004;114:C102–C109. doi: 10.1111/j.0013-0133.2003.00199.x. [DOI] [Google Scholar]
- Manning A (2003) Monopsony in motion: Imperfect competition in labor markets. Princeton UP
- McGarry BE, Gandhi AD, Grabowski DC, Barnett ML. Larger nursing home staff size linked to higher number Of COVID-19 cases in 2020. Health Aff. 2021;40(8):1261–1269. doi: 10.1377/hlthaff.2021.00323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Caswell C, Littlehale S, Niemi J, Fogel B (2009) Changes in the quality of nursing homes in the US: a review and data update. American Health Care Association, Washington, DC. Available at: https://www.ahcancal.org/research_data/quality/documents/changesinnursinghomequality.pdf. Accessed 15 July 2022
- National Consumer Voice for Quality Long-Term Care (2022) State nursing home staffing standards: Full report. Available at: https://theconsumervoice.org/issues/issue_details/staffing. Accessed 6 June 2022
- Neumark D, Salas JMI, Wascher W. Revisiting the minimum wage-employment debate: Throwing out the baby with the bathwater. Ind Labor Relat Rev. 2014;67:608–648. doi: 10.3386/w18681. [DOI] [Google Scholar]
- Neumark D, Salas JMI, Wascher W. More on recent evidence on the effects of minimum wages in the United States. IZA J Labor Policy. 2014;3(1):1–26. doi: 10.3386/w20619. [DOI] [Google Scholar]
- Ruffini K(2021) Worker earnings, service quality, and firm profitability: Evidence from nursing homes and minimum wage reforms. Working paper, dated May 7
- Sabia JJ, Burkhauser RV, Hansen B. Are the effects of minimum wage increases always small? New evidence from a case study of New York State. Ind Labor Relat Rev. 2012;65(2):350–376. doi: 10.1177/001979391206500207. [DOI] [Google Scholar]
- U.S. Bureau of Labor Statistics, U.S. Department of Labor (2019) Occupational employment and wage statistics. Available at:https://www.bls.gov/oes/. Accessed 15 July 2022
- U.S. Bureau of Labor Statistics, U.S. Department of Labor (2021a) Occupational outlook handbook, nursing assistants and orderlies. Available at https://www.bls.gov/ooh/healthcare/nursing-assistants.htm. Accessed Oct 2021
- U.S. Bureau of Labor Statistics, U.S. Department of Labor (2021b) Occupational outlook handbook, licensed practical and licensed vocational nurses. Available at https://www.bls.gov/ooh/healthcare/licensed-practical-and-licensed-vocational-nurses.htm. Accessed Oct 2021
- U.S. Bureau of Labor Statistics, U.S. Department of Labor (2021c) Occupational employment and wage statistics; OEWS data available at https://www.bls.gov/oes/tables.htm. Accessed Sept 2021
- U.S. Bureau of Labor Statistics, U.S. Department of Labor (2022) Occupational employment and wage statistics. Available at: https://www.bls.gov/oes/. Accessed 15 July 2022
- U.S. GAO (2018) Nursing home quality: Continued improvements needed in CMS’s data and oversight (GAO publication number GAO-18-694T). Accountability Office, Washington, DC
- UC Berkeley Center for Labor Research and Education (2019) Inventory of local minimum wage ordinances (Cities and Counties)
- Vaghul K, Zipperer B (2016) Historical state and sub-state minimum wage data. Washington Center for Equitable Growth. Available at: http://equitablegrowth.org/workingpapers/historical-state-and-sub-state-minimum-wage-data. Accessed 4 June 2019
- Vaghul K, Zipperer B (2019) Updated minimum wage data set. Available at: https://github.com/benzipperer/historicalminwage. Accessed 4 June 2019
- Vadean F, Allan S. The effects of minimum wage policy on the long-term care sector in England. Br J Ind Relat. 2021;59(2):307–334. doi: 10.1111/bjir.12572. [DOI] [Google Scholar]
- Walsh JE, Lane SJ, Troyer JL. Impact of medication aide use on skilled nursing facility quality. Gerontologist. 2014;54(6):976–988. doi: 10.1093/geront/gnt085. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Additional results and copies of the computer programs used to generate the results presented in the article are available from the corresponding author at pmchenry@wm.edu.


