Background
Atopic dermatitis (AD) is associated with substantial financial cost, including increased out-of-pocket (OOP) expenses. Associations and impact of OOP costs are poorly understood.
Objective
The aim of the study was to characterize the impact and associations of OOP health care expenses for AD.
Methods
A 25-question online survey was administered to National Eczema Association members (N = 113,502). Inclusion criteria (US residents aged ≥18 years; self-reported AD or primary caregiver of individual with AD) were met by 77.3% (1118 of 1447).
Results
Respondents with monthly OOP expenses greater than $200 were more likely to have increased AD severity, flares, health care provider visits, prescription polypharmacy, use of step-up therapy, frequent skin infections, and poorer disease control (P < 0.005 for all). Respondents with OOP yearly expenditures greater than $1000 had similar associations and additionally increased rates of comorbid asthma, allergic rhinitis, and anxiety/depression (P < 0.005 for all). A total of 64.6% (n = 624) reported harmful household financial impact of OOP expenses. Predictors of harmful impact included severe AD (adjusted odds ratio [95% confidence interval], 2.62 [1.11–6.19], P = 0.04), comorbid asthma (1.42 [1.07–1.87], P = 0.03), 5 health care provider visits or more in a year (2.80 [1.62–4.82], P = 0.0007), greater than $200 OOP monthly expenditures (2.16 [1.45–3.22], 0.0006), and $1000 annual OOP expenditures or more (4.56 [3.31–6.27], P < 0.0001).
Conclusions
Out-of-pocket expenses for AD significantly impact household finances. Clinical interventions are needed to minimize OOP expenses while optimizing care outcomes.
Capsule Summary:
• Atopic dermatitis (AD) is associated with significant financial cost, including increased out-of-pocket (OOP) expenses, although the impact and associations of OOP health care expenses for AD management are not well understood.
• The OOP health care expenses related to AD are associated with increased disease severity and health care utilization and significantly impact the household finances of patients and caregivers.
• Health care providers should be mindful of the OOP financial burden related to AD management and engage in shared decision making to create a treatment plan that is practical and effective and minimizes household financial impact.
Atopic dermatitis (AD) is a common chronic inflammatory skin disease that affects approximately 7% of the United States (US) population.1,2 AD is a heterogeneous disorder with variable severity, lesional distribution, disease course, and symptoms, including itch, skin-pain, sleep disruption, and mental health symptoms.2–8 Patients with AD have increased rates of comorbid allergic, autoimmune, neuropsychiatric, cardiovascular, and musculoskeletal disorders and impairment in health-related quality of life, resulting in reduced emotional, physical, and psychosocial well-being.2,9–14
The heterogeneous course and profound burden of AD leads to increased health care resource utilization (eg, outpatient, emergency, and inpatient visits) in US children and adults,7,15–17 which in turn contribute to considerable direct and indirect overall costs.17–19 Out-of-pocket (OOP) health care costs are particularly concerning to the everyday lives of AD patients and their families. Population-based studies showed that individuals with AD had multicomponent increases in OOP costs related to health care visits.14,20 However, these studies were limited by their inability to assess the impact of AD severity, control, and/or a broad range of treatments and additional supportive care measures on the financial burden and OOP costs for AD patients and caregivers. Atopic dermatitis severity was previously found to be the strongest predictor of outpatient utilization of AD care, with various socioeconomic and racial/ethnic disparities driving higher rates of emergency department, urgent care, and hospital visits.15 We hypothesized that OOP health care expenses are associated with AD severity and control and significantly contribute to financial impact on individuals and families. We sought to characterize the impact and associations of OOP health care expenses for AD management.
METHODS
Study Design
Between November 14 and December 14, 2019, a 25-question online survey was administered to all National Eczema Association (NEA) members, including 113,502 individuals with AD and family members. The survey was also advertised on online social media platforms, including Facebook. Electronic informed consent was obtained before initiation of the survey, and those who completed the survey were offered an optional chance to enter in a random drawing to win one of ten $50 gift cards. Survey response was not linked to receipt of a gift card. Inclusion criteria were limited to US residents; 18 years or older; and either personal diagnosis of AD or primary caregiver of a child, teen, or young adult with AD.
Survey Questions
Diagnosis of AD was confirmed by positive response to the question “Have [you/the person with AD] been diagnosed with atopic dermatitis by a health care provider?” Demographics included age, race/ethnicity, sex, household income, insurance coverage, and geographic setting. Current AD severity (clear/mild/moderate/severe), control (very well/moderately well/somewhat/minimally/not controlled), number of flare days in the last month (0/1–3/4–7/8–10/≥11), chronic comorbid medical conditions (allergic rhinitis/food allergy/asthma/frequent skin infections/depression/anxiety), current topical/external (antimicrobials/corticosteroids/crisaborole/pimecrolimus/tacrolimus/phototherapy) and systemic (oral corticosteroids/injectable corticosteroids/dupilumab/azathioprine/cyclosporine/methotrexate/mycophenolate mofetil/tacrolimus) prescription treatments, total number of prescriptions (0/1/2/3/4/5/≥6), and number of HCP visits for AD in the past year (0/1/2/3/4/5/≥6) were queried. Out-of-pocket expenses in the past month for co-pays and/or deductibles for doctor or other HCP office visits (excluding mental health providers) for evaluation or treatment of AD ($0/$1–$50/$51–$100/$101–$150/$151–$200/$201–$250/$251–$275/$275–$300/>$300), total yearly OOP expenses for AD across all health care and non–health care–related categories (free response), and impact of yearly OOP expenses on personal/family finances (none/minimal/moderate/significant/devastating) was also assessed.
Data Analysis
Statistical analysis was performed using SAS Version 9.4 (SAS Institute, Cary, NC). Rao-Scott χ2 tests were used for comparisons of categorical variables, including sociodemographic and AD activity measures. Kruskal-Wallis 1-way analysis of variance was used for comparison of median annual OOP costs. To determine predictors of financial impact of OOP expenses on household finances, we constructed a multivariate logistic regression model with financial impact as the dependent variable and invoked backward elimination stepwise selection. Corrected P values of 0.05 or less were considered significant.
RESULTS
Patient Characteristics
The survey was started by 1447 individuals, of which 954 (65.9%) fully completed; 1118 (77.3%) met inclusion criteria. The respondents included adults with AD (% prevalence, 77.5% [n = 866]) and parents and/or primary caregivers of children/teens (younger than 18 years, 20.0% [224]) or young adults (18–25 years, 2.5% [28]) with AD. Most respondents identified as female (76.5% [855]), White (72.4% [697]), and non-Hispanic (90.5% [871]) with employer-sponsored insurance coverage (57.7% [550]), median income of $50,000 to $74,999, and residence in a suburban location (56.6% [544]; Table 1).
TABLE 1.
Respondent Characteristics
| Variable | n (%) |
|---|---|
| Age, y | |
| ≤2 | 42 (3.8) |
| 3–5 | 69 (6.2) |
| 6–11 | 68 (6.1) |
| 12–17 | 49 (4.4) |
| 18–25 | 139 (12.4) |
| 26–35 | 130 (11.6) |
| 36–50 | 173 (15.5) |
| 51–64 | 247 (22.1) |
| ≥65 | 201 (18.0) |
| Sex | |
| Female | 855 (76.5) |
| Male | 251 (22.5) |
| Nonbinary/other | 4 (0.4) |
| Prefer not to answer | 8 (0.7) |
| Race | |
| White | 697 (72.4) |
| Black/African American | 102 (10.6) |
| Asian | 58 (6.0) |
| Native Hawaiian/Pacific Islander | 7 (0.7) |
| American Indian or Alaskan Native | 8 (0.8) |
| Multiracial | 63 (6.5) |
| Other | 28 (2.9) |
| Hispanic ethnicity | |
| No | 871 (90.5) |
| Yes | 92 (9.6) |
| Household income, $ | |
| ≤24,999 | 175 (18.3) |
| 25,000–49,999 | 190 (19.9) |
| 50,000–74,999 | 192 (20.1) |
| 75,000–99,999 | 122 (12.8) |
| 100,000–124,999 | 103 (10.8) |
| 125,000–149,999 | 61 (6.4) |
| ≥150,000 | 111 (11.6) |
| Insurance | |
| None | 41 (4.3) |
| Employer-sponsored coverage | 550 (57.7) |
| Medicaid or state assistance | 93 (9.8) |
| Medicare | 160 (16.8) |
| Policy purchased on state/federal health exchange | 37 (3.9) |
| Policy purchased on the commercial market | 29 (3.0) |
| Tricare or VA benefit | 22 (2.3) |
| Unsure | 22 (2.3) |
| Geographical setting | |
| Urban | 229 (23.8) |
| Suburban | 544 (56.6) |
| Rural | 188 (19.6) |
VA, veteran's administration.
Associations With OOP Expenses
The respondents with OOP expenditures for co-pays and/or deductibles for HCP office visits for evaluation or treatment of AD greater than $100 in the past month were more likely to have moderate and severe disease (% prevalence, 28.9% and 45.5%, P < 0.0001; Table 2). They were also more likely to report minimal disease control (41.1%, P = 0.0004), 11 days or more spent in an AD flare in the past month (39.4%, P < 0.0001), 5 HCP visits or more (49.8%, P < 0.0001), increasing prescription polypharmacy (39.7%, P < 0.0001), and use of step-up therapy, that is, systemic therapy including injectable, oral, or phototherapy (42.3%, P < 0.0001). Although those with increased OOP expenses in the past month were more likely to have comorbid food allergy (36.4%, P = 0.008) and frequent/persistent skin infections (38.4%, P = 0.022), there was no increase in the presence of asthma, allergic rhinitis, or anxiety and/or depression. Similar results were observed for the respondents with OOP expenditures greater than $200 in the past month (Table 2).
TABLE 2.
Associations With OOP Costs
| OOP Costs in the Past 30 d, $ | OOP Costs in the Past Year, $ | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable, n (%) | ≥100 | P | ≥200 | P | Median (Min–Max) | P | ≥1000 | P |
| Current AD severity | ||||||||
| Clear | 5 (20.0) | <0.0001 | 3 (12.0) | <0.0001 | 500 (0–5000) | <0.0001 | 6 (28.6) | <0.0001 |
| Mild | 44 (20.3) | 18 (8.3) | 360 (0–15,000) | 49 (26.5) | ||||
| Moderate | 135 (28.9) | 62 (13.3) | 500 (0–200,000) | 159 (38.5) | ||||
| Severe | 122 (45.5) | 73 (27.2) | 1000 (16–23,000) | 144 (62.1) | ||||
| Current AD control | ||||||||
| Minimally controlled | 94 (41.1) | 0.0004 | 54 (23.6) | 0.003 | 600 (0–200,000) | 0.16 | 87 (43.5) | 0.66 |
| Somewhat controlled | 124 (31.0) | 60 (15.0) | 600 (0–25,000) | 155 (43.4) | ||||
| Moderately well controlled | 76 (27.9) | 32 (11.8) | 500 (0–23,000) | 93 (40.8) | ||||
| Very well controlled | 15 (17.1) | 11 (12.5) | 500 (0–100,000) | 28 (36.4) | ||||
| No. flare days in the past 30 d | ||||||||
| 0 | 11 (27.5) | <0.0001 | 8 (20.0) | 0.0004 | 300 (0–5,000) | <0.0001 | 10 (30.3) | 0.0007 |
| 1–3 | 50 (21.0) | 20 (8.4) | 500 (0–100,000) | 74 (34.4) | ||||
| 4–7 | 56 (29.3) | 24 (12.6) | 500 (50–25,000) | 67 (39.9) | ||||
| 8–10 | 40 (28.6) | 21 (15.0) | 500 (50–15,000) | 44 (36.4) | ||||
| ≥11 | 153 (39.4) | 84 (21.7) | 1000 (0–200,000) | 169 (51.1) | ||||
| Comorbidities | ||||||||
| Asthma | 117 (33.8) | 0.23 | 59 (17.1) | 0.51 | 800 (0–200,000) | 0.002 | 146 (48.8) | 0.002 |
| Allergic rhinitis | 168 (33.0) | 0.22 | 86 (16.9) | 0.45 | 775 (0–200,000) | <0.0001 | 207 (47.5) | 0.0007 |
| Food allergy | 139 (36.4) | 0.008 | 83 (21.7) | <0.0001 | 1000 (2–200,000) | <0.0001 | 185 (55.7) | <0.0001 |
| Frequent/persistent skin infections | 73 (38.4) | 0.022 | 44 (23.2) | 0.003 | 1000 (2–200,000) | <0.0001 | 98 (60.1) | <0.0001 |
| Anxiety and/or depression | 121 (32.6) | 0.44 | 62 (16.7) | 0.58 | 800 (0–200,000) | 0.01 | 154 (48.4) | 0.002 |
| HCP visits in the past year | ||||||||
| 0 | 7 (6.9) | <0.0001 | 3 (2.9) | <0.0001 | 250 (0–3,000) | <0.0001 | 12 (15.2) | <0.0001 |
| 1–2 | 82 (20.5) | 36 (9.0) | 500 (0–23,000) | 98 (27.5) | ||||
| 3–4 | 110 (40.9) | 49 (18.2) | 1000 (20–200,000) | 116 (50.2) | ||||
| ≥5 | 112 (49.8) | 70 (31.1) | 1200 (2–20,000) | 137 (68.2) | ||||
| No. treatments | ||||||||
| 0 | 21 (20.6) | <0.0001 | 6 (5.9) | <0.0001 | 300 (0–5,000) | <0.0001 | 15 (19.2) | <0.0001 |
| 1–2 | 60 (19.0) | 19 (6.0) | 400 (0–20,000) | 66 (23.3) | ||||
| ≥3 | 230 (39.7) | 133 (22.9) | 1000 (0–200,000) | 283 (55.7) | ||||
| Step-up therapy | ||||||||
| No | 136 (23.3) | <0.0001 | 60 (10.3) | <0.0001 | 500 (0–25,000) | <0.0001 | 169 (33.5) | <0.0001 |
| Yes | 172 (42.3) | 98 (24.1) | 1000 (0–200,000) | 190 (53.1) | ||||
AD, atopic dermatitis; HCP, health care provider; OOP, out-of-pocket.
Similar to monthly expenditures, the respondents with increasing annual total OOP expenses for AD care were more likely to have severe disease (median expense, $1000 [range = $16–$23,000], P < 0.0001; Table 2). They were also more likely to have more days spent in an AD flare in the past month (≥11 days; $1000 [$0–$200,000], P < 0.0001), more HCP visits (≥5 visits; $1200 [$2–$20,000], P < 0.0001), increasing prescription polypharmacy (≥3 treatments; $1000 [$0–$200,000], P < 0.0001), and use of step-up therapy ($1000 [$0–$200,000], P < 0.0001). Individuals with higher annual OOP expenses were more likely have all surveyed comorbidities: asthma ($800 [$0–$200,000], P = 0.002), allergic rhinitis ($775 [$0–$200,000], P < 0.0001), food allergy ($1000 [$2–$200,000], P < 0.0001), frequent/persistent skin infections ($1000 [$2–$200,000], P < 0.0001), anxiety and/or depression ($800 [$0–$200,000], P = 0.01). Even when highest reported total annual OOP costs (eg, ≥$100,000) were removed from analysis, median expenses were unchanged and associations remained significant.
Impact of OOP Expenses
When asked about the impact of OOP expenses for AD on personal/family finances, most respondents reported a moderate impact (% prevalence, 40.1%; Fig. 1). Nearly one quarter of the respondents (24.5%) reported a significant or devastating financial impact. Those with a higher degree of moderate, significant, and devastating financial impact were more likely to have lower household income and Medicaid, absent, or uncertain insurance (P < 0.0001 for all; Table 3). They were also more likely to have increased AD severity, poorer AD control, increased number of days spent in AD flare in the past month, increased number of HCP visits, and all surveyed comorbidities (P < 0.001 for all). There was no significant relationship with other sociodemographic factors, such as age, sex, race/ethnicity, and geographic location. Positive predictors of harmful financial impact included severe AD (adjusted odds ratio, 2.62 [95% confidence interval, 1.11–6.19], P = 0.04), comorbid asthma (1.42 [1.07–1.87], P = 0.03), 5 HCP visits or more in the past year (2.80 [1.62–4.82], P = 0.0007), greater than $200 spent on co-pays and/or deductibles for HCP office visits in the past month (2.16 [1.45–3.22], 0.0006), and greater than $1000 annual expenditures for AD (4.56 [3.31–6.27], P < 0.0001; Table 4). Negative predictors included household income of $25,000 to $99,999 (0.63 [0.44–0.90], P = 0.02) and greater than $100,000 (0.27 [0.18–0.41], P < 0.0001).
Figure 1.
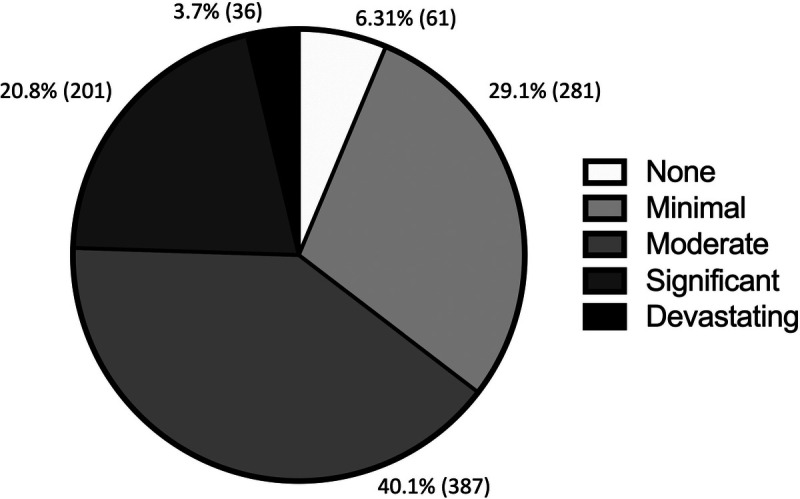
Impact of OOP health care expenses for AD on household finances.
TABLE 3.
Financial Impact of OOP Costs
| Financial Impact | ||||||
|---|---|---|---|---|---|---|
| Variable, n (%) | None | Minimal | Moderate | Significant | Devastating | P |
| Age, y | ||||||
| ≤2 | 1 (2.7) | 13 (35.1) | 16 (43.2) | 5 (13.5) | 2 (5.4) | 0.13 |
| 3–5 | 3 (4.8) | 20 (31.8) | 26 (41.3) | 12 (19.1) | 2 (3.2) | |
| 6–11 | 2 (3.3) | 13 (21.3) | 24 (39.3) | 16 (26.2) | 6 (9.8) | |
| 12–17 | 2 (4.8) | 8 (19.1) | 19 (45.2) | 11 (26.2) | 2 (4.8) | |
| 18–25 | 6 (5.2) | 29 (25.0) | 47 (40.5) | 29 (25.0) | 5 (4.3) | |
| 26–35 | 4 (3.8) | 28 (26.4) | 42 (39.6) | 29 (27.4) | 3 (2.8) | |
| 36–50 | 5 (3.4) | 41 (27.9) | 62 (42.2) | 32 (21.8) | 7 (4.8) | |
| 51–64 | 17 (7.8) | 74 (33.8) | 80 (36.5) | 44 (20.1) | 4 (1.8) | |
| ≥65 | 21 (12.0) | 55 (31.4) | 71 (40.6) | 23 (13.1) | 5 (2.9) | |
| Sex | ||||||
| Female | 40 (5.5) | 206 (27.8) | 302 (40.8) | 162 (21.9) | 31 (4.2) | 0.26 |
| Male | 21 (9.8) | 72 (33.5) | 81 (37.7) | 37 (17.2) | 4 (1.9) | |
| Nonbinary/other | 0 (0.0) | 1 (25.0) | 2 (50.0) | 1 (25.0) | 0 (0.0) | |
| Prefer not to answer | 0 (0.0) | 2 (33.3) | 2 (33.3) | 1 (16.7) | 1 (16.7) | |
| Race | ||||||
| White | 40 (5.7) | 220 (31.6) | 277 (39.7) | 135 (19.4) | 25 (3.6) | 0.18 |
| Black/African American | 12 (11.8) | 13 (12.8) | 45 (44.1) | 28 (27.5) | 4 (3.9) | |
| Asian | 3 (5.4) | 15 (26.8) | 24 (42.9) | 11 (19.6) | 3 (5.4) | |
| Native Hawaiian/Pacific Islander | 0 (0.0) | 3 (42.9) | 1 (14.3) | 2 (28.6) | 1 (14.3) | |
| American Indian or Alaskan Native | 0 (0.0) | 2 (25.0) | 4 (50.0) | 2 (25.0) | 0 (0.0) | |
| Multiracial | 3 (4.8) | 22 (34.9) | 21 (33.3) | 15 (23.8) | 2 (3.2) | |
| Other | 3 (10.7) | 5 (17.9) | 12 (42.9) | 8 (28.6) | 0 (0.0) | |
| Hispanic ethnicity | ||||||
| No | 58 (6.7) | 260 (29.9) | 343 (39.5) | 176 (20.3) | 32 (3.7) | 0.24 |
| Yes | 3 (3.3) | 20 (21.7) | 41 (44.6) | 25 (27.2) | 3 (3.3) | |
| Household income, $ | ||||||
| ≤24,999 | 11 (6.3) | 33 (18.9) | 71 (40.6) | 50 (28.6) | 10 (5.7) | <0.0001 |
| 25,000–49,999 | 9 (4.7) | 40 (21.1) | 86 (45.3) | 45 (23.7) | 10 (5.3) | |
| 50,000–74,999 | 6 (3.1) | 58 (30.4) | 74 (38.7) | 45 (23.6) | 8 (4.2) | |
| 75,000–99,999 | 13 (10.7) | 41 (33.6) | 47 (38.5) | 19 (15.6) | 2 (1.6) | |
| 100,000–124,999 | 4 (3.9) | 31 (30.1) | 44 (42.7) | 21 (20.4) | 3 (2.9) | |
| 125,000–149,999 | 4 (6.6) | 21 (34.4) | 25 (41.0) | 10 (16.4) | 1 (1.6) | |
| ≥150,000 | 12 (10.9) | 53 (48.2) | 33 (30.0) | 11 (10.0) | 1 (0.9) | |
| Insurance | ||||||
| None | 0 (0.0) | 8 (19.5) | 18 (43.9) | 13 (31.7) | 2 (4.9) | <0.0001 |
| Employer-sponsored coverage | 28 (5.1) | 182 (33.2) | 208 (38.0) | 114 (20.8) | 16 (2.9) | |
| Medicaid or state assistance | 3 (3.2) | 15 (16.1) | 48 (51.6) | 20 (21.5) | 7 (7.5) | |
| Medicare | 17 (10.6) | 50 (31.3) | 56 (35.0) | 32 (20.0) | 5 (3.1) | |
| Policy purchased on state/federal health exchange | 3 (8.1) | 6 (16.2) | 21 (56.8) | 6 (16.2) | 1 (2.7) | |
| Policy purchased on the commercial market | 2 (6.9) | 8 (27.6) | 13 (44.8) | 2 (6.9) | 4 (13.8) | |
| Tricare or VA benefit | 4 (18.2) | 4 (18.2) | 10 (45.5) | 4 (18.2) | 0 (0.0) | |
| Unsure | 2 (9.1) | 4 (18.2) | 6 (27.3) | 10 (45.5) | 0 (0.0) | |
| Geographical setting | ||||||
| Urban | 14 (6.1) | 65 (28.5) | 91 (39.9) | 50 (21.9) | 8 (3.5) | 0.99 |
| Suburban | 35 (6.5) | 159 (29.3) | 215 (39.6) | 115 (21.2) | 19 (3.5) | |
| Rural | 11 (5.9) | 56 (29.8) | 77 (41.0) | 36 (19.2) | 8 (4.3) | |
| Region | ||||||
| New England | 5 (7.7) | 16 (24.6) | 28 (43.1) | 14 (21.5) | 2 (3.1) | 0.38 |
| Mid-Atlantic | 6 (4.7) | 40 (31.3) | 50 (39.1) | 30 (23.4) | 2 (1.6) | |
| East North Central | 12 (8.3) | 40 (27.8) | 58 (40.3) | 30 (20.8) | 4 (2.8) | |
| West North Central | 5 (9.6) | 13 (25.0) | 24 (46.2) | 8 (15.4) | 2 (3.9) | |
| South Atlantic | 14 (7.6) | 48 (26.0) | 73 (39.5) | 48 (26.0) | 2 (1.1) | |
| East South Central | 2 (3.3) | 17 (27.9) | 29 (47.5) | 10 (16.4) | 3 (4.9) | |
| West South Central | 3 (3.3) | 24 (26.7) | 35 (38.9) | 21 (23.3) | 7 (7.8) | |
| Mountain | 4 (5.4) | 23 (31.1) | 33 (44.6) | 12 (16.2) | 2 (2.7) | |
| Pacific | 10 (6.2) | 59 (36.4) | 54 (33.3) | 28 (17.3) | 11 (6.8) | |
| Current AD severity | ||||||
| Clear | 1 (4.4) | 10 (43.5) | 8 (34.8) | 3 (13.0) | 1 (4.4) | <0.0001 |
| Mild | 24 (11.7) | 92 (44.7) | 60 (29.1) | 29 (14.1) | 1 (0.5) | |
| Moderate | 23 (5.0) | 138 (30.1) | 213 (46.5) | 75 (16.4) | 9 (2.0) | |
| Severe | 10 (3.9) | 34 (13.2) | 98 (38.0) | 91 (35.3) | 25 (9.7) | |
| Current AD control | ||||||
| Minimally controlled | 12 (5.4) | 47 (21.0) | 82 (36.6) | 63 (28.1) | 20 (8.9) | <0.0001 |
| Somewhat controlled | 15 (3.9) | 117 (30.0) | 171 (43.9) | 79 (20.3) | 8 (2.1) | |
| Moderately well controlled | 20 (7.8) | 83 (32.2) | 103 (39.9) | 46 (17.8) | 6 (2.3) | |
| Very well controlled | 11 (12.9) | 32 (37.7) | 28 (32.9) | 12 (14.1) | 2 (2.4) | |
| No. flare days in the past 30 d | ||||||
| 0 | 7 (18.9) | 16 (43.2) | 7 (18.9) | 6 (16.2) | 1 (2.7) | 0.0001 |
| 1–3 | 19 (8.2) | 86 (37.1) | 78 (33.6) | 43 (18.5) | 6 (2.6) | |
| 4–7 | 12 (6.5) | 49 (26.5) | 85 (46.0) | 34 (18.4) | 5 (2.7) | |
| 8–10 | 9 (6.7) | 41 (30.6) | 54 (40.3) | 27 (20.2) | 3 (2.3) | |
| ≥11 | 14 (3.7) | 89 (23.6) | 162 (43.0) | 91 (24.1) | 21 (5.6) | |
| Comorbidities | ||||||
| Asthma | 13 (3.9) | 83 (24.9) | 127 (38.0) | 96 (28.7) | 15 (4.5) | <0.0001 |
| Allergic rhinitis | 19 (3.9) | 132 (27.1) | 197 (40.4) | 123 (25.2) | 17 (3.5) | 0.0007 |
| Food allergy | 10 (2.7) | 89 (24.0) | 152 (41.0) | 96 (25.9) | 24 (6.5) | <0.0001 |
| Frequent/persistent skin infections | 4 (2.2) | 34 (18.3) | 74 (39.8) | 60 (32.3) | 14 (7.5) | <0.0001 |
| Anxiety and/or depression | 14 (4.0) | 85 (24.2) | 148 (42.1) | 89 (25.3) | 16 (4.6) | 0.003 |
| HCP visits in the past year | ||||||
| 0 | 11 (12.1) | 44 (48.4) | 29 (31.9) | 7 (7.7) | 0 (0.0) | <0.0001 |
| 1–2 | 40 (10.1) | 134 (33.7) | 152 (38.2) | 66 (16.6) | 6 (1.5) | |
| 3–4 | 6 (2.4) | 68 (27.0) | 115 (45.6) | 52 (20.6) | 11 (4.4) | |
| ≥5 | 4 (1.8) | 34 (15.3) | 90 (40.4) | 76 (34.1) | 19 (8.5) | |
AD, atopic dermatitis; HCP, health care provider; OOP, out-of-pocket; VA, veteran's administration.
TABLE 4.
Predictors of Financial Impact
| Variables | Adjusted OR | P |
|---|---|---|
| Household income, $ | ||
| ≤24,999 | 1.00 (ref) | — |
| 25,000–99,999 | 0.63 (0.44–0.90) | 0.024 |
| ≥100,000 | 0.27 (0.18–0.41) | <0.0001 |
| Current AD severity | ||
| Clear | 1.00 (ref) | — |
| Mild | 0.85 (0.36–2.00) | 0.704 |
| Moderate | 1.34 (0.58–3.08) | 0.543 |
| Severe | 2.62 (1.11–6.19) | 0.044 |
| Asthma | ||
| No | 1.00 (ref) | — |
| Yes | 1.42 (1.07–1.87) | 0.026 |
| HCP visits in the past year | ||
| 0 | 1.00 (ref) | — |
| 1–2 | 1.36 (0.84–2.20) | 0.258 |
| 3–4 | 1.71 (0.99–2.87) | 0.058 |
| ≥5 | 2.80 (1.62–4.82) | 0.0007 |
| OOP co-pays and/or deductibles for HCP office visits in the past 30 d | ||
| ≤$200 | 1.00 (ref) | — |
| >$200 | 2.16 (1.45–3.22) | 0.0006 |
| Annual OOP expenses | ||
| ≤$1000 | 1.00 (ref) | — |
| >$1000 | 4.56 (3.31–6.27) | <0.0001 |
AD, atopic dermatitis; HCP, health care provider; OOP, out-of-pocket; OR, odds ratio.
DISCUSSION
Using a nationally representative survey to characterize OOP health care expenses from the perspective of AD patients and caregivers, we discovered a number of important factors associated with OOP costs and their impact on household finances. We stratified direct health care OOP expenses in the past month for co-pays and/or deductibles for HCP office visits by patient-reported AD disease burden to better understand the associations with cost. A recent study demonstrated that this is the major category of OOP costs for AD patients and caregivers.21 We also similarly stratified direct health care OOP expenses in the past year for all expenses related to AD care. The respondents with increased OOP monthly and yearly expenditures were more likely to have increased disease severity, poor disease control, increased flares, increased number of HCP office visits, increased prescription polypharmacy, use of step-up therapy, comorbid food allergy, and frequent skin infections. Those with increased OOP yearly expenditures were additionally more likely to have comorbid asthma, allergic rhinitis, and anxiety and/or depression. The respondents with a higher degree of impact of OOP expenses on household finances were more likely to have lower household income, Medicaid, absent or uncertain insurance, increased disease severity, poor disease control, increased flares, increased number of HCP office visits, and all of the previously mentioned comorbidities. Positive predictors of this financial impact included severe AD, 5 HCP visits or more in the past year, greater than $200 spent on co-pays and/or deductibles for HCP office visits in the past month, and greater than $1000 annual expenditures for AD. These data highlight the onus that OOP costs place on AD patients and caregivers, especially those with the greatest burden of disease, and underscore the importance of personalized care to minimize household financial impact while striving to achieve better disease control.
Studies examining the associations of OOP costs in relation to patient-reported measures of disease activity (eg, severity, control, flares) are limited. A US population-based survey (National Health Interview Survey) that captured data from the previous decade showed that AD was associated with higher OOP costs, along with poorer overall health and increased HCP office visits.14 However, because this was a general health-related survey, AD-related measures were not assessed. A more recent survey in France showed that OOP costs for patients with AD are significantly higher compared with the average French household, especially among those with the most severe AD (as measured by Patient Oriented SCORing Atopic Dermatitis, a patient-reported outcome [PRO] measure of disease severity).22 Similarly, a cross-sectional telephone-based survey of 9 European countries showed elevated OOP expenses for AD patients, with higher costs incurred by those with more severe AD (as measured by patient oriented eczema measure, another PRO measure of AD activity). Compared with many other chronic inflammatory skin conditions, AD patients show a high willingness to pay for their care.23 Those with poor control of their AD, increased flare days, and/or higher disease severity understandably have the highest incentive to relieve their symptoms. Potential categories for OOP expenditures beyond HCPs and prescriptions include nonprescription health care products (eg, moisturizers, hygiene products, allergy medications, sleep aids) and complementary approaches (eg, cleaning products, clothing/bedding, nonwestern alternative medicine). Despite insurance covering few of these costs, individuals with AD have been shown to spend money in all of these categories, despite varying degrees of evidence and efficacy behind some options.21 Health care providers need to understand these potential areas of OOP expense and should fully review and discuss the treatment plan with patients during every encounter, particularly for those with the most severe burden of disease.
Atopic dermatitis is a highly heterogeneous inflammatory disorder consisting of a dynamic longitudinal course of lesional severity and extent.24 Given that every patient has different levels of baseline disease punctuated by varying frequencies and degrees of flaring, there is no one-size-fits-all treatment. As a result, clinicians and patients continually modify their treatment approach, resulting in polypharmacy, intermittent use of step-up therapy, complex and often unsustainable regimens, and use of nonevidence-based treatments.25 Our data show that polypharmacy and step-up therapy were both associated with higher OOP costs, likely reflecting the OOP contribution to prescription costs (especially more expensive step-up therapies) in addition to the overall higher OOP costs for those with the highest disease activity. Atopic dermatitis patients would benefit from a streamlined regimen, consisting of a strong foundation in basic skin care (eg, bathing and emollients), a simple, nonburdensome strategy for the use of topical therapies, implementation of long-term, systemic therapies only as warranted, and deprescription of redundant or nonevidence-based treatments used inappropriately to address AD-specific symptoms (eg, oral antihistamines). Health care providers should discuss the financial impact of OOP costs with patients alongside efficacy, safety, and clinical evidence when crafting a treatment plan consisting of multiple interventions.
Atopic dermatitis is associated with a higher risk of allergic disorders (and may predispose individuals to conditions like asthma, allergic rhinitis, food allergy), infectious conditions, and mental health symptoms of anxiety and depression.26 Furthermore, these comorbidities are associated both with increasing AD severity and higher health care utilization.12,27 We found that the presence of these comorbid conditions was associated with increasing OOP costs. The comorbid health burden of AD is often underappreciated, and a substantial number of patients can go undiagnosed and untreated, especially in the case of mental health symptoms.28 Patients may seek out additional nonprescription or complementary treatments and/or various other HCPs for relief, contributing to excess expenses. It is critical for HCPs to appreciate the full spectrum of cutaneous and noncutaneous comorbidities of AD to counsel, treat, and refer as needed for additional care to better control disease activity and reduce OOP costs.
Lower income and Medicaid, absent, or uncertain insurance were associated with higher OOP costs, and increased AD severity and both monthly and yearly OOP expenditures were positive predictors, and higher income was a negative predictor of impact on household finances. Previous studies have suggested that lower socioeconomic status, including lower household income, is associated with the development of more severe AD,29 which itself is likely driven by health care barriers related to insurance status and race, including difficulties in obtaining specialist care (like dermatology) and prescription medication coverage.14,30,31 The overall effect of low socioeconomic status goes well beyond the impact of OOP costs, as the presence of AD in this population contributes to considerable direct and indirect costs that are underestimated by current economic models and cost impact studies.32 Further studies are needed to better understand and target this public health burden to increase access for AD patients. Health care providers must be especially mindful to engage in shared decision making to create a fiscally sound and practical treatment plan rather than putting forward a 1-sided “ideal” strategy that may be challenging or even impossible for patients to implement.
Strengths of this study include a large, nationally representative sample of AD patients and caregivers who were directly queried about their real-world OOP expenses and household financial impact. The inclusion of several different measures of patient-reported burden (eg, severity, control, flare days), current treatments, number of HCP visits, and comorbid chronic diseases allowed for a detailed understanding of features associated with OOP costs and financial impact. The cross-sectional nature of this survey is an important limitation, as we were unable to assess changes in costs and impact over time. In addition, although selection bias is possible given that this Internet-based survey was completed by members of the NEA and not the overall US population, the respondent demographics indicate sufficient variety in disease severity, geographic setting, household income, and insurance status. Although self-report of expenses may not be as accurate as a claim-based database, survey data collected directly from patients and caregivers provide a more accurate representation of individual considerations regarding disease severity and household finances. Diagnosis of AD by self-report has been previously validated for similar types of surveys.33,34 Additional studies are needed to confirm these findings and better understand longitudinal associations of OOP expenditures in relation to the real-world, dynamic disease course of AD. Future analyses of financial burden should incorporate additional PROs to better understand predictors of cost and their impact on household finances, especially among those with socioeconomic and racial disparities.
In conclusion, OOP health care expenses related to AD are associated with increasing disease severity and significantly impact the household finances of patients and caregivers. Additional studies are needed to better understand longitudinal associations with cost and lessen this financial impact while striving to attain short- and long-term disease control.
Footnotes
R.C. reports personal fees from AbbVie and RegeneronSanofi. J.I.S. reports personal fees from AbbVie, Anaptysbio, Asana, EliLilly, Galderma, GlaxoSmithKline, Kiniksa, Leo, Menlo, Pfizer, Realm, RegeneronSanofi, and Roivant and grants from GlaxoSmithKline, RegeneronSanofi, and Galderma. The other authors have no funding or conflicts of interest to declare.
Supported by the National Eczema Association.
Presented at the Society of Investigative Dermatology Virtual Meeting 2021; May 6, 2021.
R.C. and W.S.B. contributed to this work equally.
R.C. had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
W.S.B., I.J.T., and J.I.S. did the study concept and design. W.S.B. and I.J.T. did the acquisition of data. R.C., W.S.B., I.J.T., and J.I.S. did the analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, and statistical analysis.
Contributor Information
Raj Chovatiya, Email: raj.chovatiya@gmail.com.
Isabelle J. Thibau, Email: isabelle@nationaleczema.org.
Jonathan I. Silverberg, Email: jonathanisilverberg@gmail.com.
REFERENCES
- 1.Hua T, Silverberg JI. Atopic dermatitis in US adults: epidemiology, association with marital status, and atopy. Ann Allergy Asthma Immunol 2018;121(5):622–624. doi: 10.1016/j.anai.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 2.Silverberg JI, Gelfand JM, Margolis DJ, et al. Patient burden and quality of life in atopic dermatitis in US adults: a population-based cross-sectional study. Ann Allergy Asthma Immunol 2018;121(3):340–347. doi: 10.1016/j.anai.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Cheng BT, Silverberg JI. Depression and psychological distress in US adults with atopic dermatitis. Ann Allergy Asthma Immunol 2019;123(2):179–185. doi: 10.1016/j.anai.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Silverberg JI, Margolis DJ, Boguniewicz M, et al. Distribution of atopic dermatitis lesions in United States adults. J Eur Acad Dermatol Venereol 2019;33(7):1341–1348. doi: 10.1111/jdv.15574. [DOI] [PubMed] [Google Scholar]
- 5.Silverberg JI, Gelfand JM, Margolis DJ, et al. Pain is a common and burdensome symptom of atopic dermatitis in United States adults. J Allergy Clin Immunol Pract 2019;7:2699–2706.e7. doi: 10.1016/j.jaip.2019.05.055. [DOI] [PubMed] [Google Scholar]
- 6.Kim JP, Chao LX, Simpson EL, et al. Persistence of atopic dermatitis (AD): a systematic review and meta-analysis. J Am Acad Dermatol 2016;75(4):681–687.e11. doi: 10.1016/j.jaad.2016.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silverberg JI, Garg NK, Paller AS, et al. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol 2015;135(1):56–66. doi: 10.1038/jid.2014.325. [DOI] [PubMed] [Google Scholar]
- 8.McCleary KK. Understanding the lived experience of eczema: the “voice of the patient” report on the eczema patient-focused drug development meeting. Updated March 20, 2020. Available at: http://www.morethanskindeep-eczema.org/report.html. Accessed June 17, 2021.
- 9.Cheng BT, Silverberg JI. Association between atopic dermatitis and lower health utility scores in US adults. Ann Allergy Asthma Immunol 2020;124(1):88–89. doi: 10.1016/j.anai.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Silverberg JI, Gelfand JM, Margolis DJ, et al. Health utility scores of atopic dermatitis in US adults. J Allergy Clin Immunol Pract 2019;7(4):1246–1252.e1. doi: 10.1016/j.jaip.2018.11.043. [DOI] [PubMed] [Google Scholar]
- 11.Chiesa Fuxench ZC, Block JK, Boguniewicz M, et al. Atopic dermatitis in America study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol 2019;139(3):583–590. doi: 10.1016/j.jid.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 12.Silverberg JI, Gelfand JM, Margolis DJ, et al. Association of atopic dermatitis with allergic, autoimmune, and cardiovascular comorbidities in US adults. Ann Allergy Asthma Immunol 2018;121(5):604–612.e3. doi: 10.1016/j.anai.2018.07.042. [DOI] [PubMed] [Google Scholar]
- 13.Silverberg JI. Selected comorbidities of atopic dermatitis: atopy, neuropsychiatric, and musculoskeletal disorders. Clin Dermatol 2017;35(4):360–366. doi: 10.1016/j.clindermatol.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silverberg JI. Health care utilization, patient costs, and access to care in US adults with eczema: a population-based study. JAMA Dermatol 2015;151(7):743–752. doi: 10.1001/jamadermatol.2014.5432. [DOI] [PubMed] [Google Scholar]
- 15.Silverberg JI, Gelfand JM, Margolis DJ, et al. Atopic dermatitis in US adults: from population to health care utilization. J Allergy Clin Immunol Pract 2019;7(5):1524–1532.e2. doi: 10.1016/j.jaip.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Singh P, Silverberg JI. Outpatient utilization patterns for atopic dermatitis in the United States. J Am Acad Dermatol 2019. doi: 10.1016/j.jaad.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 17.Narla S, Hsu DY, Thyssen JP, et al. Predictors of hospitalization, length of stay, and costs of care among adult and pediatric inpatients with atopic dermatitis in the United States. Dermatitis 2018;29(1):22–31. doi: 10.1097/DER.0000000000000323. [DOI] [PubMed] [Google Scholar]
- 18.Kwa L, Silverberg JI. Financial burden of emergency department visits for atopic dermatitis in the United States. J Am Acad Dermatol 2018;79(3):443–447. doi: 10.1016/j.jaad.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 19.Drucker AM, Wang AR, Li WQ, et al. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol 2017;137(1):26–30. doi: 10.1016/j.jid.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 20.Whiteley J, Emir B, Seitzman R, et al. The burden of atopic dermatitis in US adults: results from the 2013 National Health and Wellness Survey. Curr Med Res Opin 2016;32(10):1645–1651. doi: 10.1080/03007995.2016.1195733. [DOI] [PubMed] [Google Scholar]
- 21.Smith Begolka W, Chovatiya R, Thibau IJ, et al. Financial burden of atopic dermatitis out-of-pocket health care expenses in the United States. Dermatitis 2021. doi: 10.1097/DER.0000000000000715. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Launois R, Ezzedine K, Cabout E, et al. Importance of out-of-pocket costs for adult patients with atopic dermatitis in France. J Eur Acad Dermatol Venereol 2019;33(10):1921–1927. doi: 10.1111/jdv.15581. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23.Beikert FC, Langenbruch AK, Radtke MA, et al. Willingness to pay and quality of life in patients with atopic dermatitis. Arch Dermatol Res 2014;306(3):279–286. doi: 10.1007/s00403-013-1402-1. [DOI] [PubMed] [Google Scholar]
- 24.Hong MR, Lei D, Yousaf M, et al. A real-world study of the longitudinal course of adult atopic dermatitis severity in clinical practice. Ann Allergy Asthma Immunol 2020;125(6):686–692.e3. doi: 10.1016/j.anai.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Singh P, Silverberg J. Real-world outpatient prescription patterns for atopic dermatitis in the United States. Dermatitis 2019;30(5):294–299. doi: 10.1097/DER.0000000000000520. [DOI] [PubMed] [Google Scholar]
- 26.Silverberg JI. Comorbidities and the impact of atopic dermatitis. Ann Allergy Asthma Immunol 2019;123(2):144–151. doi: 10.1016/j.anai.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 27.Silverberg JI, Simpson EL. Association between severe eczema in children and multiple comorbid conditions and increased healthcare utilization. Pediatr Allergy Immunol 2013;24(5):476–486. doi: 10.1111/pai.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silverberg JI, Gelfand JM, Margolis DJ, et al. Symptoms and diagnosis of anxiety and depression in atopic dermatitis in U.S. adults. Br J Dermatol 2019;181(3):554–565. doi: 10.1111/bjd.17683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silverberg JI, Simpson EL. Associations of childhood eczema severity: a US population-based study. Dermatitis 2014;25(3):107–114. doi: 10.1097/DER.0000000000000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim Y, Blomberg M, Rifas-Shiman SL, et al. Racial/ethnic differences in incidence and persistence of childhood atopic dermatitis. J Invest Dermatol 2019;139(4):827–834. doi: 10.1016/j.jid.2018.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alghothani L, Jacks SK, Vander Horst A, et al. Disparities in access to dermatologic care according to insurance type. Arch Dermatol 2012;148(8):956–957. doi: 10.1001/archdermatol.2012.804. [DOI] [PubMed] [Google Scholar]
- 32.Chung J, Simpson EL. The socioeconomics of atopic dermatitis. Ann Allergy Asthma Immunol 2019;122(4):360–366. doi: 10.1016/j.anai.2018.12.017. [DOI] [PubMed] [Google Scholar]
- 33.Vissing NH, Jensen SM, Bisgaard H. Validity of information on atopic disease and other illness in young children reported by parents in a prospective birth cohort study. BMC Med Res Methodol 2012;12:160. doi: 10.1186/1471-2288-12-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Flohr C, Weinmayr G, Weiland SK, et al. How well do questionnaires perform compared with physical examination in detecting flexural eczema? Findings from the International Study of Asthma and Allergies in Childhood (ISAAC) phase two. Br J Dermatol 2009;161(4):846–853. doi: 10.1111/j.1365-2133.2009.09261.x. [DOI] [PubMed] [Google Scholar]


