Abstract
Objective
This systematic review aimed to explore an association of new TR and its quantification in patients undergoing His bundle pacing (HBP).
Methods
A literature review was conducted using Mesh terms (His bundle pacing, tricuspid regurgitation, tricuspid valve incompetence, etc.) in PubMed, EMBASE, Web of science CINAHL, and the Cochrane Library till October 2021. Relevant studies evaluating tricuspid regurgitation in HBP were included and information regarding TR and its related factors (ejection fraction (EF) and New York Heart Association (NYHA) class) were retrieved from the eligible studies.
Results
Out of 196 articles, 10 studies met the inclusion criteria, which consisted of 546 patients with HBP. The mean age of the patients ranged between 61.2 ± 12.3 and 75.1 ± 7.9 years with 54.1% males. The overall implant success rate was 79.2%. Only one study reported a 5% incidence of TR, while 9 studies reported no new TR after HBP. Four studies reported overall decrease in TR by 1 grade and 3 studies demonstrated increased TR from baseline. Two studies showed no change from baseline TR.
Conclusion
HBP causes improvement in TR grade after HBP for cardiac resynchronization therapy (CRT) as well as atrioventricular block (AVB). Further studies in the form of randomized controlled trials are required to further evaluate the effect of HBP on tricuspid valve functioning.
The overall implant success rate was 79.2%. Only one study reported a 5% incidence of TR while 9 studies reported no new TR after HBP. Four studies reported overall decrease in TR by 1 grade and 3 studies demonstrated increased TR from baseline. Two studies showed no change from baseline TR.

1. INTRODUCTION
Approximately one‐million cardiac implantable electronic devices (CIEDs) are implanted in patients with various indications worldwide (Mond & Proclemer, 2011). The most common CIED to be implanted is the pacemaker. Since the advent of the world's first pacemaker (1958), these devices have become the primary treatment for bradyarrhythmias and their indications are expanding even today (Furman & Schwedel, 1959; Glikson et al., 2021).
Cardiac implantable electronic device‐induced tricuspid regurgitation (TR) is the valvular insufficiency cause or aggravated by a right ventricular (RV) lead after pacemaker implantation. Right ventricular pacemaker leads are associated with worse outcomes. Regarding causation, it is difficult to disentangle the role of mechanical disruption of tricuspid valve by pacemaker leads from pacing induced dyssynchrony, but it is plausible that both contribute. (Cheema et al., 2021; Khurshid et al., 2014; Lamas et al., 2000; Mandras & Desai, 2021; Matusik et al., 2010; Sanchez et al., 2021).
The major risk factors for CIED‐related TR include implantable cardiac defibrillator (ICD) leads, higher number of ventricular leads, lead position with respect to the tricuspid valve (TV), and inadequate pacing positions (Höke et al., 2014; Kiehl et al., 2016). Several studies have demonstrated that ICD and CRT leads are associated with increased TR than pacemakers because their leads are thicker and less elastic (Arabi et al., 2015; Höke et al., 2014; Kim et al., 2008; Van De Heyning et al., 2019). Over the past two decades, large randomized trials have evaluated the role of biventricular pacing CRT (BiV‐CRT). The BLOCK‐HF trial showed a significant reduction in all‐cause death, HF requiring hospitalization, and >15% increase in left ventricular (LV) end‐systolic volume index, favoring BiV‐CRT over RV pacing (Curtis et al., 2016). The BioPace trial showed a non‐significant trend towards BiV‐CRT for a composite endpoint of mortality and first hospitalization with HF (HR 0.87, p = .08) (Funck et al., 2006). However, BiV‐CRT is associated with increased lead‐induced TR and is not an ideal strategy in patients with concomitant tricuspid insufficiency, in addition to other challenges and contraindications (Ahmed & Kayani, 2021; Ousdigian et al., 2014).
The His bundle pacing (HBP) results in an efficient physiological and synchronized ventricular activation by stimulation of the His‐Purkinje system directly, thus alleviating the detrimental effects of asynchronous ventricular activation occurring with RV pacing (Sharma et al., 2015). HBP can also normalize conduction in patients with bundle branch block (BBB), hence, it has a role as an alternative to CRT (Abdelrahman et al., 2018). As HBP lead can be implanted above tricuspid annulus, its effect on TV morphology is minimal, leading to reversal of TR (Grieco et al., 2021; Hasumi et al., 2018; Hu et al., 2020; Hu et al., 2021; Huang et al., 2019; Ma et al., 2021; Shan et al., 2018; Vijayaraman et al., 2017; Wu et al., 2021; Ye et al., 2021). In this systematic review, we provide an association of TR in patients undergoing HBP.
2. METHODS
2.1. Search strategies
This systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement (Moher et al., 2010).
Electronic databases, including PubMed, EMBASE, Web of Science, CINAHL, and the Cochrane Library database were searched (until October 2021) to identify primary references. All eligible English studies were included in this review. The following search terms were used: (“His bundle pacing [Mesh]” OR “His bundle pacing [Mesh]” OR “Artificial Cardiac Pacing [Mesh]” OR “Parahisian pacing [Mesh]” OR “Physiologic pacing” OR “Conduction system pacing” OR “Tricuspid Valve Insufficiency [Mesh]” OR “Tricuspid Valve Regurgitation [Mesh]” OR “Tricuspid Incompetence [Mesh]” OR “Tricuspid Regurgitation [Mesh]”). The authors also searched all of the reference lists of the reviews in the relevant fields and google scholar to identify additional relevant studies. A total of 196 studies were initially identified by the two reviewers (D.I.S. and S.M.J.Z.).
2.2. Study selection and outcomes
A web‐based software platform (Covidence) was used to eliminate duplicate studies. The two reviewers (D.I.S. and S.M.J.Z.) then reviewed the titles and abstracts of the articles independently. In case of disagreement between the two reviewers, a third researcher (J.M.) helped resolve the impasse. For possible correlations, the full text would be searched to determine the inclusion of the article.
The inclusion criteria were as follows: randomized controlled trials (RCTs), observational studies, and case series (>15 patients), which reported the incidence of TR after HBP before and after follow‐up. Study endpoints included any of the following: (1) Quantification of TR grade at baseline and follow‐up after HBP; and (2) incidence of deterioration or improvement in TR by at least one grade.
The exclusion criteria were as follows: (1) case reports, conference abstracts, animal experiments, and review articles; (2) articles published in languages other than English with no translation; (3) no echocardiographic parameters for quantification of TR.
2.3. Data extraction
The two reviewers (D.I.S. and S.M.J.Z.) independently extracted the data from the included studies: (1) basic information of the studies, author name, year of publication, and study design; (2) baseline characteristics, such as age, sample size, gender, HBP success rate, and follow‐up; (3) outcome data, including parameter used in the assessment of TR severity, the incidence of TR deterioration of improvement, EF, and NYHA class after HBP; (4) risk factors associated with TR worsening (if any). Data extraction was conducted with mutual agreement, and all conflicts were resolved by a third researcher (J.M.). If more than one follow‐up time were recorded in the study, the longest time was selected for analysis.
2.4. Outcome measures
The primary outcome was an assessment of TR grade in HBP or new TR after implantation. The secondary outcome was an assessment of QRSd.
2.5. Quality assessment
Each study was assessed for quality using the National Institute of Health (NIH) quality assessment tool for RCTs and observational studies (NIH, 2021). Studies were scored as 0–4 as poor, 5–7 as fair, and >7 as good a quality investigation.
2.6. Definition of terms
According to the American Society of Echocardiography, TR was categorized into none or trace, mild, moderate, and severe. The severity of TR was graded as grade I (none or trace), grade 2 (mild, grade 3 (moderate), and grade 4 (severe).
The change in TR of one grade was defined as worsening or improving TR grade by ≥ one grade after HBP compared with baseline in the follow‐up period. Progression from moderate to study‐specific grades beyond severe was considered to be a change of one grade, for standardization across studies and to be consistent with the American Society of Echocardiography grading. The same was held for improvement of TR grade.
2.7. Statistical analysis
For statistical analysis, Statistical Package for the Social Sciences (SPSS) version 26 (IBM Corp, Armonk, NY, USA.) was used. The quantitative variables were presented as mean and standard deviation (SD). Qualitative variables were expressed in frequency and percentages.
3. RESULTS
3.1. Baseline characteristics
A total of 196 articles were retrieved through the search strategy after excluding duplicates, and 10 articles met the criteria. The literature search process is shown in Figure 1. Baseline characteristics of the studies and degree of TR, EF, and NYHA class at baseline and at follow‐up are included in Table 1.
FIGURE 1.
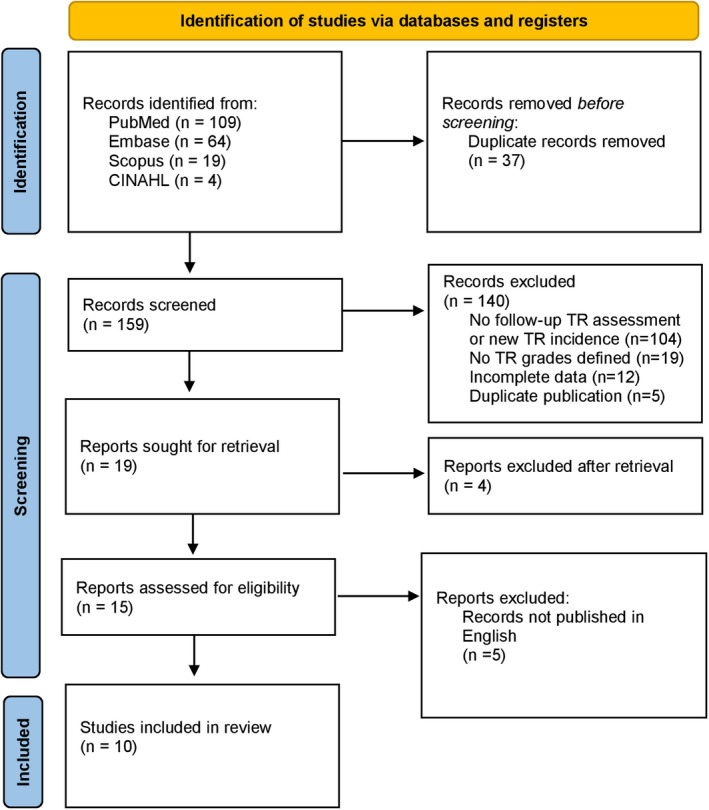
PRISMA flow chart
TABLE 1.
Baseline study characteristics
| Author | Year | Study design | Total patients | HBP patient; n (%) | Age (yrs); mean ± SD | Males; % | Type of device | Indication for HBP | HBP success rate; % | Atrial fibrillation; % | Assessment of TR severity | Incidence of new TR; n (%) | TR grade at baseline; mean ± SD | TR grade at follow‐up; mean ± SD | QRS duration before HBP (msec), mean ± SD | QRS duration after HBP (msec), mean ± SD | Baseline QRS morphology; % | Pacing percentage; % | HBP lead position; above or below TV annulus | Follow‐up; months | Study quality* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wu et al. (2021) | 2020 | Prospective cohort | 137 | 49 (38.5%) | 68.3 ± 10 | 54% | BVP HBP LBBP | Cardiac resynchronization | 51.04% | 32.7% | Overall decreased | None | 1 ± 0.9 | 0.7 ± 0.7 | 170.3 ± 19.3 | 100.7 ± 15.3 | LBBB (100%) | 99.2% | Below | 12 | 8 |
| Huang et al. (2019) | 2018 | Prospective cohort | 74 | 74 (100%) | 72.8 ± 8.3 | 58.1% | HBP | Cardiac resynchronization | 75.7% | 18.9% | Overall decreased | None | 1.0 ± 0.9 | 0.6 ± 0.6 | 173.5 ± 18.1 | 105.5 ± 19.0 | LBBB (100%) | Not reported | Above | 12 | 7 |
| Grieco et al. (2021) | 2021 | Prospective cohort | 84 | 42 (50%) | 75.1 ± 7.9 | 64% | HBP RVP | AVB | Not reported | 11% | Overall decreased | None | Severe TR (n = 3) Moderate TR (n = 9) Mild TR (n = 30) | Severe TR (n = 0) Moderate TR (n = 4) Mild TR (n = 38) | 134.9 ± 40.1 | 123.2 ± 25.9 | LBBB (31%) RBBB (14%) | Not reported | Not reported | 6 | 7 |
| Hasumi et al. (2018) | 2018 | Prospective cohort | 45 | 45 (100%) | Not reported | Not reported | HBP | AVB | Not reported | Not reported | No change | None | 3 | 1 | Not reported | Not reported | Not reported | Below | 12.5 | 6 | |
| Hu et al., 2021) | 2020 | RCT | 50 | 25 (50%) | 65.4 ± 13.5 | 42% | aHBP vHBP | AVB | 90% | 24% | Increased by grade I (n = 4) | None | Not reported | 105.9 ± 13.9 | 114.8 ± 21.2 | LBBB (20%) | Not reported | Both | 3 | 8 | |
| Hu et al. (2020) | 2020 | RCT | 50 | 25 (50%) | 61.2 ± 12.3 | 64% | HBP LBBP | AVB | 82% | 26% | Increased by grade I (n = 2) | None | Not reported | 117.1 ± 37.2 | 122.8 ± 20.1 | LBBB (20%) RBBB (20%) | Not reported | Above | 3 | 8 | |
| Ma et al. (2021) | 2020 | Prospective cohort | 52 | 37 (71.1%) | 66.8 ± 7.2 | 69.2% | HBP BVP | AVB | Not reported | 100% | Overall decreased | None | 1.4 ± 0.9 | 0.6 ± 0.7 | 110.3 ± 25.6 | 113.7 ± 17.5 | LBBB (5.4%) | 80.1% | Above | 17 | 8 |
| Shan et al. (2018) | 2017 | Prospective cohort | 18 | 16 (88.8%) | 74.8 ± 12.4 | 50% | HBP | Device upgrade | 88.9% | Not reported | No change | Not reported | 1.1 ± 0.9 | 1.2 ± 1.2 | 136.3 ± 35.1 | 101.6 ± 11.6 | LBBB (37.5%) RBBB (6.2%) | Not reported | Above | 24 | 7 |
| Vijayaraman et al. (2017) | 2017 | Prospective cohort | 20 | 20 (100%) | 74.5 ± 10.3 | 65% | HBP | HBP generator change | Not reported | 60% | Increased by grade I (n = 1) | 1 (5%) | Not reported | Not reported | 102 ± 27 | 117 ± 20 | Not reported | 77% | Above | 12 | 6 |
| Ye et al. (2021) | 2021 | Prospective cohort | 16 | 16 (100%) | 71.1 ± 3.7 | 75% | HBP LBBAP | Cardiac resynchronization | 81.6% | 100% | No change | None | Not reported | Not reported | 91 ± 10 | 100.6 ± 9 | LBBB (6.2%) | 63.1% | Above | 6 | 6 |
The included studies were published between 2017 and 2021. Two RCTs and 8 observational studies were included in the systematic review, involving 546 patients with HBP implantation, either independently or after RV lead placement. His bundle pacing was used for CRT in 3 studies, AVB in 5 studies, device upgrade to HBP in 1 study, and HBP generator change in 1 study. Patient baseline characteristics were reported in 10 articles, among 546 patients. The number and types of baseline characteristics reported varied across studies. Mean age ranged between 61.2 ± 12.3 and 75.1 ± 7.9 years and 54.1% were males. The implant success rate was 79.2% (range 51% to 90%). AF ranged between 11% to 60% in patients with HBP. In 6 studies, HBP lead was implanted above tricuspid annulus while 2 studies report implantation below the annulus.
3.2. Quality assessment
The quality evaluation of the included studies is shown in Table 1.
3.3. Primary outcomes
The reporting rate of the outcome of interest across the 10 included studies ranged from 0% to 5% (Incidence of new TR) and 9 studies reported no new incidence of TR. As for the assessment of TR severity, 3 studies reported overall decreased TR grade after HBP implantation for cardiac resynchronization. Wu et al. and Huang et al. reported an average TR grade of at least 1 at baseline and <1 after 12 months follow‐up. For indication of atrioventricular block (AVB), Grieco et al. reported improvement from moderate to mild TR grade in 7 patients and decreased TR grade from severe to moderate in 2 patients. Ma et al. reported a decrease from baseline TR grade (1.46 ± 0.96 to 0.68 ± 0.77) after 17 months follow‐up. Three studies reported an increase in TR by at least one grade. This is shown in Table 1 and Figure 3. Two studies enrolled all patients with permanent AF (Ye and Ma et al.), which demonstrated no change in TR grade after follow‐up.
FIGURE 3.
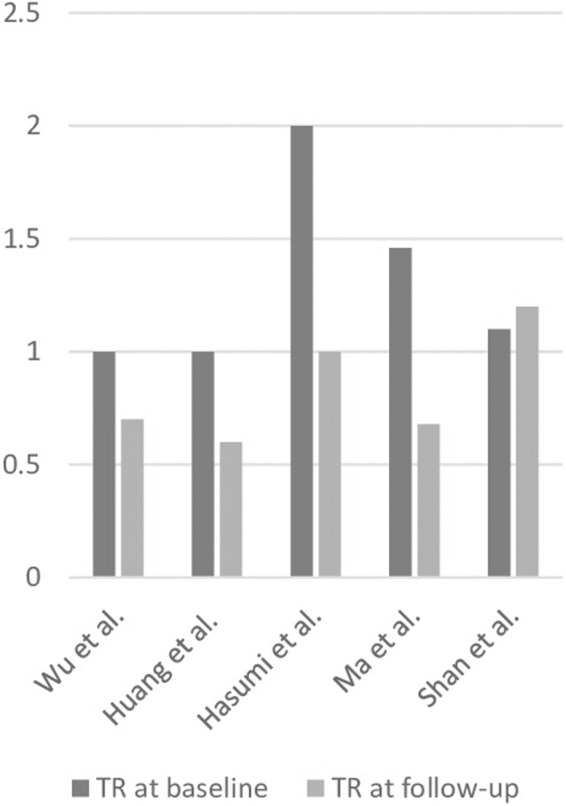
Tricuspid regurgitation grade at baseline and follow‐up
3.4. Secondary outcomes
Four studies (Wu, Huang, Grieco, and Shan et al.) reported a decrease in paced QRS duration (QRSd) while 6 studies reported an increased QRSd.
4. DISCUSSION
We systematically assessed studies on HBP with an assessment of TR, which comprised of 9 original research articles and 1 case series reporting nearly 5 years of experience from 546 patients across centers around the world (Grieco et al., 2021; Hasumi et al., 2018; Hu et al., 2020; Hu et al., 2021; Huang et al., 2019; Ma et al., 2021; Shan et al., 2018; Vijayaraman et al., 2017; Wu et al., 2021; Ye et al., 2021). This is the first systematic analysis of a patient cohort to demonstrate the incidence of TR with HBP and its quantification before and after the procedural follow‐up, demonstrating its effects on ventricular synchrony. Our systematic review shows an improvement in TR grade with a negligible risk of developing new TR after HBP (0% to 5%). Although the prevalence of TR varied considerably in these studies because the TR grading system was not uniform across studies, the cumulative reported experience supports that HBP can be a feasible option for patients having symptomatic TR, and should be considered in patients who require a high percentage of ventricular pacing. Therefore, the current study discussed the prevalence of TR after HBP implantation to improve clinicians' understanding of TR.
Studies included in this systematic review shed some light on whom the target patient may be for HBP. The majority of patients undergoing HBP had basic characteristics, which reflect that of a typical pacemaker population. Conversely, 2 studies consisted of patients with heart failure symptoms and an established indication for CRT, although the application for replacing RV apical pacing or BiV pacing has gained more interest in this patient population. Recent evidence has suggested a role of HBP in bundle branch block and LV dysfunction who are a candidate for CRT because it can lead to QRS narrowing in distal His bundle pacing (Sharma et al., 2016). However, the long‐term comparison will need to be interpreted when clinical data from prospective clinical trials are out.
4.1. Mechanism of lead‐mediated TR
The phenomenon of lead‐mediated TR was proposed in 1969 by Nachnani et al. when they that patient had a TR murmur after implantation of RV electrode (Nachnani et al., 1969). The murmur disappeared after the lead was removed. With the understanding of this mechanism, many studies have discussed the incidence, mechanism, diagnosis, and treatment of lead‐mediated TR.
After lead placement, TR can occur via multiple mechanisms (Figure 2). It can be caused by mechanical causes like scar or thrombus formation on the leads impairing closure. Laceration or perforation is another cause of TR. However, the most common mechanism in lead‐mediated TR is asynchrony, leading to abnormal RV activation from a pacemaker (Chen et al., 2007). In the 1970s, postmortem investigations demonstrated that pacemaker leads can adhere to the TV leaflets or the papillary muscles (Gibson et al., 1980). In chronic TR, a number of studies have demonstrated that adhesion of TV leaflet to the pacing lead results in restricted movement, causing an abnormal coaptation of the posterior leaflet with the anterior and septal leaflets (Addetia et al., 2019; Tatum et al., 2021).
FIGURE 2.
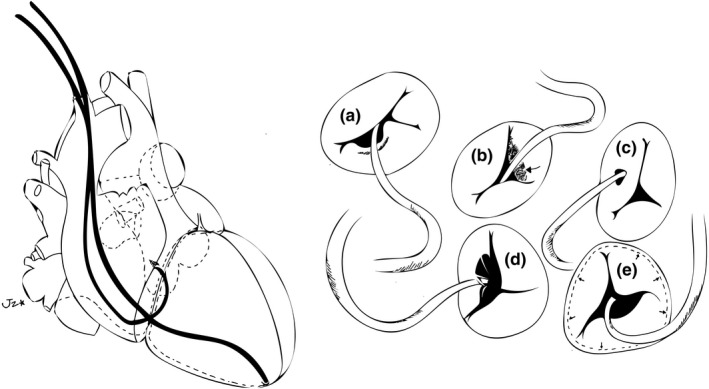
Mechanism of mechanical tricuspid regurgitation in the setting of permanent pacemaker (a) valve obstruction with leads in between the leaflets (b) Lead adherence due to scar formation and fibrosis (c) valve perforation (d) Lead entrapment in tricuspid valve apparatus (e) annular dilatation
In early experience with HBP, lead placement at the HB was performed using the standard catheters. With the advent of contemporary tools and delivery systems, mapping of the HB using the lead itself became feasible and resulted in marked improvement in implantation success rate (Qian et al., 2019). A speculative advantage in HBP may be right AV septal pacing, which can prevent RV lead‐mediated TR (Payne et al., 2018).
One study studied feasibility and safety of HBP in patients with AF. Apart from their main objective, they demonstrated that there was no change in TR and mitral regurgitation (MR) after HBP implantation at 6‐months follow‐up (Ye et al., 2021). Some studies have demonstrated AF as a risk factor for developing tricuspid regurgitation; however, the abovementioned study exhibited a lower incidence of TR after HBP implantation in patient with AF (Xu et al., 2021). One other study compared HBP and BiV pacing in candidates for CRT. As low LVEF is a risk factor for developing TR in view of dilated cardiac chambers, this study demonstrated that after HBP, baseline TR reduced from baseline at 12‐months follow‐up (Wu et al., 2021). Similarly, an abstract published in Circulation demonstrated improvement of TR significantly after HBP across all patients (p = .033), and in subgroups with reduced LVEF (p = .019) (Wey et al., 2019). Another study showed long‐term outcomes of HBP in patients with heart failure and LBBB. Apart from improved LVEF and QRSd, it demonstrated an improvement of TR from grade 3 to grade 1 (Hasumi et al., 2018). These studies demonstrated that low LVEF is a risk factor for developing TR, and LV dyssynchrony caused by right ventricular pacing can lead to reduced LVED. RV apical pacing is a well‐recognized cause of ventricular dyssynchrony, which can result in PICM. In literature, with ≥20% RV pacing burden, there is a 20% risk of developing PICM (Kiehl et al., 2016). By utilizing the His‐Purkinje system, HBP can reinstitute ventricular synchrony and reverse PICM.
This systematic review shows that after HBP, not only is there a negligible chance of new lead‐mediated TR, there is marked improvement in TR grade and EF from baseline and follow‐up (Figures 3 and 4). The included studies did not assess the cause for improvement in TR grade, but by virtue of the abovementioned principle, there seems to be a reversal of TV pathology caused by RV pacing. Hence, HBP may be an option for patients who develop lead‐mediated TR.
FIGURE 4.
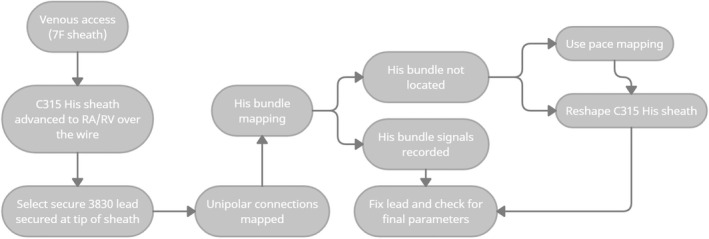
Algorithm for His bundle pacing
4.2. Standard technique and challenges
A simplified algorithm for the implantation of HBP is shown in Figure 4. Currently, SelectSecure 3830 (Medtronic) has been the most studied lead. It is implanted via delivery sheaths or catheters including the C315 HIS or the newly approved SelectSite C304 HIS catheter. The C314 HIS delivery sheath has a 7.0 F outer diameter and has a distal (primary) and a proximal (secondary) curve to direct it towards the tricuspid annulus. After venous access, the delivery sheath is advanced over a guidewire to the TV annulus. The 3830 lead is then advanced towards the tip to map the HB region in a unipolar configuration.
The system is maneuvered towards the atrioventricular (AV) septum and when an HB electrogram is identified, and when the operator is satisfied with the pacing parameters at the HB region, the lead is fixed by rotating the lead body in a clockwise direction. A torque back and spinning of the lead is generally a marker of adequate fixation. The sheath is then withdrawn to the right atrium (RA) where the lead parameters are assessed in both unipolar and bipolar configurations. Implantation of the lead distal to the disease is important in achieving low capture thresholds (Barba‐Pichardo et al., 2013; Dandamudi & Vijayaraman, 2016).
4.3. Future prospects and limitations
Despite the promised results in terms of HB mapping, 20% of the patients have more distal or widespread conduction defects, and HBP might not be able to cover come to BBBs with reasonable implantation and capture threshold. A technique for pacing LBBB via an intra‐septal approach to restore the function of the distal Purkinje conduction system was introduced by Huang and colleagues (Huang et al., 2017). However, more data are needed to assess the safety and efficacy of this technique. Therefore, LBBB pacing provides a supplementary option for patients with distal conduction disease and ventricular dyssynchrony.
As for future studies, despite the data presented above, there are no large‐scale, randomized trials comparing the effectiveness of HBP with conventional RV pacing to assess and quantify TR and its mechanism in HBP. Although the 2 included RCTs suggest a negative incidence of TR, no long‐term outcome data are available. Furthermore, large, multicenter, randomized studies comparing HBP and BiV pacing for assessment of EF and NYHA class are necessary to evaluate the clinical efficacy of HBP. There should be the creation of registries for HBP patients involving, but not limited to, TR and other echocardiographic parameters for LVEF and RV functions. Finally, in addition to data, improved lead designs and delivery tools are needed to increase the success rates of HBP.
There were several limitations to this systematic review. First, most of the included studies had no outcome measure to identify TR in a quantitative manner. Therefore, a quantitative synthesis could not be performed because the TR grading system was not standardized in different studies. Therefore, relevant data of the quantitative endpoint of TR need to be further improved. Second, most of the included studies were not randomized and controlled for confounders. The observational nature of the majority of studies might produce an inherent limitation and might impact the observed findings. Third, these studies lacked some data that may have led to deterioration or improvement of TR, such as pulmonary hypertension, mitral regurgitation, and increased RV size, etc. Fourth, there was a heterogeneity among studies regarding HBP indications. Lastly, more controlled and randomized trials should be carried out to assess the range and long‐term implications of TR with and without HBP.
5. CONCLUSION
In conclusion, HBP truly represents the most physiological form of ventricular activation. Current data suggests that HBP causes an improvement of TR grade in patients implanted with CIEDs or are candidates for CRT. However, there is a need for widespread adoption of this technique, which can help in further validation of its efficacy in large, randomized trials.
AUTHOR CONTRIBUTIONS
Syed Muhammad Jawad Zaidi involved in literature review and first drafting of the manuscript; Hasan Sohail involved in first and final drafting of the manuscript; Danish Iltaf Satti involved in literature search; Abdul Sami and Mateen Anwar are involved in first drafting of the manuscript; Jahanzeb Malik involved in conceptualization, first drafting, final drafting, methodology, literature search, and figures; Bilal Mustafa involved in first draft and formatting; Mohammad Mustafa involved in first draft, review, and editing, Amin Mehmoodi involved in supervision, first draft, and tables.
CONFLICT OF INTEREST
The authors declare no competing interests.
ETHICS STATEMENT
Not applicable.
Zaidi, S. M. J. , Sohail, H. , Satti, D. I. , Sami, A. , Anwar, M. , Malik, J. , Mustafa, B. , Mustafa, M. , & Mehmoodi, A. (2022). Tricuspid regurgitation in His bundle pacing: A systematic review. Annals of Noninvasive Electrocardiology, 27, e12986. 10.1111/anec.12986
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study
REFERENCES
- Abdelrahman, M. , Subzposh, F. A. , Beer, D. , Durr, B. , Naperkowski, A. , Sun, H. , Oren, J. W. , Dandamudi, G. , & Vijayaraman, P. (2018). Clinical outcomes of his bundle pacing compared to right ventricular pacing. Journal of the American College of Cardiology, 71(20), 2319–2330. 10.1016/j.jacc.2018.02.048 [DOI] [PubMed] [Google Scholar]
- Addetia, K. , Harb, S. C. , Hahn, R. T. , Kapadia, S. , & Lang, R. M. (2019). Cardiac implantable electronic device Lead‐induced tricuspid regurgitation. JACC: Cardiovascular Imaging, 12(4), 622–636. 10.1016/j.jcmg.2018.09.028 [DOI] [PubMed] [Google Scholar]
- Ahmed, I. , & Kayani, W. T. (2021. Available from:). Biventricular Devices. [Updated 2021 Jun 25]. In: StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK567773/ [Google Scholar]
- Arabi, P. , Özer, N. , Ateş, A. H. , Yorgun, H. , Oto, A. , & Aytemir, K. (2015). Effects of pacemaker and implantable cardioverter defibrillator electrodes on tricuspid regurgitation and right sided heart functions. Cardiology Journal, 22(6), 637–644. 10.5603/CJ.a2015.0060 [DOI] [PubMed] [Google Scholar]
- Barba‐Pichardo, R. , Manovel Sánchez, A. , Fernández‐Gómez, J. M. , Moriña‐Vázquez, P. , Venegas‐Gamero, J. , & Herrera‐Carranza, M. (2013). Ventricular resynchronization therapy by direct his‐bundle pacing using an internal cardioverter defibrillator. Europace, 15(1), 83–88. 10.1093/europace/eus228 [DOI] [PubMed] [Google Scholar]
- Cheema, M. A. , Almas, T. , Ullah, W. , & Haas, D. (2021). RV lead placement ‐ a forgotten cause of right heart failure. Ann Med Surg (Lond)., 7(67), 102461. 10.1016/j.amsu.2021.102461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, T. E. , Wang, C. C. , Chern, M. S. , & Chu, J. J. (2007). Entrapment of permanent pacemaker lead as the cause of tricuspid regurgitation. Circulation Journal, 71(7), 1169–1171. 10.1253/circj.71.1169 [DOI] [PubMed] [Google Scholar]
- Curtis, A. B. , Worley, S. J. , Chung, E. S. , Li, P. , Christman, S. A. , & M., S. J. S. (2016). Improvement in clinical outcomes with biventricular versus right ventricular pacing: The BLOCK HF study. Journal of the American College of Cardiology, 67(18), 2148–2157. 10.1016/j.jacc.2016.02.051 [DOI] [PubMed] [Google Scholar]
- Dandamudi, G. , & Vijayaraman, P. (2016). How to perform permanent his bundle pacing in routine clinical practice. Heart Rhythm, 13(6), 1362–1366. 10.1016/j.hrthm.2016.03.040 [DOI] [PubMed] [Google Scholar]
- Funck, R. C. , Blanc, J. J. , Mueller, H. H. , Schade‐Brittinger, C. , Bailleul, C. , & Maisch, B. (2006). BioPace study group. Biventricular stimulation to prevent cardiac desynchronization: Rationale, design, and endpoints of the 'Biventricular pacing for atrioventricular block to prevent cardiac desynchronization (BioPace)' study. Europace, 8(8), 629–635. 10.1093/europace/eul075 [DOI] [PubMed] [Google Scholar]
- Furman, S. , & Schwedel, J. B. (1959. Nov). An intracardiac pacemaker for stokes‐Adams seizures. The New England Journal of Medicine, 5(261), 943–948. 10.1056/NEJM195911052611904 [DOI] [PubMed] [Google Scholar]
- Gibson, T. C. , Davidson, R. C. , & DeSilvey, D. L. (1980). Presumptive tricuspid valve malfunction induced by a pacemaker lead: A case report and review of the literature. Pacing and Clinical Electrophysiology, 3(1), 88–95. 10.1111/j.1540-8159.1980.tb04307.x [DOI] [PubMed] [Google Scholar]
- Glikson, M. , Nielsen, J. C. , Kronborg, M. B. , Michowitz, Y. , Auricchio, A. , Barbash, I. M. , Barrabés, J. A. , Boriani, G. , Braunschweig, F. , Brignole, M. , Burri, H. , Coats, A. J. S. , Deharo, J. C. , Delgado, V. , Diller, G. P. , Israel, C. W. , Keren, A. , Knops, R. E. , Kotecha, D. , … Tolosana, J. M. (2021). 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy. European Heart Journal, 42(35), 3427–3520. 10.1093/eurheartj/ehab364 [DOI] [PubMed] [Google Scholar]
- Grieco, D. , Bressi, E. , Curila, K. , Padala, S. K. , Sedlacek, K. , Kron, J. , Fedele, E. , Ionita, O. , Giannuzzi, S. , Fagagnini, A. , Panattoni, G. , de Ruvo, E. , Ellenbogen, K. A. , & Calò, L. (2021). Impact of his bundle pacing on right ventricular performance in patients undergoing permanent pacemaker implantation. Pacing and Clinical Electrophysiology, 44(6), 986–994. 10.1111/pace.14249 [DOI] [PubMed] [Google Scholar]
- Hasumi, E. , Fujiu, K. , Kawata, T. , & Komuro, I. (2018). The influence of his bundle pacing on tricuspid valve functioning using three‐dimensional echocardiography. HeartRhythm Case Rep., 4(9), 437–438. 10.1016/j.hrcr.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höke, U. , Auger, D. , Thijssen, J. , Wolterbeek, R. , van der Velde, E. T. , Holman, E. R. , Schalij, M. J. , et al. (2014). Significant lead‐induced tricuspid regurgitation is associated with poor prognosis at long‐term follow‐up. Heart, 100(12), 960–968. 10.1136/heartjnl-2013-304673 [DOI] [PubMed] [Google Scholar]
- Hu, Y. , Gu, M. , Hua, W. , Niu, H. , Li, H. , Chen, X. , Zhang, N. , et al. (2020). Electrical characteristics of pacing different portions of the his bundle in bradycardia patients. Europace, 22(Suppl_2), ii27–ii35. 10.1093/europace/euaa309 [DOI] [PubMed] [Google Scholar]
- Hu, Y. , Li, H. , Gu, M. , Hua, W. , Niu, H. , Zhang, N. , Liu, X. , et al. (2021). Comparison between his‐bundle pacing and left bundle branch pacing in patients with atrioventricular block. Journal of Interventional Cardiac Electrophysiology, 62(1), 63–73. 10.1007/s10840-020-00869-w [DOI] [PubMed] [Google Scholar]
- Huang, W. , Su, L. , Wu, S. , Xu, L. , Xiao, F. , Zhou, X. , & Ellenbogen, K. A. (2017). A novel pacing strategy with low and stable output: Pacing the left bundle branch immediately beyond the conduction block. The Canadian Journal of Cardiology, 33(12), 1736.e1–1736.e3. 10.1016/j.cjca.2017.09.013 [DOI] [PubMed] [Google Scholar]
- Huang, W. , Su, L. , Wu, S. , Xu, L. , Xiao, F. , Zhou, X. , Mao, G. , Vijayaraman, P. , & Ellenbogen, K. A. (2019). Long‐term outcomes of his bundle pacing in patients with heart failure with left bundle branch block. Heart, 105(2), 137–143. 10.1136/heartjnl-2018-313415 [DOI] [PubMed] [Google Scholar]
- Khurshid, S. , Epstein, A. E. , Verdino, R. J. , Lin, D. , Goldberg, L. R. , Marchlinski, F. E. , & Frankel, D. S. (2014). Incidence and predictors of right ventricular pacing‐induced cardiomyopathy. Heart Rhythm, 11(9), 1619–1625. 10.1016/j.hrthm.2014.05.040 [DOI] [PubMed] [Google Scholar]
- Kiehl, E. L. , Makki, T. , Kumar, R. , Gumber, D. , Kwon, D. H. , Rickard, J. W. , Kanj, M. , Wazni, O. M. , Saliba, W. I. , Varma, N. , Wilkoff, B. L. , & Cantillon, D. J. (2016). Incidence and predictors of right ventricular pacing‐induced cardiomyopathy in patients with complete atrioventricular block and preserved left ventricular systolic function. Heart Rhythm, 13(12), 2272–2278. 10.1016/j.hrthm.2016.09.027 [DOI] [PubMed] [Google Scholar]
- Kim, J. B. , Spevack, D. M. , Tunick, P. A. , Bullinga, J. R. , Kronzon, I. , Chinitz, L. A. , & Reynolds, H. R. (2008). The effect of transvenous pacemaker and implantable cardioverter defibrillator lead placement on tricuspid valve function: An observational study. Journal of the American Society of Echocardiography, 21(3), 284–287. 10.1016/j.echo.2007.05.022 [DOI] [PubMed] [Google Scholar]
- Lamas, G. A. , Lee, K. , Sweeney, M. , Leon, A. , Yee, R. , Ellenbogen, K. , Greer, S. , Wilber, D. , Silverman, R. , Marinchak, R. , Bernstein, R. , Mittleman, R. S. , Lieberman, E. H. , Sullivan, C. , Zorn, L. , Flaker, G. , Schron, E. , Orav, E. J. , & Goldman, L. (2000). The mode selection trial (MOST) in sinus node dysfunction: Design, rationale, and baseline characteristics of the first 1000 patients. American Heart Journal, 140(4), 541–551. 10.1067/mhj.2000.109652 [DOI] [PubMed] [Google Scholar]
- Ma, P. P. , Yang, Y. H. , Dai, B. L. , Zhang, R. F. , Wang, N. , Li, D. N. , Yin, X. M. , et al. (2021). Brady‐arrhythmias in patients with atrial fibrillation and heart failure of reduced ejection fraction: Is his‐bundle pacing superior to biventricular pacing? Pacing and Clinical Electrophysiology, 44(7), 1193–1199. 10.1111/pace.14289 [DOI] [PubMed] [Google Scholar]
- Mandras, S. A. , & Desai, S. (2021. Available from:). Right Heart Failure. [Updated 2021 Jul 21]. In: StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459381/ [PubMed] [Google Scholar]
- Matusik, P. , Woznica, N. , & Lelakowsk, J. (2010). Atrial fibrillation before and after pacemaker implantation (WI and DDD) in patients with complete atrioventricular block. Pol Merkur Lekarski, 28(167), 345–349. [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2010). PRISMA group. Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. Int J Surg, 8(5), 336–341. 10.1016/j.ijsu.2010.02.007 Erratum in: Int J Surg. 2010;8(8):658. PMID: 20171303 [DOI] [PubMed] [Google Scholar]
- Mond, H. G. , & Proclemer, A. (2011). The 11th world survey of cardiac pacing and implantable cardioverter‐defibrillators: Calendar year 2009‐‐a world Society of Arrhythmia's project. Pacing and Clinical Electrophysiology, 34(8), 1013–1027. 10.1111/j.1540-8159.2011.03150.x [DOI] [PubMed] [Google Scholar]
- Nachnani, G. H. , Gooch, A. S. , & Hsu, I. (1969). Systolic murmurs induced by pacemaker catheters. Archives of Internal Medicine, 124, 202–205. [PubMed] [Google Scholar]
- National Institutes of Health (2021). Quality assessment tool for observational cohort and cross‐sectional studies. Available online at: https://www.nhlbi.nih.gov/health‐pro/guidelines/in‐develop/cardiovascular‐risk‐reduction/tools/cohort (Accessed 1 October 2021)
- Ousdigian, K. T. , Borek, P. P. , Koehler, J. L. , Heywood, J. T. , Ziegler, P. D. , & Wilkoff, B. L. (2014). The epidemic of inadequate biventricular pacing in patients with persistent or permanent atrial fibrillation and its association with mortality. Circulation. Arrhythmia and Electrophysiology, 7(3), 370–376. 10.1161/CIRCEP.113.001212 [DOI] [PubMed] [Google Scholar]
- Payne, J. , Garlitski, A. C. , Weinstock, J. , Homoud, M. , Madias, C. , & Estes, N. A. M. (2018). His bundle pacing. Journal of Interventional Cardiac Electrophysiology, 52(3), 323–334. 10.1007/s10840-018-0412-5 [DOI] [PubMed] [Google Scholar]
- Qian, Z. , Zou, F. , Wang, Y. , Qiu, Y. , Chen, X. , Jiang, H. , & Hou, X. (2019). Permanent his bundle pacing in heart failure patients: A systematic review and meta‐analysis. Pacing and Clinical Electrophysiology, 42(2), 139–145. 10.1111/pace.13565 [DOI] [PubMed] [Google Scholar]
- Sanchez, R. , Nadkarni, A. , Buck, B. , Daoud, G. , Koppert, T. , Okabe, T. , Houmsse, M. , et al. (2021). Incidence of pacing‐induced cardiomyopathy in pacemaker‐dependent patients is lower with leadless pacemakers compared to transvenous pacemakers. J Cardiovasc Electrophysiol, 32(2), 477–483. 10.1111/jce.14814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan, P. , Su, L. , Zhou, X. , Wu, S. , Xu, L. , Xiao, F. , Zhou, X. , Ellenbogen, K. A. , & Huang, W. (2018). Beneficial effects of upgrading to his bundle pacing in chronically paced patients with left ventricular ejection fraction <50. Heart Rhythm, 15(3), 405–412. 10.1016/j.hrthm.2017.10.031 [DOI] [PubMed] [Google Scholar]
- Sharma, P. S. , Dandamudi, G. , Naperkowski, A. , Oren, J. W. , Storm, R. H. , Ellenbogen, K. A. , & Vijayaraman, P. (2015). Permanent his‐bundle pacing is feasible, safe, and superior to right ventricular pacing in routine clinical practice. Heart Rhythm, 12(2), 305–312. 10.1016/j.hrthm.2014.10.021 [DOI] [PubMed] [Google Scholar]
- Sharma, P. S. , Huizar, J. , Ellenbogen, K. A. , & Tan, A. Y. (2016). Recruitment of bundle branches with permanent his bundle pacing in a patient with advanced conduction system disease: What is the mechanism? Heart Rhythm, 13(2), 623–625. 10.1016/j.hrthm.2015.11.012 [DOI] [PubMed] [Google Scholar]
- Tatum, R. , Maynes, E. J. , Wood, C. T. , Deb, A. K. , Austin, M. A. , O'Malley, T. J. , Choi, J. H. , et al. (2021). Tricuspid regurgitation associated with implantable electrical device insertion: A systematic review and meta‐analysis. Pacing and Clinical Electrophysiology, 44(8), 1297–1302. 10.1111/pace.14287 [DOI] [PubMed] [Google Scholar]
- Van De Heyning, C. M. , Elbarasi, E. , Masiero, S. , Brambatti, M. , Ghazal, S. , Al‐Maashani, S. , Capucci, A. , et al. (2019). Prospective study of tricuspid regurgitation associated with permanent leads after cardiac rhythm device implantation. The Canadian Journal of Cardiology, 35(4), 389–395. 10.1016/j.cjca.2018.11.014 [DOI] [PubMed] [Google Scholar]
- Vijayaraman, P. , Dandamudi, G. , Lustgarten, D. , & Ellenbogen, K. A. (2017). Permanent his bundle pacing: Electrophysiological and echocardiographic observations from long‐term follow‐up. Pacing and Clinical Electrophysiology, 40(7), 883–891. 10.1111/pace.13130 [DOI] [PubMed] [Google Scholar]
- Wey, H. E. , Desai, P. V. , Lattell, J. , Beaser, A. , Aziz, Z. A. , Nayak, H. , Tung, R. , et al. (2019). Abstract 15104: His‐bundle pacing improves tricuspid regurgitation in patients with bradyarrhythmia. Circulation, 140, A15104. 10.1161/circ.140.suppl_1.15104 [DOI] [Google Scholar]
- Wu, S. , Su, L. , Vijayaraman, P. , Zheng, R. , Cai, M. , Xu, L. , Shi, R. , Huang, Z. , Whinnett, Z. I. , & Huang, W. (2021). Left bundle branch pacing for cardiac resynchronization therapy: Nonrandomized on‐treatment comparison with his bundle pacing and biventricular pacing. The Canadian Journal of Cardiology, 37(2), 319–328. 10.1016/j.cjca.2020.04.037 [DOI] [PubMed] [Google Scholar]
- Xu, J. , Han, J. , Zhang, H. , Meng, F. , Luo, T. , Tian, B. , Wang, J. , Jiao, Y. Q. , Yu, H. M. , & Meng, X. (2021). Risk factors for postoperative recurrent tricuspid regurgitation after concomitant tricuspid annuloplasty during left heart surgery and the association between tricuspid annular circumference and secondary tricuspid regurgitation. BMC Cardiovascular Disorders, 21(1), 50. 10.1186/s12872-021-01870-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye, Y. , Zhang, K. , Yang, Y. , Jiang, D. , Pan, Y. , Sheng, X. , Wang, B. , Yu, C. , Zhang, Z. , Zhang, J. , Wang, L. , Jiang, J. , Sun, Y. , Liu, Q. , Cheng, Y. , Gao, B. , Wang, M. , He, H. , Jiang, C. , & Fu, G. (2021). Feasibility and safety of both his bundle pacing and left bundle branch area pacing in atrial fibrillation patients: Intermediate term follow‐up. Journal of Interventional Cardiac Electrophysiology. 10.1007/s10840-021-00964-6 [online ahead of print] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study


