Abstract
We examine the efficacy of MARHABA, a social marketing-informed, lay health worker (LHW) intervention with patient navigation (PN), to increase breast and cervical cancer screening among Muslim women in New York City. Muslim women were eligible if they were overdue for a mammogram and/or a Pap test. All participants attended a 1-hour educational seminar with distribution of small media health education materials, after which randomization occurred. Women in the Education + Media + PN arm received planned follow-ups from a LHW. Women in the Education + Media arm received no further contact. A total of 428 women were randomized into the intervention (214 into each arm). Between baseline and 4-month follow-up, mammogram screening increased from 16.0% to 49.0% in the Education + Media + PN arm (p<0.001), and from 14.7% to 44.6% in the Education + Media arm (p<0.001). Pap test screening increased from 16.9% to 42.3% in the Education + Media + PN arm (p<0.001) and from 17.3% to 37.1% in the Education + Media arm (p<0.001). Cancer screening knowledge increased in both groups. Between group differences were not statistically significant for screening and knowledge outcomes. A longer follow-up period may have resulted in a greater proportion of up-to-date screenings, given that many women had not yet received their scheduled screenings. Findings suggest that the educational session and small media materials were perhaps sufficient to increase breast and cervical cancer screening among Muslim American women.
Trial Registration:
Keywords: Asian Americans, Muslim Americans, Breast cancer screening, Cervical cancer screening, Community-based participatory research
Introduction
Islam is one of the fastest growing religions in the United States (US). While religious affiliation is not collected on the Census, an estimated 3.45 million Muslims lived in the US in 2017, up from 2.35 million in 2007, with a projection that the Muslim population will reach 8.1 million by 2050. Around 58% of US Muslims are immigrants, and within the Muslim population, there is great ethnic, social, and cultural diversity. Among foreign-born Muslims, the largest group hails from South Asia, followed by the Middle East and North Africa [1]. The largest concentration of US Muslims lives in New York City (NYC) and the surrounding metropolitan area; there are an estimated 700,000 Muslim residents and 250 mosques [2].
Community-based studies have found that Muslim women have lower rates of timely breast and cervical cancer screenings compared to other racial and ethnic groups, though population-wide data is limited [3, 4]. Qualitative studies have also shown low rates of timely screenings and a lack of knowledge regarding Pap testing and cervical cancer [5, 6]. Common documented barriers to breast and cervical cancer screening among Muslim women often relate to religious concerns, which include modesty, decency, and the perception that breast and cervical exams are inconsistent with Islamic beliefs and customs; exposure of the body may be perceived as a violation of modesty and can result in feelings of anxiety and embarrassment [3–5]. Additional barriers include limited knowledge of screening guidelines, language concordance, perceived discrimination, transportation barriers, and lack of insurance or underinsurance [7, 8].
Community health worker (CHW) and/or lay health worker (LHW) interventions are a promising strategy to address multilevel barriers to cancer screening; CHWs and LHWs are community-based non-professionals often coming from the communities they serve, who help fill a gap in linking underserved individuals to the health care system [9]. A systematic review on interventions to increase breast and cervical cancer screening among Asian American women found that LHW interventions helped participants address access-to-care barriers and increased preventive cancer screenings [10]. Given the diversity of the Muslim population and potentially different cancer screening barriers, LHWs can reflect their communities’ local needs and priorities, as well as tailor the health promotion interventions appropriately.
In 2013, a series of key informant interviews with Muslim leaders in NYC were conducted to understand contextual factors impacting the health-seeking behaviors of Muslim women and to solicit recommendations for development of health interventions. Key informants noted variations in ethnic beliefs and practices across diverse Muslim communities as barriers to care, asserting the importance of educational and in-language materials and messaging, and engagement of mosques and religious leaders [6]. Building on these findings, we conducted a mixed-method study with 98 Muslim women in NYC from diverse ethnic communities, which revealed low rates of timely mammogram (71%) among women ≥40 years of age and low rates of timely Pap tests (54%) among women ≥21 years of age, despite high rates of insurance and access to a primary health care provider. However, limited English proficiency, a potential barrier to care, was high. Barriers to screening included a lack of interpretation services and female healthcare providers, and limited culturally-competent care. There also was misinformation and limited knowledge about cancer screenings, as well as high stigma, when discussing cancer openly among community members. Women believed the mosque and key community and religious leaders would be an effective approach to disseminate information.
The Community Preventive Services Task Force recommends a small media approach, using videos and printed materials (e.g., brochures, pamphlets, flyers, newsletters), to educate and motivate individuals to get screened for cancer. A small Arkansas study presented African American women with a Susan G. Komen Breast Cancer Foundation shower card, in combination with an education session and breast self-examination demonstrations. The control group received no session. The intervention group had significantly higher cancer knowledge and beliefs scores compared to the control group [11].
To our knowledge, prior to our investigation, only two breast and/or cervical cancer interventions have been documented with Muslim American women. Both interventions leveraged stakeholder engagement (e.g., community-based organizations, mosques) to develop religiously-tailored messaging that addressed barriers to breast and/or cervical cancer screening. The first intervention was mosque-based and peer-led, and increased the likelihood of obtaining a mammogram in a sample of 58 South Asian and Arab/Arab American Muslim women [12]. The second intervention was piloted with 30 Somali American Muslim women and 10 male Imams in a mosque setting. It was found to be feasible and acceptable; overall attitudes towards breast and cervical cancer screening improved [13]. While these studies demonstrated the feasibility of partnering with community stakeholders to create and deliver religiously tailored interventions with Muslim American women, they had small sample sizes, lacked a comparison group, and did not evaluate the uptake of breast and cervical cancer screening. In addition, they did not integrate or evaluate a patient navigation (PN) component to address upstream healthcare-related navigation barriers.
Guided by community-based participatory research (CBPR), social marketing theory, and formative research with Muslim community partners in NYC, we co-created with community partners “Muslim Americans Reaching for Health and Building Alliances” (MARHABA), a culturally and religiously adapted LHW intervention to increase breast and cervical cancer screening among Muslim American women in NYC [14]. MARHABA is a two-arm randomized controlled trial (RCT) comparing an Education + Media + PN arm to an Education + Media arm. We hypothesize that compared to the Education + Media arm, at 4-month follow-up the Education + Media + PN arm will have higher rates of: 1) timely receipt of mammogram, and 2) timely receipt of Pap test.
Methods
The lead CHW in the MARHABA study had been an active community leader for over 20 years. She had previously worked on CHW interventions in the South Asian community, and had taken part in a CHW core competency training program which consisted of a two-part, 105-hour training. Nine LHWs were recruited from the community and trained by the CHW and project coordinators. The CHW was a full-time employee at NYU Medical Center, while the LHWs were part-time and supervised by the CHW. A specially designed project training manual provided the LHWs with detailed knowledge about cancer screenings; their training lasted approximately nine hours. Topics included: background on Muslims in the US, cancer screening recommendations, project details (goals, participation criteria, participant engagement, screening and informed consent, survey administration, the education seminar, follow-up contacts), frequently asked questions on breast and cervical cancer, and screening resources. LHWs were provided with business cards to aid in follow-up with participants. When LHWs and the CHW accompanied participants to screening visits, they used the opportunity to provide guidance on cultural tailoring care delivery to health providers serving the Muslim communities. For example, mammogram technicians were taught “right” and “left” in Bangla, and doctors were educated on Muslim cultural beliefs.
Study design and recruitment.
The MARHABA intervention was conducted in partnership with local community-based organizations (CBOs) and mosques in NYC. Muslim American women were recruited to participate in the study by LHWs through community contacts of LHWs, at mosques after prayers and/or prayer groups, and at CBOs in Brooklyn, Queens, and the Bronx. Participants were eligible for the study if they met the following criteria: 1) self-identification as Muslim; 2) female; 3) residence in a NYC borough; 4) age 40–75; and 5) self-reported receipt of mammogram greater than two years ago or never and/or self-reported receipt of Pap test greater than three years ago or never (if no hysterectomy). Women who had received breast reconstructive surgery were considered ineligible for participation.
The educational seminar was one session. It took place at mosques, community centers, homes of community members of LHWs, or in parks. Often there was a physical activity component, such as an exercise session with stretching, which was an additional incentive for women to join. The seminar was provided in-language (i.e., English, Bengali, and Arabic) by the CHW or LHW. A few of the seminars that were delivered to Indonesian women were presented in English while being translated by a hired individual into Indonesian. The U.S. Preventive Services Task Force (USPSTF) screening guidelines were included as part of the educational seminar; these guidelines recommend mammogram screening beginning at age 50, discussion with a doctor from age 40–49, and discussion about Pap screening with a doctor if older than 65 [15]. Given the propensity of women in Muslim countries presenting with breast cancer at a younger age and later stage, the full sample was recommended to initiate mammography screening [16].
During the session, all women were provided with small media health education materials (e.g., brochures and palm cards) regarding breast and cervical cancer. These materials were guided by social marketing theory [17]. They were developed in several languages (English, Bengali, Arabic, and French), and were culturally- and linguistically-adapted in order to appeal and be accessible to Muslim women. We also conducted extensive formative research with the communities to clarify the four P’s of the marketing mix to ensure the intervention materials were tailored to Muslim women. Specifically, the content of the small media materials minimized the barriers (Price) to breast and cervical cancer screening identified in the formative research (e.g., culturally-tailoring the messaging and providing guidance on cancer screening access). For example, participants received guidance on their rights to request a female healthcare provider or a provider who spoke their native language, and all materials contained information on accessing low-cost or free cancer screenings in NYC, including locations and contact information of clinical sites offering screening services. The materials framed breast and cervical cancer screening as a strategy to maintain a healthy mother role, which aligns with the community’s family-centered cultural and gender norms (Product). The intervention was delivered by trusted LHWs and in community settings frequented by women (Place). The small media materials were created in-language by an advertising firm specializing in Asian American marketing, with input from community members. Materials included a flip chart with information presented during the session, posters, brochures, and palm cards (Promotion).
After completion of the educational seminar, participants were randomized by age group into either the Education + Media + PN arm or the Education + Media arm. Family members were randomized into the same group to help prevent contamination. The Education + Media + PN arm received additional in-person or phone interactions to provide support on locating and making appointments for screening tests, which also included assistance with transportation. The additional support from the LHW was individualized to each participant’s specific needs, therefore contamination was unlikely. After four months, participants in both arms were contacted by the LHW to complete a follow-up survey in-person or by phone. The intervention took place between March 2017 and September 2018. IRB approval was obtained through NYU Grossman School of Medicine in 2017.
A total of 447 individuals were assessed for eligibility, and 428 were randomized into the intervention (214 into each study arm). In the Education + Media + PN arm, one individual was lost to follow-up, one passed away, and two became ineligible post allocation. In the Education + Media arm, one individual was lost to follow-up and two became ineligible post allocation (Figure 1).
Figure 1.
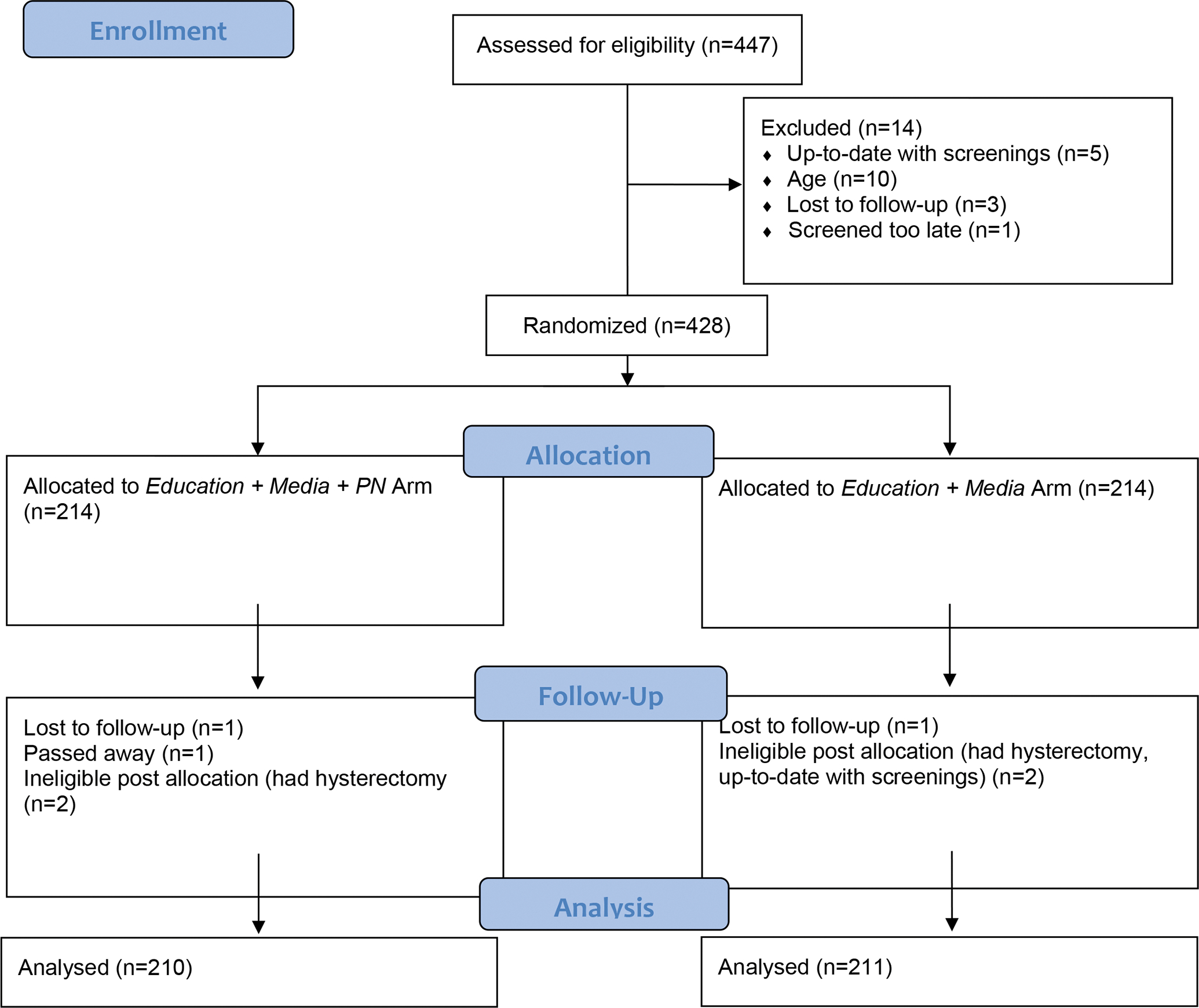
MARHABA Study CONSORT Diagram
Dependent variables.
Primary outcomes included up-to-date screenings for mammogram and Pap test. In the baseline and follow-up surveys, individuals self-reported whether they had ever received the screening tests and the date of their most recent screening test. If an individual had received a mammogram in the past two years, they were considered up-to-date for a mammogram, and if an individual had received a Pap test in the past three years, they were considered up-to-date for a Pap test. Individuals having received a hysterectomy were not included in the Pap test analysis.
Socio-demographics.
Socio-demographic variables included age, ethnicity (South Asian, Middle Eastern, and other, which included Southeast Asian and African), nativity, total years lived in the US, education (less than high school, high school graduate/some college, and college graduate), employment status (employed vs. unemployed), and marital status (married/living with a partner vs. widowed/divorced).
Health care access and preferences.
Variables included insurance status at baseline (private, public, and uninsured) and questions regarding medical care (asked at baseline and follow-up): “Do you have a healthcare provider who speaks in a language in which you can comfortably communicate,” “I prefer to receive medical care from a doctor or healthcare provider of my own race, ethnic, or religious group,” and “I prefer to receive medical care from a doctor or healthcare provider who is female.”
Scale variables.
The Perceived Ethnic Discrimination Questionnaire - Community Version (PEDQ-CV) was used to measure perceived discrimination (previously validated in a multiethnic Asian sample, which included Muslim individuals) [18]. Four subscales assessed the following types of discrimination: Stigmatization, Social Exclusion/Rejection, Threat/Aggression, and Discrimination at the Workplace. The mean of the total responses for each subscale was calculated for a measure of 1–5, with 5 representing the greatest discrimination. Religious discrimination was modified from the Everyday Discrimination Scale [19]. The mean of the total responses was calculated for a measure of 1–5, with 5 representing the greatest religious discrimination. The Spiritual Health Locus of Control scale sought to measure control over health with connection to spirituality [20]. Four subscales assessed the following areas: Spiritual/Life Faith, Active/Spiritual, God’s Grace, and Passive Spiritual. The mean of the total responses for each subscale was calculated for a measure of 1–5, with 5 representing the highest faith. Islamic modesty was modified from earlier versions of the Islamic Modesty Scale [3]. The mean of the responses was calculated for a measure of 1–5, with 5 representing the greatest modesty. Breast and cervical cancer knowledge questions were adapted from training materials; responses were coded as 1 (true) and 0 (false); breast cancer included five questions and was scored from 0 to 5, and cervical cancer included six questions and was scored from 0 to 6. All questions were asked at baseline and follow-up, and are detailed in Appendix Table 1.
Data Analysis.
Descriptive statistics present socio-demographic characteristics and outcome variables overall and by study arm. Means and standard deviations (SDs) are reported for continuous variables, and frequencies are reported for categorical variables; chi-square tests were performed for categorical variables, and t-tests were performed for continuous variables. Bivariate analyses compared screening outcomes at follow-up by baseline characteristics, stratified by study arm, to inform the logistic regression models.
Logistic generalized estimating equation (GEE) models using proc genmod were constructed to predict timely receipt of a mammogram and timely receipt of a Pap test in the Education + Media + PN arm vs. the Education + Media arm, while adjusting for time-point, socio-demographic and health access variables, breast or cervical cancer knowledge, and scale variables found to be associated with outcomes using p<0.20 in a bivariate analysis. The same models were constructed for receipt of a screening test or scheduled screenings tests during the follow-up period. All models were constructed for the entire sample, as well as, the subset using recommended age per USPSTF guidelines (age 50–74, for mammogram and age 40–65, for Pap test). Continuous GEE models using proc genmod were also constructed for change in breast and cervical cancer knowledge, and the intervention effect (the interaction between study arm and time-point) is presented. Knowledge was run for the entire sample, regardless of age or hysterectomy status. All analyses were conducted using SAS version 9.4.
Results
Table 1 presents baseline characteristics of the total analytic sample and by study arm. Mean age was 54.0 (SD=9.1). The majority (99.5%) were born outside the US. Ethnicity was predominantly South Asian (62.1%), followed by Middle Eastern (32.6%), Southeast Asian (4.8%), and African (0.5%). The majority (60.6%) had less than a high school education, spoke English not well or not at all (73.3%), and were insured (93.5%); of those insured, 89.4% had public insurance. PECD-CV subscales, religious discrimination, and cancer screening knowledge were low, while Islamic modesty was high. English fluency differed significantly by study arm; 77.9% of the Education + Media + PN arm spoke English not well or not at all (77.6%) compared to 68.9% in the Education + Media arm.
Table 1.
Baseline characteristics of randomized MARHABA participants, n=421
| Total (n=421) | Education + Media + PN Arm (n=210) | Education + Media Arm (n=211) | p-value | |
|---|---|---|---|---|
| Socio-demographics | ||||
| Age, mean (SD), y | 54.0 (9.1) | 53.8 (9.1) | 54.1 (9.1) | 0.760 |
| Born in the US | 2 (0.5) | 0 (0.0) | 2 (0.5) | 0.499 |
| Time lived in US, mean (SD), y | 11.6 (8.4) | 11.0 (8.2) | 12.1 (8.6) | 0.179 |
| Ethnicity | 0.478 | |||
| South Asian | 62.1 | 61.4 | 62.8 | |
| Middle Eastern | 32.6 | 34.3 | 31.0 | |
| Southeast Asian | 4.8 | 4.3 | 5.2 | |
| African | 0.5 | 0.0 | 1.0 | |
| Married/Living with partner, % | 85.9 | 85.7 | 86.1 | 0.904 |
| Education level, % | 0.117 | |||
| Less than high school | 60.6 | 63.5 | 57.8 | |
| High school/Some college | 23.7 | 24.5 | 22.8 | |
| College graduate | 15.7 | 12.0 | 19.4 | |
| Employed, % | 13.5 | 13.2 | 13.7 | 0.900 |
| Speaks English not well/not at all | 73.2 | 77.6 | 68.9 | 0.048 |
| Health care access and preferences | ||||
| Health Insurance | 0.962 | |||
| Private/Work or company | 4.1 | 3.9 | 4.3 | |
| Public (Medicare, Medicaid, or other) | 89.4 | 89.8 | 89.0 | |
| No health insurance | 6.5 | 6.3 | 6.7 | |
| Has a health provider speaking a comfortable language | 85.3 | 84.1 | 86.5 | 0.501 |
| Prefers to receive medical care from provider of own race, ethnic, or religious group | 62.1 | 60.7 | 63.6 | 0.727 |
| Prefers to receive medical care from a female provider | 75.2 | 76.7 | 73.7 | 0.587 |
| PECD-CV Scales, mean (SD) | ||||
| Stigmatization | 1.09 (0.31) | 1.09 (0.32) | 1.09 (0.30) | 0.780 |
| Exclusion/Rejection | 1.24 (0.44) | 1.24 (0.45) | 1.25 (0.44 | 0.926 |
| Threat | 1.06 (0.30) | 1.06 (0.35) | 1.05 (0.24) | 0.772 |
| Workplace | 1.20 (0.41) | 1.21 (0.41) | 1.19 (0.41) | 0.812 |
| Religious Discrimination, mean (SD) | 1.02 (0.28) | 1.04 (0.25) | 1.01 (0.31) | 0.426 |
| Spiritual Health Locus, mean (SD) | ||||
| Spiritual Life/Faith | 4.08 (0.92) | 4.06 (0.92) | 4.09 (0.92) | 0.737 |
| Active Spiritual | 4.41 (0.79) | 4.39 (0.82) | 4.43 (0.77) | 0.632 |
| God’s Grace | 4.41 (0.73) | 4.36 (0.80) | 4.46 (0.67) | 0.188 |
| Passive Spiritual | 2.75 (1.47) | 2.70 (1.46) | 2.80 (1.49) | 0.519 |
| Islamic Modesty, mean (SD) | 4.01 (0.73) | 4.02 (0.73) | 4.00 (0.73) | 0.725 |
| Breast cancer knowledge, mean (SD) | 2.49 (1.65) | 2.45 (1.68) | 2.53 (1.63) | 0.636 |
| Cervical cancer knowledge, mean (SD) | 2.28 (1.96) | 2.21 (1.95) | 2.35 (1.97) | 0.440 |
SD, standard deviation; US, United States
Navigation encounters by the LHWs were collected for 180 of the women (86%) in the Education + Media + PN arm. Mean encounters was 2.7, ranging from 1 to 5. Navigation encounters took place by phone or in person. Participants informed the LHW of scheduled and completed screening appointments, as well as, difficulties in making the appointments. LHWs would further explain the screening exams, further motivate the participants to be screened, and help to make appointments for participants if that assistance was requested.
Most women were not up-to-date with a mammogram at baseline (84.0% of the Education + Media + PN arm and 85.3% of the Education + Media arm). Among individuals in the Education + Media + PN arm who were not up-to-date with a mammogram at baseline (n=173), 54.9% had scheduled an appointment and 40.5% had received a mammogram by the 4-month follow-up. Among individuals in the Education + Media arm who were not up-to-date with a mammogram at baseline (n=175), 48.6% had scheduled a mammogram appointment and 36.8% had received a mammogram by the 4-month follow-up. Similarly, most women were not up-to-date with a Pap test at baseline (83.1% of the Education + Media + PN arm and 82.7% of the Education + Media arm). Among individuals in the Education + Media + PN arm who were not up-to-date with a Pap test at baseline (n=167), 38.9% had scheduled an appointment for and 30.1% had received a Pap test by the 4-month follow-up. Among individuals in the Education + Media arm who were not up-to-date with a Pap test at baseline (n=170), 33.5% had scheduled an appointment for and 25.9% had received a Pap test by the 4-month follow-up.
Mammogram screening increased significantly in both arms between baseline and the 4-month follow-up (Education + Media + PN: 16.0% to 49.0%; Education + Media: 14.7% to 44.6%. The fully adjusted odds of an up-to-date mammogram (including intervention arm, timepoint, age, ethnicity, education, marital status, English proficiency, insurance, provider speaking comfortable language, stigmatization, exclusion/rejection, passive spiritual, God’s Grace, and breast cancer knowledge) for the Education + Media + PN arm was 1.32 times the odds of the Education + Media arm (95% CI=0.86, 2.02). Subset by age (50–74), the fully adjusted odds of an up-to-date mammogram for the Education + Media + PN arm was 1.42 times the odds of the Education + Media arm (95% CI=0.81, 2.48). At the 4-month follow-up, the rate of up-to-date mammogram screening or scheduled mammogram was 62.1% in the Education + Media + PN arm compared to 56.9% in the Education + Media arm. Models for an up-to-date mammogram or a scheduled mammogram found no significant group differences. (See Table 2, GEE model results are not presented).
Table 2.
Changes in breast and cervical cancer screening and knowledge between baseline and 4-month follow-up, n=421
| Education + Media + PN Arm, n=210 | Education + Media Arm, n=211 | |||||
|---|---|---|---|---|---|---|
| Baseline, n (%) | 4-month, n (%) | p-value | Baseline, n (%) | 4-month, n (%) | p-value | |
| Mammogram Screening Uptake | ||||||
| Mammogram <2 years (age 40–75)) | 33 (16.0) | 101 (49.0) | <0.001 | 30 (14.7) | 91 (44.6) | <0.001 |
| Mammogram <2 years (age 50–74) | 26 (19.6) | 70 (52.6) | <0.001 | 20 (16.1) | 58 (46.8) | <0.001 |
| Mammogram <2 years or scheduled (age 40–75) | 33 (16.0) | 128 (62.1) | <0.001 | 30 (14.7) | 116 (56.9) | <0.001 |
| Mammogram <2 years or scheduled (age 50–74) | 26 (19.6) | 85 (63.9) | <0.001 | 20 (16.1) | 74 (59.7) | <0.001 |
| Pap Test Screening Uptake a | ||||||
| Pap test <3 years (age 40–75) | 32 (16.9) | 80 (42.3) | <0.001 | 34 (17.3) | 73 (37.1) | <0.001 |
| Pap test <3 years (age 40–65) | 28 (17.0) | 71 (43.0) | <0.001 | 31 (18.7) | 67 (40.4) | <0.001 |
| Pap test <3 years or scheduled (age 40–75) | 32 (16.9) | 95 (50.3) | <0.001 | 34 (17.3) | 84 (42.6) | <0.001 |
| Pap test <3 years or scheduled (age 40–65) | 28 (17.0) | 83 (50.3) | <0.001 | 31 (18.7) | 77 (46.4) | <0.001 |
| Cancer Knowledge | ||||||
| Breast cancer, mean (SD) | 2.5 (1.7) | 4.2 (0.9) | <0.001 | 2.6 (1.6) | 4.1 (0.9) | <0.001 |
| Cervical cancer, mean (SD) | 2.2 (1.9) | 4.6 (1.8) | <0.001 | 2.4 (2.0) | 4.5 (1.8) | <0.001 |
Denominator does not include women who have received a hysterectomy.
Pap test screening increased significantly in both arms between baseline and the 4-month follow-up (Education + Media + PN: 16.9% to 42.3%; Education + Media: 17.3% to 37.1%). The fully adjusted odds of an up-to-date Pap test (including arm, timepoint, age, ethnicity, education, marital status, English proficiency, insurance, provider speaking comfortable language, exclusion/rejection, threat/aggression, passive spiritual, spiritual life, religious discrimination, Islamic modesty, and cervical cancer knowledge) for the Education + Media + PN arm was 1.11 times the odds of the Education + Media arm (95% CI=0.72, 1.71). Subset by age (40–65), the fully adjusted odds of an up-to-date Pap test in the Education +Media + PN arm was 1.07 times the odds of the E Education + media arm (95% CI=0.68, 1.68). At 4-month follow-up, the rate of up-to-date Pap test or scheduled Pap test was 50.3% in the Education + Media + PN arm compared to 42.6% in the Education + Media arm. Models for an up-to-date Pap test or a scheduled Pap test found no significant group differences. (See Table 2, GEE model results are not presented).
Breast and cervical cancer knowledge increased significantly in both arms between baseline and 4-months, and there were no significant between group differences once placed into the adjusted models (data not presented). Mean breast cancer knowledge increased from 2.5 to 4.2 in the Education + Media + PN arm, and from 2.6 to 4.1 in the Education + Media arm. Mean cervical cancer knowledge increased from 2.2 to 4.6 in the Education + Media + PN arm, and from 2.4 to 4.5 in the Education + Media arm.
Discussion
This study presents the results of a RCT comparing the efficacy of Education + Media + PN vs. Education + Media on breast and cervical cancer screening outcomes among Muslim women living in NYC. Both arms showed a significant increase in breast and cervical cancer screening between baseline and the 4-month follow-up, suggesting that the educational session and small media materials were perhaps sufficient to drive the increase in cancer screening. An intervention study among Korean American women utilizing LHWs, follow-up counseling and navigation has also shown significant increases in cancer screening [21]. Our intervention included a small media component in addition to breast and cervical cancer education, supporting that culturally adapted small media materials may be a powerful strategy to promote behavior change.
Many women in both groups of our intervention had scheduled screenings that had not been performed by the study end. Participants reported long wait times between scheduling and attending appointments, a barrier which has been reported in other studies [22]. In the Education + Media + PN arm, an additional 13.1% had scheduled but not yet received a mammogram, and an additional 8.4% had scheduled but not yet received a Pap test; and among the Education + Media arm, an additional 12.3% had scheduled but not yet received a mammogram, and an additional 6.4% had scheduled but not yet received a Pap test.
Both groups also showed significant improvement in breast and cervical cancer knowledge between baseline and the 4-month follow-up. However, these changes were not significantly different across intervention arms, once placed into adjusted models. This gain in knowledge among both groups is not surprising, as all women received the culturally and linguistically adapted small media materials related to breast and cervical cancer knowledge. Previous studies have also shown increases in knowledge related to cancer and cancer screening among Muslim American and Asian American women after attendance at educational sessions [23, 24].
Our study has a few limitations that merit noting. First, mammogram and Pap screening status was based on self-report, and medical records were not used. This reporting approach may have biased our screening rates. Future research should strive to ascertain cancer screening outcomes using objective measures (e.g., reviewing medical records) to avoid possible self-reporting bias. Second, the 4-month follow-up period may not have been long enough to fully capture screening behavior, as many women reported having scheduled a screening, but their appointment was more than 4 months away. This lengthy wait period would lead to a potential underestimation of our primary outcome. Third, the Education + Media + PN arm had lower education levels at baseline compared to the Education + Media arm. However, the Education + Media + PN arm showed significant positive changes in cancer screening behaviors and knowledge at follow-up. Fourth, our sample was largely South Asian and Middle Eastern, thus may not be representative of the Muslim population at large, which includes a large proportion of African women. Fifth, the majority of our sample was insured, although the majority of those insured had public insurance. Research has suggested that uninsured individuals and those insured with Medicaid have worse cancer screening outcomes compared to those with private insurance or Medicare [25]. Sixth, the follow-up survey was conducted by LHWs involved in the intervention delivery, which may have increased social desirability bias in both groups. Finally, because we followed USPSTF guidelines, certain age groups in our sample were advised to discuss age screening guidelines with a doctor (40–49 for mammogram and 66–74 for Pap screening).
Our findings have implications for the development of future breast and cervical cancer screening programs among limited English-proficient, immigrant Muslim women. As positive changes in cancer screening were shown in both arms, it is likely that the educational session and small media materials that included culturally tailored information on how and where to access low-cost cancer screening services had an influence on many women before the receipt of LHW navigation. It is also important to note that our social marketing-informed small media approach was guided by our partnership with multiple community partners and our extensive formative work in the community. For example, qualitative interviews we conducted with community members highlighted healthcare barriers to cancer screening access. We specifically addressed these barriers in the intervention through tips and resources on how to navigate the healthcare system.
Overall, our project experience supports that integrating CBPR with social marketing approaches is a promising strategy to promote breast and cervical cancer screening in Muslim American communities. The small media materials were created in partnership with a multicultural advertising company and guided by input from our community partners; thus, special consideration was taken on the cultural and linguistic aspects of the media materials. The potential replicability for other immigrant groups merits exploration.
Conclusions
This study found a significant increase in breast and cervical cancer screening uptake in both study arms, demonstrating that a community-partnered approach to develop and offer an educational session with culturally-informed small media materials may have the ability to promote breast and cervical cancer screening among a hard-to-reach, low literacy community population.
Supplementary Material
Acknowledgments
The authors would like to thank the members of the MARHABA Coalition for their support and guidance. This study would not have been possible without the support our LHWs. The authors are especially grateful to all community members who participated in the study, including Women Conquering Cancer, Women in Islam, Turning Point, Adhunika, and Council of African Imams.
Funding
This study was supported by a Centers for Disease Control and Prevention (CDC) Special Interest Projects Competitive Supplement from the Cooperative Agreement 148DP001904–01 and U58DP005621; the National Institute on Minority Health and Health Disparities (NIMHD) U54MD000538; and the National Cancer Institute P30CA16087. The findings and conclusions are those of the authors and do not necessarily represent the official position of the CDC.
Footnotes
Conflicts of interest
The authors declare no conflicts of interest.
Contributor Information
Laura C. Wyatt, NYU Langone Health, Department of Population Health, New York, NY 10016, United States.
Perla Chebli, NYU Langone Health, Department of Population Health, New York, NY 10016, United States.
Shilpa Patel, Center for Health Care Strategies, Trenton, NJ 08619, United States.
Gulnahar Alam, NYU Langone Health, Department of Population Health, New York, NY 10016, United States.
Areeg Naeem, School of Dental Medicine, University at Buffalo, Buffalo, NY 14214.
Annette E. Maxwell, UCLA Fielding School of Public Health, Los Angeles, CA 90095.
Victoria H. Raveis, NYU College of Dentistry, New York, NY 10016, United States.
Joseph Ravenell, NYU Langone Health, Department of Population Health, New York, NY 10016, United States.
Simona C. Kwon, NYU Langone Health, Department of Population Health, New York, NY 10016, United States.
Nadia S. Islam, NYU Langone Health, Department of Population Health, New York, NY 10016, United States.
References
- 1.Pew Research Center, U.S. Muslims Concerned About Their Place in Society, but Continue to Believe in the American Dream.
- 2.New York Foundation. New York’s Diverse Muslim Community. December 18, 2020]; Available from: https://nyf.org/files/2019/08/NYF_Muslim_A.pdf. [Google Scholar]
- 3.Padela AI, Murrar S, Adviento B, Liao CH, Hosseinian Z, Peek M, and Curlin F, Associations Between Religion-Related Factors and Breast Cancer Screening Among American Muslims. Journal of Immigrant and Minority Health, 2015. 17(3): p. 660–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zorogastua K, Sriphanlop P, Reich A, Aly S, Cisse A, and Jandorf L, Breast and Cervical Cancer Screening among US and non US Born African American Muslim Women in New York City. Aims Public Health, 2017. 4(1): p. 78–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Padela AI, Gunter K, Killawi A, and Heisler M, Religious Values and Healthcare Accommodations: Voices from the American Muslim Community. Journal of General Internal Medicine, 2012. 27(6): p. 708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islam N, Patel S, Brooks-Griffin Q, Kemp P, Raveis V, Riley L, . . . Kwon S, Understanding Barriers and Facilitators to Breast and Cervical Cancer Screening among Muslim Women in New York City: Perspectives from Key Informants. SM J Community Med, 2017. 3(1). [PMC free article] [PubMed] [Google Scholar]
- 7.Guimond ME and Salman K, Modesty matters: cultural sensitivity and cervical cancer prevention in muslim women in the United States. Nurs Womens Health, 2013. 17(3): p. 210–6; quiz 217. [DOI] [PubMed] [Google Scholar]
- 8.Shah SM, Ayash C, Pharaon NA, and Gany FM, Arab American immigrants in New York: health care and cancer knowledge, attitudes, and beliefs. J Immigr Minor Health, 2008. 10(5): p. 429–36. [DOI] [PubMed] [Google Scholar]
- 9.Foundation CHC Allies for Quality: Lay Health Workers’ Role in Improving Health Care Quality. November 2003; Available from: https://www.chcf.org/wp-content/uploads/2017/12/PDF-AlliesForQualityBrief2.pdf.
- 10.Lu M, Moritz S, Lorenzetti D, Sykes L, Straus S, and Quan H, A systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women. BMC Public Health, 2012. 12: p. 413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall CP, Wimberley PD, Hall JD, Pfriemer JT, Hubbard E, Stacy AS, and Gilbert JD, Teaching breast cancer screening to African American women in the Arkansas Mississippi river delta. Oncol Nurs Forum, 2005. 32(4): p. 857–63. [DOI] [PubMed] [Google Scholar]
- 12.Padela AI, Malik S, Ally SA, Quinn M, Hall S, and Peek M, Reducing Muslim Mammography Disparities: Outcomes From a Religiously Tailored Mosque-Based Intervention. Health Educ Behav, 2018. 45(6): p. 1025–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pratt R, Mohamed S, Dirie W, Ahmed N, Lee S, VanKeulen M, and Carlson S, Testing a Religiously Tailored Intervention with Somali American Muslim Women and Somali American Imams to Increase Participation in Breast and Cervical Cancer Screening. J Immigr Minor Health, 2020. 22(1): p. 87–95. [DOI] [PubMed] [Google Scholar]
- 14.Islam N and Patel S, Best Practices for Partnering with Ethnic Minority-Serving Religious Organizations on Health Promotion and Prevention. AMA J Ethics, 2018. 20(7): p. E643–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Preventive Services Task Force. A & B Recommendations. 2021. January 24, 2022]; Available from: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-and-b-recommendations.
- 16.Noor S, Noor N, and Haq M, Breast Cancer in Muslim Countries: Risk Reduction Strategies. Journal in Advances in Medicine and Medical Research, 2016: p. 1–11. [Google Scholar]
- 17.Lefebvre RC and Flora JA, Social marketing and public health intervention. Health Educ Q, 1988. 15(3): p. 299–315. [DOI] [PubMed] [Google Scholar]
- 18.Kwok J, Atencio J, Ullah J, Crupi R, Chen D, Roth AR, . . . Brondolo E, The perceived ethnic discrimination questionnaire--community version: validation in a multiethnic Asian sample. Cultur Divers Ethnic Minor Psychol, 2011. 17(3): p. 271–82. [DOI] [PubMed] [Google Scholar]
- 19.Reeve BB, Willis G, Shariff-Marco SN, Breen N, Williams DR, Gee GC, . . . Levin KY, Comparing Cognitive Interviewing and Psychometric Methods to Evaluate a Racial/Ethnic Discrimination Scale. Field methods, 2011. 23(4): p. 397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holt CL, Clark EM, and Klem PR, Expansion and validation of the spiritual health locus of control scale: factorial analysis and predictive validity. J Health Psychol, 2007. 12(4): p. 597–612. [DOI] [PubMed] [Google Scholar]
- 21.Han HR, Song Y, Kim M, Hedlin HK, Kim K, Ben Lee H, and Roter D, Breast and Cervical Cancer Screening Literacy Among Korean American Women: A Community Health Worker-Led Intervention. Am J Public Health, 2017. 107(1): p. 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karliner LS, Kaplan C, Livaudais-Toman J, and Kerlikowske K, Mammography facilities serving vulnerable women have longer follow-up times. Health Serv Res, 2019. 54 Suppl 1: p. 226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmad F, Cameron JI, and Stewart DE, A tailored intervention to promote breast cancer screening among South Asian immigrant women. Soc Sci Med, 2005. 60(3): p. 575–86. [DOI] [PubMed] [Google Scholar]
- 24.Padela AI, Malik S, Din H, Hall S, and Quinn M, Changing Mammography-Related Beliefs Among American Muslim Women: Findings from a Religiously-Tailored Mosque-Based Intervention. J Immigr Minor Health, 2019. 21(6): p. 1325–1333. [DOI] [PubMed] [Google Scholar]
- 25.Marlow NM, Pavluckm AL, Bian J, Ward EM, and Halpern MT, The Relationship Between Insurance Coverage and Cancer Care: A Literature Synthesis. May 2009, RTI Press. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


