Abstract
Background
Ankle sprains remain prevalent across most team sports. However, despite divergent ankle sprain injury rates in male and female athletes, little is known about potential sex-specific risk factors for ankle sprain.
Objective
To systematically investigate the sex-specific risk factors for ankle sprain.
Methods
Combinations of the key terms were entered into PubMed, Web of Science, Embase and Cochrane Library databases, and prospective studies reporting ankle sprain risk factors in males or females were included for meta-analysis.
Results
Sixteen studies were eligible for inclusion, for a total of 3636 athletes (735 female) and 576 ankle sprains (117 female). Out of 21 prognostic factors, previous ankle sprain injury (odds ratio = 2.74, P < .001), higher body mass index (SMD = 0.50, P < 0.001), higher weight (SMD = 0.24, P = 0.02), lower isometric hip abduction strength (SMD = − 0.52, P < 0.0001) and lower dynamic balance performance (SMD = − 0.48 to − 0.22, P < 0.001–0.04) were identified as risk factors in male athletes. In female athletes, out of 18 factors eligible for meta-analysis, only lower concentric dorsiflexion strength was identified as a risk factor (SMD = − 0.48, P = 0.005).
Conclusion
This meta-analysis provides novel evidence for different risk factor profiles for ankle sprain injuries between female and male athletes. Further studies, particularly in female athletes, are needed to strengthen the evidence.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40798-022-00530-y.
Keywords: Injury, Prognostic, Sex-specific, Women, Men, Sport, Strength, Balance
Key Points
Risk factors for ankle sprain in male athletes include a previous ankle sprain, higher weight and body mass index, poor dynamic balance performance and lower hip strength.
Lower specific ankle strength was the only risk factor identified for ankle sprains in female athletes.
There are different risk factors for ankle sprain in males and females, but a shortage of data specifically in female athletes prevents stronger conclusions from being drawn.
Introduction
Ankle sprains are prevalent across a broad range of sports, accounting for up to 22.6% of all injuries in American collegiate and high school athletes [1, 2]. Incidence rates are particularly high in sports which involve large volumes of running, change of direction and jumping/landing [3, 4], evidenced by just over one quarter of National Basketball Association players sustaining an ankle sprain each season [5]. This high prevalence is exacerbated by the frequency of reinjury following an initial ankle sprain, with studies observing that up to 47% of injuries were recurrent [6].
Due to their prominence in the sports injury landscape and the tendency for ongoing complications post-injury [7, 8], the prevention of ankle sprains is paramount. While external interventions such as ankle braces have proven both convenient and effective [9, 10], the characterisation of intrinsic risk factors predisposing an athlete to injury forms a critical stage of the injury prevention process and ultimately empowers practitioners to develop targeted strategies to reduce injury risk which may also benefit long-term athletic development [11–14]. Aside from the widely reported higher injury risk associated with a previous ankle sprain [15–18], deficits in muscular strength, proprioception, dynamic balance performance and co-ordination, as well as higher or lower body mass index (BMI) have all been reported to heighten the risk of sustaining an ankle sprain [10, 17, 19–21].
Biological sex is also considered a risk factor for ankle sprain. Although there are reports of comparable incidence rates between males and females [22], a 2014 systematic review concluded that females suffer from ankle sprains at higher rates than their male counterparts [23], which aligns with recent evidence indicating sex-specific general injury patterns in team sports [24] and running [25]. Sex-based differences in factors such as joint laxity and sensorimotor control may contribute to this injury rate discrepancy [26, 27], and there is early evidence that ankle sprain injury history influences future ankle sprain risk in males but not females [15]. However, very few studies have directly compared ankle sprain risk factors between sexes, and aggregated data approaches obscure potential sex-based differences. This uncertainty regarding the extent to which the risk factors for ankle sprain differ between males and females may inhibit the development of more targeted and effective strategies to mitigate injury risk. Therefore, the objective of this study was to generate a summary from the available evidence through a meta-analysis identifying the intrinsic risk factors for ankle sprain in male and female athletes.
Methods
This systematic review and meta-analysis were conducted in accordance with the PRISMA guidelines for reporting systematic reviews and meta-analyses [28].
Search Strategy
One investigator (JM) conducted a systematic literature search of articles published between January 2000 and September 2021 using PubMed, Web of Science, Embase and Cochrane Library databases. For these, the terms “ankle sprain” OR “ankle injury” were combined (AND) with “risk*” OR “predict*”. All identified article titles and abstracts were then exported to Rayyan [29]. Within Rayyan, two authors (JM and AZ) screened articles for eligibility firstly according to title and abstract and the remaining articles had their full text screened. The bibliographical information of included articles was also examined for further relevant articles.
Eligibility Criteria
At the title and abstract screening stage, publications were considered relevant if they (1) included a prospective design, (2) demonstrated visible documentation of ankle injury, (3) included reporting of at least one risk factor or prognostic factor and (4) were published in an English peer-reviewed journal. Studies were excluded if they were related to other types of injury rather than ankle sprain, if they were reviews, if they clearly included populations that were not involved in structured sport participation, or if they did not investigate risk factors. During title and abstract screening, if insufficient information was available to determine study eligibility, the study was passed through to the full-text screening stage for further inspection.
The eligibility criteria used at the full-text screening stage were similar. Articles were screened for inclusion based on the following criteria: (1) prospective cohort design, (2) included ankle sprain injury data, (3) reported at least one potential internal risk factor for ankle sprain injury, (4) reported specific and separate data for male or female athletes (or both separately), (5) published in the English language, (6) publication in a peer-reviewed journal, (7) reporting of data specifically on ankle sprains rather than general ankle injury or general injury, (8) included participants involved in structured sport participation. Ankle sprain injuries were defined as injuries prohibiting an athlete from full participation in training for a minimum of one day. Studies which included active participants who were not necessarily involved in structured sport (for example, those in military populations), retrospective studies, studies which used an intervention, studies which did not provide data for males and/or females separately and studies which did not provide separate data for injured and uninjured groups were ruled ineligible for inclusion. In the event of conflict between the two reviewers regarding eligibility of articles, a third reviewer (CK) was utilised to form a majority decision.
Data Extraction
Study characteristics such as sex, observation period, sport type, level of play and sample size were extracted. The number of ankle sprain injuries and the rate of injuries per season were extracted (outcome measurements), as well as the potential risk factors (prognostic measurements). The prognostic measurements were included with mean and standard deviation. For studies that reported the mean and standard error, this was converted to standard deviation. Dichotomous variables were included using the raw data. Units reported in anything but metric units were subsequently converted to metric units to allow meta-analysis. All data extraction was completed by one author (CK).
Study Quality and Risk of Bias Assessment
The risk of bias assessment was undertaken by two reviewers separately (CK and JM) using a modified version of the “Quality in Prognosis Studies” (QUIPS) tool [30, 31]. The QUIPS uses six different categories to measure the risk of bias. The category “study participation” is used to assess the risk of selection bias. For this purpose, 5 questions are asked which must be answered with either yes or no. “Study attrition”, “prognostic outcome measurement”, “outcome measurement”, “study confounding” and “statistical analysis and reporting” form the remaining 5 categories. Here also several questions are asked, which must be answered with yes or no. To fulfill a low risk in a category, at least 75% of the questions must be answered with yes. To be rated as a low-risk study, at least 5 low-risk categories must be achieved. The “outcome measurement” category also has a special role. Since this category has only three questions, all of them must be answered with yes and to be marked as a low-risk study, this category must be fulfilled. The QUIPS has been previously described [30, 31] and was also used by previous risk factor reviews [32–35].
Statistical Analysis
The meta-analysis was performed using Review Manager (version 5.4.1) [36] and included all risk factors with more than one study in females and males. Continuous data of the prognostic measurements were converted into standardised mean differences (SMD) and 95% confidence intervals, with the SMD reflecting the magnitude of the difference between injured and uninjured athletes. For dichotomous variables, the raw data were analysed with the method of Mantel–Haenszel, and the effect measure was reported as odds ratio and 95% confidence intervals. Data were pooled between studies using a random effects model [37] and summarised in a forest plot. This was chosen because it more conservatively estimates effect sizes and mitigates potential methodological differences and statistical heterogeneity. Z statistics and P-values were calculated to assess if the effect was statistically significant. Statistical significance was set at P ≤ 0.05. Heterogeneity was assessed using the I2 statistics, with a higher value indicating a higher heterogeneity [38].
Results
Search Results
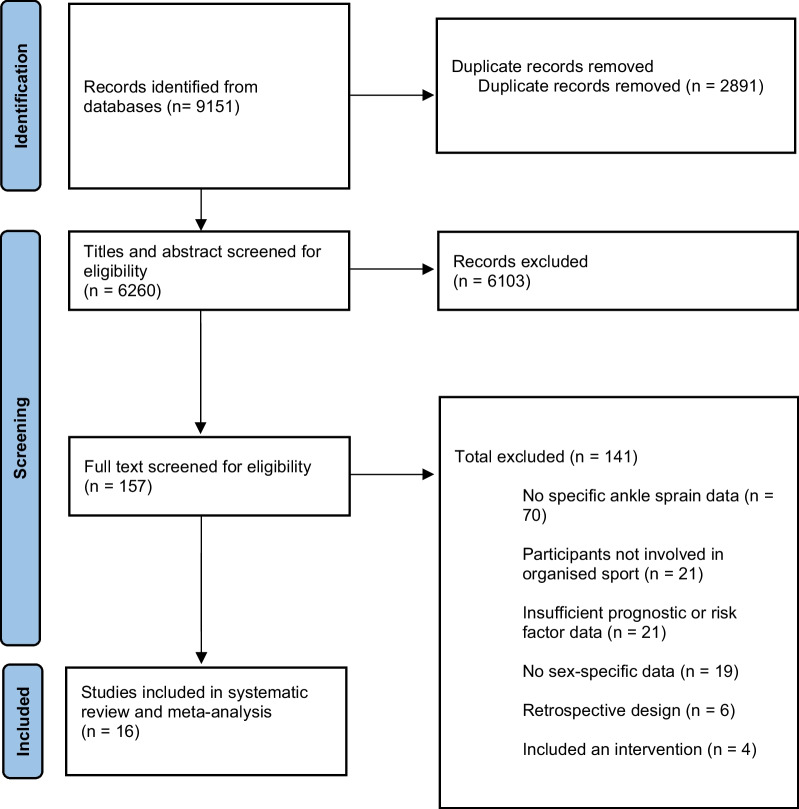
The systematic search yielded 9151 articles. After removal of duplicates, 6260 articles remained. A total of 157 articles were included for full-text analysis after selection of titles and abstracts. Of these 157, 70 were excluded due to a lack of specific ankle sprain injury data, 21 were removed due to their participants not being involved in organised sport, 21 were excluded for insufficient prognostic or risk factor data, 19 were removed due to not providing sex-specific data, 6 were excluded due to a retrospective design and 4 were eliminated due to using an intervention, leading to an overall exclusion of 141 manuscripts at this stage of screening. Therefore 16 articles were ultimately able to satisfy the inclusion criteria of the meta-analysis (Fig. 1) [16–21, 39–48]. These included studies were published between 2001 and 2021.
Fig. 1.
PRISMA flow diagram of the identification and selection of the studies included in this meta-analysis. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Description of the Included Studies
Table 1 provides details of the included studies. The eligible studies captured 576 ankle sprains (male 459, female 117) in a pool of 3636 athletes (male 2901, female 735). A total of 2079 of these athletes participated at an amateur level of sport (57.2%), 745 at a subelite level (20.5%) and 812 on an elite level (22.3%), as self-described by the studies. The rate of ankle sprains per season was similar in males (11.5%) and females (11.4%).
Table 1.
Descriptions of included studies
| Study | Sex | Sample | Level | Ankle sprains | Prognostic measurements | Length of tracking |
|---|---|---|---|---|---|---|
| Attenborough et al. 2017 [39] | Female | 94 netball players | Subelite, amateur | 11 | Age, Height, Weight, Injury history, SEBT (dynamic balance), CMJ, inversion–eversion (ankle joint laxity), CAIT-Y (joint instability), demi- pointe test (static balance), foot lift test (static balance), level of play | 1 season |
| Beynnon et al. 2001[40] | Female and male | 68 female and 50 male college athletes from various sports | Subelite |
f: 13 m: 7 |
Weight, Height, Dorsiflexion ROM, anterior drawer (ankle joint laxity), concentric strength (plantarflexion, dorsiflexion, inversion, eversion), eccentric strength(plantarflexion, dorsiflexion, inversion, eversion)leg dominance, modified Beighton method (generalszed joint laxity), anatomic foot type, inversion ROM (unweighted), eversion ROM (unweighted), rearfoot varus/valgus ROM (unweighted), forefoot/rearfoot relationship, Dorsiflexion ROM (knee extended, weightbearing), calcaneus varus/valgus (weightbearing), tibial varus valgus (weightbearing), concentric and eccentric ratio (dorsiflexion/plantarflexion, eversion/inversion), A-P centre of gravity sway (static balance) | 2 seasons |
| DeRidder et al. 2016 [41] | Male | 133 youth soccer players | Subelite | 12 | Age, BMI, isometric strength (hip flexion, extension, abduction, adduction, external rotation, internal rotation), playing experience, leg dominance, adjusted body size, exposure | 3 seasons |
| Engebretsen et al. 2010 [42] | Male | 508 professional soccer players | Elite | 43 | Age, Weight, Height, BMI, Injury history, anterior drawer (ankle joint laxity), Dorsiflexion ROM FAOS function score, single leg balance test (static balance), clinical examination, foot type, standing rearfoot alignment, hallux position, supination ROM, pronation ROM, playing position | 1 season |
| Fousekis et al. 2012 [43] | Male | 100 professional soccer players | Elite | 17 | Age, Weight, Height, BMI, anterior drawer (ankle joint laxity), concentric and eccentric strength (dorsiflexion and plantarflexion) dorsiflexion ROM, plantarflexion ROM, lower limb functional length, tibia length, proprioception (all not included parameters are dichotomous) | 1 season |
| Gribble et al. 2015 [21] | Male | 539 high school and college American football athletes | Amateur | 54 | Age, Weight, Height, BMI, Injury history, SEBT (dynamic balance), modified FMS | 1 season |
| Hartley et al. 2018 [20] | Female and male | 167 female and 384 male collegiate athletes from various sports | Subelite |
f: 21 m: 38 |
BMI, Injury history, YBT (dynamic balance), YBT asymmetry, Dorsiflexion ROM, modified BESS (static balance) | 2 seasons |
| Kawaguchi et al. 2021 [44] | Male | 145 collegiate soccer players | Subelite | 31 | Age, Weight, Height, BMI, Injury history, Dorsiflexion ROM, Playing experience, muscle mass, fat mass, general joint laxity, bilateral balance test (force plate), unilateral balance test (force plate), height of navicular tubercle, knee extension ROM, hip internal rotation ROM, muscle flexibility (Iliopsoas, quadriceps, hamstring, gastrocnemius, soleus), isometric strength (knee extension and flexion, hip abduction) | 1 season |
| Kofotolis et al. 2007 [18] | Male | 312 soccer players | Amateur | 139 | Injury history | 2 seasons |
| Kofotolis et al. 2007 [45] | Female | 204 professional basketball players | Elite | 32 | Injury history | 2 seasons |
| McCann et al. 2018 [46] | Female | 43 collegiate soccer athletes | Subelite | 8 | Weight, Height, BMI, Injury history | 1 season |
| Powers et al. 2017 [19] | Male | 185 youth and adult professional soccer players | Subelite, elite | 25 | Age, Weight, Height, BMI, Injury history, isometric strength (hip abduction) | 1 season |
| Saki et al. 2021 [16] | Male | 152 youth athletes from various sports | Amateur | 34 | Age, Weight, Height, BMI, Injury history, Dorsiflexion ROM, Plantarflexion ROM, navicular drop, Q angle, tibia vara, tibia rotation, knee recurvatum | 2 seasons |
| Tyler et al. 2006 [17] | Male | 152 American football high-school athletes | Amateur | 15 | Injury history, BMI (dichotomous) | 1–3 seasons |
| Willems et al. 2005 [47] | Male | 241 sport students | Amateur | 44 |
Age, Weight, Height, BMI, Dorsiflexion ROM, Plantarflexion ROM, joint position sense, flamingo balance, standing broad jump, shuttle run, endurance shuttle, concentric and eccentric strength (inversion, eversion, plantarflexion, dorsiflexion), Inversion ROM, Eversion ROM, metatarsophalangeal-1-joint flexion ROM, metatarsophalangeal-1-joint extension ROM, hip external rotation ROM, hip internal rotation ROM, calcaneus position subtalar joint in neutral position (weighted, unweighted, and weighted with subtalar joint not in neutral position), postural control (force-plate), muscle reaction time (peroneus longus, peroneus brevis, tibialis anterior, gastrocnemius) |
1 season |
| Willems et al. 2005 [48] | Female | 159 sport students | Amateur | 32 | Age, Weight, Height, BMI, Dorsiflexion ROM, Plantarflexion ROM, joint position sense, concentric and eccentric strength (inversion, eversion, plantarflexion, dorsiflexion), Inversion ROM, Eversion ROM, metatarsophalangeal-1-joint flexion ROM, metatarsophalangeal-1-joint extension ROM, hip external rotation ROM, hip internal rotation ROM, calcaneus position subtalar joint in neutral position (weighted, unweighted, and weighted with subtalar joint not in neutral position), postural control (force-plate) | 1 season |
SEBT Star excursion balance test, CMJ Counter movement jump, CAIT-Y Cumberland ankle instability tool-youth, f Female, M Male, ROM Range of motion, A-P Anterior–posterior, BMI Body mass index, FAOS Foot and ankle outcome score, FMS Functional movement screen, YBT Y-Balance Test, BESS Balance error scoring system, Q angle Quadriceps angle. Bold text denotes outcomes that were eligible for meta-analysis
There were 10 studies investigating males only, 4 investigating females only and two studies investigating both sexes separately. The age range for males was 10–34, whereas the age range for included females was 17–26.
The included male population came from soccer (52.5%), American football (29.4%), multisport (8.69%), volleyball (2.9%), basketball (2.7%), baseball (1.9%), lacrosse (1.5%), tennis (0.3%) and handball (0.2%). The included female population came from basketball (32.5%), multisport (24.9%), soccer (15%), netball (12.8%), field hockey (4.2%), softball (4.1%), volleyball (4.1%) and lacrosse (2.5%).
Six studies reported any ankle sprain [18, 20, 32, 39, 40, 45], six studies reported lateral ankle sprains only [21, 41, 44, 46–48], three studies reported non-contact ankle sprains only [17, 19, 43], and one study investigated non-contact lateral ankle sprains only [16].
For the studies that reported the complete exposure hours, the ankle sprain incidence rates ranged from 0.75 to 1.74 injures per 1000 exposure hours in females and 0.36–2.17 injuries per 1000 exposure hours in males.
Overview of Results of Risk of Bias Assessment (QUIPS)
Risk of bias assessment details is provided in Table 2. In general, a low risk of bias was detected for studies included in this review. Specifically, low risk of bias was found in 11 studies (68.75%) [18–21, 40–46] and high risk of bias in 5 studies (31.25%) [16, 17, 39, 47, 48]. The authors were able to reach complete consensus in the assessment of risk of bias. “Study confounding” was most frequently identified as a potential source of bias (37.5% of all studies), followed by “outcome measurement” (31.25%), “study attrition” (25%) and “study participation” (6.25%). The items “prognostic factor measurement” and “statistical analysis and reporting” were met by all studies.
Table 2.
QUIPS risk of bias assessment for included studies
| Study | Potential risk of bias item | Risk of bias | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Attenborough et al. 2017 [39] | + | + | + | − | − | + | High |
| Beynnon et al. 2001 [40] | + | + | + | + | − | + | Low |
| DeRidder et al. 2016 [41] | + | + | + | + | + | + | Low |
| Engebretsen et al. 2010 [42] | + | + | + | + | + | + | Low |
| Fousekis et al. 2012 [43] | + | + | + | + | + | + | Low |
| Gribble et al. 2016 [21] | + | + | + | + | + | + | Low |
| Hartley et al. 2018 [20] | + | + | + | + | + | + | Low |
| Kawaguchi et al. 2021 [44] | + | + | + | + | + | + | Low |
| Kofotolis et al. 2007 [18] | + | − | + | + | + | + | Low |
| Kofotolis et al. 2007 [45] | + | − | + | + | + | + | Low |
| McCann et al. 2018 [46] | + | + | + | + | − | + | Low |
| Powers et al. 2017 [19] | + | − | + | + | + | + | Low |
| Saki et al. 2021 [16] | + | − | + | − | + | + | High |
| Tyler et al. 2006 [17] | − | + | + | − | − | + | High |
| Willems et al. 2005 [47] | + | + | + | − | − | + | High |
| Willems et al. 2005 [48] | + | + | + | − | − | + | High |
QUIPS Quality in Prognosis Studies. 1: study participation, 2: study attrition, 3: prognostic factor measurement, 4: outcome measurement, 5: study confounding variables, 6: statistical analysis and reporting
Overview of Results from Meta-Analysis
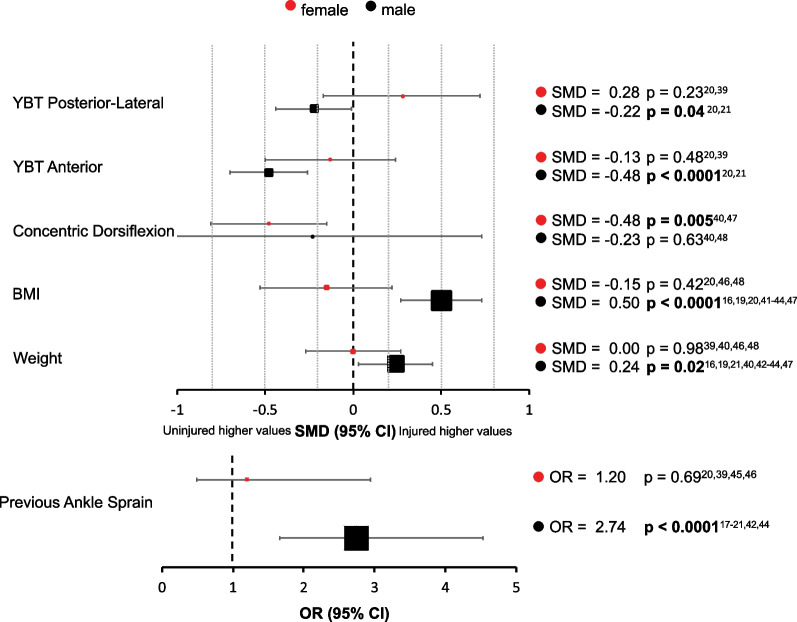
A total of 21 risk factors could be included in the meta-analysis, of which 17 factors allowed sex comparison. Isometric hip abduction, plantarflexion ROM, hip internal rotation and anterior drawer test for ankle could only be analysed for the male population due to an absence of studies in females. Risk factors were subsequently classified into athlete characteristics (including age, height, weight, BMI and ankle sprain injury history), strength, dynamic balance, joint range of motion and joint laxity. For the male population, previous injury, higher BMI and weight, deficient Y-Balance Test (YBT) anterior reach and posterior-lateral reach distance and poor isometric hip abduction strength were identified as risk factors for ankle sprain injury, whereas in the female population, only concentric dorsiflexion strength was shown to be a significant risk factor (Fig. 2). Forest plots for all risk factors are available in Additional file 1.
Fig. 2.
Summary forest plot including variables identified as risk factors for ankle sprain in males and females, with standardised mean difference or odds ratio and 95% confidence intervals. The size of the marker represents the sample size (larger marker = larger subject pool). YBT Y-Balance Test, BMI body mass index, OR odds ratio
Athlete Characteristics
For male athletes, the meta-analysis revealed an association between higher weight (SMD = 0.24, 95% CI 0.03–0.45, P = 0.02, I2 = 56%) [16, 19, 21, 40, 42–44, 47], higher BMI (SMD = 0.50, 95% CI 0.27–0.73, P < 0.0001, I2 = 69%) [16, 19, 21, 40, 42–44, 47], a previously injured ankle (OR = 2.74, 95% CI 1.66–4.53, P < 0.0001, I2 = 72%) [17–21, 42, 44] and the occurrence of an ankle sprain. Age (SMD = 0.19, 95% CI − 0.06–0.43, I2 = 69%) [16–21, 41–44, 47] and height (SMD = − 0.07 95% CI − 0.45–0.32, I2 = 87%) [16, 19, 21, 42–44, 47] were not associated with sustaining an ankle sprain in males. No athlete characteristic risk factor (age[ SMD = − 0.23 95% CI − 0.56 to − 0.10, I2 = 0%] [39, 48], weight [SMD = − 0.00 95% CI − 0.27–0.27, I2 = 0%] [39, 40, 46, 48], height [SMD = 0.14 95% CI − 0.34–0.62, I2 = 51%] [39, 46, 48], BMI [SMD = − 0.15 95% CI − 0.53–0.22, I2 = 39%] [20, 46, 48], previous ankle sprain[OR = 1.20 95% CI 0.49–2.94, I2 = 60%] [20, 35, 39, 46]) had an influence on the occurrence of an ankle sprain in female athletes.
Strength
Reduced concentric dorsiflexion strength in females (SMD = − 0.48, 95% CI − 0.81 to − 0.15, P = 0.005, I2 = 0%) [40, 48] and reduced isometric hip abduction in males (SMD = − 0.52, 95% CI − 0.78 to − 0.26, P < 0.0001, I2 = 0%) [19, 41, 44] were associated with an increased risk of ankle sprain. It should also be noted that no studies investigated the influence of isometric hip abduction strength on ankle sprain incidence in females. The other strength parameters revealed no association with an ankle sprain, either in male (concentric plantarflexion [SMD = − 0.09 95% CI − 0.85–0.67, I2 = 69%] [40, 47], dorsiflexion [SMD = − 0.23 95% CI − 1.20–0.73, I2 = 80%] [40, 47], inversion [SMD = − 0.14 95% CI − 0.44–0.17, I2 = 0%] [40, 47] and eversion [SMD = 0.21 95% CI − 0.09–0.51, I2 = 0%] [40, 47]; eccentric inversion [SMD = − 0.08 95% CI − 0.45–0.28, I2 = 14%] [40, 47] and eversion [SMD = 0.14 95% CI − 0.16–0.45, I2 = 0%] [40, 47]), or in female athletes (concentric plantarflexion [SMD = − 0.13 95% CI − 0.46–0.19, I2 = 0%] [40, 48], inversion [SMD = − 0.03 95% CI − 0.36–0.29, I2 = 0%] [40, 48] and eversion [SMD = − 0.21 95% CI − 0.54–0.11, I2 = 0%] [40, 48]; eccentric inversion [SMD = − 0.08 95% CI − 0.59–0.42, I2 = 51%] [40, 48] and eversion [SMD = − 0.12 95% CI − 0.45–0.21, I2 = 0%] [40, 48]).
Dynamic Balance
Reduced Y-Balance Test anterior reach distance (SMD = − 0.48, 95% CI − 0.70 to − 0.26, P < 0.0001, I2 = 0%) [20, 21] and posterior-lateral reach distance (SMD = − 0.22, 95% CI − 0.44 to − 0.01, P = 0.04, I2 = 0%) [20, 21] in the male athletes were associated with the occurrence of ankle sprain. Posterior-medial reach (SMD = − 0.04 95% CI − 0.26–0.17, I2 = 0%) [20, 21] distance had no influence on injury risk. For female athletes, no difference in the injured and the uninjured population was observed in the YBT (anterior [SMD = − 0.13 95% CI − 0.50–0.24, I2 = 0%] [20, 39], posterior-lateral [SMD = 0.28 95% CI − 0.17–0.72, I2 = 28%] [20, 39], posterior-medial [SMD = 0.15 95% CI − 0.51–0.82, I2 = 66%] [20, 39]).
Range of Motion and Joint Laxity
Ankle joint laxity in the form of the ankle anterior drawer test did not reveal an association with higher risk of ankle sprain in male athletes (OR = 1.49 95% CI 0.83–2.69, I2 = 0%) [40, 42, 43]. No factor related to joint range of motion showed a relationship with risk of ankle sprain in male (dorsiflexion [SMD = − 0.03 95% CI − 0.56 to − 0.10, I2 = 0%] [16, 20, 40, 42, 44, 47], plantarflexion [SMD = − 0.28 95% CI − 0.76–0.20, I2 = 73%] [16, 47], inversion [SMD = − 0.07 95% CI − 0.54–0.40, I2 = 34%] [40, 47], eversion [SMD = 0.16 95% CI − 0.59–0.91, I2 = 68%] [40, 47] and hip internal rotation [SMD = − 0.03 95% CI − 0.30–0.24, I2 = 16%] [44, 47]) or female athletes (dorsiflexion [SMD = 0.12 95% CI − 0.15–0.38, I2 = 0%] [20, 40, 48], inversion [SMD = − 0.04 95% CI − 0.36–0.29, I2 = 0%] [40, 48], eversion [SMD = 0.17 95% CI − 0.24–0.57, I2 = 28%] [40, 48].
Discussion
This is the first study to systematically identify sex differences in intrinsic risk factors for ankle sprain in athletes using a meta-analytic approach, with the major finding that different risk factors have been reported for males and females. Males with a previous ankle sprain, higher weight and body mass index, lower isometric hip abduction strength and worse performance in multiple dynamic balance directions were identified as having an elevated risk for ankle sprains. However, only females with lower concentric dorsiflexion strength were detected to be at a higher risk of sustaining an ankle sprain. Our findings not only preliminarily suggest divergent risk factors between males and females, but also highlight a clear paucity of data regarding female-specific risk factors for ankle sprain injury in athletes. Only 20.2% of participants in our analyses were female, which likely contributed to a lack of evidence for further risk factors for female athletes. Therefore, it cannot be ruled out that there are other under-researched factors contributing to ankle sprain risk in female athletes.
A key finding of this study is that previous ankle sprain was identified as a leading risk factor for future ankle sprain in male athletes but not in female athletes, which is supported by Wikstrom and colleagues [15]. Evidence indicates that those with a history of ankle sprain display alterations in central processing which purportedly feed into future ankle sprain injury risk. These alterations include differences in visual processing during single leg tasks [49], shifts in muscular activation strategies during landing tasks [50], and changes in muscle activation patterns in both the injured and healthy limbs during perturbed walking tasks [51]. However, given that these findings are from mixed-sex studies, it remains unclear why ankle sprain history is a risk factor for males but not females. Considering findings that ankle sprain patients often develop prolonged changes in ankle joint laxity and local muscle weakness, it is conceivable that deficient local ankle muscle strength would play a role in increased vulnerability for subsequent ankle sprain risk in male athletes [52, 53]. However, contrary to this notion is that no significant relationship between local ankle strength and ankle sprains was detected in males in our study and instead, female athletes with deficient concentric dorsiflexion strength were more likely to sustain an ankle sprain. Although mixed-sex studies report lower dorsiflexion strength in people with a history of ankle sprain [54], our results indicate that females with deficits in concentric dorsiflexion strength are at a higher risk of ankle sprain regardless of injury history and that dorsiflexion strength should therefore be considered an independent risk factor.
Although local ankle muscle strength was not significantly associated with ankle sprain risk in male athletes, we identified an association between global strength and ankle sprains, with male athletes demonstrating lower isometric hip abduction strength at a higher risk of injury. In support of this finding is mixed-sex evidence suggesting that people with hip-abductor weakness exhibit altered ankle mechanics during single leg landing and balance tasks [55, 56]. Further, males and females with a history of ankle sprain demonstrate altered hip muscle activation strategies during landing under fatigued conditions [50], as well as lower hip abduction strength than healthy controls [57]. This may further explain identification of a previous ankle sprain as a risk factor for a future ankle sprain injury in men. However, despite the mechanistic evidence which links hip function and factors relevant for ankle sprain risk in mixed-sex studies, the relationship between isometric hip abduction strength and ankle sprain in females remains unclear due to a complete absence of studies. We therefore recommend that future studies investigate the role of isometric hip abduction strength in ankle sprain incidence specifically in females.
Our analysis also revealed that deficient dynamic balance performance in multiple directions was a risk factor for ankle sprain in males but not females. In pooled-sex studies, deficits in dynamic balance performance persist at least six months following an initial injury [58], and those with a history of ankle sprain also experience greater decrements in dynamic balance performance under fatigued conditions than healthy controls [59]. This may underpin the association between ankle sprain history and future ankle sprain risk in male athletes. Females typically score higher than males on tests commonly used to assess dynamic balance [60], and female athletes experience no significant decrements in Star excursion balance test performance following a whole-body fatiguing protocol [61] which may help to explain the lack of relationship between dynamic balance and ankle sprain risk in female athletes. Despite neuromuscular training programmes enhancing dynamic balance performance [62], our finding that dynamic balance has no influence on ankle sprain incidence in female athletes may also elucidate the inconclusive effects of neuromuscular training programmes on ankle injury prevention in female soccer players [63]. This is supported by evidence showing that neuromuscular training incorporating only balance exercises is less effective for preventing ankle sprains than multimodal exercise programmes using a combination of balance, strength or stretching exercises [64]. Further, there are inconclusive findings regarding whether or not balance training can improve other neuromuscular parameters [65], and therefore training designed to mitigate the risk of ankle sprain in females is recommended to look beyond only balance and address many components of neuromuscular development. For example, although not eligible for meta-analyses due to a lack of studies, there is isolated evidence that deficits in joint position sense during ankle inversion (considered an indicator of proprioception) and poor co-ordination also influence ankle sprain risk in females [48]. Further, given recent findings that postural control under fatigued conditions is also altered in the premenstrual phase for female athletes [66], combined with increasing evidence for hormonal influences on anterior cruciate ligament injury risk in female athletes [67, 68], interactions between neuromuscular control, menstrual cycle phase and ankle sprain injury risk warrant further investigation.
Finally, both weight and BMI were associated with ankle sprain incidence rate in male but not female athletes. Importantly, these risk factors likely interact with other risk factors to jointly influence the risk of ankle sprain injury in male athletes. Tyler et al. [17] observed that an overweight high school American football player with a history of ankle sprain was 19 times more likely to sustain an ankle sprain than a player who was within a normal weight range and had no history of ankle sprain. Indeed, risk factors that are independently identified likely interact to influence injury risk in a joint fashion [69, 70], as highlighted throughout this discussion. Further evidence of this comes again from the male-specific risk factors in the current study, with De Ridder and colleagues [41] suggesting that decreases in hip strength may contribute to reduced dynamic control of the hip joint, which likely influences performance on dynamic balance tests [71].
Overall, previous studies on movement-related mechanisms contributing to sports injuries have often neglected or underestimated the influence of female vs. male characteristics. Therefore, the reasons for the different injury risk factors between males and females are not fully understood. Sex differences have been observed for jump [72] and jump landing biomechanics [73] as well as change of direction [74], squatting and side-step tasks [75], indicating different strategies of neuromuscular control to stabilise the ankle joint during challenging movements. This is supported by our finding that dorsiflexion strength is associated with ankle sprain risk in females but not in males. Another factor that has often been discussed in relation to the injury risk in females is a greater joint laxity and lower joint resistance to translation and rotation movements when compared with males [26, 76]. However, in our meta-analysis no factor related to joint range of motion showed a relationship with risk of ankle sprain in both females and males.
It would be negligent to not comment on a central issue which is not only a limitation of our study, but more importantly, a shortcoming of the ankle sprain and sport science literature in general: the presence of systematic bias resulting in a distinct lack of female-specific research [77, 78]. In the case of our analysis, this gap is further highlighted by the pooled sample sizes. Of the 3636 athletes, only 20.2% were females, and of the 576 ankle sprains, only 20.3% occurred in females. These percentages are even comfortably below the recent revelations that between 34 and 39% of participants in sports and exercise medicine and science research are females [77, 78]. Such disparities in sample sizes between sexes may have further contributed to the absence of risk factors found for female ankle sprains in our study and ultimately limit our ability to make strong conclusions regarding female-specific risk factors for ankle sprain. Indeed, when considered alongside the evidence that females experience ankle sprains at higher rates, our finding of fewer risk factors for ankle sprain in women highlights the insufficiency of current data.
Importantly, our analysis also highlights the hazards of pooling sexes to interpret results. When studies were combined for sexes in the current study, six variables were detected as risk factors for ankle sprain, but when males were removed from the analysis, only one risk factor remained significant for females. This result has important implications for the interpretation of findings from sports injury studies, indicating that findings from male and mixed-sex studies should not simply be extrapolated and applied to females without due consideration.
Limitations
A central limitation of this study has been outlined in the preceding paragraphs, and the authors emphasise that further female-specific data are needed to make stronger conclusions regarding whether mechanisms or methodology underlie the observed sex-differences in ankle sprain risk factors. Additionally, in the same way that studies pooling results for sexes limit insight into the sex-dependent risk factors for ankle sprain, our approach to combining studies likely masks sport-dependent, age-dependent and level-dependent risk factors for ankle sprain injury risk. It is certainly conceivable that elite basketballers with well-developed physical capacities demonstrate different risk factors for ankle sprain than adolescent amateur soccer players, and there is ample existing evidence for different ankle sprain injury rates between sports [3, 79]. We also recognise that different types of ankle sprain injury and different mechanisms of injury likely have unique risk factors, and we therefore acknowledge this as a limitation of our study. The methodological heterogeneity should also be considered when interpreting our results, particularly for risk factors where the I2 value is high, such as male concentric dorsiflexion strength (I2 = 80%).
Recommendations
The results of this analysis provide practitioners with clear targets for reducing ankle sprain injury in male athletes. Data on previous injury history should be considered in all cases, and all interventions should target the development of isometric hip abduction strength and dynamic balance performance, alongside potential reductions in BMI in specific cases. Indeed, there is evidence that a balance training intervention can drastically reduce the elevated injury risk that arises from ankle sprain history and a higher BMI in male high school American football players [80]. Further, although outside the scope of this study, external ankle support appears to improve ankle sprain avoidance and reoccurrence outcomes [81, 82]. The absence of multiple risk factors in our study should not discourage practitioners from performing injury risk screening and implementing injury prevention programmes in female athletes. We acknowledge and emphasise that our findings do not entirely dismiss some risk factors due to issues arising from small sample sizes and low quality of evidence. We therefore suggest that the development of concentric dorsiflexion strength should be considered an integral component of screening and interventions and should be implemented as part of a wider neuromuscular training programme in order to mitigate the risk of ankle sprain injury in female athletes. As it is plausible that different types of ankle sprain have different risk factors, we recommend that future studies seek to identify ankle sprain injury type-specific risk factors and elucidate the mechanisms underlying specific injury risk factors in order to provide practitioners with more actionable information. For example, it is currently unclear why dorsiflexion strength is associated with ankle sprain injury in females but not males.
Conclusion
These results provide the first meta-analytic evidence that male and female athletes may have unique risk factors for ankle sprains. However, the strength of this conclusion is somewhat limited due to methodological considerations, and the risk factors which drive higher ankle sprain injury rates in female athletes remain largely elusive based on the available evidence. We therefore encourage future studies to disaggregate their data according to sex wherever possible, as well as to seek further elucidation of the contributions of isometric hip abduction strength, joint laxity and injury history to ankle sprain incidence specifically in female athletes.
Supplementary Information
Additional file 1. Forest plots for potential risk factors for ankle sprain in males and female athletes.
Acknowledgements
Not applicable.
Author Contributions
JM contributed to study planning, literature search, article screening and manuscript writing. CK contributed to article screening, data extraction, data analysis and manuscript drafting. KH contributed to study conception, study planning, manuscript editing and manuscript revision. AZ contributed to study conception, study planning, article screening and manuscript review. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. No sources of funding were used to assist in the preparation of this manuscript.
Availability of Data and Materials
The data from the current review are presented in the article/electronic supplementary material and are available from the corresponding author upon request.
Declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing interests
Joel Mason, Christoph Kniewasser, Karsten Hollander and Astrid Zech declare that they have no competing interests relevant to the content of this review.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311. [PMC free article] [PubMed] [Google Scholar]
- 2.Nelson AJ, Collins CL, Yard EE, Fields SK, Comstock RD. Ankle injuries among United States high school sports athletes, 2005–2006. J Athl Train. 2007;42(3):381. [PMC free article] [PubMed] [Google Scholar]
- 3.Fong DT, Hong Y, Chan LK, Yung PSH, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 4.Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, Hertel J, Hiller CE, Kaminski TW, McKeon PO, Refshauge KM. Evidence review for the 2016 international ankle consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 5.Herzog MM, Mack CD, Dreyer NA, Wikstrom EA, Padua DA, Locher MS, DiFiori JP, Marshall SW. Ankle sprains in the national basketball association, 2013–2014 through 2016–2017. Am J Sports Med. 2019;47(11):2651–2658. doi: 10.1177/0363546519864678. [DOI] [PubMed] [Google Scholar]
- 6.Pasanen K, Ekola T, Vasankari T, Kannus P, Heinonen A, Kujala UM, Parkkari J. High ankle injury rate in adolescent basketball: a 3-year prospective follow-up study. Scand J Med Sci Sports. 2017;27(6):643–649. doi: 10.1111/sms.12818. [DOI] [PubMed] [Google Scholar]
- 7.Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572–588. doi: 10.4085/1062-6050-344-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamacher D, Hollander K, Zech A. Effects of ankle instability on running gait ankle angles and its variability in young adults. Clin Biomech. 2016;33:73–78. doi: 10.1016/j.clinbiomech.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 9.McGuine TA, Brooks A, Hetzel S. The effect of lace-up ankle braces on injury rates in high school basketball players. Am J Sports Med. 2011;39(9):1840–1848. doi: 10.1177/0363546511406242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vuurberg G, Hoorntje A, Wink LM, Van Der Doelen BF, Van Den Bekerom MP, Dekker R, Van Dijk CN, Krips R, Loogman MC, Ridderikhof ML, Smithuis FF. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018;52(15):956. doi: 10.1136/bjsports-2017-098106. [DOI] [PubMed] [Google Scholar]
- 11.Meeuwisse WH, Tyreman H, Hagel B, Emery C. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. 2007;17(3):215–219. doi: 10.1097/JSM.0b013e3180592a48. [DOI] [PubMed] [Google Scholar]
- 12.Van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. Sports Med. 1992;14(2):82–99. doi: 10.2165/00007256-199214020-00002. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 14.Daneshjoo A, Mokhtar AH, Rahnama N, Yusof A. The effects of injury prevention warm-up programmes on knee strength in male soccer players. Biol Sport. 2013;30(4):281. doi: 10.5604/20831862.1077554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wikstrom EA, Cain MS, Chandran A, Song K, Regan T, Migel K, Kerr ZY. Lateral ankle sprain and subsequent ankle sprain risk: a systematic review. J Athl Train. 2021;56(6):578–585. doi: 10.4085/1062-6050-168-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saki F, Yalfani A, Fousekis K, Sodejani SH, Ramezani F. Anatomical risk factors of lateral ankle sprain in adolescent athletes: a prospective cohort study. Phys Ther Sport. 2021;48:26–34. doi: 10.1016/j.ptsp.2020.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Tyler TF, Mchugh MP, Mirabella MR, Mullaney MK, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34(3):471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 18.Kofotolis ND, Kellis E, Vlachopoulos SP. Ankle sprain injuries and risk factors in amateur soccer players during a 2-year period. Am J Sports Med. 2007;35(3):458–466. doi: 10.1177/0363546506294857. [DOI] [PubMed] [Google Scholar]
- 19.Powers CM, Ghoddosi N, Straub RK, Khayambashi K. Hip strength as a predictor of ankle sprains in male soccer players: a prospective study. J Athl Train. 2017;52(11):1048–1055. doi: 10.4085/1062-6050-52.11.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartley EM, Hoch MC, Boling MC. Y-balance test performance and BMI are associated with ankle sprain injury in collegiate male athletes. J Sci Med Sport. 2018;21(7):676–680. doi: 10.1016/j.jsams.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 21.Gribble PA, Terada M, Beard MQ, Kosik KB, Lepley AS, McCann RS, Pietrosimone BG, Thomas AC. Prediction of lateral ankle sprains in football players based on clinical tests and body mass index. Am J Sports Med. 2016;44(2):460–467. doi: 10.1177/0363546515614585. [DOI] [PubMed] [Google Scholar]
- 22.Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33(10):1485–1491. doi: 10.1177/0363546505275490. [DOI] [PubMed] [Google Scholar]
- 23.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 24.Zech A, Hollander K, Junge A, Steib S, Groll A, Heiner J, Nowak F, Pfeiffer D, Rahlf AL. Sex differences in injury rates in team-sport athletes: a systematic review and meta-regression analysis. J Sport Health Sci. 2021;11(1):104–114. doi: 10.1016/j.jshs.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hollander K, Rahlf AL, Wilke J, Edler C, Steib S, Junge A, Zech A. Sex-specific differences in running injuries: a systematic review with meta-analysis and meta-regression. Sports Med. 2021;52(5):1011–1039. doi: 10.1007/s40279-020-01412-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ericksen H, Gribble PA. Sex differences, hormone fluctuations, ankle stability, and dynamic postural control. J Athl Train. 2012;47(2):143–148. doi: 10.4085/1062-6050-47.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quatman CE, Ford KR, Myer GD, Paterno MV, Hewett TE. The effects of gender and pubertal status on generalized joint laxity in young athletes. J Sci Med Sport. 2008;11(3):257–263. doi: 10.1016/j.jsams.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. B Med J. 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Sys Rev. 2016;5(1):1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hayden JA, Côté P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144(6):427–437. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- 31.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 32.Green B, Bourne MN, Pizzari T. Isokinetic strength assessment offers limited predictive validity for detecting risk of future hamstring strain in sport: a systematic review and meta-analysis. Br J Sports Med. 2018;52(5):329–336. doi: 10.1136/bjsports-2017-098101. [DOI] [PubMed] [Google Scholar]
- 33.Green B, Bourne MN, van Dyk N, Pizzari T. Recalibrating the risk of hamstring strain injury (HSI): A 2020 systematic review and meta-analysis of risk factors for index and recurrent hamstring strain injury in sport. Br J Sports Med. 2020;54(18):1081–1088. doi: 10.1136/bjsports-2019-100983. [DOI] [PubMed] [Google Scholar]
- 34.Schut L, Wangensteen A, Maaskant J, Tol JL, Bahr R, Moen M. Can clinical evaluation predict return to sport after acute hamstring injuries? A systematic review. Sports Med. 2017;47(6):1123–1144. doi: 10.1007/s40279-016-0639-1. [DOI] [PubMed] [Google Scholar]
- 35.Reurink G, Goudswaard GJ, Tol JL, Verhaar JA, Weir A, Moen MH. Therapeutic interventions for acute hamstring injuries: a systematic review. Br J Sports Med. 2012;46(2):103–109. doi: 10.1136/bjsports-2011-090447. [DOI] [PubMed] [Google Scholar]
- 36.Review Manager (RevMan) [Computer program]. Version 5.2. Copenhagen: the Nordic Cochrane centre, the Cochrane collaboration, 2012.
- 37.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 38.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. B Med J. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Attenborough AS, Sinclair PJ, Sharp T, Greene A, Stuelcken M, Smith RM, Hiller CE. The identification of risk factors for ankle sprains sustained during netball participation. Phys Ther Sport. 2017;23:31–36. doi: 10.1016/j.ptsp.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 40.Beynnon BD, Renström PA, Alosa DM, Baumhauer JF, Vacek PM. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19(2):213–220. doi: 10.1016/S0736-0266(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 41.De Ridder R, Witvrouw E, Dolphens M, Roosen P, Van Ginckel A. Hip strength as an intrinsic risk factor for lateral ankle sprains in youth soccer players: a 3-season prospective study. Am J Sports Med. 2017;45(2):410–416. doi: 10.1177/0363546516672650. [DOI] [PubMed] [Google Scholar]
- 42.Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for acute ankle injuries among male soccer players: a prospective cohort study. Scand J Sci Med Sports. 2010;20(3):403–410. doi: 10.1111/j.1600-0838.2009.00971.x. [DOI] [PubMed] [Google Scholar]
- 43.Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40(8):1842–1850. doi: 10.1177/0363546512449602. [DOI] [PubMed] [Google Scholar]
- 44.Kawaguchi K, Taketomi S, Mizutani Y, Inui H, Yamagami R, Kono K, Takagi K, Kage T, Sameshima S, Tanaka S, Haga N. Hip abductor muscle strength deficit as a risk factor for inversion ankle sprain in male college soccer players: a prospective cohort study. Orthop J Sports Med. 2021;9(7). 10.1177/23259671211020287. [DOI] [PMC free article] [PubMed]
- 45.Kofotolis N, Kellis E. Ankle sprain injuries: a 2-year prospective cohort study in female Greek professional basketball players. J Athl Train. 2007;42(3):388. [PMC free article] [PubMed] [Google Scholar]
- 46.McCann RS, Kosik KB, Terada M, Beard MQ, Buskirk GE, Gribble PA. Acute lateral ankle sprain prediction in collegiate women's soccer players. Int J Sports Phys Ther. 2018;13(1):12. [PMC free article] [PubMed] [Google Scholar]
- 47.Willems TM, Witvrouw E, Delbaere K, Mahieu N, De Bourdeaudhuij L, De Clercq D. Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study. Am J Sports Med. 2005;33(3):415–423. doi: 10.1177/0363546504268137. [DOI] [PubMed] [Google Scholar]
- 48.Willems TM, Witvrouw E, Delbaere K, Philippaerts R, De Bourdeaudhuij I, De Clercq D. Intrinsic risk factors for inversion ankle sprains in females–a prospective study. Scand J Med Sci Sports. 2005;15(5):336–345. doi: 10.1111/j.1600-0838.2004.00428.x. [DOI] [PubMed] [Google Scholar]
- 49.Song K, Burcal CJ, Hertel J, Wikstrom EA. Increased visual use in chronic ankle instability: a meta-analysis. Med Sci Sports Exerc. 2016;48(10):2046–2056. doi: 10.1249/MSS.0000000000000992. [DOI] [PubMed] [Google Scholar]
- 50.Webster KA, Pietrosimone BG, Gribble PA. Muscle activation during landing before and after fatigue in individuals with or without chronic ankle instability. J Athl Train. 2016;51(8):629–636. doi: 10.4085/1062-6050-51.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin CI, Khajooei M, Engel T, Nair A, Heikkila M, Kaplick H, Mayer F. The effect of chronic ankle instability on muscle activations in lower extremities. PLoS ONE. 2021;16(2):e0247581. doi: 10.1371/journal.pone.0247581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cordova ML, Sefton JM, Hubbard TJ. Mechanical joint laxity associated with chronic ankle instability: a systematic review. Sports Health. 2010;2(6):452–459. doi: 10.1177/1941738110382392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J Athl Train. 2002;37(4):487. [PMC free article] [PubMed] [Google Scholar]
- 54.Feger MA, Snell S, Handsfield GG, Blemker SS, Wombacher E, Fry R, Hart JM, Saliba SA, Park JS, Hertel J. Diminished foot and ankle muscle volumes in young adults with chronic ankle instability. Orthop J Sports Med. 2016;4(6). 10.1177/2325967116653719. [DOI] [PMC free article] [PubMed]
- 55.Lee SP, Powers C. Fatigue of the hip abductors results in increased medial–lateral center of pressure excursion and altered peroneus longus activation during a unipedal landing task. Clin Bomech. 2013;28(5):524–529. doi: 10.1016/j.clinbiomech.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 56.Lee SP, Powers CM. Individuals with diminished hip abductor muscle strength exhibit altered ankle biomechanics and neuromuscular activation during unipedal balance tasks. Gait Posture. 2014;39(3):933–938. doi: 10.1016/j.gaitpost.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 57.Khalaj N, Vicenzino B, Heales LJ, Smith MD. Is chronic ankle instability associated with impaired muscle strength? Ankle, knee and hip muscle strength in individuals with chronic ankle instability: a systematic review with meta-analysis. Br J Sports Med. 2020;54(14):839–847. doi: 10.1136/bjsports-2018-100070. [DOI] [PubMed] [Google Scholar]
- 58.Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Dynamic balance deficits 6 months following first-time acute lateral ankle sprain: a laboratory analysis. J Orthop Sports Phys Ther. 2015;45(8):626–633. doi: 10.2519/jospt.2015.5653. [DOI] [PubMed] [Google Scholar]
- 59.Steib S, Zech A, Hentschke C, Pfeifer K. Fatigue-induced alterations of static and dynamic postural control in athletes with a history of ankle sprain. J Athl Train. 2013;48(2):203–208. doi: 10.4085/1062-6050-48.1.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kramer TA, Sacko RS, Pfeifer CE, Gatens DR, Goins JM, Stodden DF. The association between the functional movement screent, y-balance test, and physical performance tests in male and female high school athletes. Int J Sports Phys Ther. 2019;14(6):911. [PMC free article] [PubMed] [Google Scholar]
- 61.Baghbani F, Woodhouse LJ, Gaeini AA. Dynamic postural control in female athletes and nonathletes after a whole-body fatigue protocol. J Strength Cond Res. 2016;30(7):1942–1947. doi: 10.1519/JSC.0000000000001275. [DOI] [PubMed] [Google Scholar]
- 62.Faude O, Rössler R, Petushek EJ, Roth R, Zahner L, Donath L. Neuromuscular adaptations to multimodal injury prevention programs in youth sports: a systematic review with meta-analysis of randomized controlled trials. Front Physiol. 2017;8:791. doi: 10.3389/fphys.2017.00791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Crossley KM, Patterson BE, Culvenor AG, Bruder AM, Mosler AB, Mentiplay BF. Making football safer for women: a systematic review and meta-analysis of injury prevention programmes in 11 773 female football (soccer) players. Br J Sports Med. 2020;54(18):1089–1098. doi: 10.1136/bjsports-2019-101587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hübscher M, Zech A, Pfeifer K, Hänsel F, Vogt L, Banzer W. Neuromuscular training for sports injury prevention: a systematic review. Med Sci Sports Exerc. 2010;42(3):413–421. doi: 10.1249/MSS.0b013e3181b88d37. [DOI] [PubMed] [Google Scholar]
- 65.Zech A, Hübscher M, Vogt L, Banzer W, Hänsel F, Pfeifer K. Balance training for neuromuscular control and performance enhancement: a systematic review. J Athl Train. 2010;45(4):392–403. doi: 10.4085/1062-6050-45.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kacem M, Borji R, Sahli S, Rebai H. The disturbing effect of neuromuscular fatigue on postural control is accentuated in the premenstrual phase in female athletes. Front Physiol 2021;12. 10.3389/fphys.2021.736211 [DOI] [PMC free article] [PubMed]
- 67.Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36(6):1073–1080. doi: 10.1177/0363546507313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Herzberg SD, Motu’apuaka ML, Lambert W, Fu R, Brady J, Guise JM. The effect of menstrual cycle and contraceptives on ACL injuries and laxity: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5(7). 10.1177/2325967117718781. [DOI] [PMC free article] [PubMed]
- 69.Ruddy JD, Cormack SJ, Whiteley R, Williams MD, Timmins RG, Opar DA. Modeling the risk of team sport injuries: a narrative review of different statistical approaches. Front Physiol. 2019;10:829. doi: 10.3389/fphys.2019.00829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mason J, Wellmann K, Groll A, Braumann KM, Junge A, Hollander K, Zech A. Game exposure, player characteristics, and neuromuscular performance influence injury risk in professional and youth field hockey players. Orthop J Sports Med. 2021;9(4):232596712199516. doi: 10.1177/2325967121995167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wilson BR, Robertson KE, Burnham JM, Yonz MC, Ireland ML, Noehren B. The relationship between hip strength and the Y balance test. J Sport Rehabil. 2018;27(5):445–450. doi: 10.1123/jsr.2016-0187. [DOI] [PubMed] [Google Scholar]
- 72.Fuchs PX, Menzel HJ, Guidotti F, Bell J, von Duvillard SP, Wagner H. Spike jump biomechanics in male versus female elite volleyball players. J Sports Sci. 2019;2(21):2411–2419. doi: 10.1080/02640414.2019.1639437. [DOI] [PubMed] [Google Scholar]
- 73.Quatman CE, Ford KR, Myer GD, Hewett TE. Maturation leads to gender differences in landing force and vertical jump performance: a longitudinal study. Am J Sports Med. 2006;34(5):806–813. doi: 10.1177/0363546505281916. [DOI] [PubMed] [Google Scholar]
- 74.Thomas C, Dos’ Santos T, Comfort P, Jones PA. Male and female soccer players exhibit different knee joint mechanics during pre-planned change of direction. Sports Biomech. 2020;29:1–4. doi: 10.1080/14763141.2020.1830160. [DOI] [PubMed] [Google Scholar]
- 75.Mendiguchia J, Ford KR, Quatman CE, Alentorn-Geli E, Hewett TE. Sex differences in proximal control of the knee joint. Sports Med. 2011;41(7):541–557. doi: 10.2165/11589140-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, Georgoulis T, Hewett TE, Johnson R, Krosshaug T, Mandelbaum B. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42(6):394–412. doi: 10.1136/bjsm.2008.048934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cowley ES, Olenick AA, McNulty KL, Ross EZ. “Invisible sportswomen”: the sex data gap in sport and exercise science research. Women Sport and Phys Act J. 2021;29(2):146–151. [Google Scholar]
- 78.Costello JT, Bieuzen F, Bleakley CM. Where are all the female participants in sports and exercise medicine research? Eur J Sport Sci. 2018;14(8):847–851. doi: 10.1080/17461391.2014.911354. [DOI] [PubMed] [Google Scholar]
- 79.Wiersma AJ, Brou L, Fields SK, Comstock RD, Kerr ZY. Epidemiologic comparison of ankle injuries presenting to US emergency departments versus high school and collegiate athletic training settings. Inj Epidemiol. 2018;5(1):1–10. doi: 10.1186/s40621-018-0163-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McHugh MP, Tyler TF, Mirabella MR, Mullaney MJ, Nicholas SJ. The effectiveness of a balance training intervention in reducing the incidence of noncontact ankle sprains in high school football players. Am J Sports Med. 2007;35(8):1289–1294. doi: 10.1177/0363546507300059. [DOI] [PubMed] [Google Scholar]
- 81.Verhagen EA, Bay K. Optimising ankle sprain prevention: a critical review and practical appraisal of the literature. Br J Sports Med. 2010;44(15):1082–1088. doi: 10.1136/bjsm.2010.076406. [DOI] [PubMed] [Google Scholar]
- 82.Stotz A, John C, Gmachowski J, Rahlf AL, Hamacher D, Hollander K, Zech A. Effects of elastic ankle support on running ankle kinematics in individuals with chronic ankle instability and healthy controls. Gait Posture. 2021;87:149–155. doi: 10.1016/j.gaitpost.2021.04.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Forest plots for potential risk factors for ankle sprain in males and female athletes.
Data Availability Statement
The data from the current review are presented in the article/electronic supplementary material and are available from the corresponding author upon request.