Abstract
OBJECTIVE:
The objective of the present study was to evaluate and compare primary and secondary implant stability of conical endosteal implants placed using osseodensification osteotomy and conventional osteotomy techniques.
MATERIALS AND METHODS:
The present invivo study was designed as a prospective, observational study in which a total of 26 endosteal implants were placed in the posterior edentulous regions of upper and lower jaws in 13 patients divided into two groups, Group A and Group B. In Group A, implants were placed using osseodensification osteotomy technique while in Group B, conventional osteotomy technique was used. Primary implant stability was measured in both groups immediately after implant placement while secondary implant stability was measured in both groups at an interval of 4 months. Statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 20.00 (SPSS Inc., Chicago, IL, USA) while an independent t-test, also, called Student's t-test was used to conduct the analysis.
RESULTS:
The mean value of primary implant stability in Group A was found to be 74.5 as against that in Group B which was 62.08 (P-value 0.001). Likewise, the mean value of secondary implant stability in Group A after 4 months’ interval was 70.92 while in Group B, it was found to be 63.69 (P-value 0.001).
CONCLUSIONS:
The dental implants placed with the osseodensification technique showed higher mean primary and secondary implant stability values when compared to implants placed by the conventional technique.
Keywords: Bone-to-implant contact percentage, bone volume percentage, osseodensification, osteotomy, primary implant stability, secondary implant stability
Introduction
Osseointegration of dental implants is a prime requisite for the success of any implant treatment, and this itself is an outcome of a multitude of variables that play a significant role behind it. In the year 1981, Albrektsson et al.[1] proposed six major factors of osseointegration including implant material, implant surface and design, condition of bone, surgical technique used, and the loading conditions. The mechanical stability of implants at the time of surgery, also, known as primary implant stability, is an essential factor to achieve implant osseointegration while the osseointegration process that follows after a successful implant placement procedure leading to the apposition of new bone on the implant surface leads to achieving secondary implant stability.[2]
The movements that occur atbone-to-implant interfaces induce stress which hinders the osseointegration process.[3,4] In this context, movements above 50–100 micrometers range have been seen to negatively influence the osseointegration process by inducing bone resorption at bone-to-implant interfaces.[5,6,7] Therefore, a high initial (primary) implant stability is essential for successful osseointegration of implants with the adjacent bone, and this itself is influenced by several factors including implant design, size, macro-and micro-surface, quality and quantity of bone, and the surgical technique used for implant placement in addition to the operator's skills. In case of poor bone density, the insufficient bone present around implants could negatively affect the histo-morphometric parameters such as bone-to-implant contact (BIC) percentage and bone volume (BV) percentage, eventually, affecting both the primary and secondary stabilities.[2]
A plethora of studies have highlighted the significance of the surgical technique used in improving primary implant stability. In the similar context, few of the studies have proposed the use of osteotomes while implant site preparation to condense bone to increase BIC percentage and BV percentage in cases with poor bone support.[8,9,10,11,12] Explicitly designed implants in cases with low-density bone have, also, been developed and used.[13] One of the studies has, also, demonstrated that implant site preparation with multi-stepped drills increases primary implant stability, further supporting the key role that surgical procedures and equipments have on the overall implant stability.[14]
In line with the above-stated facts, a new osteotomy preparation technique, termed osseodensification technique, was introduced by Huwais in the year 2013 for the placement of endosteal implants.[15] In contrast with the conventional osteotomy technique, osseodensification technique leads to the preservation of bone that is cut during surgical preparation of implant bed with the help of specially designed burs to increase the density of bone as has been reported in an invitro study.[16,17,18] The present study aimed to evaluate and compare primary and secondary implant stability of conical endosteal implants placed using osseodensification osteotomy and conventional osteotomy techniques.
Materials and Methods
The present invivo study was designed as a prospective, observational study that aimed at comparing the primary and secondary implant stability of conical endosteal implants placed using osseodensification osteotomy and conventional osteotomy techniques. The study protocol was approved by the Institutional Ethics Committee before the start of the study. In the present study, a total of 13 patients divided into two groups, Group A and Group B, who required implant-supported prostheses in posterior edentulous regions of upper and lower jaws were selected from the outpatient department while 26 endosteal implants were placed using a split-mouth design. The study included two posterior edentulous regions with low-density bone, that is, D3 (350–850 HU) bone receiving two endosteal implants. For the present study, patients within an age range of 20–60 years with good oral hygiene were included while patients with known systemic disorders including diabetes, patients with untreated periodontal disease, those who had received irradiation in the head and neck area, patients with parafunctional habits, smokers, and pregnant and lactating females were excluded. The selected patients were explained in detail about the protocol of the study while a written informed consent was obtained before their inclusion in the study. After case history elicitation and a thorough general physical and local examination, patients were subjected to a pre-operative analysis of the surgical area first clinically and then, using cone-beam computed tomography examination.
Surgical Procedure: For the present study, patients were divided into two groups, that is, Group A and Group B wherein in Group A, 13 endosteal implants were placed using osseodensification osteotomy technique while in Group B, a similar number of implants were placed using conventional osteotomy technique. MIS Lance (screw type, internal hex, Israel) conical dental implants of various diameters and lengths were used for the purpose of the present study. Also, primary implant stability was measured in both the groups immediately after implant placement while secondary implant stability was measured at an interval of 4 months. To minimize post-operative swelling and discomfort, all the patients were kept on antibiotic therapy including 500mg amoxicillin and 125mg clavulanate potassium (Augmentin 625mg, Glaxo SmithKline, Mumbai) 24h before the surgery which was continued for 5 days post-surgery. Paracetamol, 325mg [Zydus Cadila Healthcare Ltd. (Alidac), Mumbai] and dexamethasone, 0.75mg [Zydus Cadila Healthcare Ltd. (Alidac), Mumbai] were, also, given half an hour before commencing the surgery. The surgical site was prepared following standard operating protocol. The surgical site was anesthetized using 2% lignocaine hydrochloride containing 1:80,000 concentration of adrenaline (Indoco Remedies Ltd., Mumbai) following which a mid crestal incision was given at the implant recipient site in addition to asulcular incision on the adjacent teeth with a Bard-Parker Blade no. 15. Also, a full-thickness mucoperiosteal flap was raised for the smooth conduct of the procedure and for obtaining better visibility and gaining access.
Group A (Study Group): In Group A patients, the implant site was prepared using Densah Burs (Versah, LLC, Jackson MI) [Figure 1] following the decision tree for osseodensification protocol [Table 1]. The implant site was drilled to the desired depth using a Pilot Drill (clockwise with a drill speed of 800–1,200rpm) using copious irrigation. Depending upon the implant type and diameter selected, the procedure was started with the help of the narrowest Densah Bur, that is, if a 3.75mm implant was to be placed, drilling was performed in a clockwise direction using a 2.0mm bur followed by a change of the drill motor to reverse (counter-clockwise with a drill speed of 800–1,500rpm) with copious irrigation depending on the density of the bone. Gradually, wider diameter burs were used, that is, 2.3mm, 3.0mm, and 3.3mm [Figure 2] while the implant was placed into the osteotomy site to the desired depth with a torque indicating ratchet wrench.
Figure 1.
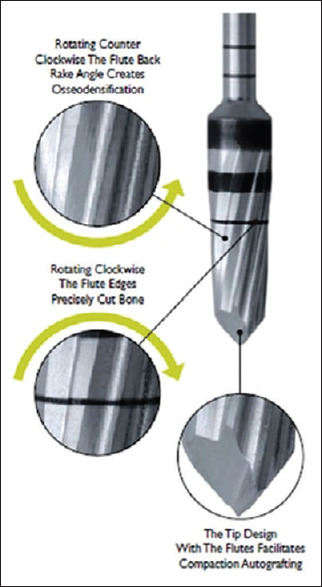
Densah Burs (Versah, LLC, Jackson MI) used during osseodensification protocol
Table 1.
Decision tree for osseodensification protocol
| Implant diameter (in mm) | Drill | Bur 1 | Bur 2 | Bur 3 |
|---|---|---|---|---|
| 3.5, 3.7, 3.8mm | Pilot Drill | 2.0mm (VT1525) | 3.0mm (VT2535) | - |
| 4.0, 4.2, 4.3mm | Pilot Drill | 2.3mm (VT1828) | 3.3mm (VT2838) | - |
| 4.5, 4.7, 4.8mm | Pilot Drill | 2.0mm (VT1525) | 3.0mm (VT2535) | 4.0mm (VT3545) |
| 5.0, 5.2, 5.3mm | Pilot Drill | 2.3mm (VT1828) | 3.3mm (VT2838) | 4.3mm (VT3848) |
Figure 2.
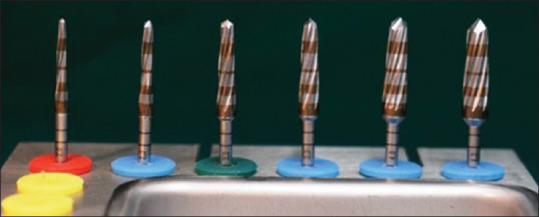
Wider diameter Densah Burs (Versah, LLC, Jackson MI) used, that is, 2.3mm, 3.0mm, and 3.3mm
Group B (Control Group): In Group B patients, the implant site was prepared up to the desired depth using a Pilot Drill (with a drill speed of 800–1,000rpm) using copious irrigation followed by conventional drills in sequence as per the MIS Lance implant diameter protocol, that is, if a 3.75mm implant was to be placed, the conventional drills (MIS Lance, screw type, internal hex, Israel) of gradually wider diameter ranging from D2.40, D3.20, and D3.60 (with a drill speed of 400–600rpm) using copious irrigation were used while the implant was placed into the osteotomy site to the desired depth.
Assessment of Primary and Secondary Implant Stability: Resonance frequency analysis (RFA) test was used to evaluate implant stability based on the principle of a vibrating fork that when a frequency of audible range is repeatedly vibrated onto an implant, then, depending on the bone-implant interface, resonance occurs. Also, the stronger the interface is, the higher is the frequency perceived. The primary and secondary implant stability for each implant was measured with the RFA device (Osstell™, Savedalen, Sweden) [Figure 3a and b]. A smart peg (Type 32) was placed in the implant with the help of a smart peg mount (4–6 Ncm). Based on the above test, the results were displayed on the instrument recognized as implant stability quotient (ISQ) which is scaled from 1 to 100. The higher the numbers, the greater is the implant stability. RFA was recorded in two planes, that is, in both buccolingual and mesiodistal planes. A mean of the ISQ values for each patient was calculated [Table 2] while the results obtained were tabulated and subjected to statistical analysis. Standard prosthetic procedures were used for the fabrication of prosthesis while implant-protected occlusion was given to the patients who were, then, followed-up for 1 year.
Figure 3.
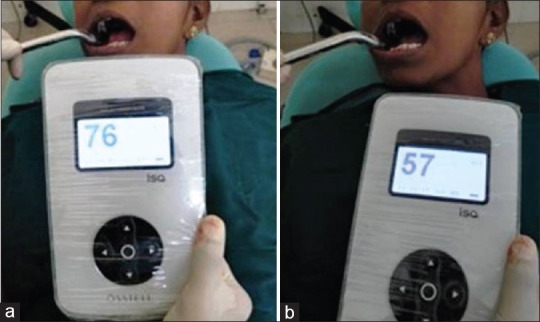
(a and b) RFA device (Osstell™, Savedalen, Sweden) with results displayed in a patient
Table 2.
Primary and secondary implant stability values
| Sr.No. | Osseodensification technique (Group A) | Conventional technique (Group B) | ||
|---|---|---|---|---|
|
|
|
|||
| Primary implant stability (ISQ) | Secondary implant stability (ISQ) | Primary implant stability (ISQ) | Secondary implant stability (ISQ) | |
| 1 | 73 | 65 | 59 | 60 |
| 2 | 71 | 69 | 60 | 62 |
| 3 | 75 | 73 | 62 | 64 |
| 4 | 80 | 75 | 75 | 68 |
| 5 | 68 | 70 | 57 | 62 |
| 6 | 75 | 73 | 57 | 62 |
| 7 | 80 | 75 | 51 | 68 |
| 8 | 73 | 69 | 60 | 69 |
| 9 | 75 | 79 | 62 | 66 |
| 10 | 67 | 66 | 56 | 59 |
| 11 | 73 | 70 | 61 | 63 |
| 12 | 81 | 68 | 73 | 61 |
| 13 | 82 | 70 | 74 | 64 |
| Mean | 74.85 | 70.92 | 62.08 | 63.69 |
| SD | 4.79 | 3.93 | 7.41 | 3.20 |
| Max. | 82 | 79 | 75 | 69 |
| Min. | 67 | 65 | 51 | 59 |
Primary implant stability: measured immediately after implant placement; Secondary implant stability: measured after 4 months; SD: standard deviation; ISQ: implant stability quotient
Data analysis
The normality of implant stability values was tested in the two groups by Kolmogorov–Smirnov test wherein it was found that the implant stability values in the two groups followed a normal distribution. Therefore, an independent t-test, also, called the two-sample t-test, independent-samples’ t-test or Student's t-test was used that determines whether there is a statistically significant difference between the means in two unrelated groups using the Statistical Package for Social Sciences (SPSS) version 20.00 (SPSS Inc., Chicago, IL, USA) while statistical significance was set at 5% level of significance (P < 0.05).
Results
Table 1 shows the decision tree for osseodensification protocol for Group A patients while Table 2 shows the RFA test values as recorded in two planes, that is, buccolingual and mesiodistal planes for which a mean of the ISQ values for each patient wascalculated. Table 3 and Graph 1 show a comparison of the overall mean values for primary implant stability between Group A (osseodensification osteotomy group) and Group B (conventional osteotomy group) using an independent t-test. The mean value of primary implant stability in Group A was found to be 74.5 as against that in Group B which was 62.08 (P = 0.001) inferring the results to be statistically significant with increased primary implant stability for Group A than Group B. Likewise, Table 4 and Graph 2 show a comparison of the overall mean values for secondary implant stability between Group A and Group B using independent t-test wherein the mean value of secondary implant stability in Group A (osseodensification osteotomy group) after 4 months interval was 70.92 while in Group B (conventional osteotomy group), itwas found to be 63.69 (P = 0.001) inferring that increased secondary implant stability was shown in Group A (osseodensification osteotomy group) than Group B (conventional osteotomy group).
Table 3.
Comparison of overall mean values for primary implant stability between Group A and Group B
| Groups | Mean | SD | Mean Diff. | 95% CI | t | df | P | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Lower | Upper | |||||||
| Group A (OD) | 74.85 | 4.79 | ||||||
| Group B (CT) | 62.08 | 7.41 | 12.77 | 7.72 | 17.82 | 5.2170 | 24 | <0.0001 |
OD: osseodensification technique; CT: conventional technique
Graph 1.
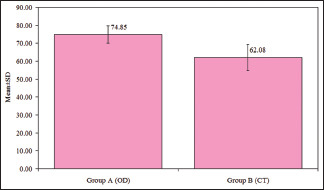
Comparison of overall mean values for primary implant stability between Group A and Group B. Group A: study group (osseodensification technique). Group B: control group (conventional technique)
Table 4.
Comparison of overall mean values for secondary implant stability between Group A and Group B
| Groups | Mean | SD | Mean Diff. | 95% CI | t | df | P | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Lower | Upper | |||||||
| Group A (OD) | 70.92 | 3.93 | ||||||
| Group B (CT) | 63.69 | 3.20 | 7.23 | 4.33 | 10.13 | 5.1490 | 24 | <0.0001 |
OD: osseodensification technique; CT: conventional technique
Graph 2.
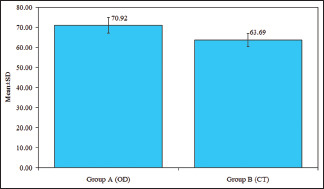
Comparison of overall mean values for secondary implant stability between Group A and Group B. Group A: study group (osseodensification technique). Group B: control group (conventional technique)
Discussion
The major aim of successful implant therapy is to achieve adequate primary implant stability which, in turn, depends upon a plethora of factors including bone density, implant thread type and geometry, and the surgical technique used for implant placement.[19,20,21,22] During osteotomy site preparation, maintenance and preservation of bone leads to an enhanced primary implant stability while an enhanced and facilitated BIC percentage enhances the secondary implant stability. Once primary implant stability is assured, bone remodeling becomes vital for the establishment of secondary implant stability and it is directly related to patient factors and implant surface characteristics such as surface energy, composition, topography, and roughness.[23,24]
The concept of improving bone density around implants to increase primary implant stability has been extensively explored in numerous studies that focused mainly on achieving improved initial implant stability in sites with specific anatomic constraints.[25] The surgical technique adopted for implant placement is another major aspect to be considered in this regard. In this context, a plethora of studies have suggested undersized implant site preparations to implant diameter reducing excessive bone loss to enhance primary implant stability.[2] It has, also, been argued and as reported by Büchter et al.,[26] in conventional osteotomy techniques, bone remodeling is hampered due to microdamage brought to the bone at ultra-structural levels and that initial implant stability may be significantly decreased in such cases after implant placement while delaying secondary implant stability due tothe time that is needed to repair these microdamages.
One of the prominent alternative techniques used previously to improve bone density around implants in challenging scenarios comprised of ridge expansion technique utilizing screw-type expanders which have been reported to expand the bone creating osteotomy site without removing the bone, but rather displacing it.[27,28,29] However, thin bone including buccal plate fractures are a significant point to be considered during these types of procedures since they may affect initial implant stability.[29]
The osseodensification technique is a non-subtractive, multi-stepped osteotomy technique that allows bone preservation and autografting compaction along the walls of the osteotomy site, thereby, enhancing primary implant stability. The densifying burs present a cutting chisel and tapered shank allowing them to progressively increase the diameter as they are moved deeper into the bone which controls the expansion process accomplished at high speed operating both clockwise and counter-clockwise directions. Another significant point to be noted is that the densifying burs taken in counter-clockwise direction exert the densification process more efficiently than when in clockwise direction and thus, are utilized specifically in low-density bone.[2,16,17,18]
In line with the above concepts, the findings of the present study suggested that implants placed with the osseodensification osteotomy technique (Group A) showed the highest mean primary implant stability (P = 0.001) [Table 3] and secondary implant stability (P = 0.001) [Table 4] values when compared with conventional osteotomy group (Group B). The results obtained in the present study were found to be in accordance with similar other studies including the studies conducted by Trisi et al.,[2] Boustany et al.,[12] Abboud et al.,[14] Lahens et al.,[17] and Huwais and Meyer[18] which showed osseodensification technique to be a promising technique to increase primary implant stability as well as in maintaining secondary implant stability increasing BV percentage around implants inserted in low-density bone as against the conventional technique for implant placement.
To summarize, osseodensification osteotomy technique is essentially a process that leads to the burnishing of the bone by redistributing bone chips chiseled-out on the surface while surgical preparation of implant bed through plastic deformation results in an improved bone density around implants. Also, the mean differences in the primary and secondary implant stability values found in the present study were remarkable when compared between osseodensification and conventional osteotomy techniques and this was following the results obtained from previous similar studies, thereby, making osseodensification osteotomy technique, a promising surgical technique for achieving good primary and secondary implant stabilityfor successful long-term clinical outcomes.
Conclusions
From the results obtained in the present study, it could be concluded that dental implants placed using osseodensification technique showed higher mean primary and secondary implant stability values when compared to implants placed using the conventional technique. The osseodensification osteotomy technique used in the present invivo study demonstrated increased BV percentage as well, around implants inserted even in low-density bone with respect to the conventional osteotomy technique. The observations made in the present study, thus, suggested that in low-density bone and in cases with narrow ridges, implant site preparation done using osseodensification technique gave promising results with high primary and secondary stabilities when compared with the conventional technique.
Limitations and further scope of the study
One of the possible limitations of the present study was the smaller sample size used while the patients were kept on follow-up for around 1 year which mandates further studies to be conducted in this regard with longer follow-up periods in longitudinal study designs on broader sample size. Furthermore, a detailed histo-morphometric analysis is, also, desired to analyze the bone-implant interface to further verify the presented hypothesis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank all the patients who contributed tothe study, without them this study would not have been feasible.
References
- 1.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants: Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 2.Trisi P, Berardini M, Falco A, Podaliri Vulpiani M. New osseodensification implant site preparation method to increase bone density in low-density bone: In-vivo evaluation in sheep. Implant Dent. 2016;25:24–31. doi: 10.1097/ID.0000000000000358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang PK, Chen YC, Huang CC, Lu WH, Chen YC, Tsai HH. Distribution of micro-motion in implants and alveolar bone with different thread profiles in immediate loading: A finite element study. Int J Oral Maxillofac Implants. 2012;27:e96–101. [PubMed] [Google Scholar]
- 4.Sakka S, Coulthard P. Implant failure: Etiology and complications. Med Oral Patol Oral Cir Bucal. 2011;16:e42–4. doi: 10.4317/medoral.16.e42. [DOI] [PubMed] [Google Scholar]
- 5.Pilliar RM, Lee JM, Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res. 1986;208:108–13. [PubMed] [Google Scholar]
- 6.Brunski JB. Avoid pitfalls of overloading and micro-motion of intra-osseous implants. Dent Implantol Update. 1993;4:77–81. [PubMed] [Google Scholar]
- 7.Søballe K, Hansen ES, Brockstedt-Rasmussen H, Bünger C. Hydroxyapatite coating converts fibrous tissue to bone around loaded implants. J Bone Joint Surg Br. 1993;75:270–8. doi: 10.1302/0301-620X.75B2.8444949. [DOI] [PubMed] [Google Scholar]
- 8.Friberg B, Ekestubbe A, Sennerby L. Clinical outcome of brånemark system implants of various diameters: A retrospective study. Int J Oral Maxillofac Implants. 2002;17:671–7. [PubMed] [Google Scholar]
- 9.Turkyilmaz I, Aksoy U, McGlumphy EA. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: A clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res. 2008;10:231–7. doi: 10.1111/j.1708-8208.2008.00084.x. [DOI] [PubMed] [Google Scholar]
- 10.Alghamdi H, Anand PS, Anil S. Undersized implant site preparation to enhance primary implant stability in poor bone density: A prospective clinical study. J Oral Maxillofac Surg. 2011;69:e506–12. doi: 10.1016/j.joms.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Summers RB. A new concept in maxillary implant surgery: The osteotome technique. Compendium. 1994;15:152–154-6. 158. [PubMed] [Google Scholar]
- 12.Boustany CM, Reed H, Cunningham G, Richards M, Kanawati A. Effect of a modified stepped osteotomy on the primary stability of dental implants in low-density bone: A cadaver study. Int J Oral Maxillofac Implants. 2015;30:48–55. doi: 10.11607/jomi.3720. [DOI] [PubMed] [Google Scholar]
- 13.Munjal S, Munjal S, Hazari P, Mahajan H, Munjal A, Mehta DS. Evaluation of specifically designed implants placed in the low-density jaw bones: A clinico-radiographical study. Contemp Clin Dent. 2015;6:40–3. doi: 10.4103/0976-237X.149290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abboud M, Delgado-Ruiz RA, Kucine A, Rugova S, Balanta J, Calvo-Guirado JL. Multi-stepped drill design for single-stage implant site preparation: Experimental study in Type 2 bone. Clin Implant Dent Relat Res. 2015;17:e472–85. doi: 10.1111/cid.12273. [DOI] [PubMed] [Google Scholar]
- 15.Huwais S, editor. Inventor; Fluted osteotome and surgical method for use.US Patent Application US2013/0004918; 3 January. 2013 [Google Scholar]
- 16.Huwais S, editor. Geneva, Switzerland: World Intellectual Property Organization Publication; 2014. Autografting Osteotome. WO2014/077920. [Google Scholar]
- 17.Lahens B, Neiva R, Tovar N, Alifarag AM, Jimbo R, Bonfante EA, et al. Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone: An experimental study in sheep. J Mech Behav Biomed Mater. 2016;63:56–65. doi: 10.1016/j.jmbbm.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Huwais S, Meyer EG. A novel osseous densification approach in implant osteotomy preparation to increase biomechanical primary stability, bone mineral density, and bone-to-implant contact. Int J Oral Maxillofac Implants. 2017;32:27–36. doi: 10.11607/jomi.4817. [DOI] [PubMed] [Google Scholar]
- 19.Dos Santos MV, Elias CN, Cavalcanti Lima JH. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res. 2011;13:215–23. doi: 10.1111/j.1708-8208.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- 20.Coelho PG, Granato R, Marin C, Teixeira HS, Suzuki M, Valverde GB, et al. The effect of different implant macro-geometries and surface treatment in early biomechanical fixation: An experimental study in dogs. J Mech Behav Biomed Mater. 2011;4:1974–81. doi: 10.1016/j.jmbbm.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 21.Elias CN, Oshida Y, Lima JH, Muller CA. Relationship between surface properties (roughness, wettability and morphology) of titanium and dental implant removal torque. J Mech Behav Biomed Mater. 2008;1:234–42. doi: 10.1016/j.jmbbm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Kim DR, Lim YJ, Kim MJ, Kwon HB, Kim SH. Self-cutting blades and their influence on primary stability of tapered dental implants in a simulated low-density bone model: A laboratory study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:573–80. doi: 10.1016/j.tripleo.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Bischof M, Nedir R, Szmukler-Moncler S, Bernard JP, Samson J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin Oral Implants Res. 2004;15:529–39. doi: 10.1111/j.1600-0501.2004.01042.x. [DOI] [PubMed] [Google Scholar]
- 24.Coelho PG, Jimbo R, Tovar N, Bonfante EA. Osseointegration: Hierarchical designing encompassing the macro-meter, micro-meter, and nano-meter length scales. Dent Mater. 2015;31:37–52. doi: 10.1016/j.dental.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Zitzmann NU, Schärer P. Sinus elevation procedures in the resorbed posterior maxilla: Comparison of the crestal and lateral approaches. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:8–17. doi: 10.1016/s1079-2104(98)90391-2. [DOI] [PubMed] [Google Scholar]
- 26.Büchter A, Kleinheinz J, Wiesmann HP, Kersken J, Nienkemper M, Weyhrother Hv, et al. Biological and biomechanical evaluation of bone remodelling and implant stability after using an osteotome technique. Clin Oral Implants Res. 2005;16:1–8. doi: 10.1111/j.1600-0501.2004.01081.x. [DOI] [PubMed] [Google Scholar]
- 27.Cortes AR, Cortes DN. Non-traumatic bone expansion for immediate dental implant placement: An analysis of 21 cases. Implant Dent. 2010;19:92–7. doi: 10.1097/ID.0b013e3181d46f46. [DOI] [PubMed] [Google Scholar]
- 28.Mazzocco F, Nart J, Cheung WS, Griffin TJ. Prospective evaluation of the use of motorized ridge expanders in guided bone regeneration for future implant sites. Int J Periodontics Restorative Dent. 2011;31:547–54. [PubMed] [Google Scholar]
- 29.Lee EA, Anitua E. Atraumatic ridge expansion and implant site preparation with motorized bone expanders. Pract Proced Aesthet Dent. 2006;18:17–22. [PubMed] [Google Scholar]


