Abstract
Retrograde intrarenal surgery (RIRS) is nowadays more and more indicated in pyelocaliceal stones. Holmium and Thulium lasers are the main lasers used. Fragmenting (basketing) or dusting, despite the new technology, still have residual stones (even having 250 microns). This study evaluates second-look flexible ureteroscopy for residual fragments. We analyzed 246 patients (October 2020–March 2022) on which we used Moses Holmium technology (187 cases) in Group 1 and Soltive Laser System (59 cases) in Group 2. The average stone size was 13.1 mm (range 11–29), and the average stone density was 1026 HU (range 870–1752). We used 270 µm for Ho: YAG laser and 150 µm for TFL. For Holmium, we applied energy 0.4J and frequency 80 Hz. For TFL, we applied fine dusting (0.15 J/100 Hz) and dusting (0.5 J/30 Hz). After three months, we practiced the second flexible ureteroscopy. Both groups were compared for completely visual stone-free rates. Stone-free rate at 3 months (second flexible ureteroscopy) was 86.63% (n=162/187) in Group 1 and 96,61% (n=57/59) in Group 2, respectively. The stone-free correlation with the CT preoperative evaluation was 160/187–85.56% for Holmium and 55/59–93.22% for TFL. We found residual stones after the second flexible ureteroscopy in 25 cases after Holmium laser treatment and only in 2 cases after TFL. In all these cases, we finally obtained zero residual stones. The second flexible ureteroscopy could achieve complete residual stone removal and real stone-free status. Despite a slight difference between these two laser technologies, the second look decreases the residual fragments.
Keywords: retrograde intrarenal surgery, second-look flexible ureteroscopy, residual stone fragments
INTRODUCTION
Urolithiasis represents a common finding in the general population, affecting approximately 12% of the world population during their lifetime [1], with continuous increasing prevalence and recurrence rates yearly [2]. Although men are more affected than women, with the highest incidence between 20 and 50 years old, it can occur regardless of age and sex [3, 4]. Most urinary stones are located in the kidney, requiring different interventions. The introduction of the extracorporeal shock wave lithotripsy (ESWL) in the 1980s has revolutionized the modern minimally invasive stone treatment, and ever since, together with percutaneous nephrolithotomy (PCNL) has significantly decreased the need for open surgery while achieving stone-free rates of up to 80% [5, 6]. The continuous evolution and modernization of flexible endoscopes have promoted retrograde intrarenal surgery (RIRS) among the most frequent minimally-invasive procedure for most cases of kidney stones, according to both European [7] and American [8] guidelines on urolithiasis with promising results on stone-free rates [9, 10] and perioperative related morbidity [11].
The miniaturization of instruments and technological advances in image quality, maneuverability and laser lithotripsy systems have endorsed RIRS as a safe and efficient method of treatment for intrarenal stones [12, 13]. The actual gold standard of laser (light activation by the stimulated emission of radiation) technology in renal stone lithotripsy is HO: YAG (Holmium: Yttrium-Aluminum-Garnet) [14, 15], with three decades of demonstrating clinical potential and safeness in flexible endoscopic procedures [16]. New technology has emerged recently, with promising preliminary results on stone fragmentation and overall performance: Thulium fiber laser [17–19]. In mid-summer 2020, OlympusTM launched the Solvite SuperPulsed Thulium Fiber Laser System for clinical application in endourology, with general availability and favorable results presented by several authors [20, 21].
The objective of laser lithotripsy in renal stones is to safely fragment stones into smaller parts (fragments-basketing) which can be easily extracted with various probes, or completely fragmenting the stones in "dust", which is defined as particles smaller than 250 µm on floating and sedimentation criteria and which can be easily evacuated on the ureteroscope's working channel, achieving the stone-free status [22, 23]. The latter was defined as no stones or residual stones of less than 2–4 mm on postoperative control KUB or non-contrast enhanced computed tomography [24, 25]. Different imaging techniques have been proposed to determine the success of stone fragmentation after various urological stone-related procedures, such as ultrasound, renal radiography and computed tomography. Recently, the idea of a second-look ureteroscopy procedure has emerged to evaluate the pyelocaliceal system for accurate visualization and certainty of an actual stone-free status [26, 27] and, if not already achieved, to serve as a supplementary curative technique in definitive stone treatment.
Considering the importance of achieving a good stone-free status, whenever it can be achieved, to decrease other post interventional stone-related events, this study aimed to determine the efficacy of a second-look ureteroscopy for a real analysis of residual fragments after dusting lithotripsy using both Holmium and Thulium laser fibers.
Material and methods
A retrospective analysis of 246 patients who underwent retrograde flexible ureteroscopy for pyelocaliceal stones was conducted between October 2020 and March 2022 at the Urology Department from Sf. Ioan Emergency Hospital in Bucharest, Romania. In 187 cases, Moses Holmium laser technology (distance mode) was used as laser lithotripsy (Group 1), while in 59 cases Soltive Laser system using Thulium laser fiber was the choice for stone dusting. In all cases, dusting and fine dusting were the pre-setting of frequency and energy of the laser systems. A detailed representative diagram of patients included in the study, along with the specific type of laser lithotripsy used for each group of patients, is represented in Figure 1.
Figure 1.
Group-patient diagram and modalities of treatment.
In all cases, a CT urography (urography – CT) was conducted to evaluate the anatomy of the renourinary system and determine the stone density. The average stone size was 13.1 mm (ranging between 11–29 mm, measured as the longest dimension on imaging visualization) with a mean density of 1026 HU (range between 870–1752 HU).
The exclusion criteria were abnormalities of the renourinary system, incomplete data on stone type and loss of follow-up patients, cases where flexible ureteroscopy was performed by different surgeons and cases where incomplete stone dusting was performed due to intraoperative complications (e.g. bleeding followed by poor visualization).
All interventions were performed by a single, experienced surgeon with over 5000 flexible ureteroscopies performed on patients under general anesthesia. Sterile urine culture was mandatory in all cases before every procedure, and antibiotic prophylaxis was performed with a single-dose second-generation cephalosporin. All patients were previously catheterized with a Double J stent extracted at the beginning of the procedure. A ureteral access sheath was placed to facilitate access to the renal pelvis. All procedures were performed with reusable flexible ureteroscopes from Pussen (Pussen PU3033 A 7.5 Fr and Pussen 3022 9.5 Fr). In Group 1, the laser lithotripsy was performed with Moses Holmium technology, using a standard 270 µm laser fiber. In Group 2, the Soltive Laser System was used with a Thulium laser fiber of 150 µm. A Dormia basket probe was used to extract stones whenever larger fragments occurred. At the end of the procedure, a 6 Fr Double J stent was placed to avoid any obstructive postoperative complications due to residual stone fragments, steinstrasse or blood clots from bleeding. All the extracted stone fragments were sent for analysis for a complete metabolic evaluation and recurrence prevention.
The second-look flexible ureteroscopy was performed after 3 months to evaluate the pyelocaliceal system for residual stones. A CT scan was performed preoperatively for all symptomatic patients (renal colic, flank pain) to evaluate the possible residual stones. An auxiliary laser lithotripsy procedure was performed for any stone fragment larger than 1 mm to achieve a true stone-free status. In none of these cases, ureteral sheets were used, and no Double J stent was inserted. Each patient was informed about the procedures and other alternative surgical and/or medical treatment modalities. Patients chose the surgical approach after counseling with the surgeon.
Data were analyzed using Microsoft Excel software (Microsoft Corporation, Redmond, WA, USA). Simple descriptive statistics were calculated. The relationship of variables was analyzed using frequency and percentage.
Results
A total of 246 patients were included in this study; demographic information for each selected patient, such as age, sex, body mass index (BMI), and location of the stone, was registered. The mean age was relatively similar in both groups Group 1 – 47.51 and Group 2 – 48.94, while the BMI value showed overweight patients in both groups, as follows Group 1 – 26.83 (range from 18 to 37), while in Group 2 – 25.05 (range from 20 to 37). A higher predilection was observed for male patients in both groups Group 1 – 56.14%, Group 2 – 54.23%, compared to female patients, Group 1 – 43.85%, Group 2 – 45.76%. The right-side location of stones was a more common finding, 57.75% and 69.49% respectively, compared to the left side (42.24% and 30.5%, respectively). More detailed information on the demographic characteristics of both groups is represented in Table 1.
Table 1.
Demographic information of the studied groups.
| Age (years) | BMI (kg/m2) | Female | Male | Left side | Right side | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | n | % | n | % | n | % | n | % | n | % | |
| Group 1 | 47.51 | 14.72 | 26.83 | 3.32 | 82 | 43.85 | 105 | 56.14 | 79 | 42.24 | 108 | 57.75 | 187 | 76.01 |
| Group 2 | 48.94 | 15.93 | 25.05 | 4.06 | 27 | 45.76 | 32 | 54.23 | 18 | 30.5 | 41 | 69.49 | 59 | 23.98 |
| Total | 47.85 | 15.02 | 26.90 | 3.29 | 109 | 44.3 | 137 | 55.69 | 97 | 39.43 | 149 | 60.56 | - | - |
The dimensions of stones were relatively similar in both of the selected groups, with a mean value of 13.1 mm. The stone density was slightly higher in the Thulium group, representing a mean value of 1045.1 HU, compared with the Holmium laser group, which accounted for a mean value of 1020.45 HU. An overall mean of 1026.36 HU in the entire study was determined. In all cases, small fragments or stone dust was sent for the biochemical study of stone composition. The most frequent lithiasis type was calcium oxalate, encountered in 148 (79.14%) cases in Group 1 and 41 (69.49%) in Group 2. It was followed by calcium phosphate: 28 (14.97%) in Group 1 and 15 (25.42%) in Group 2 and uric acid stones, which were encountered in 9 cases (4.81%) in Group 1 and 3 (5.08%) in Group 2. The least common stone type was cystine stones encountered in 2 cases (1.06%) in Group 1. A more detailed representation of stone-related clinical data is represented in Table 2.
Table 2.
Stone-related clinical data.
| Stone characteristics | Stone composition | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stone size (mm) | Stone density (HU) | Calcium oxalate | Calcium phosphate | Uric acid | Cystine | |||||||
| Mean | SD | Mean | SD | n | % | n | % | n | % | n | % | |
| Group 1 | 13.05 | 3.27 | 1020.45 | 110.85 | 148 | 79.14 | 28 | 14.97 | 9 | 4.81 | 2 | 1.06 |
| Group 2 | 13.25 | 4.74 | 1045.1 | 109.19 | 41 | 69.49 | 15 | 25.42 | 3 | 5.08 | - | - |
| Total | 13.1 | 3.66 | 1026.36 | 110.73 | 189 | 76.82 | 43 | 17.47 | 12 | 4.87 | 2 | 0.81 |
The mean operative time was relatively similar in the Holmium laser Group 1 – 66.14 min, compared to the Thulium laser Group 2 – 64.06 min (Table 3). The overall mean operative time in the entire study was 65.65 min (range 45–90 min). Regarding postoperative complications, hematuria was the most frequent symptom encountered for 12 cases (6.41%) in Group 1 and 4 (6.77%) in Group 2. Other less frequent postoperative complications were noted as fever, which was encountered for 6 cases (3.2%) in Group 1 and 3 cases (5.08%) in Group 2 and renal colic, which was encountered for only 1 case (0.53%) in Group 1. All data presented were registered for the first main intervention; the mean operative time was much lower in the second-look RIRS, and no postoperative events were encountered after the second intervention. All postoperative complications after the first intervention were graded as Grade 1 or Grade 2 on Clavien-Dindo Classification System and were treated conservatory for a maximum of 3 days; no additional surgical or endoscopic procedures were required.
Table 3.
Operative time and perioperative events.
| Operative time (min) | Postoperative events | |||||||
|---|---|---|---|---|---|---|---|---|
| Hematuria | Fever | Renal colic | ||||||
| Mean | SD | n | % | n | % | n | % | |
| Group 1 | 66.14 | 13.62 | 12 | 6.41 | 6 | 3.2 | 1 | 0.53 |
| Group 2 | 64.06 | 15.01 | 4 | 6.77 | 3 | 5.08 | - | - |
| Total | 65.65 | 13.96 | 16 | 6.5 | 8 | 3.25 | 1 | 0.4 |
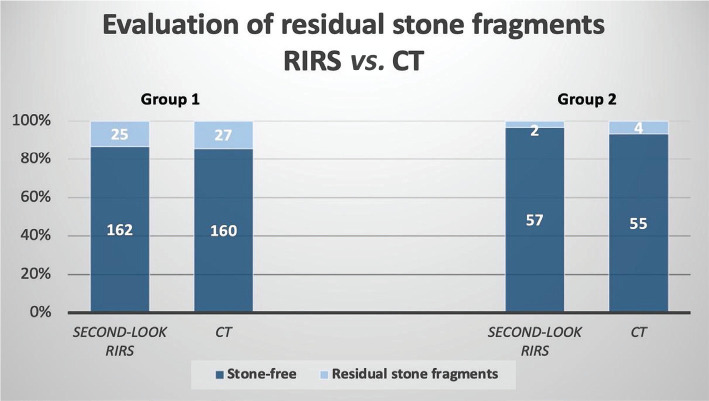
All symptomatic patients underwent a non-contrast-enhanced CT to evaluate the residual fragments after the first intervention. After 3 months, a second-look flexible ureteroscopy was performed to assess the "true" stone-free status. In Group 1 (holmium laser), imaging investigations determined 160 cases out of 187 as stone-free (85.56%). In contrast, in Group 2 (Thulium laser), 55 of the 59 patients were considered stone-free (93.22%). Subsequently, all of these patients underwent a second flexible ureteroscopy which revealed better "real stone-free" status than imaging investigations. Thus, in Group 1, out of 187 patients, 162 were diagnosed as stone-free visually, representing 86.63%, while in Group 2 – 57 of the 59 patients did not show any residual fragment (96.61%) after the second intervention, highlighting a better evaluation of the true stone-free status after a close visualization of the pyelocaliceal system using flexible ureteroscopy. A visual diagram of both groups comparing stone-free rates and residual fragments by both imaging and interventional evaluation is represented in Figure 2.
Figure 2.
Comparing stone-free rates and residual fragments evaluation by flexible ureteroscopy and computer tomography in both groups (*RIRS – retrograde intrarenal surgery; CT – computer tomography).
Discussion
Nephrolithiasis is a severe, recurrent condition that affects up to 10% of the adult population in the European Union annually [28]. The European Association of Urology recommends RIRS as a first-line treatment in kidney stones with dimensions between 1 and 2 cm, representing a significant volume of cases [7]. Laser technology has revolutionized the lithotripsy of kidney stones, representing the standard management in flexible ureteroscopy, with high-performance Holmium-type lasers able to exceed the recommended size and operate large kidney stones with good patient results [29]. Furthermore, the introduction of the Thulium laser in modern endourology seems to further revolutionize the management of kidney stones with superior results regarding stone dusting and postoperative stone-free status. The results of this study are similar to the data in the literature, obtaining over 90% stone-free rates in the second group, the one that uses the Thulium laser and over 85% in the first group, corresponding to the Holmium laser [30, 31].
Demographic factors play an important role in the development and evolution of kidney stones. The mean age of the incidence of kidney stones in the present study group was around 50 years of age, probably considering the known risk factors that occur, such as dietary factors, recurrent urinary tract infections and body weight; the effect of aging on lithiasis has been studied [32]. Most patients who presented stones in the study group were overweight, averaging approximately 27 kg/m2. Studies in obese patients with urinary stones have shown variable risk factors, such as urinary pH, systemic inflammation and oxidative stress being the primary places as having a negative influence on the prevalence of this pathology [33]. In the present study, both groups determined the highest incidence of kidney stones among the male population (55.7% vs. 44.3%). Recent studies show a changing trend in the incidence of lithiasis in relation to gender, with a significant increase in this disease among the female population, especially during adolescence [34]. Also, the risk of developing chronic kidney disease (CKD) is higher for female patients, so this pathology must be treated with higher caution [35].
The size of the calculus is a very important aspect of obtaining a stone-free outcome. With the advancement of laser lithotripsy technology in flexible ureteroscopy, the indication of stone dusting of voluminous stones acquires a more accentuated contour. The average size of the stones in the current study was 13.1 mm. Data from the literature suggest the possibility of managing large stones or difficult cases with promising results in the stone-free rates of the patient after the intervention [36–39] and even performing flexible ureteroscopy for staghorn stones in selected cases [40, 41]. In the present study, the mean density of the stones (measured in Hounsfield units at the CT examination) was 1026.36 HU. The most common type of stone was calcium oxalate (76.8%), followed by calcium phosphate (17.47%), uric acid (4.87%) and cystine (0.81%). A large study in the United States showed similar rates in the prevalence of matrix types that make up kidney stones, with a major predominance of calcium oxalate monohydrate and calcium phosphate, accounting for over 93% of their components [42].
The average operative time was 65 minutes, and the postoperative incidents were mostly represented by hematuria, fever and renal colic. These complications are among the most common in this endourological procedure, with data from the literature showing relatively similar prevalence rates [43, 44]. There were no major complications, such as perforation or ureteral avulsion, significant bleeding that required blood transfusion or sepsis in the postoperative period, these incidents being known to be among the most serious complications [45].
Computed tomography (CT) is the best imaging investigation for diagnosing and following patients with kidney stones. The sensitivity and specificity of this radiological investigation are approximately 95%. In a few cases, especially when the size of the stones is <3 mm, they can escape radiological detection and cannot be observed by this investigation [46]. Except for a few cases, such as indinavir stones or matrix proteases, all types of stones are seen on CT [47]. However, there are exceptional situations when various pathologies associated with the kidney can be confused with kidney stones. These elements of confusion with urinary stones include Randall's plaque, calcifications of the papilla or renal mucosa, or isolated cases of nephrocalcinosis [48]. These elements of calcification may be a reason for misinterpretation of spiral CT images in a patient known to have kidney stones and who is being monitored after surgery. The CT evaluation of the operated patients in this study showed a small number of patients – 2 cases in Group 1 and 2 cases in Group 2 in which the CT examination revealed the existence of post interventional residual lithiasis. Still, subsequent endoscopic investigation denied their presence during the extensive and thorough pyelocalicoscopy examination.
An important limitation of this study is the small number of patients. A higher number of patients could prove an even greater significance of the second look ureteroscopy or, in turn, disprove this percentage of false-positive imaging results in the diagnosis of residual kidney stones. Another limitation is that the study was developed in a single center, and a single experienced surgeon performed all interventions. These premises may represent the pioneer of a larger future study involving more patients from different centers and interventions performed by surgeons with variable experience for better results and to draw definitive conclusions.
Conclusion
Following the consistent assessment of all patients after flexible ureteroscopy by systematic CT evaluations of endoscopic control and re-evaluation of the pyelocaliceal system, this study demonstrates that direct, optical and modern endoscopic visualization is superior to imaging investigations in detecting residual fragments after stone lithotripsy. This is the only feasible tool to determine the "true" stone-free rate condition after endourological interventions of urinary stones.
Acknowledgments
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the ethics committee of the Sanador Hospital and Sf. Ioan Emergency Clinical Hospital, Bucharest, and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments (9419/19.04.2022).
Consent to participate
Informed written consent was provided by each participant.
Authorship
PG and CM contributed to conceptualization. BG and CM contributed to the methodology. RM, DG contributed to validation. CM, PG, DG and RM contributed to the investigation. CM and RM contributed to resources. CM and PG contributed to writing and original draft preparation. BG, CM and PG contributed to writing, review and editing. BG, RM and DG contributed to visualization. BG and PG contributed to supervision. All authors read and agreed to the published version of the manuscript.
References
- 1.Chauhan CK, Joshi MJ, Vaidya ADB. Growth inhibition of struvite crystals in the presence of herbal extract Commiphora. Journal of Materials Science. 2008;20(1):85–92. doi: 10.1007/s10856-008-3489-z. [DOI] [PubMed] [Google Scholar]
- 2.Knoll T. Epidemiology, pathogenesis and pathophysiology of urolithiasis. European Urology Supplements. 2010;9(12):802–806. doi: 10.1016/j.eursup.2010.11.006. [DOI] [Google Scholar]
- 3.Edvardsson VO, Indridason OS, Haraldsson G, Kjartansson O, Palsson R. Temporal trends in the incidence of kidney stone disease. Kidney International. 2013;83(1):146–152. doi: 10.1038/ki.2012.320. [DOI] [PubMed] [Google Scholar]
- 4.Moe OW. Kidney stones: pathophysiology and medical management. The Lancet. 2006;367(9507):333–344. doi: 10.1016/s0140-6736(06)68071-9. [DOI] [PubMed] [Google Scholar]
- 5.Chaussy CG, Fuchs GJ. Current state and future developments of noninvasive treatment of human urinary stones with extracorporeal shock wave lithotripsy. J Urol. 1989 Mar;141(3 Pt 2):782–9. doi: 10.1016/s0022-5347(17)41010-x. [DOI] [PubMed] [Google Scholar]
- 6.Deem S, Defade B, Modak A, Emmett M, et al. Percutaneous nephrolithotomy versus extracorporeal shock wave lithotripsy for moderate sized kidney stones. Urology. 2011 Oct;78(4):739–43. doi: 10.1016/j.urology.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Türk C, Neisius A, Petřík A, Seitz C, et al. European Association of Urology 2021. the Netherlands: Arnhem; 2021. EAU Guidelines on Urolithiasis. [Google Scholar]
- 8.Assimos D, Krambeck A, Miller NL, Monga M, et al. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART II. J Urol. 2016 Oct;196(4):1161–9. doi: 10.1016/j.juro.2016.05.091. [DOI] [PubMed] [Google Scholar]
- 9.Reddy TG, Assimos DG. Optimizing Stone-free Rates With Ureteroscopy. Rev Urol. 2015;17(3):160–4. [PMC free article] [PubMed] [Google Scholar]
- 10.Ghani K, Wolf J. What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat Rev Urol. 2015;12:281–288. doi: 10.1038/nrurol.2015.74. [DOI] [PubMed] [Google Scholar]
- 11.Somani BK, Giusti G, Sun Y, Osther PJ, et al. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: the Clinical Research Office of Endourological Society URS Global study. World journal of urology. 2017;35(4):675–681. doi: 10.1007/s00345-016-1909-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alenezi H, Denstedt JD. Flexible ureteroscopy: Technological advancements, current indications and outcomes in the treatment of urolithiasis. Asian J Urol. 2015;2(3):133–141. doi: 10.1016/j.ajur.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alexander B, Fishman AI, Grasso M. Ureteroscopy and laser lithotripsy: technologic advancements. World J Urol. 2015 Feb;33(2):247–56. doi: 10.1007/s00345-014-1402-6. [DOI] [PubMed] [Google Scholar]
- 14.Terry RS, Whelan PS, Lipkin ME. New devices for kidney stone management. Curr Opin Urol. 2020 Mar;30(2):144–148. doi: 10.1097/MOU.0000000000000710. [DOI] [PubMed] [Google Scholar]
- 15.Fried NM, Irby PB. Advances in laser technology and fibre-optic delivery systems in lithotripsy. Nat Rev Urol. 2018 Sep;15(9):563–573. doi: 10.1038/s41585-018-0035-8. [DOI] [PubMed] [Google Scholar]
- 16.Denstedt JD, Razvi HA, Sales JL, Eberwein PM. Preliminary experience withHolmiumm: YAG laser lithotripsy. J Endourol. 1995 Jun;9(3):255–8. doi: 10.1089/end.1995.9.255. [DOI] [PubMed] [Google Scholar]
- 17.Traxer O, Rapoport L. Tsarichenko D V03-02 first clinical study on superpulse thulium fiber laser for lithotripsy. J Urol. 2018;199(4):e321–e322. [Google Scholar]
- 18.Kronenberg P, Somani B. Advances in Lasers for the Treatment of Stones-a Systematic Review. Curr Urol Rep. 2018 May 17;19(6):45. doi: 10.1007/s11934-018-0807-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Traxer O, Keller EX. Thulium fiber laser: the new player for kidney stone treatment? A comparison with Holmium:YAG laser. World J Urol. 2020 Aug;38(8):1883–1894. doi: 10.1007/s00345-019-02654-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olympus Olympus Launches the Soltive SuperPulsed Thulium Fiber Laser System for Urology, Launched. 2020. Jun 17, Available from: https://www.olympus-europa.com/company/en/news/press-releases/2020-06-17t08-50-00/olympus-launches-the-soltive-superpulsed-thulium-fiber-laser-system-for-urology.html.
- 21.Traxer O, Corrales M. Managing Urolithiasis with Thulium Fiber Laser: Updated Real-Life Results-A Systematic Review. J Clin Med. 2021;10(15):3390. doi: 10.3390/jcm10153390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keller EX, De Coninck V, Doizi S, Daudon M, Traxer O. What is the exact definition of stone dust? An in vitro evaluation. World J Urol. 2021 Jan;39(1):187–194. doi: 10.1007/s00345-020-03178-z. [DOI] [PubMed] [Google Scholar]
- 23.Santiago JE, Hollander AB, Soni SD, Link RE, Mayer WA. To Dust or Not To Dust: a Systematic Review of Ureteroscopic Laser Lithotripsy Techniques. Curr Urol Rep. 2017 Apr;18(4):32. doi: 10.1007/s11934-017-0677-8. [DOI] [PubMed] [Google Scholar]
- 24.Bhat A, Singh V, Bhat M, Khandelwal N, Bhat A. Comparison of antegrade percutaneous versus retrograde ureteroscopic lithotripsy for upper ureteric calculus for stone clearance, morbidity, and complications. Indian J Urol. 2019 Jan-Mar;35(1):48–53. doi: 10.4103/iju.IJU_89_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rippel CA, Nikkel L, Lin YK, Danawala Z, et al. Residual fragments following ureteroscopic lithotripsy: incidence and predictors on postoperative computerized tomography. J Urol. 2012 Dec;188(6):2246–51. doi: 10.1016/j.juro.2012.08.040. [DOI] [PubMed] [Google Scholar]
- 26.Cebeci OÖ, Özkan TA, Yalçın MS, Dillioğlugil Ö, Çevik İ. Effectiveness of Second-look Flexible Ureteroscopy to Achieve A True Stone-Free Status in Retrograde Intrarenal Surgery. J Urol Surg. 2022;9:40–46. [Google Scholar]
- 27.Cebeci OO, Özkan TA, Yalcin MS, Dillioglugil O, Cevik I. Second-Look Flexible Ureterorenoscopy: A Technique Proposal to Achieve Real Stone Free Status. Authorea. 2021 January 22; doi: 10.22541/au.161131535.53003454/v1. [DOI] [Google Scholar]
- 28.Talati J, Tiselius HG, Albala D, YE Z, editors. Urolithiasis. London: Springer; 2012. Osther PJS Epidemiology of Kidney Stones in the European Union. [DOI] [Google Scholar]
- 29.Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG. Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater--is this the new frontier? J Urol. 2008 Mar;179(3):981–4. doi: 10.1016/j.juro.2007.10.083. [DOI] [PubMed] [Google Scholar]
- 30.Ulvik Ø, Æsøy MS, Juliebø-Jones P, Gjengstø P, Beisland C. Thulium Fibre Laser versus Holmium:YAG for Ureteroscopic Lithotripsy: Outcomes from a Prospective Randomised Clinical Trial. Eur Urol. 2022 Jul;82(1):73–79. doi: 10.1016/j.eururo.2022.02.027. [DOI] [PubMed] [Google Scholar]
- 31.Geavlete B, Multescu R, Iordache V, Geavlete P. Romanian National premiere with the new Thulium SuperPulsed Laser in the endourological treatment of urolithiasis. J Med Life. 2021;14(3):316–322. doi: 10.25122/jml-2021-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krambeck AE, Lieske JC, Li X, Bergstralh EJ, et al. Effect of age on the clinical presentation of incident symptomatic urolithiasis in the general population. J Urol. 2013;189(1):158–164. doi: 10.1016/j.juro.2012.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poore W, Boyd CJ, Singh NP, Wood K, et al. Obesity and Its Impact on Kidney Stone Formation. Rev Urol. 2020;22(1):17–23. [PMC free article] [PubMed] [Google Scholar]
- 34.Gillams K, Juliebø-Jones P, Juliebø SØ Somani BK. Gender Differences in Kidney Stone Disease (KSD): Findings from a Systematic Review. Curr Urol Rep. 2021;22(10):50. doi: 10.1007/s11934-021-01066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gambaro G, Croppi E, Bushinsky D, Jaeger P, et al. The Risk of Chronic Kidney Disease Associated with Urolithiasis and its Urological Treatments: A Review. J Urol. 2017 Aug;198(2):268–273. doi: 10.1016/j.juro.2016.12.135. [DOI] [PubMed] [Google Scholar]
- 36.Riley JM, Stearman L, Troxel S. Retrograde ureteroscopy for renal stones larger than 2.5 cm. J Endourol. 2009 Sep;23(9):1395–8. doi: 10.1089/end.2009.0391. [DOI] [PubMed] [Google Scholar]
- 37.Geraghty RM, Ishii H, Somani BK. Outcomes of flexible ureteroscopy and laser fragmentation for treatment of large renal stones with and without the use of ureteral access sheaths: Results from a university hospital with a review of literature. Scand J Urol. 2016 Jun;50(3):216–9. doi: 10.3109/21681805.2015.1121407. [DOI] [PubMed] [Google Scholar]
- 38.Huang JS, Xie J, Huang XJ, Yuan Q, et al. Flexible ureteroscopy and laser lithotripsy for renal stones 2 cm or greater: A single institutional experience. Medicine (Baltimore) 2020 Oct 23;99(43):e22704. doi: 10.1097/MD.0000000000022704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arslan F, Ergun O, Kosar A, Yavuz AH. Results of minimally invasive surgical treatment of allograft lithiasis in live-donor renal transplant recipients: a single-center experience of 3758 renal transplantations. Urolithiasis. 2019 Jun;47(3):273–278. doi: 10.1007/s00240-018-1051-0. [DOI] [PubMed] [Google Scholar]
- 40.Keller EX, De Coninck V, Doizi S, Traxer O. The role of ureteroscopy for treatment of staghorn calculi: A systematic review. Asian J Urol. 2020 Apr;7(2):110–115. doi: 10.1016/j.ajur.2019.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Niwa N, Matsumoto K, Ohigashi T. Clinical Outcomes of Retrograde Intrarenal Surgery as a Primary Treatment for Staghorn Calculi: A Single-Center Experience. Clinical Medicine Insights: Urology. 2019 January;12 doi: 10.1177/1179561119854772. [DOI] [Google Scholar]
- 42.Grant C, Guzman G, Stainback RP, Amdur RL, Mufarrij P. Variation in Kidney Stone Composition Within the United States. J Endourol. 2018 Oct;32(10):973–977. doi: 10.1089/end.2018.0304. [DOI] [PubMed] [Google Scholar]
- 43.Cruz-Ruíz J, Negrete-Pulido OR, Méndez-Probst CE. Complications of retrograde ureteroscopy. Prevention, early recognition, and treatment. Revista mexicana de urología. 2021;78(3):233–242. doi: 10.24245/revmexurol.v78i3.1944. [DOI] [Google Scholar]
- 44.de la Rosette J, Denstedt J, Geavlete P, Keeley F, et al. CROES URS Study Group. The clinical research office of the endourological society ureteroscopy global study: indications complications and outcomes in 11,885 patients. J Endourol. 2014 Feb;28(2):131–9. doi: 10.1089/end.2013.0436. [DOI] [PubMed] [Google Scholar]
- 45.Almusafer M, Jawad Al-Tawri AM. Complications of ureteroscopic stone lithotripsy: A multicentre local study. Hamdan Med J. 2019;12:119–25. doi: 10.4103/HMJ.HMJ_73_18. [DOI] [Google Scholar]
- 46.Coursey CA, Casalino DD, Remer EM, Arellano RS, et al. ACR Appropriateness Criteria® acute onset flank pain--suspicion of stone disease. Ultrasound Q. 2012 Sep;28(3):227–33. doi: 10.1097/RUQ.0b013e3182625974. [DOI] [PubMed] [Google Scholar]
- 47.Schwartz BF, Schenkman N, Armenakas NA, Stoller ML. Imaging characteristics of indinavir calculi. J Urol. 1999 Apr;161(4):1085–7. [PubMed] [Google Scholar]
- 48.Chi T, Miller J, Stoller ML. Randall plaque versus renal stone? Transl Androl Urol. 2012;1(1):66–70. doi: 10.3978/j.issn.2223-4683.2011.12.06. [DOI] [PMC free article] [PubMed] [Google Scholar]