Abstract
The retroperitoneum (RP) might be affected by a variety of infections, inflammations, and tumors, including benign and malignant ones. Although primary malignant tumors are the most prevalent ones in this anatomic area, metastatic and invasive tumors rarely involve the retroperitoneum. Gastrointestinal stromal tumors (GISTs) are considered as the most common tumors that invade the retroperitoneum, but, to the best of our knowledge, it is the first time a surgery team has encountered the appendiceal tumor as a huge retroperitoneal mass. A 68‐year‐old man was referred to the emergency department with abdominal distension and weight loss. In his course of hospitalization, a huge right retroperitoneal mass was detected by a computed tomography (CT) scan; after that, the patient underwent laparotomy, evacuation of massive mucinous tissue located in the right retroperitoneum, and right hemicolectomy due to appendiceal tumor. The histopathological examination showed “mucinous appendiceal neoplasm.” This is the first case study showing the invasion of an appendiceal tumor through the visceral peritoneum into the retroperitoneum, so an invasion of the peritoneal tumor to the retroperitoneum should be considered when a urologist approaches retroperitoneal masses.
Keywords: appendiceal tumor, multiloculated mucinous collection, retroperitoneal mass
1. BACKGROUND
The retroperitoneum (RP) might be affected by a variety of infections, inflammations, rare benign tumors, or malignant neoplasms that can be either primary or metastatic. Malignant tumors of the retroperitoneum happen four times more frequently than benign lesions. 1 , 2
Benign retroperitoneal tumors (RPT) are usually detected clinically, and the most common one is neurogenic tumors (30%), followed by teratomas (15%). However, malignant RPTs are very rare tumors, accounting for 0.1%–0.2% of all malignant tumors. 3 Most of them are primary tumors arising from the mesodermal system; the most common type is liposarcoma, but metastatic tumors may also involve the retroperitoneum. 3 , 4 When considering urologic malignancies, metastatic RPTs may originate from the kidney, bladder, or genitalia. 5
Invasion of malignant tumors to the retroperitoneal is very rare and has usually been reported as an unusual presentation of gastrointestinal stromal tumors (GISTs). 6 , 7 On the contrary, appendiceal tumors are rare and usually manifest as appendicitis. Most are harmless and can be handled with appendectomy. 8 The World Health Organization (WHO) classifies three subtypes of mucinous appendiceal neoplasms: mucinous adenoma, low‐grade appendiceal mucinous neoplasm (LAMN), and mucinous adenocarcinoma. 9 This case report presents a novel case of an appendix tumor that manifested with retroperitoneal mass by invasion from the peritoneal cavity.
2. CASE PRESENTATION
A 68‐year‐old male patient without any underlying diseases was admitted to the general surgery department with weight loss which started from 6 months before admission and slow progressive abdominal distention and abdominal pain about 2 weeks before admission. The pattern of pain was constant, but it switched from the vague to the sharp type about 2 days before admission. The patient had a negative history of neurologic symptoms, fever, hematuria, gastrointestinal bleeding, and constipation. During the physical examination, significant distention and a palpable mass in the periumbilical area above the pelvic cavity with expansion to the right side were identified. There was no tenderness or guarding in the abdomen. In the laboratory data, no leukocytosis (white blood cells: 7300) but mild anemia (hemoglobin: 12.5 mg/dl) was found. Urine analysis and renal and liver function tests were in the normal range. Spiral computed tomography (CT) of the abdomen and pelvic region revealed a normal right kidney displaced by a large cystic lesion in the retroperitoneum on the right side, with a multiloculated cystic appearance and infiltrating the right psoas muscle. It extended inferiorly to the level of the right side of the lower abdomen and pelvic cavity. Also, it had a pressure effect on the adjacent part of the urinary bladder (Figure 1).
FIGURE 1.
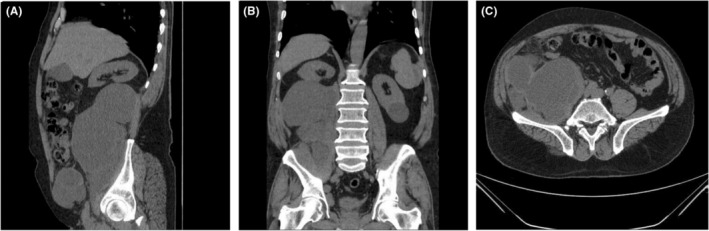
(A–C) Spiral computed tomography of the abdomen and pelvic
On the 3rd day of admission, the patient underwent exploratory laparotomy due to intractable abdominal pain by the urology and general surgery teams. Laparotomy was done through midline incision, and after the incision of the white line of Toldt, the right retroperitoneum was explored. The appendix tumor which invaded the visceral peritoneum was found. Then, the general surgery team dissected, divided, and removed the appendix from the retroperitoneum. Right hemicolectomy was done from 10 cm before the ileocecal valve up to the mid transverse colon. An end‐to‐end ileocolic anastomosis was performed. In addition, the multiloculated mucinous collection was drained, and the resected tissue was sent for pathology laboratory. Postoperative histopathological analyses revealed that the tumor size was 4 × 2.5 × 1 cm, and the tumor type was mucinous appendiceal neoplasm. However, no metastasis or lymph node involvement was detected (Figure 2).
FIGURE 2.
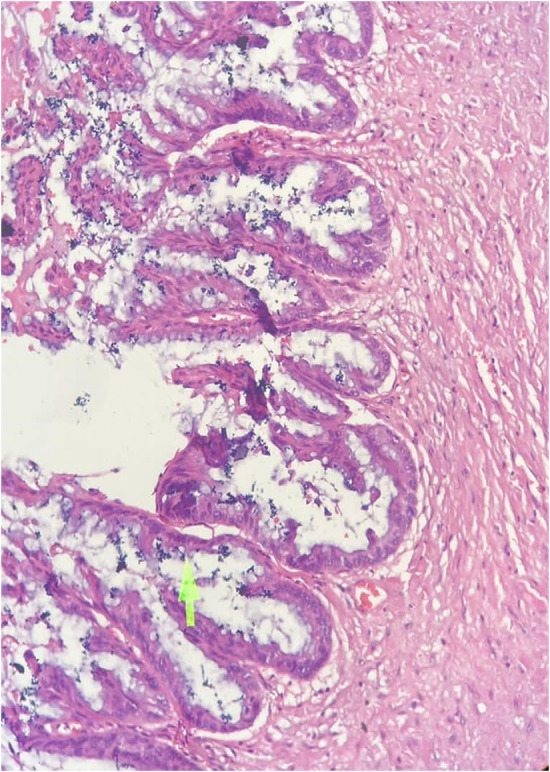
Histopathological of Mucinous appendiceal neoplasm
The patient had an uneventful postoperative course and was discharged 10 days after surgery. We referred him to an oncologist, and eight courses of chemotherapy (FOLFOX regimen) has been prescribed every 2 weeks for prophylaxis. Fortunately, 1.5‐year follow‐up of the patient was completely uneventful and no complications or medical complaints were detected.
3. DISCUSSION AND CONCLUSIONS
In this study, we present a unique case of mucinous appendiceal neoplasm that invaded from the intraperitoneum to the retroperitoneum. To the best of our knowledge, this is the first case study in which a tumor has invaded the visceral peritoneum into the retroperitoneum. Park et al. 7 reported a 32‐year‐old man with extra‐GIST (EGIST) referred to the hospital with dysuria and abdominal mass. Preoperative ultrasound and magnetic resonance imaging (MRI) revealed a lobulated mixed echoic mass in the retroperitoneum with heterogeneous enhancement. The patient underwent surgical excision of the tumor and a low anterior resection because of the invasion to the wall of the rectum. In our case, no adhesion around the tissue was also found, but the tumor extended inferiorly to the right side of the lower abdomen and pelvic cavity.
Engin et al. 6 reported a case of GIST with a mesenteric and retroperitoneal invasion that also entered the small bowel serosa, colonic submucosa, and the left ureter, which presented with abdominal bulging, weight loss, and hematuria. It is inconsistent with our patient, but it can generally be concluded that the penetration of the tumors through the visceral peritoneum can be due to the weakness of this layer.
Appendiceal pathologies may have strange clinical features. They may be misdiagnosed with hydatid cyst in preoperative clinical and radiologic evaluations, while some benign conditions, such as appendiceal abscess due to the perforated appendix and benign mucocele, may mimic neoplasm. 10 , 11
Mucinous appendiceal neoplasms are rare but necessary to be detected with imaging due to their malignancy potential. Peritoneal seeding and pseudomyxoma peritonei can occur in both malignant and low‐grade appendiceal neoplasms. 9
Regardless of their clinical seriousness, mucinous neoplasms may be challenging to diagnose since the symptoms are usually mild or non‐specific. They often present with weight loss, nausea, fatigue, a palpable mass, and acute appendicitis. If there is strong clinical suspicion of appendiceal mucinous neoplasm, preoperative diagnosis is mandatory in order to perform the best surgical treatment 12 ; however, this was not the case for our patient because the clinical presentation was as a RP mass.
Roma et al. 13 reported a late‐stage diagnosis of appendiceal mucinous adenocarcinoma with a rare presentation, such as scrotal pain, abscess, and inguinal drainage, but our patient developed with typical symptoms, like abdominal pain, weight loss, and palpable mass, without any appendicitis alarm.
A laparoscopic approach to retroperitoneal mass has been described in some studies. Agrusa et al. 14 successfully performed laparoscopic resection of left dedifferentiated liposarcoma; however, they suggested more studies for better comparison of laparoscopic and open resection of this entity.
Although we performed open surgery on this patient, we believe laparoscopic operation could be a good choice for exploration and hemicolectomy. Furthermore, laparoscopic right hemicolectomy using the complete mesocolic excision (CME) seems to be a safe technique in patients with right‐side colon cancer. 15
In conclusion, in the approach to retroperitoneal mass, we should consider unusual cases, such as invasive intraperitoneal tumors, like appendiceal ones, while precise preoperative work ups and surgical management, including laparoscopic or open surgeries, may avoid delays in diagnosis and the occurrence of catastrophic complications. Furthermore, patients with retroperitoneal mass presenting with gastrointestinal symptoms may profit from some additional work ups, such as MRI and colonoscopy.
AUTHOR CONTRIBUTIONS
The first four authors have made substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data. They have also been involved in drafting the manuscript, revising it critically for important intellectual content, and finally approving f the final version to be published. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
ETHICAL APPROVAL
This study was approved as a case report by ethics committee of Shiraz University of Medical Sciences.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor‐in‐chief of this journal.
ACKNOWLEDGMENTS
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Salehipour M, Haghpanah A, Dehghani A, et al. Retroperitoneal mass, a rare manifestation of mucinous adenocarcinoma of appendix: A case report. Clin Case Rep. 2022;10:e06602. doi: 10.1002/ccr3.6602
DATA AVAILABILITY STATEMENT
The material and data of the case report is the authors' own original work obtained from this case, which has not been previously published elsewhere.
REFERENCES
- 1. Strauss DC, Hayes AJ, Thomas JM. Retroperitoneal tumours: review of management. Ann R Coll Surg Engl. 2011;93(4):275‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Healy J, Reznek RH. The peritoneum, mesenteries and omenta: normal anatomy and pathological processes. Eur Radiol. 1998;8(6):886‐900. [DOI] [PubMed] [Google Scholar]
- 3. Sassa N. Retroperitoneal tumors: review of diagnosis and management. Int J Urol. 2020;27(12):1058‐1070. [DOI] [PubMed] [Google Scholar]
- 4. Neville A, Herts BR. CT characteristics of primary retroperitoneal neoplasms. Crit Rev Comput Tomogr. 2004;45(4):247‐270. [PubMed] [Google Scholar]
- 5. Osman S, Lehnert BE, Elojeimy S, et al. A comprehensive review of the retroperitoneal anatomy, neoplasms, and pattern of disease spread. Curr Probl Diagn Radiol. 2013;42(5):191‐208. [DOI] [PubMed] [Google Scholar]
- 6. Engin G, Asoglu O, Kapran Y, Mert G. A gastrointestinal stromal tumor with mesenteric and retroperitoneal invasion. World J Surg Oncol. 2007;5(1):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Park S‐S, Min B‐W, Kim W‐B, et al. Malignant extragastrointestinal stromal tumor of retroperitoneum. Acta Oncol. 2005;44(5):497‐499. [DOI] [PubMed] [Google Scholar]
- 8. Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41(1):75‐80. [DOI] [PubMed] [Google Scholar]
- 9. Van Hooser A, Williams TR, Myers DT. Mucinous appendiceal neoplasms: pathologic classification, clinical implications, imaging spectrum and mimics. Abdom Radiol (NY). 2018;43(11):2913‐2922. [DOI] [PubMed] [Google Scholar]
- 10. Sikar HE, Çetin K, Gündoğan E, Alinak Gündoğan G, Kaptanoğlu LJM, Oncology C. Retroperitoneal mucinous cystadenoma of the appendix mimicking hydatid cyst: a case report. Mol Clin Oncol. 2016;5(2):345‐347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yildiz BD, Abbasoglu O. Two unusual presentations of appendiceal masses. Int J Surg. 2008;6(6):e9‐e11. [DOI] [PubMed] [Google Scholar]
- 12. Agrusa A, Romano G, Galia M, et al. Appendiceal mucinous neoplasms: an uncertain nosological entity. Report of a case. G Chir. 2016;37(2):86‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roma K, Baldwin M, Sedmak D, Silva M, Stellar W, Many G. Late stage diagnosis of mucinous adenocarcinoma of the appendix: a case report of an unusual tumor with a rare presentation. BMC Gastroenterol. 2020;20(1):1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Agrusa A, Di Buono G, Buscemi S, et al. Dedifferentiated retroperitoneal large liposarcoma and laparoscopic treatment: is it possible and safe? The first literature case report. Int J Surg Case Rep. 2019;57:113‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Di Buono G, Buscemi S, Cocorullo G, et al. Feasibility and safety of laparoscopic complete mesocolic excision (CME) for right‐sided colon cancer: short‐term outcomes. A randomized clinical study. Ann Surg. 2021;274(1):57‐62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The material and data of the case report is the authors' own original work obtained from this case, which has not been previously published elsewhere.


