Abstract
Background.
Given low base rates of suicidal thoughts and behaviors (STBs) in national samples of adolescents, clarifying the sociodemographic and clinical correlates among psychiatric inpatients may afford insights into potential risk factors that predict STBs onset.
Method.
Adolescents (N=970; ages 12–19 years) admitted for acute, psychiatric inpatient care completed baseline clinical interviews and self-report measures assessing demographics and early life adversity. Lifetime and 12-month STBs prevalence were obtained, allowing for the estimate of STBs persistence (i.e., rates of those with both current and past STBs) and transition rates (i.e., proportion of ideators that transition to plans or attempts). Univariate and multivariate logistic regression tested sociodemographic and clinical correlates of STBs.
Results.
Age-of-onset for STBs occurred in early adolescence. Most patients reported suicide ideation with nearly half of patients making a plan and one-third a suicide attempt. Although relatively modest, the strongest correlates of lifetime attempts were depressive disorders, physical abuse, and non-suicidal self-injury. Knowing a peer that had attempted suicide also increased the likelihood of a suicide attempt, especially among attempters who transitioned from ideation to planned attempts.
Conclusion.
STBs are highly prevalent among adolescents admitted for acute psychiatric inpatient treatment. The modest effects suggest that correlates, particularly those related to suicide attempts, are widely distributed. As a history of physical abuse and knowing a peer with a suicide attempt history are related to transitioning from ideation to action, these may be critical factors to target in the deployment of future suicide prevention and treatment programs.
Keywords: Suicide, Non-Suicidal Self-Injury, Contagion, Physical Abuse, Comorbidity
Introduction
Suicide is the second leading cause of death among adolescents in the United States, and rates of youth suicide attempts have increased by over 40% in the past decade (Ivey-Stephenson et al., 2020). Known correlates of suicidal thoughts and behaviors (STBs), such as early life adversity and mental disorders, are more prevalent among adolescent inpatients (Franklin et al., 2017; Tunnard et al., 2014), and this group is at high-risk for suicide-related outcomes. Indeed, approximately 80% of adolescents in residential or inpatient settings report suicidal thinking (Venta & Sharp, 2014), and rates of lifetime suicide attempts range from 38–63% (Andover & Gibb, 2010; Groschwitz et al., 2015; Thompson et al., 2020; Venta & Sharp, 2014). Consequently, it is critical to clarify reliable correlates of STBs in adolescent psychiatric patients, as this may inform the development of intervention programs that reduce the needless loss of life.
Although the majority of adolescents with lifetime STBs satisfy diagnostic criteria for at least one mental disorder (Nock et al., 2013), most individuals with mental disorders do not attempt suicide (Sisti et al., 2020), suggesting that there may be other clinical and sociodemographic factors that increase STB risk. Prior epidemiological research among adolescents has identified promising correlates of STBs in the general population (Nock et al., 2013), however, given that suicidal behaviors occur with low base rates, it is often challenging to identify risk factors that are more central to psychiatric populations. Focusing on large samples of adolescent psychiatric inpatients among whom STBs are more common may afford a unique opportunity to clarify clinical and sociodemographic correlates related to STBs.
Depressive disorders are consistently associated with the emergence of STBs across age groups (Bernal et al., 2007; Gili et al., 2019; Im et al., 2017; Miret et al., 2013; Nock et al., 2010, 2013). Among adolescents and adults in the general population, depressive disorders are central for the development of suicidal ideation and are distally related to suicide attempts (Franklin et al., 2017; Tunnard et al., 2014). Anxiety disorders also may relate to STBs, though this relationship has not been consistent (Bentley et al., 2016; Hill et al., 2011). Patients reporting externalizing disorders characterized by diminished inhibitory control and greater impulsivity (e.g., attention deficit hyperactivity disorder [ADHD], substance use disorder, conduct disorder) also have shown elevated rates of STBs (Nock et al., 2010, 2013; Poorolajal et al., 2016). Perhaps owing to the complexity and severity of the clinical presentation, comorbidity increases risk for STBs above and beyond specific disorders (Gili et al., 2019; Hoertel et al., 2015). This highlights the importance of clarifying whether there are specific mental disorder profiles that may confer heightened risk for suicidal behaviors (Auerbach et al., 2019).
The current report includes data from adolescent patients (N=970) admitted to an inpatient treatment program. In our prior research with subsamples of this larger dataset, we demonstrated that, relative to ideators, attempters reported increased interpersonal stress exposure (Stewart et al., 2019), greater peer victimization (Stewart et al., 2018), increased anhedonia severity and associated reward learning impairments (Auerbach et al., 2015), increased impulsivity (i.e., negative urgency [Auerbach et al., 2017]) and risky behavior engagement (Stewart, Esposito, et al., 2017; Stewart et al., 2018), and diminished attentional control (Stewart, Glenn, et al., 2017). Building on this research, we aimed to clarify the lifetime and 12-month prevalence of STBs, and then, test sociodemographic and clinical correlates of STBs that may contribute to the transition from ideation to action among these high-risk adolescents.
Methods
Participants
The initial sample consisted of 980 adolescents recruited from an acute, insurance-based inpatient treatment program in the greater Boston area from July 2012 to April 2017. Participants were admitted for acute inpatient care given a range of clinical issues including safety concerns (e.g., presence of STBs and/or non-suicidal self-injury [NSSI]), elevated psychiatric symptoms, and/or non-response following outpatient treatment (Zambrowicz et al., 2019). Ten participants did not complete the Self-Injurious Thoughts and Behaviors Interview (SITBI), and thus, our final sample included 970 adolescents (71.06% female) ages 12 to 19 years (M=15.58, SD=1.42). Table 1 summarizes the sociodemographic and clinical history of the participants.
Table 1.
Sociodemographic and Clinical Correlates Among Adolescents Admitted for Acute Psychiatric Treatment
| Category | Mean (SD) / n (%) |
|---|---|
| Sex, n (%) | |
| Female | 658 (71.06) |
| Male | 268 (28.94) |
| Age, mean (SD) | 15.58 (1.42) |
| Race, n (%) | |
| White | 772 (81.09) |
| Black | 19 (2.00) |
| Asian | 53 (5.57) |
| Pacific Islander | 3 (0.32) |
| Native American | 7 (0.74) |
| 2 or more races | 98 (10.29) |
| Annual household income, n (%) | |
| < $50,000 | 139 (22.64) |
| $50,000 – $100,000 | 262 (42.67) |
| > $100,000 | 213 (34.69) |
| Parental education, n (%) | |
| Did not complete 4-year degree | 156 (16.97) |
| Did complete 4-year degree | 763 (83.02) |
| Lifetime depressive disorder n (%) | |
| Present | 835 (86.17) |
| Not present | 134 (13.83) |
| Lifetime bipolar disorder n (%) | |
| Present | 44 (4.54) |
| Not Present | 925 (95.46) |
| Any current anxiety disorder, n (%) | |
| Present | 504 (52.01) |
| Not present | 465 (47.99) |
| Current ADHD, n (%) | |
| Present | 172 (17.75) |
| Not Present | 797 (82.25) |
| Substance or Alcohol Use Disorder (Past 6 months), n (%) | |
| Present | 49 (5.06) |
| Not Present | 920 (94.94) |
| Number of current psychiatric disorders, mean (SD) | 2.25 (1.44) |
| Lifetime sexual abuse, n (%) | |
| Present | 224 (23.55) |
| Not present | 727 (76.45) |
| Lifetime physical abuse, n (%) | |
| Present | 156 (16.39) |
| Not present | 796 (83.61) |
| Lifetime NSSI, n (%) | |
| Present | 693 (71.52) |
| Not present | 276 (28.48) |
| Peer with SA history, n (%) | |
| Present | 346 (35.93) |
| Not present | 617 (64.07) |
Note. The following disorders were included in the number of current psychiatric disorders variable: Any Depressive Disorder (Major Depressive Disorder, Dysthymia), Any Bipolar Disorder (I, II, Not Otherwise Specified), All Anxiety Disorders (Panic, Agoraphobia, Separation, Social, Specific Phobia, Generalized), Obsessive Compulsive Disorder, Posttraumatic Stress Disorder, Substance or Alcohol Use Disorder, Attention Deficit Hyperactivity Disorder, Conduct Disorder, Oppositional Defiant Disorder, any Psychotic Disorder, Anorexia Nervosa, Bulimia Nervosa, Binge Eating Disorder, and any Adjustment Disorder. ADHD = Attention Defecit Hyperactivty Disorder, SD = Standard Deviation, NSSI = Non-Suicidal Self-Injury, SA = Suicide Attempt.
Procedure
All study procedures were approved by the Institutional Review Board. Legal guardians and participants ages 18 to 19 years provided informed consent, while participants ages 13 to 17 years provided informed assent. Within 48 hours of admission to the inpatient treatment program, participants were administered clinical interviews assessing mental disorders and STBs. All study staff received a minimum of 25 hours of training prior to interview administration. Participants also reported demographic information and completed self-report questionnaires.
Clinical Instruments
Mini International Neuropsychiatric Interview for Children and Adolescents 6.0 (MINI-KID).
The MINI-KID is a structured diagnostic interview used to assess the prevalence of mental disorders that probed DSM-IV-TR criteria. The MINI-KID has been shown to have strong validity and reliability among youth (Sheehan et al., 2010).
Self-Injurious Thoughts and Behaviors Interview Short-Form (SITBI).
The SITBI is a structured clinical interview used to assess suicidal thoughts and behaviors. Participants reported on lifetime and 12-month prevalence and frequency of suicidal ideation, plans, attempts, and NSSI. Participants provided information related to STB age-of-onset (AOO), as well as whether anyone in their life had made a suicide attempt and, if so, the nature of that relationship. In the present paper, we focused on peer attempt history, which included both personal friends and romantic partners. The SITBI shows strong psychometric properties among adolescents in outpatient (Nock et al., 2007) and inpatient settings (Venta & Sharp, 2014).
Childhood Trauma Questionnaire (CTQ).
The CTQ is a 25-item self-report measure that assesses childhood traumatic experiences. Items are rated on a 5-point scale ranging from 1 (never true) to 5 (very often true), with higher scores indicating more severe abuse and/or neglect. Following published guidelines (Bernstein & Fink, 1998), we dichotomized the 5-item subscales to index the presence/absence of physical (scores ≥ 8) and sexual (scores ≥ 6) abuse. Dichotomized scores are preferred, as continuous abuse severity is typically highly positively skewed, and the presence/absence scores are associated with superior criterion-related validity in clinical samples (Bernstein et al., 2003). The present study focused on physical and sexual abuse. The reliability of items in the physical (α=0.81) and sexual abuse (α=0.94) subscales was good and excellent, respectively.
Data Analysis
All analyses were conducted in R version 4.0.2 (R Core Team, 2017), and data that support the findings of this study are available from the corresponding author upon reasonable request. Prevalence estimates, transition rates, persistence, and their associated 95% confidence intervals (CI) were obtained using the propCI function from the prevalence v0.4.0 package (Devleesschauwer et al., 2014). Following prior guidelines (Mortier et al., 2018), transition rates reflected the proportion of: (a) suicide planners among ideators (i.e., transition rate = N lifetime (or past 12-month) plans / N lifetime ideation), (b) attempters among lifetime ideators who do not report lifetime plans (i.e., transition rate = N lifetime (or past 12-month) attempt not preceded by plan / N lifetime ideation without lifetime plan (or plan with age of onset not preceding first attempt), and (c) attempters among lifetime ideators who report prior plans (i.e., transition rate = N lifetime (or past 12-month) attempt preceded by plan / N lifetime ideation with lifetime plan (unless age of onset of first attempt preceded first plan). Eleven participants had a first attempt that was not preceded by plans but later made attempts proceeded by plans; we used the information from the first attempt to classify these participants. For 12-month prevalence estimates, participants with plans preceding the most recent attempt in the past year were considered planned attempters, regardless of initial attempt status. We defined persistence as the number of individuals with an STB (i.e., ideation, plan, attempt) both within and prior to the past 12 months, divided by the total number of individuals with that STB at any point (i.e., recent, lifetime, or both). Seven participants were missing data regarding ideation persistence, and twelve were missing data regarding plan and attempt persistence. Seven participants were missing AOO data for ideation, two were missing data for plans, and three were missing data for attempts.
Logistic regressions were used to test correlates of lifetime STBs. All logistic regression analyses were conducted using the glm function from the stats v3.6.2 package in R. First, sociodemographic and clinical correlates of interest were entered into separate univariate logistic regression models with absence/presence of ideation, plans, attempts, plans among ideators, unplanned attempts, or planned attempts as the outcome variable. All significant (p<.05) correlates were then entered into multivariate logistic regression models for each STB. Results are reported as odds ratios (OR; univariate regression) or adjusted odds ratios (aOR; multivariate regression) with associated 95% CIs. The sociodemographic correlates included: sex (female vs. male), age (17+, 15–16, vs. 12–14), race (non-White vs. White), annual household income (>$100,000, $50,000-$100,000, vs. <$50,000), and parental education level (did not complete a 4-year degree vs. did complete a 4-year degree). Age categories (17+, 15–16, 12–14) were based on the Centers for Disease Control and Prevention (CDC) developmental milestone guidelines that define “Young Teens” as ages 12–14 years and “Teenagers” as 15–17 years (CDC, 2021). Given the small number of participants 18 years or older (N = 87), we grouped these participants in the 17+ years category to provide more balanced cell sizes. Clinical correlates included: any lifetime depressive disorder (MINI-KID), any current anxiety disorder (MINI-KID), current ADHD (MINI-KID), number of current psychiatric disorders (4+, 3, 2, vs. 0–1; MINI-KID), lifetime sexual abuse (CTQ), lifetime physical abuse (CTQ), lifetime NSSI history (SITBI), and knowing a peer with suicide attempt history (SITBI). As the MINI-KID is only designed to assess current episodes for anxiety disorders and ADHD, we could not test associations with these as lifetime diagnoses.
Results
STB Prevalence, Age of Onset, and Persistence Rates
The lifetime and 12-month prevalence of suicide ideation, plans, and attempts are summarized in Table 2. Lifetime and 12-month suicide ideation were common in the vast majority of patients. Approximately half of patients made a plan to end their life, and nearly one-third of patients made a suicide attempt in the 12 months prior to admission. AOO for STBs began in early- to mid-adolescence with the majority reporting a persistence of ideation and, to a lesser extent, plans and attempts (Figures 1A–1C). Over one-fifth of ideators made an initial lifetime suicide attempt without a plan, while nearly half of lifetime ideators reported an initial planned attempt. The majority of adolescents who transitioned from ideation to plans did so within one year of ideation of onset, whereas transitioning from ideation to both planned and unplanned attempts were more evenly distributed over time (Figure 1D).
Table 2.
Prevalence, age of onset, and persistence of suicidal thoughts and behaviors
| Lifetime % (95% CI) |
12-Month % (95% CI) |
Age of Onset Mean (SD) |
Persistence a % (95% CI) |
|
|---|---|---|---|---|
| STB prevalence | ||||
| Ideation | 86.80 (84.51 – 88.87) | 83.40 (80.91 – 85.69) | 13.02 (2.38) | 66.59 (63.27 – 68.78) |
| Plan | 56.08 (52.89 – 59.23) | 50.93 (47.73 – 54.12) | 13. 89 (2.20) | 41.17 (36.95 – 45.48) |
| Attempt | 35.26 (32.25 – 38.36) | 30.31 (27.34 – 33.31) | 14.43 (1.93) | 17.89 (13.90 – 22.45) |
| STB transition rates | ||||
| Plan among lifetime ideators | 64.49 (61.12 – 67.73) | 58.67 (55.26 – 62.02) | 13.90 (2.20) | 41.62 (37.39 – 45.94) |
| Attempt among lifetime ideators without prior plan | 26.03 (21.27 – 31.25) | 23.86 (19.19 – 29.04) | 14.47 (1.97) | 20.25 (12.04 – 30.80) |
| Attempt among lifetime ideators with prior plan | 48.58 (44.23 – 52.94) | 50.75 (46.52 – 54.96) | 14.28 (1.93) | 17.41 (12.89 – 22.72) |
Note.
Persistence is defined as the number of individuals with an STB both within and prior to the past 12 months divided by the total number of individuals with that STB; Age of Onset and Persistence items were missing from the following: Age of Onset (Ideation = 7, Plan = 2, Attempt = 3) and Persistence (Ideation = 7, Plan = 12, Attempt = 12); CI = Confidence Interval.
Figure 1A.
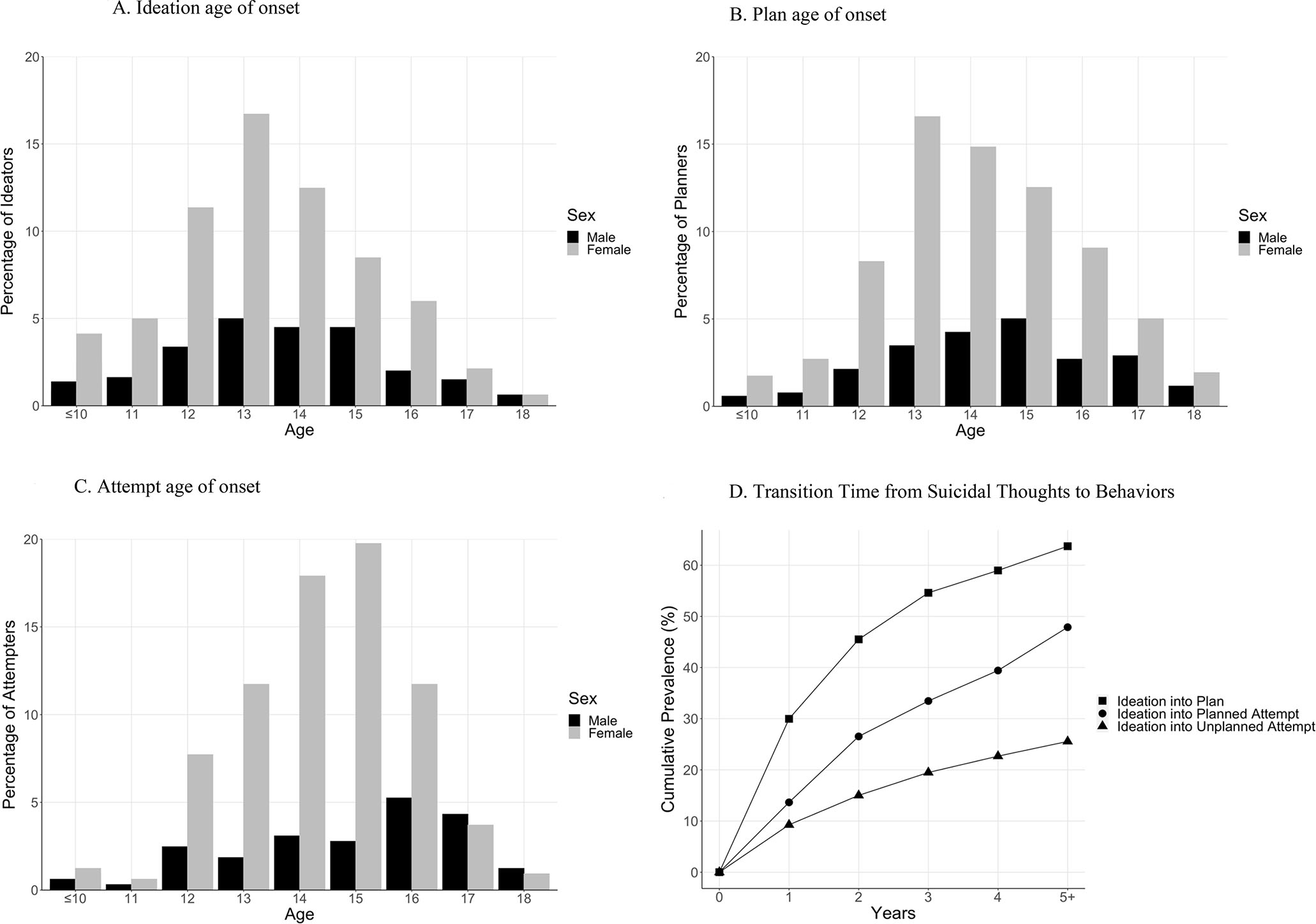
Note. All age of onset (AOO) percentages reflect sex (male [black] or female [gray]) relative to the total sample size per group; (A) AOO by sex for suicidal ideation (n=802; 27.18% male, 72.82% female); (B) AOO by sex for suicide plans (n=519; 24.28% male, 75.72% female), (C) AOO by sex for suicide attempts (n=324; 22.53% male, 77.47% female); (D) The transition time from ideation to plans (black square), planned attempts (black circle), and unplanned attempts (black triangle).
Sociodemographic and Clinical Correlates of Lifetime Suicidal Thoughts and Behaviors
Suicide Ideation.
Univariate analyses indicated that identifying as female, relative to male, was associated with higher odds of lifetime suicide ideation. Clinical correlates were similar to those identified in prior research (Andover & Gibb, 2010; Brown et al., 2012; Maniglio, 2011; Nock et al., 2013; Tunnard et al., 2014), including lifetime depressive disorders, current anxiety disorders, number of current disorders, lifetime NSSI, and prior sexual abuse all relating to increased odds of lifetime ideation. Knowing a peer that previously attempted suicide also significantly increased the odds of reporting ideation (Table 1S). However, in the multivariate model, only lifetime depressive disorders and NSSI history were significant related to suicidal ideation above and beyond the other correlates (Table 3), showing that prior depressive disorders and NSSI engagement were associated with a 6- and 7-fold higher odds of reporting lifetime ideation, respectively.
Table 3.
Multivariate sociodemographic and clinical correlates of lifetime suicidal thoughts and behavior
| Ideation aOR (95% CI) |
Plan aOR (95% CI) |
Attempt aOR (95% CI) |
Plans Among Ideators aOR (95% CI) |
Attempt Among Ideators Without Plan aOR (95% CI) |
Attempt Among Ideators With Plan aOR (95% CI) |
|
|---|---|---|---|---|---|---|
| Sex (Female > Male) | 0.73 (0.45 – 1.18) | 0.92 (0.65 – 1.30) | 1.05 (0.74 – 1.50) | 1.01 (0.70 – 1.45) | 1.90 (0.97 – 3.74) | -- |
| Age (years) | ||||||
| 17+ | -- | -- | -- | -- | 3.15 (1.40 – 7.09)** | -- |
| 15–16 | -- | -- | -- | -- | 2.25 (1.06 – 4.80)* | -- |
| 12–14 | -- | -- | -- | -- | (Reference) | -- |
| Any lifetime depressive disorder | 5.88 (3.54 – 9.77)*** | 1.89 (1.22 – 2.94)** | 1.86 (1.14 – 3.03)* | -- | -- | -- |
| Any current anxiety disorder | 1.25 (0.67 – 2.34) | 0.98 (0.65 – 1.48) | 1.03 (0.69 – 1.56) | 0.95 (0.62 – 1.47) | -- | -- |
| Number of current psychiatric disorders | ||||||
| 4+ | 1.83 (0.68 – 4.90) | 2.61 (1.46 – 4.68)** | 1.15 (0.64 – 2.04) | 2.37 (1.29 – 4.36)** | -- | -- |
| 3 | 1.51 (0.65 – 3.53) | 2.01 (1.90 – 3.41)** | 1.10 (0.65 – 1.86) | 1.89 (1.08 – 3.29)* | -- | -- |
| 2 | 1.31 (0.68 – 2.52) | 1.62 (1.05 – 2.48)* | 0.94 (0.61 – 1.47) | 1.55 (0.99 – 2.42) | -- | -- |
| 0 – 1 | (Reference) | (Reference) | (Reference) | (Reference) | -- | -- |
| Lifetime sexual abuse | 1.63 (0.81 – 3.30) | 1.04 (0.72 – 1.51) | 1.35 (0.95 – 1.91) | 1.06 (0.73 – 1.54) | 1.17 (0.61 – 2.25) | 1.23 (0.81 – 1.86) |
| Lifetime physical abuse | -- | 1.24 (0.82 – 1.88) | 1.92 (1.30 – 2.84)** | -- | 2.67 (1.31 – 5.42)** | 1.82 (1.13 – 2.95)* |
| Lifetime NSSI | 6.98 (4.25 – 11.49)*** | 4.11 (2.88 – 5.86)*** | 2.76 (1.85 – 4.13)*** | 2.83 (1.94 – 4.13)*** | 2.11 (1.06 – 4.18)* | 1.57 (0.92 – 2.67) |
| Peer with SA history | 1.10 (0.66 – 1.82) | 1.04 (0.76 – 1.42) | 1.48 (1.09 – 2.01)* | -- | -- | 1.93 (1.33 – 2.80)*** |
| Overall Model χ2 | 178.69*** | 147.94*** | 92.79*** | 59.23*** | 29.13*** | 29.57*** |
Note. Adjusted odds ratios and 95% confidence intervals were calculated using multiple logistic regression; aOR = odds ratio; CI = confidence interval; NSSI = non-suicidal self-injury; SA = suicide attempt; χ2 = Chi-square test to evaluate overall model fit
p < 0.001
p < 0.01
p < 0.05
Suicide Plans.
Although univariate models showed a number of correlates of suicide plans (Table 1S), only lifetime depressive disorders, number of current disorders, and lifetime NSSI were significant in the multivariate model (Table 3). Furthermore, multivariate analyses show that number of current disorders and lifetime NSSI are strong indicators of adolescents transitioning from suicidal thinking to planning—showing a 2- to 3-fold greater odds (Table 3).
Suicide Attempts.
Univariate models showed significant associations with a wide range of sociodemographic and clinical correlates (Table 1S). By comparison, fewer significant correlates emerged in the multivariate analyses, and these effects were modest. Lifetime depressive disorder history and physical abuse were associated with a near 2-fold greater odds of making a suicide attempt, and lifetime NSSI history was related to a 2-fold greater likelihood of making an attempt as well as transitioning from ideation to an unplanned attempt. Knowing a peer who made a suicide attempt was associated with significantly greater odds of a suicide attempt, as well as with transitioning from ideation to an attempt preceded by a suicide plan. Lifetime physical abuse also increased the odds of a later attempt, whether or not the attempt was preceded by a suicide plan (Table 3).
Discussion
The increased rates of STBs among adolescents over the past decade is a major public health concern. Identifying predictors of STBs is necessary to prevent suicide, yet common correlates, such as MDD, lack sensitivity and often fail to predict changes in STBs over time (Franklin et al., 2017). In an effort to address this gap, the present study leveraged data from a large sample of adolescents receiving acute psychiatric inpatient treatment. Lifetime and 12-month prevalence of STBs were strikingly high and persistent, with AOO often occurring in early adolescence. Additionally, a number of promising correlates related to STBs offer new insights regarding potential sociodemographic and clinical risk factors that warrant investigation in future longitudinal studies.
As expected, lifetime rates of STBs in our sample were markedly higher than in the general adolescent population (Nock et al., 2013), but they aligned with prevalence estimates reported in studies of inpatient youth (Andover & Gibb, 2010; Groschwitz et al., 2015; Thompson et al., 2020; Venta & Sharp, 2014). Approximately one-third of participants reported making at least one lifetime suicide attempt. This high prevalence rate is concerning as it reflects adolescents’ current psychological distress and may portend future impairment in adulthood. Indeed, prior work has demonstrated that youth attempts are associated with later life mental disorders as well as poorer physical health, social dysfunction, and engagement in risky behaviors (e.g., violence, precocious sexual behaviors (Brière et al., 2015; Goldman-Mellor et al., 2014). We also found that STBs are recurrent, as 20% of adolescents who reported an attempt in the past year also reported having made at least one prior attempt. Coupled with extant research demonstrating that prior attempts are strong predictors of later death by suicide (Bostwick et al., 2016), the high rate of recurrence of suicidal behaviors underscores the urgent need for improved acute risk management and longer-term follow-up care. Unfortunately, adolescents’ compliance with follow-up outpatient care is generally low (Gould et al., 2003), and thus, improving treatment engagement remains a critical barrier to reduce suicidal behaviors (Lizardi & Stanley, 2010).
The high transition rates from suicide ideation to plans and planned attempts also highlight a need for improved short- and long-term mental health care among youth with early onset STBs. Towards this goal, it is important to understand what characteristics increase the likelihood that suicidal ideation will escalate to suicidal behavior. Consistent with prior research (Nock et al., 2013), we found that lifetime depressive disorders were strongly associated with lifetime ideation; however, they were not associated with the occurrence of suicide plans or attempts among lifetime ideators. Similarly, the number of current mental disorders was not associated with the presence of attempts among ideators. These findings suggest that the distress linked to psychopathology (e.g., depression symptoms, comorbid diagnoses) may be associated with suicidal thoughts, but is not uniquely implicated in the transition from suicide ideation to behaviors. Lifetime physical abuse, however, may be a risk factor of interest as it related to increased odds of transitioning to attempts. This finding aligns with prior work (Joiner et al., 2007; Zatti et al., 2017) and with the interpersonal theory of suicide (ITS; Van Orden et al., 2010). Specifically, the ITS posits that painful and aversive experiences like physical abuse increase a person’s capability to engage in suicidal behavior by reducing fear of death and increasing pain tolerance over time (Van Orden et al., 2010). Physical abuse may contribute to suicide capability directly (i.e., exposure to pain during abuse episodes) or indirectly via its associations with general risky behavior engagement (Stewart et al., 2018). Similarly, NSSI may serve as another key source of pain habituation (Hamza et al., 2012; Joiner et al., 2012). Prior research among adolescent inpatients generally supports an association between NSSI and suicide attempts (Andover & Gibb, 2010; Groschwitz et al., 2015), which facilitated the transition from ideation to both planned and unplanned attempts in the present study.
An important correlate of transitioning to planned attempts was knowing a peer who had made at least one suicide attempt themselves. This finding adds to the existing literature on suicide contagion, the phenomenon by which exposure to suicide facilitates the emergence of STBs in others (Mueller & Abrutyn, 2015; Swanson & Colman, 2013). Adolescents may be more susceptible to contagion than adults (Hawton et al., 2020), and this vulnerability is heightened when the exposure to suicide is from a same-aged peer (Swanson & Colman, 2013). However, the mechanisms through which contagion occurs are currently unclear. It may be, for example, that what appears to be suicide contagion is instead the result of assortative relating, or rather, individuals at high-risk for suicide are more likely to befriend those who are similarly high-risk. In this view, suicide clusters are the result of underlying shared risk factors rather than contagion (Hawton et al., 2020; Joiner Jr, 2003). This perspective, however, may not fully account for the increase in suicidal behaviors that occurs after exposure to a peer’s suicide attempt (Randall et al., 2015). Among adolescents in the general population, heightened STBs are associated with disclosed, but not undisclosed, peer attempts (Mueller & Abrutyn, 2015). These disclosed attempts may provide a model for adolescents’ distress response and present suicide as a more salient option, while undisclosed attempts do not (Mueller & Abrutyn, 2015). Related work likewise demonstrates that the relationship between knowing someone who has attempted suicide and one’s own suicide planning behaviors is partially mediated by one’s belief that suicide is acceptable, indicating that increased suicide acceptability may be a key mechanism of contagion (Kleiman, 2015). Clarifying the role of social contagion in the transition from ideation to attempts, particularly within inpatient settings where adolescents form lasting friendships with youth with a suicide attempt history, may offer a key inroad for future suicide prevention efforts.
There are several limitations that should be considered for future research. First, the sample was recruited from an insurance-based treatment program in the greater Boston area and is not nationally representative. The generalizability of findings is limited to ethnically and socio-demographically similar populations. Second, although sex assigned at birth was assessed, data on gender identity and expression were not available. Transgender adolescents report higher rates of STBs than cisgender youth (Perez-Brumer et al., 2017; Toomey et al., 2018); thus, we may have missed important STB correlates for relevant to diverse gender locations. Likewise, we have not assessed sexual orientation and, notably, non-heterosexual orientation has been linked to STBs in adolescent community samples (Stone et al., 2014). Third, the retrospective study design precludes the ability to definitively disambiguate correlation from causation. Last, although youth were in treatment when they participated, we did not assess their full treatment history. Treatment response may improve symptom trajectories, and accordingly, future research should clarify the role that timing, type, and intensity of treatment may play in the emergence and persistence of STBs.
In summary, the present study highlights several promising correlates, including physical abuse, NSSI, and knowing a peer who attempted suicide, that may be critical to understanding the onset and progression of STBs in adolescent inpatients. Focusing on these characteristics may enhance our recognition of youth at risk for transitioning from ideation to action, and relatedly, may serve as promising targets for the deployment of future prevention and intervention efforts.
Supplementary Material
Highlights.
One-third of adolescent inpatients report a lifetime history of suicide attempts.
Approximately 65% of adolescent inpatients with a lifetime plan attempt suicide.
Knowing peers who attempt suicide may facilitate the transition from ideation to action.
Acknowledgements
This project was supported by the National Institute of Mental Health U01MH116923, Tommy Fuss Fund, and Simches fund awarded to RPA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or of any other sponsor.
Footnotes
Conflict of Interest Disclosures
Dr. Auerbach is an unpaid scientific advisor for Ksana Health. All other authors report no biomedical financial interests or potential conflicts of interest.
References
- Andover MS, & Gibb BE (2010). Non-suicidal self-injury, attempted suicide, and suicidal intent among psychiatric inpatients. Psychiatry Research, 178(1), 101–105. [DOI] [PubMed] [Google Scholar]
- Auerbach RP, Millner AJ, Stewart JG, & Esposito EC (2015). Identifying differences between depressed adolescent suicide ideators and attempters. Journal of Affective Disorders, 186, 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, Demyttenaere K, Ebert DD, Green JG, & Hasking P (2019). Mental disorder comorbidity and suicidal thoughts and behaviors in the world health organization world mental health surveys international college student initiative. International Journal of Methods in Psychiatric Research, 28(2), e1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Stewart JG, & Johnson SL (2017). Impulsivity and suicidality in adolescent inpatients. Journal of Abnormal Child Psychology, 45(1), 91–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, & Nock MK (2016). Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: A meta-analytic review. Clinical Psychology Review, 43, 30–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernal M, Haro JM, Bernert S, Brugha T, de Graaf R, Bruffaerts R, Lépine JP, de Girolamo G, Vilagut G, & Gasquet I (2007). Risk factors for suicidality in Europe: Results from the ESEMED study. Journal of Affective Disorders, 101(1–3), 27–34. [DOI] [PubMed] [Google Scholar]
- Bostwick JM, Pabbati C, Geske JR, & McKean AJ (2016). Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. American Journal of Psychiatry, 173(11), 1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brière FN, Rohde P, Seeley JR, Klein D, & Lewinsohn PM (2015). Adolescent suicide attempts and adult adjustment. Depression and Anxiety, 32(4), 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DL, Jewell JD, Stevens AL, Crawford JD, & Thompson R (2012). Suicidal risk in adolescent residential treatment: Being female is more important than a depression diagnosis. Journal of Child and Family Studies, 21(3), 359–367. [Google Scholar]
- Centers for Disease Control and Prevention. (2021, September 23). Young Teens (12–14 years old). Centers for Disease Control and Prevention. Retrieved October 8, 2021 from https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/adolescence.html [Google Scholar]
- Devleesschauwer B, Togerson P, Charlier J, Levecke B, Praet N, Roelandt S, Smit S, Dorny P, Berkvens D, & Speybroeck N (2014). prevalence: Tools for prevalence assessment studies. R Package Version 0.4.0. http://cran.r-project.org/package=prevalence [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187. [DOI] [PubMed] [Google Scholar]
- Gili M, Castellví P, Vives M, de la Torre-Luque A, Almenara J, Blasco MJ, Cebrià AI, Gabilondo A, Pérez-Ara MA, & Miranda-Mendizabal A (2019). Mental disorders as risk factors for suicidal behavior in young people: A meta-analysis and systematic review of longitudinal studies. Journal of Affective Disorders, 245, 152–162. [DOI] [PubMed] [Google Scholar]
- Goldman-Mellor SJ, Caspi A, Harrington H, Hogan S, Nada-Raja S, Poulton R, & Moffitt TE (2014). Suicide attempt in young people: A signal for long-term health care and social needs. JAMA Psychiatry, 71(2), 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould MS, Greenberg TED, Velting DM, & Shaffer D (2003). Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry, 42(4), 386–405. [DOI] [PubMed] [Google Scholar]
- Groschwitz RC, Kaess M, Fischer G, Ameis N, Schulze UM, Brunner R, Koelch M, & Plener PL (2015). The association of non-suicidal self-injury and suicidal behavior according to DSM-5 in adolescent psychiatric inpatients. Psychiatry Research, 228(3), 454–461. [DOI] [PubMed] [Google Scholar]
- Hamza CA, Stewart SL, & Willoughby T (2012). Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clinical Psychology Review, 32(6), 482–495. [DOI] [PubMed] [Google Scholar]
- Hawton K, Hill NT, Gould M, John A, Lascelles K, & Robinson J (2020). Clustering of suicides in children and adolescents. The Lancet Child & Adolescent Health, 4(1), 58–67. [DOI] [PubMed] [Google Scholar]
- Hill RM, Castellanos D, & Pettit JW (2011). Suicide-related behaviors and anxiety in children and adolescents: A review. Clinical Psychology Review, 31(7), 1133–1144. [DOI] [PubMed] [Google Scholar]
- Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F, & Blanco C (2015). Mental disorders and risk of suicide attempt: A national prospective study. Molecular Psychiatry, 20(6), 718–726. [DOI] [PubMed] [Google Scholar]
- Im Y, Oh W-O, & Suk M (2017). Risk factors for suicide ideation among adolescents: Five-year national data analysis. Archives of Psychiatric Nursing, 31(3), 282–286. [DOI] [PubMed] [Google Scholar]
- Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, Lowry R, & Brown M (2020). Suicidal Ideation and Behaviors Among High School Students — Youth Risk Behavior Survey, United States, 2019. MMWR Supplements, 69(1), 47–55. 10.15585/mmwr.su6901a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE Jr (2003). Contagion of suicidal symptoms as a function of assortative relating and shared relationship stress in college roommates. Journal of Adolescence, 26(4), 495–504. [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr, Sachs-Ericsson NJ, Wingate LR, Brown JS, Anestis MD, & Selby EA (2007). Childhood physical and sexual abuse and lifetime number of suicide attempts: A persistent and theoretically important relationship. Behaviour Research and Therapy, 45(3), 539–547. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Ribeiro JD, & Silva C (2012). Nonsuicidal self-injury, suicidal behavior, and their co-occurrence as viewed through the lens of the interpersonal theory of suicide. Current Directions in Psychological Science, 21(5), 342–347. [Google Scholar]
- Kleiman EM (2015). Suicide acceptability as a mechanism of suicide clustering in a nationally representative sample of adolescents. Comprehensive Psychiatry, 59, 17–20. [DOI] [PubMed] [Google Scholar]
- Lizardi D, & Stanley B (2010). Treatment engagement: A neglected aspect in the psychiatric care of suicidal patients. Psychiatric Services, 61(12), 1183–1191. [DOI] [PubMed] [Google Scholar]
- Maniglio R (2011). The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatrica Scandinavica, 124(1), 30–41. [DOI] [PubMed] [Google Scholar]
- Miret M, Ayuso-Mateos JL, Sanchez-Moreno J, & Vieta E (2013). Depressive disorders and suicide: Epidemiology, risk factors, and burden. Neuroscience & Biobehavioral Reviews, 37(10), 2372–2374. [DOI] [PubMed] [Google Scholar]
- Mortier P, Auerbach RP, Alonso J, Bantjes J, Benjet C, Cuijpers P, Ebert DD, Green JG, Hasking P, & Nock MK (2018). Suicidal thoughts and behaviors among first-year college students: Results from the WMH-ICS project. Journal of the American Academy of Child & Adolescent Psychiatry, 57(4), 263–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller AS, & Abrutyn S (2015). Suicidal disclosures among friends: Using social network data to understand suicide contagion. Journal of Health and Social Behavior, 56(1), 131–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. [DOI] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, & Kessler RC (2010). Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry, 15(8), 868–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Brumer A, Day JK, Russell ST, & Hatzenbuehler ML (2017). Prevalence and correlates of suicidal ideation among transgender youth in California: Findings from a representative, population-based sample of high school students. Journal of the American Academy of Child & Adolescent Psychiatry, 56(9), 739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poorolajal J, Haghtalab T, Farhadi M, & Darvishi N (2016). Substance use disorder and risk of suicidal ideation, suicide attempt and suicide death: A meta-analysis. Journal of Public Health, 38(3), e282–e291. [DOI] [PubMed] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing. R Foundation for Statistic Computing, Vienna, Austria. https://www.R-project.org/ [Google Scholar]
- Randall JR, Nickel NC, & Colman I (2015). Contagion from peer suicidal behavior in a representative sample of American adolescents. Journal of Affective Disorders, 186, 219–225. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, Milo KM, Stock SL, & Wilkinson B (2010). Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). The Journal of Clinical Psychiatry, 71(3), 313–326. [DOI] [PubMed] [Google Scholar]
- Sisti D, Mann JJ, & Oquendo MA (2020). Toward a Distinct Mental Disorder—Suicidal Behavior. JAMA Psychiatry, 77(7), 661–662. [DOI] [PubMed] [Google Scholar]
- Stewart JG, Esposito EC, Glenn CR, Gilman SE, Pridgen B, Gold J, & Auerbach RP (2017). Adolescent self-injurers: Comparing non-ideators, suicide ideators, and suicide attempters. Journal of Psychiatric Research, 84, 105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Glenn CR, Esposito EC, Cha CB, Nock MK, & Auerbach RP (2017). Cognitive control deficits differentiate adolescent suicide ideators from attempters. The Journal of Clinical Psychiatry, 78(6), 614–621. [DOI] [PubMed] [Google Scholar]
- Stewart JG, Shields GS, Esposito EC, Cosby EA, Allen NB, Slavich GM, & Auerbach RP (2019). Life stress and suicide in adolescents. Journal of Abnormal Child Psychology, 47(10), 1707–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Valeri L, Esposito EC, & Auerbach RP (2018). Peer victimization and suicidal thoughts and behaviors in depressed adolescents. Journal of Abnormal Child Psychology, 46(3), 581–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone DM, Luo F, Ouyang L, Lippy C, Hertz MF, & Crosby AE (2014). Sexual orientation and suicide ideation, plans, attempts, and medically serious attempts: Evidence from local youth risk behavior surveys, 2001–2009. American Journal of Public Health, 104(2), 262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson SA, & Colman I (2013). Association between exposure to suicide and suicidality outcomes in youth. CMAJ, 185(10), 870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson E, Spirito A, Frazier E, Thompson A, Hunt J, & Wolff J (2020). Suicidal thoughts and behavior (STB) and psychosis-risk symptoms among psychiatrically hospitalized adolescents. Schizophrenia Research, 218, 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey RB, Syvertsen AK, & Shramko M (2018). Transgender adolescent suicide behavior. Pediatrics, 142(4), e20174218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunnard C, Rane LJ, Wooderson SC, Markopoulou K, Poon L, Fekadu A, Juruena M, & Cleare AJ (2014). The impact of childhood adversity on suicidality and clinical course in treatment-resistant depression. Journal of Affective Disorders, 152, 122–130. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venta A, & Sharp C (2014). Extending the concurrent validity of the Self-Injurious Thoughts and Behaviors Interview to inpatient adolescents. Journal of Psychopathology and Behavioral Assessment, 36(4), 675–682. [Google Scholar]
- Zambrowicz R, Stewart JG, Cosby E, Esposito EC, Pridgen B, & Auerbach RP (2019). Inpatient Psychiatric Care Outcomes for Adolescents: A Test of Clinical and Psychosocial Moderators. Evidence-Based Practice in Child and Adolescent Mental Health, 4(4), 357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatti C, Rosa V, Barros A, Valdivia L, Calegaro VC, Freitas LH, Ceresér KMM, da Rocha NS, Bastos AG, & Schuch FB (2017). Childhood trauma and suicide attempt: A meta-analysis of longitudinal studies from the last decade. Psychiatry Research, 256, 353–358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


