Abstract
The COVID-19 pandemic has demonstrated the importance of large-scale campaigns to facilitate vaccination adherence. Social media presents unique opportunities to reach broader audiences and reduces the costs of conducting national or global campaigns aimed at achieving herd immunity. Nonetheless, few studies have reviewed the effectiveness of prior social media campaigns for vaccination adherence, and several prior studies have shown that social media campaigns do not increase uptake rates. Hence, our objective is to conduct a systematic review to examine the effectiveness of social media campaigns and to identify the reasons for the mixed results of prior studies. Our methodology began with a search of seven databases, which resulted in the identification of 92 interventions conducted over digital media. Out of these 92 studies, only 15 adopted social media campaigns for immunization. We analyzed these 15 studies, along with a coding scheme we developed based on reviews of both health interventions and social media campaigns. Multiple coders, who were knowledgeable about social media campaigns and healthcare, analyzed the 15 cases and obtained an acceptable level of inter-coder reliability (> .80). The results from our systematic review show that only a few social media campaigns have succeeded in enhancing vaccination adherence. In addition, few campaigns have utilized known critical success factors of social media to induce vaccination adherence. Based on these findings, we discuss a set of research questions that informatics scholars should consider when identifying opportunities for using social media to resolve one of the most resilient challenges in public health. Finally, we conclude by discussing how the insights drawn from our systematic reviews contribute to advancing theories, such as social influence and the health belief model, into the realm of social media–based health interventions.
Keywords: Systematic review, Social media campaigns, Digital health, Vaccines, Interventions
1. Introduction
Even before the COVID-19 vaccination program started in the US, interventions to increase immunization rates were a focus of systematic reviews to counteract declining immunization rates (Asare et al., 2021, Crocker-Buque et al., 2017, Falcone, 2019, Jarrett et al., 2015, Lott et al., 2020, Niccolai and Hansen, 2015, Nour, 2019, Odone et al., 2015, Ortiz et al., 2019, Ou and Youngstedt, 2020, Smulian et al., 2016). However, most of these reviews focused on narrow regions or clinician–patient communication, and thus their findings are not directly applicable to social media–based intervention campaigns disseminated to broader audiences. The COVID-19 pandemic and the lagging uptake rates for other routine vaccines have demonstrated that broader campaigns are essential to achieving herd immunity. To this end, social media has been suggested for these media’s affordances to reach diverse populations and facilitate learning, health behavior modification, and emotional regulation (Al-Fraihat et al., 2020, Blumberg et al., 2016). Within this study, we define “social media campaigns” as vaccination interventions primarily conducted on or disseminated via social media.
Previous systematic reviews of social media campaigns focus on one type of vaccine (e.g., the human papillomavirus [HPV], Ortiz et al., 2019) or are outdated in light of recent changes in vaccination recommendations and advances in social technologies (e.g., Cooney et al., 2010). Furthermore, several prior studies have shown that social media campaigns are unsuccessful in increasing uptake rates (Cates et al., 2011, Ortiz et al., 2019), and these findings contradict other studies demonstrating the effectiveness of social media in fostering behavioral changes in areas such as education and marketing (Al-Fraihat et al., 2020, Blumberg et al., 2016). Accordingly, there is a need for an updated systematic review of various vaccines to reconcile the conflicting findings.
We met this need by achieving two specific aims in our systematic review. First, we conducted an up-to-date search (with studies up to January 2022) of prior social media campaigns for a broader range of vaccines and examined the effectiveness of these campaigns in facilitating vaccination adherence, as measured by improvements in intermediate processes (e.g., knowledge, attitudes, and intentions) and final uptake rates. Second, we identified the reasons for the successful and unsuccessful results reported in prior studies. More specifically, we ascribed the successes and failures of the reviewed campaigns to the use of the critical success factors known to induce behavioral modifications. In this way, the current study contributes to the advancement of generalizable scientific knowledge on the diffusion of social influence (or “word-of-mouth”) via social networks and the health belief model (HBM).
Instead of focusing only on COVID-19 vaccines, the scope of this systematic review includes campaigns to foster the acceptance of routine vaccines against various contagious diseases, including HPV, early childhood immunizations (e.g., measles, mumps, and rubella [MMR]), and influenza. The inclusion of various immunizations is necessary to achieve our goal of conducting a comprehensive literature review that is not concentrated on only one type of vaccine. This broader inclusion also informs future campaigns against a wide range of outbreaks during and in the aftermath of the COVID-19 pandemic.
2. Materials and methods
2.1. Processes for the systematic literature review
The search keywords (Table 1 ) centered on three themes: social media, interventions, and vaccination. We referred to the Medical Subject Headings (MeSH), which is “a controlled and hierarchically organized vocabulary produced by the National Library of Medicine” (https://www.nlm.nih.gov/mesh), to derive variations in these themes. These variations were used in combination with Boolean operators, such as “social media” AND [“intervention” OR “campaign”] AND “immunization.” Seven databases were searched: PubMed, PsycINFO, Communication and Mass Media Complete, Sociological Abstracts, Web of Science, EBSCO Academic Search Complete, and the Educational Resource Information Center. The scope of our search was publications from January 2010 to January 2022. From our searches, we found both individual studies and systematic review papers. For the systematic review papers, we populated all the papers and reviewed all of them to ensure the comprehensiveness of our review.
Table 1.
Search terms used in the systematic review.
| Keyword Theme | Keywords Variations Searched Referring to MeSH |
|---|---|
| Social media | social media, social marketing, online social networking, social networking, Web 2.0, Twitter, Facebook, Instagram |
| Interventions and campaigns | health promotion, health campaigns, early intervention education, community health education, persuasive communication, communication, communication programs, health communication, intervention |
| Vaccination | immunization programs, inoculation, vaccination awareness, vaccination campaign, vaccination promotion, anti-vaccination movement |
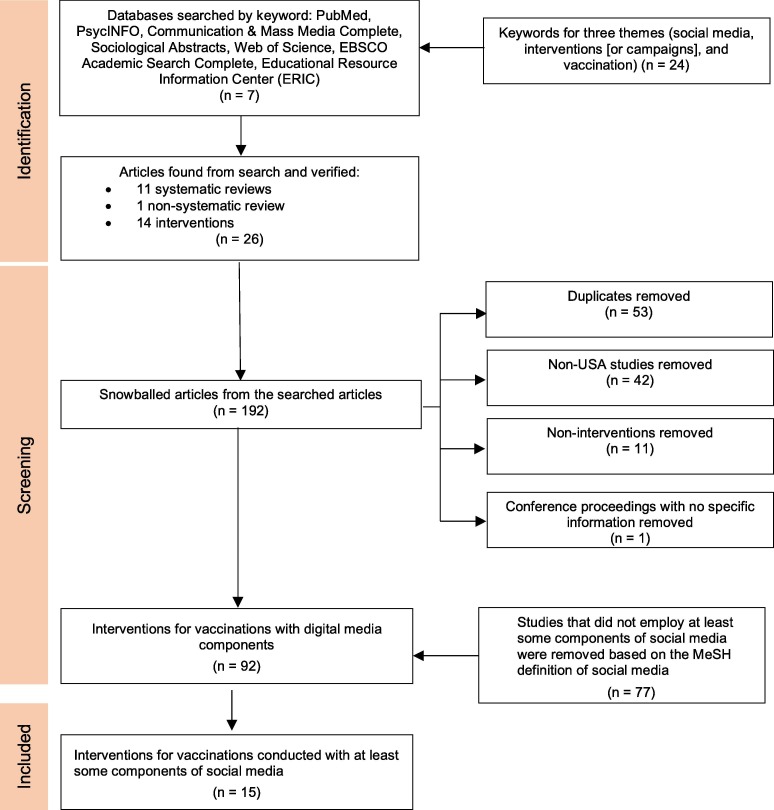
We found a total of 192 studies, as illustrated in Fig. 1 . Fifty-three of these were duplicates and were thus omitted. Exclusion criteria included non-English papers, those not in peer-reviewed publications, those located outside the US, and those published before 2010. These criteria led to the exclusion of 42 studies that focused on countries outside the US, 11 studies that were not interventions, and one study that contained a summary of conference proceedings. There were overlaps in the studies according to the exclusion criterion. An example is a non-US study that was not an intervention and was found more than once (i.e., duplicates). Following the exclusion of ineligible studies, 92 articles remained.
Fig. 1.
Systematic review processes. * Overlaps exist in the studies excluded per each criterion noted above.
Of these 92 studies, we selected campaigns conducted with at least some components of social media. Social media is defined as follows:
“Platforms that provide the ability and tools to create and publish information accessed via the Internet. Generally, these platforms have three characteristics with content user generated, high degree of interaction between creator and viewer, and easily integrated with other sites” (MeSH 2021,https://www.nlm.nih.gov/mesh).
According to this definition, studies that relied on reminders/recalls, phone calls and text messages, stand-alone videos (e.g., video clips played to participants in in-person education), and websites with no interactive components (e.g., static websites without any prompt for user input) were excluded. A total of 15 campaigns that conducted inoculation interventions using social media were identified.
2.2. Development of a coding scheme
Fig. 2 depicts the subsequent procedures for coding the interventions identified in the systematic literature review.
Fig. 2.
Coding of the Interventions Identified from the Systematic Literature Review.
As shown in Fig. 2, our next step was to code the studies we found in our literature review. We chose deductive instead of inductive coding to achieve the aim of this study. As mentioned in the Introduction, one of our aims was to examine the effectiveness of social media campaigns in facilitating vaccination adherence. Achieving this aim requires fair, consistent, and objective evaluations of each campaign. Accordingly, deductive coding (in which researchers assign a predefined set of codes [e.g., success vs non-success] to a dataset) is more suitable than inductive coding (proper for extracting themes and theories from data; Mayring, 2000).
For fair deductive coding, researchers need to develop a scheme or predefined set of codes to achieve reliable, objective, and replicable results (Krippendorff, 1980). Thus, we developed our coding scheme (Table 2 ) based on the conventions used to report the outcomes of health interventions and the factors commonly employed in other social media campaigns for health. Our rationale for choosing these two areas is as follows. First, an intervention that follows common conventions in health interventions can fairly describe the effectiveness of existing social media health campaigns. Second, because these conventions do not include social media–specific components, we needed to capture the idiosyncrasies of social media campaigns for health.
Table 2.
Coding Scheme.
| Codes | Definition | Levels (which appeared in the 15 reviewed studies, or which could potentially appear based on an external standard, such as the US Census) |
|---|---|---|
| Codes relevant to health interventions | ||
|
Target contagious disease(s) against which the vaccine campaign is disseminated |
|
|
Main (sub)population groups whom the campaign serves and is disseminated to |
|
|
The geographic location(s) where the campaign was delivered. Author-provided locations (e.g., city, state) are translated into the five regions defined by the US Census regional divisions |
|
|
The geographic location(s) where the campaign was delivered. Author-provided locations (e.g., city, state) are translated into the three levels of urbanicity in the US Census |
|
|
When the campaign was delivered. If the campaign year was not stated in the study, then use the publication year |
|
|
Whether the campaign intended to (1) increase uptake rates of immunization or (2) achieve proximal changes (e.g., knowledge, attitude, intentions) |
|
|
Whether the increased uptake rates were statistically significant |
|
| Codes relevant to social media campaigns for health | ||
|
Whether content was customized to the identity of the (sub)population groups to which the campaign recipients belong (Schmid et al., 2008) |
|
|
Whether the campaign employed any imagery, such as posters, images, photos, videos, memes |
|
|
Whether the campaign utilized the social connection feature (e.g., friends’ lists and subscriptions) that fosters interactions among campaign recipients or between recipients and healthcare providers |
|
|
Whether a vaccination campaign used social media as the main channel to disseminate interventions OR as part of a larger intervention that encompasses other media (e.g., in-person vaccine clinics supplemented by social media campaign) |
|
2.2.1. Codes relevant to health interventions
To develop codes that relate to common attributes reported in health interventions, we referred to Consolidated Standards of Reporting Trials (CONSORT)1 . CONSORT provides standards for participants, interventions, and outcomes to ensure adequate reporting of randomized controlled trials.1 However, CONSORT was developed for all randomized controlled trials (RCTs), not only for RCTs in inoculation interventions; thus, we referred to the 92 prior inoculation interventions that we identified in our systematic review (see the second-to-last rectangle in Fig. 1) to include components pertinent to vaccination campaigns.
As a result, we chose seven common attributes: (1) target contagious diseases for vaccinations, (2) populations that the vaccines serve, (3) geographic regions where the interventions were delivered, (4) the urbanicity of those regions, (5) years of interventions, (6) intended outcomes, and (7) success in increasing uptake rates.
Target diseases refer to various types of contagious diseases and viruses (e.g., HPV, influenza, early childhood immunizations, and the unspecified encompassing general vaccine hesitancy) against which vaccines are administrated. Populations served refers to the group(s) that these vaccines serve (e.g., male and female college students, adolescents, prenatal women, young adults, ethnic minority women, and sexual minority men). The geographic regions reported in the campaigns were recategorized into West, Midwest, Northeast, South, and Pacific, as per the U.S. Census regional divisions. We also labeled the urbanicity of campaign sites as urban, rural, or reservations, as per the U.S. Census classification. Regarding the years in which interventions took place, we included the timeframe in which the interventions were delivered, as specified by the study authors. For studies in which timeframes were missing, we used publication years.
Intended outcomes refer to the goals that a campaigner attempts to achieve. Intended outcomes encompass increasing knowledge and awareness of, as well as attitudes toward, vaccines, the severity of the target diseases, behavioral intentions to adopt the vaccines, and, finally, uptake rates. When coding uptake rates, we also noted whether the campaign resulted in statistically significant differences between treatment and control groups or between pre- and post-tests. In our categorization of successful cases, we did not include campaigns that simply reported increased uptake rates without a statistical test to prevent issues with small sample sizes and the absence of control groups, among others.
2.2.2. Codes relevant to social media campaigns for health
The first set of codes is relevant to health interventions but does not include those about social media campaigns. Hence, we developed a second set of codes for the factors commonly used in social media campaigns that successfully induce healthy behaviors. In other words, this second set of factors refers to the approaches adopted in social media campaigns to facilitate vaccination adherence. We term the codes “critical success factors” to refer to the requirements that foster the achievement of a project’s goal (Hoerbst & Schweitzer, 2015). To develop this set of codes, we reviewed successful social media health campaigns and extracted the factors commonly used in those campaigns. In addition, we checked whether these factors were used in the 92 immunization intervention studies (see the second-to-last rectangle in Fig. 1) to ensure that the selected factors were pertinent to immunization campaigns. This additional step for triangulation was necessary because not all social media health campaigns aimed to foster vaccination adherence, and we therefore needed to verify whether the factors were relevant to promoting immunization acceptance.
In our search for critical success factors, we recognized that prior successful social media campaigns strived to foster the audience’s sustained engagement with the content (Edney et al., 2018). Prior researchers have noted how challenging it is to garner endorsements from the public while competing against the copious amounts of content available on social media platforms. To foster engagement in health campaigns, researchers have suggested three strategies: (1) target messages to the identity of a sub-population with which the audience identifies; (2) use visual aids (such as imagery); and (3) foster social connections among participants (either recipient to recipient OR recipients to providers; Edney et al., 2018, Kostygina et al., 2020, Rus and Cameron, 2016).
The first strategy—i.e., message targeting—refers to the practice of customizing content to the identity of a sub-population group with which the individuals associate themselves and thus differs from that of personalizing messages in which content is adapted to an individual’s needs and preferences (Schmid et al., 2008). This targeting approach is anchored in the notion of social identity as related to shaping one’s choice of certain behaviors to fulfill the need to belong to a reference group (Shih and Huang, 2014, Stets and Burke, 2000, Walther et al., 2010).
Rus and Cameron’s (2016) study involving 10 diabetes-related Facebook groups demonstrated that messages targeted at the diabetes patients’ identities predict higher engagement among social media users. Message targeting has also been positively associated with increased vaccine uptake. Kim et al. (2020) created content featuring Korean American women sharing their stories and experiences of receiving the HPV vaccine. Young Korean-American women who viewed the video were twice as likely to report receiving the HPV vaccine or scheduling an appointment for the HPV vaccine as the control group of women who read factual information from the Centers for Disease Control (CDC). Lee et al. (2018) created culturally grounded content featuring Khmer-American mothers’ and daughters’ first-person stories about HPV and vaccination. Khmer-American girls who viewed the culturally grounded video reported a higher intention to receive HPV vaccination than the control group.
The second factor, the use of visual aids, is a strong predictor of recipients’ engagement in social media health campaigns (Edney et al., 2018, Kim et al., 2022, Rus and Cameron, 2016). A health campaign for activity trackers achieved higher engagement among the audience by featuring an image of the product (Edney et al., 2018). The use of visual aids also succeeded in increasing vaccination adherence: photographs of vaccine-preventable diseases stimulated uptake for parents with infants receiving recommended early childhood vaccines (Papachrisanthou et al., 2016). Dempsey and Zimet (2015) pinpointed image-heavy comic books and brochures as sources of information that raised vaccine rates among patients and parents. Papachrisanthou et al. (2016) demonstrated the effectiveness of visual educational materials in enhancing vaccination adherence among infants of low-income parents.
The third common factor is the use of social connection features embedded in social networking sites (Kostygina et al., 2020). Social media’s primary technical feature is networking, which connects individuals to other individuals (Boyd & Ellison, 2007). This sense of connection is conducive to motivating individuals to remain engaged with the campaigns, modify their behaviors, and adopt preventive behaviors. Harnessing social connections is thus a promising strategy for improving interest and engagement in health campaigns (Kostygina et al., 2020). In the prior immunization interventions, these connections were used to foster either patient-to-patient or patient-to-provider interactions. For example, Lott et al.'s (2020) review of HPV vaccine interventions targeting minority populations found that sharing information with mothers and daughters together at community dinners (Winer et al., 2016) was one of the most effective ways of raising HPV vaccination rates. In addition, interactive educational text messages, whereby parents could request additional information about the influenza vaccine from healthcare providers, significantly increased uptake rates among children compared with text-only communications (Hofstetter et al., 2015).
In addition to these three factors, several of the 15 social media campaigns used social media to supplement larger integrated interventions. For instance, Shropshire et al. (2013) operated a vaccine clinic on a college campus and used social media to encourage students to visit the clinic. As such, we added a new code to indicate whether the campaign was conducted primarily on a social media site or through another medium (including face-to-face interactions) supplemented by social media.
2.3. Coding processes
Two coders who were unaware of the research purposes were hired to analyze the 15 studies independently against the scheme presented in Table 2. The two coders had sufficient knowledge of and training in health communication and social media and were thus capable of understanding the coding scheme and applying it to each of the 15 studies. For the first seven attributes (Codes 1–7 in Table 2), the coders were instructed to honor the terms that the authors used in their articles. For instance, they were instructed to note the campaign site, such as New York City, New York, and then to find which region this site belongs to according to U.S. Census regional divisions and urbanicity. Likewise, for the last code, 11, the coders honored the authors’ descriptions of whether a social media platform was used as a primary site or as a supplement to the main intervention. As we followed the authors’ terms, there was little room for subjective interpretation.
In contrast, Codes 8, 9, and 10 required some degree of subjective judgment, as various terms were used to describe message targeting, visual aids, and social connection features. Thus, we checked the intercoder reliability between the two coders. Inter-coder reliability, measured in Cohen’s Kappa, was 82.9 %, which is considered strong in the social sciences (Miles & Huberman, 1994). Given this high intercoder reliability, we proceeded to analyze the results after minor disagreements were resolved between the coders.
3. Results
The summary of our analyses is presented in Table 3, Table 4 . Due to the small sample size (n = 15), our goal was to identify gaps in the existing literature and opportunities for conducting social media campaigns rather than reach a quantitative conclusion.
Table 3.
Results of Our Analyses of the 15 Campaigns along the Codes Related to Interventions.
| Authors | Target disease | Population(s) served | Region of the campaign site | Urbanicity of the site | Years of interventions | Intended outcomes | Significant increases in uptake rates |
|---|---|---|---|---|---|---|---|
| Hughes et al. (2020) | HPV | Male college students (over 18) at a large university |
|
None specified | 2016 |
|
Yes. A total of 16 males received the HPV vaccine during the four weeks preceding campaign recruitment and implementation. This increase was statistically significant (p < 0.05). |
| Bonnevie et al. (2020) | Influenza | African Americans and Hispanics (18–64). |
|
None specified | 2018–2019 |
|
Yes. Higher vaccination rates were reported among those who had seen the campaign than among those who had not seen it (p = 0.005). |
| Glanz et al. (2017) | Early childhood immunizations for babies up to 200 days old | Pregnant women in their third trimester who belong to Kaiser Permanente (18 or older) |
|
None specified | 2013–2016 |
|
Yes. Mean ranks for days under-vaccinated were significantly lower in the social-media arm versus control (p = 0.02) but not statistically different between the interactive web and control (p = 0.08) or between social media and interactive web arms (p = 0.63). Infants in the social media arm were more likely to be up to date than infants in the control arm (odds ratio [OR] = 1.92; 95 % confidence interval [CI], 1.07–3.47). |
| Daley et al. (2018) | General vaccine hesitancy | Women, recruited during pregnancy (18 or older) |
|
None specified | 2013–2016 |
|
Not applicable. The social media and interactive web interventions were associated with significant improvements in attitudes regarding vaccination benefits and significant reductions in parental concerns about vaccination risks compared to the control arm among vaccine-hesitant parents (p < 0.05). |
| Mohanty et al. (2018) | HPV | Adolescents (13–18) with a Facebook account and living in Philadelphia |
|
Urban | 2012–2013 |
|
Unclear. 176 doses of the HPV vaccine were administered to 152 unique adolescents, but no statistical testing was conducted. |
| Allen et al. (2020) | HPV | Women aged 18–26 years residing in low-come housing in Massachusetts |
|
Presumably Urban | 2019 |
|
Not applicable. There was no statistically significant change in the intent to be vaccinated in the next six months (p = 1.000) or 12 months (p = 0.617) after the campaign among those who had not yet started or completed vaccination. |
| Lee and Cho (2017) | HPV | College students (age 18–28) at a large university |
|
None specified | 2017 |
|
Not applicable. No statistically significant medium effect between newspaper and Facebook in terms of the intention to receive the vaccines (p = 0.94) |
| Brandt et al. (2020) | HPV | College students (aged 18–22) at a large university |
|
Urban | 2020 |
|
No. The awareness of the severity of HPV infections and the susceptibility to acquiring HPV increased significantly (p < 0.1), but the differences in HPV vaccination between the intervention and control groups were not significant. |
| Lyson et al. (2019) | HPV | Females aged 18 and older |
|
None specified | 2019 |
|
Not applicable. No significant increases in knowledge or behaviors among study participants upon conclusion of the study. |
| Ortiz et al. (2018) | HPV | Adolescents (13–18) |
|
None specified | None specified |
|
No. Knowledge has increased in some comparisons, but the vaccination rate itself did not increase to a statistically significant level. |
| Huang et al. (2018) | Influenza | Students on a college campus who consist mostly of young adults at a large university. |
|
None specified | 2011–2016 |
|
Yes. The enhanced intervention increased vaccinations by 85% (incidence rate ratio = 1.85, 95% CI 1.75–1.96). |
| Gerend et al. (2020) | HPV | Male and female college students (18 and up) in a large university. |
|
Urban | 2019 |
|
Unclear. Over a 75% increase in HPV vaccine doses administered to students in the 2018 vs 2019 spring semester was reported, but statistical significance was not tested. |
| Shropshire et al. (2013) | Influenza | College students at a large southern university. |
|
None specified | 2011–2012 |
|
Unclear. Nearly a 30% increase was seen in flu vaccination rates in Fall 2011 compared to Fall 2010, but no statistical test was conducted. |
| Sundstrom et al. (2018) | HPV | Women and men college students (aged 18–24) at a large university. |
|
Urban | 2014 |
|
Unclear. In total, 60% of participants who responded to an anonymous web-based survey evaluation indicated that they received the HPV vaccine because of campaign messages, but no statistical test was conducted. |
| Patel et al. (2014) | HPV | Young women (aged 19–26) who belong to nine Planned Parenthood health centers |
|
None specified | 2014 |
|
No. The reminder system did not increase completion rates (p = 0.881). |
Table 4.
Results of Our Analyses of the 15 Campaigns along the Codes Related to Critical Success Factors for Social Media Campaigns.
| Authors | Media Type | Primary vs Integrated | Message Targeting | Visual Aid | Social Connections |
|---|---|---|---|---|---|
| Hughes et al. (2020) |
|
Primary | Yes. Targeted male college students. |
|
Yes. Facebook groups were used. |
| Bonnevie et al. (2020) |
|
Primary | Yes. “Native advertising”–tailored messages to the style of that individual’s social feed. This style appears to reflect the ethnic minority group (African or Hispanic Americans) to which the individual belongs. |
|
Yes. Influencers used their existing connections with their followers to disseminate messages promoting flu shots. |
| Glanz et al. (2017) |
|
Primary (as one of the main treatment groups) | Yes. The vaccine content and website design were developed to reflect the needs and interests of pregnant women and the parents of young children. |
|
Yes. Social media technologies included a blog, discussion forum, chat room, and “Ask a Question” portal to ask experts questions if needed. |
| Daley et al. (2018) |
|
Primary (as one of the main treatment groups) | Yes. Same as Glanz et al. (2017) |
|
Yes. Same as Glanz et al. (2017) |
| Mohanty et al. (2018) |
|
Primary | Yes. Targeted the sense of the Philadelphia community. |
|
None Specified |
| Allen et al. (2020) |
|
Primary | None Specified |
|
None Specified |
| Lee and Cho (2017) |
|
Primary (as one of the main treatment groups) | None Specified |
|
None Specified |
| Brandt et al. (2020) |
|
Primary | Yes. The campaign messages emphasized college students with the time they had gained from preventing HPV and HPV-related cancer. |
|
Yes. The study investigators provided answers to the questions and stimulated interactions. |
| Lyson et al. (2019) |
|
Primary | None Specified |
|
Yes. Participants could share their messages with their online group, and everyone could then comment on the shared messages. |
| Ortiz et al. (2018) |
|
Primary | None Specified |
|
None specified |
| Huang et al. (2018) |
|
Integrated | Yes. A personalized social media campaign designed to appeal to students’ community identities. |
|
Yes. Outreach through dormitory-specific email lists and social media sites |
| Gerend et al. (2020) |
|
Integrated | Yes, campaign materials incorporated university colors. |
|
None specified, although student-and-clinician communications were encouraged. |
| Shropshire et al. (2013) |
|
Integrated | None specified |
|
Yes. A Facebook event was created by the College of Public Health. |
| Sundstrom et al. (2018) |
|
Integrated | Yes. Messages were based on the HBM and understanding of the target audience. |
|
None specified |
| Patel et al. (2014) |
|
Integrated | None specified |
|
None specified |
3.1. Analyses of campaigns along the codes relevant to interventions
We found disparities in campaigns in several areas, most notably target diseases, populations, and regions. As shown in Fig. 3 and Table 3, except for one study that did not specify a vaccine type, the extant campaigns have addressed only three immunizations: HPV, influenza, and early childhood immunization. HPV received the most attention (10 out of 15 studies). Given that it is recommended that a series of HPV shots be started in adolescence (Markowitz et al., 2014), the subpopulation groups served in these 15 studies are concentrated on those aged 13–17 years, 18–26 years, and college students. In addition, perhaps due to lower influenza immunization rates among African Americans (40.4 %) compared to non-Hispanic White adults (55.5 %)2 , racial minority women were studied (Bonnevie et al., 2020). Pregnant women were also included (Glanz et al., 2017). No other vaccines or subpopulation groups were studied (Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9 ).
Fig. 3.
Breakdown of 15 studies by Target Disease and Vaccine Types.
Fig. 4.
Breakdown of 15 studies by subpopulation groups served.
Fig. 5.
Breakdown of 15 studies by the regions of campaign sites (some conducted in more than one region).
Fig. 6.
Breakdown of 15 studies by intended outcomes.
Fig. 7.
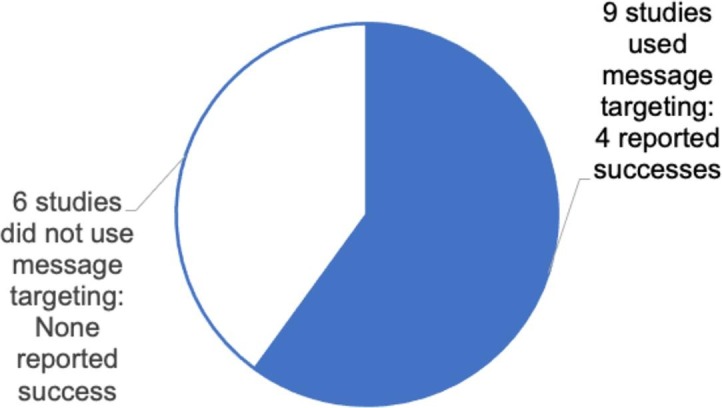
Use of message targeting in 15 studies.
Fig. 8.

Use of visual aids in 15 studies.
Fig. 9.

Use of social features in 15 studies.
We found a similar disparity in terms of campaign region. The South received the most attention (7), followed by the Northeast (3), the West (3), and the Midwest (1) and the Pacific (1). Likewise, most of these studies were conducted in urban areas, and no study was conducted in rural areas or reservations.
In terms of the years in which interventions were conducted, we found a slight increase around 2014–2016 (6), but the interventions were otherwise spread throughout the years.
Finally, most studies (11) intended to increase uptake rates as the final outcome of their campaigns. The other intended outcomes included cognition, attitudes, and intentions, in line with the HBM. Other than one study that used metrics in Google Analytics (Bonnevie et al., 2020), no other social media–specific outcomes, such as virality, influence, or conversion rate (i.e., intent-to-vaccinate rate), were mentioned.
Despite having increased uptake rates as the final intended outcome in 11 of these campaigns, only three studies reported significant increases in immunization behaviors. The rest of the studies in which vaccination uptake rates were measured reported either non-significant increases or did not conduct any statistical testing for various reasons. Even among studies that had other intended outcomes, only one (Daley et al., 2018) reported significant improvements in those variables.
3.2. Analyses of the campaigns along codes related to social media campaigns for health
We found similar disparities regarding the three critical success factors of social media campaigns (Table 4). First, we found that 11 studies used social media as the main site to conduct campaigns, while the remaining four used social media to aid the main campaigns conducted elsewhere.
As shown in Table 4, more than half of the studies used message targeting for sub-population groups. For instance, Hughes et al. (2020) customized their messages to the identity of male college students regarding how to guard their future against HPV infections. Targeting messages to the identities of the universities in which the campaigns were conducted was found by Gerend et al., 2020, Huang et al., 2018, and Sundstrom et al. (2018). In addition, messages were targeted according to the identities of racial subgroups, age groups, and geographic regions. Bonnevie et al. (2020) utilized “native advertising,” wherein targeted messaging reflected the style of content in participants’ social media feeds. Since this campaign targeted African- and Hispanic-American racial subgroups that use distinctive terminologies rooted in their cultures (Kim et al., 2021), the messages appeared to be customized for these racial minority groups. Likewise, Glanz et al. (2017) targeted their messages to prenatal women’s lifestyles, interests, and concerns, and Mohanty et al. (2018) appealed to the sense of belonging to the Philadelphia community. The rest of the studies (6 out of 15) did not target their messages to the identities of the subgroups their interventions targeted.
The use of visual aids has been underutilized, with only five studies adopting any sort of imagery in their campaigns. Hughes et al., 2020, Bonnevie et al., 2020 posted informative videos on social media sites, and Sundstrom et al. (2018) posted infographics through social media to provide facts and statistics about HPV. Huang et al.’s (2018) campaign disseminated posters that featured visuals of university mascots and college students via social media sites. The remaining studies (10 out of 15) did not adopt visual aids.
Lastly, more than half of the campaigns adopted social media’s connecting features to facilitate connections among participants. Hughes et al. (2020) used Facebook groups, and Lyson et al. (2019) used other social-media groups to encourage participants to share their messages with other members. Shropshire et al. (2013) created a Facebook event to promote a vaccine clinic to an existing social network within an academic department. Some researchers have also used social connections to facilitate connections between participants and campaign administrators (including healthcare providers). For example, Glanz et al., 2017, Daley et al., 2018 created an “Ask a Question” page where participants could directly ask healthcare experts questions about vaccinations. Bonnevie et al. (2020) facilitated connections between their hired social media influencers and the influencers’ followers to disseminate messages encouraging the acceptance of influenza vaccines. Brandt et al. (2020) provided answers to participants’ questions to stimulate interactions on social media. Huang et al. (2018) conducted outreach activities by leveraging networks on the college dormitory’s social media sites. However, the rest of the studies (7 out of 15) did not use any features for social connections.
4. Discussion
The first purpose of this discussion section is to delineate both the practical implications and future research opportunities drawn from our analyses of the 15 social media campaigns. The second objective is to illustrate how our systematic review contributes to advancing theories of social influence and HBM within the nomological network of the existing body of literature. We also noted the limitations of this study.
4.1. Implications and research questions for fostering vaccination adherence
4.1.1. Underutilization of social media campaigns for immunization
Our systematic review identified only 15 social media campaigns from 92 media-related studies. This small number of social media campaigns suggests that most interventions still rely on older media, such as reminder-recall cards, phone calls, text messages, vaccination sites, and in-person education. Moreover, of the 15 studies, only 10 campaigns used social media as their primary medium, while the remainder adopted social media as a secondary aid. Although digital health is suggested as a solution to alleviate health disparities in underserved populations by enhancing care coordination, quality, and cost-effectiveness (Brewer et al., 2020), our analyses reveal that social media campaigns are still underutilized for immunizations.
Informatics researchers should consider applying accumulated knowledge of social media’s advantages in reaching, engaging, persuading, and inducing positive behavioral changes among broader audiences (Xie et al., 2022). This wealth of knowledge regarding social media’s capacity will help resolve one of the most resilient challenges in public health: immunization. Toward this end, we suggest the following research question:
-
•
Can existing knowledge of social media’s affordances for broad scope and high speed of reach, persuasion, and behavioral modifications be applied to alleviate pervasive vaccine hesitancy and instead foster vaccination adherence?
4.1.2. The need to expand the coverage of social media campaigns
As shown in Table 3, most social media campaigns thus far have concentrated on HPV vaccines. This focus on HPV may be attributed to the newer approval of an HPV vaccine in 2014 and the subsequent expansion of the age range recommended to receive the vaccine. More specifically, the Food and Drug Administration approved Gardasil 9 in December 2014, and the Federal Advisory Committee on Immunization Practices recommended that all girls and boys receive the vaccine at age 11 or 12 or as early as age nine, and that adolescents and young adults aged 13–26 be given a “catch-up” vaccination (Markowitz et al., 2014). As such, a disproportionate amount of attention was given to HPV and younger recipients of inoculation. Simultaneously, given that social media usage rates are higher among younger individuals than among older individuals (Pew Research, 2019), social media campaigns have targeted the former.
In contrast, other vaccines have received tangential attention, although the uptake rates of these vaccines show large variances across regions, urbanicity, and age groups. For instance, the majority of campaigns were conducted in the South and Northeast, whereas only one campaign was conducted in the Midwest and the Pacific. Furthermore, all campaigns were carried out in urban areas, with none in rural areas. The negligence of specific regions and rural areas, combined with age groups, can exacerbate disparities in vaccination coverage. Specifically, pneumococcal vaccination for older adults has demonstrated substantial differences across the urbanicity of regions (Gatwood et al., 2020, Talbert et al., 2018, Tsai et al., 2021). The overall mean vaccination rate for pneumococcal vaccines among the elderly (aged 65 or older) in urban areas was 40 % higher than in rural communities (Talbert et al., 2018).
Hence, there is a critical need to expand the coverage of vaccination campaigns via social media campaigns, given that usage rates of social media have expanded to include groups from younger individuals to older adults in broader regions (Pew Research Center, 2021). In 2021, 50 % of individuals aged 65 or older used Facebook, which has more than quadrupled since 2010, when 11 % of individuals aged 65 or older used any type of social media (Pew Research Center, 2021). Likewise, 66 % of rural residents used social media in 2021, compared to 39 % in 2010 (Pew Research Center, 2021). Expanding the scope of social media campaigns will contribute to counteracting vaccine hesitancy. Accordingly, we propose the following research question:
-
•
Does social media succeed in alleviating vaccine hesitancy and fostering vaccination adherence in these harder-to-reach populations, including the elderly, who reside in rural areas?
4.1.3. The need to develop measurement tools appropriate for social media campaigns
Most of the studied interventions (11 out of 15) aimed to increase or measure uptake rates as an outcome of the campaigns. Of these 11 studies, four interventions succeeded in increasing uptake rates, three failed, and the remaining four did not conduct the statistical testing required for us to assess their significant efficacy. Additionally, even in the four studies that aimed not to increase uptake rates but rather to enhance other process variables (such as knowledge, attitudes, and behavioral intentions), only one achieved its goals.
These results may suggest that social media campaigns are ineffective for inoculation. Rather, we believe that the results indicate a need to evaluate whether the existing measures are appropriate for assessing the success of social media campaigns for immunization. All 15 campaigns measured the effectiveness of the interventions immediately after the conclusion of an active campaign without considering any potential latent impact from the campaign over time. This approach, without considering the timing of the assessment, overlooks an important aspect of how social media campaigns diffuse their influence, according to the theory of social influence. Social media campaigns disseminate interventions via networks of connected people through a process called “cascading” (Aral and Dhillon, 2018, Kempe et al., 2005). The cascading model explains how social contagion or “word-of-mouth” diffusion occurs via digital social networks (Aral and Dhillon, 2018, Kempe et al., 2005). The timeframe over which cascading occurs is a crucial consideration (Aral & Walker, 2014). For example, a node, u, becomes active at time t; u can then influence an inactive neighbor v and cause v to become potentially influential at t + 1 (Kempe et al., 2005). In addition, prior researchers have noted the importance of identifying the timeframe in which interventions should be delivered to optimize the efficacy of interventions for the Ebola virus (Echeng and Delphine Rexson, 2018).
Nonetheless, all 15 campaigns examined the effectiveness of their campaigns immediately after the conclusion of their interventions, which could potentially fail to capture the actual effects of campaigns that could have been observed after a lapse of time. In their empirical investigations of social influence on Instagram, Argyris et al. (2020) demonstrated that a node’s influence occurred over two years. Although this time interval can be negligible in some cases, as shown in the viral spread of content, the time interval is an important factor in the context of vaccines that must be administered at predefined timeframes. Examples of these vaccines are HPV (two doses with a six-month interval between the two), some COVID-19 vaccines (one month between the doses), and most childhood booster shots. Thus, a time interval must be included when measuring the effectiveness of a social media campaign to represent the campaign’s effectiveness fully, which will eventually help expand the theory of social influence. As such, the following research questions are proposed:
-
•
What is an appropriate timeframe to measure the effectiveness of a social media campaign for immunization? How long will it take for campaigns to promote vaccine acceptance?
-
•
How does this timeframe interact with different types of vaccines that require an interval between doses? How does it interact with vaccines recommended for administration at intervals?
Another challenge in measuring the effectiveness of social media campaigns is using scales developed based on the HBM. The HBM was developed in the early 1950s to understand people’s failure to adopt disease-prevention measures (LaMorte, 2019). Accordingly, the outcome variables encompass knowledge about contagious diseases, the severity of the diseases, the efficacy of vaccines, self-efficacy in making vaccination decisions, and intentions to adopt the vaccines; all these choices assume rational decision-making. Vaccine hesitancy, however, refers to emotional resistance to adopting vaccines, which cannot be explained using the rational constructs included in the HBM (Larson et al., 2022). Furthermore, multiple social media content with ulterior political motives often propagate vaccine hesitancy (Zakharchenko et al., 2022). Thus, developing and including an updated and expanded scale on vaccine hesitancy in survey instruments is crucial to capturing the irrational and multidimensional nature of vaccine hesitancy and to expanding HBM into the realm of emotional decision-making. In this regard, the following research questions are proposed:
-
•
What is a suitable instrument for measuring vaccine hesitancy or the emotional decision to delay or refuse immunization despite having access to it?
-
•
How is vaccine hesitancy integrated into the existing framework of the HBM, which assumes rational decision-making?
Finally, no past studies have included any success indicators for social media campaigns, excluding Bonnevie et al. (2020), who used an existing generic analytics tool (i.e., Google Analytics). On the contrary, several attempts have recently been made to measure the impact of social media posts on decision-making and behavioral changes in other fields. These metrics include well-known measures, such as impressions (number of views), reach (the number of people who have viewed content), engagement count (the number of likes, comments, and shares on posts), and share count (the number of times content was reposted or shared). In addition, these metrics have recently been expanded to include virality scores (the extent to which a post is reproduced and diffused) and social influence scores (the influence of a post in encouraging people to vaccinate). Developments and refinements of these metrics will benefit researchers’ ability to capture the effectiveness of social media campaigns. Accordingly, the following questions are proposed for future research:
-
•
How do we operationalize the virality score, social influence score, and conversion rate (i.e., intent to vaccinate)?
-
•
How do we demonstrate a causal relationship between exposure to social media campaigns and vaccine acceptance?
4.1.4. Need to adopt critical success factors for social media campaigns
The 15 studied interventions seldom used all three common success factors ([1] targeting messages to the identities of the subpopulation, [2] the use of visual aids, and [3] the use of social connection features). As noted earlier, targeting messages to a sub-population group’s identity and using social connection features to foster interactions among participants increased the participants’ engagement in the content. Moreover, the use of visual aids is pertinent to immunization campaigns because visual aids are processed faster, receive selective attention, and are retained longer in memory than texts (Geniole et al., 2022, Peterson et al., 2017). Visual aids are, therefore, persuasive among those with lower digital literacy and a high level of vaccine hesitancy. Along this line, future researchers should consider the following questions:
-
•
Does using all critical success factors enhance the effectiveness of social media campaigns for immunization? Would these effects vary across audiences’ demographic factors?
-
•
Are there interactions among the three critical success factors, such that using one factor augments or hampers the effectiveness of the other two?
-
•
Are there any other critical social media success factors that can enhance the effectiveness of immunization campaigns?
4.2. Contributions and limitations
This systematic review provides contributions to generalizable scientific knowledge. First, this review expands on the current literature on social media campaigns for health and suggests the critical need to accumulate more research and develop a proper measurement for assessing social media campaigns. We identified gaps in existing social media–based immunization campaigns and proposed specific research questions as a first step toward meeting these needs. These questions will help informatics researchers explore social media in specific and digital health in general to solve a substantial challenge in public health.
In addition, we described how researchers could expand theories through research on social media campaigns for immunization. Specifically, this research contributes to advancing theories of social influence by identifying the time interval needed for cascading recommendations through social networks. In addition, this research contributes to expanding the HBM by integrating irrational and multidimensional vaccine hesitancy into the current rational decision-making model for adopting preventive behaviors.
Moreover, the coding scheme we developed facilitates the identification of critical success factors in social media campaigns. The three common success factors and detailed descriptions of how they can be adopted in social media vaccination campaigns can be translated into a unique set of affordances for social media in inducing behavioral modifications.
Finally, this review expands the extant knowledge regarding vaccine hesitancy and adherence. By demonstrating lower success rates of prior interventions, we clearly showed the resilience of vaccine hesitancy, corroborating Larson et al.’s (2022) argument. Larson et al. (2022) have challenged the prevailing unidimensional views about vaccine hesitancy, equating it with misjudgment or a flawed decision, and instead have argued that vaccine hesitancy is a firm belief cultivated and reinforced by diverse factors (such as politics, religion, culture, and lifestyle) in our society (Zakharchenko et al., 2022). Additionally, our results showing how a small number of interventions succeeded, in comparison to a large number of failed campaigns, provide insight into designing an efficacious intervention. For example, we have shown that interventions with targeted messages to the subpopulation’s identities have often been successful. This finding advances Calo et al.’s (2021) results that social media messages that appeal to herd immunity significantly increase individuals’ intentions to accept vaccinations. Similarly, Lazić et al. (2021)’s online experiment showed that nudges to inform participants of the social benefits of herd immunity effectively increased vaccination intentions among participants. Expanding these findings obtained from experiments, our review has shown that cultivating the sentiment of a community can be a useful message to promote vaccination adherence among the public.
Like any other study, this study has limitations. Among others, we should note that we did not conduct inductive coding but opted for deductive coding. Given the small number of interventions we found, inductive coding could have been helpful because it allowed for extracting meanings, themes, and theories from a dataset (Corbin & Strauss, 2008). However, we chose deductive coding to obtain the aim of this study, which is to examine the effectiveness of these campaigns in facilitating vaccineation adherence. As more research is being accumulated on social media campaigns to counter vaccine hesitancy, future researchers may consider applying inductive coding to extract deeper meanings of prior interventions.
Declaration of Competing Interest
The authors have no competing interest to report.
Acknowledgements
This study was supported by the National Institutes of Health, National Library of Medicine (1R21LM013638-01) and the Diversity Research Network's Launch Award Program at Michigan State University.
Footnotes
Data availability
No data was used for the research described in the article.
References
- Al-Fraihat D., Joy M., Masadeh R., Sinclair J. Evaluating E-learning systems success: An empirical study. Comput. Hum. Behav. 2020;102:67–86. doi: 10.1016/j.chb.2019.08.004. [DOI] [Google Scholar]
- Allen J.D., Hollander J., Gualtieri L., Alarcon Falconi T.M., Savir S., Agénor M. Feasibility of a twitter campaign to promote HPV vaccine uptake among racially/ethnically diverse young adult women living in public housing. BMC Public Health. 2020;20(1):830. doi: 10.1186/s12889-020-08824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aral S., Dhillon P.S. Social influence maximization under empirical influence models. Nat. Hum. Behav. 2018;2(6):375–382. doi: 10.1038/s41562-018-0346-z. [DOI] [PubMed] [Google Scholar]
- Aral S., Walker D. Tie Strength, Embeddedness, and Social Influence: A Large-Scale Networked Experiment. Manage. Sci. 2014;60(6):1352–1370. doi: 10.1287/mnsc.2014.1936. [DOI] [Google Scholar]
- Argyris Y.A., Wang Z., Kim Y., Yin Z. The effects of visual congruence on increasing consumers’ brand engagement: An empirical investigation of influencer marketing on Instagram using deep-learning algorithms for automatic image classification. Comput. Hum. Behav. 2020;112 doi: 10.1016/j.chb.2020.106443. [DOI] [Google Scholar]
- Asare M., Popelsky B., Akowuah E., Lanning B.A., Montealegre J.R. Internal and external validity of social media and mobile technology-driven HPV vaccination interventions: systematic review using the reach, effectiveness, adoption, implementation, maintenance (RE-AIM) framework. Vaccines. 2021;9(3):197. doi: 10.3390/vaccines9030197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg F., Rice J., Dickmeis A. Emotions, Technology, and Social Media. Academic Press; 2016. Chapter 6—Social media as a venue for emotion regulation among adolescents; pp. 105–116. [DOI] [Google Scholar]
- Bonnevie E., Rosenberg S.D., Kummeth C., Goldbarg J., Wartella E., Smyser J. Using social media influencers to increase knowledge and positive attitudes toward the flu vaccine. PLoS One. 2020;15(10):e0240828. doi: 10.1371/journal.pone.0240828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd D.M., Ellison N.B. Social Network Sites: Definition, History, and Scholarship. J. Comput.-Mediat. Commun. 2007;13(1):210–230. doi: 10.1111/j.1083-6101.2007.00393.x. [DOI] [Google Scholar]
- Brandt H.M., Sundstrom B., Monroe C.M., Turner-McGrievy G., Larsen C., Stansbury M., Magradey K., Gibson A., West D.S. Evaluating a Technology-Mediated HPV Vaccination Awareness Intervention: A Controlled, Quasi-Experimental, Mixed Methods Study. Vaccines. 2020;8(4):749. doi: 10.3390/vaccines8040749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer L.C., Fortuna K.L., Jones C., Walker R., Hayes S.N., Patten C.A., Cooper L.A. Back to the Future: Achieving Health Equity through Health Informatics and Digital Health. JMIR Mhealth Uhealth. 2020;8(1):e14512. doi: 10.2196/14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calo W.A., Gilkey M.B., Shah P.D., Dyer A.-M., Margolis M.A., Dailey S.A., Brewer N.T. Misinformation and other elements in HPV vaccine tweets: An experimental comparison. J. Behav. Med. 2021;44(3):310–319. doi: 10.1007/s10865-021-00203-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates J.R., Shafer A., Diehl S.J., Deal A.M. Evaluating a County-Sponsored Social Marketing Campaign to Increase Mothers’ Initiation of HPV Vaccine for Their Preteen Daughters in a Primarily Rural Area. Soc. Mark. Q. 2011;17(1):4–26. doi: 10.1080/15245004.2010.546943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooney F., Ryan A., Schinaia N., Breslin A. Using electronic mail to improve MMR uptake amongst third level students. Ir. Med. J. 2010;103(3):72–74. [PubMed] [Google Scholar]
- Corbin J., Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. SAGE. 2008 doi: 10.4135/9781452230153. [DOI] [Google Scholar]
- Crocker-Buque T., Mindra G., Duncan R., Mounier-Jack S. Immunization, urbanization and slums—A systematic review of factors and interventions. BMC Public Health. 2017;17(1) doi: 10.1186/s12889-017-4473-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley, M. F., Narwaney, K. J., Shoup, J. A., Wagner, N. M., & Glanz, J. M. (2018). Addressing parents’ vaccine concerns: A randomized trial of a social media intervention. Am. J. Prevent. Med., 55(1), Article 1. http://dx.doi.org.proxy1.cl.msu.edu/10.1016/j.amepre.2018.04.010. [DOI] [PMC free article] [PubMed]
- Dempsey, A.F., & Zimet, G.D., 2015. Interventions to improve adolescent vaccination: What may work and what still needs to be tested. Am. J. Prevent. Med., 49(6, Suppl 4), S445–S454. https://doi.org/10.1016/j.ame3pre.2015.04.013. [DOI] [PubMed]
- Echeng B.B, Delphine Rexson B. Optimal Control Dynamics: Control Interventions for Eradication of Ebola Virus Infection. Int. J. Math. Sci. Comput. 2018;4(3):42–65. doi: 10.5815/ijmsc.2018.03.04. [DOI] [Google Scholar]
- Edney S., Bogomolova S., Ryan J., Olds T., Sanders I., Maher C. Creating Engaging Health Promotion Campaigns on Social Media: Observations and Lessons from Fitbit and Garmin. J. Med. Internet Res. 2018;20(12):e10911. doi: 10.2196/10911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcone A.L. Improving influenza immunization rates in the uninsured. J. Am. Assoc. Nurse Pract. 2019;31(7):391–395. doi: 10.1097/JXX.0000000000000166. [DOI] [PubMed] [Google Scholar]
- Gatwood J., Shuvo S., Hohmeier K.C., Hagemann T., Chiu C.-Y., Tong R., Ramachandran S. Pneumococcal vaccination in older adults: An initial analysis of social determinants of health and vaccine uptake. Vaccine. 2020;38(35):5607–5617. doi: 10.1016/j.vaccine.2020.06.077. [DOI] [PubMed] [Google Scholar]
- Geniole S.N., Bird B.M., Witzel A., McEvoy J.T., Proietti V. Preliminary evidence that brief exposure to vaccination-related internet memes may influence intentions to vaccinate against COVID-19. Comput. Hum. Behav. 2022;131 doi: 10.1016/j.chb.2022.107218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend M.A., Murdock C., Grove K. An intervention for increasing HPV vaccination on a university campus. Vaccine. 2020;38(4):725–729. doi: 10.1016/j.vaccine.2019.11.028. [DOI] [PubMed] [Google Scholar]
- Glanz J.M., Wagner N.M., Narwaney K.J., Kraus C.R., Shoup J.A., Xu S., O’Leary S.T., Omer S.B., Gleason K.S., Daley M.F. Web-based Social Media Intervention to Increase Vaccine Acceptance: A Randomized Controlled Trial. Pediatrics. 2017;140(6):e20171117. doi: 10.1542/peds.2017-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerbst A., Schweitzer M. A Systematic Investigation on Barriers and Critical Success Factors for Clinical Information Systems in Integrated Care Settings. Yearb. Med. Inform. 2015;24(01):79–89. doi: 10.15265/IY-2015-018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter A.M., Vargas C.Y., Camargo S., Holleran S., Vawdrey D.K., Kharbanda E.O., Stockwell M.S. Impacting delayed pediatric influenza vaccination: A randomized controlled trial of text message reminders. Am. J. Prev. Med. 2015;48(4):392–401. doi: 10.1016/j.amepre.2014.10.023. [DOI] [PubMed] [Google Scholar]
- Huang J.J., Francesconi M., Cooper M.H., Covello A., Guo M., Gharib S.D. Community health workers on a college campus: Effects on influenza vaccination. J. Am. Coll. Health. 2018;66(4):317–323. doi: 10.1080/07448481.2018.1440582. [DOI] [PubMed] [Google Scholar]
- Hughes C.T., Kirtz S., Ramondetta L.M., Lu Q., Cho D., Katzin C., Kahlor L.A. Designing and Implementing an Educational Social Media Campaign to Increase HPV Vaccine Awareness among Men on a Large College Campus. Am. J. Health Educ. 2020;51(2):87–97. doi: 10.1080/19325037.2020.1722297. [DOI] [Google Scholar]
- Jarrett C., Wilson R., O’Leary M., Eckersberger E., Larson H.J. Strategies for addressing vaccine hesitancy – a systematic review. Vaccine. 2015;33(34):4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- Kempe D., Kleinberg J., Tardos É. In: Caires L., Italiano G.F., Monteiro L., Palamidessi C., Yung M., editors. vol. 3580. Springer; Berlin Heidelberg: 2005. Influential Nodes in a Diffusion Model for Social Networks; pp. 1127–1138. (Automata, Languages and Programming). [DOI] [Google Scholar]
- Kim M., Lee H., Kiang P., Aronowitz T., Sheldon L.K., Shi L., Allison J. A Storytelling Intervention in a Mobile, Web-Based Platform: A Pilot RCT to Evaluate the Preliminary Effectiveness to Promote HPV Vaccination in Korean American College Women. Health Educ. Behav. 2020;47(2):258–263. doi: 10.1177/1090198119894589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Park S.Y., Robert L.P. Bridging the Health Disparity of African Americans Through Conversational Agents. Digital Govern.: Res. Practice. 2021;2(1):1–7. doi: 10.1145/3428122. [DOI] [Google Scholar]
- Kim S.C., Zhao X., Brophy N.S., Walker M.W., Alexander T.N. Visual Attention to the Source Matters: Using Eye Tracking to Understand the FDA’s ‘Every Try Counts’ Campaign Message Effectiveness. Nicotine Tob. Res. 2022;24(2):280–284. doi: 10.1093/ntr/ntab185. [DOI] [PubMed] [Google Scholar]
- Kostygina, G., Tran, H., Binns, S., Szczypka, G., Emery, S., Vallone, D., Hair, E., 2020. Boosting Health Campaign Reach and Engagement through Use of Social Media Influencers and Memes. Social Media + Society, 6(2), 2056305120912475. https://doi.org/10.1177/2056305120912475.
- Krippendorff, K. (1980). Validity in Content Analysis. In Computerstrategien für die Kommunikationsanalyse (E. Mochmann, pp. 69–112). Campus-Verlag. https://repository.upenn.edu/asc_papers/291.
- LaMorte, W. (2019, 9). The Health Belief Model. Behavioral Change Models, Boston University School of Public Health. https://sphweb.bumc.bu.edu/otlt/mph-modules/sb/behavioralchangetheories/behavioralchangetheories2.html.
- Larson H.J., Gakidou E., Murray C.J.L. The vaccine-hesitant moment. N. Engl. J. Med. 2022;387(1):58–65. doi: 10.1056/NEJMra2106441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazić A., Kalinova K.N., Packer J., Pae R., Petrović M.B., Popović D., Sievert D.E.C., Stafford-Johnson N. Social nudges for vaccination: How communicating herd behaviour influences vaccination intentions. Br. J. Health Psychol. 2021;26(4):1219–1237. doi: 10.1111/bjhp.12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M.J., Cho J. Promoting HPV vaccination online: Message design and media choice. Health Promot. Pract. 2017;18(5):645–653. doi: 10.1177/1524839916688229. [DOI] [PubMed] [Google Scholar]
- Lee H., Kim M., Cooley M.E., Kiang P.-N.-C., Kim D., Tang S., Shi L., Thiem L., Kan P., Peou S., Touch C., Chea P., Allison J. Using narrative intervention for HPV vaccine behavior change among Khmer mothers and daughters: A pilot RCT to examine feasibility, acceptability, and preliminary effectiveness. Appl. Nurs. Res. 2018;40:51–60. doi: 10.1016/j.apnr.2017.12.008. [DOI] [PubMed] [Google Scholar]
- Lott B.E., Okusanya B.O., Anderson E.J., Kram N.A., Rodriguez M., Thomson C.A., Rosales C., Ehiri J.E. Interventions to increase uptake of Human Papillomavirus (HPV) vaccination in minority populations: A systematic review. Prev. Med. Rep. 2020;19 doi: 10.1016/j.pmedr.2020.101163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyson H.C., Le G.M., Zhang J., Rivadeneira N., Lyles C., Radcliffe K., Pasick R.J., Sawaya G., Sarkar U., Centola D. Social Media as a Tool to Promote Health Awareness: Results from an Online Cervical Cancer Prevention Study. J. Cancer Educ. 2019;34(4):819–822. doi: 10.1007/s13187-018-1379-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz, L.E., Dunne, E.F., Saraiya, M., Chesson, H.W., Curtis, C.R., Gee, J., Bocchini, J.A., Unger, E.R., Centers for Disease Control and Prevention (CDC), 2014. Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep., 63(RR-05), 1–30. [PubMed]
- Mayring P. Qualitative content analysis. Forum Qual. Sozialforschung/Forum: Qualitative Soc. Res. 2000;1(2) doi: 10.17169/fqs-1.2.1089. [DOI] [Google Scholar]
- Miles, M.B., Huberman, A.M., 1994. Qualitative Data Analysis: An Expanded Sourcebook (2nd ed.). SAGE Publications, Inc. https://psycnet.apa.org/record/1995-97407-000.
- Mohanty S., Leader A.E., Gibeau E., Johnson C. Using Facebook to reach adolescents for human papillomavirus (HPV) vaccination. Vaccine. 2018;36(40):5955–5961. doi: 10.1016/j.vaccine.2018.08.060. [DOI] [PubMed] [Google Scholar]
- Niccolai L.M., Hansen C.E. Practice- and Community-Based Interventions to Increase Human Papillomavirus Vaccine Coverage: A Systematic Review. JAMA Pediatr. 2015;169(7):686. doi: 10.1001/jamapediatrics.2015.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nour, R. (2019). A Systematic Review of Methods to Improve Attitudes towards Childhood Vaccinations. Cureus, 11(7), Article 7. https://doi.org/10.7759/cureus.5067. [DOI] [PMC free article] [PubMed]
- Odone A., Ferrari A., Spagnoli F., Visciarelli S., Shefer A., Pasquarella C., Signorelli C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: A systematic review. Hum. Vaccin. Immunother. 2015;11(1):72–82. doi: 10.4161/hv.34313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz, R.R., Shafer, A., Cates, J., Coyne-Beasley, T., 2018. Development and evaluation of a social media health intervention to improve adolescents’ knowledge about and vaccination against the Human Papillomavirus. Global Pediatric Health, 5, 2333794X1877791. https://doi.org/10.1177/2333794X18777918. [DOI] [PMC free article] [PubMed]
- Ortiz R.R., Smith A., Coyne-Beasley T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccin. Immunother. 2019;15(7–8):1465–1475. doi: 10.1080/21645515.2019.1581543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ou L., Youngstedt S.D. The Role of Vaccination Interventions to Promote HPV Vaccine Uptake Rates in a College-Aged Population: A Systematic Review. J. Cancer Educ. 2020 doi: 10.1007/s13187-020-01806-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papachrisanthou M.M., Lorenz R.A., Loman D.G. Increasing Immunization Adherence Among Infants of Low-income Parents: The Effects of Visually Enhanced Education. J. Nurse Pract. 2016;12(5):304–310. doi: 10.1016/j.nurpra.2015.12.021. [DOI] [Google Scholar]
- Patel A., Stern L., Unger Z., Debevec E., Roston A., Hanover R., Morfesis J. Staying on track: A cluster randomized controlled trial of automated reminders aimed at increasing human papillomavirus vaccine completion. Vaccine. 2014;32(21):2428–2433. doi: 10.1016/j.vaccine.2014.02.095. [DOI] [PubMed] [Google Scholar]
- Peterson M., Wise K., Ren Y., Wang Z., Yao J. Memorable Metaphor: How Different Elements of Visual Rhetoric Affect Resource Allocation and Memory for Advertisements. J. Curr. Issues Res. Advert. 2017;38(1):65–74. doi: 10.1080/10641734.2016.1233155. [DOI] [Google Scholar]
- Pew Research Center. (2021, April 7). Social Media Fact Sheet. https://www.pewresearch.org/internet/fact-sheet/social-media/?menuItem=2fc5fff9-9899-4317-b786-9e0b60934bcf.
- Pew Research. (2019, June 12). Demographics of Social Media Users and Adoption in the United States [References]. https://www.pewresearch.org/internet/fact-sheet/social-media/.
- Rus H.M., Cameron L.D. Health Communication in Social Media: Message Features Predicting User Engagement on Diabetes-Related Facebook Pages. Ann. Behav. Med. 2016;50(5):678–689. doi: 10.1007/s12160-016-9793-9. [DOI] [PubMed] [Google Scholar]
- Schmid K.L., Rivers S.E., Latimer A.E., Salovey P. Targeting or tailoring? Mark. Health Serv. 2008;28(1):32–37. [PMC free article] [PubMed] [Google Scholar]
- Shih H.-P., Huang E. Influences of Web interactivity and social identity and bonds on the quality of online discussion in a virtual community. Inf. Syst. Front. 2014;16(4):627–641. doi: 10.1007/s10796-012-9376-7. [DOI] [Google Scholar]
- Shropshire A.M., Brent-Hotchkiss R., Andrews U.K. Mass media campaign impacts influenza vaccine obtainment of university students. J. Am. Coll. Health. 2013;61(8) doi: 10.1080/07448481.2013.830619. Article 8. [DOI] [PubMed] [Google Scholar]
- Smulian E.A., Mitchell K.R., Stokley S. Interventions to increase HPV vaccination coverage: A systematic review. Hum. Vaccin. Immunother. 2016;12(6) doi: 10.1080/21645515.2015.1125055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stets J.E., Burke P.J. Identity theory and social identity theory. Soc. Psychol. Q. 2000:224–237. [Google Scholar]
- Sundstrom B., Brandt H.M., Gray L., Young Pierce J. It’s My Time: Applying the health belief model to prevent cervical cancer among college-age women. JCOM. 2018;22(2):161–178. doi: 10.1108/JCOM-06-2016-0044. [DOI] [Google Scholar]
- Talbert J., Schadler A., Freeman P. Rural/urban disparities in pneumococcal vaccine service delivery among the fee-for-service medicare population. Rural and Underserved Health Research Center. 2018 https://www.ruralhealthresearch.org/publications/1168 [Google Scholar]
- Tsai Y., Lindley M.C., Zhou F., Stokley S. Urban-Rural Disparities in Vaccination Service Use Among Low-Income Adolescents. J. Adolesc. Health. 2021;69(1):114–120. doi: 10.1016/j.jadohealth.2020.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walther J.B., Carr C.T., Choi S.S.W., DeAndrea D.C., Kim J., Tong S.T., Van Der Heide B. Interaction of interpersonal, peer, and media influence sources online. A Networked Self: Identity, Community, and Culture on Social Network Sites. 2010;17:17–38. [Google Scholar]
- Winer R.L., Gonzales A.A., Noonan C.J., Buchwald D.S. A Cluster-Randomized Trial to Evaluate a Mother-Daughter Dyadic Educational Intervention for Increasing HPV Vaccination Coverage in American Indian Girls. J. Community Health. 2016;41(2):274–281. doi: 10.1007/s10900-015-0093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie L., Pinto J., Zhong B. Building community resilience on social media to help recover from the COVID-19 pandemic. Comput. Hum. Behav. 2022;134 doi: 10.1016/j.chb.2022.107294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakharchenko O., Avramenko R., Zakharchenko A., Korobchuk A., Fedushko S., Syerov Y., Trach O. Multifaceted Nature of Social Media Content Propagating COVID-19 Vaccine Hesitancy: Ukrainian Case. Procedia Comput. Sci. 2022;198:682–687. doi: 10.1016/j.procs.2021.12.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.