Abstract
Purpose
This study aimed to understand the cough characteristics and health journeys among community-based chronic cough (CC) patients, and their characteristics associated with healthcare visits.
Methods
A population-based cross-sectional study was conducted in 2020, using the South Korea and Taiwan National Health and Wellness Survey (NHWS) and CC surveys. Patients with current CC were defined by daily coughing for > 8 weeks in the past 12 months and currently coughing at the time of survey. The survey items pertained to CC patients’ treatment journey and cough characteristics.
Results
Patients with current CC in South Korea and Taiwan, respectively, had cough duration for 3.45 ± 5.13 years and 5.75 ± 7.28 years and cough severity visual analogue scale (VAS) scores of 4.50 ± 2.15 and 4.46 ± 1.92 out of 0–10 scale, with 70.3% and 57.9% having spoken with a physician about cough. Compared to CC patients who had not visited healthcare professionals for cough, those who visited reported more severe cough (VAS: 3.89 ± 1.71 vs. 4.6 ± 2.02; p = 0.009), worse cough-specific quality of life (Leicester Cough Questionnaire: 16.20 ± 3.23 vs.13.45 ± 2.68, p < 0.001), greater symptom severity (Hull Airway Reflux Questionnaire: 16.73 ± 15.16 vs. 24.57 ± 13.38; p < 0.001), and more urinary incontinence (13.6 vs. 26.5%, p = 0.027). More than 50% of patients perceived cough medication(s) as not or a little useful and 25% felt their physicians did not well understand how CC impacts their life.
Conclusion
Cough is frequently severe and persistent among community-based CC patients. They experience several issues in their health journey, including treatment ineffectiveness and physician’s understanding. Further efforts are warranted to reduce CC burden in the community.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00408-022-00586-3.
Keywords: Chronic cough, Treatment journey, Disease burden, Cough-specific health-related quality of life
Introduction
Cough is a vital protective reflex to prevent aspiration and enhance airway clearance [1, 2]. However, cough is also one of the most common symptoms for patients seeking care [3]. Particularly, chronic cough (CC), defined by cough persisting for more than 8 weeks, is a major cause of morbidity affecting quality of life (QoL) [4]. The prevalence of CC has been estimated to be about 10% globally [5] and 2–5% in East Asia [6].
During the last decades, several international and national guidelines have been developed for guiding the management of CC patients [7–9]. Several studies reported the characteristics of CC among patients visiting clinics [10–14]; however, there is limited knowledge about cough characteristics and healthcare journey in the community. Large general population-based studies [15–17] reported the prevalence of CC and its impact on health-related QoL; they mostly reported the simple presence of CC but lacked detailed cough information because they were designed to investigate general health issues. Further understanding of cough characteristics and health journey experiences of CC patients in the community will help us to understand the disease burden and identify unmet clinical needs.
Herein, the present study sought to understand (i) cough characteristics in CC patients in the community of South Korea and Taiwan, e.g., cough duration, severity, or cough-specific QoL; (ii) their healthcare journeys; and to explore (iii) cough characteristics associated with healthcare professional (HCP) visits.
Methods
Study Design
This is a cross-sectional study, including data from the 2020 South Korea and Taiwan National Health and Wellness Survey (NHWS) as well as CC surveys. The NHWS were conducted in a total of 11 countries/territories, including South Korea and Taiwan, collecting self-reported patient characteristics, disease status, and patient-reported outcomes (PROs). The 2020 South Korea and Taiwan NHWS survey was conducted in January–February 2020 and was described elsewhere [18].
To further understand CC patients’ experience including the impact of CC on QoL and healthcare journey, the add-on CC survey was conducted in March–April 2020 to all eligible respondents from the NHWS who met the eligibility criteria. Both the NHWS survey and the CC survey were approved by the Pearl Pathways Institutional Review Board (IN, USA). All respondents completed the NHWS and the CC survey in local language(s)—Korean (South Korea) and traditional Chinese (Taiwan). All respondents provided informed consent prior to participating.
Study Population
NHWS
Potential respondents to the NHWS, aged 18 years or older, were recruited through an existing, general purpose (i.e., not healthcare specific) web-based consumer panel. All panelists explicitly agreed to be a panel member. While recruiting the respondents, a stratified random sampling procedure, with strata by sex and age, was implemented to ensure that the demographic composition is representative of the respective general adult population in South Korea and Taiwan. There were no exclusion criteria.
CC Survey
Among the respondents of the 2020 South Korea and Taiwan NHWS, those who self-reported coughing daily for > 8 weeks in the past 12 months and had current cough at the time of surveys (defined as current CC patients) were invited to participate in the add-on CC survey. Respondents who self-reported any form of lung cancer, having interstitial lung disease, or currently taking an ACE inhibitor were excluded. The patients were divided into subgroups based on their cough severity visual analogue scale (VAS) 2 weeks’ prior to the time of survey (mild CC ≤ 4, vs. severe > 4 of 10) [19].
Cough Parameters and Patient-Reported Outcomes
Baseline demographic and general health-related parameters were collected through the NHWS (please see Methods in Supplementary Information for more details). In the CC survey, cough-specific parameters were collected, such as years experiencing CC, cough severity, impact, cough-related conditions or behaviors, and health journey experiences. The cough severity was assessed by a VAS ranging from 0 (no cough) to 10 (extremely severe cough). Conditions or behaviors related to CC were defined by patients’ responses to the question “Has a doctor ever told you that any of the following conditions or behaviors are related to your chronic cough?”
Cough-specific QoL was measured by Leicester Cough Questionnaire (LCQ), with the total score range of 3–21 points [20]. Symptom severity associated with cough hypersensitivity was measured by Hull Airway Reflux Questionnaire (HARQ) [21]. The HARQ is a 14-item, self-administered instrument that measures specific symptoms related to cough, with the total score ranging from 0 to 70 (please see Methods in Supplementary Information for more details).
The patient journey included HCPs seen and currently seeing for CC, experience with HCPs, diagnostic tests, medications and diagnoses, and patients’ satisfaction with previous treatments.
Statistical Analysis
Descriptive statistics were reported using counts and percentages for categorical variables and means and standard deviations (SDs) (or standard errors [SEs] as indicated) for continuous variables. Patient experience, health journey, and medications were also summarized descriptively. Multivariate comparisons of LCQ and HARQ scores were conducted between mild CC (VAS ≤ 4) and severe CC (VAS > 4) patients using generalized linear models (GLMs) with identity link function to control for covariates, including age and sex. Finally, bivariate comparisons were conducted to compare the characteristics of patients who had visited HCPs for their CC and those who had not; the comparisons were conducted by combining patients from South Korea and Taiwan together due to the limited sample sizes. All statistical analyses were performed using IBM SPSS Statistics Version 25 [22] and R version 3.6.3 [23]. P values of less than 0.05 were considered statistically significant.
Results
Study Subjects
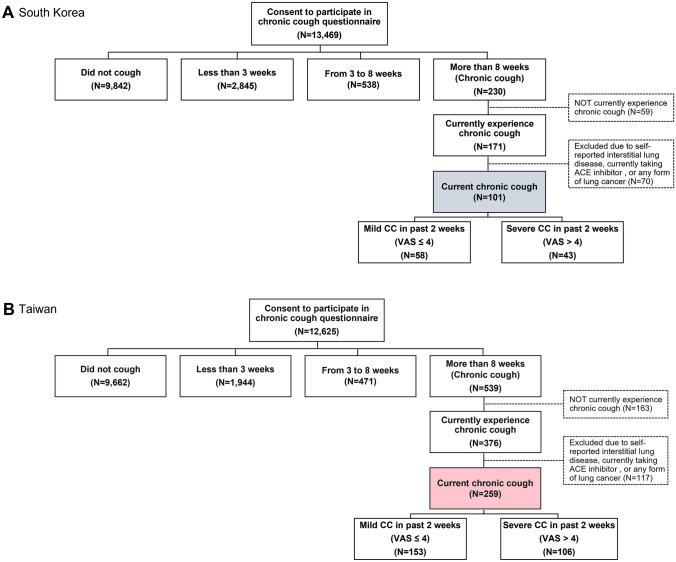
Based on the selection criteria, a total of 360 subjects with current CC (101 from South Korea and 259 from Taiwan) were identified (Fig. 1A and B). Patients in South Korea were aged 43.93 ± 13.99 years (mean ± SD) and 55.4% were females and those in Taiwan were aged 48.69 ± 14.35 years and 45.2% were females (Table 1).
Fig. 1.
Respondent flowchart
Table 1.
Cough-related clinical characteristics of chronic cough patients in the 2020 South Korea and Taiwan National Health and Wellness Survey
| South Korea (N = 101) | Taiwan (N = 259) | ||||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | ||
| Age | 101 | 43.93 | 13.99 | 259 | 48.69 | 14.35 | |
| Years experienced CC | 71 | 3.45 | 5.13 | 167 | 5.75 | 7.28 | |
| Cough severity VAS score over the past 2 weeks | 101 | 4.50 | 2.15 | 259 | 4.46 | 1.92 | |
| Cough severity VAS score on the worst day during the past 2 weeks | 101 | 5.67 | 2.32 | 259 | 5.76 | 2.31 | |
| LCQ total score | 101 | 13.85 | 3.41 | 259 | 13.99 | 3.27 | |
| HARQ total score | 101 | 25.59 | 15.58 | 259 | 22.18 | 13.30 | |
| % | % | ||||||
| Sex | Female | 55.4% | 45.2% | ||||
| Male | 44.6% | 54.8% | |||||
| Cough more severe at a certain time of year | No | 32.4% | 53.4% | ||||
| Yes | 67.6% | 46.6% | |||||
| Cough more severe in | Spring (March, April, May) | 36.0% | 11.1% | ||||
| Summer (June, July, August) | 0.0% | 1.9% | |||||
| Fall/Autumn (September, October, November) | 0.0% | 11.1% | |||||
| Winter (December, January, February) | 64.0% | 75.9% | |||||
| How often do you cough up phlegm when coughing | Never | 6.9% | 6.6% | ||||
| Rarely | 23.8% | 37.8% | |||||
| Sometimes | 42.6% | 32.4% | |||||
| Often | 18.8% | 18.1% | |||||
| Always | 7.9% | 5.0% | |||||
| Cough start/exacerbate with cold or flu-like illness | No | 50.5% | 37.8% | ||||
| Yes | 32.7% | 38.6% | |||||
| Do not know | 16.8% | 23.6% | |||||
| Smoking status | Not smoked in the last 12 months | 56.4% | 74.1% | ||||
| Not currently smoking but smoked in last 12 months | 3.0% | 1.9% | |||||
| Currently smoking | 40.6% | 23.9% | |||||
| Experienced urinary incontinence while coughing | No | 59.4% | 82.2% | ||||
| Yes | 40.6% | 17.8% | |||||
| Experienced post-nasal drip | No | 33.7% | 27.4% | ||||
| Yes | 66.3% | 72.6% | |||||
CC chronic cough; HARQ Hull Airway Reflux Questionnaire; LCQ Leicester Cough Questionnaire; VAS visual analogue scale
CC Patient Characteristics
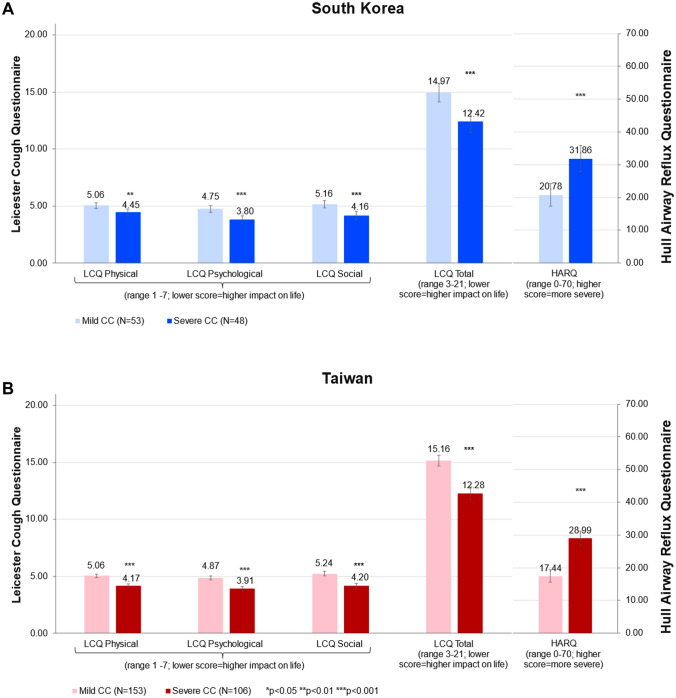
Patients with current CC in South Korea had cough persisting for 3.45 ± 5.13 years, while those in Taiwan had cough for 5.75 ± 7.28 years (Table 1). The cough severity VAS scores in South Korea and Taiwan over the past two weeks were 4.50 ± 2.15 and 4.46 ± 1.92, respectively. In South Korea, 42.6% of patients were considered to have severe CC (VAS > 4) and 40.9% in Taiwan had severe CC (Fig. 1). Total LCQ scores in South Korea and Taiwan were 13.85 ± 3.41 and 13.99 ± 3.27, while HARQ scores were 25.59 ± 15.58 and 22.18 ± 13.30, respectively (Table 1). Cough severity was significantly associated with greater cough burden as measured by the LCQ (total and all domain scores) and HARQ scores (Fig. 2). Those with severe CC had mean LCQ total scores of 12.42 and 12.28 in South Korea and Taiwan, respectively, and the differences with those of mild CC were 2.55 and 2.88, respectively, exceeding the minimal important difference of 1.3 for the scale.
Fig. 2.
Comparison of LCQ and HARQ scores between mild and severe CC patients in South Korea (upper panel) and Taiwan (lower panel). Note: Data are presented as mean ± standard error (SE). CC chronic cough; HARQ Hull Airway Reflux Questionnaire; LCQ Leicester Cough Questionnaire; QoL quality of life. Asterisks (***) indicate significance of p < 0.001
More than 40% of patients (South Korea: 67.6%; Taiwan: 46.6%) felt that cough was more severe at a certain time of year; cough was more severe during winter (South Korea: 64.0%; Taiwan: 75.9%) and spring (South Korea: 36.0%); however, spring was not remarkable in Taiwan (11.1%) (Table 1). A quarter of patients (South Korea: 26.7%; Taiwan: 23.1%) often or always coughed up phlegm. In South Korea, 40.6% were still smoking, and 23.6% in Taiwan were currently smoking. The proportion of patients experiencing urinary incontinence when coughing was 40.6% in South Korea and 17.8% in Taiwan, respectively. Urinary incontinence was significantly more frequent in females than in males (41.6 vs. 8.0%; p < 0.001).
CC Patient Journey: Healthcare Visits
Among CC patients in South Korea and Taiwan, 70.3% and 57.9% had, respectively, reported having ever spoken with a physician for cough (Table 2). The most common types of HCPs patients first sought medical consultation were otolaryngologist (South Korea: 33.7%; Taiwan: 45.9%), primary care physician (20.8%; 11.2%), and pulmonologist (11.9%; 9.3%) (Table 2). Other common HCPs consulted after the patients’ first HCP visit were otolaryngologist, primary care physician, and pulmonologist in South Korea and otolaryngologist, traditional oriental physician, and pulmonologist in Taiwan (Supplementary Table 1). In South Korea, 53.7% of the HCPs first seen were in clinics, followed by semi-hospitals (31.7%) and tertiary hospitals (14.6%). In Taiwan, 68.9% of the HCPs first seen were in clinics, followed by area hospitals (12.3%), regional hospitals (10.4%), and medical centers (8.5%) (Table not shown).
Table 2.
History and experiences of seeking HCPs for CC in South Korea and Taiwan
| South Korea (N = 101) | Taiwan (N = 259) | ||
|---|---|---|---|
| % | % | ||
| History and experiences of seeking HCPs for CC | |||
| Ever spoken with a physician for cough | No | 29.7 | 42.1 |
| Yes | 70.3 | 57.9 | |
| HCP first seen for CC | None | 18.8 | 18.1 |
| Primary care physician (Family physician; Internist) | 20.8 | 11.2 | |
| Pulmonologist | 11.9 | 9.3 | |
| Allergist | 2.0 | 4.6 | |
| Otolaryngologist | 33.7 | 45.9 | |
| Head and neck surgeon | 0.0 | 0.0% | |
| Gastroenterologist | 11.9 | 1.5 | |
| Urologist | 0.0 | 0.0 | |
| Traditional oriental Physician | 1.0 | 7.3 | |
| Other | 0.0 | 1.9 | |
| How knowledgeable is your physician in how to evaluate and treat CC (N = 71/150) | Not at all knowledgeable | 0.0 | 4.7 |
| A little knowledgeable | 16.9 | 32.0 | |
| Somewhat knowledgeable | 54.9 | 52.0 | |
| Extremely knowledgeable | 28.2 | 11.3 | |
| Physicians have a good understanding of how CC impacts your life (N = 71/150) | No | 23.9 | 28.7 |
| Yes | 76.1 | 71.3 | |
| Feel that your doctor(s) (N = 71/150) | Ordered too many tests (such as x-rays, CT scans, breathing tests) | 7.0 | 4.7 |
| Did not order enough tests (such as x-rays, CT scans, breathing tests) | 16.9 | 26.0 | |
| Ordered the appropriate tests | 59.2 | 52.0 | |
| None of the above | 16.9 | 17.3 | |
| Feel that your doctor(s) (N = 71/150) | Sent you to too many additional doctors, like specialists | 1.4 | 3.3 |
| Did not send you to enough or the right doctors/specialists | 15.5 | 38.7 | |
| Sent you to the right doctors/specialists | 49.3 | 28.7 | |
| None of the above | 33.8 | 29.3 | |
| Diagnostics tests conducted to evaluate CC | |||
| Chest imaging (X-ray or CT scan) | 40.6 | 40.2 | |
| Spirometry | 35.6 | 22.4 | |
| Allergy test | 19.8 | 14.7 | |
| Sinus imaging (X-ray or CT scan) | 9.9 | 5.8 | |
| GI testing (Endoscopy/Barium swallow, esophageal pH testing) | 8.9 | 12.4 | |
| Bronchoscopy | 14.9 | 8.1 | |
| I do not know | 6.9 | 12.7 | |
| None | 25.7 | 34.7 | |
CC chronic cough; CT computed tomography; HCP healthcare provider
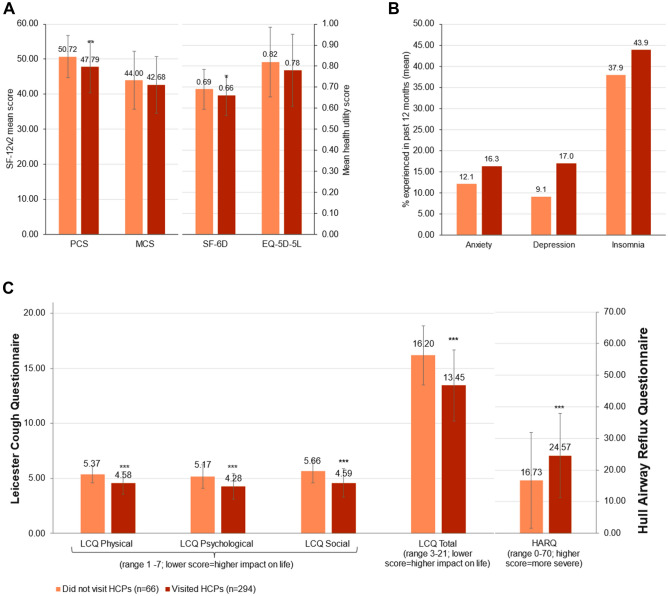
Table 3 describes pooled analyses of patients who had not visited any HCPs compared to those who had visited HCPs for CC. Age, cough duration, sex, or smoking status did not significantly differ between two groups. However, patients who had visited HCPs for CC had more severe cough, experienced more cough-related urinary incontinence and post-nasal drip than those who had not. In addition, patients who had visited HCPs reported significantly greater burden and cough symptom severity than those who had not, as measured by poorer PCS score in the SF-12v2 (47.79 ± 7.47 vs. 50.72 ± 6.01; p = 0.003), SF-6D score (0.66 ± 0.10 vs. 0.69 ± 0.09; p = 0.029), LCQ total score (13.45 ± 2.68 vs. 16.20 ± 3.23; p < 0.001) and domain scores, and also higher HARQ scores (24.57 ± 13.38 vs. 16.73 ± 15.16; p < 0.001). The proportion of self-reported anxiety, depression, or insomnia was numerically higher among those who had visited HCPs for CC, but the difference was not statistically different (Fig. 3).
Table 3.
Comparison of cough characteristics between patients who did not visit HCPs (n = 66) vs. CC patients who had visited HCPs (n = 294) for CC
| CC patients who did not visit HCPs (n = 66) | CC patients who visited HCPs (n = 294) | p value | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Age | 47.09 | 13.95 | 47.42 | 14.51 | 0.868 | |
| Years experienced CC (n = 32/206) | 5.28 | 6.98 | 5.03 | 6.77 | 0.849 | |
| Cough severity VAS score over the past 2 weeks | 3.89 | 1.71 | 4.6 | 2.02 | 0.009 | |
| Cough severity VAS score on the worst day during the past 2 weeks | 4.83 | 2.12 | 5.94 | 2.3 | < 0.001 | |
| % | % | |||||
| Sex | Female | 40.9% | 49.7% | 0.198 | ||
| Male | 51.9% | 50.3% | ||||
| How often do you cough up phlegm when coughing | Never | 13.6% | 5.1% | 0.033 | ||
| Rarely | 28.8% | 35.0% | ||||
| Sometimes | 42.4% | 33.7% | ||||
| Often | 12.1% | 19.7% | ||||
| Always | 3.0% | 6.5% | ||||
| Smoking status | Not smoked in the last 12 months | 54.5% | 72.4% | 0.17 | ||
| Not currently smoking but smoked in last 12 months | 3.0% | 2.0% | ||||
| Currently smoking | 32.4% | 25.5% | ||||
| Experienced urinary incontinence while coughing | No | 86.4% | 73.5% | 0.027 | ||
| Yes | 13.6% | 26.5% | ||||
| Experienced post-nasal drip | No | 53.0% | 23.8% | < 0.001 | ||
| Yes | 47.0% | 76.2% | ||||
CC chronic cough; HCP healthcare provider; VAS visual analogue scale
Fig. 3.
Comparison of general health-related QoL, cough-specific QoL, and HARQ scores between CC patients who had not visited HCPs and those who had visited HCPs. Note: Data are presented as mean ± standard deviation (SD). CC chronic cough; EQ-5D-5L 5-level EQ-5D version, HARQ Hull Airway Reflux Questionnaire; LCQ Leicester Cough Questionnaire; SF-12 12-item short-form survey; SF-6D short-form six dimension; MCS mental component summary; PCS physical component summary; QoL quality of life. Asterisks (**) indicate significance of p < 0.01 and (***) indicate significance of p < 0.001
CC Patient Journey: Diagnoses and Treatments
Among those who had spoken with a physician for CC, about one-quarter of them felt that their physician was not very knowledgeable or did not have good understanding of how CC impacts their life (Table 2). Although more than half patients in South Korea and Taiwan (59.2%; 52.0%) felt their doctor(s) ordered the appropriate number of tests, 38.7% and 15.5% of Taiwanese and Korean patients, respectively, felt their doctor(s) did not send them to enough or the right doctors/specialists. The most common tests conducted were chest imaging (X-ray or CT scan) (South Korea: 40.6%; Taiwan: 40.2%), spirometry (35.6%; 22.4%), and allergy test (19.8%; 14.7%), while about 30% of the patients had not taken any tests. A proportion of the patients were not aware of the types of tests (South Korea: 6.9%; Taiwan: 12.7%) (Table 2).
Around one-fifth of patients had not received a diagnosis (“none” or “do not know”) for their CC from a physician (Table 4). The most common diagnoses were allergic rhinitis (36.6%), chronic rhinitis (29.7%), and habit cough (24.8%) in South Korea and were post-nasal drip (38.6%) and rhinitis (allergic: 32.8%; nasal: 30.5%) in Taiwan.
Table 4.
Physician-diagnosed underlying conditions or behaviors related to CC
| South Korea (N = 101) | Taiwan (N = 259) | |
|---|---|---|
| Underlying conditionsa | % | % |
| Allergic rhinitis | 36.6 | 32.8 |
| Asthma | 20.8 | 12.7 |
| Chronic bronchitis | 22.8 | 21.6 |
| Chronic obstructive pulmonary disease (COPD) | 2.0 | 2.3 |
| Chronic rhinitis | 29.7 | 7.7 |
| Chronic sinusitis | 12.9 | 10.4 |
| Emphysema | 0.0 | 1.2 |
| Gastro-esophageal reflux disease (GERD) | 18.8 | 22.4 |
| I cough out of habit | 24.8 | 15.1 |
| Nasal allergies | 22.8 | 30.5 |
| Nasal polyps | 1.0 | 4.6 |
| Post-nasal drip | 16.8 | 38.6 |
| Sinus bronchial syndrome | 2.0 | 3.9 |
| Vocal cord dysfunction | 3.0 | 3.5 |
| None | 9.9 | 9.3 |
| Others | 3.0 | 3.9 |
| I do not know | 11.9 | 9.7 |
CC chronic cough
aConditions or behaviors related to CC were defined by patients’ responses to the question “Has a doctor ever told you that any of the following conditions or behaviors are related to your chronic cough?” Patients were allowed to choose multiple underlying diseases. If there were no underlying diseases, patients were allowed to choose only “I don’t know” or “None”
Most patients reported ever taking medication(s) for CC (South Korea: 85.1%; Taiwan: 80.7%) (Table 5). Commonly used medications were anti-tussives (60.4%), antibiotics (18.8%), and 1st-generation antihistamines (17.8%) in South Korea, while anti-tussives (50.2%), nasal steroids (25.9%), and cough drops (25.5%) were common in Taiwan (Table 4). Use of codeine or hydrocodone-containing products was reported by 11.9% and 28.2% of patients in South Korea and Taiwan, respectively, and the duration of regular use was 9.25 ± 8.11 months in South Korea and 18.68 ± 45.65 months in Taiwan. However, more than half of patients perceived anti-tussive medications (including anti-tussives, anti-epileptics, 1st generation antihistamines, or cough drops) as “not at all” or “a little bit” useful to treat their CC (Table 5).
Table 5.
Self-reported history of medications given for treating CC
| South Korea | |||||
|---|---|---|---|---|---|
| Medication Usage | How well did the medication treat your chronic cough? (%) | ||||
| Medication | (N = 101) | Not at all | A little bit | Somewhat | A great deal |
| None | 14.9% | – | – | – | – |
| Anti-tussives (such as common cold medicine) | 60.4% | 11.5% | 45.9% | 34.4% | 8.2% |
| Anti-epileptics (such as gabapentin) | 2.0% | 0.0% | 100.0% | 0.0% | 0.0% |
| Proton pump inhibitors | 14.9% | 0.0% | 46.7% | 46.7% | 6.7% |
| H2 blockers | 1.0% | 100.0% | 0.0% | 0.0% | 0.0% |
| Nasal Steroids | 5.9% | 16.7% | 33.3% | 50.0% | 0.0% |
| Inhaled steroids | 2.0% | 0.0% | 0.0% | 50.0% | 50.0% |
| Oral steroids | 2.0% | 0.0% | 50.0% | 0.0% | 50.0% |
| Beta-agonists | 3.0% | 0.0% | 66.7% | 33.3% | 0.0% |
| 1st-generation antihistamines | 17.8% | 5.6% | 50.0% | 38.9% | 5.6% |
| 2nd-generation antihistamines | 13.9% | 0.0% | 35.7% | 50.0% | 14.3% |
| Cough drops | 16.8% | 23.5% | 58.8% | 11.8% | 5.9% |
| Antibiotics | 18.8% | 21.1% | 31.6% | 31.6% | 15.8% |
| ICS-LABA | 6.9% | 0.0% | 42.9% | 42.9% | 14.3% |
| Prescribed Traditional Oriental Medicine | 10.9% | 0.0% | 45.5% | 54.5% | 0.0% |
| Traditional Oriental Medicine bought over the counter | 5.9% | 33.3% | 16.7% | 50.0% | 0.0% |
| Others | 4.0% | 50.0% | 50.0% | 0.0% | 0.0% |
| Ever taken codeine or hydrocodone-containing products for ≥ 1 month | 11.9% | Duration of regular use (months) | |||
| Mean | SD | ||||
| 9.25 | 8.11 | ||||
| Taiwan | |||||
|---|---|---|---|---|---|
| Medication usage | How well did the medication treat your chronic cough? (%) | ||||
| Medication | (N = 259) | Not at all | A little bit | Somewhat | A great deal |
| None | 19.3% | – | – | – | – |
| Anti-tussives | 50.2% | 16.9% | 60.8% | 20.8% | 1.5% |
| Anti-epileptics | 1.9% | 40.0% | 40.0% | 20.0% | 0.0% |
| Proton pump inhibitors | 11.2% | 10.3% | 51.7% | 31.0% | 6.9% |
| H2 blockers | 5.8% | 13.3% | 53.3% | 26.7% | 6.7% |
| Nasal Steroids | 25.9% | 10.4% | 64.2% | 20.9% | 4.5% |
| Inhaled steroids | 9.7% | 12.0% | 44.0% | 36.0% | 8.0% |
| Oral steroids | 5.8% | 0.0% | 60.0% | 20.0% | 20.0% |
| Beta-agonists | 13.5% | 11.4% | 42.9% | 34.3% | 11.4% |
| 1st-generation antihistamines | 13.1% | 5.9% | 64.7% | 29.4% | 0.0% |
| 2nd-generation antihistamines | 11.6% | 13.3% | 50.0% | 33.3% | 3.3% |
| Cough drops | 25.5% | 25.8% | 66.7% | 7.6% | 0.0% |
| Antibiotics | 12.4% | 15.6% | 50.0% | 28.1% | 6.3% |
| ICS-LABA | 8.9% | 4.3% | 39.1% | 47.8% | 8.7% |
| Prescribed Traditional Oriental Medicine | 21.6% | 16.1% | 58.9% | 19.6% | 5.4% |
| Traditional Oriental Medicine bought over the counter | 22.8% | 23.7% | 57.6% | 16.9% | 1.7% |
| Others | 2.3% | 0.0% | 50.0% | 50.0% | 0.0% |
| Ever taken codeine or hydrocodone-containing products for ≥ 1 month | 28.2% | Duration of regular use (months) | |||
| Mean | SD | ||||
| 18.68 | 45.65 | ||||
ICS-LABA inhaled corticosteroid and long-acting β2-agonist
Discussion
The present study investigated cough characteristics and healthcare journey of CC patients in community-based populations of South Korea and Taiwan. As reflected by cough PRO scores, the severity and impact of cough was considerable even among CC patients in the community. The LCQ and HARQ scores in this study had exceeded the normative values of healthy individuals suggested from other countries [24, 25]. We examined their healthcare journeys and found several unmet needs in physician’s knowledge and understanding of CC, diagnostic investigations, and treatment effectiveness. The observed patterns were similar between two countries, despite their differences in demographics, cough seasonality, and healthcare system. To our knowledge, this is the first description of community-based CC patients’ cough characteristics and healthcare journeys in South Korea and Taiwan and is also one of the very few reported globally [26–28].
We speculate that the impact of cough, or cough severity perceived by a patient, is a key factor defining CC as a disease and that cough-related healthcare utilization is a proxy marker of the impact that patients experienced with CC. In the present study, about one-fifth of patients in South Korea and Taiwan did not visit any HCPs for their CC; and HCP visits were significantly associated with several cough characteristics, e.g., cough severity, cough-specific QoL, cough-induced urinary incontinence, or post-nasal drip sensation, but not with cough duration. These findings cannot make any firm conclusions because other unmeasured factors may underlie HCP visits, e.g., cough frequency, other complications, or socioeconomic status; however, they suggest that cough severity and impact are likely important characteristics that define CC as a disease.
In CC patients’ health journey, two issues were noted: (1) lack of effective anti-tussive and (2) proper diagnosis. More than 50% of patients had taken anti-tussives (South Korea: 60.4%; Taiwan: 50.2%), and the mean duration of regularly taking codeine was around one year, but more than half of them found very little effectiveness. These findings are consistent with recent studies of European and Korean patients that reported limited effectiveness of currently available anti-tussives [11, 29]. Indeed, these remain as major unmet needs for refractory or unexplained CC patients.
About 20% of patients reported not receiving any diagnosis for CC. Furthermore, 20–30% of patients felt that their physicians were not as knowledgeable in CC management, nor have a good understanding of the impact. Moreover, chest imaging, which is routinely recommended in cough guidelines, was performed in about 40% of the patients, which is surprising given that bronchoscopy (8.1–14.9%) and GI testing (8.9–12.4%) were frequently done. These findings imply that there are unmet needs to provide optimal/adequate managements for CC in the community and that further efforts are warranted to implement international or national cough guidelines to non-specialist clinics.
Interestingly, unlike in South Korea, a male predominance (54.8%) was noted in CC patients in Taiwan, which is similar to those observed at specialist cough clinics in Guangzhou, China [30]. This might be attributed to ethnic or environmental factors distinct to Taiwan and Southeast China [31]. However, the present study was not designed to investigate the sex difference, and the findings warrant further investigation.
Other differences were noted in the patient characteristics between South Korea and Taiwan. Urinary incontinence was more frequent in South Korean patients than in Taiwanese (40.6% vs. 17.8%), although cough scores were comparable. This is likely attributed to the sex difference as urinary incontinence is a common cough-related complication among female patients [32, 33]. In addition, 40.6% of current CC patients in South Korea were current smokers, similar to the Korean National Health and Nutrition Examination Surveys results (43.0–47.7%) [15, 34]. The proportion of current smokers in Taiwan in this study was less than that reported in a previous study (23.6 vs 31.6%) [35], potentially attributed by a decline in smoking prevalence in Taiwan [36, 37].
We observed that current smokers were frequent among CC subjects in both community populations, which contrasted with the observations at specialist cough clinics where most are never or non-current smokers [31, 38]. This might suggest a difference in CC patient characteristics between community and specialist cough clinics. However, it may be partly due to the limitation of current definition used to identify CC, because the duration-based definition do not well differentiate protective cough responses against irritant exposure (such as cigarette smoke) from hypersensitivity cough [39]. In our view, the duration-based simple definition does not capture the key nature of the disease.
There are limitations of this study. The survey is a cross-sectional study; hence no causal relationships could be concluded. All data were self-reported, therefore recall bias and self-representation bias should be acknowledged. Although the NHWS is broadly representative of the Korean and Taiwanese general adult population, individuals without internet access or those unfamiliar with online administration including those of older age or with severe comorbidities and disabilities are likely to be under-represented in this study. This might underlie a younger age distribution of the present study respondents, compared to those attending specialist cough clinics [38, 40]. Secondly, there may be unmeasured demographic or clinical factors that could influence the patients’ health journey and warrant further investigation. Nevertheless, the present survey provided an opportunity to identify cough-related characteristics as well as the patient journey in the community of South Korea and Taiwan. Respondents of the NHWS were recruited using a stratified random sampling procedure, with strata by sex and age, to ensure that the demographic composition is representative of the respective adult population in each country/territory.
In conclusion, this is the first study describing cough characteristics and healthcare utilization of CC patients in the community-based populations of South Korea and Taiwan. Cough is frequently severe and persistent among community-based CC patients. They experience several issues in their health journey, including treatment ineffectiveness and physician’s understanding. Further efforts are warranted to reduce the burden of CC in the community.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Cerner Enviza received funding from Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA to conduct the study and develop the manuscript. The authors acknowledge Dr. Yirong Chen of Cerner Enviza for the support in the statistical analysis and Dr. Amanda Woo of Cerner Enviza for providing medical writing and editorial support. The authors thank the developers of the CC module, Jonathan Schelfhout and Bob Boggs from the Center for Observational Real-world Evidence, Merck & Co., Inc., Rahway, NJ, USA, for their support and advice in developing the Taiwan and Korea chronic cough module.
Author Contributions
SHK contributed to the concept or design of the study. SHK, W-JS, and C-JY equally contributed to the analysis or interpretation of the data, drafting of the article, and critical revision for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Funding
This study was funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Declarations
Conflict of interest
SH Kang is an employee of MSD, Korea. WJ Song has received research grants from MSD and AstraZeneca, consulting fees from MSD and AstraZeneca, and lecture fees from MSD, AstraZeneca, GSK, and Novartis. CJ Yu declares no conflict of interest.
Ethical Approval
The 2020 National Health and Wellness Survey (NHWS) (protocol # 19-KANT-211) and CC Survey (protocol #20-KANT-215) were approved by the Pearl Pathways Institutional Review Board (Indianapolis, Indiana, USA).
Consent to Participate
Informed online consent was obtained from all individual participants included in the study.
Consent to Publish
The authors affirmed that the study participants had provided informed consent for the contents in this article to be published.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Woo-Jung Song and Chong-Jen Yu contributed equally.
Contributor Information
Woo-Jung Song, Email: swj0126@amc.seoul.kr.
Chong-Jen Yu, Email: jefferycjyu@ntu.edu.tw.
Suk Hyun Kang, Email: sukhyun.kang@merck.com.
References
- 1.Morice AH, Fontana GA, Sovijarvi ARA, Pistolesi M, Chung KF, Widdicombe J, et al. The diagnosis and management of chronic cough. Eur Respir J. 2004;24(3):481–492. doi: 10.1183/09031936.04.00027804. [DOI] [PubMed] [Google Scholar]
- 2.Irwin RS, Curley FJ, French CL. Chronic cough: the spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Am Rev Respir Dis. 1990;141(3):640–647. doi: 10.1164/ajrccm/141.3.640. [DOI] [PubMed] [Google Scholar]
- 3.Morice AH, Members C. The diagnosis and management of chronic cough. Eur Respir J. 2004;24(3):481–492. doi: 10.1183/09031936.04.00027804. [DOI] [PubMed] [Google Scholar]
- 4.French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of chronic cough on quality of life. Arch Intern Med. 1998;158(15):1657–1661. doi: 10.1001/archinte.158.15.1657. [DOI] [PubMed] [Google Scholar]
- 5.Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015;45(5):1479–1481. doi: 10.1183/09031936.00218714. [DOI] [PubMed] [Google Scholar]
- 6.Song WJ, Faruqi S, Klaewsongkram J, Lee SE, Chang YS. Chronic cough: an Asian perspective. Part 1: epidemiology. Asia Pac Allergy. 2015;5(3):136–44. doi: 10.5415/apallergy.2015.5.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morice AH, Millqvist E, Bieksiene K, Birring SS, Dicpinigaitis P, Ribas CD, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55(1):20. doi: 10.1183/13993003.01136-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irwin RS, French CL, Chang AB, Altman KW, Adams TM, Altman KW, et al. Classification of cough as a symptom in adults and management algorithms. Chest. 2018;153(1):196–209. doi: 10.1016/j.chest.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song DJ, Song WJ, Kwon JW, Kim GW, Kim MA, Kim MY, et al. KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res. 2018;10(6):591–613. doi: 10.4168/aair.2018.10.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeiger RS, Schatz M, Zhou Y, Xie F, Bali V, Schelfhout J, et al. Risk factors for persistent chronic cough during consecutive years: a retrospective database analysis. J Allergy Clin Immunol Pract. 2022;S2213–2198(22):00233–241. doi: 10.1016/j.jaip.2022.02.032. [DOI] [PubMed] [Google Scholar]
- 11.Kang SY, Won HK, Lee SM, Kwon JW, Kim MH, Jo EJ, et al. Impact of cough and unmet needs in chronic cough: a survey of patients in Korea. Lung. 2019;197(5):635–639. doi: 10.1007/s00408-019-00258-9. [DOI] [PubMed] [Google Scholar]
- 12.Morice AH, Birring SS, Smith JA, McGarvey LP, Schelfhout J, Martin Nguyen A, et al. Characterization of patients with refractory or unexplained chronic cough participating in a phase 2 clinical trial of the P2X3-receptor antagonist gefapixant. Lung. 2021;199(2):121–129. doi: 10.1007/s00408-021-00437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiner M, Dexter PR, Heithoff K, Roberts AR, Liu Z, Griffith A, et al. Identifying and characterizing a chronic cough cohort through electronic health records. Chest. 2021;159(6):2346–2355. doi: 10.1016/j.chest.2020.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Lai K, Huang L, Zhao H, Wu F, Zhen G, Deng H, et al. Clinical characteristics of patients with chronic cough in Guangdong, China: a multicenter descriptive study. BMC Pulm Med. 2021;21(1):305. doi: 10.1186/s12890-021-01642-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Won HK, Lee JH, An J, Sohn KH, Kang MG, Kang SY, et al. Impact of chronic cough on health-related quality of life in the Korean adult general population: the Korean National Health and Nutrition Examination Survey 2010–2016. Allergy Asthma Immunol Res. 2020;12(6):964–979. doi: 10.4168/aair.2020.12.6.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ford AC, Forman D, Moayyedi P, Morice AH. Cough in the community: a cross sectional survey and the relationship to gastrointestinal symptoms. Thorax. 2006;61(11):975–979. doi: 10.1136/thx.2006.060087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satia I, Mayhew AJ, Sohel N, Kurmi O, Killian KJ, O’Byrne PM, et al. Prevalence, incidence and characteristics of chronic cough among adults from the Canadian Longitudinal Study on Aging. ERJ Open Res [Internet]. 2021 Apr 1 [cited 2022 Apr 7];7(2). Available from: https://openres.ersjournals.com/content/7/2/00160-2021 [DOI] [PMC free article] [PubMed]
- 18.Yu CJ, Song WJ, Kang SH. The disease burden and quality of life of chronic cough patients in South Korea and Taiwan. World Allergy Organ J. 2022;15(9):100681. doi: 10.1016/j.waojou.2022.100681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kubo T, Tobe K, Okuyama K, Kikuchi M, Chen Y, Schelfhout J, et al. Disease burden and quality of life of patients with chronic cough in Japan: a population-based cross-sectional survey. BMJ Open Respir Res. 2021;8(1):e000764. doi: 10.1136/bmjresp-2020-000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MDL, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ) Thorax. 2003;58(4):339–343. doi: 10.1136/thorax.58.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hull Cough Hypersensitivity Questionnaire [Internet]. International Society for the Study of Cough. [cited 27 Apr 2020]. Available from: http://www.issc.info/HullCoughHypersensitivityQuestionnaire.html
- 22.IBM Corp (2017) IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp
- 23.R Core Team (2020) R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing
- 24.Morice AH, Faruqi S, Wright CE, Thompson R, Bland JM. Cough hypersensitivity syndrome: a distinct clinical entity. Lung. 2011;189(1):73–79. doi: 10.1007/s00408-010-9272-1. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds JE, Jetté ME, Wright ML, Sundar KM, Gillespie AI, Slovarp LJ. Normative values for the leicester cough questionnaire in healthy individuals. Ann Otol Rhinol Laryngol. 2022;14:34894221112517. doi: 10.1177/00034894221112517. [DOI] [PubMed] [Google Scholar]
- 26.Birring SS, Currie CJ, Holden SE, Jenkins-Jones S, Berni ER, Jones B, et al. The financial burden of treating patients presenting with acute and chronic cough. Curr Med Res Opin. 2021;37(12):2175–2184. doi: 10.1080/03007995.2021.1982685. [DOI] [PubMed] [Google Scholar]
- 27.Tobe K, Kubo T, Okuyama K, Kikuchi M, Chen Y, Schelfhout J, et al. Web-based survey to evaluate the prevalence of chronic and subacute cough and patient characteristics in Japan. BMJ Open Respir Res. 2021;8(1):e000832. doi: 10.1136/bmjresp-2020-000832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hull JH, Langerman H, Ul-Haq Z, Kamalati T, Lucas A, Levy ML. Burden and impact of chronic cough in UK primary care: a dataset analysis. BMJ Open. 2021;11(12):e054832. doi: 10.1136/bmjopen-2021-054832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chamberlain SAF, Garrod R, Douiri A, Masefield S, Powell P, Bücher C, et al. The impact of chronic cough: a cross-sectional European Survey. Lung. 2015;193(3):401–408. doi: 10.1007/s00408-015-9701-2. [DOI] [PubMed] [Google Scholar]
- 30.Lai K, Long L, Yi F, Tang J, Chen Z, Chen F, et al. Age and sex distribution of chinese chronic cough patients and their relationship with capsaicin cough sensitivity. Allergy Asthma Immunol Res. 2019;11(6):871–884. doi: 10.4168/aair.2019.11.6.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung KF, McGarvey L, Song WJ, Chang AB, Lai K, Canning BJ, et al. Cough hypersensitivity and chronic cough. Nat Rev Dis Primer. 2022;8(1):45. doi: 10.1038/s41572-022-00370-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang C, Feng Z, Chen Z, Xu D, Li Y, Lai K, et al. The risk factors for urinary incontinence in female adults with chronic cough. BMC Pulm Med. 2022;22(1):276. doi: 10.1186/s12890-022-02069-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dicpinigaitis PV. Prevalence of stress urinary incontinence in women presenting for evaluation of chronic cough. ERJ Open Res [Internet]. 2021 Jan 1 [cited 2022 Oct 6];7(1). Available from: https://openres.ersjournals.com/content/7/1/00012-2021 [DOI] [PMC free article] [PubMed]
- 34.Koo HK, Jeong I, Lee SW, Park J, Kim JH, Park SY, et al. Prevalence of chronic cough and possible causes in the general population based on the Korean National Health and Nutrition Examination Survey. Medicine (Baltimore) 2016;95(37):e4595. doi: 10.1097/MD.0000000000004595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin HC, Cho SH, Ghoshal AG, Muttalif ARBA, Thanaviratananich S, Bagga S, et al. Respiratory diseases and the impact of cough in Taiwan. Medicine (Baltimore) 2016;95(27):e3854. doi: 10.1097/MD.0000000000003854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiang CY, Chang HY. A population study on the time trend of cigarette smoking, cessation, and exposure to secondhand smoking from 2001 to 2013 in Taiwan. Popul Health Metr. 2016;5(14):38. doi: 10.1186/s12963-016-0109-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chiu NY, Chang CJ. Tobacco and smoking cessation. Taiwan J Psychiatry. 2019;33(3):125. doi: 10.4103/TPSY.TPSY_26_19. [DOI] [Google Scholar]
- 38.Won HK, Kang SY, Kang Y, An J, Lee JH, Lee SM, et al. Cough-related laryngeal sensations and triggers in adults with chronic cough: symptom profile and impact. Allergy Asthma Immunol Res. 2019;11(5):622–631. doi: 10.4168/aair.2019.11.5.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Song WJ, Chang YS, Faruqi S, Kang MK, Kim JY, Kang MG, et al. Defining chronic cough: a systematic review of the epidemiological literature. Allergy Asthma Immunol Res. 2016;8(2):146–155. doi: 10.4168/aair.2016.8.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dicpinigaitis PV, Birring SS, Blaiss M, McGarvey LP, Morice AH, Pavord ID, et al. Demographic, clinical, and patient-reported outcome data from 2 global, phase 3 trials of chronic cough. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2022;S1081–1206(22):00406–409. doi: 10.1016/j.anai.2022.05.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.