Abstract
Introduction:
Antenatal depression and suicidal ideation represent serious pregnancy-related complications, yet comprehensive estimates of the prevalence and predictors of these diagnoses among birthing people remain unclear.
Objective:
This study aimed to characterize trends in the prevalence of depression and suicidal ideation diagnoses identified among pregnant individuals prior to giving birth.
Methods:
This study included 536,647 individuals aged 15–44 years continuously enrolled in a single commercial health insurance plan for one year before childbirth from 2008 to 2018. The primary outcomes included depression or suicidal ideation based on identification of the relevant ICD-9 and ICD-10 diagnosis codes during pregnancy.
Results:
Rates (95 % CIs) of depression increased by 39 % from 540 (520–560) per 10,000 individuals in 2008 to 750 (730–770) per 10,000 individuals in 2018. Suicidal ideation increased by 100 % from 15 (12–18) per 10,000 individuals in 2008 to 44 (39–50) per 10,000 individuals in 2018. Black birthing people experiencing the sharpest proportional increases.
Conclusions:
The prevalence of depression and suicidal ideation occurring during pregnancy substantially increased over a ten-year period. Further, suicidal ideation diagnosis increased the most for among Black birthing people compared to all groups, resulting in a need for future studies in this area to determine the reasons for an increase in diagnosis and any change in resulting treatment of follow up.
Keywords: Pregnancy, Depression, Suicidal ideation, Trends, Mental health
1. Introduction
Maternal mortality and morbidity steadily increased from 1990 through 2015 in the United States and up to two-thirds of cases may have been preventable if addressed earlier (Davis et al., 2019; Kassebaum et al., 2014). Depression and suicidal ideation are major risk factors for mortality or morbidity and represent serious complications during pregnancy (Cohen et al., 2004). Untreated depression during the perinatal period has profound effects on birthing people and their offspring (Ogunyemi et al., 2018; Simonovich et al., 2021). Past studies found racial differences in antenatal depressive symptoms and suicidal ideation where minority (Black and Asian) adults experience higher rates of depression symptoms (Gavin et al., 2011a; Gavin et al., 2011b). There is a discrepancy between rates of depressive symptoms and diagnosis rates in non-gravid populations, where racial minority adults have higher depressive symptoms, but are less likely to have a resulting diagnosis (Simpson et al., 2007). Past studies found that racial minority adults are more likely to have a substance use disorder diagnosis but less likely to receive a mood disorder diagnosis even when symptoms are present (Boyd et al., 2011; Delphin-Rittmon et al., 2015; Simpson et al., 2007).
To date, few studies have included diverse pregnant samples to document depression diagnoses during pregnancy. Previous studies on antenatal depression and suicidal ideation focused on regional samples, often limited to a single time point (Alhusen et al., 2015; Baer et al., 2016). This study aimed to characterize trends in depression and suicidal ideation diagnoses among racially and ethnically diverse pregnant individuals prior to giving birth over a ten-year period.
2. Methods
This study examined trends in depression and suicidal ideation diagnoses identified in the year before birth among individuals aged 15–44 using the Optum™ Clinformatics™ Data Mart (CDM). CDM is a statistically deidentified database of administrative medical claims for members across all 50 US states derived from a large claims data warehouse. We identified hospital deliveries from 2008 to 2018 and restricted the sample to those with continuous enrollment in a single employer-based health plan for at least 1 year before a live birth. We identified individuals with depression and suicidal ideation during pregnancy using standardized International Classification of Disease-9th and 10th Revision- Clinical Modification diagnosis and procedure codes present at least once in either inpatient or outpatient claims (CCS). We described demographic and clinical characteristics including age, insurance type, other mental health conditions, and substance use disorder for all individuals and for those with depression or suicidal ideation during pregnancy. Optum data contained a race/ethnicity classification including Black, White, Asian, Hispanic, and Other; outcome variation by this classification represents the primary predictor of interest. The data source includes race/ethnicity identified using a combination of self-report, public records, and demographic derivations based on a third-party algorithm (E-Tech). The University of Michigan Institutional Review Board approved this study.
3. Results
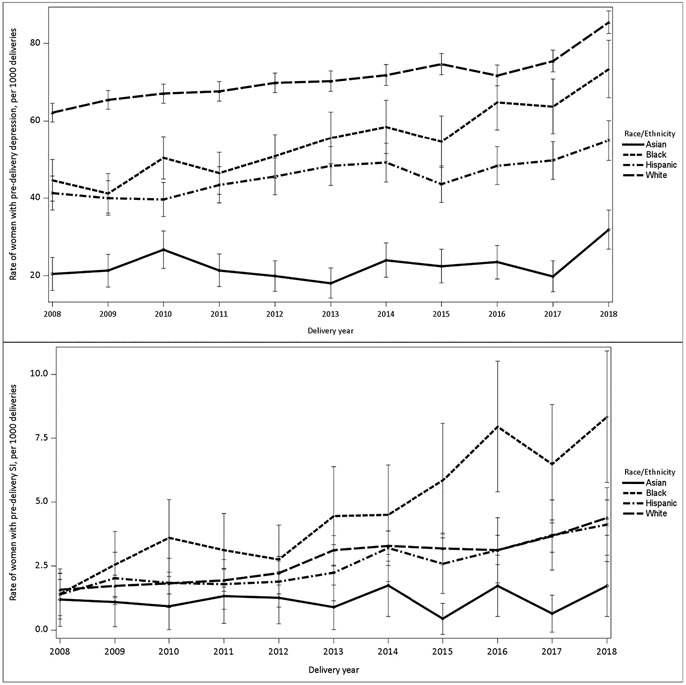
Of the 536,647 commercially insured childbearing individuals that met study criteria between 2008 and 2018, 36,766 (6.8 %) had a diagnosis for either depression or suicidal ideation during pregnancy over the study period. Rates (95 % CIs) of depression increased by 39 % from 540 (520–560) per 10,000 individuals in 2008 to 750 (730–770) per 10,000 individuals in 2018. Suicidal ideation increased by 193 % from 15 (12–18) per 10,000 individuals in 2008 to 44 (39–50) per 10,000 individuals in 2018 (Fig. 1.). Across all racial and ethnic categories, both antenatal depression and suicidal ideation increased over a ten-year period. Black birthing people experienced the sharpest proportional increases. Depression rates among Black birthing people rose by 66 % from 440 (390–490) per 10,000 individuals in 2008 to 730 (660–800) per 10,000 individuals in 2018. Suicidal ideation rates among Black birthing people rose by 700 % from 10 (4–24) per 10,000 individuals in 2008 to 80 (50–100) per 10,000 individuals in 2018 (Table 1).
Fig. 1.
Trends in antenatal depression and antenatal suicidal ideation by race among commercially insured childbearing individuals, 2008–2018 (N = 536,647).
Table 1.
Demographic characteristics of study sample (N = 536,647), overall and by antenatal depression and suicidal ideation, 2008–2018.
| Category | All individuals 2008 | All individuals 2018 | Antenatal depression 2008 |
Antenatal depression 2018 |
Antenatal suicidal ideation 2008 |
Antenatal suicidal ideation 2018 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|||||||
| N | % (95 % CI) | n | % (95 % CI) | n | % (95 % CI) | n | % (95 % CI) | n | % (95 % CI) | n | % (95 % CI) | |
| Age | ||||||||||||
| ≤18 | 1096 | 1.72% [0.95,2.50] |
321 | 0.59% [−0.25,1.43] |
80 | 7.30 % [5.76,8.84] |
64 | 19.94 % [15.54,24.33] |
16 | 1.46% [0.75,2.17] |
23 | 7.17% [4.33,10.00] |
| 19–26 | 9903 | 15.58 % [14.87,16.29] |
8113 | 14.91 % [14.13,15.68] |
508 | 5.13 % [4.70,5.56] |
816 | 10.06 % [9.40,10.71] |
32 | 0.32 % [0.21,0.43] |
116 | 1.43% [1.17,1.69] |
| 27–34 | 34,200 | 53.81 % [53.28,54.34] |
29,231 | 53.71 % [53.14,54.28] |
1674 | 4.89 % [4.67,5.12] |
1856 | 6.35 % [6.07,6.63] |
31 | 0.09 % [0.06,0.12] |
59 | 0.20% [0.15,0.25] |
| 35–39 | 14,470 | 22.77 % [22.08,23.45] |
13,595 | 24.98 % [24.25,25.71] |
863 | 5.96 % [5.58,6.35] |
1011 | 7.44 % [7.00,7.88] |
12 | 0.08 % [0.04,0.13] |
32 | 0.24% [0.15,0.32] |
| ≥ 40 | 3891 | 6.12% [5.37,6.88] |
3161 | 5.81 % [4.99,6.62] |
318 | 8.17% [7.31,9.03] |
341 | 10.79 % [9.71,11.87] |
7 | 0.18 % [0.05,0.31] |
12 | 0.38 % [0.17,0.59] |
| Race | ||||||||||||
| Asian | 4215 | 6.63 % [5.88,7.38] |
4644 | 8.53 % [7.73,9.34] |
86 | 2.04 % [1.61,2.47] |
148 | 3.19% [2.68,3.69] |
5 | 0.12% [0.01,0.22] |
8 | 0.17% [0.05,0.29] |
| Black | 5679 | 8.93 % [8.19,9.68] |
4797 | 8.81 % [8.01,9.62] |
253 | 4.46 % [3.92,4.99] |
352 | 7.34 % [6.60,8.08] |
8 | 0.14 % [0.04,0.24] |
40 | 0.83 % [0.58,1.09] |
| Hispanic | 7934 | 12.48% [11.76,13.21] |
7524 | 13.83 % [13.05,14.61] |
328 | 4.13 % [3.70,4.57] |
413 | 5.49 % [4.97,6.00] |
11 | 0.14 % [0.06,0.22] |
31 | 0.41 % [0.27,0.56] |
| Unknown/missing | 6940 | 10.92 % [10.19,11.65] |
2603 | 4.78% [3.96,5.60] |
366 | 5.27% [4.75,5.80] |
197 | 7.57 % [6.55,8.58] |
13 | 0.19 % [0.09,0.29] |
10 | 0.38 % [0.15,0.62] |
| White | 38,792 | 61.03 % [60.55,61.52] |
34,853 | 64.04 % [63.54,64.55] |
2410 | 6.21 % [5.97,6.45] |
2978 | 8.54 % [8.25,8.84] |
61 | 0.16 % [0.12,0.20] |
153 | 0.44% [0.37,0.51] |
| Income | ||||||||||||
| ≤400 % FPL | 329 | 0.52 % [−0.26,1.29] |
473 | 0.87% [0.03,1.71] |
21 | 6.38 % [3.73,9.04] |
37 | 7.82 % [5.39,10.25] |
8 | 1.69% [0.53,2.86] |
||
| >400 % FPL | 48,706 | 76.63 % [76.25,77.01] |
41,961 | 77.10 % [76.70,77.51] |
2659 | 5.46 % [5.26,5.66] |
3209 | 7.65 % [7.39,7.90] |
64 | 0.13 % [0.10,0.16] |
167 | 0.40% [0.34,0.46] |
| Region | ||||||||||||
| Great Lakes/Northern Plains | 15,110 | 23.77 % [23.09,24.45] |
14,846 | 27.28 % [26.56,28.00] |
972 | 6.43 % [6.04,6.82] |
1391 | 9.37 % [8.90,9.84] |
25 | 0.17 % [0.10,0.23] |
92 | 0.62% [0.49,0.75] |
| Mountain | 5745 | 9.04 % [8.30,9.78] |
5695 | 10.46 % [9.67,11.26] |
366 | 6.37 % [5.74,7.00] |
491 | 8.62 % [7.89,9.35] |
10 | 0.17 % [0.07,0.28] |
25 | 0.44% [0.27,0.61] |
| Northeast | 6441 | 10.13 % [9.40,10.87] |
5375 | 9.88% [9.08,10.67] |
391 | 6.07 % [5.49,6.65] |
356 | 6.62 % [5.96,7.29] |
8 | 0.12% [0.04,0.21] |
10 | 0.19% [0.07,0.30] |
| Pacific | 7100 | 11.17% [10.44,11.90] |
6172 | 11.34 % [10.55,12.13] |
244 | 3.44 % [3.01,3.86] |
384 | 6.22 % [5.62,6.82] |
5 | 0.07 % [0.01,0.13] |
15 | 0.24% [0.12,0.37] |
| Southeast | 29,107 | 45.79 % [45.22,46.37] |
22,110 | 40.63 % [39.98,41.28] |
1468 | 5.04 % [4.79,5.29] |
1463 | 6.62 % [6.29,6.94] |
50 | 0.17 % [0.12,0.22] |
99 | 0.45% [0.36,0.54] |
| Unknown | 57 | 0.09 % [−0.69,0.87] |
223 | 0.41 % [−0.43,1.25] |
2 | 3.51 % [−1.42,8.43] |
3 | 1.35% [−0.18,2.87] |
1 | 0.45% [−0.44,1.33] |
||
| Insurance | ||||||||||||
| POS | 41,705 | 65.62 % [65.16,66.07] |
40,318 | 74.09 % [73.66,74.51] |
2260 | 5.42 % [5.20,5.64] |
3002 | 7.45 % [7.19,7.70] |
67 | 0.16 % [0.12,0.20] |
159 | 0.39 % [0.33,0.46] |
| EPO or HMO | 19,648 | 30.91 % [30.27,31.56] |
12,603 | 23.16 % [22.42,23.89] |
1009 | 5.14% [4.83,5.44] |
887 | 7.04 % [6.59,7.48] |
25 | 0.13 % [0.08,0.18] |
53 | 0.42% [0.31,0.53] |
| PPO | 2038 | 3.21 % [2.44,3.97] |
772 | 1.42% [0.58,2.25] |
148 | 7.26% [6.13,8.39] |
82 | 10.62 % [8.44,12.80] |
6 | 0.29 % [0.06,0.53] |
12 | 1.55% [0.68,2.43] |
| Indemnity/other | 169 | 0.27 % [−0.51,1.04] |
728 | 1.34% [0.50,2.17] |
26 | 15.38 % [9.89,20.88] |
117 | 16.07 % [13.40,18.75] |
18 | 2.47% [1.34,3.60] |
||
| Other mental health conditions | ||||||||||||
| No | 59,377 | 93.42 % [93.22,93.62] |
44,996 | 82.68 % [82.33,83.03] |
1757 | 2.96 % [2.82,3.10] |
1050 | 2.33 % [2.19,2.47] |
||||
| Yes | 4183 | 6.58 % [5.83,7.33] |
9425 | 17.32 % [16.55,18.08] |
1686 | 40.31 % [38.82,41.79] |
3038 | 32.23 % [31.29,33.18] |
||||
| Substance-related disorder | ||||||||||||
| No | 60,882 | 95.79 % [95.63,95.95] |
48,240 | 88.64 % [88.36,88.93] |
2979 | 4.89 % [4.72,5.06] |
2886 | 5.98 % [5.77,6.19] |
54 | 0.09 % [0.07,0.11] |
82 | 0.17% [0.13,0.21] |
| Yes | 2678 | 4.21 % [3.45,4.97] |
6181 | 11.36 % [10.57,12.15] |
464 | 17.33 % [15.89,18.76] |
1202 | 19.45 % [18.46,20.43] |
44 | 1.64% [1.16,2.12] |
160 | 2.59% [2.19,2.98] |
FPL = federal poverty level; POS = point of service; EPO = exclusive provider organization; HMO = health maintenance organization; PPO = preferred provider organization.
4. Discussion
Depression and suicidal ideation diagnoses during pregnancy increased significantly between 2008 and 2018 in a sample of 536,647 commercially insured birthing people. The results provide an estimate of diagnosis rates of depression and suicidal ideation during pregnancy. Most studies on mental health during pregnancy limit describing the prevalence of depression symptomology to a single time point. This study found that an upward trend in depression diagnosis and suicidal ideation diagnosis, similar to trends suicidal ideation increasing among female adolescents and Black youth (Lindsey et al., 2019; Pontes et al., 2020) This study also describes trends over time and the differences in depression diagnosis and suicidal ideation diagnosis by racial and ethnic categories. The rate of depression diagnosis during pregnancy increased disproportionately across racial and ethnic groups, and Black birthing people experienced the sharpest increase. Suicidal ideation diagnosis increased the most for among Black birthing people compared to all groups, resulting in a need for future studies to determine the reasons behind this increase and any change in the resulting treatment of follow up.
A diagnosis can lead to treatment and mental health services, but many barriers, such as culturally responsive communication from providers, persist (Atdjian and Vega, 2005). Past studies documented the way minority adults communicate mental health problems with White providers and the limitations of White providers identifying mental health needs (Bailey et al., 2019). In a recent qualitative report, Black women were more likely to speak with their providers about thoughts of self-harm and suicidal ideation than depression because they perceived providers would only listen to them about serious topics of harm or imminent risks (Hsieh et al., 2021). The risk for reporting suicidal ideation can vary from the first pregnancy and across subsequent pregnancies (Kim et al., 2016). Kim and colleagues found that depression and suicidal ideation during a first pregnancy as strongly associated with depression and suicidal ideation during the postpartum period and recurrence in following pregnancies. By reporting the trends in diagnosis over time, this study presents a story of the overall increase of antenatal depression and suicidal ideation diagnoses.
Recognizing depression in birthing people during pregnancy represents an early, but necessary, step in the perinatal mental health treatment pathway (Byatt et al., 2015) to support individuals in the postpartum period and beyond. An increase in diagnoses could reflect a growing awareness of mental health conditions during pregnancy and its consequences. In addition, the overall increase might result from swift moving policy reform to integrate mental health into primary care settings.
This study has multiple strengths and some limitations. The study presented findings from a privately insured sample and does not provide estimates for rates of depression for publically insured individuals. More than half of births in the United States are covered under public insurance options and thus not including publically insured individuals is a limitation of this study. This study focused on depression and suicidal ideation diagnosis during pregnancy, whereas other studies found that the full spectrum of mental health problems such as bipolar disorder or trauma that can lead to adverse perinatal outcomes (Baer et al., 2016). Despite these limitations, an estimate of the trends in diagnoses over time is important for clinical decision making and evaluation of policy making to determine if diagnoses rates are increasing.
5. Conclusion
This study found increasing trends in antenatal depression and antenatal suicidal ideation diagnoses during pregnancy and the greatest increase exists for Black birthing people. Given recent societal events such as COVID-19 and the public death of George Floyd, these timely findings have clinical relevance. This study highlights the need to pay closer attention to minoritized birthing people, particularly Black women. Identifying patterns and trends in mental health conditions during pregnancy provides critical evidence to support early prevention and interventions in the postpartum period. Several studies find that suicidal ideation during the perinatal period has increased over time (Admon et al., 2021) and can be succesfully identified through depression screening practices (Kim et al., 2015; Kim et al., 2014). Diagnosis is during pregnancy important and remains essential to identify those in need of mental health treatment during pregnancy and possibly extending to the postpartum period.
Acknowledgments
This research was supported by grant R01MH120124 from the National Institute of Mental Health and the Office of Research on Women’s Health and from the National Institute of MInority Health and Health Disparities R01 MD014958.
Footnotes
CRediT authorship contribution statement
Author contributions are as follows: Tabb KM: Conceptualization, Writing - Original draft preparation, Dalton VK: Supervision, Writing - Reviewing and editing, Tilea A: Data curation, Formal analysis Writing - Reviewing and editing, Kolenic GE: Validation and Editing, Admon LK: Writing - Reviewing and editing, Hall SV: Validation and Editing, Zhang X: Data curation, Formal analysis, Ryckman KK Writing - Reviewing and editing, Zivin K: Supervision, Writing - Reviewing and editing, Funding acquisition.
Conflict of interest
No authors have conflicts of interest to disclose.
References
- Admon LK, Dalton VK, Kolenic GE, Ettner SL, Tilea A, Haffajee RL, Brownlee RM, Zochowski MK, Tabb KM, Muzik M, 2021. Trends in suicidality 1 year before and after birth among commercially insured childbearing individuals in the United States, 2006–2017. JAMA Psychiat. 78, 171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhusen JL, Frohman N, Purcell G, 2015. Intimate partner violence and suicidal ideation in pregnant women. Arc.Womens Ment. Health 18, 573–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atdjian S, Vega WA, 2005. Disparities in mental health treatment in US racial and ethnic minority groups: implications for psychiatrists. Psychiatr. Serv 56, 1600–1602. [DOI] [PubMed] [Google Scholar]
- Baer RJ, Chambers CD, Bandoli G, Jelliffe-Pawlowski LL, 2016. Risk of preterm birth by subtype among medi-cal participants with mental illness. Am. J. Obstet. Gynecol 215, 519.e511–519.e519. [DOI] [PubMed] [Google Scholar]
- Bailey RK, Mokonogho J, Kumar A, 2019. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr. Dis. Treat 15, 603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd RC, Joe S, Michalopoulos L, Davis E, Jackson JS, 2011. Prevalence of mood disorders and service use among US mothers by race and ethnicity: results from the National Survey of American life. J. Clin. Psychiatry 72. [DOI] [PubMed] [Google Scholar]
- Byatt N, Levin LL, Ziedonis D, Simas TAM, Allison J, 2015. Enhancing participation in depression care in outpatient perinatal care settings: a systematic review. Obstet. Gynecol 126, 1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- <span /> CCS, H., Healthcare Cost and Utilization Project (HCUP) Clinical Classifications Software (CCS).
- Cohen LS, Nonacs R, Viguera AC, Reminick A, 2004. Diagnosis and treatment of depression during pregnancy. CNSSpectr. 9, 209–216. [DOI] [PubMed] [Google Scholar]
- Davis NL, Smoots AN, Goodman DA, 2019. Pregnancy-related deaths: data from 14 US maternal mortality review committees. Education 40, 8–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delphin-Rittmon ME, Flanagan EH, Andres-Hyman R, Ortiz J, Amer MM, Davidson L, 2015. Racial-ethnic differences in access, diagnosis, and outcomes in public-sector inpatient mental health treatment. Psychol. Serv 12, 158. [DOI] [PubMed] [Google Scholar]
- <span /> E-Tech, Ethnic Technologies.
- Gavin AR, Melville JL, Rue T, Guo YQ, Tabb Dina K, Katon WJ, 2011a. Racial differences in the prevalence of antenatal depression. Gen. Hosp. Psychiat 33, 87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin AR, Tabb KM, Melville JL, Guo YQ, Katon W, 2011b. Prevalence and correlates of suicidal ideation during pregnancy. Arch. Womens Ment. Health 14, 239–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh W-J, Sbrilli MD, Huang WD, Hoang T-M, Meline B, Laurent HK, Tabb KM, 2021. Patients’ perceptions of perinatal depression screening: a qualitative study: study examines perinatal depression screening. Health Aff 40, 1612–1617. [DOI] [PubMed] [Google Scholar]
- Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, Shackelford KA, Steiner C, Heuton KR, Gonzalez-Medina D, Barber R, Huynh C, Dicker D, Templin T, Wolock TM, Ozgoren AA, Abd-Allah F, Abera SF, Abubakar I, Achoki T, Adelekan A, Ademi Z, Adou AK, Adsuar JC, Agardh EE, Akena D, Alasfoor D, Alemu ZA, Alfonso-Cristancho R, Alhabib S, Ali R, Al Kahbouri MJ, Alla F, Allen PJ, AlMazroa MA, Alsharif U, Alvarez E, Alvis- Guzman N, Amankwaa AA, Amare AT, Amini H, Ammar W, Antonio CAT, Anwari P, Arnlov J, Arsenijevic VSA, Artaman A, Asad MM, Asghar RJ, Assadi R, Atkins LS, Badawi A, Balakrishnan K, Basu A, Basu S, Beardsley J, Bedi N, Bekele T, Bell ML, Bernabe E, Beyene TJ, Bhutta Z, Bin Abdulhak A, Blore JD, Basara BB, Bose D, Breitborde N, Cardenas R, Castaneda-Orjuela CA, Castro RE, Catala-Lopez F, Cavlin A, Chang JC, Che X, Christophi CA, Chugh SS, Cirillo M, Colquhoun SM, Cooper LT, Cooper C, Leite ID, Dandona L, Dandona R, Davis A, Dayama A, Degenhardt L, De Leo D, del Pozo-Cruz B, Deribe K, Dessalegn M, Dharmaratne SD, Dilmen U, Ding EL, Dorrington RE, Driscoll TR, Ermakov SP, Esteghamati A, Faraon EJA, Farzadfar F, Felicio MM, Fereshtehnejad SM, de Lima GMF, Forouzanfar MH, Franca EB, Gaffikin L, Gambashidze K, Gankpe FG, Garcia AC, Geleijnse JM, Gibney KB, Giroud M, Glaser EL, Goginashvili K, Gona P, Gonzalez-Castell D, Goto A, Gouda HN, Gugnani HC, Gupta R, Gupta R, Hafezi-Nejad N, Hamadeh RR, Hammami M, Hankey GJ, Harb HL, Havmoeller R, Hay SI, Pi IBH, Hoek HW, Hosgood HD, Hoy DG, Husseini A, Idrisov BT, Innos K, Inoue M, Jacobsen KH, Jahangir E, Jee SH, Jensen PN, Jha V, Jiang GH, Jonas JB, Juel K, Kabagambe EK, Kan HD, Karam NE, Karch A, Karema CK, Kaul A, Kawakami N, Kazanjan K, Kazi DS, Kemp AH, Kengne AP, Kereselidze M, Khader YS, Khalifa SEAH, Khan EA, Khang YH, Knibbs L, Kokubo Y, Kosen S, Defo BK, Kulkarni C, Kulkarni VS, Kumar GA, Kumar K, Kumar RB, Kwan G, Lai T, Lalloo R, Lam H, Lansingh VC, Larsson A, Lee JT, Leigh J, Leinsalu M, Leung R, Li XH, Li YC, Li YM, Liang J, Liang XF, Lim SS, Lin HH, Lipshultz SE, Liu SW, Liu Y, Lloyd BK, London SJ, Lotufo PA, Ma JX, Ma S, Machado VMP, Mainoo NK, Majdan M, Mapoma CC, Marcenes W, Marzan MB, Mason-Jones AJ, Mehndiratta MM, Mejia-Rodriguez F, Memish ZA, Mendoza W, Miller TR, Mills EJ, Mokdad AH, Mola GL, Monasta L, Monis JD, Hernandez JCM, Moore AR, Moradi-Lakeh M, Mori R, Mueller UO, Mukaigawara M, Naheed A, Naidoo KS, Nand D, Nangia V, Nash D, Nejjari C, Nelson RG, Neupane SP, Newton CR, Ng M, Nieuwenhuijsen MJ, Nisar MI, Nolte S, Norheim OF, Nyakarahuka L, Oh IH, Ohkubo T, Olusanya BO, Omer SB, Opio JN, Orisakwe OE, Pandian JD, Papachristou C, Park JH, Caicedo AJP, Patten SB, Paul VK, Pavlin BI, Pearce N, Pereira DM, Pesudovs K, Petzold M, Poenaru D, Polanczyk GV, Polinder S, Pope D, Pourmalek F, Qato D, Quistberg DA, Rafay A, Rahimi K, Rahimi-Movaghar V, Raju M, Rana SM, Refaat A, Ronfani L, Roy N, Pimienta TGS, Sahraian MA, Salomon JA, Sampson U, Santos IS, Sawhney M, Sayinzoga F, Schneider IJC, Schumacher A, Schwebel DC, Seedat S, Sepanlou SG, Servan-Mori EE, Shakh-Nazarova M, Sheikhbahaei S, Shibuya K, Shin HH, Shiue I, Sigfusdottir ID, Silberberg DH, Silva AP, Singh JA, Skirbekk V, Sliwa K, Soshnikov SS, Sposato LA, Sreeramareddy CT, Stroumpoulis K, Sturua L, Sykes BL, Tabb KM, Talongwa RT, Tan F, Teixeira CM, Tenkorang EY, Terkawi AS, Thorne-Lyman AL, Tirschwell DL, Towbin JA, Tran BX, Tsilimbaris M, Uchendu US, Ukwaja KN, Undurraga EA, Uzun SB, Vallely AJ, van Gool CH, Vasankari TJ, Vavilala MS, Venketasubramanian N, Villalpando S, Violante FS, Vlassov VV, Vos T, Waller S, Wang HD, Wang LH, Wang XR, Wang YP, Weichenthal S, Weiderpass E, Weintraub RG, Westerman R, Wilkinson JD, Woldeyohannes SM, Wong JQ, Wordofa MA, Xu GL, Yang YC, Yano Y, Yentur GK, Yip P, Yonemoto N, Yoon SJ, Younis MZ, Yu CH, Jin KY, Zaki ME, Zhao Y, Zheng YF, Zhou MG, Zhu J, Zou XN, Lopez AD, Naghavi M, Murray CJL, Lozano R, 2014. Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JJ, La Porte L, Zhou Y, Adams M, Silver RK, 2016. Persistence of depression and suicide risk within and across pregnancies [7I]. Obstet. Gynecol 127, 75S. [Google Scholar]
- Kim JJ, La Porte LM, Saleh MP, Allweiss S, Adams MG, Zhou Y, Silver RK, 2015. Suicide risk among perinatal women who report thoughts of self-harm on depression screens. Obstet. Gynecol 125, 885–893. [DOI] [PubMed] [Google Scholar]
- Kim JJ, Silver RK, La Porte LM, Zhou Y, Allweiss SB, Adams MG, 2014. Clinical correlates of maternal suicidal ideation detected by perinatal depression screening. Obstet. Gynecol 123, 60S. [Google Scholar]
- Lindsey MA, Sheftall AH, Xiao Y, Joe S, 2019. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogunyemi D, Jovanovski A, Liu J, Friedman P, Sugiyama N, Creps J, Madan I, 2018. The contribution of untreated and treated anxiety and depression to prenatal, intrapartum, and neonatal outcomes. Am.J.Perinatol. Rep 8, e146–e157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pontes NM, Ayres CG, Pontes MC, 2020. Trends in depressive symptoms and suicidality: youth risk behavior survey 2009–2017. Nurs. Res 69, 176–185. [DOI] [PubMed] [Google Scholar]
- Simonovich SD, Nidey NL, Gavin AR, Piñeros-Leaño M, Hsieh W-J, Sbrilli MD, Ables-Torres LA, Huang H, Ryckman K, Tabb KM, 2021. Meta-analysis of antenatal depression and adverse birth outcomes in US populations, 2010–20: study is a meta-analysis of antenatal depression and adverse birth outcomes in the US, 2010–20. Health Aff. 40, 1560–1565. [DOI] [PubMed] [Google Scholar]
- Simpson SM, Krishnan LL, Kunik ME, Ruiz P, 2007. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatry Q. 78, 3–14. [DOI] [PubMed] [Google Scholar]