Abstract
The aim of the study was to reveal whether marathon running influences regulators of lipid metabolism i.e. angiopoietin-like protein 4 (ANGPTL4), interleukin 6 (IL-6) and tumor necrosis factor-α (TNF-α). Plasma concentration of ANGPTL4, IL-6, TNF-α and lipids were determined in samples collected from 11 male runners before the marathon, immediately after the run and at 90 min of recovery. Plasma ANGPTL4 increased during exercise from 55.5 ± 13.4 to 78.1 ± 15.0 ng/ml (P < 0.001). This was accompanied by a significant increase in IL-6, TNF-α, free fatty acids (FFA) and glycerol (Gly) and a decrease in triacylglycerols (TG). After 90 min of recovery ANGPTL4 and TG did not differ from the exercise values, while plasma IL-6, TNF-α, FFA and Gly concentration were significantly lower. The exercise-induced increase in plasma concentration of ANGPTL4 correlated positively with the rise in plasma IL-6, TNF-α, FFA and Gly and negatively with the duration of the run. The increase in plasma IL-6 and TNF-α correlated positively with the rise in Gly. Summarizing, marathon running induced an increase in plasma ANGPTL4 and the value was higher in faster runners. The increase in plasma FFA, IL-6 and TNF-α concentration during a marathon run may be involved in plasma ANGPTL4 release, which could be a compensatory mechanism against FFA-induced lipotoxicity and oxidative stress. All of the analyzed cytokines may stimulate lipolysis during exercise.
Subject terms: Fat metabolism, Fatty acids, Interleukins, Tumour-necrosis factors
Introduction
The energy substrates for prolonged exercise, such as a marathon run, involve both carbohydrates and lipids. The highest oxidation of fatty acids occurs at 63% of maximal oxygen uptake (VO2max), which closely reflects the intensity of a marathon run in slower, recreational runners, while faster runners perform at higher intensities (70–75% of VO2max) and shift more towards carbohydrates1,2. The exercise duration is also important: after 90–120 min of exercise the contribution of fatty acids oxidation towards covering energy demand increases significantly3. Practically, lipid metabolism is of great importance for marathon runners in order to avoid the “hitting the wall” phenomenon and conditioning the aerobic capacity is one of the key factors in the adaptation to endurance training4,5. The source of fatty acids oxidized during exercise originates from triacylglycerols (TG) stored in skeletal muscles and adipose tissue, as well as in chylomicrons and very low density lipoproteins (VLDL) circulating in blood6–8. Lipolysis of intracellular TG is catalysed successively by three lipases: adipose triglyceride lipase, hormone-sensitive lipase and monoacyglycerol lipase7,8. Hydrolysis of plasma TG-rich lipoproteins takes place at the luminal surface of capillary endothelium with the participation of lipoprotein lipase (LPL)9,10. It was demonstrated that baseline LPL activity of both adipose tissue and skeletal muscles was significantly higher in long-distance runners than in untrained men11,12.
Besides other hormones, neurotransmitters and cytokines, the molecules involved in glucose and lipid metabolism during various forms of physical activity, as well as in inflammatory processes, include angiopoietin-like protein 4 (ANGPTL4), interleukin 6 (IL-6) and tumor necrosis factor-α (TNF-α)13–15. All of them stimulate intracellular adipocyte lipolysis, thus increasing the plasma level of free fatty acids (FFA) and glycerol (Gly)16–18. Moreover, ANGPTL4 catalyses the inactivation of the LPL monomers and locally reduces the uptake of TG-derived fatty acids into the tissue19–21. Makoveichuk et al. found that ANGPTL4 was a crucial mediator of the inhibitory effect of TNF-α on LPL activity in adipose tissue22. Interestingly, experimental studies have shown that TNF-α, unlike IL-6, exerts no effect on the oxidation of fatty acids in muscles, but increases its incorporation into diacylglycerols23.
It was demonstrated that the expression of ANGPTL4 was highly stimulated by FFA which are agonists for peroxisome proliferator-activated receptors (PPARs) in myocytes, cardiomyocytes, macrophages (PPAR-δ), adipocytes (PPARγ) and hepatocytes (PPARα)10,19,24. Several studies showed that strenuous exercise associated with muscle soreness markedly induced the expression of ANGPTL4 in adipose tissue, skeletal muscles and the liver25–27. Contracting skeletal muscles were also found to be the main sources of circulating IL-6 and TNF-α during exercise, while in the recovery period the molecules were mainly released from adipose tissue28–30. The other factors that can stimulate the production and secretion of ANGPTL4, IL-6 and TNF-α include: low glucose availability, inflammation, oxidative stress, catecholamines, hypoxia and hyperthermia13,24,28,31.
It has been proven that prolonged strenuous exercise triggers an omnidirectional inflammatory response which involves the release of both pro-inflammatory (IL-1, IL-8, TNF-α, IFN-γ, VEGF) and anti-inflammatory (IL-2, IL-4, IL-10, IL-13) plasma cytokines32. The balance between pro- and anti-inflammatory cytokines release is critical for prevention of excessive inflammation and for promotion of tissue repair process. The major role in the immune response is played by toll-like receptors (trans-membrane proteins, TLR) that are widely distributed in both the immune and other body cells such as myocytes, adipocytes and hepatocytes33. Some studies reported that ANGPTL4 was involved in acute inflammatory response and showed a potentially anti-inflammatory activity34,35. A marked increase in plasma concentration of IL-1 receptor antagonist, IL-6, IL-8, IL-10 and TNF-α was observed in endurance-trained men immediately after the marathon completion36,37. To the best of our knowledge, to date, no studies have been conducted to assess the effect of a marathon run on plasma ANGPTL4 in healthy, endurance-trained men.
The purpose of the present study was to investigate the effect of a marathon run on plasma ANGPTL4 and to find out whether the exercise-induced changes in plasma ANGPTL4 are related to those of plasma IL-6, TNF-α and lipids concentration.
Materials and methods
Subjects
The study included eleven well-trained endurance runners with three years’ experience in physical training and endurance events. Table 1 presents the general characteristics of the subjects. None of the subjects had serum lipid parameters outside the normal range. The whole research was performed in accordance with relevant regulations, including the Declaration of Helsinki. The procedure was approved by the Local Ethics Committee at Medical University of Warsaw, permission number KB/73/A/2014. All subjects signed the informed consent statement and underwent a medical examination prior to being included in a study.
Table 1.
Subject characteristics (n = 11).
| Parameters | Mean ± SEM |
|---|---|
| Age (years) | 33.7 ± 1.2 |
| Body height (cm) | 177.2 ± 1.9 |
| Body mass (kg) | 75.0 ± 2.0 |
| Body mass index (kg/m2) | 24.0 ± 0.8 |
| Maximal oxygen consumption (ml/kg/min) | 54.8 ± 1.2 |
| Running history (years) | 3.0 ± 0.6 |
| Training volume (km/week) | 60.4 ± 4.5 |
| Training time (h/week) | 5.6 ± 0.6 |
| Running time in present race (h) | 4.1 ± 0.2 |
| Running speed in present race (km/h) | 10.6 ± 0.5 |
| Average running intensity (%VO2max) | 67.8 ± 1.4 |
Experimental protocol
The subjects were recruited from marathoners who completed a street marathon of a distance of 42.2 km (Warsaw Marathon). The run was held in September when the air temperature typically oscillates between 13 and 16 °C with 55–60% humidity and 1020–1021 hPa atmospheric pressure. The race started at 9:00 a.m., and the runners had to reach the finish line within 7 h. Our subjects’ individual finishing times ranged from 3.17 to 5.71 h. However, the average running speeds measured at 10, 21, 30 and 42.2 km were not significantly different from each other and amounted to 10.6 ± 0.5; 11.1 ± 0.5; 10.8 ± 0.6; and 10.2 ± 0.6 km/h, respectively. The subjects ran at the estimated mean intensity of 67.8 ± 1.4% of VO2peak. There were 15 service points every 2–3 km along the marathon route with water, isotonic drinks and high-carbohydrate snacks (bananas, lump sugar, drops, carbohydrate gels). The analysis of the runners’ reports revealed a mean intra-marathon energy intake of 848.4 ± 62.7 kcal and fluid intake of 2.79 ± 0.16 l. The mean hourly intake of carbohydrates was recorded at 51.9 ± 2.2 g/h and was in accordance with the recommendation of the American College of Sports Medicine to maintain oxidation of carbohydrates and delay fatigue38.
One week before the run, the subjects underwent the incremental, graded exercise test on a T2000 treadmill (GE, USA) until volitional exhaustion to determine their peak oxygen uptake. The treadmill speed started at 6 km/h and was increased by 2 km/h every 3 min. Pulmonary ventilation, O2 uptake, CO2 production were recorded using the Vmax 29 system (SensorMedics, USA).
On the day of the marathon, after a 30-min pre-run resting period, immediately after the run and at the 90 min of recovery blood samples were taken from the antecubital vein to determine the plasma concentration of ANGPTL4, IL-6, TNF-α, TG, FFA, Gly, total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C) and glucose. Blood samples were collected in EDTA containing tubes and centrifuged at 1700×g for 15 min at 4 °C. Plasma samples were frozen at − 20 °C and then transported and stored at − 80 °C until assay. Whole-blood samples were used to measure lactate (LA) concentration and the hematocrit. The 90-min recovery period was selected based on the data from the available literature39,40.
Blood sample analysis
The plasma ANGPTL4 concentration was measured by enzyme-linked immunosorbent assay using DuoSet ELISA Development kit (R&D Systems, USA) that recognized full-length ANGPTL4 in human plasma41. The intra-assay coefficient of variation of this method was 7.6% ± 0.7 (n = 70), while inter-assay coefficient of variation was 16.8% ± 1.8 (n = 33). High-sensitivity ELISA kits (Quantikine HS ELISA Human Immunoassay) provided by R&D Systems (USA) were used for the pre-run blood samples for IL-6 and TNF-α, because these cytokines exist at very low levels in peripheral blood. The intra-assay coefficient of variation of these methods for IL-6 and TNF-α equaled 4.1%, and 2.0%, respectively. Quantitative sandwich ELISA kits (R&D Systems, USA) were used for the post-run and recovery blood samples for IL-6 and TNF-α. The intra-assay coefficients of variation of these methods for IL-6 and TNF-α was 2.6%. The plasma FFA concentration was measured using standard enzymatic colorimetric assay (ACS-ACOD Method, Wako Chemicals GmbH, Germany). The intra-assay coefficient of variation was 1.5%. The plasma concentration of TG, Gly, TC, LDL-C and HDL-C was determined by enzymatic methods using manual diagnostic kits (Randox Laboratories Limited, United Kingdom). The intra-assay coefficients of variation for these assays did not exceed 6.4%. Plasma glucose concentration was measured enzymatically using Glucose Oxidase Reagent Set (Pointe Scientific Inc., USA). Lactate concentration was determined using strip analyzer Lactate Scout (EKF Diagnostics, Germany). Hematocrit was measured in duplicate. Whole blood samples (~ 9 μl) were transferred to heparinized microcapillary tubes and analyzed by an automated system following microcentrifugation. Hematocrit was used to calculate percent changes in plasma volume. The percentage changes in plasma volume were calculated using Van Beaumont's equation42.
Statistical analysis
The statistical analysis was performed according to the previously presented scheme40. The data are presented as means with standard errors (SEM). The normality of variables distribution was checked with the Shapiro–Wilk test. The homogeneity of variances was tested with the Levene test. Normally distributed parameters were compared using one-way analysis of variance (ANOVA) for repeated measures. When the ANOVA revealed a statistically significant effect (P < 0.05), the Bonferroni test was used for “post hoc” comparisons. Variables with non-normal distribution (TNF-α, IL-6, FFA, Gly, LA, TC, LDL-C, TG/HDL-C), were compared using the Friedman ANOVA rank test and the Wilcoxon test with the Bonferroni correction for multiple comparisons (P < 0.02). Correlation coefficients were calculated between normally distributed variables (the exercise-induced increases, deltas) using the Pearson’s linear regression analysis and Spearman’s correlations for the non-normally distributed recovery data (P < 0.05 was accepted as the level of significance). For calculations, the Statistica 6 software was used (Statsoft Inc., USA).
Results
ANGPTL4, TNF-α, IL-6, FFA, Gly, TG, TC, HDL-C and LDL-C
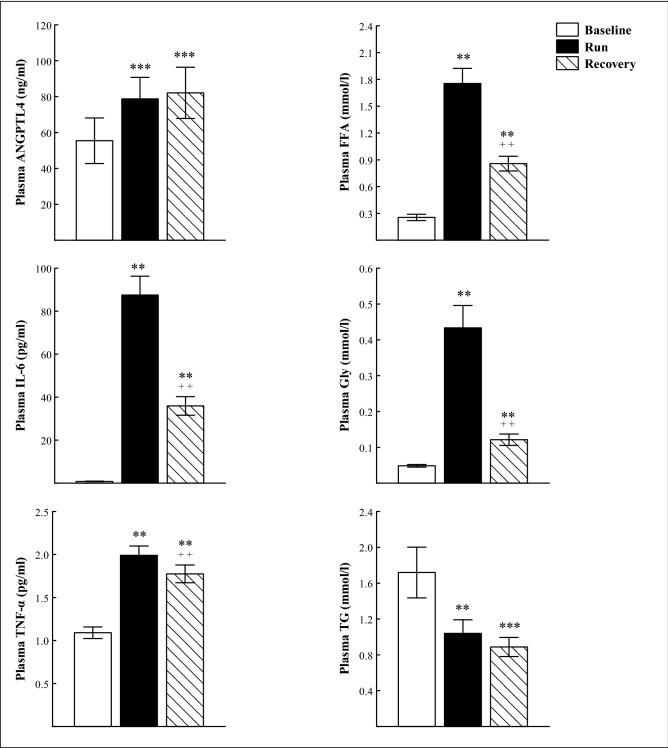
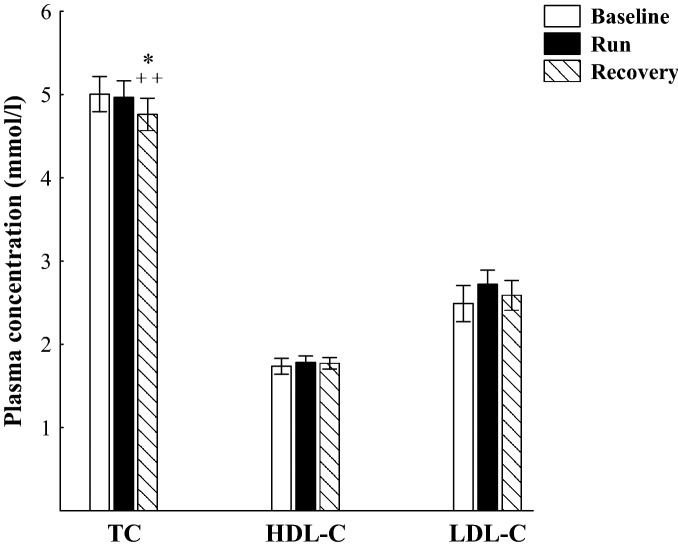
Immediately after the marathon run, a significant increase was found in plasma concentration of ANGPTL4 (P < 0.001), TNF-α, IL-6, FFA and Gly (P < 0.01), whereas TG concentration was observed to decrease (P < 0.01; Fig. 1). Directly after the run, plasma concentration of TC and its fractions (HDL-C and LDL-C) did not differ from the baseline values (Fig. 2), but molar ratio of TG/HDL-C was significantly reduced (P < 0.01; Table 2). Plasma ANGPTL4 concentration recorded 90 min after the run was similar to that obtained immediately after the exercise, whereas plasma concentration of TNF-α and IL-6, as well as FFA and Gly, were significantly decreased compared to the exercise values (P < 0.01), but they were still higher than the baseline values (P < 0.01; Fig. 1). During the recovery, plasma TG concentration remained unaffected but it was significantly lower than before the run (P < 0.001; Fig. 1). At the 90 min of recovery plasma TC concentration was markedly decreased compared to the exercise (P < 0.01) and baseline (P < 0.02) values (Fig. 2), whereas the average molar ratios of TC/HDL-C and TG/HDL-C were significantly reduced compared to the baseline values (Table 2).
Figure 1.
The plasma concentration of angiopoietin-like protein 4 (ANGPTL4), interleukin 6 (IL-6), tumor necrosis factor-α (TNF-α), free fatty acids (FFA), glycerol (Gly) and triacylglycerols (TG) before (Baseline), immediately after marathon run (Run) and at the 90 min of recovery (Recovery). The values are mean ± SEM (n = 11). Asterisks denote significant differences from the resting values: **P < 0.01, ***P < 0.001. Crosses denote significant differences from the exercise values: ++P < 0.01.
Figure 2.
The plasma concentration of total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C) and low-density lipoprotein-cholesterol (LDL-C) before (Baseline), immediately after marathon run (Run) and at the 90 min of recovery (Recovery). The values are mean ± SEM (n = 11). Asterisks denote significant differences from the resting values: *P < 0.02. Crosses denote significant differences from the exercise values: ++P < 0.01.
Table 2.
The molar ratios of total cholesterol to high-density lipoprotein-cholesterol (TC/HDL-C) and triacylglycerols to high-density lipoprotein-cholesterol (TG/HDL-C) before (Baseline), immediately after marathon (Run) and at 90 min of recovery (Recovery) (n = 11). The values are means ± SEM. Asterisks denote significant differences from the resting values: **P < 0.01.
| Parameters | Baseline | Run | Recovery |
|---|---|---|---|
| TC/HDL-C | 2.95 ± 0.17 | 2.83 ± 0.14 | 2.72 ± 0.13 ** |
| TG/HDL-C | 1.10 ± 0.25 | 0.61 ± 0.11 ** | 0.52 ± 0.07 ** |
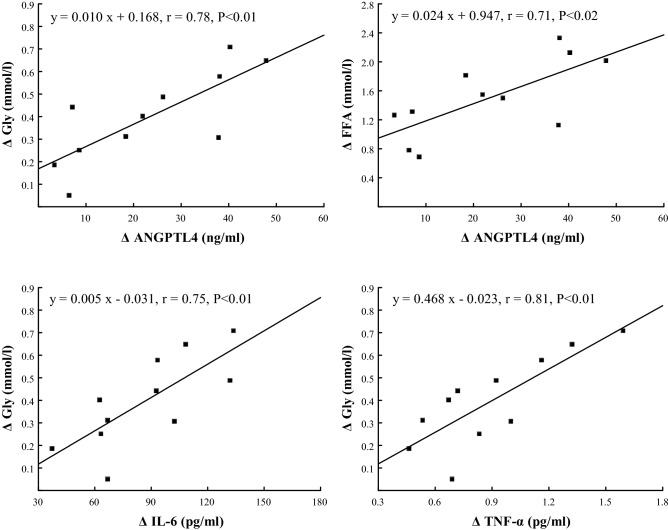
The exercise-induced increase in plasma concentration of ANGPTL4 correlated positively with the rise in plasma IL-6 (r = 0.71, P < 0.02), TNF-α (r = 0.83, P < 0.01), FFA (r = 0.71, P < 0.02) and Gly (r = 0.78, P < 0.01) (Figs. 3 and 4), and correlated negatively with the duration of the run (r = − 0.73, P < 0.02) (Fig. 5). The exercise-induced changes in plasma IL-6 concentration correlated with the fluctuation of plasma TNF-α concentration (r = 0.80, P < 0.01) (Fig. 3). The increases in plasma IL-6 and TNF-α correlated positively with those of Gly (r = 0.75 and r = 0.81, respectively, both P < 0.01) (Fig. 4). The exercise-induced increases in plasma FFA and Gly correlated negatively with individual running times (r = − 0.64, r = − 0.60, respectively, both P < 0.05) (Fig. 5). The positive correlation between plasma concentration of IL-6 and TNF-α was found at the 90th min of recovery (r = 0.73, P < 0.05).
Figure 3.
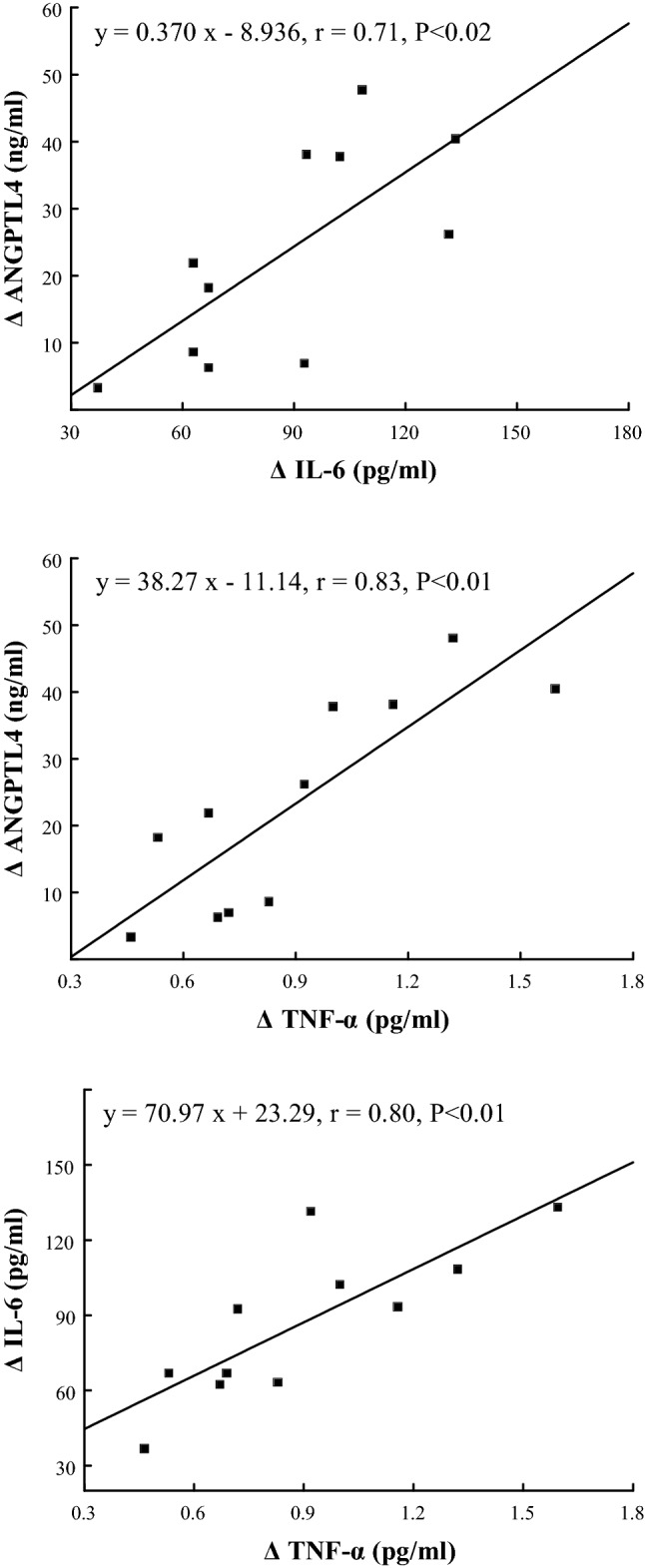
The relationships between exercise-induced changes in plasma concentration of angiopoietin-like protein 4 (ANGPTL4) and those of plasma interleukin 6 (IL-6), tumor necrosis factor-α (TNF-α) as well as between exercise-induced changes in plasma concentration of IL-6 and TNF-α.
Figure 4.
The relationships between exercise-induced changes in plasma concentration of free fatty acids (FFA), glycerol (Gly) and those of plasma angiopoietin-like protein 4 (ANGPTL4), interleukin 6 (IL-6) and tumor necrosis factor-α (TNF-α).
Figure 5.
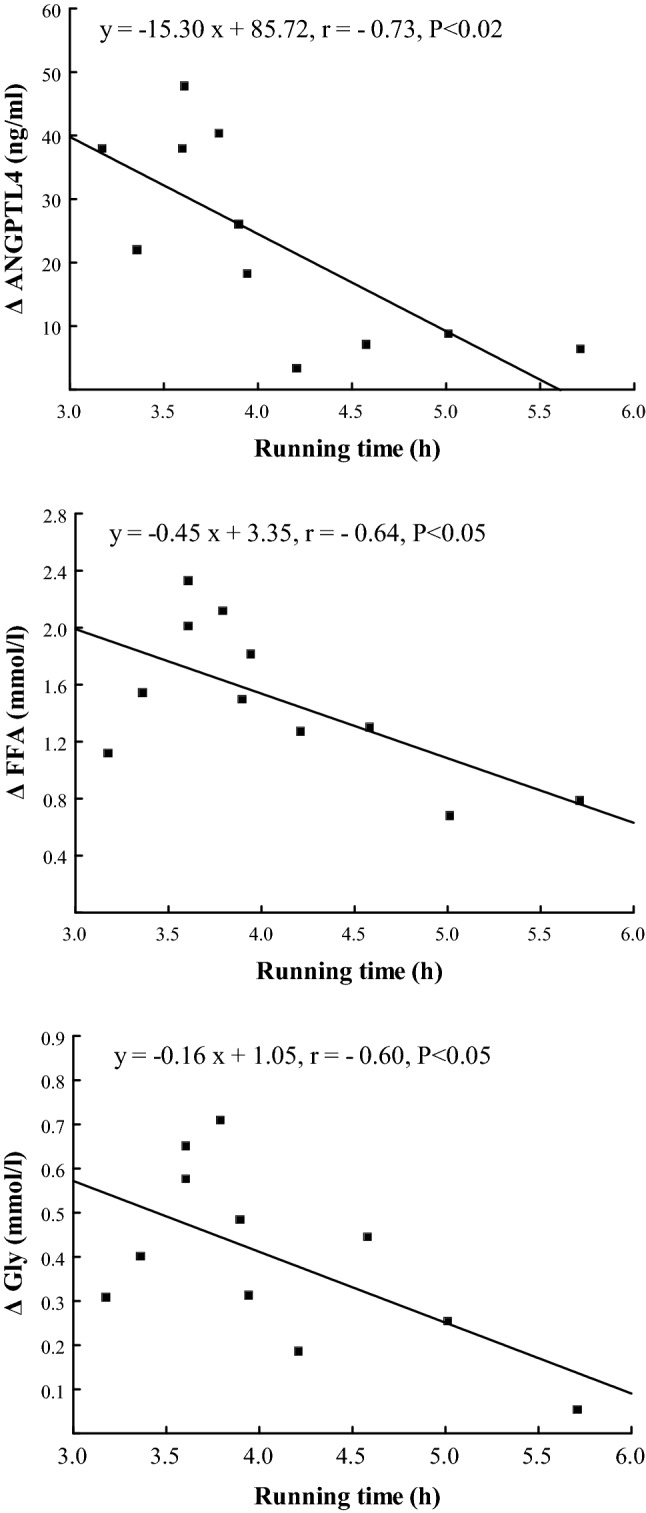
The relationships between exercise-induced changes in plasma concentration of angiopoietin-like protein 4 (ANGPTL4), free fatty acids (FFA) and glycerol (Gly) and running times obtained by marathoners.
Glucose, LA, Hematocrit
Plasma glucose concentration did not differ significantly from the baseline level. Plasma LA concentration was significantly increased immediately after the run (a rise from 1.66 ± 0.16 mmol/l to 3.93 ± 0.40 mmol/l was recorded) (P < 0.01). The exercise-induced changes in plasma LA correlated negatively with individual running times (r = − 0.68, P < 0.03). No significant changes were found in hematocrit.
Discussion
The new finding of the present study is that the marathon run induced a significant increase in the plasma ANGPTL4 concentration in healthy, endurance-trained, young men, which was accompanied by a significant increase in plasma concentration of IL-6, TNF-α, FFA and Gly. Furthermore, significant positive correlations were found between exercise-induced increases in plasma ANGPL4 and those of plasma IL-6, TNF-α, FFA and Gly. The positive relationship between exercise-induced changes in plasma ANGPTL4 and those of plasma FFA shown in this study confirmed the data obtained in our previous investigation performed in healthy young men during a mountain ultra-marathon run40. We argued then that the elevated level of ANGPTL4 increased plasma FFA and the raised FFA would boost the release of ANGPTL4. Many authors have reported that ANGPTL4 may, independently of other factors such as catecholamines, cortisol, glucagon, growth hormone, IL-6 or TNF-α, stimulate adipocyte tissue lipolysis leading to the elevation of plasma FFA level18,43. It has also been shown that ANGPTL4 simultaneously raises plasma TG level by suppressing lipoprotein lipase (LPL)-mediated clearance of plasma TG-rich lipoproteins31,44. The inhibition of LPL by ANGPTL4 occurs before GPIHBP1 (glycosylphosphatidylinositol-anchored high density lipoprotein-binding protein 1) interaction with LPL and its transport to the luminal site of the capillary endothelium19,21.
In the present study the exercise-induced increase in plasma concentration of ANGPTL4, FFA and Gly was observed to reach higher values in faster runners (who deplete carbohydrate stores more rapidly) and the rise correlated negatively with the running time. Moro et al. have found that the rate of adipose tissue lipolysis and plasma FFA concentration depend on the availability of glycogen in working muscles45. A greater lipolytic response could not be explained solely by significant changes in lipolytic stimuli, such as increased catecholamines, atrial natriuretic peptide, growth hormone, cortisol and IL-6 or a decrease in circulating insulin during moderate intensity exercise. The emerging evidence indicates that contracting skeletal muscles can release specific substances called exerkines which enable remote signaling with adipose tissue46. Therefore, the present results may suggest that ANGPTL4 could play a role of an exerkine that is produced in case of reduced glycogen availability in working skeletal muscles or in the liver to promote lipolysis in adipose tissue.
The data obtained by Kersten et al. suggest that the effect of endurance exercise, severe energy restriction and fasting on plasma ANGPTL4 may be mediated by an elevated plasma FFA via PPARα and PPARβ/δ24. Robciuc et al. demonstrated that the activation of PPARδ/retinoic X receptor (RXR) upregulated ANGPTL4 gene expression causing the inhibition of LPL activity and LPL-dependent FFA uptake in myotubes19. The activation of the FFA-PPARδ/RXR-ANGPTL4 axis functions as a negative feedback mechanism that may serve to protect the skeletal muscle fibers from lipid overload and the related oxidative stress19,34. Interestingly, Staiger et al. found that the induction of the ANGPTL4 gene expression in myotubes was independent of the degree of saturation and the length of the FFA47. The PPAR/RXR heterodimer can be activated by FFA produced locally via LPL-mediated TG hydrolysis of VLDL and chylomicrons, as well as by FFA derived from adipocyte lipolysis. Strong evidence suggests that 5′AMP-activated protein kinase (AMPK) activation, as would occur in exercising muscle, counteracted FFA induction of ANGPTL425.
The exercise-induced increase in plasma ANGPTL4 observed in the present study correlated positively with the changes in plasma TNF-α and IL-6. Several studies have reported increased plasma IL-6 and TNF-α levels in endurance-trained men immediately following a marathon run37,48. Cho et al. found that TNF-α released from infiltrated macrophages stimulated ANGPTL4 expression in mesenchymal stem cells by retinoic acid receptor-related orphan receptor which binds to ANGPTL4 gene promoter35. It was also showed that human recombinant TNF-α increased plasma concentration of IL-6, which in turn inhibited TNF-α production17,36. TNF-α, unlike IL-6, had no impact on muscle fatty acid oxidation but it increased the release of free fatty acids from adipose tissue and their incorporation into diacylglycerol, which may be involved in the development of TNF-α-induced insulin resistance in skeletal muscles23. Bernecker et al. reported a twofold increase in TNF-α after a marathon run in addition to a nearly 100-fold increase in IL-6 values37. Several studies showed that IL-6 release from contracting muscle was regulated in response to exercise, being affected by the intensity and duration of exercise as well as by energy substrates availability and muscle mass involved28,49. The main stimulus for IL-6 synthesis and release during exercise is provided by muscle contraction, however, the transcription factors that are known to regulate IL-6 synthesis could also be activated by the decrease in muscle glycogen content and increased formation of reactive oxygen species49. Moreover, IL-6 produced in contracting skeletal muscles can act in an autocrine manner and stimulate muscle IL-6 synthesis50. Lipid turnover is enhanced by IL-6, stimulating fat oxidation and lipolysis in conjunction with catecholamines and cortisol16,51. IL-6 has also been reported to mobilize extracellular substrates and augment substrate delivery during exercise52. In several studies IL-6 was found to correlate positively with an increase in FFA which are an important energy substrate during strenuous endurance exercise16,51.
It has been reported that muscle and joint trauma results in the activation of circulating monocytes which, in turn, produce large quantities of pro-inflammatory IL-1, IL-6, and TNF-α53. Starkie et al. speculated that more than a 100-fold increase in plasma IL-6 concentration after a marathon run could be attributed to muscle damage36. The authors found that the elevated plasma IL-6 was accompanied by an increase in creatine kinase which is an indicator of muscle membrane damage. However, some studies have shown that the muscle damage-induced production of IL-6 is significantly lower than the production of IL-6 triggered by muscle contractions54. There is evidence that IL-6 and TNF-α are released from both damaged myofibers and infiltrating immune cells (fibro-adipogenic progenitors (FAP cells, muscle interstitial mesenchymal cells) and macrophages and neutrophils), which is required for muscle regeneration and repair30,55,56.
The present study also showed significant positive correlations between exercise-induced increases in plasma Gly and both IL-6 and TNF-α. This indicates that these cytokines may be involved in adipose tissue lipolysis and fatty acid mobilization during the marathon run. Interestingly, FFA have been suggested to induce chronic low-grade inflammation and activate the innate immune system. It was found that saturated FFA induced inflammation, while polyunsaturated FFA produced anti-inflammatory effect57. Hartung et al. noted a progressive increase in the ratio of unsaturated to saturated FFA during the marathon run58. Some authors suggested that local FFA efflux from adipocytes may be an important regulator of inflammation and macrophage recruitment to adipocyte tissue59. There is some evidence that saturated fatty acids serve as a ligand for TLR4, thereby inducing the inflammatory changes in both adipocytes and macrophages through the nuclear factor kappa B (NF-κB) activation60. NF-κB dimers activate the transcription of many κB-dependent genes, such as the genes of pro-inflammatory cytokines, including IL-6, TNF-α and IL-1β. Adipose tissue macrophages are a prominent source of these pro-inflammatory cytokines and together with adipocytes interact in a paracrine manner60. Polyunsaturated fatty acids, unlike saturated fatty acids, can reduce the synthesis of TNF-α and IL-6 by downregulating NF-κB. The anti-inflammatory effects of IL-6 have been shown to be related to a crosstalk between muscle tissue and adipose tissue.
Conclusions
Marathon running induced an increase in plasma ANGPTL4 and the value was higher in faster runners. Increases in plasma FFA, IL-6 and TNF-α are probably involved in the release of ANGPTL4. Significant positive relationships between plasma ANGPTL4 and FFA may indicate that the elevated level of FFA stimulates ANGPTL4 release to circulation and the increased concentration of ANGPTL4 could increase FFA mobilization from adipose tissue. Enhanced ANGPTL4 secretion is a potential compensatory mechanism which prevents FFA-induced lipotoxicity and oxidative stress, especially in the tissues uninvolved in the exercise. ANGPTL4, IL-6 and TNF-α may, independently from catecholamines and other factors, stimulate adipose tissue lipolysis during prolonged exercise.
Acknowledgements
The study was partly supported by the National Science Centre of Poland, research grant N N404 204739. The authors would also like to thank Lidia Wiśnik (technician) for her technical support.
Abbreviations
- ANGPTL4
Angiopoietin-like protein 4
- FFA
Free fatty acids
- Gly
Glycerol
- HDL-C
High density lipoprotein-cholesterol
- IL-6
Interleukin 6
- LA
Lactate
- LPL
Lipoprotein lipase
- LDL-C
Low density lipoprotein-cholesterol
- TC
Total cholesterol
- TG
Triacylglycerols
- TNF-α
Tumor necrosis factor-α
- VLDL
Very low density lipoproteins
- VO2 max
Maximal oxygen uptake
Author contributions
A.W.Z., K.K., T.M., M.G. contributed to the conception and design of the experiments. K.K., T.M., M.G. conducted the experiment. A.W.Z., M.G., K.K., T.M. analyzed the data. M.G., K.K. wrote the manuscript. All authors participated in interpreting the data, revising the article and approving the final version for publication and agree with the order of presentation of the authors.
Data availability
All the data are available on request from the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Monika Górecka and Krzysztof Krzemiński.
References
- 1.Achten J, Jeukendrup AE. Maximal fat oxidation during exercise in trained men. Int. J. Sports Med. 2003;24:603–608. doi: 10.1055/s-2003-43265. [DOI] [PubMed] [Google Scholar]
- 2.Spriet LL. Regulation of substrate use during the marathon. Sports Med. 2007;37:332–336. doi: 10.2165/00007256-200737040-00015. [DOI] [PubMed] [Google Scholar]
- 3.De Feo P, et al. Metabolic response to exercise. J. Endocrinol. Investig. 2003;26:851–854. doi: 10.1007/BF03345235. [DOI] [PubMed] [Google Scholar]
- 4.Carter SL, Rennie C, Tarnopolsky MA. Substrate utilization during endurance exercise in men and women after endurance training. Am. J. Physiol. Endocrinol. Metab. 2001;280:E898–E907. doi: 10.1152/ajpendo.2001.280.6.E898. [DOI] [PubMed] [Google Scholar]
- 5.Goodpaster BH, He J, Watkins S, Kelley DE. Skeletal muscle lipid content and insulin resistance: Evidence for a paradox in endurance-trained athletes. J. Clin. Endocrinol. Metab. 2001;86:5755–5761. doi: 10.1210/jcem.86.12.8075. [DOI] [PubMed] [Google Scholar]
- 6.Morio B, Holmbäck U, Gore D, Wolfe RR. Increased VLDL-TAG turnover during and after acute moderate-intensity exercise. Med. Sci. Sports Exerc. 2004;36:801–806. doi: 10.1249/01.mss.0000126498.04454.c0. [DOI] [PubMed] [Google Scholar]
- 7.Watt MJ, Cheng Y. Triglyceride metabolism in exercising muscle. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2017;1862:1250–1259. doi: 10.1016/j.bbalip.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Lass A, Zimmermann R, Oberer M, Zechner R. Lipolysis—A highly regulated multi-enzyme complex mediates the catabolism of cellular fat stores. Prog. Lipid Res. 2011;50:14–27. doi: 10.1016/j.plipres.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldberg IJ, et al. Lipolytic enzymes and free fatty acids at the endothelial interface. Atherosclerosis. 2021;329:1–8. doi: 10.1016/j.atherosclerosis.2021.05.018. [DOI] [PubMed] [Google Scholar]
- 10.Kersten S. Physiological regulation of lipoprotein lipase. Biochim. Biophys. Acta. 2014;1841:919–933. doi: 10.1016/j.bbalip.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 11.Savard R, Després JP, Deshaies Y, Marcotte M, Bouchard C. Adipose tissue lipid accumulation pathways in marathon runners. Int. J. Sports Med. 1985;6:287–291. doi: 10.1055/s-2008-1025853. [DOI] [PubMed] [Google Scholar]
- 12.Vaisberg M, et al. Lipid transfer to HDL is higher in marathon runners than in sedentary subjects, but is acutely inhibited during the run. Lipids. 2012;47:679–686. doi: 10.1007/s11745-012-3685-y. [DOI] [PubMed] [Google Scholar]
- 13.Raschke S, Eckel J. Adipo-myokines: Two sides of the same coin-mediators of inflammation and mediators of exercise. Mediat. Inflamm. 2013;2013:320724. doi: 10.1155/2013/320724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cullen T, Thomas AW, Webb R, Hughes MG. Interleukin-6 and associated cytokine responses to an acute bout of high-intensity interval exercise: The effect of exercise intensity and volume. Appl. Physiol. Nutr. Metab. 2016;41:803–808. doi: 10.1139/apnm-2015-0640. [DOI] [PubMed] [Google Scholar]
- 15.Weigert C, Hoene M, Plomgaard P. Hepatokines-a novel group of exercise factors. Pflugers Arch. 2019;471:383–396. doi: 10.1007/s00424-018-2216-y. [DOI] [PubMed] [Google Scholar]
- 16.Van Hall G, et al. Interleukin-6 stimulates lipolysis and fat oxidation in humans. J. Clin. Endocrinol. Metab. 2003;88:3005–3010. doi: 10.1210/jc.2002-021687. [DOI] [PubMed] [Google Scholar]
- 17.Plomgaard P, Fischer CP, Ibfelt T, Pedersen BK, van Hall G. Tumor necrosis factor-alpha modulates human in vivo lipolysis. J. Clin. Endocrinol. Metab. 2008;93:543–549. doi: 10.1210/jc.2007-1761. [DOI] [PubMed] [Google Scholar]
- 18.McQueen AE, et al. The C-terminal fibrinogen-like domain of angiopoietin-like 4 stimulates adipose tissue lipolysis and promotes energy expenditure. J. Biol. Chem. 2017;292:16122–16134. doi: 10.1074/jbc.M117.803973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robciuc MR, et al. Angiopoietin-like 4 mediates PPAR delta efect on lipoprotein lipase-dependent fatty acid uptake but not on beta-oxidation in myotubes. PLoS One. 2012;7:e46212. doi: 10.1371/journal.pone.0046212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Makoveichuk E, Vorrsjö E, Olivecrona T, Olivecrona G. Inactivation of lipoprotein lipase in 3T3-L1 adipocytes by angiopoietin-like protein 4 requires that both proteins have reached the cell surface. Biochem. Biophys. Res. Commun. 2013;441:941–946. doi: 10.1016/j.bbrc.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 21.Kristensen KK, et al. Unfolding of monomeric lipoprotein lipase by ANGPTL4: Insight into the regulation of plasma triglyceride metabolism. Proc. Natl. Acad. Sci. U. S. A. 2020;117:4337–4346. doi: 10.1073/pnas.1920202117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makoveichuk E, Vorrsjö E, Olivecrona T, Olivecrona G. TNF-α decreases lipoprotein lipase activity in 3T3-L1 adipocytes by up-regulation of angiopoietin-like protein 4. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids. 2017;1862:533–540. doi: 10.1016/j.bbalip.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Bruce CR, Dyck DJ. Cytokine regulation of skeletal muscle fatty acid metabolism: Effect of interleukin-6 and tumor necrosis factor-alpha. Am. J. Physiol. Endocrinol. Metab. 2004;287:E616–E621. doi: 10.1152/ajpendo.00150.2004. [DOI] [PubMed] [Google Scholar]
- 24.Kersten S, et al. Caloric restriction and exercise increase plasma ANGPTL4 levels in humans via elevated free fatty acids. Arterioscler. Thromb. Vasc. Biol. 2009;29:969–974. doi: 10.1161/ATVBAHA.108.182147. [DOI] [PubMed] [Google Scholar]
- 25.Catoire M, et al. Fatty acid-inducible ANGPTL4 governs lipid metabolic response to exercise. Proc. Natl. Acad. Sci. U. S. A. 2014;111:E1043–E1052. doi: 10.1073/pnas.1400889111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Norheim F, et al. Regulation of angiopoietin-like protein 4 production during and after exercise. Physiol. Rep. 2014;2:e12109. doi: 10.14814/phy2.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ingerslev B, et al. Angiopoietin-like protein 4 is an exercise-induced hepatokine in humans, regulated by glucagon and cAMP. Mol. Metab. 2017;6:1286–1295. doi: 10.1016/j.molmet.2017.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pedersen BK, Febbraio MA. Muscle as an endocrine organ: Focus on muscle-derived interleukin-6. Physiol. Rev. 2008;88:1379–1406. doi: 10.1152/physrev.90100.2007. [DOI] [PubMed] [Google Scholar]
- 29.Lyngsø D, Simonsen L, Bülow J. Interleukin-6 production in human subcutaneous abdominal adipose tissue: The effect of exercise. J. Physiol. 2002;543:373–378. doi: 10.1113/jphysiol.2002.019380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhan M, Jin B, Chen SE, Reecy JM, Li YP. TACE release of TNF-alpha mediates mechanotransduction-induced activation of p38 MAPK and myogenesis. J. Cell Sci. 2007;120:692–701. doi: 10.1242/jcs.03372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mandard S, et al. The fasting-induced adipose factor/angiopoietin-like protein 4 is physically associated with lipoproteins and governs plasma lipid levels and adiposity. J. Biol. Chem. 2006;281:934–944. doi: 10.1074/jbc.M506519200. [DOI] [PubMed] [Google Scholar]
- 32.Svensson M, Lexell J, Deierborg T. Effects of physical exercise on neuroinflammation, neuroplasticity, neurodegeneration, and behavior: What we can learn from animal models in clinical settings. Neurorehabil. Neural. Repair. 2015;29:577–589. doi: 10.1177/1545968314562108. [DOI] [PubMed] [Google Scholar]
- 33.Zbinden-Foncea H, Raymackers JM, Deldicque L, Renard P, Francaux M. TLR2 and TLR4 activate p38 MAPK and JNK during endurance exercise in skeletal muscle. Med. Sci. Sports Exerc. 2012;44:1463–1472. doi: 10.1249/MSS.0b013e31824e0d5d. [DOI] [PubMed] [Google Scholar]
- 34.Georgiadi A, et al. Overexpression of angiopoietin-like protein 4 protects against atherosclerosis development. Arterioscler. Thromb. Vasc. Biol. 2013;33:1529–1537. doi: 10.1161/ATVBAHA.113.301698. [DOI] [PubMed] [Google Scholar]
- 35.Cho DI, et al. Antiinflammatory activity of ANGPTL4 facilitates macrophage polarization to induce cardiac repair. JCI Insight. 2019;4:e125437. doi: 10.1172/jci.insight.125437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Starkie RL, Rolland J, Angus DJ, Anderson MJ, Febbraio MA. Circulating monocytes are not the source of elevations in plasma IL-6 and TNF-alpha levels after prolonged running. Am. J. Physiol. Cell Physiol. 2001;280:C769–C774. doi: 10.1152/ajpcell.2001.280.4.C769. [DOI] [PubMed] [Google Scholar]
- 37.Bernecker C, et al. Evidence for an exercise induced increase of TNF-α and IL-6 in marathon runners. Scand. J. Med. Sci. Sports. 2013;23:207–214. doi: 10.1111/j.1600-0838.2011.01372.x. [DOI] [PubMed] [Google Scholar]
- 38.Convertino VA, et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 1996;28:i–vii. doi: 10.1097/00005768-199610000-00045. [DOI] [PubMed] [Google Scholar]
- 39.Henderson GC, et al. Lipolysis and fatty acid metabolism in men and women during the postexercise recovery period. J. Physiol. 2007;584:963–981. doi: 10.1113/jphysiol.2007.137331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Górecka M, et al. Effect of mountain ultra-marathon running on plasma angiopoietin-like protein 4 and lipid profile in healthy trained men. Eur. J. Appl. Physiol. 2020;120:117–125. doi: 10.1007/s00421-019-04256-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smart-Halajko MC, et al. The relationship between plasma angiopoietin-like protein 4 levels, angiopoietin-like protein 4 genotype, and coronary heart disease risk. Arterioscler. Thromb. Vasc. Biol. 2010;30:2277–2282. doi: 10.1161/ATVBAHA.110.212209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Beaumont W. Evaluation of hemoconcentration from hematocrit measurements. J. Appl. Physiol. 1972;32:712–713. doi: 10.1152/jappl.1972.32.5.712. [DOI] [PubMed] [Google Scholar]
- 43.Robciuc MR, et al. Serum angiopoietin-like 4 protein levels and expression in adipose tissue are inversely correlated with obesity in monozygotic twins. J. Lipid Res. 2011;52:1575–1582. doi: 10.1194/jlr.P015867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gutgsell AR, Ghodge SV, Bowers AA, Neher SB. Mapping the sites of the lipoprotein lipase (LPL)-angiopoietin-like protein 4 (ANGPTL4) interaction provides mechanistic insight into LPL inhibition. J. Biol. Chem. 2019;294:2678–2689. doi: 10.1074/jbc.RA118.005932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moro C, et al. Influence of lipolysis and fatty acid availability on fuel selection during exercise. J. Physiol. Biochem. 2014;70:583–591. doi: 10.1007/s13105-013-0306-z. [DOI] [PubMed] [Google Scholar]
- 46.Chow LS, et al. Exerkines in health, resilience and disease. Nat. Rev. Endocrinol. 2022;18:273–289. doi: 10.1038/s41574-022-00641-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Staiger H, et al. Muscle-derived angiopoietin-like protein 4 is induced by fatty acids via peroxisome proliferator-activated receptor (PPAR)-delta and is of metabolic relevance in humans. Diabetes. 2009;58:579–589. doi: 10.2337/db07-1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alves MDJ, et al. Changes in cytokines concentration following long-distance running: A systematic review and meta-analysis. Front. Physiol. 2022;13:838069. doi: 10.3389/fphys.2022.838069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fischer CP. Interleukin-6 in acute exercise and training: What is the biological relevance? Exerc. Immunol. Rev. 2006;12:6–33. [PubMed] [Google Scholar]
- 50.Keller P, et al. Interleukin-6 production by contracting human skeletal muscle: Autocrine regulation by IL-6. Biochem. Biophys. Res. Commun. 2003;310:550–554. doi: 10.1016/j.bbrc.2003.09.048. [DOI] [PubMed] [Google Scholar]
- 51.Petersen EW, et al. Acute IL-6 treatment increases fatty acid turnover in elderly humans in vivo and in tissue culture in vitro. Am. J. Physiol. Endocrinol. Metab. 2005;288:E155–E162. doi: 10.1152/ajpendo.00257.2004. [DOI] [PubMed] [Google Scholar]
- 52.Pedersen BK, et al. The metabolic role of IL-6 produced during exercise: Is IL-6 an exercise factor? Proc. Nutr. Soc. 2004;63:263–267. doi: 10.1079/PNS2004338. [DOI] [PubMed] [Google Scholar]
- 53.Northoff H, Berg A. Immunologic mediators as parameters of the reaction to strenuous exercise. Int. J. Sports Med. 1991;12:S9–S15. doi: 10.1055/s-2007-1024743. [DOI] [PubMed] [Google Scholar]
- 54.Croisier JL, et al. Effects of training on exercise-induced muscle damage and interleukin 6 production. Muscle Nerve. 1999;22:208–212. doi: 10.1002/(sici)1097-4598(199902)22:2<208::aid-mus8>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 55.Joe AW, et al. Muscle injury activates resident fibro/adipogenic progenitors that facilitate myogenesis. Nat. Cell Biol. 2010;12:153–163. doi: 10.1038/ncb2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang C, et al. Interleukin-6/signal transducer and activator of transcription 3 (STAT3) pathway is essential for macrophage infiltration and myoblast proliferation during muscle regeneration. J. Biol. Chem. 2013;288:1489–1499. doi: 10.1074/jbc.M112.419788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Volpe CM, Nogueira-Machado JA. The dual role of free fatty acid signaling in inflammation and therapeutics. Recent Pat. Endocr. Metab. Immune Drug Discov. 2013;7:189–197. doi: 10.2174/18715303113139990041. [DOI] [PubMed] [Google Scholar]
- 58.Hartung GH, Myhre LG, Nunneley SA, Tucker DM. Plasma substrate response in men and women during marathon running. Aviat. Space Environ. Med. 1984;55:128–131. [PubMed] [Google Scholar]
- 59.Michaud A, Pelletier M, Noël S, Bouchard C, Tchernof A. Markers of macrophage infiltration and measures of lipolysis in human abdominal adipose tissues. Obesity (Silver Spring) 2013;21:2342–2349. doi: 10.1002/oby.20341. [DOI] [PubMed] [Google Scholar]
- 60.Suganami T, et al. Role of the Toll-like receptor 4/NF-kappaB pathway in saturated fatty acid-induced inflammatory changes in the interaction between adipocytes and macrophages. Arterioscler. Thromb. Vasc. Biol. 2007;27:84–91. doi: 10.1161/01.ATV.0000251608.09329.9a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data are available on request from the corresponding author.