1. Limitations of schizophrenia paradigm
The DSM-5 definition of schizophrenia faces existential challenges. First, despite decades of efforts, reliability of this diagnosis remains low with interrater kappa =0.46 (Regier et al., 2013) and temporal stability kappa =0.47 (Bromet et al., 2011). Reliability problems are inherent to the paradigm that applies a categorical diagnosis to a psychopathology continuum, producing arbitrary boundaries. Second, these boundaries obscure many similarities with other conditions. For instance, schizophrenia and bipolar disorder are mutually exclusive diagnoses, but many patients have features of both, and these disorders have over-lapping etiology with the genetic correlation rg = 0.71 (Stahl et al., 2019). Third, many people in the general population have subthreshold psychotic experiences but do not fit existing diagnoses (Linscott and Van Os, 2013). Fourth, schizophrenia diagnosis is heterogeneous and includes symptoms that are largely unrelated. For example, in an epidemiologic first-episode psychosis sample, correlations between negative and positive symptoms ranged r = 0.00–0.08 (Kotov et al., 2016).
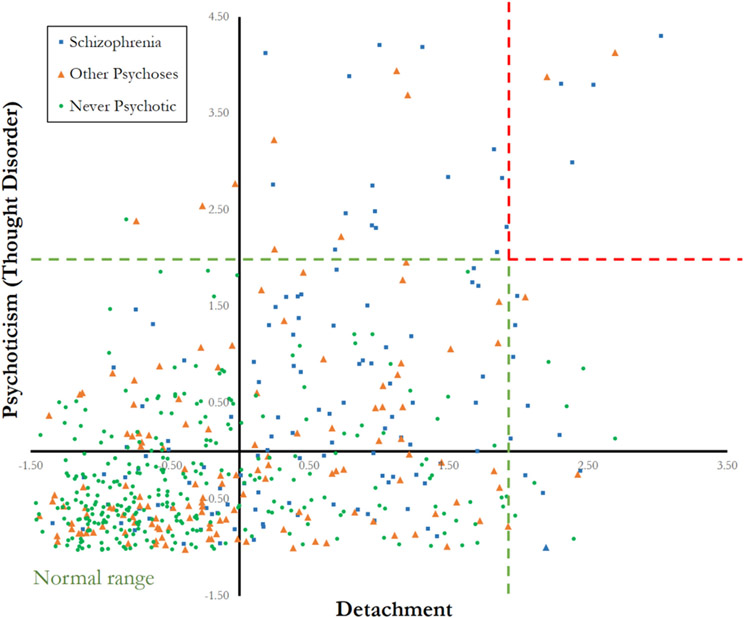
These challenges are illustrated in Fig. 1, which plots participants along two fundamental dimensions: psychoticism (thought disorder) and detachment. This plot reflects typical symptom burden. Participants were assessed in the community, and their symptoms were not acute but nevertheless very disabling for the majority (Kotov et al., 2017a). Schizophrenia, other psychotic disorders, and never-psychotic groups differ substantially on average, but are highly overlapping without any zones of rarity. Some patients show clear elevations on psychoticism or detachment, but few are elevated on both, underscoring heterogeneity of these diagnoses.
Fig. 1. Symptom severity in schizophrenia, other psychoses, and never psychotic adults along two spectra.
Note: Data from the Suffolk County Mental Health Project (Cicero et al., 2019), a 20-year follow-up of psychotic disorders after first hospitalization and demographically-matched never-psychotic participants. It includes 131 participants with schizophrenia, 144 with other psychotic disorders, and 304 never psychotic. Axes are scores on the Eccentric Perceptions (psychoticism) and Detachment scales of the Schedule for Non-adaptive and Adaptive Personality (Clark et al., 2014). Scores were standardized in the full sample, and z-score < 1.96 defined normal range designated with green lines. Jitter was applied to make all data points visible.
2. HiTOP reconceptualization of schizophrenia
The Hierarchical Taxonomy Of Psychopathology (HiTOP) was developed to address the aforementioned challenges across psychopathology (Kotov et al., 2017b, 2021). This model emerged from research on the quantitative nosology, an effort to organize psychopathology according to patterns of co-occurrence among signs and symptoms. This approach has a long history (e.g., Lorr et al., 1963; Moore, 1930; Wittenborn, 1951) and produced numerous widely used instruments, such as the Child Behavior Checklist and Brief Psychiatric Rating Scale (Achenbach and Rescorla, 2001; Overall and Gorham, 1962). HiTOP is developed and continually revised by a consortium of psychologists and psychiatrists who study psychiatric classification. The consortium includes over 165 members and published over 24 peer-reviewed papers (https://renaissance.stonybrookmedicine.edu/HITOP). The consortium recently reviewed evidence regarding the HiTOP model for psychosis-related psychopathology (Kotov et al., 2020). We discuss implications of this evidence for schizophrenia.
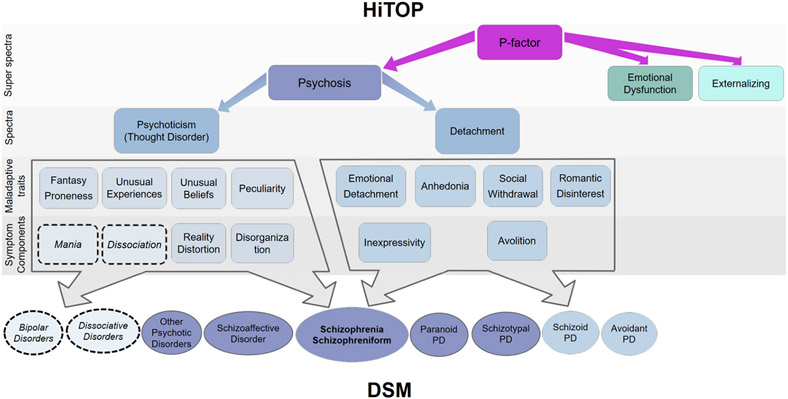
The HiTOP model of psychosis-related psychopathology is depicted in Fig. 2. It describes psychopathology dimensionally, recognizing continuity between schizophrenia, psychotic disorders, certain non-psychotic disorders (e.g., schizotypal personality disorder, dissociative disorders), and normal functioning. Extensive research has supported this continuity (Krueger et al., 2018; Haslam et al., 2020). Also, HiTOP addresses heterogeneity by identifying 14 specific dimensions of symptoms and traits within this domain. These dimensions are internally coherent and replicated (Kotov et al., 2020). The 14 dimensions are correlated and form two empirical spectra: psychoticism and detachment. HiTOP model uses term “thought disorder” for the former, but here we refer to it as “psychoticism” to avoid confusion with “formal thought disorder,” which is only a small component of this spectrum. Indeed, psychoticism includes positive schizotypy traits and positive symptoms. It ranges from conventional and uncreative thinking to perception, cognition, and behavior disconnected from reality. Detachment includes normal introversion, negative schizotypy traits, and negative symptoms. This spectrum ranges from goal-oriented, sociable, and expressive behavior to apathy, disinterest in people, and blunted affect. The spectra are related and jointly form a large psychosis superspectrum (Ringwald et al., 2021).
Fig. 2. Schizophrenia in HiTOP.
Note: Dashed circles indicate that mania and dissociation are include in the model provisionally, because evidence supporting their inclusion is limited. Thought disorder is given in parentheses because it is the term currently used in HiTOP for the psychoticism spectrum. This model integrates evidence from 261 studies of psychopathology structures and 293 studies of their validity and utility (Kotov et al., 2021). This work considered all relevant evidence, including studies that directly measured HiTOP constructs, modeled constructs statistically, or identified common patterns across conditions comprising constructs (e.g., problems that define the detachment spectrum). Construct names differed across studies and were aligned to a common nomenclature.
Fig. 2 does not detail other superspectra, but they are similarly characterized dimensionally and hierarchically. The psychosis superspectrum does not include depression because it is within the emotional dysfunction superspectrum, and substance abuse because it is within the externalizing superspectrum. The superspectra interact (giving rise to the general p-factor), so a comprehensive evaluation would benefit from assessment of all superspectra.
3. Validity and utility of reconceptualization
A number of studies considered validity of psychoticism, detachment, and psychosis dimensions. Each dimension shows coherence on genetic liabilities, environmental risk factors, cognitive and neuro-biologic deficits, antecedents, course, and treatment response (Kotov et al., 2020). Mania is an exception that shares many features with other psychoticism constructs, but is distinguished by less chronic course, better outcome, and response to lithium. Hence, placement of mania within the psychosis superspectrum is provisional, pending further research.
Moreover, the HiTOP model has shown greater reliability, explanatory power, prognostic value, and clinical utility than schizophrenia diagnosis (Kotov et al., 2020). For example, meta-analytic estimates of reliability were 0.81 for psychoticism and 0.85 for detachment (Markon et al., 2011), a nearly 2-fold improvement over schizophrenia diagnosis. Also, HiTOP dimensions explained more variance than psychotic disorder diagnoses in community functioning, cognitive deficits, and neurophysiologic biotypes (Hanlon et al., 2019; Reininghaus et al., 2019). In first-episode psychosis, the prognostic power of dimensions was twice that of diagnoses for predicting 20-year outcomes: remission, community functioning, neural deficits, and diabetes onset (Martin et al., 2021); replicating previous findings (Kotov et al., 2020).
HiTOP builds on the existing practice of selecting treatment according to presenting symptoms, offering a rigorous framework for symptom-based dimensional case conceptualization. This approach showed strong evidence of clinical utility for personality disorders and preliminary evidence for psychotic disorders (Bornstein and Natoli, 2019; Mościcki et al., 2013).
4. Implications for science and practice
The HiTOP approach to schizophrenia has several scientific implications (Table 1). We elaborate on three. First, HiTOP considers schizophrenia a term used for people elevated on two spectra and encourages research on these fundamental dimensions instead. It is particularly important to study detachment regardless of psychosis. Indeed, many people with schizophrenia pathophysiology may develop negative symptoms without psychosis. They are invisible to studies based on traditional diagnoses, distorting our understanding of pathophysiology. Psychosis is the most salient clinical feature, but it is not necessarily most informative etiologically. For example, polygenic risk scores for schizophrenia predict negative symptoms more strongly than positive symptoms (Legge et al., 2021).
Table 1.
Main research implications of HiTOP reconceptualization of schizophrenia.
| Research considerations | Traditional diagnosis | HiTOP model |
|---|---|---|
| Schizophrenia concept | A distinct group of patients | Arbitrary designation for patients elevated above a threshold on two fundamental spectra |
| Role of psychotic symptoms | Necessary diagnostic feature | Not necessary, an extreme end of just one dimension |
| Etiology and pathophysiology | Implied to be largely discrete and specific to schizophrenia | Discrete and specific mechanisms are expected to be rare. The majority of mechanisms are expected to be present across the general population and implicated in many disorders |
| Expectations for case-control study design | Can efficiently isolate common features of schizophrenia group | Is not representative, as it excludes people who are (a) not clear cases or controls and (b) cases with significant comorbidities. Is biased as cases recruited from treatment settings differ from controls on many irrelevant features (intelligence, distress, medication exposure, etc) |
| Optimal design | Case-control with strict inclusion/exclusion criteria | Inclusive population-based studies (perhaps enriched for high scores on spectra) with detailed phenotyping allowing to determine which effects are specific to psychopathology of interest and which are general |
| Participant selection | Definite cases but optimally antipsychotic-naïve or washed out from medications | Moderate severity of psychoticism and detachment (e.g., maladaptive traits) is acceptable. Such people are far more common and usually had no prior treatment. |
| Measurement | Differential diagnosis to separate schizophrenia cases from related disorders (e.g., semi-structured diagnostic interview) | Core description is 2 spectra, which can be elaborate as scores on 14 subdimensions. It covers traits and symptoms. Other HiTOP spectra can be assessed to obtain comprehensive profile. Various interviews, self-report, and informant-report tools are available |
| Scalability | Diagnostic interview is required, low scalability | Brief self-reports can be collected online in large samples and confirmed by interview in subsamples |
Second, HiTOP suggests that abnormalities seen in schizophrenia are on the continuum with normal functioning, and mechanisms under-pinning these deficits can be studied in the general population. For example, polygenic risk for schizophrenia is continuously distributed in the community (Docherty et al., 2020). A shift from the case-control design to large population-based studies can address many limitations of the former (Preacher et al., 2005). Comprehensive profiling of psychopathology can readily reveal which mechanisms and treatments are specific to problem of interest and which are general.
Third, HiTOP conceptualization is aligned with evidence that many patients show mild elevations on the spectra at a young age and eventually progress to frank psychosis (Debbané et al., 2015; Poulton et al., 2000). This emphasizes importance of dimensional description for research on risk and prevention of psychotic disorders.
Clinical applications are outlined in Table 2 and illustrated in Box 1. In particular, diagnosis is reconceptualized as patient’s profile across relevant dimensions rather than a list of categorical descriptors. Overall severity of psychotic disorder is represented by elevations on the two spectra. Specific problems are captured by the 14 dimensions. Symptom dimensions describe current problems. Maladaptive traits assess typical levels of these problems, thus characterizing their chronicity. HiTOP describes psychological dysfunction (e.g., hallucinations, reduced libido) rather than its consequences for functioning in society (e.g., homelessness, no romantic partner). In this, HiTOP is aligned with ICD-11, which recognizes psychopathology whether the person is disabled by it or not (Clark et al., 2017). Although the HiTOP model does not include functioning in society, HiTOP assessment typically includes functioning measures to complement the psychopathology profile.
Table 2.
Main clinical applications of HiTOP reconceptualization of schizophrenia.
| Clinical considerations |
Traditional diagnosis | HiTOP model |
|---|---|---|
| General features | ||
| Reliability | kappa =0.46 for schizophrenia (Regier et al., 2013) | ICC = 0.81 for psychoticism, ICC = 0.85 for detachment (Markon et al., 2011) |
| Validity | Original motivation for schizophrenia was to identify cases with poor prognosis, high impairment, and distinct etiology (Jablensky, 2007) | Appears to be twice more informative than psychotic disorder diagnosis regarding prognosis, community functioning, and neurobiology (Kotov et al., 2020; Martin et al., 2021) |
| Clinical Utility | Efficiently conveys key clinical information with one term. Diagnosis is used more for administrative requirements than treatment decisions (First et al., 2018) | Surveys of clinicians indicate greater utility of dimensional than categorical nosology: robust evidence for personality disorders, emerging evidence for psychotic disorders (Bornstein and Natoli, 2019; Mościcki et al., 2013) |
| Applications | ||
| Risk assessment/Prevention | Attenuated psychosis syndrome is included as a condition for further study | Promises detailed description of risk as elevations on dimensions. It is compatible with clinical high risk and staging models |
| Diagnosis | List of categorical descriptors, severity specifiers are available for some disorders | Patient’s profile across dimensions. Mild, moderate, and marked degree of elevation are indicated on the profile |
| Treatment selection | Existing treatments are approved for traditional diagnoses. Usually provides only one threshold to guide all clinical decisions | Aligned with the common practice of treating symptoms; offers to formalize and supports this approach; also will ultimately allow multiple thresholds tailored to particular clinical actions |
| Tracking treatment progress | Includes criteria for remission | Progression can be tracked as continuous trajectories rather than transition over an arbitrary threshold |
ICC = intraclass correlation coefficient.
Box 1. Clinical application of HiTOP conceptualization to two simulated patients diagnosed with schizophrenia.
Greg A. is a 35-year-old unemployed single man first hospitalized with psychosis 8 years ago. Mr. A’s HiTOP profile reveals a high elevation on the psychoticism spectrum. All subdimensions are elevated except for disorganization and peculiarity. This is consistent with medical records indicating frequent episodes of auditory hallucinations and religious delusions, and two episodes of mania. Psychoticism traits are more elevated than symptoms, which indicates that although psychosis is currently in remission, it is likely to recur. Mr. A is prescribed antipsychotics but frequently stops taking them. Detachment spectrum and its components are in the normal range. This agrees with Mr. A’s report that he maintains an extensive social network and active lifestyle. Given high risk of recurrence indicated by HiTOP profile and history of medication non-adherence, Mr. A was offered depot antipsychotics and referred for cognitive-behavioral therapy for psychosis.
Susan B. is a 50-year-old female employed as a data entry clerk. She first experienced psychosis 16 years ago. HiTOP profile reveals very mild elevation on the psychoticism spectrum, driven entirely by traits of unusual experiences and beliefs rather than symptoms. This pattern aligns with prior history of psychosis that completely remitted and has not recurred in the last five years. Ms. B takes antipsychotics reliably, although she gained considerable weight at the start of treatment and remained obese since. She recently developed diabetes. Detachment spectrum is highly elevated, with most prominent elevations on avolition, anhedonia, and social withdrawal. This is consistent with Ms. B’s report that she lives alone, does not initiate social interactions, and spends her free time aimlessly watching television. Given low risk of psychosis indicated by HiTOP profile and medical history suggesting negative side effects of antipsychotics, Ms. B was offered to discontinue antipsychotics, with weekly monitoring of reality distortion symptoms using a self-report tool on patient portal. HiTOP profile also indicated high negative symptoms, and Ms. B was referred for social skills training psychotherapy, which is efficacious for these symptoms.
Schizophrenia diagnosis provided the same guidance in both cases, indicating that antipsychotics, cognitive-behavior therapy, and social skills training would be efficacious. Additional clinical information was needed to tailor treatment to each patient. HiTOP provided this information, assessing it systematically and quantitatively. HiTOP approach is aligned with the clinical practice of taking careful history and addressing prominent symptoms.
Clinical actions are often dichotomous (e.g., start treatment or wait); therefore, continuous scores require clinical ranges. These ranges can be specified in reference to the general population (e.g., >97.5th percentile considered moderately elevate and > 99th percentile markedly elevated), similar to many laboratory tests or neuropsychological testing (Ruggero et al., 2019). Different actions can be indicated for different ranges, rather than yoking all decisions to the diagnostic threshold.
Importantly, the HiTOP profile is only one element of a psychiatric evaluation. Clinicians also consider medical comorbidities, stressors, and treatment history to develop case conceptualization. HiTOP contributes to this process a quantified, detailed, and systematic description of psychopathology. Such in-depth assessment may be unnecessary in acute settings, where a singular problem needs rapid intervention. However, detailed understanding is valuable in long-term management of a chronic disorder. HiTOP is particularly useful for prevention, as it thoroughly characterizes subthreshold psychopathology, a potent risk factor not captured by diagnostic manuals. HiTOP can be useful in clinical staging models (Shah et al., 2020), offering detailed characterization of psychopathology across levels of severity.
Overall, the traditional schizophrenia diagnosis is not aligned with the continuous and multidimensional nature of psychopathology. This concept can be effective in acute treatment settings, but a more accurate model would enhance prevention, long-term management, and research. DSM-5 has introduced psychosis symptom severity ratings, and HiTOP fully embraces this approach. The traditional schizophrenia concept offers valuable continuity and can be used in parallel with HiTOP, but we predict that eventually the dimensional approach will make this categorical diagnosis obsolete.
Acknowledgements
This work was supported by the National Institutes of Health (MH110434 to R.K.).
Role of funding
Funding from the National Institute of Mental Health (MH110434) supported collection of data presented in Fig. 1.
Footnotes
Declaration of competing interest
The authors (RK, KJ, WL, ARD, WTC) have no conflicts of interest to disclose.
CRediT authorship contribution statement
All authors contributed to conceptualization and writing of this manuscript. WL performed analyses displayed in Fig. 1.
References
- Achenbach TM, Rescorla LA, 2001. Manual for the ASEBA School-age Forms & Profiles: Child Behavior Checklist for Ages 6-18, Teacher’s Report Form, Youth Self-report: An Integrated System of Multi-informant Assessment. University of Vermont Research Center for Children, Youth, and Families, Burlington, VA. [Google Scholar]
- Bornstein RF, Natoli AP, 2019. Clinical utility of categorical and dimensional perspectives on personality pathology: a meta-analytic review. Personal. Disord. Theory Res. Treat 10, 479–490. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Kotov R, Fochtmann LJ, Carlson GA, Tanenberg-Karant M, Ruggero C, Chang SW, 2011. Diagnostic shifts during the decade following first admission for psychosis. Am. J. Psychiatr 168, 1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero DC, Jonas KG, Li K, Perlman G, Kotov R, 2019. Common taxonomy of traits and symptoms: linking schizophrenia symptoms, schizotypy, and normal personality. Schizophr. Bull 45, 1336–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Simms LJ, Wu KD, Casillas A, 2014. Schedule for Nonadaptive and Adaptive Personality, 2nd Edition (SNAP-2): Manual for Administration, Scoring, and Interpretation. University of Notre Dame, South Bend, IN. [Google Scholar]
- Clark LA, Cuthbert B, Lewis-Fernández R, Narrow WE, Reed GM, 2017. Three approaches to understanding and classifying mental disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s research domain criteria (RDoC). Psychol. Sci. Public Interest 18, 72–145. [DOI] [PubMed] [Google Scholar]
- Debbané M, Eliez S, Badoud D, Conus P, Flückiger R, Schultze-Lutter F, 2015. Developing psychosis and its risk states through the lens of schizotypy. Schizophr. Bull 41, S396–S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docherty AR, Shabalin AA, Adkins DE, Mann F, Krueger RF, Bacanu SA, Campbell A, Hayward C, Porteous DJ, McIntosh AM, Kendler KS, 2020. Molecular genetic risk for psychosis is associated with psychosis risk symptoms in a population-based UK cohort: findings from generation Scotland. Schizophr. Bull 46, 1045–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Rebello TJ, Keeley JW, Bhargava R, Dai Y, Kulygina M, Reed GM, 2018. Do mental health professionals use diagnostic classifications the way we think they do? A global survey. World Psychiatry 17, 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon FM, Yeo RA, Shaff NA, Wertz CJ, Dodd AB, Bustillo JR, Stromberg SF, Lin DS, Abrams S, Liu J, Mayer AR, 2019. A symptom-based continuum of psychosis explains cognitive and real-world functional deficits better than traditional diagnoses. Schizophr. Res 208, 344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam N, McGrath MJ, Viechtbauer W, Kuppens P, 2020. Dimensions over categories: a meta-analysis of taxometric research. Psychol. Med 50, 1418–1432. [DOI] [PubMed] [Google Scholar]
- Jablensky A, 2007. Living in a kraepelinian world: Kraepelin’s impact on modern psychiatry. History of Psychiatry 18 (3), 381–388. [DOI] [PubMed] [Google Scholar]
- Kotov R, Foti D, Li K, Bromet EJ, Hajcak G, Ruggero CJ, 2016. Validating dimensions of psychosis symptomatology: neural correlates and 20-year outcomes. J. Abnorm. Psychol 125, 1103–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Fochtmann L, Li K, Tanenberg-Karant M, Constantino EA, Rubinstein J, Perlman G, Velthorst E, Fett AKJ, Carlson G, Bromet EJ, 2017a. Declining clinical course of psychotic disorders over the two decades following first hospitalization: evidence from the Suffolk county mental health project. Am. J. Psychiatr 174, 1064–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, et al. , 2017b. The hierarchical taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J. Abnorm. Psychol 126, 454–477. [DOI] [PubMed] [Google Scholar]
- Kotov R, Jonas KG, Carpenter WT, Dretsch MN, Eaton NR, Forbes MK, Forbush KT, Hobbs K, Reininghaus U, Slade T, South SC, 2020. Validity and utility of hierarchical taxonomy of psychopathology (HiTOP): IPsychosis superspectrum. World Psychiatry 19, 151–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Cicero DC, Conway CC, DeYoung CG, Eaton NR, Forbes MK, Hallquist MN, Latzman RD, Mullins-Sweatt SN, et al. , 2021. The hierarchical taxonomy of psychopathology (HiTOP): a quantitative nosology based on consensus of evidence. Annu. Rev. Clin. Psychol 17, 83–108. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Kotov R, Watson D, Forbes MK, Eaton NR, Ruggero CJ, Simms LJ, Widiger TA, Achenbach TM, Bach B, Bagby RM, et al. , 2018. Progress in achieving quantitative classification of psychopathology. World Psychiatry 17, 282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legge SE, Cardno AG, Allardyce J, Dennison C, Hubbard L, Pardiñas AF, Richards A, Rees E, Di Florio A, Escott-Price V, Zammit S, 2021. Associations between schizophrenia polygenic liability, symptom dimensions, and cognitive ability in schizophrenia. JAMA Psychiatry 78, 1143–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linscott RJ, Van Os J, 2013. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol. Med 43, 1133–1149. [DOI] [PubMed] [Google Scholar]
- Lorr M, Klett CJ, McNair DM, 1963. Syndromes of Psychosis. Pergamon Press, New York. [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ, 2011. The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychol. Bull 137, 856–879. [DOI] [PubMed] [Google Scholar]
- Martin EA, Jonas KG, Lian W, Foti D, Donaldson KR, Bromet EJ, Kotov R, 2021. Predicting long-term outcomes in first-admission psychosis: does the hierarchical taxonomy of psychopathology aid DSM in prognostication? Schizophr. Bull 47, 1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TV, 1930. The empirical determination of certain syndromes underlying praecox and manic-depressive psychoses. Am. J. Psychiatr 86, 719–738. [Google Scholar]
- Mościcki EK, Clarke DE, Kuramoto SJ, Kraemer HC, Narrow WE, Kupfer DJ, Regier DA, 2013. Testing DSM-5 in routine clinical practice settings: feasibility and clinical utility. Psychiatr. Serv 64, 952–960. [DOI] [PubMed] [Google Scholar]
- Overall JE, Gorham DR, 1962. The brief psychiatric rating scale. Psychol. Rep 10, 799–812. [Google Scholar]
- Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H, 2000. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch. Gen. Psychiatry 57, 1053–1058. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, MacCallum RC, Nicewander WA, 2005. Use of the extreme groups approach: a critical reexamination and new recommendations. Psychol. Methods 10, 178–192. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Clarke DE, Kraemer HC, Kuramoto SJ, Kuhl EA, Kupfer DJ, 2013. DSM-5 field trials in the United States and Canada, part II: test-retest reliability of selected categorical diagnoses. Am. J. Psychiatr 170, 59–70. [DOI] [PubMed] [Google Scholar]
- Reininghaus U, Böhnke JR, Chavez-Baldini U, Gibbons R, Ivleva E, Clementz BA, Pearlson GD, Keshavan MS, Sweeney JA, Tamminga CA, 2019. Transdiagnostic dimensions of psychosis in the bipolar-schizophrenia network on intermediate phenotypes (B-SNIP). World Psychiatry 18, 67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringwald WR, Forbes MK, Wright AG, 2021. Meta-analysis of structural evidence for the hierarchical taxonomy of psychopathology (HiTOP) model. Psychol. Med 1–14. [DOI] [PubMed] [Google Scholar]
- Ruggero CJ, Kotov R, Hopwood CJ, First M, Clark LA, Skodol AE, Mullins-Sweatt SN, Patrick CJ, Bach B, Cicero DC, Docherty A, 2019. Integrating the hierarchical taxonomy of psychopathology (HiTOP) into clinical practice. J. Consult. Clin. Psychol 87, 1069–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah JL, Scott J, McGorry PD, Cross SP, Keshavan MS, Nelson B, Wood SJ, Marwaha S, Yung AR, Scott EM, Öngür D, 2020. Transdiagnostic clinical staging in youth mental health: a first international consensus statement. World Psychiatry 19, 233–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahl EA, Breen G, Forstner AJ, McQuillin A, Ripke S, Trubetskoy V, Mattheisen M, Wang Y, Coleman JR, Gaspar HA, De Leeuw CA, 2019. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat. Genet 51, 793–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittenborn JR, 1951. Symptom patterns in a group of mental hospital patients. J. Consult. Psychol 15, 290–302. [DOI] [PubMed] [Google Scholar]