Abstract
Objective
It is well known that spontaneous non-aneurysmal subarachnoid hemorrhage (SAH), also known as sine materia SAH (smSAH), has usually a better course and prognosis than its aneurysmal counterpart (aSAH). This might depend on different inflammatory mechanisms initiated by bleeding events of different origins. The aim of the present study was to explore the systemic inflammatory response in spontaneous SAH, comparing aSAH and smSAH.
Methods
We performed a prospective observational study over a consecutive series of patients with SAH. For these patients, we collected all clinical data and, furthermore, performed venous blood sampling over six time points to analyze blood cells. We further performed the analysis of lymphocytes and monocytes by means of flow cytometry to quantify common subtypes. Statistical analysis included a t-student test, Chi-square test, multivariate logistic regression, and ROC analysis.
Results
48 patients were included: six (12.5%) with a diagnosis of spontaneous smSAH, and forty-two patients (87.5%) with aSAH. Significant differences on Day 0 were found for neutrophils and a systemic neuro-inflammatory index, namely, systemic inflammatory response index (SIRI). At the ROC analysis, neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and SIRI exhibited satisfactory predictive power on day 0. At the multivariable logistic regression analysis, the combined index (NLR, LMR, SIRI at day 0) yielded an OR of 0.59 (95% CI 0.29–1.21]). LMR at day 0 yielded an OR of 1.25 ([95% CI 0.94–1.68]), NLR at day 0 exhibited an OR of 0.68 ([95% CI 0.42–1.09]), and SIRI at day 0 displayed an OR of 0.31 ([95% CI 0.06–1.49]).
Conclusion
This preliminary study indicated a possible role of some inflammatory indices that point out the importance of innate and adaptive immunity in the etiopathogenetic mechanisms. Drugs modulating these responses could eventually counteract or, at least, reduce secondary damage associated with SAH.
Keywords: SAH, aneurysmal SAH, sine materia SAH, SAH of unknown origin, systemic inflammation, neutrophils, inflammatory indices
Background
Spontaneous subarachnoid hemorrhage (SAH) is associated, in most cases, with the rupture of an intracranial aneurysm, and represents a severe life-threatening event, in both the acute and delayed phases, accounting for 5% of all strokes, with an overall mortality rate of 30–70% and severe neurological impairment in 10–20% of surviving patients.1–3 In some patients (approximately 15–20% of cases), however, no aneurysm or source of hemorrhage can be detected, even after repeated exams, and this scenario is defined as sine materia SAH (smSAH), SAH of unknown origin, non-aneurysmal SAH (naSAH), angiographically negative SAH, or SAH with negative angiographic findings. smSAH represents a highly heterogeneous condition in terms of epidemiology, clinical course, and related clinical and functional outcomes, including complications, hospital stay, and overall prognosis.4 The precise cause of bleeding is yet to be identified, even though several hypotheses about possible sources of bleeding have been formulated, including the rupture of perforating arteries or capillaries, such as the pontine arteries, the presence of microaneurysms, cavernous or arteriovenous malformations, bleeding from the superficial (perimesencephalic/prepontine) or deep venous system (like the basal veins of Rosenthal), or hemorrhage arising from basilar trunk dissections.5,6 Although even in these patients subarachnoid blood is not harmless, and recent studies have shown possible vasospasm, re-bleeding, hydrocephalus, seizure, cognitive impairment, and depression among sequelae,7–9 the prognosis of smSAH patients is much better when compared with aneurysmal SAH (aSAH).10
Given its inherent heterogeneity, the clinical course, and the epidemiology of smSAH are not well characterized in the extant scholarly literature. Indeed, only a few case series11–15 can be utilized to define the risk factors, clinical/neurological and radiographic manifestations, prognosis, and outcomes in smSAH, as well as its etiopathogenesis. For instance, while primary hemorrhage damages the brain parenchyma directly,3 through various cellular and molecular mechanisms and cascades/pathways, also secondary brain injury can occur. Inflammatory events play a major role in the activation and promotion of programmed cell death at the central nervous system level.16 However, while the inflammatory events have been widely studied in aSAH,17 there is a lack of data concerning inflammation and inflammatory markers in naSAH, with a few notable exceptions.18,19 Therefore, the present study was devised, with the aim of comparing the systemic inflammatory response in patients with aSAH and in patients with spontaneous SAH of unknown origin. Patients with aSAH analyzed in the present study belong to a study cohort already described in a previous publication,20 where the inflammatory systemic response in aSAH patients was assessed in relation to vasospasm. Recruitment for this study (including patients with smSAH) occurred contemporaneously with our prior study. Since in aSAH patients, the brain immune inflammatory responses have been shown to correlate with complications, such as early brain injury, delayed cerebral ischemia, and long-term outcomes and sequelae,17 and given the milder course of smSAH, we hypothesized that systemic inflammatory response biomarkers could reflect a stronger inflammatory status affecting the brain vasculature and parenchyma after aSAH and could potentially discriminate between aSAH and smSAH from the onset of the disease (day 0).
Methods
Patients and Methods
Study Design and Outline
The present investigation was designed as a prospective, observational, multicentric pilot study. Its protocol has been in-depth reviewed and fully approved by the Ethics Board of the two hospitals with neurosurgical units that managed patients with spontaneous SAH in the study setting (Genoa, Italy): namely, the Polyclinic Hospital San Martino IRCCS, Genoa, Italy, which acted as the leading institution for this study (24th May 2013, with the registration number 51/13) and E.O. Ospedali Galliera, Genoa (4th March 2013, with the registration number PG 905/13). The study was conducted in accordance with the Helsinki Declaration of 1975 (revised in 1983) and its subsequent amendments.
The management of SAH patients was done according to the European – American Guidelines for the Management of SAH.21,22
At the two study hospitals, in the time period between June 21st 2013 and June 21st 2016, a consecutive series of patients with spontaneous (ie, non-traumatic) SAH with admission CT scans carried out within 24 hours after SAH were recruited, after informed consent. This was signed by the patients themselves whenever possible or by their closest relatives/legal guardians when the patients were unable to sign. Diagnosis of the intracranial aneurysm was performed by means of CT angiography (CTA), or, when CTA was either not clear or negative, or whenever required for treatment purposes, by digital subtraction angiography (DSA). SAH patients with negative DSA study underwent a second DSA study after 4–10 days. In the present study analysis, also patients with spontaneous smSAH were included, differently from our previous publication.20
Six time points were set as follows: day 0, days 3–4, days 6–8, days 10–11, days 13–15, and days 18–21 after aSAH, since i) we aimed to capture both the acute and post-acute phase of the event, and ii) the diagnosis of smSAH requires repeated exams and an accurate radiographic/diagnostic work-up.23 These specific time points were chosen in that approximately two-thirds of aSAH patients develop vasospasm from 3 to 14 days after initial rupture.24,25 At each time-point, blood work included routine exams, and, moreover, an additional sample was collected for further cytometric characterization (see20).
Exclusion criteria were the following: death before days 6–8, re-bleeding, moribund patients at admission, co-existing immunological disorder, severe sepsis, and inadequate flow-cytometry acquisition/characterization. Sine materia spontaneous SAH patients were included in the study and categorized as such only after repeated follow-up studies of negative vessel imaging, which confirmed the absence of an aneurysm. Few patients in not homogenous conditions (such as those with re-bleeding, those with acute severe neurological deterioration, and those with the onset of severe sepsis) would have confounded the picture, requiring a larger sample size to reach an adequate power analysis threshold.
Data collected included sex/gender, age, history of allergy, cigarette smoking, alcohol abuse, family history positive for SAH, previous stroke or cerebrovascular accidents, cardiopathy, dyslipidemia, diabetes mellitus, hypertension, use of statins before and/or during hospitalization, consumption of tranexamic acid before aneurysm occlusion, Glasgow Coma Score (GCS), World Federation of Neurosurgical Societies (WFNS) SAH grading scale, Hunt-Hess and Fisher scores, modality and timing of aneurysm treatment (surgical or endovascular), presence of multiple aneurysms, steroid therapy during hospitalization, troponin rise at admission, and the insurgence of infective complications. Further, variations of neurological status at each time point were annotated as well, and the modified Rankin (mRS) score was marked at the last time point.
The following study methods have been described in more detail in a recent publication from our group,20 to which the reader is kindly referred.
Furthermore, we computed the following inflammatory indexes: i) Neutrophil-to-Lymphocyte ratio (NLR), ii) Lymphocyte-to-Monocyte ratio (LMR), iii) Platelet-to-Monocyte ratio (PMR), iv) systemic inflammation response index or SIRI (Neutrophils × Monocytes/Lymphocytes), and v) systemic immune-inflammation index or SII (Neutrophils × Platelets/Lymphocytes).
Laboratory Methods
Leukocyte phenotyping has been described in a recent publication by our group.20 Peripheral blood mononuclear cells (PBMC) were isolated from human peripheral whole blood by Ficoll-Paque density gradient centrifugation, and the pellet was re-suspended with a dilution of 1×106 cells/mL in Fluorescence-Activated Cell Sorting (FACS) buffer. 100μL suspension was then distributed in 4 tubes:
Tube 1: not stained, containing 100μL of the PBMC suspension.
Tube 2: for CD3 assessment: 100μL of the PBMC suspension, Monoclonal antibodies (3μL CD3 FITC - BD Bioscience 561,806 + 40μL FACS Buffer);
Tube 3: for T and B cell phenotyping; 100μL of the PBMC suspension, Monoclonal antibodies (3μL CD3 FITC + 3μL CD4 PE - BD Bioscience 555,347 + 2μL CD8 PE-Cy7 - BD Bioscience 557,746 + 3μL CD19 PE-Cy5 - BD Bioscience 555,414);
Tube 4: for monocytes (M1, M2) and natural killers (NK) phenotyping: (3μL CD3 FITC + 2μL CD56 PE-Cy7 - BD Bioscience 557,747 + 3μL CD16APC - BD Bioscience 561,248 + 2μL CD14APC-Cy7 - BD Bioscience 561,384 + 3μL HLA-Dr PerCP - BD Bioscience 347,402).
Incubation for staining was carried out at 4°C for 30 minutes and the tubes were subsequently washed with 2mL FACS buffer, spinned at 1500rpm × 5min, dechanted, and re-suspended in 500μL of FACS buffer.
The tubes were analyzed with FACScanto 2 BD USA and with BD FACSdiva v8.1.
Statistical Methods
Prior to statistical processing and analysis, data were visually inspected for the identification of potential outliers, to see which statistical test was the most adequate based on the distribution of data. The normality of data distribution was checked with Shapiro–Wilk’s test. Given the small sample size employed, this test was preferred over other tests, such as the D’Agostino-Pearson omnibus test. Univariate analyses (Student’s t-test or its non-parametric test in case of violation of normality of data distribution and chi-squared test) were used to compare the two groups (aSAH and smSAH) for age and sex/gender distributions, co-morbidities, risk factors for aSAH, clinical status, and radiological scores at presentation, treatment modality, and complications. Given the exploratory nature of the present studies, concerning the different time points, both uncorrected and corrected p-values for multiple comparisons were calculated (with significance thresholds of 0.05 and 0.05/6 (0.008), respectively). Moreover, only for the sake of completeness, formal repeated measures analyses were conducted. Multivariable logistic regression analysis (conducted on those variables significant at the univariate analysis and adjusting for confounding factors such as age and sex/gender) was carried out to shed light on differences in the inflammatory response between aSAH and smSAH patients.
Moreover, receiver operating characteristic (ROC) analysis was conducted to investigate whether cellular immunological parameters could discriminate according to the SAH type (aSAH versus smSAH), based on our initial hypothesis. For this purpose, the area under the curve (AUC) was calculated for those parameters significant in the univariate analysis as predictor variables and SAH type as a classification variable. Furthermore, the Youden’s J index was used to determine the best cut-off point to achieve acceptable sensitivity and specificity levels.
Using the G*Power software (v3.1.9.6, University of Kiel, Germany) for calculating the a priori sample size power, for repeated measurement analysis, assuming an alpha error probability of 0.05, a power of 0.80, and two independent groups (aSAH and smSAH), with 6 different time points, and no information about correlations among the serial measurements,26 expecting a small-to-medium effect size (with f ranging from 0.20 to 0.25) based on the existing literature,10 the overall minimum sample size requested was found to vary between 24 and 36, with the minimum requested number of smSAH patients ranging from 4 to 5, assuming a 15% prevalence rate. Furthermore, post-hoc power analysis of the sample size demonstrated the statistical robustness of our study.
GraphPad Prism Software Mac v7, “Statistical Package for Social Sciences” (SPSS v24 for Windows, IBM, Armonk, NY, USA) and MedCalc Statistical Software version 17.9.7 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2017) were used for statistical analyses. Figures with a p-value less than 0.05 were considered statistically significant.
Results
Between June 21st, 2013, and June 21st 2016, 63 patients affected by spontaneous SAH were recruited with a 100% rate of study participation. For study analysis purposes, 15 of 63 patients (23.8%) have been excluded: 6 patients were moribund at admission (ie, unsalvageable patients), and one patient re-bled, for 6 patients flow-cytometric analysis had not been possible for technical problems, and, finally, 2 patients with aSAH had no cranial window for transcranial Doppler (TCD), nor any instrumental work-up documenting vasospasm. 48 patients have, thus, been included: six patients (12.5%) had a diagnosis of spontaneous smSAH, whereas forty-two patients had aSAH (87.5%).
At admission (see Table 1), the two groups did not statistically differ in sex/gender distribution and age, and there were no differences in the history of cigarette smoking, allergy, hypertension, cardiopathy, dyslipidemia, previous stroke, and family history of aSAH. Also, the mean Fisher score was not significantly different (2.79±1.14 in the aSAH group versus 2.67±0.82 in the SmSAH group, p=0.76), even though the distribution was different, with 14/42 Fisher grade IV patients in the aSAH group and 0 in the SmSAH group. Interestingly, the two patient groups had significantly different neurological scores at presentation: the mean GCS score was 14±2.6 in the aSAH group and 15±0.5 in the SmSAH group (p=0.0425), WFNS was 1.93±1.18 in the aSAH group and 1.33±0.516 in the smSAH group (p=0.0015). However, the mean Hunt Hess scale was not significantly different between these groups.
Table 1.
Characteristics of the Patients Included in the Study and of Treatment Modality (Significance Was Assessed with Chi-Squared Test, Where Not Specified or the Two-Tailed t-Test or the Mann Whitney Test)
| aSAH (42 Pts) | Sine Materia SAH (6 Pts) | P value | |
|---|---|---|---|
| Gender: M;F | 13; 29 | 3;3 | 0.35 |
| Age (mean, SD) | 58.26± 15.07 | 55.5 ± 15.40 | t-test unpaired with Welch correction, 2 tails 0.695 |
| Allergy | 7/41 | 2/6 | 0.344 |
| History of smoking | 22/39 | 3/6 | 0.77 |
| Hypertension | 24/42 | 2/6 | 0.22 |
| Cardiopathy | 2/42 | 1/5 | 0.26 |
| Previous stroke | 3/42 | 1/6 | 0.5 |
| Dyslipidemia | 22/36 | 4/6 | 0.8 |
| Family history for SAH | 4/40 | 0/6 | 0.42 |
| Fisher scale (mean, SD) | 2.79± 1.14 | 2.67 ± 0.82 | t-test unpaired with Welch correction, 2 tails 0.76 |
| I | 9 | 1 | |
| II | 5 | 0 | |
| III | 14 | 5 | |
| IV | 14 | 0 | |
| GCS (mean, SD) | 14± 2.6 | 15 ± 0.5 | t-test unpaired with Welch correction, 2 tails 0.0425(*) |
| WFNS (mean, SD) | 1.93 ± 1.18 | 1.33± 0.516 | t-test unpaired with Welch correction, 2 tails 0.0015(**) |
| I | 21 | 4 | |
| II | 11 | 2 | |
| III | 3 | 0 | |
| IV | 6 | 0 | |
| V | 1 | 0 | |
| Hunt Hess (mean, SD) | 2.21± 1.14 | 1.83 ± 0.41 | t-test unpaired with Welch correction, 2 tails 0.132 |
| I | 12 | 1 | |
| II | 18 | 5 | |
| III | 5 | 0 | |
| IV | 5 | 0 | |
| V | 2 | 0 | |
| Treatment | |||
| Surgical/endovascular | 8/ 34 | 0/0 | Not applicable |
| Haematoma evacuation | 5/42 | 0/6 | 0.37 |
| External ventricular drainage | 15/41 | 0/6 | 0.0726 |
| Tranex before treatment | 15/42 | 0/6 | 0.0775 |
| Statins before SAH | 3/41 | 0/6 | 0.494 |
| Statins after SAH | 5/42 | 0/6 | 0.372 |
| Steroids | 23/42 | 0/6 | 0.012 |
| Infection | 19/42 | 2/6 | 0.582 |
| Positive blood culture | 5/42 | 1/6 | 0.742 |
| Vasospasm | 21/42 | 3/6 | >0.99 |
| Ischemia (CT findings) | 15/42 | 0/6 | 0.0775 |
| Outcome as mRS | Mann Whitney test p=0.0022 (**) | ||
| 0 | 10/42 | 6/6 | |
| 1 | 9/42 | 0/6 | |
| 2 | 3/42 | 0/6 | |
| 3 | 1/42 | 0/6 | |
| 4 | 11/42 | 0/6 | |
| 5 | 7/42 | 0/6 | |
| 6 | 1/42 | 0/6 |
As it could be expected, the mRS score registered at the last study timepoint was significantly different (p=0.0022), with all smSAH patients having an mRS score of 0.
While none of our smSAH patients required any surgical treatment, all aSAH patients had a procedure for aneurysm occlusion (8 surgical and 34 endovascular), in addition in 5 patients, a hematoma associated with aSAH had to be surgically evacuated and in 15 patients external ventricular drainage has been positioned for acute hydrocephalus (Table 1).
The analysis of the administration of specific drugs intended as ever administered or not (tranexamic acid before aneurysm occlusion rather than steroids during hospitalization or statins before and/or after hospitalization) did never reach statistical significance between the two groups (Table 1). More in detail, the blood sampling on day 0 was performed at arrival after the CT scan and before any possible administration of steroids, tranexamic acid, or statins. This is because smSAH patients were initially treated as SAH patients until they received a diagnosis of smSAH, after repeated examinations and an intense radiographic/diagnostic work-up.
Concerning complications during the observed timeframe (days 0–21 after SAH), also the incidence of any infection (eg, pneumonia, or urinary tract infection) or positive blood culture was recorded and did not reach a statistically significant difference between the two groups.
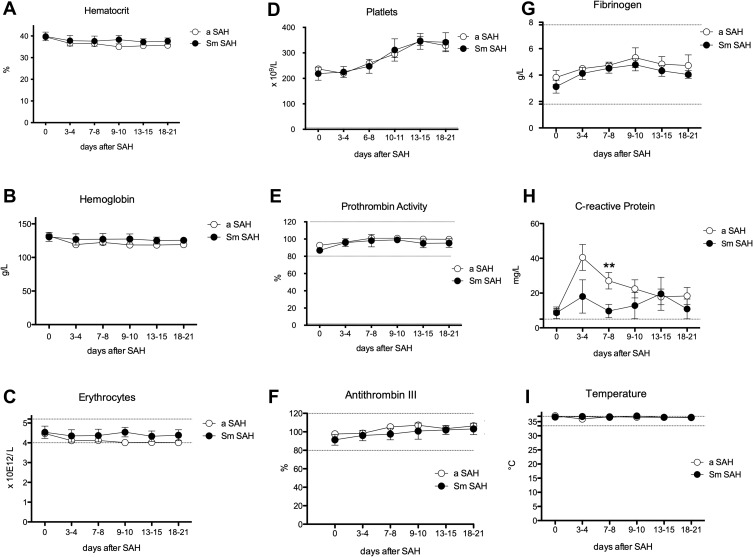
No significant differences could be found in terms of hematocrit, hemoglobin, erythrocytes, platelets, prothrombin activity, antithrombin III, fibrinogen, and temperature (Figure 1, Table 2). Of note, C-reactive protein (CRP) was significantly higher in the aSAH patient group on days 7–8: 27.10±4.72 mg/L (N=40) versus 9.68±3.85 mg/L (N=5) in the smSAH group, p=0.0097 (Figure 1).
Figure 1.
Erythrocytes, platelets, and inflammatory markers over time after spontaneous SAH. (A) Hematocrit; (B) Hemoglobin (C) Erythrocytes; (D) Platelets; (E) Prothrombin activity; (F) Antithrombin III; (G) Fibrinogen; (H) C-reactive protein; (I) Temperature. Graphs showing mean values of patients, 48 patients at the 6 time points defined as days after SAH. The vertical bars show mean and standard error. Patients with aneurysm-related SAH (aSAH) n=42, in white circles and patients with sine materia SAH, also called SAH of unknown origin (Sm SAH) n=6, in black circles. The stars indicate statistical significance at the unpaired two-tailed t-test made at each time point. Small dotted horizontal lines indicate in the graph the normal range reference values where available and/or useful.
Table 2.
Values at Day 0 Followed Over Time in aSAH Amd Sm Patients, Respectively. Mean Values and SD are Presented and results of Univariate Analysis (Two-Tailed tTest)
| Measures at Day 0 | aSAH (42 Pts) | smSAH (6 Pts) | p value |
|---|---|---|---|
| Haemoglobin (g/L) | 132.6 (15.6) | 130.6 (4.89) | 0.838 |
| Haematocrit (%) | 39.6 (4.1) | 39.8 (3.8) | 0.926 |
| Eritrocytes (x109/L) | 4.47 (0.56) | 4.53 (0.76) | 0.855 |
| Platelets (x109/L) | 237.26 (54.72) | 218.5 (62.96) | 0.514 |
| Prothrombin Activity (%) | 92.71 (10.57) | 86.83 (7.25) | 0.121 |
| Antithrombin III (%) | 97.63(13.24) | 91.33 (14.08) | 0.342 |
| Fibrinogen (g/L) | 3.82 (3.2) | 3.13 (1.10) | 0.346 |
| C Reactive Protein (mg/L) | 9.36 (11.05) | 10.15 (7.7) | 0.861 |
| Temperature °C | 36.75 (0.39) | 36.63 (0.27) | 0.392 |
| Leukocytes (x109/L) | 13.18 (5.61) | 10.41 (2.77) | 0.079 |
| Neutrophils (x109/L) | 10.97 (5.48) | 7.2 (3.4) | 0.045 |
| Neutrophils (%) | 83.29 (9.29) | 77.03 (13.28) | 0.419 |
| Lymphocytes (x109/L) | 1.39 (0.93) | 2.03(1.45) | 0.448 |
| Lymphocytes (%) | 10.99 (7.78) | 17.7(9.45) | 0.253 |
| Monocytes (x109/L) | 0.62 (0.43) | 0.45 (0.40) | 0.481 |
| Monocytes (%) | 4.37 (2.61) | 4.33 (3.23) | 0.979 |
| Eosinophils (x109/L) | 0.02 (0.04) | 0.05 (0.1) | 0.630 |
| Eosinophils (%) | 0.29 (0.45) | 0.53(0.85) | 0.619 |
| Basophils (x109/L) | 0.036 (0.049) | 0.025 (0.05) | 0.693 |
| Basophils (%) | 0.32 (0.33) | 0.43 (0.33) | 0.584 |
| Lymphocytes CD4 (x109/L) | 0.41 (0.33) | 0.67 (0.70) | 0.510 |
| Lymphocytes CD4 (%) | 31.55 (12.86) | 30.38 (16.98) | 0.878 |
| Lymphocytes CD8 | 0.20 (0.21) | 0.32 (0.34) | 0.556 |
| Lymphocytes CD8% | 13.64 (7.18) | 12.78 (7.02) | 0.791 |
| Lymphocytes B | 0.17 (0.19) | 0.20 (0.12) | 0.693 |
| Lymphocytes B % | 12.38 (7.57) | 9.73 (4.68) | 0.277 |
| NK Lymphocytes (x109/L) | 0.48 (0.48) | 0.77 (0.42) | 0.272 |
| NK Lymphocytes % | 35.61 (18.04) | 41.77 (27.42) | 0.616 |
| CD14++ CD16- DR+ Monocytes (x109/L) | 0.47 (0.40) | 0.38 (0.38) | 0.681 |
| CD14++ CD16- DR+ Monocytes (%) | 78.73 (15.16) | 73.38 (13.49) | 0.407 |
| CD14+ CD16+ DR+ Monocytes (x109/L) | 0.05 (0.04) | 0.04 (0.02) | 0.604 |
| CD14+ CD16+ DR+ Monocytes (%) | 13.34 (11.18) | 12.02 (10.05) | 0.780 |
| Neutrophil-to- Lymphocyte ratio | 10.99 (7.21) | 5.15 (5.71) | 0.130 |
| Platelet-to-Lymphocyte ratio | 245.46 (161.95) | 158.96 (87.06) | 0.303 |
| Lymphocyte-to-Monocyte ratio | 3.15 (2.88) | 6.05 (3.24) | 0.066 |
| Systemic Inflammation Response Index | 7.15 (8.26) | 1.41 (0.87) | 0.048 |
| Systemic Immune-Inflammation Index | 2437.55 (1983.30) | 1384.92 (770.48) | 0.280 |
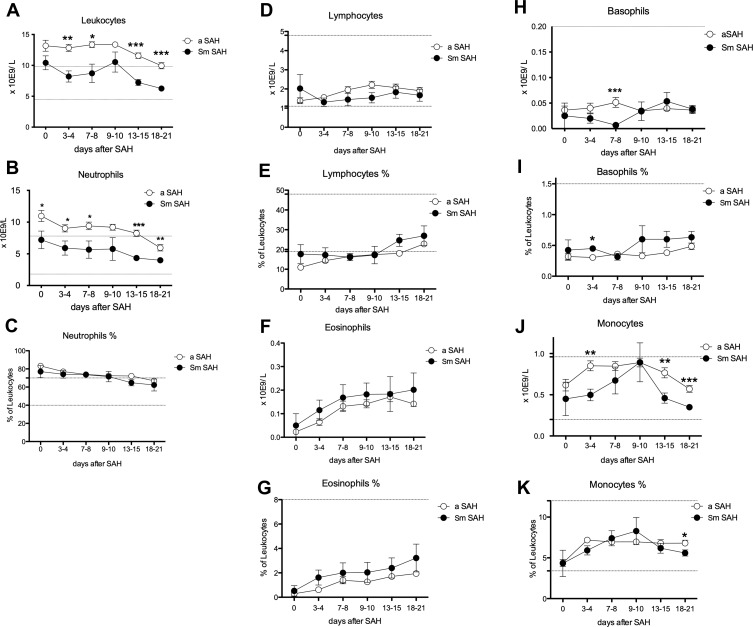
Of the other analyzed parameters, a trend towards significant differences on Day 0 was found for Leukocytes for aSAH versus smSAH, 13.18±5.61 × 109/L (N=40) versus 10.41±2.77 × 109/L (N=6), p 0.079. Of all measures, only Leukocytes presented significant differences over several time points (days 3–4, days 7–8, days 13–15, and days 18-21) as shown by the two-way ANOVA and Bonferroni Post-hoc test (Figure 2A). In the aSAH group at each time point Leukocytes were above the upper limit, while in the smSAH patient group mean values were within the range of normality. However, these findings could not be confirmed in the repeated measures analysis (F=0.16, p=0.689).
Figure 2.
Circulating Leukocyte subpopulations over time after spontaneous SAH. (A) Leukocytes; (B) Neutrophils; (C) % of Neutrophils (D) Lymphocytes; (E) % of Lymphocytes; (F) Eosinophils; (G) % of Eosinophils; (H) Basophils; (I) % of Basophils; (J) Monocytes; (K) % of Monocytes. Graphs showing mean values of patients, 48 patients at the 6 time points defined as days after SAH. The vertical bars show mean and standard error. Patients with aneurysm-related SAH (aSAH) n=42, in white circles and patients with sine materia SAH, also called SAH of unknown origin (Sm SAH) n=6, in black circles. The stars indicate statistical significance at the unpaired two-tailed t-test made at each time point, * with p-value <0.05, ** with p-value <0.01, and *** with p-value <0.001. Small dotted horizontal lines indicate in the graph the normal range reference values where available and/or useful.
Neutrophils were higher in the aSAH group on day 0, 10.97±5.48 × 109/L (N=39) versus 7.20±3.40 × 109/L (N=6), p= 0.045, and Neutrophils were significantly higher on almost all time points in aSAH patients (as shown by the t-test at each time point, but not confirmed by the two-way ANOVA and by the repeated measures analysis) (Figure 2).
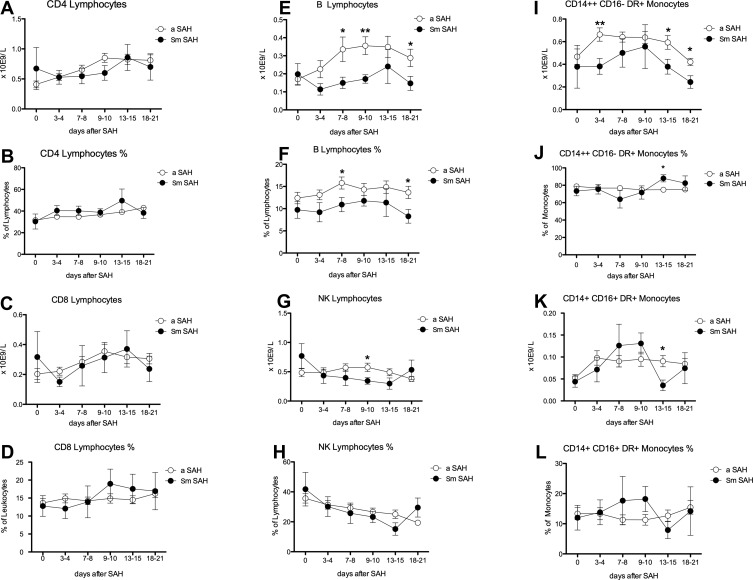
Lymphocytes did not show different levels or trends between the two groups. Nevertheless, we detected higher levels of Basophils on days 7–8 in the aSAH group (Figure 2), but a higher percentage of Basophils in the smSAH group on days 3–4 (Figure 2). B Lymphocytes raised more in aSAH patients from time point 3–4 days with significant differences on days 7–8, 9–10, and 18–21 (Figure 3). Also, the B Lymphocyte % was higher in aSAH patients on days 7–8 and 18-21 (Figure 3). Again, in the aSAH patient group, NK Lymphocytes were higher on days 9–10 (Figure 3).
Figure 3.
Blood lymphocyte subsets and monocyte counts after spontaneous SAH. (A) CD4 positive Lymphocytes; (B) % of CD4 positive Lymphocytes; (C) CD8 positive Lymphocytes; (D) % of CD8 positive Lymphocytes; (E) B Lymphocytes; (F) % of B Lymphocytes; (G) Natural Killer (NK) Lymphocytes; (H) % of Natural Killer (NK) Lymphocytes; (I) CD CD14++ CD16- of DR+ Monocytes; (J) % of CD14++ CD16- Monocytes. (K) 14+ CD16+ of DR+ Monocytes; (L) % of CD14+ CD16+ of DR+ Monocytes. Graphs showing mean values of patients, 48 patients at the 6 time points defined as days after SAH. The vertical bars show mean and standard error. Patients with aneurysm-related SAH (aSAH) n=42, in white circles and patients with sine materia SAH, also called SAH of unknown origin (Sm SAH) n=6, in black circles. The stars indicate statistical significance at the unpaired two-tailed t-test made at each time point, * with p-value <0.05 and ** with p-value <0.01. Small dotted horizontal lines indicate in the graph the normal range reference values where available and/or useful.
Monocytes were higher in the aSAH patient group on days 3–4, 13–15, and 18–21 (Figure 2). A slightly but significantly higher percentage of Monocytes was detected on days 18–21 in these patients (Figure 2). Of Monocytes subgroups, CD14++ CD16- DR+ monocytes were especially high in aSAH on days 3–4, and on days 13–15 and 18–21 (Figure 3). Nevertheless, smSAH patients showed a greater percentage of CD14++ CD16- DR+ Monocytes on days 13–15 (Figure 3). CD14+CD16+ DR+ Monocytes were higher again in aSAH patients on 13–15 days (Figure 3).
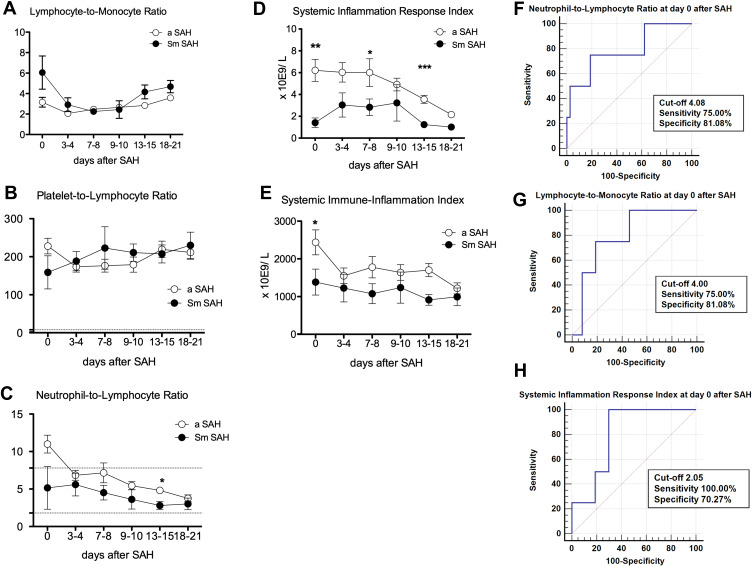
Figure 4.
Inflammatory indices over time after spontaneous SAH and ROC curves analysis at day 0. (A) Lymphocytes-to-Monocyte Ratio; (B) Platelet-to-Lymphocyte Ratio; (C) Neutrophil-to-Lymphocyte Ratio; (D) Systemic Inflammation Response Index; (E) Systemic Immune-Inflammation Index; (F) Neutrophil-to-Lymphocyte Ratio; (G) Lymphocyte-to-Monocyte Ratio; (H) Systemic Inflammation Response Index. Graphs (A-E) showing mean values of patients, 48 patients at the 6 time points defined as days after SAH. The vertical bars show mean and standard error. Patients with aneurysm-related SAH (aSAH) n=42, in white circles and patients with sine materia SAH, also called SAH of unknown origin (Sm SAH) n=6, in black circles. The stars indicate statistical significance at the unpaired two-tailed t-test made at each time point, * with p-value <0.05, ** with p-value <0.01, and *** with p-value <0.001. Small dotted horizontal lines indicate in the graph the normal range reference values where available and/or useful.
In terms of systemic neuro-inflammatory markers (Figure 4), we found differences for NLR, on days 13–15, whereas no differences could be found for PLR and LMR. SIRI was significantly different between the two groups on day 0, days 7–8, and days 13–15. At the ROC analysis, NLR, LMR, and SIRI exhibited satisfactory predictive power on day 0.
In the multivariable logistic regression analysis (Table 3), the combined index (NLR, LMR, and SIRI on day 0) yielded an OR of 0.59 ([95% CI 0.29–1.21], p=0.1472), whereas for WFNS and GCS ORs of 0.10 ([95% CI 0.00–2.98], p=0.1808) and of 0.43 ([95% CI 0.11–1.75], p=0.2393) were computed, respectively. LMR at day 0 yielded an OR of 1.25 ([95% CI 0.94–1.68], p=0.1274), NLR on day 0 exhibited an OR of 0.68 ([95% CI 0.42–1.09], p=0.1096), and SIRI on day 0 displayed an OR of 0.31 ([95% CI 0.06–1.49], p=0.1441).
Table 3.
Multivariable Logistic Regression (Best Model Shown)
| Variable | Coefficient | Std. Error | Odds Ratio | 95% CI | p-value |
|---|---|---|---|---|---|
| Combined index (NLR, LMR, SIRI) | −0.53 | 0.37 | 0.59 | 0.29 to 1.21 | 0.1472 |
| Age | 0.01 | 0.05 | 1.01 | 0.92 to 1.12 | 0.7852 |
| Sex | −0.42 | 1.32 | 0.66 | 0.05 to 8.75 | 0.7517 |
| WFNS | −2.35 | 1.75 | 0.10 | 0.00 to 2.98 | 0.1808 |
| GCS | −0.84 | 0.72 | 0.43 | 0.11 to 1.75 | 0.2393 |
| Constant | 15.37 | 12.94 | 0.2349 |
Finally, no statistically significant correlations were found between WFNS and Fisher (correlation coefficient 0.27, p=0.0692) and between GCS and Fisher (correlation coefficient −0.25, p=0.0812).
Discussion
In the present investigation, statistically significant differences on Day 0 between smSAH and aSAH patients were found for neutrophils, and one systemic inflammatory response indicator. The aim of our study was to identify predictors of smSAH versus aSAH in terms of systemic inflammatory response on day 0, furthermore, we also wanted to explore differences over several time points in the systemic inflammatory response after SAH and its temporal trend. Besides assessing the predictive power of potential biomarkers, our study aimed to assess whether there were differences in inflammatory nature to enrich pathophysiological hypotheses on the different nature of bleeding: eg, arterial versus venous blood in aSAH versus smSAH, respectively.27 In general, there are a few studies on this issue. Moreover, most of the available studies are principally interested in prognosis and in delayed ischemic injury associated with neuroinflammation.
Concerning the epidemiology of smSAH, despite the relatively small sample size utilized in the present study, our figures well reflect those reported in larger studies. For instance, in a case series from Finland consisting of 996 patients with spontaneous SAH, 86 (8.6%) were of unknown origin.28 In a Danish study on diagnostic follow-up for non-aneurysmal SAH, out of 639 patients with spontaneous SAH, 74 (11%) were non-aneurysmal.29 In a German study on 1068 patients with spontaneous SAH diagnosed with CT scan, 179 (16.7%) were sine materia (among them, 47 (26.3%) were perimesencephalic and 132 (73.7%) were non–perimesencephalic).30 Finally, in the “Barrow Ruptured Aneurysm Trial” (BRAT) database, out of 472 enrolled patients, 57 patients received a diagnosis of smSAH (11.9%).31 These percentages are well comparable with the one found in our study, where non-aneurysmal spontaneous SAH occurred in 9.5% of the initial sample (6 out of 63 eligible patients) and in 12.5% of the final sample (6 out of 48 patients).
Concerning the immune response to SAH, in a study,18 no differences in terms of leukocyte count could be found among three patient groups, namely, those with perimesencephalic and non-perimesencephalic smSAH, those with aSAH without and those complicated with cerebral vasospasm. The authors found that patients with smSAH had a more benign illness and a better prognosis compared with aSAH patients and this had been linked to lower levels of the systemic inflammatory stress response. These findings were replicated in another investigation by the same group.19
In terms of inflammatory indices, we found that NLR at time point 0 with a cut-off value of 4.1 could distinguish between aSAH and smSAH. In the existing scholarly literature, NLR is a peripheral biomarker that has been found to be able to predict a number of unfavorable outcomes in SAH patients, including rebleeding, delayed cerebral ischemia, post-operative infections, and poor functional outcomes, which impose neurological dysfunctions and a high burden of morbidity and disability in survivors.32 Optimal cut-off values ranged from 4 to 12.5, depending on the specific type of SAH, its physiopathology, and the outcome under study. Bolton et al33 performed a single-center, retrospective study and found that, in a sample of 96 aSAH patients, a combination of NLR, PLR and CRP (namely, NLR on day 2, PLR on days 1 and 2, and CRP on days 3, 4 and 5) could be predictive of the insurgence of delayed cerebral ischemia. Similarly, Wu et al34 found that NLR>11.47 predicted the occurrence of delayed cerebral ischemia in SAH patients. In another retrospective study, Dowlati et al35 found that, in a sample of 418 aSAH patients, NLR >8.0 (OR 3.19 [95% CI 1.40–7.62]) was independently associated with refractory cerebral vasospasm. Chang et al36 found that an NLR value >6.48 was predictive of poor functional outcome (OR 1.71 [95% CI 1.07–2.74]), and Giede-Jeppe et al37 computed an NLR threshold of 7.05 to be associated with unfavorable functional outcomes. Jamali et al38 found that NLR ≥ 12.5 at admission correlated with mortality in aSAH patients. Of note, Zhang et al39 found that NLR could distinguish between SAH and non-traumatic acute headache, with a threshold value of 4, a sensitivity and a specificity of 98.6% and 64.8%, respectively, which are in line with our values.
We found that PLR at time point 3 could differentiate between aSAH and smSAH. The optimal cut-off was 152.5, while Zhang et al39 computed a threshold of 175 to separate patients with SAH from those with a non-traumatic acute headache with a specificity of 92.96%, and a sensitivity of 44.44%. We could not find other similar, comparable studies.
We computed an LMR cut-off value of 4 at time point 0 to distinguish between SAH and smSAH. In perfect line with our findings, Yi et al40 computed an LMR value of 4.2 (OR 1.74 [95% CI 1.48–2.98]) as predictor of outcomes in SAH patients.
We also found that a SIRI >2 at time point 2 could discriminate between aSAH and smSAH. Yun et al41 computed a SIRI value of 3.2 as predictive of unfavorable outcomes in aSAH patients (OR 1.82 [95% CI 1.46–3.24]). However, differently from this study, we could not find SII to have predictive power. Li et al42 found a cut-off value for SII of 3.63 correlated with cerebral vasospasm in SAH patients.
These findings, taken altogether, underline that, in general, smSAH has a prognosis that matches the best aSAH cases and that can be predicted by systemic inflammatory response biomarkers.
Strengths and Limitations of the Study
This study has several strengths, including its novelty. To the best of our knowledge, it is, indeed, one of the very few investigations to systematically explore the systemic immune response in smSAH, for which, in general, a relatively limited amount of (epidemiological, clinical, and physiopathological) information is available.
However, the present investigation is not without any limitations, that should be properly acknowledged. Given the heterogeneity underlying the “complex phenotype” of smSAH, this study should be considered as a pilot study and all findings are just preliminary and exploratory, warranting further research and external validation of our predictive model. As such, the meaning of “predictive” inflammatory response biomarkers should be verified on larger scales, stratifying according to perimesencephalic and non-perimesencephalic SAH and, eventually, to other clinical, neurological, and radiographic/diagnostic features, in order to see if and how systemic immune response differs among these sub-groups. Moreover, future studies should conduct chemokine and cytokine analysis, which might help understand the specific processes underlying the response to SAH in aSAH and smSAH patients.
Conclusions
To summarize, neuroinflammatory biomarkers, including new ones such as NLR, LMR, and SIRI, can convey precious information about innate and adaptive immunity and can suggest new targets for effective neuroprotective treatments.43 In particular, the components of innate immunity seem to play a major role in the pathogenesis of SAH, with various phenotypes being associated with clinical prognosis and outcomes.25,44 SAH induces an early intracerebral infiltration and peripheral activation of innate immunity,45 as corroborated by clinical observations and animal studies. Future studies could further explore the role of innate immune cells in SAH and discover potentially druggable pathways, opening the way for new pharmacological compounds and molecules.46 Probably, differences in innate systemic inflammatory response account for differences in neurological status both in the early phase as well as for different outcomes and possibly different levels of secondary brain injury. Transposed to our comparison between SAH of unknown origin and aSAH, this could account for the differences in severity and outcome.
Funding Statement
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this work was supported by a young investigator award to S.B. by the Umberto Veronesi Foundation (nonprofit organization) and a post-doctoral fellowship for the years 2013–2014 to S. B. for her project. The authors are indebted to Finsea Group - Italy, for a generous-free donation in support to the present study to the Department of Neurosurgery, San Martino Hospital for the present project (used as contribution for the acquirement of part of the laboratory reagents).
Ethical Approval
The protocol for this prospective, observational, multicentric study was approved on 24th May 2013, with the registration number 51/13 by the Ethical Committee of the Polyclinic Hospital San Martino IRCCS, Genoa, Italy and by the Ethical Committee of the E.O. Ospedali Galliera on 4th March 2013 with the registration number PG 905/13.
Informed Consent
Informed consent was signed by the patient himself/herself whenever possible or by his/her closest relative where the patient was unable to sign.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Hop JW, Rinkel GJ, Algra A, van Gijn J. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke. 1997;28(3):660–664. doi: 10.1161/01.STR.28.3.660 [DOI] [PubMed] [Google Scholar]
- 2.Mayberg MR. Cerebral vasospasm. Neurosurg Clin N Am. 1998;9(3):615–627. doi: 10.1016/S1042-3680(18)30256-0 [DOI] [PubMed] [Google Scholar]
- 3.Sweeney K, Silver N, Javadpour M. Subarachnoid haemorrhage (spontaneous aneurysmal). BMJ Clin Evid. 2016;2016:548. [PMC free article] [PubMed] [Google Scholar]
- 4.Alhoobi M, Abu-Qadous F, Khan M, et al. Ten Years’ Experiences in the Treatment of Nonaneurysmal Subarachnoid Hemorrhage: a Retrospective Analysis of Outcome Parameters in a Single-Center Study. Asian J Neurosurg. 2020;15(2):315–321. doi: 10.4103/ajns.AJNS_315_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanjilal S, Mehrotra A, Singh V, et al. Non-aneurysmal subarachnoid hemorrhage: is the deep venous system the hidden culprit? Acta Neurochir. 2022;164(7):1827–1835. doi: 10.1007/s00701-022-05222-w [DOI] [PubMed] [Google Scholar]
- 6.Boswell S, Thorell W, Gogela S, Lyden E, Surdell D. Angiogram-negative subarachnoid hemorrhage: outcomes data and review of the literature. J Stroke Cerebrovasc Dis. 2013;22(6):750–757. doi: 10.1016/j.jstrokecerebrovasdis.2012.02.001 [DOI] [PubMed] [Google Scholar]
- 7.Burke T, Hughes S, Carr A, Javadpour M, Pender N, Systematic A. Review of Cognitive Outcomes in Angiographically Negative Subarachnoid Haemorrhage. Neuropsychol Rev. 2018;28(4):453–469. doi: 10.1007/s11065-018-9389-1 [DOI] [PubMed] [Google Scholar]
- 8.Germano A, Caruso G, Caffo M, et al. Does subarachnoid blood extravasation per se induce long-term neuropsychological and cognitive alterations? Acta Neurochir. 1998;140(8):805–811. doi: 10.1007/s007010050182 [DOI] [PubMed] [Google Scholar]
- 9.Mohan M, Islim AI, Rasul FT, et al. Subarachnoid haemorrhage with negative initial neurovascular imaging: a systematic review and meta-analysis. Acta Neurochir. 2019;161(10):2013–2026. doi: 10.1007/s00701-019-04025-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang MD, Fu QH, Song MJ, Ma WB, Zhang JH, Wang ZX. Novel Subgroups in Subarachnoid Hemorrhage and Their Association With Outcomes-A Systematic Review and Meta-Regression. Front Aging Neurosci. 2020;12:573454. doi: 10.3389/fnagi.2020.573454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hui FK, Tumialan LM, Tanaka T, Cawley CM, Zhang YJ. Clinical differences between angiographically negative, diffuse subarachnoid hemorrhage and perimesencephalic subarachnoid hemorrhage. Neurocrit Care. 2009;11(1):64–70. doi: 10.1007/s12028-009-9203-2 [DOI] [PubMed] [Google Scholar]
- 12.Beseoglu K, Pannes S, Steiger HJ, Hanggi D. Long-term outcome and quality of life after nonaneurysmal subarachnoid hemorrhage. Acta Neurochir. 2010;152(3):409–416. doi: 10.1007/s00701-009-0518-8 [DOI] [PubMed] [Google Scholar]
- 13.Renou P, Tourdias T, Fleury O, Debruxelles S, Rouanet F, Sibon I. Atraumatic nonaneurysmal sulcal subarachnoid hemorrhages: a diagnostic workup based on a case series. Cerebrovasc Dis. 2012;34(2):147–152. doi: 10.1159/000339685 [DOI] [PubMed] [Google Scholar]
- 14.Kumar S, Goddeau RP, Selim MH, et al. Atraumatic convexal subarachnoid hemorrhage: clinical presentation, imaging patterns, and etiologies. Neurology. 2010;74(11):893–899. doi: 10.1212/WNL.0b013e3181d55efa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konczalla J, Platz J, Schuss P, Vatter H, Seifert V, Guresir E. Non-aneurysmal non-traumatic subarachnoid hemorrhage: patient characteristics, clinical outcome and prognostic factors based on a single-center experience in 125 patients. BMC Neurol. 2014;14:140. doi: 10.1186/1471-2377-14-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schneider UC, Xu R, Vajkoczy P. Inflammatory Events Following Subarachnoid Hemorrhage (SAH). Curr Neuropharmacol. 2018;16(9):1385–1395. doi: 10.2174/1570159X16666180412110919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeyu Z, Yuanjian F, Cameron L, Sheng C. The role of immune inflammation in aneurysmal subarachnoid hemorrhage. Exp Neurol. 2021;336:113535. doi: 10.1016/j.expneurol.2020.113535 [DOI] [PubMed] [Google Scholar]
- 18.Muroi C, Bellut D, Coluccia D, Mink S, Fujioka M, Keller E. Systemic interleukin-6 concentrations in patients with perimesencephalic non-aneurysmal subarachnoid hemorrhage. J Clin Neurosci. 2011;18(12):1626–1629. doi: 10.1016/j.jocn.2011.03.022 [DOI] [PubMed] [Google Scholar]
- 19.Muroi C, Seule M, Sikorski C, Dent W, Keller E. Systemic interleukin-6 levels reflect illness course and prognosis of patients with spontaneous nonaneurysmal subarachnoid hemorrhage. Acta Neurochir Suppl. 2013;115:77–80. doi: 10.1007/978-3-7091-1192-5_17 [DOI] [PubMed] [Google Scholar]
- 20.Bacigaluppi S, Ivaldi F, Bragazzi NL, et al. An Early Increase of Blood Leukocyte Subsets in Aneurysmal Subarachnoid Hemorrhage Is Predictive of Vasospasm. Front Neurol. 2020;11:587039. doi: 10.3389/fneur.2020.587039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43(6):1711–1737. doi: 10.1161/STR.0b013e3182587839 [DOI] [PubMed] [Google Scholar]
- 22.Steiner T, Juvela S, Unterberg A, et al. European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 2013;35(2):93–112. doi: 10.1159/000346087 [DOI] [PubMed] [Google Scholar]
- 23.Marcolini E, Hine J. Approach to the Diagnosis and Management of Subarachnoid Hemorrhage. West J Emerg Med. 2019;20(2):203–211. doi: 10.5811/westjem.2019.1.37352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dorsch N. A clinical review of cerebral vasospasm and delayed ischaemia following aneurysm rupture. Acta Neurochir Suppl. 2011;110(Pt 1):5–6. doi: 10.1007/978-3-7091-0353-1_1 [DOI] [PubMed] [Google Scholar]
- 25.Roa JA, Sarkar D, Zanaty M, et al. Preliminary results in the analysis of the immune response after aneurysmal subarachnoid hemorrhage. Sci Rep. 2020;10(1):11809. doi: 10.1038/s41598-020-68861-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang H. Sample size determination and power analysis using the G*Power software. J Educ Eval Health Prof. 2021;18:17. doi: 10.3352/jeehp.2021.18.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Schaaf IC, Velthuis BK, Gouw A, Rinkel GJ. Venous drainage in perimesencephalic hemorrhage. Stroke. 2004;35(7):1614–1618. doi: 10.1161/01.STR.0000131657.08655.ce [DOI] [PubMed] [Google Scholar]
- 28.Ronkainen A, Hernesniemi J. Subarachnoid haemorrhage of unknown aetiology. Acta Neurochir. 1992;119(1–4):29–34. doi: 10.1007/BF01541778 [DOI] [PubMed] [Google Scholar]
- 29.Bashir A, Mikkelsen R, Sorensen L, Sunde N. Non-aneurysmal subarachnoid hemorrhage: when is a second angiography indicated? Neuroradiol J. 2018;31(3):244–252. doi: 10.1177/1971400917743100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maslehaty H, Petridis AK, Barth H, Mehdorn HM. Diagnostic value of magnetic resonance imaging in perimesencephalic and nonperimesencephalic subarachnoid hemorrhage of unknown origin. J Neurosurg. 2011;114(4):1003–1007. doi: 10.3171/2010.6.JNS10310 [DOI] [PubMed] [Google Scholar]
- 31.Elhadi AM, Zabramski JM, Almefty KK, et al. Spontaneous subarachnoid hemorrhage of unknown origin: hospital course and long-term clinical and angiographic follow-up. J Neurosurg. 2015;122(3):663–670. doi: 10.3171/2014.10.JNS14175 [DOI] [PubMed] [Google Scholar]
- 32.Cai L, Zeng H, Tan X, Wu X, Qian C, Chen G. The Role of the Blood Neutrophil-to-Lymphocyte Ratio in Aneurysmal Subarachnoid Hemorrhage. Front Neurol. 2021;12:671098. doi: 10.3389/fneur.2021.671098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bolton WS, Gharial PK, Akhunbay-Fudge C, Chumas P, Mathew RK, Anderson IA. Day 2 neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios for prediction of delayed cerebral ischemia in subarachnoid hemorrhage. Neurosurg Focus. 2022;52(3):E4. doi: 10.3171/2021.12.FOCUS21642 [DOI] [PubMed] [Google Scholar]
- 34.Wu Y, He Q, Wei Y, et al. The association of neutrophil-to-lymphocyte ratio and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: possible involvement of cerebral blood perfusion. Neuropsychiatr Dis Treat. 2019;15:1001–1007. doi: 10.2147/NDT.S190477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dowlati E, Mualem W, Carpenter A, et al. Early Fevers and Elevated Neutrophil-to-Lymphocyte Ratio are Associated with Repeat Endovascular Interventions for Cerebral Vasospasm in Patients with Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care. 2022;36(3):916–926. doi: 10.1007/s12028-021-01399-7 [DOI] [PubMed] [Google Scholar]
- 36.Chang JJ, Dowlati E, Triano M, et al. Admission Neutrophil to Lymphocyte Ratio for Predicting Outcome in Subarachnoid Hemorrhage. J Stroke Cerebrovasc Dis. 2021;30(9):105936. doi: 10.1016/j.jstrokecerebrovasdis.2021.105936 [DOI] [PubMed] [Google Scholar]
- 37.Giede-Jeppe A, Reichl J, Sprugel MI, et al. Neutrophil-to-lymphocyte ratio as an independent predictor for unfavorable functional outcome in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2019;132(2):400–407. doi: 10.3171/2018.9.JNS181975 [DOI] [PubMed] [Google Scholar]
- 38.Jamali SA, Turnbull MT, Kanekiyo T, et al. Elevated Neutrophil-Lymphocyte Ratio is Predictive of Poor Outcomes Following Aneurysmal Subarachnoid Hemorrhage. J Stroke Cerebrovasc Dis. 2020;29(4):104631. doi: 10.1016/j.jstrokecerebrovasdis.2019.104631 [DOI] [PubMed] [Google Scholar]
- 39.Zhang Y, Yang P, Gu B, Wang J. Comparison of the Diagnostic Values of Neutrophil, Neutrophil to Lymphocyte Ratio, and Platelet to Lymphocyte Ratio in Distinguishing Spontaneous Subarachnoid Hemorrhage from Nontraumatic Acute Headache. Clin Lab. 2019;65(10):845. [DOI] [PubMed] [Google Scholar]
- 40.Yi HJ, Lee DH, Sung JH. Inflammation-based Scores are Associated with the Prognosis of Patients with Aneurysmal Subarachnoid Hemorrhage After Neuro-intervention. Curr Neurovasc Res. 2020;17(5):676–685. doi: 10.2174/1567202617999201117120905 [DOI] [PubMed] [Google Scholar]
- 41.Yun S, Yi HJ, Lee DH, Sung JH. Systemic Inflammation Response Index and Systemic Immune-inflammation Index for Predicting the Prognosis of Patients with Aneurysmal Subarachnoid Hemorrhage. J Stroke Cerebrovasc Dis. 2021;30(8):105861. doi: 10.1016/j.jstrokecerebrovasdis.2021.105861 [DOI] [PubMed] [Google Scholar]
- 42.Li J, Zhou K, Wang L, Cao Q. Predictive Model of Cerebral Vasospasm in Subarachnoid Hemorrhage Based on Regression Equation. Scanning. 2022;2022:3397967. doi: 10.1155/2022/3397967 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Nobrega Lima Rodrigues de Morais A, Ribeiro Baylão VM, Martins Silva T, Gomes Dos Santos A, Azevedo M, J. M. de Oliveira A. Is neutrophil-lymphocyte ratio a useful tool for predicting outcome in subarachnoid hemorrhage? A systematic review. Neurosurg Rev. 2021;44(6):3023–3028. doi: 10.1007/s10143-021-01484-7 [DOI] [PubMed] [Google Scholar]
- 44.Kox M, Pompe J, Hoedemaekers A, Pickkers P. Does subarachnoid haemorrhage affect the innate immune response? Intensive Care Med. 2007;33(7):1303. doi: 10.1007/s00134-007-0664-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gris T, Laplante P, Thebault P, et al. Innate immunity activation in the early brain injury period following subarachnoid hemorrhage. J Neuroinflammation. 2019;16(1):253. doi: 10.1186/s12974-019-1629-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu F, Liu Z, Li G, et al. Inflammation and Oxidative Stress: potential Targets for Improving Prognosis After Subarachnoid Hemorrhage. Front Cell Neurosci. 2021;15:739506. doi: 10.3389/fncel.2021.739506 [DOI] [PMC free article] [PubMed] [Google Scholar]