African relevance
-
•
The issue of trauma and injury is a major global health concern, particularly in Africa, where it is also called the silent epidemic.
-
•
This study provides information on the clinical profiles of patients admitted to the national trauma center of Ethiopia, Alert Hospital, in order to better understand the burden of this global health concern and the immediate outcomes for patients in Ethiopia, the second most populous country in Africa.
-
•
We anticipate that this study will add to the body of research needed in the field, support efforts to reduce trauma, and enhance hospital trauma care in Africa.
Keywords: Clinical profile, Trauma, Emergency, Injury, Outcome
Abstract
Introduction
The term traumatic injury refers to physical injuries that present quickly and with a great deal of severity. These injuries can result from blunt, penetrating, and other causes. The best patients' outcomes are achieved when all parts of a trauma care system are in place. In low-resource settings, these facilities are scarce and their requirements high. Identifying patient profiles and evaluating these in relation to patient outcomes will help to guide interventions and monitor progress.
Methods
This study aimed to examine the clinical profile and outcomes of trauma patients at ALERT Hospital, Ethiopia's busiest national trauma center. A retrospective cross-sectional chart review of 362 patients admitted from January 2019 to December 2019 at Alert Hospital trauma and emergency department was conducted.
Results
The male-to-female ratio was 2.5:1, with trauma more prevalent among those in the age group of 24–33. Comparatively more injuries 98 (27.1%) occur between 8 and 6 a.m. and 90 (24.9%) of patients were transported by ambulance to the hospital. Among patients referred to the hospital, 247 (68.2%) patients received pre-hospital treatment. Interpersonal Violence (IPV) accounts for 31.8% of all accidents, followed by Road Traffic Accidents (RTA), which account for 30.7%. The Kampala Trauma Severity score (KTS) II showed mild trauma (82.3%), moderate trauma (11%), and severe trauma account (6.6%). A total of 44.2% of the victims suffered soft tissue injuries and 24% suffered extremity fractures, with 11.3% sustaining polytrauma. The mortality rate was 3.6%, with RTA, head injury, polytrauma, the severity of the injury, and patients with CPR were statistically associated factors.
Discussion
IPV and RTA were the two most frequent causes of injuries, with most trauma victims being young. A great deal of emphasis needs to be given to preventing injury and improving prehospital emergency services.
Introduction
The term traumatic injury is used to describe an injury requiring prompt medical attention and intervention to save the patient's life or the injured body part or limb. Globally, trauma is the number one cause of death and disability: affecting people of all ages, races, sexes, income levels, and geographical locations (1). Injuries due to blunt, penetrating, and other insults may lead to trauma. In order for trauma patients to have good outcomes, all aspects of trauma care must be in place, including a robust prehospital care system, competent human workers, buildings, equipment, and a continuous supply of resources ([1], [2], [3]).
Worldwide, injuries cause an average of over 5 million deaths per year, or 16,000 deaths per day (2). Global injuries deaths are higher than deaths due to Human immunodeficiency virus /acquired immunodeficiency syndrome (HIV/AIDS), malaria, and tuberculosis combined, more than 5 million deaths per year and are expected to be the seventh leading cause of death worldwide by 2030. Trauma is seen as a substantial economic burden in many countries worldwide. It is the third-largest cause of mortality in the United States among people aged 1 to 44, accounting for 59 % of deaths in this age group and 20 % of all deaths. Trauma causes 37.7 million emergency hospital visits per year, costing $671 billion yearly (4).
There is also little evidence to assess the outcomes of traumatic injuries in these regions, making the quality of emergency and trauma care in Low-Middle Income Countries (LMICs) understudied (5). Plus, patients' outcomes after trauma are directly related to a nation's economic status, and developing countries suffer a lot as a result. As an example, if we look at the mortality rate, which includes both prehospital and in-hospital deaths, it is 35% in high-income countries, 55% in middle-income countries, and 63% in low-income countries (6). According to data from a hospital-based injury surveillance registry in Sub-Saharan Africa, one of the poorest regions in the world, the mortality rate is higher in younger people compared to developed nations. The most common causes of injury that resulted in in-hospital admission were road traffic accidents, falls, and assaults (7).
The most frequently witnessed trauma in Ethiopia and the leading cause of death and disability from accidents is a Road Traffic Accident (RTA). In Addis Ababa, Ethiopia's capital city, injury-related death affects most of the productive groups of the society. It is attributed to 7% of all deaths, mostly male (8). According to statistics, Ethiopia is one of the countries with the most road traffic accidents each year. Over 2000 persons are killed in road traffic collisions every year, with pedestrians accounting for 48%, passengers for 45%, and drivers for 7% (9).
An evaluation of the patterns and outcomes of injury-related illnesses is crucial for improving trauma management in the country. There may be differences in the approximate figures of traumatic injury profiles and outcomes, findings between regional and other tertiary hospitals in Addis Ababa due to weather patterns, industrial aggregation, massive construction activities, geographical features, cultural differences, heavy traffic, etc. As a result, a comprehensive national study is needed better to understand these characteristics and the outcomes of patients. However, this study will describe the patient characteristics and injury outcomes at a national trauma center (ALERT Hospital) to answer the following research questions: What factors influence the outcomes of an injury? What types of organ/system injuries are common in emergencies? How do these injuries occur? We hope the outcomes from these studies will help develop further research and improve patients' outcomes.
Methods
Study design and setting
After receiving ethical approval from ALERT hospital, Department of Emergency Medicine Ethics Committee (Ref No: EM/SM/107/2021 dated 17/07/2021), an institution-based retrospective chart and electronic medical records review was conducted in the ALERT hospital trauma center emergency department from January 2019 to December 2019.
Sampling method
A single proportion formula was used to calculate the sample size to estimate injury prevalence. The Prevalence of injury was obtained from the previous study conducted in the Gedeo region, P = 0.466 (28), confidence interval = 95%, the margin of error = 5%, and non-response rate 5 %. Thus, the required sample size was 382 injury patients visiting the trauma center emergency department. Systematic random sampling technique was used, using a computer list of patient registries, by sampling fraction (k)= N/nf = 7,500/382 =20 the first chart review was selected using the lottery method, then the subsequent patient's chart review was obtained by adding the sample fraction.
Data collection tools and procedure
Information was collected using a pre-tested data collection form which was adapted from the World Health Organization (WHO) injury surveillance guideline and necessary modifications were made to the questionary tool (10), which included the following details: 1) sociodemographic profile, 2) clinical profile, 3) injury grading scoring, and 4) outcome from the emergency department, in the demographic profile, age, sex, place of residence, and in the clinical profile, type, and mechanism of injury, anatomical site of injury, a surgical procedure done within the Emergency Room, types of vehicle used to arrive at the hospital, time to reach the hospital and all others were noted in the review time. Also, information on prehospital care was included. Prehospital care in this study was defined as the care given at the health facilities or sites where the patients were referred, not the scene where the trauma occurred.
The Kampala trauma Severity scoring (KTS II) method was used to measure trauma severities and predict their outcome (11). To quantify injury severity, patient age, systolic blood pressure on admission, the respiratory rate on admission, and the neurological status of the patients were examined using AVPU, which classified them as Alert, respond to Voice, respond to Pain or Unresponsive, and score for serious injuries was collected and calculated to scale the severity of trauma.
Data were first checked manually for completeness, then coded and entered into Epi-Data version 4.6. The entered data were transferred to Statistical Package for the Social Sciences (SPSS) version 25. The data were cleaned by visualizing, calculating frequencies, and sorting. The association between the dependent and independent variable were investigated by Fisher's exact test estimating association. We stated the exact P-value of significance ≤ 0.05 to recognize highly relevant associations. Data were summarized using tables and figures and statistical summary measures used for presentation.
Results
Over one year, a total of 7500 trauma patients were treated at the trauma center emergency department of ALERT Hospital from January 2019 - to December 2019. In this study, 380 patients' cards were systematically selected for further analysis, and of 380 only 362 trauma patient cards were discovered to have complete records, resulting in a 95.3% completeness rate. The age range is 14 to 90, with a median age of 33. The majority 259 (71.5%) of trauma patients in this study were male, and 129 (35.6%) of patients were aged between 24-33 years, with a mean age of 35. Regarding their residence, the majority, 306 (84.5%), of trauma patients were urban dwellers. (See Table 1)
Table 1.
Sociodemographic characteristics of patients visiting ALERT trauma center emergency department.
| Variables | Frequency | Percent | |
|---|---|---|---|
| Sex | Male | 259 | 71.5 |
| Female | 103 | 28.5 | |
| Total | 362 | 100.0 | |
| Age | 14 – 23 | 120 | 33.1 |
| 24 – 33 | 129 | 35.6 | |
| 34 – 43 | 58 | 16.0 | |
| 44 – 53 | 24 | 6.6 | |
| 54 – 64 | 21 | 5.8 | |
| ≥65 | 10 | 2.8 | |
| Total | 362 | 100.0 | |
| Place of residence | Urban | 306 | 84.5 |
| Rural | 56 | 15.5 | |
| Total | 362 | 100.0 |
Most trauma patients, 261 (72.1%), arrived at the hospital after one hour of injury. The majority of the accidents, 98 (27.1 percent), occurred during the daytime, between 08:00. a.m. and 11:59 a.m. Out of 362 patients, 251 (69.3%) live in Addis Ababa, and Oromia 85 (23.5%), which surrounds Addis Ababa, is the second most prevalent place of patient residency. Mode of arrival at the hospital showed that 90 (24.9%) of patients were transported by ambulance, 216 (59.7%) by taxi, and 115 (31.8 %) by walking. Patients’ triage category showed that: red 21 (5.8%), orange 37 (10.2%), yellow 267 (73.8%), green 37, (10.2%). 187 (51.7%), were referred to a hospital from a primary health center, while the rest were either private 36 (9.9%) or recommended by another regional hospital 24 (6.6 %). 115 (32.8%) of patients admitted to the hospital did not receive prehospital emergency care. The majority of patients, 157 (43.4%), live within less than a 5-kilometer radius of the hospital. About 53 (14.6%) patients drank alcohol and were intoxicated at the time of trauma. (See Table 2)
Table 2.
baseline clinical information of patients visiting ALERT trauma center emergency department.
| Variables | Frequency (%) | |||
|---|---|---|---|---|
| Duration of trauma | ||||
| Less than 1 hours | 53 (14.6) | |||
| Greater than 1 hour | 261 (72.1) | |||
| 1 day | 34 (9.4) | |||
| Greater than 1 day | 14 (3.9) | |||
| Total | 362 (100) | |||
| Time of injury | ||||
| 00:00 – 03:59 am | 38 (10.5) | |||
| 04:00 am – 07:59 am | 72 (19.9) | |||
| 08:00 am – 11:59 am | 98 (27.1) | |||
| 12:00 pm – 15:59 pm | 73 (20.2) | |||
| 16:00 pm – 19:59 pm | 47 (13.0) | |||
| 20:00 pm – 23:59 pm | 34 (9.4) | |||
| Total | 362 (100) | |||
| Region of referral | ||||
| Addis Ababa | 251 (69.3) | |||
| Amhara | 12 (3.3) | |||
| Benishangul Gumuz | 1 (0.3) | |||
| Diredawa | 1 (0.3) | |||
| Oromia | 85 (23.5) | |||
| SNNPE | 12 (3.3) | |||
| Total | 362 (100) | |||
| Mode of arrival to the hospital | ||||
| Ambulance | 90 (24.9) | |||
| Bajaj | 2 (0.6) | |||
| Taxi | 216 (59.7) | |||
| Private car | 31 (8.6) | |||
| Walking | 22 (6.1) | |||
| Others | 1 (0.3) | |||
| Total | 362 (100) | |||
| Triage Categories | ||||
| Red | 21 (5.8) | |||
| Orange | 37 (10.2) | |||
| Yellow | 267 (73.8) | |||
| Green | 37 (10.2) | |||
| Total | 362 (100) | |||
| Intent of trauma | ||||
| Unintentional (accidental) | 233 (64.4) | |||
| Intentional self-harm (suicide) | 5 (1.4) | |||
| Assault (interpersonal violence) | 121 (33.4) | |||
| Undetermined (awaiting result of investigation) | 2 (0.6) | |||
| Unknown | 1 (0.3) | |||
| Total | 362 (100) | |||
| Distance of patient's injury site and hospital in kilometer | ||||
| Less than 5 km | 157 (43.4) | |||
| 5–15km | 153 (42.3) | |||
| 16–25km | 6 (1.7) | |||
| 26–35km | 2 (0.6) | |||
| 36–45km | 1 (0.3) | |||
| Greater than 45km | 43 (11.9) | |||
| Total | 362 (100) | |||
| The interval between injury and arrival | ||||
| Immediate (<1hr) | 52 (14.4) | |||
| Within hrs. (1-24hrs) | 260 (71.8) | |||
| Within days (>24hrs) | 50 (13.8) | |||
| Total | 362 (100) | |||
| Referral source | ||||
| Self | 115 (31.8) | |||
| Health center | 187 (51.7) | |||
| Private clinic | 36 (9.9) | |||
| Government | 24 (6.6) | |||
| Total | 362 (100) | |||
| Treatment given before arrival | ||||
| Yes | 247 (68.2) | |||
| No | 115 (31.8) | |||
| Total | 362 (100) | |||
| Is the patient used alcohol? | ||||
| Yes | 53 (14.6) | |||
| No | 309 (85.4) | |||
| Total | 362 (100) | |||
The total Prevalence of mortality in this study was 3.6 %. Interpersonal violence was the most common mechanism of injury, accounting for 115 (31.8%), followed by RTA, 111 (30.7%), and falls 85 (23.5%). Gunshot and burn injury were the least common mechanisms of trauma, accounting for 2 (0.6%) and 4 (1.1%), respectively. Pedestrians 69 (62.1%) were affected mainly by RTA, followed by passengers 29 (26.2%), and commonly vehicles involved in RTA were Bajaj,50 (45%), and Minibus 36 (32.5%). The most prevalent anatomical site of injury was the head 107 (29.6%) followed by upper extremity, 75 (20.7%), and polytrauma, 41 (11.3%), while spine trauma was the least prevalent form of injury 3 (0.8 %) (See Table 3).
Table 3.
Clinical profile of patients visiting ALERT trauma center emergency department.
| Variables | Frequency | Percent | |
|---|---|---|---|
| Mechanism of injury | RTA | 111 | 30.7 |
| Fall down | 85 | 23.5 | |
| Stab injury | 11 | 3.0 | |
| Gunshot | 2 | .6 | |
| Industrial (machine injury) | 34 | 9.4 | |
| Burn | 4 | 1.1 | |
| Fighting | 115 | 31.8 | |
| Total | 362 | 100.0 | |
| If trauma is due to RTA | Pedestrian | 69 | 62.1 |
| Motorcyclist | 9 | 8.1 | |
| Passenger | 29 | 26.2 | |
| Driver | 4 | 3.6 | |
| Total | 111 | 100.0 | |
| Types of vehicles for RTA | Minibus | 36 | 32.5 |
| Heavy good vehicle | 8 | 7.2 | |
| Taxi | 5 | 4.5 | |
| Bajaj | 50 | 45 | |
| Motorcycle | 12 | 10.8 | |
| Total | 111 | 100.0 | |
| Anatomical site of injury | Head | 107 | 29.6 |
| Chest | 31 | 8.6 | |
| Abdomen | 8 | 2.2 | |
| Upper extremities | 75 | 20.7 | |
| Lower extremities | 64 | 17.7 | |
| Spine | 3 | .8 | |
| Pelvic | 13 | 3.6 | |
| Polytrauma | 41 | 11.3 | |
| Maxillofacial | 20 | 5.5 | |
| Total | 362 | 100.0 | |
| Kampala trauma severity score | Milled | 298 | 82.3 |
| Moderate | 40 | 11.0 | |
| Sever | 24 | 6.6 | |
| Total | 362 | 100.0 | |
| Duration of hospitalization | Less than 24hr | 183 | 50.6 |
| Greater than 24hrs | 178 | 49.2 | |
| Unknown | 1 | 0.3 | |
| Total | 362 | 100.0 |
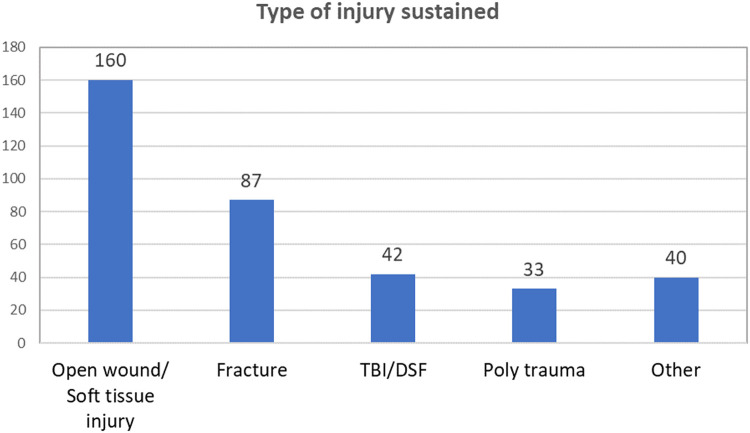
Soft tissue injury is the most common injury type, accounting for 160 (44.2%), and extremities fracture is the second most common injury type in Emergency Room (ER) during the research period, accounting for 87 (24%), followed by Traumatic Brain injury/Depressed Skull fracture (TBI/DSF) and Polytrauma, which account for 42 (11.6%) and 33 (9.1%), respectively. (See Figure 1)
Fig. 1.
Bar diagram showing types of injury sustained at ALERT hospital trauma center emergency department.
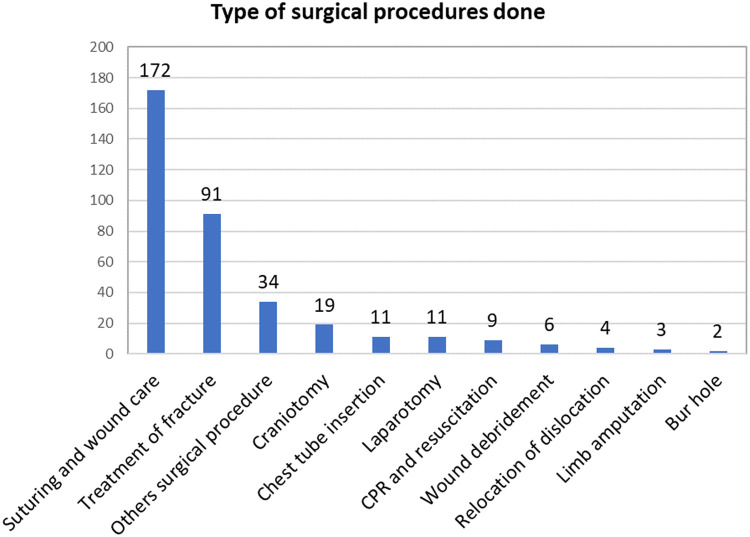
The surgical procedures were the reduction of fracture and application of cast 91 (25.1%), suturing and dressing 172 (47.5%), and chest tube insertion in 11 (3%). Reduction of dislocation in 4 (1.1%), Craniotomy 19 (52%), Bur hole2 (0.6%), Limb amputation 3 (0.8%), Laparotomy 11 (3%), Cardio Pulmonary Resuscitation (CPR) and resuscitation 9 (2.5%), and Others surgical procedure with joint management were 34 (9.4%). (See Figure 2)
Fig. 2.
Bar diagram showing surgical procedure done at ALERT hospital trauma center emergency department.
The majority of injured patients, 183 (50.6%), were treated and discharged, while 128 (35.4%) were admitted to trauma wards. About 27 (7.5%) patients were needed to be admitted to an intensive care unit. The remaining 11 (3%) patients were assessed in the emergency room and referred to other hospitals. Thirteen (3.6%) of injured patients died after arriving at the emergency department and receiving CPR.
The Pearson chi-square and Fisher's exact test were calculated to assess the relationship between patient clinical profile and ER mortality. The resulting numbers show that mechanism of injury, Anatomical site of injury, injury type, trauma severity, and type of surgical treatment given is statistically highly associated factor for mortality than others, with (p-value = 0.002, 0.000, 0.000, 0.000, 0.000) respectively.
Discussion
In this study, retrospective data from patients' cards were used to provide an in-depth picture of the immediate outcome of injuries treated at ALERT hospital in Addis Ababa, Ethiopia. The findings of this study revealed that the most common injury result was a minor injury, which required mild medical care (82.3%), followed by mild injury (11%), and severe injury, which required intense medical/surgical management (6.6%).
However, a study conducted at Tikur Anbessa specialized hospital showed moderate (71%) and severe (14.6%) injuries. A similar study conducted at Jimma hospital reported that 2.7% presented as severe, 41.3% moderate, and 26% as minor injuries) (13). The difference between these three hospitals could be explained by possible differences used to define moderate or severe injury in the respective studies.
This study found that among the total 24 (6.6 %) severely injured half patients, 12 (50%) were transported by taxi and private vehicle, while the remaining 12 (50%) were transported and arrived at the hospital by ambulance. The findings from this study also support the statement that Addis Ababa Ethiopia, like other poor African nations, has a poor, unplanned, and fragmented pre-hospital care system (14). And lower and has greater variation than a study done at Menelik Memorial hospital 72.7% (12) The difference can be explained by the fact that Menelik II memorial hospital is close to the Addis Ababa fire and emergency center, which means that more patients are referred to the hospital by the dispatch center than ALERT hospital, which is located in the city's point.
The analysis of the possible causes of severe injuries showed that 62.5% were due to RTAs and 20.8% were due to falls accidents. A similar finding was noted by Kifle et al. (13) which was 49.7% was caused by RTAs, 12.5% by stab injury, and 11.4 % by cut by a sharp tool, whereas B. Tadesse et al. reports RTA (38.3%) followed by interpersonal violence (31.5%) and fall (21.2%) are the possible cause for severe trauma in Tikur Anbessa Specialized Hospital (13).
In this study the mortality rate was 3.6%, this implies that a higher proportion of death is reported at the emergency department which is not comparable with the study that was reported from Tikur Anbessa specialized hospital (1.47%), Menelik hospital (1.5%), India (1%), Canada (1.2%), and Korea (0.6%) ([15], [16], [17], [18]). However, the result is within the expected worldwide range (0.5%-6%) and much lower than the study conducted in Dilla hospital (6%), and sub-Saharan Africa (4.2%) (7,19). This inconsistency may be due to variation in the study sample, study settings, lack of prehospital care, availability of different specialties for trauma care, and lack of Advanced Trauma Life Support (ATLS) and emergency care training among health care workers in this study setting.
When we looked at the success rates of CPR for patients exclusively arrested in the ER, we found Return of spontaneous circulation (ROSC) rates of 23.1%, which is close to the 30.2 % ROSC rate of cardiac arrest cases in the ER published by Malaysia University Hospital (20), but lower than a prospective observational study of CPR outcomes in the Emergency Department of the Aga Khan University Hospital, Karachi, Pakistan that found ROSC rate of 59% (21). The difference could be due to sampling size, study design, or setting, and countries are reporting successful cardiac arrest resuscitation to have effective systems in place to assist and transport patients, including effective point to point communication centers, well-equipped ambulances, and highly skilled and experienced prehospital care teams (22). In Ethiopia, such systems are not available (13,22,23), which has a significant negative influence on patient outcomes and, as a result, leads to a low success rate on overall patient outcomes.
In this study, the average duration from accident to hospital admission for total trauma patients was 3 hours, with 11 (84.6%) of arrived dead at the hospital after 1 hour and the golden hour had gone. which is lower than the study done in Lusaka, Zambia, where a large percentage of patients arrived within 6 hours of injury (62.2%) (25), and much higher than the meantime from accident to hospital admission in the United States of America (USA) (64.6 min) (26), Germany 68 min (27).
Also, this study revealed that 24% of trauma patients arrived in the ALERT hospital ER by ambulance. However, almost all trauma patients arriving at the hospital ER by ambulance were transported from the health center, private hospital, and other regional hospital settings, where they may have received resuscitation, not directly from the injury scene. This is significantly higher than the 20.3% found in a previous study of emergency medical care utilization in Addis Ababa hospitals, in Lusaka, Zambia (5.8%) and much lower than in the USA, which reported (82.5%) ([23], [24], [25]) These differences might be influenced by various variables, including distance to health-care facilities, the idea that private car and taxi is faster, or a lack of awareness of the Emergency Medical Service (EMS) contact number. More work is needed to promote awareness about using emergency medical services to transport trauma patients to hospitals.
As a result of the Fisher's exact test model, this study found that RTA, Head injury, polytrauma, severely injured and those patient with CPR is statistically highly associated factor for mortality than other variables (p-value = 0.002, <0.001, <0.001, <0.001, <0.001) respectively. In the United Kingdom (UK), using the chi-square test model trauma patient's mortality or improvement is significantly associated with the Glasgow coma scale (GCS), age, and respiratory rate (28). A study done in Germany due to the logistic regression model found that shock and bleeding variables and age were strongly predictive of mortality (27). The difference might be attributable to the association model they utilized, the number of trauma patients, data availability, and the analytic approach.
In this study interpersonal violence is the most common accident that brings people to the emergency department, accounting for 31.8 % of all emergency room visits, most violence occurred towards males (87%) who were younger aged between 24-33 and 34.8% of those who are alcoholics and intoxicated at the time of trauma, which is comparable with a study done in Ethiopia, Mekelle public hospital (31.1%), in Ethiopian, Gedeo Dilla hospital (30.1%), Lusaka, Zambia (38.2%) and have a greater variation to a study done at Tikur Anbessa specialized hospital (20%), and South Africa (20.9%), (9,29,25,30,31). The differences might be related to referrals from health centers, where most low-acuity triage referrals are sent to hospitals for medico-legal paperwork and certification purposes rather than therapeutic care, which physicians can only provide.
Road traffic injuries accounted for 30.7% of all injuries, which is greater than the 14.1% reported by Mekelle Public Hospital and, but far lower than the 36.5% reported by Menelik II Specialized Hospital, 49.1% Tikur Anbessa and Yekatit 12 hospital, 47.3% reported by Gedio Dilla Hospital and India 75% (9,16,32,29,17). RTA was the primary cause of mortality in this study (92.3%), which is greater than the study published in Ethiopian University Hospitals (52.2%) (19), and Saudi Arabia (60%) of patients died in road traffic accidents (33). Variation in RTA prevalence might be attributable to research sample size, geographical location of the research setting, and death from RTA is much higher related to multi-factorial, which might be explained by patients presenting with traffic-related injuries being more severe than other mechanisms of trauma.
Conclusion
The two most frequent causes of injuries were IPV and road traffic accidents, with most trauma victims being young and greater than 30 % not receiving emergency care. There is a need to have urgent injury prevention and management strategies and establish a Prehospital Emergency Medical Service System. The findings of this study are anticipated to contribute to providing clear and convincing support for the Ministry of Health to enhance prehospital care service as well as alarm the road safety authority and traffic management to act on road safety and the use of safety measures in the three-wheeler/Bajaj transportation system. Future studies can be directed to pre-hospital access and long-term follow-up outcomes of injury victims to account for exact mortality and morbidity due to such unfortunate events.
Limitations
The findings of this study rely on secondary data, as most retrospective studies are, for this reason incomplete or missed patient information in the chart might not accurately reflect trauma patients' mortality. The other limitation was that the design we employed was limited to investigate prehospital factors more reliably hence, most fatalities which might have occurred at the scene of the accident might be underrepresented, necessitating further collaborative prospective researches and surveillance-based approaches.
Dissemination of results
The findings of this study were presented to Addis Ababa University College of Health Science as partial fulfillment of the requirements for a Master's degree by the corresponding author in his thesis research. The comments from internal and external evaluators during the thesis presentation were critically appraised and reviewed. The results of this study were also shared with the staff members of the ALERT comprehensive specialized hospital and the Emergency Directorate of the Ministry of Health.
Authors contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: TA contributed 37%; AA and MK contributed 7.5% each; YB, EB, and FK contributed 16% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
There are no conflicts of interest declared by the authors.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.afjem.2022.10.013.
Appendix. Supplementary materials
References
- 1.Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health. 2000;90(4):523–526. doi: 10.2105/ajph.90.4.523. https://pubmed.ncbi.nlm.nih.gov/10754963/ [cited 2022 Feb 16]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chandran A, Hyder AA, Peek-Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev. 2010;32(1):110–120. doi: 10.1093/epirev/mxq009. https://pubmed.ncbi.nlm.nih.gov/20570956/ [cited 2022 Feb 16]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rush C. Guidelines for Essential Trauma Care. J Emerg Nurs. 2006;32(1):89–90. [Google Scholar]
- 4.Khorgami Z, Fleischer WJ, Chen YJA, Mushtaq N, Charles MS, Howard CA. Ten-year trends in traumatic injury mechanisms and outcomes: A trauma registry analysis. Am J Surg. 2018;215(4):727–734. doi: 10.1016/j.amjsurg.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 5.Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Global Health [Internet] 2018 Nov 1;6(11):e1196–e1252. doi: 10.1016/S2214-109X(18)30386-3. http://www.thelancet.com/article/S2214109X18303863/fulltext [cited 2022 Feb 16]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charles Mock, World Health Organization International Society of Surgery., International Association of Trauma Surgery and Intensive Care. Guidelines for essential trauma care. World Health Org. 2004:93. [Google Scholar]
- 7.Tyson AF, Varela C, Cairns BA, Charles AG. Hospital mortality following trauma: an analysis of a hospital-based injury surveillance registry in sub-Saharan Africa. J Surg Educ. 2015;72(4):e66–e72. doi: 10.1016/j.jsurg.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Anteneh A, Endris BS. Injury related adult deaths in Addis Ababa, Ethiopia: Analysis of data from verbal autopsy. BMC Pub Health. 2020;20(1):1–8. doi: 10.1186/s12889-020-08944-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amdeslasie F, Kidanu M, Lerebo W, Ali D. Patterns of Trauma in Patient Seen At the Emergency Clinics of Public Hospitals in Mekelle. Northern Ethiopia. Ethiopian Med J. 2016;54(2):63–68. [PubMed] [Google Scholar]
- 10.INJURY SURVEILLANCE GUIDELINES. 2001 [cited 2022 Feb 16]; Available from: http://www.hdnet.org
- 11.Weeks SR, Juillard CJ, Monono ME, Etoundi GA, Ngamby MK, Hyder AA, et al. Is the Kampala trauma score an effective predictor of mortality in low-resource settings? A comparison of multiple trauma severity scores. World J Surg. 2014;38(8):1905–1911. doi: 10.1007/s00268-014-2496-0. https://pubmed.ncbi.nlm.nih.gov/24715042/ [cited 2022 Feb 16]Available from. [DOI] [PubMed] [Google Scholar]
- 12.Tadesse B, Tekilu S, Nega B, Seyoum N. Pattern of Injury and Associated Variables as Seen in the Emergency Department at Tikur Anbessa Specialized Referral Hospital, Addis Ababa, Ethiopia. East Cent. Afr. J. Surg 2005;19(1):73–82. Retrieved from https://www.ajol.info/index.php/ecajs/article/view/102446.
- 13.Woldemichael K, Berhanu N. Magnitude and pattern of injury in jimma university specialized hospital, South west ethiopia. Ethiopian J Health Sci. 2011;21(3):155–15565. [PMC free article] [PubMed] [Google Scholar]
- 14.Firew T, Gebreyesus A, Woldeyohannes L, Ebrahim F, Patel S. Human resources for emergency care systems in Ethiopia: Challenges and triumphs. African J Emerg Med. 2020 doi: 10.1016/j.afjem.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byun CS, Park IH, Oh JH, Bae KS, Lee KH, Lee E. Epidemiology of trauma patients and analysis of 268 mortality cases: Trends of a single center in Korea. Yonsei Med J. 2015;56(1):220–226. doi: 10.3349/ymj.2015.56.1.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laytin AD, Seyoum N, Kassa S, Juillard CJ, Dicker RA. Patterns of injury at an Ethiopian referral hospital: using an institutional trauma registry to inform injury prevention and systems strengthening. African J Emerg Med. 2020;10(2):58–63. doi: 10.1016/j.afjem.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chowdhury S, pratim Chakraborty P. Clinicoepidemiological profile of trauma patients admitting to the emergency department of a tertiary care hospital in eastern India. J Family Med Primary Care. 2017;6(2):169–170. doi: 10.4103/jfmpc.jfmpc_621_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moore L, Stelfox HT, Evans D, Hameed SM, Yanchar NL, Simons R, et al. Trends in injury outcomes across Canadian trauma systems. JAMA Surg. 2017;152(2):168–174. doi: 10.1001/jamasurg.2016.4212. [DOI] [PubMed] [Google Scholar]
- 19.Abate semagn, Abafita BJ, Kassim HM, Basu B. Epidemiology and outcomes of injuries among trauma patients in Ethiopia: A 5 -years retrospective Analysis. In 2019. p. 1–23. [DOI] [PMC free article] [PubMed]
- 20.Chew KS, Idzwan ZM, Hisamuddin NAR, Kamaruddin J, Wan Aasim WA. Outcomes of cardiopulmonary resuscitation performed in Emergency Department, Hospital Universiti Sains Malaysia. Med J Malaysia. 2008;63(1):4–8. [PubMed] [Google Scholar]
- 21.Rehmani R, Baqir M, Amanullah S. Return of spontaneous circulation and survival at hospital discharge in patients with out-of-hospital and emergency department cardiac arrests in a tertiary care centre. J Pakistan Med Assoc. 2007;57(6):278–281. [PubMed] [Google Scholar]
- 22.Eckstein M, Stratton SJ, Chan LS. Cardiac arrest resuscitation evaluation in Los Angeles: CARE-LA. Ann Emerg Med. 2005;45(5):504–509. doi: 10.1016/j.annemergmed.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 23.Zewdie A. EC EMERGENCY MEDICINE AND CRITICAL CARE Research Article Assessment of Trauma Care in Tertiary Center. Addis Ababa Ethiopia. 2020;2:1–8. May. [Google Scholar]
- 24.Sultan M, Abebe Y, Tsadik AW, Ababa A, Yesus AG, Mould-Millman NK. Trends and barriers of emergency medical service use in Addis Ababa. Ethiopia. BMC Emerg Med. 2019;19(1):1–8. doi: 10.1186/s12873-019-0242-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seidenberg P, Cerwensky K, Brown RO, Hammond E, Mofu Y, Lungu J, et al. Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka. Zambia. African J Emerg Med. 2014;4(3):115–122. [Google Scholar]
- 26.Jarman MP, Curriero FC, Haut ER, Porter KP, Castillo RC. Associations of distance to trauma care, community income, and neighborhood median age with rates of injury mortality. JAMA Surg. 2018;153(6):535–543. doi: 10.1001/jamasurg.2017.6133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huber-Wagner S, Lefering R, Qvick M, Kay MV., Paffrath T, Mutschler W, et al. Outcome in 757 severely injured patients with traumatic cardiorespiratory arrest. Resuscitation. 2007;75(2):276–285. doi: 10.1016/j.resuscitation.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 28.Aljerian N, Alhaidar S, Alothman A, AlJohi W, Albaqami FA, Alghnam SA. Association between the mode of transport and in-hospital medical complications in trauma patients: findings from a level-I trauma center in Saudi Arabia. Ann Saudi Med. 2018;38(1):8–14. doi: 10.5144/0256-4947.2018.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abafita Bedru Jemal, Abate Semagn Mekonnen, Kasim Hilemariam Mulugeta, Basu Bivash. Pattern and outcomes of injuries among trauma patients in Gedeo Zone, Dilla, South Ethiopia: a 5 years retrospective analysis. Ethiopian J Health Sci. 2020;30(5) doi: 10.4314/ejhs.v30i5.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taye M, Munie T. Trauma registry in Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2003;41:221–6. [PubMed]
- 31.Nicol A, Knowlton LM, Schuurman N, Matzopoulos R, Zargaran E, Cinnamon J, et al. Trauma surveillance in Cape Town, South Africa: An analysis of 9236 consecutive trauma center admissions. JAMA Surg. 2014;149(6):549–556. doi: 10.1001/jamasurg.2013.5267. [DOI] [PubMed] [Google Scholar]
- 32.Mengistu Z, Azaj A. Trauma severities scores and their prediction of outcome among trauma patients in two hospitals of Addis Ababa, Ethiopia. Ethiop Med J. 2012;50(3):231–237. Jul. [PubMed] [Google Scholar]
- 33.Issam Barrimah, Midhet F., Sharaf F., et al. Epidemiology of road traffic injuries in qassim region, saudi arabia: consistency of police and health data. Int. J. Health Sci. 2012;6(1):31–41. doi: 10.12816/0005971. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.