Summary
Background
Universal health coverage (UHC) is a core element of Sustainable Development Goals and has become a global healthcare priority. China has been committing to provide all citizens with affordable and equitable basic healthcare over past decades. However, progress towards UHC in China has not been comprehensively assessed. This study aims to comprehensively evaluate the progress towards UHC in China by examining trends in service coverage and financial protection from 1993 to 2018, and estimating the probability of achieving UHC targets by 2030.
Methods
Following the framework proposed by World Health Organization and World Bank, we selected 12 prevention service indicators, 12 treatment service indicators, and two financial protection indicators to evaluate China's progress towards UHC. We used data from four nationally representative household surveys to assess the trends in service coverage and financial protection between 1993 and 2018, as well as their inequalities across subgroups. Meta-analysis was used to construct the composite prevention and treatment indices. The regression-based relative index of inequality was used to measure the income-related inequality of UHC indicators. Bayesian linear regression was conducted to predict progress towards UHC by 2030, and the probability of achieving UHC targets.
Findings
Of the 24 service coverage indicators used in this study, most of them experienced improvements between 1993 and 2018. The composite prevention index increased from 65.6% (95% CI: 52.1%–77.9%) to 87.7% (95% CI: 81.8%–92.6%) and the composite treatment index increased from 57.1% (95% CI: 43.5%–70.1%) to 75.5% (95% CI: 66.6%–83.5%). The inequalities of service coverage experienced significant declines during this period. Based on our projections, most indicators except ones in the area of non-communicable diseases (NCD) will achieve the 80% coverage target by 2030, and the prevention and treatment indices will increase to 92.7% (95% CrI: 90.3%–94.7%) and 83.2% (95% CrI: 75.1%–88.8%) by then. However, we observed limited reductions in the incidences of catastrophic health expenditure and medical impoverishment. Inequalities in financial protection remained large in 2018.
Interpretation
China had made significant progress in improving healthcare service coverage and reducing inequalities between 1993 and 2018. However, China faces great challenges in improving financial protection and controlling NCD on its path towards UHC. Establishment of a primary-healthcare-based integrated delivery system and provision of better financial protection for vulnerable population should be prioritized.
Funding
None.
Keywords: Universal health coverage, Healthcare service coverage, Financial protection, Bayesian analysis, Inequality, China
Research in context.
Evidence before this study
We searched PubMed, Google Scholar, and China National Knowledge Infrastructure (CNKI) using the terms “universal health coverage”, or “universal coverage”, combined with “evaluation”, “measurement”, “assessment”, or “China” for original publications between Jan 1, 2012 and July 1, 2022. We found that although some previous studies discussed the concept of UHC in China, they seldom examined temporal trends of detailed UHC indicators in last decades or made projections of UHC indicators to quantify the probability of achieving UHC targets by 2030.
Added value of this study
To the best of our knowledge, this study is the first attempt to systematically evaluate progress towards UHC in China using a wide range of indicators of healthcare service coverage and financial protection. Our study examined temporal trends in healthcare service coverage and financial protection and their inequalities across subgroups from 1993 to 2018 when most major healthcare reforms happened in China, based on data from multiple household surveys and the framework proposed by WHO and World Bank. We also used a Bayesian analysis to estimate the probability of achieving UHC targets by 2030. The results of this study showed that China had made significant progress in improving healthcare service coverage and reducing inequalities between 1993 and 2018. However, China faces great challenges in improving financial protection and controlling NCD on its path towards UHC.
Implications of all the available evidence
Findings from this study can provide important implications for identifying key interventions in need and setting future healthcare policy priorities in China. We suggest that China needs to develop effective policies to restructure its hospital-centered and fragmented delivery system and establish a primary-healthcare-based integrated delivery system. Provision of better financial protection for vulnerable groups should also be prioritized. We believe that our findings would not only be of interest to Chinese readers, but also provide policy implications for other developing countries.
Introduction
Universal health coverage (UHC), which means that all individuals have access to essential healthcare services without suffering financial hardship, is a core element of Sustainable Development Goals adopted by the United Nations.1 It now has become a global healthcare priority. Many developing countries have incorporated UHC targets into their national healthcare policy formation.2,3 According to its definition, UHC commonly includes two dimensions: healthcare service coverage and financial protection. World Bank and World Health Organization (WHO) set the goal that all countries should achieve the UHC targets of at least 80% coverage of essential health services and 100% of financial protection by 2030.4
A framework with a series of indicators has been developed by WHO and World Bank to monitor progress towards UHC.4 Previous studies used these indicators to conduct global cross-country comparative analyses and examine country-specific temporal trend.5, 6, 7, 8, 9, 10 These analyses provide useful insights for policymakers to identify areas that needs strengthening. However, to date, few studies have used this framework to comprehensively evaluate progress towards UHC in China. Although some previous studies discussed the concept of UHC in China,11, 12, 13 they seldom examined temporal trends of detailed UHC indicators in last decades or made projections of UHC indicators to quantify the probability of achieving UHC targets by 2030.
As the largest country in the Western-Pacific region, the Chinese healthcare system has experienced a dramatic transition over the past decades. Inspired by the spirit of the market-oriented economic reform, the Chinese government had reformed its socialistic healthcare system that was created before 1978 and had adopted a laissez-faire policy since 1986 that defaulted health care to market forces and self-reliance.14 These reforms had resulted in widespread discontent among Chinese people towards inaccessible and unaffordable healthcare services. In 2000, China ranked fourth from the bottom among 191 countries in equity of healthcare financing.15 More than 75% of the Chinese population were not covered by any health insurance and the share of out-of-pocket expenditure in total health expenditure was close to 60% then. The widespread complaints and the outbreak of SARS in 2003 pushed Chinese leaders to reform China's healthcare system. Between 2003 and 2008, the Chinese government successively launched the New Rural Cooperative Medical Scheme for rural residents and the Urban Resident Basic Medical Insurance scheme for child, elderly, disabled, and unemployed residents who were not covered by the Urban Employee Basic Medical Insurance. As a result, by the end of 2008, more than 90% of Chinese population had been covered by social health insurance. Furthermore, China launched a complex and ambitious healthcare system reform plan in 2009, committing to provide all citizens with affordable and equitable basic healthcare. The Chinese government further increased its fiscal investments in healthcare to improve health insurance coverage and strengthen healthcare delivery system. These reform measures led to improvements in health access, financial protection, and population satisfaction.16, 17, 18 However, gaps remained in quality of care, control of non-communicable diseases (NCD), efficiency in delivery, and control of health expenditures.19
Our study aims to comprehensively evaluate the progress towards UHC in China. Using data from multiple household surveys and following the framework proposed by WHO and World Bank, this study examined temporal trends in healthcare service coverage and financial protection from 1993 to 2018 when most major healthcare reforms happened in China, and their inequalities across subgroups. Based on these results, we used a Bayesian analysis to estimate the probability of achieving UHC targets by 2030. Findings from this study could provide important implications for identifying key interventions in need and setting future healthcare policy priorities in China, and could also provide lessons for other developing countries in the Western-Pacific region.
Methods
Data source
We used data from four nationally representative household surveys to assess progress towards UHC in China: National Health Service Survey (NHSS), China Health Nutrition Survey (CHNS), Chinese Household Income Project (CHIP), and National Rural Fixed-Point Survey (RFPS). To examine indicators of health service coverage, we used NHSS and CHNS datasets. NHSS is a serial cross-sectional survey launched in 1993 with six waves of available datasets comprising the years of 1993, 1998, 2003, 2008, 2013, and 2018. It is conducted by the National Health Commission of China with a multistage stratified random sampling method and covers 31 provinces across China. CHNS is an ongoing open longitudinal survey conducted by University of North Carolina at Chapel Hill and Chinese Center for Disease Control and Prevention. It was launched in 1989 and employed a multistage random-cluster sampling process to select samples from nine provinces across China. We used waves of 1993, 1997, 2004, 2009, 2011, and 2015 for analysis in this study. Details of NHSS and CHNS on sampling methods and questionnaires were described in previous studies.16,20,21
To examine trends in financial protection, we used CHIP and RFPS datasets. CHIP is one of the most informative national surveys on household income, expenditures, and wealth.22,23 It is a serial cross-sectional survey with six available waves of 1988, 1995, 2002, 2007, 2013, and 2018. We used the last five waves for our analysis. In addition, we used data from RFPS to complement our results on financial protection in 1995 and 2002, given that questionnaires on household expenditures for rural households in CHIP 1995 and 2002 were not consistent with other waves. The RFPS was initiated in 1986 under the guidance of the Ministry of Agriculture of China. Its sample is selected based on a multi-stage stratified random sampling strategy and covers 31 provinces across China.24,25 Similar with CHIP, RFPS collects extensive information on household income and expenditures.26 More details on the four household surveys used in this study are available in supplementary notes in Appendix A.
It should be noted that the survey timing of waves across these household surveys were not identical. In studies that covered numerous indicators over a long period, such differences in the timing of survey waves were not rare. Existing literature usually regarded adjacent years as the same period to address this inconsistency,6,7,9 given that the UHC progress was seldom a sudden and discontinuous change. We followed this practice in the main analysis. In the latter part, we also examined whether inconsistencies in timing of survey waves would have a great impact on our results and conclusions. Ethical approval was not required for this study because only secondary datasets were used.
UHC indicators
Following the framework proposed and recommended by WHO and World Bank,27 we examined two dimensions of UHC in this study: healthcare service coverage and financial protection. We classified healthcare service coverage indicators into two categories: prevention services and treatment services. Since it was unrealistic to monitor indicators for all healthcare services, we selected 12 prevention indicators and 12 treatment indicators to capture the breadth of healthcare services. The detailed procedures of selecting indicators are shown in Appendix A. Our indicators covered the four tracer areas recommended by WHO and World Bank, as shown in Appendix Table S1. Detailed definitions for every indicator and their data source are shown in Table 1. Prevention indicators used in this study are at least four antenatal care visits (ANC4); postnatal care of mother; BCG immunization; DPT3 immunization; Polio3 immunization; Measles immunization; Hepatitis B (HB3) immunization; non-use of tobacco; non-overweight; non-underweight; improved water; and adequate sanitation. These indicators were recommended by the WHO and were widely used in the previous studies that assessed progress towards UHC at the global and country level.6, 7, 8, 9, 10,28,29 Other common indicators such as breast cancer screening and cervical cancer screening were not included as no series data was available between 1993 and 2018.
Table 1.
Definition of indicators of universal health coverage.
| Indicators | Definition | Data sources |
|---|---|---|
| Prevention indicators | ||
| ANC4 | The proportion of woman who received at least four antenatal care visits during their last pregnancy. | NHSS |
| Postnatal care of mother | The proportion of woman who received at least one postnatal care during their last pregnancy. | NHSS |
| BCG immunization | The proportion of children aged 1–4 years who received at least one dose of BCG vaccine. | NHSS |
| DPT3 immunization | The proportion of children aged 1–4 years who received at least three doses of DPT vaccine. | NHSS |
| Polio3 immunization | The proportion of children aged 1–4 years who received at least three doses of polio vaccine. | NHSS |
| Measles immunization | The proportion of children aged 1–4 years who received at least one dose of measles vaccine. | NHSS |
| HB3 immunization | The proportion of children aged 1–4 years who received at least three doses of hepatitis B vaccine. | NHSS |
| Non-use of tobacco | The proportion of adults aged 14 years or older who do not smoke at the survey time. | CHNS |
| Non-overweight | The proportion of individuals aged 18–65 years who are not overweight (BMI <24.0). | CHNS |
| Non-underweight | The proportion of individuals aged 18–65 years who are not underweight (BMI ≥ 18.5). | CHNS |
| Improved water | The proportion of households whose main source of drinking water is tap water. | NHSS |
| Adequate sanitation | The proportion of households who use flush toilet. | NHSS |
| Treatment indicators | ||
| Institutional delivery | The proportion of woman who gave birth at a health facility during their last childbirth (ie, hospital, maternal and child healthcare institution, and township hospital). | NHSS |
| Skilled birth attendance | The proportion of woman who gave birth with assistance from skilled health providers (ie, doctors, nurses, and midwives) during their last childbirth. | NHSS |
| Normal blood pressure | The proportion of individuals who are not hypertension patients (DBP <90 mmHg, SBP <140 mmHg; are not diagnosed as hypertension by physicians; and do not take hypotensive drugs). | CHNS |
| Hypertension awareness | The proportion of individuals who have been diagnosed as hypertension by physicians in participants with hypertension. | CHNS |
| Hypertension treatment | The proportion of individuals who take antihypertensive medications among the participants with hypertension. | CHNS |
| Hypertension control | The proportion of individuals whose DBP is less than 90 mmHg and SBP is less than 140 mmHg among the participants with hypertension. | CHNS |
| Tuberculosis treatment | The proportion of individuals who visited the medical facility due to TB among the participants with TB in the two weeks preceding the survey. | NHSS |
| Outpatient care seeking when needed | The proportion of individuals who sought outpatient care among those who felt ill or uncomfortable in the two weeks preceding the survey. | NHSS |
| Outpatient care seeking when needed (aged 0–4) | The proportion of children aged 0–4 years who sought outpatient care among those who felt ill or uncomfortable in the two weeks preceding the survey. | NHSS |
| Inpatient care seeking when needed | The proportion of individuals who were admitted in hospital among those who were diagnosed to be hospitalized by physicians in one year preceding the survey. | NHSS |
| Inpatient care seeking when needed (aged 0–4) | The proportion of children aged 0–4 years who were admitted in hospital among those who were diagnosed to be hospitalized by physician in one year preceding the survey. | NHSS |
| Travel time to the nearest medical facility | The proportion of households whose travel time to the nearest medical facility are less than 10 min. | NHSS |
| Financial protection | ||
| Catastrophic healthcare expenditure | The proportion of households whose healthcare expenditure were at least 40% of the household non-food expenditure. | CHIP, RFPS |
| Medical impoverishment | The difference in the poverty headcount with and without out-of-pocket health spending included in household total consumption. Poverty line is defined as 2300 RMB per person-year in 2010 and it will be adjusted using the consumer price index for each year. | CHIP, RFPS |
Notes: NHSS = National Health Services Survey, including waves of 1993, 1998, 2003, 2008, 2013, and 2018 in our study; CHNS = China Health and Nutrition Survey, including waves of 1993, 1997, 2004, 2009, 2011, and 2015 six waves in our study; CHIP = Chinese Household Income Project, including waves of 1995, 2002, 2007, 2013, and 2018 in our study; RFPS = National Rural Fixed-Point Survey, including waves of 1995 and 2002 in our study; ANC4 = At least four antenatal care visits; BCG = Bacillus Calmette - Guerin vaccine; DPT3 = three doses of diphtheria, pertussis, and tetanus vaccine; Polio3 = three doses of polio vaccine; HB3 = three doses of Hepatitis B vaccine; DBP = diastolic blood pressure; SBP = systolic blood pressure; BMI = body-mass index; TB = tuberculosis.
The 12 treatment indicators are institutional delivery; skilled birth attendance; normal blood pressure; hypertension awareness; hypertension treatment; hypertension control; tuberculosis (TB) treatment; outpatient care seeking when needed; outpatient care seeking when needed for children aged 0 to 4; inpatient care seeking when needed; inpatient care seeking when needed for children aged 0 to 4; and travel time to the nearest medical facility. We did not include treatments for acute respiratory infection and diarrhea in our indicator list due to data availability. We also did not use inpatient admission in the previous 12 months as an indicator because of over-hospitalization was common in China.19 Instead, we used outpatient and inpatient care seeking when needed to reflect the general coverage of healthcare services. Outpatient and inpatient care seeking for the whole population were used to measure healthcare access and capacity, and outpatient and inpatient care seeking when needed for children aged 0 to 4 were used to measure the progress in the area of reproductive, maternal, newborn and child health (RMNCH), as shown in Appendix Table S1.
Catastrophic health expenditure (CHE) and medical impoverishment are two common indicators to measure financial protection in health. Consistent with existing literature, the incidence of CHE in our study was defined as the proportion of households whose healthcare expenditure was at least 40% of the non-food expenditure. This definition captures a household's ability to pay for health care and could produce comparable results with previous studies related to China.17,19 The incidence of medical impoverishment (MI) refers to the difference in the poverty headcount with and without out-of-pocket health spending included in household total consumption. We used 2300 RMB per person-year in 2010 as the poverty line and it was adjusted using the consumer price index for each year. This poverty line was consistent with the national poverty line set by the Chinese government in its anti-poverty campaign and the poverty line set by the World Bank (1.9 US Dollars per person-day in 2010). Supplementary notes in Appendix A shows details of the calculation of the two financial protection indicators.
There were some missing values for some indicators in our study. We thus tested differences in means of demographic and income variables between the full sample and the used sample in our study to examine whether missing data would be a threat for our study. We found no statistically significant differences (as shown in Appendix Table S2), suggesting that missing data in our study would not be a great concern in our study.
Statistical analysis
We estimated variable means with 95% confidence intervals (CIs) and used χ2 tests to test for statistical significance of differences between survey years. We used corresponding cross-sectional weights for each survey to ensure that our results were nationally representative when calculating financial protection indicators (more details in supplementary notes in Appendix A). As for service coverage indicators, we did not use cross-sectional weights in the calculation because NHSS and CHNS employed a multi-stage stratified cluster random sampling strategy to ensure national representativeness and information on weights were not available. Similar with previous studies,7,9,10 we used the meta-analysis to calculate the composite prevention index based on all prevention indicators, and the composite treatment index based on all treatment indicators. The advantage of meta-analysis compared with other methods was its transparency and repeatability.30 Considering means of some indicators in our study were close to the boundary line, we used random-effects meta-analysis on the basis of the Freeman-Tukey transformation method.31
In addition to examine the overall trends, we stratified data by urban/rural residence status and regions to examine inequalities of UHC indicators. We also constructed income quartiles by household income per capita to investigate changes in income-related inequality of UHC indicators. Specifically, we used the regression-based relative index of inequality (RII) to measure the income-related inequality of UHC indicators between poor and rich households for the years of 1993, 2008 and 2018 and examined changes during this period.32 The value of RII indicates changes in outcome from the poorest group to the richest group relative to the variable mean.
Furthermore, following the literature,7,9,10 we used a Bayesian linear regression model to predict trends for all indicators by 2030 and to estimate the probability of reaching the UHC targets of at least 80% coverage of essential services. We included the year as the covariate in the model with a non-informative prior, as shown in supplementary notes in Appendix A. We performed logit transformation on the proportion before the analysis, and all calculations were conducted as such and then transformed back to probabilities. Using two chains, we applied the Markov Chain Monte Carlo algorithm to obtain 1000 samples from the posterior distribution of the parameter of interest and the first 5000 iterations were discarded as burn-ins. A potential scale reduction factor in Gelman-Rubin diagnostic was used as a quantitative measure of convergence in addition to visual checks on the similarity of outputs from two chains.33 Bayesian models were developed in JAGS version 4.3.0 and implemented in R version 4.1.1.
Role of the funding source
The authors did not receive any specific funding for this study.
Results
Trends in service indicators
Table 2 reports the trends of UHC indicators between 1993 and 2018. During this period, the composite prevention index increased from 65.6% (95% CI: 52.1%–77.9%) to 87.7% (95% CI: 81.8%–92.6%) and the composite treatment index increased from 57.1% (95% CI: 43.5%–70.1%) to 75.5% (95% CI: 66.6%–83.5%). Almost all service coverage indicators experienced significant improvements between 1993 and 2018. For example, the coverage of ANC4, adequate sanitation, and institutional delivery increased by 70.3 percentage points (pp), 47.3 pp, and 59.9 pp, respectively. The shares of respondents seeking outpatient and inpatient care when needed also increased substantially. However, the share of population without overweight decreased from 79.6% (95% CI: 78.6%–80.5%) to 51.4% (95% CI: 50.3%–52.6%), and the proportion of population with normal blood pressure declined from 87.2% (95% CI: 86.5%–87.8%) to 64.0% (95% CI: 63.0%–65.0%).
Table 2.
Trends of UHC indicators between 1993 and 2018.
| Coverage (95% confidence interval) |
Difference |
|||||
|---|---|---|---|---|---|---|
| 1993–1995 | 2007–2009 | 2015–2018 | 1993–2008 | 2008–2018 | 1993–2018 | |
| Prevention indicators | ||||||
| ANC4 | 22.6 (22.1–23.0) | 65.8 (64.7–66.9) | 92.9 (92.4–93.4) | 43.2∗∗∗ | 27.1∗∗∗ | 70.3∗∗∗ |
| Postnatal care of mother | 46.0 (45.5–46.5) | 55.6 (54.5–56.7) | 74.6 (73.8–75.4) | 9.6∗∗∗ | 19.0∗∗∗ | 28.6∗∗∗ |
| BCG immunization | 88.1 (67.7–97.8)† | 98.8 (98.6–99.0) | 99.3 (98.3–99.8)† | 10.7∗∗∗ | 0.5∗ | 11.2∗∗∗ |
| DPT3 immunization | 81.6 (63.5–93.3)† | 90.7 (90.1–91.3) | 93.7 (88.5–96.8)† | 9.1∗∗∗ | 3.0∗∗∗ | 12.1∗∗∗ |
| Polio3 immunization | 83.0 (65.0–94.3)† | 92.4 (91.9–92.9) | 94.9 (89.9–97.7)† | 9.4∗∗∗ | 2.5∗∗∗ | 11.9∗∗∗ |
| Measles immunization | 83.0 (55.2–96.8)† | 92.1 (91.6–92.6) | 97.3 (92.9–99.3)† | 9.1∗∗∗ | 5.2∗∗∗ | 14.3∗∗∗ |
| HB3 immunization | 58.9 (23.8–86.6)† | 93.3 (92.8–93.8) | 96.5 (91.3–98.9)† | 34.4∗∗∗ | 3.2∗∗∗ | 37.6∗∗∗ |
| Non-use of tobacco | 70.8 (69.9–71.7) | 73.4 (72.6–74.3) | 76.5 (75.7–77.3) | 2.6∗∗∗ | 3.1∗∗∗ | 5.7∗∗∗ |
| Non-overweight | 79.6 (78.6–80.5) | 59.7 (58.6–60.7) | 51.4 (50.3–52.6) | −19.9∗∗∗ | −8.3∗∗∗ | −28.2∗∗∗ |
| Non-underweight | 91.7 (91.0–92.3) | 94.2 (93.7–94.7) | 95.3 (94.8–95.7) | 2.5∗∗∗ | 1.1∗∗∗ | 3.6∗∗∗ |
| Improved water | 43.2 (42.7–43.6) | 57.2 (56.8–57.6) | 77.9 (77.6–78.2) | 14.0∗∗∗ | 20.7∗∗∗ | 34.7∗∗∗ |
| Adequate sanitation | 21.2 (20.8–21.5) | 33.4 (33.0–33.8) | 68.5 (68.2–68.8) | 12.2∗∗∗ | 35.1∗∗∗ | 47.3∗∗∗ |
| Composite prevention index | 65.6 (52.1–77.9) | 78.8 (63.6–90.7) | 87.7 (81.8–92.6) | 13.2∗∗∗ | 8.9∗∗∗ | 22.1∗∗∗ |
| Treatment indicators | ||||||
| Institutional delivery | 38.7 (38.2–39.1) | 88.6 (87.9–89.3) | 98.6 (98.4–98.8) | 49.9∗∗∗ | 10.0∗∗∗ | 59.9∗∗∗ |
| Skilled birth attendance | 80.5 (80.2–80.9) | 91.9 (91.3–92.5) | 97.4 (94.7–98.9)† | 11.4∗∗∗ | 5.5∗∗∗ | 16.9∗∗∗ |
| Normal blood pressure | 87.2 (86.5–87.8) | 72.4 (71.5–73.2) | 64.0 (63.0–65.0) | −14.8∗∗∗ | −8.4∗∗∗ | −23.2∗∗∗ |
| Hypertension awareness | 31.0 (28.5–33.6) | 43.7 (41.9–45.5) | 44.7 (43.0–46.4) | 12.7∗∗∗ | 1.0 | 13.7∗∗∗ |
| Hypertension treatment | 17.0 (15.1–19.2) | 35.1 (33.4–36.9) | 36.8 (35.1–38.4) | 18.1∗∗∗ | 1.7 | 19.8∗∗∗ |
| Hypertension control | 5.6 (4.5–6.9) | 11.3 (10.2–12.5) | 11.8 (10.8–13.0) | 5.7∗∗∗ | 0.5 | 6.2∗∗∗ |
| Tuberculosis treatment | 59.4 (53.4–65.4) | 74.3 (67.0–81.5) | 90.6 (84.4–96.8) | 14.9∗∗∗ | 16.3∗∗∗ | 31.2∗∗∗ |
| Outpatient care seeking | 63.6 (63.1–64.1) | 62.4 (61.9–62.9) | 88.2 (88.0–88.4) | −1.2∗∗∗ | 25.8∗∗∗ | 24.6∗∗∗ |
| Outpatient care seeking (aged 0–4) | 80.3 (79.0–81.6) | 80.3 (78.5–82.1) | 85.8 (84.7–87.0) | 0.0 | 5.5∗∗∗ | 5.5∗∗∗ |
| Inpatient care seeking | 75.2 (74.3–76.0) | 76.8 (76.1–77.5) | 78.5 (78.1–78.9) | 1.6∗∗∗ | 1.7∗∗∗ | 3.3∗∗∗ |
| Inpatient care seeking (aged 0–4) | 83.0 (80.7–85.4) | 92.5 (90.4–94.6) | 90.6 (89.2–91.9) | 9.5∗∗∗ | −1.9 | 7.6∗∗∗ |
| Time to the nearest medical facility | 63.3 (50.8–74.2)† | 69.9 (69.5–70.3) | 81.7 (81.5–82.0) | 6.6∗∗∗ | 11.8∗∗∗ | 18.4∗∗∗ |
| Composite treatment index | 57.1 (43.5–70.1) | 68.0 (58.4–76.8) | 75.5 (66.6–83.5) | 10.9∗∗∗ | 7.5∗∗∗ | 18.4∗∗∗ |
| Financial protection | ||||||
| Catastrophic health expenditure | 3.5 (3.1–4.0) | 7.9 (7.4–8.5) | 3.6 (3.5–3.7) | 4.4∗∗∗ | −4.3∗∗∗ | 0.1 |
| Medical impoverishment | 1.4 (1.1–1.8) | 2.1 (1.8–2.4) | 1.9 (1.8–2.0) | 0.7∗∗∗ | −0.2 | 0.5∗∗∗ |
Notes: ∗∗∗, ∗∗, and ∗ denote the significance at the 1%, 5%, and 10% level, respectively. The results for immunization rates in 1993 and 2018, skilled birth attendance in 2018, and travel time to the nearest medical facility in 1993 were imputed using Bayesian linear regression. Hence, for these values, we used † to distinguish. In this table, NHSS included waves of 1993, 2008, and 2018, CHNS included waves of 1993, 2009, and 2015, and CHIP included waves of 1995, 2007, and 2018. ANC4 = At least four antenatal care visits; BCG = Bacillus Calmette - Guerin vaccine; DPT3 = three doses of diphtheria, pertussis, and tetanus vaccine; Polio3 = three doses of polio vaccine; HB3 = three doses of Hepatitis B vaccine. Composite prevention index and composite treatment index were computed using meta-analysis. Coverage of indicators in 1997–1998, 2002–2004, and 2011–2013 are presented in Appendix Table S3.
By the end of 2018, most prevention indicators had reached or been close to the target of 80% coverage. The coverages of BCG, DPT3, Polio3, Measles, and HB3 immunization exceeded 90%. The proportion of non-tobacco users and the coverage of improved water reached 76.5% (95% CI: 75.7%–77.3%) and 77.9% (95% CI: 77.6%–78.2%), respectively. Treatment indicators showed different patterns. The coverages of institutional delivery, skilled birth attendance, and TB treatment exceeded 90%. The proportion of respondents seeking outpatient and inpatient care when needed were around 80%. However, hypertension treatment and control were far below the target, though there were great improvements between 1993 and 2018. Of the 36.0% of the population that were hypertensive in 2018, only 44.7% (95% CI: 43.0%–46.4%) were aware of their hypertension, 36.8% (95% CI: 35.1%–38.4%) were under treatment and only 11.8% (95% CI: 10.8%–13.0%) were effectively controlled.
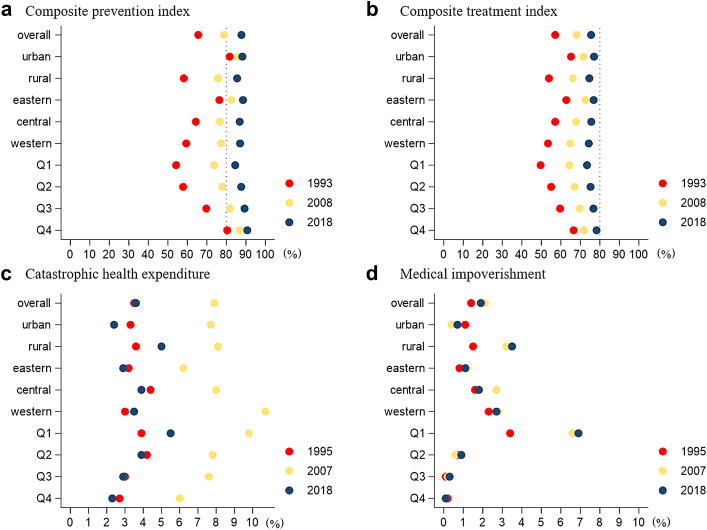
Fig. 1 further shows that the composite prevention and treatment indices varied by urban/rural areas, regions, and income quartiles within China. In the years of 1993, 2008, and 2018, urban areas always performed better in coverage of prevention and treatment services than rural areas. However, the urban-rural gaps had significantly narrowed during this period. In 1993, the urban-rural gaps in composite prevention and treatment indices were 23.5 pp and 11.3 pp, respectively, while their gaps had been reduced to 2.7 pp and 2.4 pp in 2018, as shown in Appendix Tables S4 and S5. The variations by regions presented a similar pattern. The eastern region always had better composite indices than the central and western regions, but their differences had largely shrunk during this period. The gaps between eastern and western regions in composite prevention and treatment indices were 17.0 pp and 9.4 pp in 1993, while these numbers declined to 1.5 pp and 2.5 pp in 2018. Fig. 1 also suggests that the income-related inequality experienced significant decline between 1993 and 2018. For example, the gap between the poorest and the richest income quartiles in the composite prevention was as large as 26.2 pp in 1993, while this number was only 6.2 pp in 2018.
Fig. 1.
Trends in service coverage and financial protection by various subgroups in China. Notes: Coverage of a. Composite prevention index, b. Composite treatment index, c. Catastrophic health expenditure, d. Medical impoverishment by urban/rural areas, regions and income quartiles. In Fig. 1a and b, red, yellow, and blue dots represent the years of 1993, 2008, and 2018, respectively. In Fig. 1c and d, red, yellow, and blue dots represent the years of 1995, 2007, and 2018, respectively. Q1–Q4 represents income quartiles from the poorest to the richest by household income per capita.
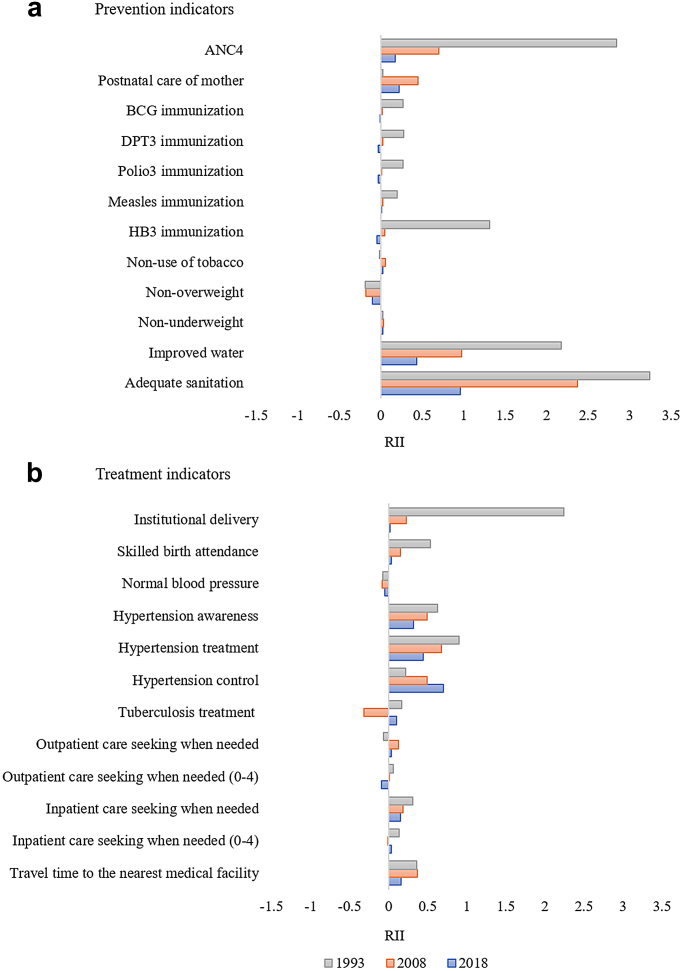
In addition, we measured income-related inequality for each service indicator using RII. Fig. 2 shows the RIIs for 24 service indicators in 1993, 2008, and 2018. RIIs for most indicators except non-overweight and normal blood pressure were positive, suggesting that the richer group had better coverage of these services in most cases. In 1993, adequate sanitation had the highest RII among 24 service coverage indicators, following by ANC4, improved water, institutional delivery, and HB3 immunization. The absolute value of RIIs for other service coverage indicators were less than 1.0 in 1993, as shown in Appendix Table S6. In 2018, the absolute value of RIIs for most indicators were no more than 1.0, suggesting narrowing income-related inequality in service coverage. The RIIs for ANC4, five immunization indicators, institutional delivery, skilled birth attendance were close to zero in 2018, suggesting that coverage of those services was almost not related to household income. In contrast, RIIs for hypertension-related indicators, improved water, and adequate sanitation were modestly larger, suggesting further direction in reducing income-related inequality.
Fig. 2.
Income inequality by relative inequality index (RII) for 24 service indicators from 1993 to 2018. Notes: a. RIIs for 12 prevention indicators; b. RIIs for 12 treatment indicators. ANC4 = At least four antenatal care visits; RII = relative index of inequality; BCG = Bacillus Calmette - Guerin vaccine; DPT3 = three doses of diphtheria, pertussis, and tetanus vaccine; Polio3 = three doses of polio vaccine; HB3 = three doses of Hepatitis B vaccine.
Trends in financial protection
The last two rows of Table 2 shows incidences of CHE and MI in selected waves between 1995 and 2018. The incidence of CHE increased from 1995 to 2007, and decreased afterwards. Specifically, CHE incidence measured by the 40% threshold increased from 3.5% (95% CI: 3.1%–4.0%) in 1995, to 5.6% (95% CI: 5.0%–6.2%) in 2002, and to 7.9% (95% CI: 7.4%–8.5%) in 2007. Then it decreased gradually to 5.1% (95% CI: 4.7%–5.5%) in 2013, and to 3.6% (95% CI: 3.5%–3.7%) in 2018, as show in Appendix Table S7. The differences from 1995 to 2007 and from 2007 to 2018 are all statistically significant (p-value < 0.0001), while the differences from 1995 to 2018 are not (p-value = 0.58). The incidence of MI showed a similar pattern during this period. It experienced an increase of 0.7 pp from 1995 to 2007 (p-value < 0.0001). Then it went down by 0.2 pp from 2007 to 2018 though this decrease was not statistically significant (p-value = 0.13).
Fig. 1c shows trends in CHE incidence for various subgroups, which were largely consistent with national statistics. The incidences of CHE in both urban and rural areas went up first between 1995 and 2007 and then went down afterwards. Trends by regions and income quartiles showed the same temporal trend during this period. In most survey years, urban area and eastern region had lower CHE incidence than their counterparts; the wealthiest quartile also had better financial protection than poorer quartiles. Fig. 1d show the trends in MI incidence for various subgroups. For most subgroups, their MI incidences experienced an increase between 1995 and 2007 and then stabilized without statistically significant changes between 2007 and 2018. One exception was the central region. Between 2007 and 2018, its MI incidence experienced a reduction of 0.9 pp (p-value < 0.0001), as shown in Appendix Table S8. Similar with findings on CHE incidence, in all survey years, we found large gaps in MI incidence between urban and rural areas, across regions, and by income quartiles. Subgroups in rural areas, in central and western region, and from poor quartiles were more vulnerable to medical impoverishment. Moreover, their gaps had not been significantly reduced during this period.
Projections of UHC indicators by 2030
We made projections of 24 healthcare service indicators, composite prevention index, and composite treatment index, using their trends between 1993 and 2018. Due to large fluctuations in CHE and medical impoverishment during this period, we could not make robust projections of financial protection and thus they were not included in the main result. In the sensitivity analysis, we used trends between 2007 and 2018 to make projections of CHE and MI by 2030.
Among prevention indicators, national coverage of ANC4 and five childhood vaccinations (BCG, DPT3, Polio3, Measles, and HB3) had already met the target by 2018. The proportion of non-underweight population also reached 95.3% (95% CI: 94.8%–95.7%) in 2018. For the rest of prevention indicators, most of them were projected to meet the target by 2030 if present trends continue, as shown in Table 3. Two exceptions are the proportion of non-overweight people and non-tobacco users. For the proportion of non-overweight population, its probability of target achievement by 2030 was almost zero. The projected proportion of non-tobacco users by 2030 was 78.9% (95% CrI: 74.7%–82.9%) and its probability of target achievement was only 21.5%. Moreover, it should be noted that the coverages of postnatal care and adequate sanitation were projected to slightly exceed 80%. However, there was still uncertainty in reaching the target for these two indicators because their target achievement probabilities were 54.7% and 66.2%, respectively.
Table 3.
Predicted coverage by 2025 and 2030, and the probability of reaching 80% target by 2030.
| Predicted coverage in year (95% credible interval) |
Probability of reaching 80% target by 2030 | ||
|---|---|---|---|
| 2025 | 2030 | ||
| Prevention indicators | |||
| ANC4 | 96.4 (94.2–98.0) | 98.2 (96.7–99.1) | 100.0 |
| Postnatal care of mother | 76.5 (66.9–84.7) | 80.1 (69.6–88.5) | 54.7 |
| BCG immunization | 99.6 (98.5–100.0) | 99.7 (98.7–100.0) | 100.0 |
| DPT3 immunization | 95.0 (87.3–98.6) | 95.6 (85.8–99.3) | 99.0 |
| Polio3 immunization | 96.0 (88.8–99.0) | 96.6 (88.5–99.4) | 99.2 |
| Measles immunization | 97.9 (91.0–99.8) | 98.1 (89.9–99.9) | 99.4 |
| HB3 immunization | 98.1 (93.0–99.7) | 98.7 (94.0–99.9) | 99.8 |
| Non-use of tobacco | 77.9 (74.5–81.3) | 78.9 (74.7–82.9) | 21.5 |
| Non-overweight | 36.3 (29.9–43.5) | 30.0 (23.1–38.2) | 0.0 |
| Non-underweight | 96.4 (94.8–97.5) | 96.8 (95.0–98.0) | 100.0 |
| Improved water | 83.7 (74.7–90.0) | 87.5 (78.3–93.2) | 95.2 |
| Adequate sanitation | 74.9 (62.0–85.2) | 81.7 (68.2–90.9) | 66.2 |
| Treatment indicators | |||
| Institutional delivery | 99.6 (99.2–99.8) | 99.8 (99.7–99.9) | 100.0 |
| Skilled birth attendance | 98.6 (96.5–99.6) | 99.1 (97.3–99.8) | 100.0 |
| Normal blood pressure | 52.5 (42.9–61.5) | 45.5 (34.4–56.6) | 0.0 |
| Hypertension awareness | 60.5 (43.8–75.1) | 65.4 (46.5–81.4) | 3.7 |
| Hypertension treatment | 58.0 (42.2–72.0) | 65.2 (46.5–79.8) | 2.5 |
| Hypertension control | 23.8 (12.8–38.1) | 29.2 (14.1–48.6) | 0.0 |
| Tuberculosis treatment | 91.6 (85.4–95.7) | 93.6 (87.4–97.3) | 99.9 |
| Outpatient care seeking when needed | 85.0 (72.3–93.2) | 87.7 (73.9–95.6) | 92.4 |
| Outpatient care seeking when needed (0–4) | 86.4 (80.0–91.7) | 87.3 (79.3–93.2) | 96.7 |
| Inpatient care seeking when needed | 82.3 (71.8–89.6) | 83.6 (71.2–91.6) | 80.7 |
| Inpatient care seeking when needed (0–4) | 94.1 (89.2–97.1) | 94.7 (89.1–97.9) | 100.0 |
| Travel time to the nearest medical facility | 82.0 (71.8–90.1) | 83.9 (71.9–92.4) | 80.9 |
Notes: Predicted coverage of prevention and treatment indicators and the probability of reaching 80% coverage target were estimated from Bayesian linear regression. ANC4 = At least four antenatal care visits; BCG = Bacillus Calmette - Guerin vaccine; DPT3 = three doses of diphtheria, pertussis, and tetanus vaccine; Polio3 = three doses of polio vaccine; HB3 = three doses of Hepatitis B vaccine. 95% credible intervals are reported in parentheses.
Similarly, most treatment indicators were projected to meet the target by 2030. The share of population with access to medical facility within 10 min was projected to increase from 81.7% (95% CI: 81.5%–82.0%) in 2018 to 83.9% (95% CrI: 71.9%–92.4%) in 2030, and its target achievement probability reached 80.9%. The proportions of population seeking outpatient and inpatient care when needed were projected to increase to 87.7% (95% CrI: 73.9%–95.6%) and 83.6% (95% CrI: 71.2%–91.6%) by 2030, respectively. However, target achievement probabilities for four hypertension indicators were all close to zero, suggesting great challenges in chronic disease management and control in China. Of the population with hypertension in 2030, only 65.4% (95% CrI: 46.5%–81.4%) were projected to be aware of their hypertension, 65.2% (95% CrI: 46.5%–79.8%) to be under treatment and only 29.2% (95% CrI: 14.1%–48.6%) to be effectively controlled.
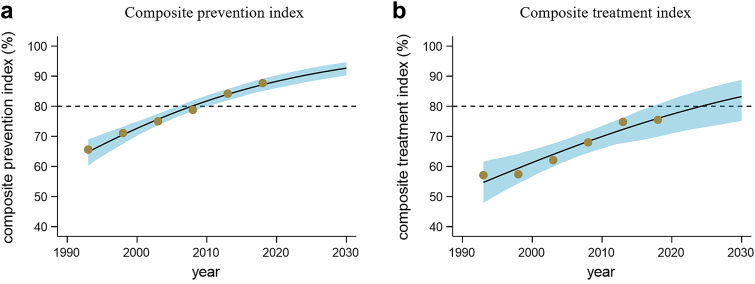
Fig. 3 shows results for projection of the composite prevention and treatment indices. By 2018, the composite prevention index had already exceeded 80% and it was projected to increase to 92.7% (95% CrI: 90.3%–94.7%) by 2030 if the current trend continues. Its target achievement probability was 100.0%. The composite treatment index was projected to increase from 75.5% (95% CI: 66.6%–83.5%) in 2018 to 83.2% (95% CrI: 75.1%–88.8%) in 2030. Its target achievement probability was 89.0%.
Fig. 3.
Projection of Composite prevention and treatmentindicesin China, 1993–2030. Notes: a. Predicted coverage of composite prevention index. b. Predicted coverage of composite treatment index. Brown dots represent the observed coverage from 1993 to 2018. The black line is the predicted coverage using Bayesian linear regression based on observed values. The shaded area represents the 95% credible interval from Bayesian linear regression. The dotted horizontal line is the 80% target.
Robustness tests and sensitivity analysis
First, the findings of this study rely on the linear assumption. To test this assumption, we used restricted cubic splines model with three knots and generalized additive model with three degrees of freedom to fit our logit-transformed observed data, and compared their adjusted R squares with that in the linear model. The Appendix Table S9 shows that the adjusted R squares of the linear model, splines model and generalized additive model are similar, suggesting the valid usage of the Bayesian linear model in our study. Furthermore, to further examine the validity of extrapolation, we made projections based on observed data from 1993 to 2008, and compared the predicted values with observed data. Appendix Table S10 suggests that differences in predicted and observed coverage are small for most indicators. Last, we made projections using the trends from 2003 and onwards, and their results are shown in Appendix Table S11. It shows that the probability of achieving 80% coverage target for most indicators remained unchanged. In addition, Appendix Table S11 shows that incidences of CHE and MI will decrease to 1.6% (95% CrI: 0.5%–4.0%) and 1.9% (95% CrI: 0.3%–6.4%), suggesting that attainment of 100% coverage of financial protection will be very challenging for China if there are no proper policy instruments.
Second, we conducted a sensitivity analysis to test whether inconsistencies in the timing of survey waves would have a great impact on our results and conclusions. Specifically, we made projections of CHNS indicators in 1998, 2003, 2008, 2013 and 2018, and combined these predicted data with observed data from NHSS to calculate the composite prevention and treatment indices. We presented the results of this sensitivity analysis in the Appendix Table S12. It shows that differences in the time of survey waves have limited impacts on our results and conclusions.
Third, we tested whether the composite prevention and treatment indices in the meta-analysis were driven by a small number of indicators. Specifically, we dropped an indicator every time and then calculated the composite prevention and treatment indices again to see whether the results would change substantially. As shown in Appendix Table S13, the values of composite prevention and treatment indices remained almost unchanged in this sensitivity test.
Fourth, following the existing literature,34 we applied multiplicity correction for primary outcomes to test the robustness of our study. Appendix Tables S14 and S15 provide the adjusted confidence intervals and they show that our main results for subgroup analyses remain unchanged.
Discussion
To the best of our knowledge, this study is the first attempt to systematically evaluate progress towards UHC in China using a wide range of indicators of healthcare service coverage and financial protection. We found that China had made laudable progress in healthcare service coverage between 1993 and 2018. Of the 12 prevention indicators and 12 treatment indicators used in this study, most of them experienced improvements during this period. By 2018, the composite prevention index had already exceeded 80% and the composite treatment index was close to the target of 80% coverage. Our projection suggested that China would be 100 percent sure to meet the UHC target in overall coverage of prevention services by 2030 and the probability of achieving the target in overall treatment coverage was close to 90%.
In areas of RMNCH, infectious diseases, and service capacity and access, China had made impressive progress. All indicators in these areas were projected to achieve the 80% coverage target by 2030. In 2018, the coverages of ANC4, skilled birth attendance, and institutional delivery in China exceeded 90%. The coverage of postnatal care for mother also reached 75%, which was on track to meet the UHC target. These results were consistent with previous findings.35,36 One review study found the maternal mortality rate, neonatal mortality rate, infant mortality rate and under-5 mortality rate during 1990–2019 showed a decreasing trend, along with an increasing hospital delivery rate, improved antenatal care, and better post-partum care.36 These achievements were largely attributable to the strong political will and community consensus within China.36 In addition, we observed significant improvements in infectious disease prevention and treatment indicators. Coverages of children vaccine immunization and tuberculosis treatment were nearly under universal coverage in 2018, and 77.9% and 68.5% of Chinese population had access to improved water and adequate sanitation. Last, China achieved great improvements in service capacity and access during this period, especially after the year of 2008. This progress was largely related to the complex and ambitious healthcare system reform plan in 2009, with the aim of providing all citizens with affordable and equitable basic healthcare.37 To achieve this goal, the Chinese government substantially increased fiscal investments in healthcare to strengthen infrastructure construction and to expand social health insurance. As a result, government health expenditure as a share of total health expenditure (THE) increased from 24.7% in 2008 to 30.4% in 2020 and the share of THE in total government expenditures rose from 5.7% to 8.4% during the same period.
However, progress in areas of chronic disease management and control was challenging and will be far below the 80% coverage target if existing trends continue. As shown in this study as well as in other featured studies, the prevalence of hypertension in China was growing rapidly, and rates of awareness, treatment and control stayed lower than those in developed countries.38,39 The status of diabetes showed a similar pattern in China, with an increasing prevalence, and low rates of awareness, treatment, and control.40 These results were partly attributable to the fact that the delivery system in China was hospital-centric, fragmented, and treatment-focused.19 The weak primary care system in China could not serve the needs of an ageing population with an increasing burden of non-communicable diseases. Therefore, China should restructure its delivery system and establish a primary-healthcare-based integrated delivery system. In addition, we find challenges in controlling tobacco and overweight in China, which are important risk factors for chronic diseases in China. As suggested in other studies, China should take more effective measures to combat the tobacco epidemic and obesity.41,42 Strong political will and leadership from the Chinese government are needed along with active participation of all related sectors in the Chinese society.
This study also found narrowing inequalities in healthcare service coverage. The rural-urban gaps had been substantially suppressed, though rural areas had lower coverage in 2018. The regional variations became smaller during the same period, given that the central and western region experienced larger improvements than the eastern region. Also, we found reduced income-related inequalities in most indicators. The poorest group experienced the largest increases in both composite prevention and treatment indices among the four income quartiles. For most prevention and treatment indicators, their RIIs in 2018 were smaller than those in 1993. These results were consistent with other studies, suggesting shrinking socioeconomic differences in healthcare use and outcomes in last decades.19,43
Financial protection was the other challenge for China in the progress towards UHC. We found rising incidences of CHE and MI between 1995 and 2007. This rising trend was largely attributable to the market-oriented healthcare reform and the collapse of social health insurance scheme since 1980s.44 When the Chinese government decided to expand social health insurance coverage and launch the healthcare reform after 2007, we observed improvements in financial protection. Even so, the status of financial protection in China was unsatisfactory compared to other countries. According to WHO and World Bank, the incidence of medical impoverishment in China ranked the 17th highest among 146 countries; the incidences of CHE using 10% and 25% thresholds in China ranked the 7th and the 3rd highest among approximately 160 countries, respectively.29 Households in rural areas, from central and western provinces, and in low-income groups were much more vulnerable to financial hardship due to out-of-pocket healthcare expenditure. Unaffordability of healthcare services was perceived to be one of top-three concerned social issues in China in 2018.45
Our study has several limitations. First, our projections are based on current trends and many factors would affect our results. On the one hand, the effect of COVID-19 on China's progress towards UHC is not considered in our study. The COVID-19 pandemic and the consequent slowdown of economic growth and social development may pose greater challenges for China in meeting the UHC targets. On the other hand, policies launched around and after 2018 could affect the current trends. For example, the health poverty alleviation project has significantly improved financial protection and decreased the incidence of CHE and MI in China.46 Hence, the projection results in our study should be treated with caution. Second, due to data availability, some critical indicators are not available such as breast and cervical cancer screening. As the trends in these indicators are similar with hypertension, the lack of these indicators may have limited impacts on our results but would influence the precision of the composition prevention and treatment indices. For example, according to the NHSS, cervical cancer screening rate increased from 24.3% in 2013 to 26.8% in 2018, and breast cancer screening rate was 26.5% in 2013 and 28.3% in 2018. These trends suggest that there are large rooms for improvement in chronic disease prevention and control in China. Last, we do not make projections of UHC indicators for subgroups because of wide credible intervals. Therefore, we cannot obtain the variations in probability of meeting UHC target across subgroups. These are important issues to be addressed in future research.
In conclusion, China has made great progress in healthcare service coverage, especially in the areas of RMNCH, infectious diseases, and service capacity and access in the past decades. Inequalities by rural/urban area, regions, and income quartiles have been substantially reduced. These achievements have laid a solid foundation for China in meeting the UHC targets by 2030. China has a 100% probability in meeting the UHC targets in the coverage of prevention services by 2030 and the probability of achieving the target in treatment service coverage is close to 90%. However, insufficient progress in NCD management and control is a challenge for China's progress towards UHC, and the performance of NCD indicators will be well below the 80% coverage target if current trends continue. Another challenge for China is the high incidences of CHE and MI, compared to other countries. Inequalities in financial protection remained large in 2018, suggesting that subgroups in rural areas, from central and western regions, and in poor quartiles were more vulnerable to financial hardship. China needs to develop effective policies to restructure its hospital-centered and fragmented delivery system and establish a primary-healthcare-based integrated delivery system. It will contribute to increase the efficiency in the health sector and contain the growth of healthcare expenditure. Provision of better financial protection for vulnerable groups should also be prioritized.
Contributors
HF contributed to the study design and conceptualization. YL, CZ, and PZ implemented the data analysis. YL and HF contributed to the methodology. HF and WY contributed to supervision and control. YL and HF wrote the original draft. HF, CZ, and WY revised and edited the draft. All authors discussed the results, contributed to revisions of the manuscript, and approved the final version.
Data sharing statement
We used four nationally representative household surveys in China: National Health Service Survey (NHSS), China Health Nutrition Survey (CHNS), Chinese Household Income Project (CHIP), and National Rural Fixed-Point Survey (RFPS). CHNS data and CHIP data are publicly available, while NHSS data and RFPS data are available upon requests. CHNS data files are available from https://www.cpc.unc.edu/projects/china. CHIP data files are available from http://www.ciidbnu.org/chip/. NHSS data can be obtained from the National Health Commission of the People's Republic of China. RFPS data can be obtained from the Research Center for Rural Economic in Ministry of Agriculture and Rural Affairs of the People's Republic of China.
Declaration of interests
The authors declare that they have no competing interests.
Acknowledgements
The authors would like to thank the seminar participants at Peking University for helpful comments.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2022.100646.
Appendix A. Supplementary data
References
- 1.United Nations Transforming our world: the 2030 agenda for sustainable development New York: Seventieth United Nations General Assembly. https://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E
- 2.World Health Organization Regional Office for the Western Pacific Universal health coverage: moving towards better health: action framework for the Western Pacific Region. http://iris.wpro.who.int/handle/10665.1/13371
- 3.Atun R., de Andrade L.O.M., Almeida G., et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385(9974):1230–1247. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization, World Bank . World Health Organization; Geneva: 2015. Tracking universal health coverage: first global monitoring report. [Google Scholar]
- 5.Wagstaff A., Neelsen S. A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study. Lancet Global Health. 2020;8(1):e39–e49. doi: 10.1016/S2214-109X(19)30463-2. [DOI] [PubMed] [Google Scholar]
- 6.Han S.M., Rahman M.M., Rahman M.S., et al. Progress towards universal health coverage in Myanmar: a national and subnational assessment. Lancet Global Health. 2018;6(9):e989–e997. doi: 10.1016/S2214-109X(18)30318-8. [DOI] [PubMed] [Google Scholar]
- 7.Rahman M.S., Rahman M.M., Gilmour S., Swe K.T., Krull Abe S., Shibuya K. Trends in, and projections of, indicators of universal health coverage in Bangladesh, 1995–2030: a Bayesian analysis of population-based household data. Lancet Global Health. 2018;6(1):e84–e94. doi: 10.1016/S2214-109X(17)30413-8. [DOI] [PubMed] [Google Scholar]
- 8.Nikoloski Z., McGuire A., Mossialos E. Evaluation of progress toward universal health coverage in Myanmar: a national and subnational analysis. PLoS Med. 2021;18(10) doi: 10.1371/journal.pmed.1003811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taniguchi H., Rahman M.M., Swe K.T., Hussain A., Shibuya K., Hashizume M. Trends and projections of universal health coverage indicators in Iraq, 2000–2030: a national and subnational study. Soc Sci Med. 2021;270 doi: 10.1016/j.socscimed.2020.113630. [DOI] [PubMed] [Google Scholar]
- 10.Zhang C., Rahman M.S., Rahman M.M., Yawson A.E., Shibuya K. Trends and projections of universal health coverage indicators in Ghana, 1995-2030: a national and subnational study. PLoS One. 2019;14(5) doi: 10.1371/journal.pone.0209126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tao W., Zeng Z., Dang H., et al. Towards universal health coverage: lessons from 10 years of healthcare reform in China. BMJ Global Health. 2020;5(3) doi: 10.1136/bmjgh-2019-002086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu X., Wang Z., Zhang H., Meng Q. Measuring and evaluating progress towards universal health coverage in China. Journal of global health. 2021;11 doi: 10.7189/jogh.11.08005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen M., Zhou G., Si L. Ten years of progress towards universal health coverage: has China achieved equitable healthcare financing? BMJ Global Health. 2020;5(11) doi: 10.1136/bmjgh-2020-003570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yip W., Hsiao W.C. The Chinese health system at a crossroads. Health Aff. 2008;27:460–468. doi: 10.1377/hlthaff.27.2.460. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization . World Health Organization; Geneva: 2000. The World Health Report 2000: health systems: improving performance. [Google Scholar]
- 16.Meng Q., Xu L., Zhang Y., et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 17.Ta Y., Zhu Y., Fu H. Trends in access to health services, financial protection and satisfaction between 2010 and 2016: has China achieved the goals of its health system reform? Soc Sci Med. 2020;245 doi: 10.1016/j.socscimed.2019.112715. [DOI] [PubMed] [Google Scholar]
- 18.Zhu Y., Li Y., Wu M., Fu H. How do Chinese people perceive their healthcare system? Trends and determinants of public satisfaction and perceived fairness, 2006–2019. BMC Health Serv Res. 2022;22(1):1–13. doi: 10.1186/s12913-021-07413-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yip W., Fu H., Chen A.T., et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–1204. doi: 10.1016/S0140-6736(19)32136-1. [DOI] [PubMed] [Google Scholar]
- 20.Wang M., Luo X., Xu S., et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7(1):35–45. doi: 10.1016/S2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 21.Popkin B.M., Du S., Zhai F., Zhang B. Cohort profile: the China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435–1440. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li S., Sato H., Sicular T. Cambridge University Press; 2013. Rising inequality in China: challenges to a harmonious society. [Google Scholar]
- 23.Gao Q., Yang S., Li S. Labor contracts and social insurance participation among migrant workers in China. China Econ Rev. 2012;23(4):1195–1205. [Google Scholar]
- 24.He G., Wang S. Do college graduates serving as village officials help rural China? Am Econ J Appl Econ. 2017;9(4):186–215. [Google Scholar]
- 25.Tian X., Yi F., Yu X. Rising cost of labor and transformations in grain production in China. China Agric Econ Rev. 2019;12(1):158–172. [Google Scholar]
- 26.Bai C.-E., Wu B. Health insurance and consumption: evidence from China's new cooperative medical scheme. J Comp Econ. 2014;42(2):450–469. [Google Scholar]
- 27.Ties B., Patrick E., David E., Tim E., Marie-Paule K., Adam W. Monitoring progress towards universal health coverage at country and global levels. PLoS Med. 2014;11(9) doi: 10.1371/journal.pmed.1001731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization, World Bank . World Health Organization; Geneva: 2017. Tracking universal health coverage: 2017 global monitoring report. [Google Scholar]
- 29.World Health Organization, World Bank . World Bank; Washington, DC: 2021. Tracking universal health coverage: 2021 global monitoring report. [Google Scholar]
- 30.Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. John Wiley & Sons; 2021. Introduction to meta-analysis. [Google Scholar]
- 31.Nyaga V.N., Arbyn M., Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Publ Health. 2014;72(1):1–10. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wagstaff A., O'Donnell O., Van Doorslaer E., Lindelow M. World Bank Publications; 2007. Analyzing health equity using household survey data: a guide to techniques and their implementation. [Google Scholar]
- 33.Gelman A., Carlin J.B., Stern H.S., Rubin D.B. Chapman and Hall/CRC; 1995. Bayesian data analysis. [Google Scholar]
- 34.Biran N., Ip A., Ahn J., et al. Tocilizumab among patients with COVID-19 in the intensive care unit: a multicentre observational study. Lancet Rheumatol. 2020;2(10):e603–e612. doi: 10.1016/S2665-9913(20)30277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liang J., Li X., Kang C., et al. Maternal mortality ratios in 2852 Chinese counties, 1996–2015, and achievement of millennium development goal 5 in China: a subnational analysis of the global burden of disease study 2016. Lancet. 2019;393(10168):241–252. doi: 10.1016/S0140-6736(18)31712-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qiao J., Wang Y., Li X., et al. A Lancet Commission on 70 years of women's reproductive, maternal, newborn, child, and adolescent health in China. Lancet. 2021;397:2497–2536. doi: 10.1016/S0140-6736(20)32708-2. [DOI] [PubMed] [Google Scholar]
- 37.Yip W.C.-M., Hsiao W.C., Chen W., Hu S., Ma J., Maynard A. Early appraisal of China's huge and complex health care reforms. Lancet. 2012;379:833–842. doi: 10.1016/S0140-6736(11)61880-1. [DOI] [PubMed] [Google Scholar]
- 38.Wang Z., Chen Z., Zhang L., et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 39.Lu J., Lu Y., Wang X., et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1. 7 million adults in a population-based screening study (China PEACE Million Persons Project) Lancet. 2017;390(10112):2549–2558. doi: 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 40.Wang L., Peng W., Zhao Z., et al. Prevalence and treatment of diabetes in China, 2013-2018. JAMA. 2021;326(24):2498–2506. doi: 10.1001/jama.2021.22208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang G., Wang Y., Wu Y., Yang J., Wan X. The road to effective tobacco control in China. Lancet. 2015;385(9972):1019–1028. doi: 10.1016/S0140-6736(15)60174-X. [DOI] [PubMed] [Google Scholar]
- 42.Wang Y., Zhao L., Gao L., Pan A., Xue H. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. 2021;9(7):446–461. doi: 10.1016/S2213-8587(21)00118-2. [DOI] [PubMed] [Google Scholar]
- 43.Levy M., Chen Y., Clarke R., et al. Socioeconomic differences in health-care use and outcomes for stroke and ischaemic heart disease in China during 2009–16: a prospective cohort study of 0. 5 million adults. Lancet Global Health. 2020;8(4):e591–e602. doi: 10.1016/S2214-109X(20)30078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blumenthal D., Hsiao W. Privatization and its discontents—the evolving Chinese health care system. N Engl J Med. 2005;353(11):1165–1170. doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 45.Zhang J., Ye X., Ge Y., Jin S., Zhu X. People's satisfaction on livelihood remains at high level - annual report on the people's livelihood survey in China. Manage World. 2019;35(10):1–10. (in Chinese) [Google Scholar]
- 46.Chen C., Pan J. The effect of the health poverty alleviation project on financial risk protection for rural residents: evidence from Chishui City, China. Int J Equity Health. 2019;18(1):1–16. doi: 10.1186/s12939-019-0982-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.