Abstract
Purpose
Refugees are vulnerable to psychiatric disorders because of risk factors linked to migration. Limited evidence exist on the impact of the neighbourhood in which refugee resettle. We examined whether resettling in a socioeconomically disadvantaged neighbourhood increased refugees’ risk of psychiatric disorders.
Methods
This register-based cohort study included 42,067 adults aged 18 years and older who came to Denmark as refugees during 1986-1998. Resettlement policies in those years assigned refugees in a quasi-random fashion to neighbourhoods across the country. A neighbourhood disadvantage index was constructed using neighbourhood-level data on income, education, unemployment, and welfare receipt. Main outcomes were psychiatric diagnoses and psychiatric medication usage ascertained from nationwide patient and prescription drug registers, with up to 30-year follow-up. Associations of neighbourhood disadvantage with post-migration risk of psychiatric disorders were examined using Cox proportional hazards and linear probability models adjusted for individual, family, and municipality characteristics.
Results
The cumulative risk of psychiatric diagnoses and medication was 13.7% and 46.1%, respectively. Refugees’ risk of psychiatric diagnoses and psychiatric medication usage was higher among individuals assigned to high-disadvantage compared with low-disadvantage neighbourhoods in analyses including fixed effects for assigned municipality (psychiatric diagnoses: hazard ratio (HR) = 1.14, 95% CI: 1.04, 1.25; psychiatric medication: HR = 1.05, 95% CI: 1.00, 1.11). Consistent results were found using linear probability models. Results for diagnostic categories and subclasses of medications suggested that the associations were driven by neurotic and stress-related disorders and use of anxiolytic medications.
Conclusion
Resettlement in highly disadvantaged neighbourhoods was associated with an increase in refugees’ risk of psychiatric disorders, suggesting that targeted placement of newly arrived refugees could benefit refugee mental health. The results contribute quasi-experimental evidence to support links between neighbourhood characteristics and health.
Keywords: Psychiatric disorders, mental health, neighbourhood disadvantage, refugees, quasi-experimental design
Introduction
Refugees living in Western countries have a higher risk of psychiatric disorders compared to the native population and non-refugee migrants [1-3]. In Denmark, the risk of psychiatric disorders in refugees compared to native Danes has been estimated to be 50% higher among women and twice as high among men [4]. In part, this is due to pre-migration and trans-migration traumatic experiences [5,6]. Additional, post-migration stressors, such as unemployment, limited social support, and barriers to accessing health and social services, have been found to have a pronounced effect on refugees’ mental health [5-8]. The extent to which refugees experience post-migration stressors may depend on the characteristics of the neighbourhood in which they resettle, although limited evidence exists on whether neighbourhood factors shape refugee mental health.
Only one prior study conducted in Sweden examined neighbourhood effects specifically on refugee mental health, finding no clear association with risk of depression and anxiety [9]. Reviews of studies in the general population of Western countries, suggest that living in disadvantaged neighbourhood environments is associated with increased risk of psychiatric disorders [10,11]. This evidence mainly comes from correlational observational studies, which provide inadequate policy guidance due to the potential of confounding bias, as poor pre-existing mental health may contribute to settlement in a disadvantaged neighbourhood and later mental health problems [12,13]. One randomized study, the Moving to Opportunity (MTO) experiment in the United States, showed mental health benefits for adults receiving a housing voucher allowing them to move out of high-poverty public housing developments to low-poverty neighbourhoods [14,15]. Neighbourhood environments may be particularly important for refugees, who constitute a population vulnerable to poor mental health outcomes [3]. Further evidence on neighbourhood effects on mental health for refugee populations is needed, particularly experimental or quasi-experimental evidence to overcome methodological problems with confounding.
In the present study we examined whether neighbourhood socioeconomic characteristics were associated with long-term risk of psychiatric disorders among adult refugees to Denmark. We used a quasi-experimental approach, taking advantage of a Danish dispersal policy during 1986-1998 that assigned incoming refugees to neighbourhoods across the country in an arbitrary or “quasi-random” fashion. We ascertained outcomes on psychiatric disorders in this population for up to three decades, employing unique national population and health register data. We tested the hypothesis that resettling in a socioeconomically disadvantaged neighbourhood was associated with an increased long-term risk of experiencing a psychiatric disorder.
Methods
Data sources
Data were drawn from several national registers that include the entire Danish population (Table 1). Individual-level data from different registers were linked using the unique identification number assigned to all Danish residents, including refugees when they obtain their residence permit [16]. Socio-demographic data were obtained from Statistics Denmark (the Danish census bureau) [17]. Data on psychiatric disorders were obtained from the Psychiatric Central Register, which contains information on admissions to psychiatric inpatient facilities since 1970 and information on contacts with psychiatric outpatient clinic and emergency services since 1995 [18]. In this register, disease diagnoses are based on the International Classification of Diseases, Eight Revision (ICD-8) through 1994 and subsequently on the Tenth Revision (ICD-10). Additional data on psychiatric disorders were drawn from the Prescription Drug Register, which contains information on drug prescriptions since 1995, including Anatomical Therapeutic Chemical (ATC) codes for purchased drugs [19].
Table 1.
Register data used in the study
| Data Element | Register | Years | Variables |
|---|---|---|---|
| Neighbourhood characteristics | Statistics Denmark registers | 1986-1998 | Income, unemployment, education, and welfare benefits at the parish level |
| Baseline characteristics of individuals | Statistics Denmark registers | 1986-1998 | Country of origin, year of arrival, age, sex, marital status, and number of children |
| Inpatient psychiatric hospital stays | Psychiatric Central Register | 1986-2019, February | ICD-8 and -10 and diagnosis dates |
| Contacts with outpatient psychiatric clinics and psychiatric emergency care units | Psychiatric Central Register | 1995-2019, February | ICD-8 and -10 and diagnosis dates |
| Prescription of psychiatric medications | Prescription Drug Register | 1995-2019, June | Anatomical Therapeutic Chemical codes and dates of prescription redemption |
Abbreviation: ICD International Classification of Diseases
Note: Due to changes in the reporting standards for the patient registers we had access to a shorter follow-up time for the Psychiatric Central Register than the Prescription Drug Register.
Danish Dispersal Policy
During 1986-1998, Denmark implemented a dispersal policy universally across the country for newly arrived refugees, which aimed to distribute the growing number of incoming refugees more evenly across counties and municipalities in proportion to the population size of each county and municipality [20]. Placement officers had access only to information on refugees’ age, marital status, family size, and nationality [21]. Therefore, neighbourhood placement was unlikely to be influenced by unobserved factors that typically confound studies of the relationship between neighbourhoods and health. Refugees were free to find their own residence, although official statistics suggest that at least 90% of incoming refugees were provided with a place of residence under the terms of the dispersal policy [22]. After resettlement, refugees were offered language courses and social welfare support lasting 18 months. Additionally, they were covered by a free universal healthcare system available to all Danish residents [23]. The policy resulted in an arbitrary or quasi-random assignment of incoming refugees to neighbourhoods with different levels of socioeconomic disadvantage. We leveraged the natural experiment created by this policy to estimate the associations of neighbourhood characteristics with refugee mental health outcomes. This empirical strategy has been used in previous studies, with analyses supporting the assumption of quasi-random neighbourhood assignment, conditional on the limited amount of pre-specified information on personal characteristics made available to placement officers [21,22,24,25]. The policy succeeded in changing the location patterns of refugees. The year before the policy was introduced refugees mainly lived in the population dense municipalities of Denmark, but the year after the policy ended, refugees where living in almost all Danish municipalities (Fig. S1). Importantly, the policy placed no restrictions on relocation, and welfare support was not conditional on staying in the assigned residence. The current study, which focused on estimating associations with the initial quasi-random neighbourhood assignment, therefore is akin to a randomized encouragement design, similar to the MTO trial.
Study population and sampling
The study population of refugees was defined using criteria similar to those developed in prior studies of the dispersal policy, as individual-level register data on refugee status is not available for this time period (Fig. 1) [24,22,25]. Immigrants included in the study had to have obtained a Danish residence permit between 1986-1998 and had to have arrived from one of the eight largest refugee-sending countries in the period: former Yugoslavia, Iraq, Iran, Afghanistan, Sri Lanka, Vietnam, Somalia, and Lebanon. Mainly Palestinians arrived from Lebanon. Residence permits granted to refugees from these countries accounted for 93% of the total 76,209 residence permits granted to refugees in the period (Table S1). Immigrants from former Yugoslavia who obtained residence permits before 1992 were excluded, as very few permits were granted to people from this area in the earlier years [26]. We also excluded individuals who were younger than 18 years old when they obtained their residence permit, and those who were married to someone already residing in Denmark. The latter were likely to have obtained a residence permit on the grounds of family reunification and therefore were not subject to the dispersal policy. The final analytic sample consisted of 42,067 individuals.
Fig. 1.
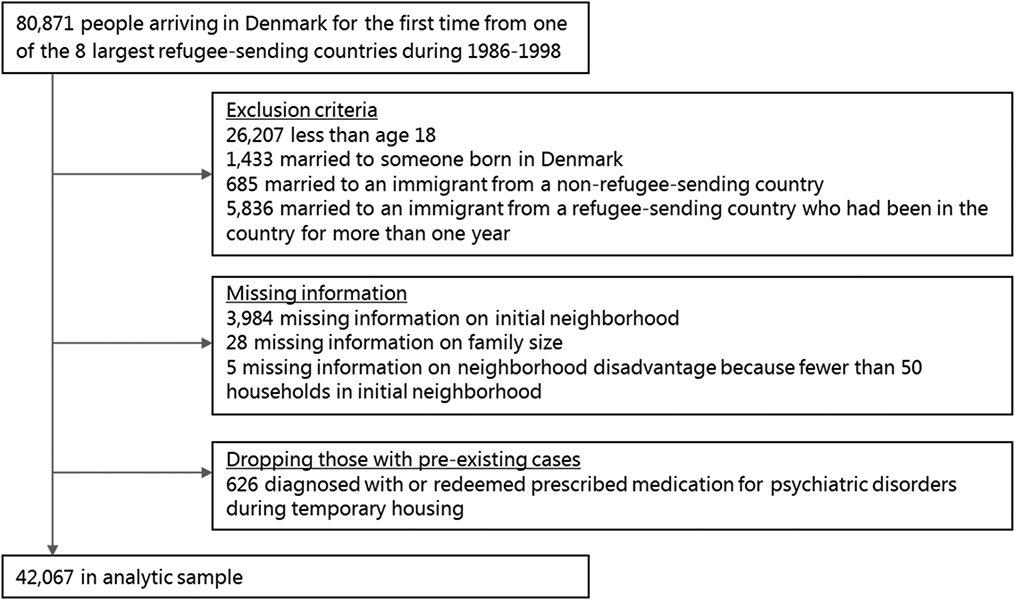
Flowchart
Measures
Outcomes
The primary outcomes were first-time psychiatric hospital contacts (inpatient, outpatient clinic, or emergency services) and first-time redemption of a prescription for psychiatric medication. Most medications registered in the Prescription Drug Register are prescribed by a general practitioner [19]. Thus, the prescription-related outcomes may reflect a psychiatric disorder that is being treated solely by a general practitioner and never diagnosed in a psychiatric hospital setting.
For first-time psychiatric hospital contacts, as in previous studies [27,4], we examined outcomes separately for the three most common diagnostic categories: schizophrenia and related disorders, mood disorders, and neurotic and stress-related disorders. We also included a composite variable representing one or more diagnoses in any of the above categories. For first-time redemption of a prescribed psychiatric medication, we examined the outcome separately for three subclasses of medications: antipsychotics, anxiolytics, and antidepressants. We also included a composite variable representing one or more redeemed prescriptions for medications in any of the above categories. Participants could receive more than one diagnosis or medication. Details on the specific ICD and ATC codes used in this study are available in the supplement (Table S2).
Exposure
The primary exposure was socioeconomic neighbourhood disadvantage in the initial neighbourhood assigned to refugees. Official records do not document the actual neighbourhood assigned by placement officials, and instead we used residential history data from the Danish registers to define the first neighbourhood of residence. Since refugees stayed in temporary housing in the country of assignment for 6-7 months on average [20], we considered the second location as the neighbourhood of assignment if the individual relocated to another neighbourhood within the county within one year of obtaining a residence permit. Otherwise, the first neighbourhood of residence recorded in the registers was defined as the neighbourhood of assignment. Refugees could refuse to live in the neighbourhood of assignment, in which case they were reassigned to a neighbourhood in another county. However, the reassignment rate was low and in most cases it took place after the initial move to the neighbourhood of assignment [20,21], which is the location we observe in the residential history data.
Neighbourhoods were defined based on parish borders. Parishes are the smallest geographical unit available in Danish registers and have been used to define neighbourhoods in prior work [28-30]. After excluding parishes with fewer than 50 family units, to avoid unstable statistical estimates and protect privacy, our data consisted of 2,097 parishes nested within 271 municipalities. Parishes differed in size from 0.1 to 159 km2 (median 16 km2) with populations ranging from 101 to 20,848 people (median 1,133 people).
We aggregated individual-level data for the total Danish population to the parish level for the period 1986-1998. Similar to previous studies, we created a socioeconomic neighbourhood disadvantage index based on neighbourhood-level indicators of income, education, employment, and welfare assistance [31,28,32]. To do so, we conducted principal component analysis that included four standardized variables: 1) median equivalized disposable family income, 2) median years of education among inhabitants aged 25-69 years, 3) percent of unemployed inhabitants aged 18-59 years, and 4) percent of families receiving welfare benefits. For each year we calculated a composite index value for all neighbourhoods using the variable loadings from the first principal component, i.e., the linear combination of variables that explained the largest amount of variance. Additional information is available in the supplement (Tables S3-S6 and Fig. S1).
To allow for non-linear relationships between the exposure and outcomes, we classified neighbourhoods by tertiles of disadvantage (low, moderate, and high) to achieve an equal number of individuals from the study population in each category.
Covariates
We adjusted for the characteristics available to placement officers. These included sex, age categories (18-24, 25-29, 30-34 years, etc.), country of origin, number of children (0, 1, 2, 3, ≥4), and marital status (married vs. unmarried). We additionally adjusted for fixed effects (i.e., indicator variables) for the year of placement, to account for secular trends. We further adjusted for fixed effects for initial municipality to strengthen the causal identification of the estimates by accounting for all time-invariant unobserved confounding factors at the municipality level. Such factors could for example be related to rural/urban areas, organization of and access to treatment, and geographical differences in health behaviors.
Statistical analysis
Characteristics of the study population at the time of placement and cumulative risk of psychiatric disorders were examined descriptively by looking at percentages by neighbourhood socioeconomic disadvantage level in the initial neighbourhood. We next estimated the association of neighbourhood disadvantage with each of the outcomes for psychiatric disorders using two sets of models: Cox proportional hazards and ordinary least squares (OLS) models.
First, we estimated Cox proportional hazards models, which have the advantage of accounting for time-to-event and censoring due to death or emigration. Participants were followed from the date of resettlement in the assigned neighbourhood until the first date of contact with a psychiatric service/first date of redeemed prescription of psychiatric medication, emigration, death or end of the study. The end of follow-up was February 2019 for clinical contacts with psychiatric services and June 2019 for redeeming a prescribed medication. Multivariable models were estimated adjusted for the covariates listed above and initial municipality was included as a strata variable. Thus, identification of neighbourhood estimates was based on differences in outcomes for refugees placed in neighbourhoods with different levels of disadvantage within the same municipality. The proportional hazard assumption was not found to be violated based on graphical inspections of scaled Schoenfeld residuals versus time.
Differential left censoring, due to differences in the years the outpatient, inpatient and prescription drug registers were established (Table 1), may possibly bias estimates from Cox models. Therefore, in secondary analyses we applied linear probability models (OLS models with a binary dependent variable) also adjusted for the covariates listed above and including fixed effects at the municipal level. Estimates from these models represent absolute effect measures and can be interpreted as a percentage-point difference in cumulative risk.
In subgroup analyses, we examined whether associations between neighbourhood disadvantage and psychiatric disorders differed by sex, age at placement, marital status, and presence of children by including interaction terms between these variables and level of neighbourhood socioeconomic disadvantage. Subgroup analyses were preformed using both Cox and linear probability models to examine interactions on a multiplicative and additive scale, respectively.
Finally, we conducted sensitivity analyses to test the robustness of the main estimates. To reduce the likelihood of capturing pre-existing cases, we analysed the data excluding all individuals who experienced one of the outcomes within the first two years of resettlement and those who died or emigrated within this period. Next, we excluded refugees from former Yugoslavia who in most cases were granted provisional asylum for up to two years, during which they were accommodated in special refugee centers across the country. Yugoslavs were also covered by a dispersal policy allowing placement in more rural parts of the country [26]. These special regulations may have resulted in different effects of the dispersal policy among refugees from former Yugoslavia.
In all analyses robust standard errors were clustered by municipality to account for correlated observations at the municipality level and nested levels such as neighbourhoods and families. All tests were 2-sided, and a P-value below 0.05 was considered statistically significant; 95% confidence intervals (CI) indicated precision of the estimates. The analyses were performed using the statistical software Stata version 16.
Results
Descriptive characteristics
In the study cohort of 42,067 adult refugees, nearly half were younger than 30 years of age at placement and 43.2% were women (Table 2). Three-fifths were married and 44.6% had children. The largest number arrived from former Yugoslavia (32.2%), Somalia (13.5%), Iraq (12.9%), or Iran (12.2%), or were Palestinians arriving mainly from Lebanon (12.3%).
Table 2.
Characteristics of the study population, overall and by tertile of neighbourhood socioeconomic disadvantage level
| Total | Neighbourhood disadvantage | ||||
|---|---|---|---|---|---|
| (n = 42,067) | Low (n = 13,517) |
Moderate (n = 14,270) |
High (n = 14,280) |
||
| n | % | % | % | % | |
| Panel A. Predictor variables | |||||
| Female | 18,155 | 43.2 | 41.7 | 43.9 | 43.9 |
| Married at resettlement | 25,220 | 60.0 | 57.5 | 62.0 | 60.3 |
| Age at resettlement (years) | |||||
| 18-24 | 10,664 | 25.4 | 26.1 | 23.7 | 26.3 |
| 25-29 | 9,176 | 21.8 | 22.2 | 21.1 | 22.2 |
| 30-34 | 6,876 | 16.4 | 16.2 | 16.6 | 16.3 |
| 35-39 | 4,715 | 11.2 | 11.3 | 11.9 | 10.4 |
| 40-44 | 2,933 | 7.0 | 6.8 | 7.4 | 6.8 |
| 45-49 | 1,836 | 4.4 | 4.2 | 4.5 | 4.3 |
| ≥50 | 5,867 | 14.0 | 13.3 | 14.9 | 13.7 |
| Number of children at resettlement | |||||
| 0 | 23,288 | 55.4 | 57.2 | 53.0 | 56.0 |
| 1 | 6,034 | 14.3 | 13.3 | 15.7 | 13.9 |
| 2 | 6,900 | 16.4 | 16.0 | 17.3 | 15.9 |
| 3 | 3,047 | 7.2 | 6.8 | 7.4 | 7.5 |
| ≥4 | 2,798 | 6.7 | 6.7 | 6.6 | 6.7 |
| Education at resettlement | |||||
| Basic education | 8,062 | 19.2 | 18.4 | 19.1 | 19.9 |
| Upper secondary education | 13,865 | 33.0 | 32.2 | 33.7 | 32.9 |
| Higher education | 7,501 | 17.8 | 17.9 | 17.7 | 18.0 |
| Unknown | 12,639 | 30.0 | 31.5 | 29.5 | 29.2 |
| Country of origin | |||||
| Former Yugoslavia | 13,551 | 32.2 | 28.2 | 39.2 | 29.1 |
| Somalia | 5,663 | 13.5 | 11.2 | 11.8 | 17.3 |
| Afghanistan | 947 | 2.3 | 2.6 | 2.0 | 2.2 |
| Sri Lanka | 3,479 | 8.3 | 9.0 | 9.6 | 6.2 |
| Iraq | 5,430 | 12.9 | 13.2 | 10.8 | 14.8 |
| Iran | 5,123 | 12.2 | 15.3 | 10.8 | 10.6 |
| Vietnam | 2,686 | 6.4 | 5.1 | 5.8 | 8.2 |
| Lebanon (Palestinians) | 5,188 | 12.3 | 15.6 | 10.1 | 11.5 |
| Panel B. Outcomes, cumulative risk | |||||
| Psychiatric diagnoses | |||||
| Schizophrenia and related disorders | 941 | 2.2 | 2.4 | 2.1 | 2.2 |
| Mood disorders | 2,633 | 6.3 | 6.0 | 6.2 | 6.5 |
| Neurotic and stress-related disorders | 4,529 | 10.8 | 10.6 | 10.9 | 10.9 |
| Any of the above | 5,749 | 13.7 | 13.4 | 13.8 | 13.8 |
| Psychiatric medication | |||||
| Antipsychotics | 7,584 | 18.0 | 18.0 | 18.5 | 17.6 |
| Antidepressants | 16,017 | 38.1 | 37.2 | 39.7 | 37.3 |
| Anxiolytics | 10,418 | 24.8 | 24.4 | 25.4 | 24.4 |
| Any of the above | 19,385 | 46.1 | 45.2 | 47.6 | 45.4 |
The characteristics of the study population by neighbourhood disadvantage levels appeared to be well balanced upon visual investigation for variables available to the placement officers and additionally for educational level, which was unobserved at the time of placement (Table 2). This supported the assumption of quasi-random assignment to neighbourhoods with different disadvantage levels. The imbalance observed for country of origin was likely driven by an increasing shortage of available housing in low-disadvantage areas over time. For example, refugees from Sri Lanka and Iran who arrived primarily at the beginning of the policy period (Table S1) were less likely to be assigned to neighbourhoods with a high level of disadvantage.
During the follow-up, 941 (2.2%) of the refugees were diagnosed with schizophrenia and related disorders, 2,633 (6.3%) with mood disorders, 4,529 (10.8%) with neurotic and stress-related disorders, and 5,749 (13.7%) with at least one diagnosis in any of these three diagnosis categories (Table 2). During the follow-up, 7,584 (18.0%) of the refugees were prescribed antipsychotics, 16,017 (38.1%) antidepressants, 10,418 (24.8%) anxiolytics, and 19,385 (46.1%) at least one of these categories of medication.
Neighbourhood disadvantage and psychiatric disorders
Assignment to high-disadvantage neighbourhoods was associated with a 14% higher hazard of any psychiatric diagnosis (HR: 1.14, 95% CI: 1.04, 1.25) compared to assignment to low-disadvantage neighbourhoods among refugees (Table 3). Looking at the individual diagnostic categories, an association was observed for neurotic and stress-related disorders such that refugees assigned to high-disadvantage neighbourhoods compared to low-disadvantage neighbourhoods had an increased hazard (HR: 1.14, 95% CI: 1.02, 1.28). No difference was seen for schizophrenia or mood disorders. All coefficients for moderate-disadvantage neighbourhoods compared to low-disadvantage neighbourhoods were statistically non-significant with confidence intervals including one.
Table 3.
Hazard ratios for the association of tertile of neighbourhood socioeconomic disadvantage level with psychiatric diagnoses and psychiatric medication
| Moderate disadvantage | High disadvantage | |
|---|---|---|
| Hazard ratio (95% CI) |
Hazard ratio (95% CI) |
|
| Psychiatric diagnoses | ||
| Schizophrenia and related disorders | 0.88 (0.76, 1.01) | 0.89 (0.74, 1.06) |
| Mood disorders | 0.97 (0.84, 1.12) | 1.07 (0.92, 1.24) |
| Neurotic and stress-related disorders | 1.05 (0.94, 1.17) | 1.14* (1.02, 1.28) |
| Any of the above | 1.02 (0.93, 1.13) | 1.14** (1.04, 1.25) |
| Psychiatric medication | ||
| Antipsychotics | 0.98 (0.89, 1.08) | 1.04 (0.95, 1.14) |
| Antidepressants | 1.01 (0.95, 1.07) | 1.05 (0.98, 1.12) |
| Anxiolytics | 0.99 (0.93, 1.06) | 1.07* (1.01, 1.14) |
| Any of the above | 1.00 (0.95, 1.06) | 1.05* (1.00, 1.11) |
p<0.05
p<0.01
Note: N = 42,067. Estimates are from Cox proportional hazards models with low-disadvantage neighbourhoods as the reference. All models are adjusted for age, sex, country of origin, number of children, marital status, year of resettlement, as well as strata for initial municipality.
For psychiatric medication, assignment to high-disadvantage neighbourhoods was associated with a 5% increased hazard of use of any psychiatric medication (HR: 1.05, 95% CI: 1.00, 1.11) compared to assignment to low-disadvantage neighbourhoods (Table 3). Looking at the subclasses of medications, an association was observed for anxiolytic use (HR: 1.07, 95% CI: 1.01, 1.14) among refugees assigned to high-disadvantage neighbourhoods, however, no association was observed for antipsychotic or antidepressant use. All coefficients for moderate-disadvantage neighbourhoods compared to low-disadvantage neighbourhoods were statistically non-significant with confidence intervals including one.
Results from analyses using linear probability models were consistent with the results from the primary analyses (Table 4). Assignment to high-disadvantage neighbourhoods compared to low-disadvantage neighbourhoods was associated with a 1.82 percentage point difference (95% CI: 0.61, 3.03) in the risk of any psychiatric diagnosis and a 2.18 percentage point difference (95% CI: 0.52, 3.84) in the risk of being prescribed any psychiatric medication.
Table 4.
Risk differences for the association of tertile of neighbourhood socioeconomic disadvantage level with psychiatric diagnoses and psychiatric medication
| Moderate disadvantage | High disadvantage | ||
|---|---|---|---|
| Number of eventsa |
Percentage-point difference (95% CI) |
Percentage-point difference (95% CI) |
|
| Psychiatric diagnoses | |||
| Schizophrenia and related disorders | 1,432 | −0.22 (−0.72, 0.27) | −0.16 (−0.77, 0.45) |
| Mood disorders | 3,431 | −0.10 (−1.10, 0.89) | 0.36 (−0.61, 1.34) |
| Neurotic and stress-related disorders | 5,937 | 0.34 (−0.87, 1.55) | 1.39* (0.08, 2.71) |
| Any of the above | 7,546 | 0.39 (−0.97, 1.74) | 1.82** (0.61, 3.03) |
| Psychiatric medication | |||
| Antipsychotics | 9,583 | 0.28 (−1.26, 1.81) | 1.09 (−0.18, 2.36) |
| Antidepressants | 19,432 | 0.47 (−1.14, 2.08) | 1.54 (−0.24, 3.33) |
| Anxiolytics | 12,275 | 0.31 (−0.95, 1.57) | 1.96** (0.71, 3.21) |
| Any of the above | 23,269 | 0.38 (−1.30, 2.05) | 2.18* (0.52, 3.84) |
p<0.05
p<0.01
The number of events in these analyses differ from the numbers shown in Table 1 due to no censoring if leaving the country.
Note: N = 42,067. Estimates are from linear probability models with low-disadvantage neighbourhoods as the reference. All models are adjusted for age, sex, country of origin, number of children, marital status, year of resettlement, and fixed effects for initial municipality.
Subgroup analyses
The association of high neighbourhood disadvantage with psychiatric diagnoses and psychiatric medication did not differ by sex, marital status, children, or age at the time of placement (Table S7-S10).
Sensitivity analyses
Excluding study participants who experienced one of the outcomes within two years of neighbourhood assignment (N = 34,011) did not alter the findings (Table S11). After excluding refugees from former Yugoslavia (N = 28,516), results were similar albeit less precisely estimated for the association of high neighbourhood disadvantage with any psychiatric diagnosis (HR: 1.11, 95% CI: 0.99, 1.26) as well as use of anxiolytics (HR: 1.07, 95% CI: 0.99, 1.15) and use of any psychiatric medication (HR: 1.08, 95% CI: 1.01, 1.17) (Table S12). A larger attenuation was seen for the association of high neighbourhood disadvantage with neurotic and stress-related disorders (HR: 1.08, 95% CI: 0.93, 1.25). Finally, the association of high neighbourhood disadvantage with antidepressant became statistically significant (HR: 1.12, 95% CI: 1.02, 1.22).
Discussion
This study leveraged a natural experiment in which refugees were quasi-randomly assigned to neighbourhoods with different levels of disadvantage, yielding new evidence on the association of neighbourhood factors with long-term psychiatric disorders. Consistent with our hypothesis, resettling in a socioeconomically disadvantaged neighbourhood was associated with an increased long-term risk of being diagnosed with a psychiatric disorder or being prescribed psychiatric medication among refugees. Results were consistent using both Cox proportional hazards models and linear probability models. The estimated associations from the primary analysis represented a 14% increase in the risk of a psychiatric diagnosis and a 5% increase in the risk of psychiatric medication on average during follow-up for refugees in high-disadvantage compared with low-disadvantage neighbourhoods. Although the magnitude of these effect sizes is modest at the individual level, it is potentially important at a population level [33]. Additionally, refugees to Denmark were provided with generous welfare benefits and universal healthcare coverage and larger associations may be seen in settings such as the U.S. with a weaker safety net for vulnerable groups [34,35]. The duration of exposure to high-disadvantage neighbourhoods is also likely to affect the strength of the association, but because the dispersal policy put no restriction on relocation, the length of exposure for each individual differed. Half of the study sample left the quasi-randomly assigned neighbourhood within the first five years after resettlement, and if refugees moved from disadvantaged to advantaged neighbourhoods it may have weakened the estimated associations. Importantly, movements to neighbourhoods with other levels of disadvantage did not bias our results, as these moves represent mediators rather than confounders.
When studying diagnostic categories and subclasses of medication we found that effect estimates were strongest and most precise for neurotic and stress-related disorders and use of anxiolytic medications suggesting that neighbourhood effects may be particularly salient for anxiety symptoms. However, the results for the other two subgroups of psychiatric diagnosis, schizophrenia and mood disorders, may have been affected by limited power to detect an association. Additionally, for the other two subgroups of psychiatric medication, antipsychotics and antidepressants, there was an increased risk for those placed in disadvantaged neighbourhoods, although confidence intervals were wide. Further research is needed to identify if associations between neighbourhood disadvantage and psychiatric disorders differ depending on the type of disorder.
Several mediating pathways may explain our findings of an association between resettling in a disadvantaged neighbourhood and increased long-term risk of psychiatric disorders. Neighbourhood socioeconomic disadvantage could increase exposure to neighbourhood disorder, crime, noise, and lack of amenities. These conditions can function as stressors that influence secondary mechanisms such as sense of control, mistrust, sleep deprivation, and substance use [36,37]. People in disadvantaged neighbourhoods also may experience a lack of social support and cohesion making them more vulnerable to mental health issues. Employment and economic opportunities may also mediate the association between neighbourhood disadvantage and psychiatric disorders [36], although earlier studies on the Danish refugee dispersal policy and the MTO experiment found no relationship between neighbourhood disadvantage and labour market outcomes [21,14]. The association between initial neighbourhood placement and psychiatric disorders found in this study may additionally be mediated by later neighbourhood disadvantage, as previous research on the Danish refugee dispersal policy has shown that assignment to a disadvantaged neighbourhood increased the probability of moving to another disadvantaged neighbourhood [21].
Our results are inconsistent with one prior quasi-experimental study from Sweden that used a similar refugee dispersal policy to examine the association between socioeconomic neighbourhood disadvantage and depression/anxiety [9]. In that study, refugees in high-disadvantage neighbourhoods had lower rates of depression/anxiety (HR: 0.96, 95% CI: 0.92, 1.00), although as stated by the authors “estimates were close to the null and thus susceptible to being explained by small amounts of bias” [9]. Analyses in that study were limited by incomplete access to data on treatment for depression/anxiety in a larger part of the follow-up period than the current study, which may have influenced the results [9]. Two Swedish correlational observational studies in the general population found that living in neighbourhoods with high socioeconomic disadvantage was associated with an increased risk of psychiatric hospital admission and psychiatric medication prescriptions, independent of individual-level socio-demographic characteristics [38,39]. Whereas these findings were consistent with our results, the two studies also identified a gradient effect between socioeconomic neighbourhood disadvantage and risk of psychiatric disorders. In contrast, we found no difference in risk of the outcomes when comparing assignment to moderate- and low-disadvantage neighbourhoods. This discrepancy may be due to bias in the observational studies in Sweden, true differences in the gradient of effects of neighbourhood disadvantage between Sweden and Denmark, or insufficient power in the current study to detect a gradient. The current study included parameters for all 271 municipalities in our statistical models (i.e., municipality fixed effects), which reduced precision of estimates.
Strengths of this study included use of a natural experiment to strengthen causal inferences and comprehensive longitudinal data on the entire population allowing us to study outcomes up to three decades after resettlement. Using a quasi-experimental design allowed us to limit the mechanisms of selective residential mobility and obtain more rigorous estimates of the implications of social causation on the association between neighbourhood disadvantage and mental health [40,41].
This study also had several limitations. First, the results may not be generalizable to non-refugees or to refugees settling in other countries with less welfare assistance and without universal healthcare. Second, refugees in the current study arrived in Denmark between 1986 and 1998, and results may be less relevant for newly arrived refugees due to potential cohort effects. Third, data on the type of residence permits given to immigrants in the study period was not available and we therefore used criteria’s developed in previous studies to define our study population of refugees [22,25]. Consequently, there is a chance of misclassification. Fourth, the Danish register data include information on neighbourhood of residence rather than neighbourhood assigned and although official statistics suggest adherence of over 90% to the dispersal policy [22], there may nevertheless be some bias in the resulting estimates by including study respondents who did not adhere to the quasi-experimental design. Fifth, until 1995 outcome data were available only for inpatient psychiatric hospital contacts. For that reason, we could not identify individuals in the study population using outpatient services or redeeming prescriptions for medication before 1995. If refugees placed in low disadvantage neighbourhoods were more likely to receive such treatments before that year, this could bias our results towards the null. Sixth, we had limited ability to exclude people with existing psychiatric disorders at the time of neighbourhood placement. However, if pre-existing cases were randomly distributed across neighbourhoods, as we would expect, it should not bias our results, and a sensitivity analysis excluding those with diagnoses in the first two years after resettlement demonstrated results similar to our primary models. Finally, many people with serious psychiatric conditions do not receive care, and undertreatment may be particularly common for refugees [42]. If undertreatments were more severe in disadvantaged neighbourhoods, our findings would be conservative.
Conclusions
This study is among the first to examine the association of neighbourhood disadvantage with risk of psychiatric disorders among refugees using a quasi-experimental design. Our results show that resettlement in highly disadvantaged neighbourhoods was associated with an increased risk of psychiatric disorders among refugees. This suggest that targeted placement of newly arrived refugees in less disadvantaged neighbourhoods and efforts to reduce neighbourhood-level socioeconomic disadvantage may improve mental health in this population. Promoting the health and wellbeing of one of the most vulnerable populations in society also may contribute to integration efforts. Future studies could examine which specific neighbourhood factors are most important and examine potential pathways for investing community resources and facilitating development of targeted community interventions.
Supplementary Material
Funding:
This work was supported by the National Institute on Aging of the National Institutes of Health, Award Number R01AG063385.
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Availability of data and material: Data cannot be shared publicly because access to micro data from Danish registers require approval from Statistics Denmark. Information on the rules and the organizational framework for researcher’s access to micro data from Danish registers can be found here: dst.dk/en/TilSalg/Forskningsservice
Ethics approval: This study was approved by the Danish Data Protection Agency (record number 2016-051). Registry-based studies do not require ethical board approval in Denmark, and the data were analysed anonymously. As a result, participant consent was not obtained.
Reference
- 1.Henkelmann JR, de Best S, Deckers C, Jensen K, Shahab M, Elzinga B, Molendijk M (2020) Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych open 6 (4):e68. doi: 10.1192/bjo.2020.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fazel M, Wheeler J, Danesh J (2005) Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The Lancet 365 (9467):1309–1314. doi: 10.1016/S0140-6736(05)61027-6 [DOI] [PubMed] [Google Scholar]
- 3.Lindert J, Ehrenstein OSv, Priebe S, Mielck A, Brähler E (2009) Depression and anxiety in labor migrants and refugees – A systematic review and meta-analysis. Social Science & Medicine 69 (2):246–257. doi: 10.1016/j.socscimed.2009.04.032 [DOI] [PubMed] [Google Scholar]
- 4.Norredam M, Garcia-Lopez A, Keiding N, Krasnik A (2009) Risk of mental disorders in refugees and native Danes: a register-based retrospective cohort study. Social Psychiatry and Psychiatric Epidemiology 44 (12):1023. doi: 10.1007/s00127-009-0024-6 [DOI] [PubMed] [Google Scholar]
- 5.Bogic M, Njoku A, Priebe S (2015) Long-term mental health of war-refugees: a systematic literature review. BMC International Health and Human Rights 15 (1):29. doi: 10.1186/s12914-015-0064-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller KE, Rasmussen A (2017) The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiol Psychiatr Sci 26 (2):129–138. doi: 10.1017/S2045796016000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jannesari S, Hatch S, Prina M, Oram S (2020) Post-migration Social–Environmental Factors Associated with Mental Health Problems Among Asylum Seekers: A Systematic Review. Journal of Immigrant and Minority Health 22 (5):1055–1064. doi: 10.1007/s10903-020-01025-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen W, Hall BJ, Ling L, Renzaho AMN (2017) Pre-migration and post-migration factors associated with mental health in humanitarian migrants in Australia and the moderation effect of post-migration stressors: findings from the first wave data of the BNLA cohort study. The Lancet Psychiatry 4 (3):218–229. doi: 10.1016/S2215-0366(17)30032-9 [DOI] [PubMed] [Google Scholar]
- 9.Raphael E, White JS, Li X, Cederin K, Glymour MM, Sundquist K, Sundquist J, Hamad R (2020) Neighborhood deprivation and mental health among immigrants to Sweden. Epidemiology 31 (3). doi: 10.1097/ede.0000000000001160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Truong KD, Ma S (2006) A Systematic Review of Relations between Neighborhoods and Mental Health. Journal of Mental Health Policy and Economics 9 (3):137–154 [PubMed] [Google Scholar]
- 11.Richardson R, Westley T, Gariépy G, Austin N, Nandi A (2015) Neighborhood socioeconomic conditions and depression: a systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology 50 (11):1641–1656. doi: 10.1007/s00127-015-1092-4 [DOI] [PubMed] [Google Scholar]
- 12.Oakes JM (2004) The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Social Science & Medicine 58 (10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004 [DOI] [PubMed] [Google Scholar]
- 13.Mair C, Roux AVD, Galea S (2008) Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health 62 (11):940–946. doi: 10.1136/jech.2007.066605 [DOI] [PubMed] [Google Scholar]
- 14.Kling JR, Liebman JB, Katz LF (2007) Experimental Analysis of Neighborhood Effects. Econometrica 75 (1):83–119. doi: 10.1111/j.1468-0262.2007.00733.x [DOI] [Google Scholar]
- 15.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, Sanbonmatsu L (2012) Neighborhood Effects on the Long-Term Well-Being of Low-Income Adults. Science 337 (6101):1505–1510. doi: 10.1126/science.1224648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmidt M, Pedersen L, Sørensen HT (2014) The Danish Civil Registration System as a tool in epidemiology. European Journal of Epidemiology 29 (8):541–549. doi: 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 17.Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H (2011) Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scandinavian Journal of Public Health 39 (7_suppl):12–16. doi: 10.1177/1403494811399956 [DOI] [PubMed] [Google Scholar]
- 18.Mors O, Perto GP, Mortensen PB (2011) The Danish Psychiatric Central Research Register. Scand J Public Health 39 (7_suppl):54–57. doi: 10.1177/1403494810395825 [DOI] [PubMed] [Google Scholar]
- 19.Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M (2016) Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol 46 (3):798–798f. doi: 10.1093/ije/dyw213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Damm AP (2005) The Danish Dispersal Policy on Refugee Immigrants 1986-1998: A Natural Experiment? Working Paper 05–03. Department of Economics, Aarhus School of Business, [Google Scholar]
- 21.Damm AP (2014) Neighborhood quality and labor market outcomes: Evidence from quasi-random neighborhood assignment of immigrants. Journal of Urban Economics 79:139–166. doi: 10.1016/j.jue.2013.08.004 [DOI] [Google Scholar]
- 22.Damm AP (2009) Ethnic Enclaves and Immigrant Labor Market Outcomes: Quasi Experimental Evidence. Journal of Labor Economics 27 (2):281–314. doi: 10.1086/599336 [DOI] [Google Scholar]
- 23.Schmidt M, Schmidt SAJ, Adelborg K, Sundboll J, Laugesen K, Ehrenstein V, Sorensen HT (2019) The Danish health care system and epidemiological research: from health care contacts to database records. Clinical epidemiology 11:563–591. doi: 10.2147/clep.s179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamad R, Öztürk B, Foverskov E, Pedersen L, Sørensen HT, Bøtker HE, White JS (2020) Association of Neighborhood Disadvantage With Cardiovascular Risk Factors and Events Among Refugees in Denmark. JAMA Network Open 3 (8):e2014196–e2014196. doi: 10.1001/jamanetworkopen.2020.14196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Damm AP, Dustmann C (2014) Does Growing Up in a High Crime Neighborhood Affect Youth Criminal Behavior? The American Economic Review 104 (6):1806–1832 [Google Scholar]
- 26.Ankestyrelsen (2014) Bosniske krigsflygtninge fra medio 90’erne: Fakta om integration, 2014 [Bosnian war refugees from the mid-90s: Facts about integration, 2014]. Copenhagen: Ankestyrelsen. [Google Scholar]
- 27.Hvidtfeldt C, Petersen JH, Norredam M (2019) Prolonged periods of waiting for an asylum decision and the risk of psychiatric diagnoses: a 22-year longitudinal cohort study from Denmark. International Journal of Epidemiology 49 (2):400–409. doi: 10.1093/ije/dyz091 [DOI] [PubMed] [Google Scholar]
- 28.Meijer M, Engholm G, Grittner U, Bloomfield K (2013) A socioeconomic deprivation index for small areas in Denmark. Scandinavian Journal of Public Health 41 (6):560–569. doi: 10.1177/1403494813483937 [DOI] [PubMed] [Google Scholar]
- 29.Schofield P, Thygesen M, Das-Munshi J, Becares L, Cantor-Graae E, Pedersen C, Agerbo E (2017) Ethnic density, urbanicity and psychosis risk for migrant groups – A population cohort study. Schizophrenia Research 190:82–87. doi: 10.1016/j.schres.2017.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meijer M, Mette Kejs A, Stock C, Bloomfield K, Ejstrud B, Schlattmann P (2012) Population density, socioeconomic environment and all-cause mortality: A multilevel survival analysis of 2.7 million individuals in Denmark. Health & Place 18 (2):391–399. doi: 10.1016/j.healthplace.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 31.White JS, Hamad R, Li X, Basu S, Ohlsson H, Sundquist J, Sundquist K (2016) Long-term effects of neighbourhood deprivation on diabetes risk: quasi-experimental evidence from a refugee dispersal policy in Sweden. The Lancet Diabetes & Endocrinology 4 (6):517–524. doi: 10.1016/S2213-8587(16)30009-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allik M, Leyland A, Travassos Ichihara MY, Dundas R (2020) Creating small-area deprivation indices: a guide for stages and options. J Epidemiol Community Health 74 (1):20–25. doi: 10.1136/jech-2019-213255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Normman GR (2002) Methods to explain the clinical significance of health status measures. Mayo Clinic Proceedings 77 (4):371–383 [DOI] [PubMed] [Google Scholar]
- 34.MacFarlan M, Oxley H (1996) Social transfers: spending patterns, institutional arrangements and policy responses. OECD Economic Studies No. 27. doi:doi: 10.1787/eco_studies-v1997-1-en [DOI] [Google Scholar]
- 35.Heckman J, Landersø R (2021) Lessons for Americans from Denmark about inequality and social mobility. Labour Economics:101999. doi: 10.1016/j.labeco.2021.101999 [DOI] [Google Scholar]
- 36.Hill TD, Maimon D (2013) Neighborhood Context and Mental Health. In: Aneshensel CS, Phelan JC, Bierman A (eds) Handbook of the Sociology of Mental Health. Springer Netherlands, Dordrecht, pp 479–501. doi: 10.1007/978-94-007-4276-5_23 [DOI] [Google Scholar]
- 37.Blair A, Ross NA, Gariepy G, Schmitz N (2014) How do neighborhoods affect depression outcomes? A realist review and a call for the examination of causal pathways. Social Psychiatry and Psychiatric Epidemiology 49 (6):873–887. doi: 10.1007/s00127-013-0810-z [DOI] [PubMed] [Google Scholar]
- 38.Sundquist K, Ahlen H (2006) Neighbourhood income and mental health: A multilevel follow-up study of psychiatric hospital admissions among 4.5 million women and men. Health & Place 12 (4):594–602. doi: 10.1016/j.healthplace.2005.08.011 [DOI] [PubMed] [Google Scholar]
- 39.Crump C, Sundquist K, Sundquist J, Winkleby MA (2011) Neighborhood Deprivation and Psychiatric Medication Prescription: A Swedish National Multilevel Study. Annals of Epidemiology 21 (4):231–237. doi: 10.1016/j.annepidem.2011.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caspi A (2002) Social selection, social causation, and developmental pathways: empirical strategies for better understanding how individuals and environments are linked across the life-course. In: Caspi A, Pulkkinen L (eds) Paths to Successful Development: Personality in the Life Course. Cambridge University Press, Cambridge, pp 281–301. doi: 10.1017/CBO9780511489761.012 [DOI] [Google Scholar]
- 41.Schmidt NM, Nguyen QC, Osypuk TL (2018) Experimental and Quasi-Experimental Designs in Neighborhood Health Effects Research: Strengthening Causal Inference and Promoting Translation. In: Neighborhoods and Health. 2 edn. Oxford University Press, New York. doi: 10.1093/oso/9780190843496.003.0006 [DOI] [Google Scholar]
- 42.de Montgomery CJ, Petersen JH, Jervelund SS (2020) Psychiatric healthcare utilisation among refugee adolescents and their peers in Denmark. Social Psychiatry and Psychiatric Epidemiology 55 (11):1457–1468. doi: 10.1007/s00127-020-01878-w [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


