Abstract
Introduction:
Burn patients undergo daily painful wound care procedures, including washing, debridement, and dressing. This systematic review and meta-analysis aimed to examine the effect of virtual reality (VR)-based interventions on pain during wound care in burn patients.
Methods:
A comprehensive systematic search was conducted on international electronic databases such as Scopus, PubMed, and Web of Science with keywords extracted from Medical Subject Headings such as "Virtual reality", "Virtual reality therapy", "Virtual reality exposure therapy", "Virtual reality immersion therapy", "Exergaming”, “Active-video gaming”, “Burns”, “Wound healings”, “Pain”, and “Pain management” from the earliest to May 6, 2022. The Joanna Briggs Institute (JBI) critical appraisal checklist was used to assess the quality of randomized control trials and quasi-experimental studies.
Results:
1,293 patients with burns were included in 30 studies, and their mean age was 22.89 (SD=7.63) years. 70.72% of the participants were male, and 67.05% were in the intervention group. This meta-analysis showed that VR significantly decreased pain severity in the intervention group compared to the control group (standard mean difference (SMD): -0.70, 95%CI: -0.97 to -0.43, Z=5.05, P<0.001, I2:82.0%). Immersive VR intervention showed statistically significant effects in reducing pain intensity among the intervention group, compared to the control group (SMD: -0.73, 95%CI: -0.97 to -0.49, Z=5.88, P<0.001, I2:69.3%); however, this finding was not the same for non-immersive VR (SMD: -0.62, 95%CI: -1.43 to 0.19, Z=1.51, P=0.132, I2:91.2%).
Conclusion:
It is suggested that health policymakers and managers equip burn wards with immersive VR devices to provide the basis for this intervention when caring for patients with burn wounds.
Key Words: Virtual reality, burns, wound healing, pain, pain management, systematic review, meta-analysis
1. Introduction
Based on the latest data from the World Health Organization, it is estimated that approximately 11 million people suffer severe burns that require medical care each year (1). Patients with severe burns suffer irreversible physical and psychological consequences. They also undergo daily painful wound care procedures, including washing, debridement, and dressing changes (2). Proper burn wound management requires an accurate examination of the burn patient and appropriate treatment decisions (3-18). Patients describe burn pains as excruciating, sharp, tender, or aching during wound care, which causes the patient to remain quiet and not respond verbally or even complain of pain (19). Lack of adequate pain control impacts burn patients' recovery negatively and is detrimental to the patient's physical and mental health, confidence, and adherence to the treatment regimen. (20).
Pharmacological intervention, such as use of opioid analgesics, is the first method of controlling pain in burn patients (21). Close monitoring of the intensity of pain, dose adjustment according to pain, and regular patient evaluation are necessary for the administration of opioids because of the different side effects and the possibility of physiological dependence or addiction (22). Therefore, in addition to pharmacotherapy, it is necessary to use cognitive and behavioural approaches, such as distraction, reappraisal, information provision, relaxation training, and operant conditioning to reduce the need to use more opioids. Distraction can be used in various ways, such as through illustration, music, games, and attention tasks (23). Numerous theories have been proposed to explain how distraction affects the control or reduction of pain perception (24).
Virtual reality (VR) is innovative, and one of the novel methods used to distract patients from pain (25). VR technology, which can provide a comprehensive experience of the computer world, was originally built for gaming purposes but it now has expanded applicability in the health care industry and other sectors of the economy (26). Immersion in the virtual world allows patients to be distracted from painful procedures (27). Studies in the United States and Europe have shown that combining VR therapy and analgesics significantly reduces pain perception (28-30). The availability of inexpensive VR technology has provided a good opportunity for its use in healthcare environments (23). It is impossible to consider technology's advantages without considering its disadvantages and side effects. Major disadvantages of VR include the need to teach the patient and provider how to use it, nausea, and motion sickness (31). Previous studies on the effectiveness of VR technology for reducing the pain of burn patients have reported conflicting results. A study by Hoffman et al. (2019) showed that using of VR intervention significantly reduced the pain of burn wound debridement, while another study by Konstantatos et al. (2009) found that VR had no effect on reducing the pain intensity during dressing change on a burn patient (25, 32). Previous systematic reviews and meta-analyses had some limitations. One meta-analysis evaluated the effect of VR on pain during burn wound care procedures and excluded cross-over and parallel study designs in the analysis. The overall effect was reported in six studies (33). Another meta-analysis reported the effect of fully immersive VR on pain experienced during dressing changes in hospitalized children and adolescents with severe burns based only on four studies (34). The present meta-analysis included parallel, cross-over or within-subjects studies on paediatric and adult populations to report the overall effect. Comprehensive sub-group and sensitivity analyses were also conducted in the present study. This study provides a systematic review and meta-analysis of VR-based interventions for pain control in burn patients during wound care.
2. Methods:
2.1. Study registration and reporting
This systematic review and meta-analysis was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist (35).
2.2. Search strategy
A comprehensive systematic search was conducted on international electronic databases such as Scopus, PubMed, Web of Science, and Iranian electronic databases such as Iranmedex, and Scientific Information Database (SID) with keywords extracted from Medical Subject Headings such as "Virtual reality", "Virtual reality therapy", "Virtual reality exposure therapy", "Virtual reality immersion therapy", "Exergaming”, “Active-video gaming”, “Burns”, “Wound healings”, “Pain”, and “Pain management” from the earliest to May 6, 2022. For example, the search strategy in PubMed/MEDLINE database included search terms such as ((“Virtual reality”) OR (“Virtual realities”) OR (“Virtual reality therapy”) OR (“Virtual reality therapies”) OR (“Virtual reality exposure therapy”) OR (“Virtual reality immersion therapy”) OR (“Computer simulation”) OR (“Computer simulations”) OR (“Exergaming”) OR (“Multimedia”) OR (“Multimedium”) OR (“Mobile applications”) OR (“Mobile apps”) OR (“Portable software apps”) OR (“Computer-assisted therapy”) OR (“Computer-assisted therapies”) OR (“Active-video gaming”)) AND ((“Wounds”) OR (“Wound healings”) OR (“Dressing change”)) AND ((“Pain”) OR (“Pain management”)) AND ((“Burns”) OR (“Burns patients”) OR (“Patients”) OR (“Clients”)). Keywords were combined with Boolean operators "AND" and "OR". Persian keywords equivalent to the mentioned words were searched in Persian databases. Two researchers performed the search processes, separately. This review does not include gray literature such as expert opinions, conference presentations, dissertations, research and committee reports, and ongoing research. Gray literature includes articles produced in print and electronic formats but not evaluated by a commercial publisher (36).
2.3. Inclusion and exclusion criteria
In this review, randomized control trials (RCTs) that were published in English and Persian languages and utilized parallel, cross-over or within-subjects designs focusing on the effect of different VR methods on pain of burn patients during burn wound care were included. Letters to the editor, case reports, conference proceedings, qualitative studies, and reviews were excluded.
2.4. Study selection
Data management was conducted using EndNote 8X software. Strategies included eliminating duplicate studies, evaluating the title and abstract, and evaluating the full text of articles. The selection criteria of the studies were evaluated by two researchers, separately, based on the inclusion and exclusion criteria. Disagreements between the two researchers were examined and resolved by a third researcher. Finally, the resource list was evaluated manually to prevent data loss.
2.5. Data extraction and quality assessment
The researchers extracted information from the studies used in this systematic review and meta-analysis, including first author’s name, year of publication, location, design, sample size, type of intervention, duration of the study, duration of intervention and follow-up, male/female ratio, age, type of control group, tool characteristics, specific Statistical tests, and key results of studies. The Joanna Briggs Institute (JBI) critical appraisal checklist was used to assess the quality of RCTs and quasi-experimental studies (37). JBI assesses the internal validity, the similarity of participants of compared groups, the reliability of outcomes measured, and the appropriateness of statistical analysis of RCT and quasi-experimental studies in 13 and 9 items, respectively. The quality of the studies in the systematic review and meta-analysis was evaluated by two researchers, separately, using a three-point reading range including "yes" (score 1), "no" (score 2), and "not applicable / not clear" (score 0). (38). The quality assessment levels of the studies in the JBI checklists were good (≥8), fair (6-7), and poor (≤5) (37).
2.6. Statistical analysis
Data required for meta-analysis such as sample size of each intervention and control group, standard deviation (SD), study design (parallel, cross-over), type of intervention (immersive and non-immersive), risk of bias with JBI tool (good, fair, and poor), age group (paediatrics, adults, and both) of participants, and type of painful procedure (dressing, physiotherapy and debridement) were entered into Excel software. Data of studies that reported confidence interval, range, standard error and interquartile range (IQR) were converted to SD. To calculate the overall effect, the sample size, mean change and SD change were used in both intervention and control groups. The forest-plot chart reported the standard mean difference (SMD) with the random-effect model (inverse-variance heterogeneity). A 95% confidence interval (CI) was used to determine the significance level (P-value<0.05). The overall negative effect was considered an indicator of the effectiveness of the VR intervention. Heterogeneity was investigated with I2 value. I2 above 50% was considered as substantial heterogeneity (39). Sub-group analysis based on study design, type of intervention, risk of bias based on JBI tool, age group of participants, and type of painful procedure was performed. Publication bias was checked using the funnel plot, and then egger's and Begg's tests were used to measure the statistical significance. The trim and fill test was performed according to the significance of these two tests. Sensitivity analysis was performed to determine the dependence of "overall effect size" on each study included in the meta-analysis.
3. Results:
3.1. Study selection
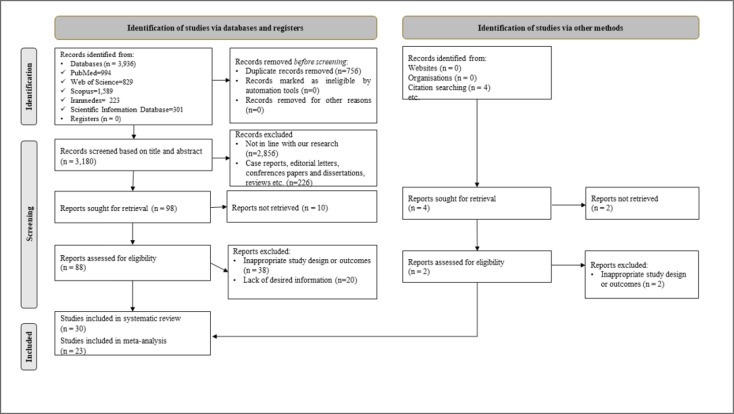
A total of 3,936 studies were obtained through a comprehensive search of electronic databases. After removing duplicate articles, 3,180 articles remained. 2,856 studies were deleted after reviewing the title and abstract of the articles due to inconsistencies with the purpose of the present review. 226 studies were excluded due to their non-experimental design. After evaluating the full texts of 88 studies, thirty-eight were excluded due to issues in design. In addition, twenty studies were excluded due to a lack of required information. Finally, thirty studies (25, 28-30, 32, 40-64) were used in this systematic review. Meta-analysis was performed on 23 RCTs with parallel, cross-over or within-subjects designs. The results of another seven quasi-RCTs were qualitatively reported (Figure 1).
Figure 1.
Flow diagram of the study selection process
3.2. Study characteristics
A total of 1,293 patients with burns were included in 30 studies (25, 28-30, 32, 40-64), and their mean age was 22.89 (SD=7.63) years. 70.72% of the participants were male, and 67.05% were in the intervention group. Twenty-three studies (25, 28, 30, 32, 41-50, 52-54, 56, 59, 60, 62-64) were RCTs with parallel, cross-over or within-subjects designs, while seven studies (29, 40, 51, 55, 57, 58, 61) had quasi-experimental designs. Of the studies in this systematic review and meta-analysis, twelve (25, 43, 47, 50-53, 55, 56, 59, 60, 62) reported the duration of the study with an average of 19.58 months. Eighteen studies (25, 28-30, 32, 41-44, 46-49, 52, 55, 58, 60, 63) reported duration of intervention with an average of 18.22 minutes. Of the studies in this systematic review and meta-analysis, thirteen (25, 30, 40, 42, 44, 46, 48, 49, 52, 56, 59, 62, 64) were conducted in the USA, and four (32, 41, 45, 50) in Australia, two (43, 51) in the Netherlands, two (54, 61) in Iran, two (28, 55) in Canada, two (57, 63) in Egypt, two (29, 58) in the UK, one (47) in South Africa, one (53) in China, and a study (60) in South Korea. Twenty-seven studies (25, 28-30, 32, 40-50, 52-54, 56, 57, 59-64) had a control group. Eleven studies (29, 40, 45, 50, 53, 54, 57, 58, 62-64) used VAS (Visual analog scale), nine (25, 30, 42, 44, 46, 48, 49, 59, 61) studies GRS (Graph rating scale), and seven (28, 45, 50, 53, 55, 57, 62) studies utilized FLACC (Faces, legs, activity, cry and consolability) to measure pain in participants (Table 1).
Table 1.
Basic characteristics of the studies included in this systematic review and meta-analysis
| First Author/year | Location | Study characteristics 1. Design 2. Sample Size (I/C) 3. Intervention 4. Duration of study 5. Duration of intervention 6. Duration of follow-up |
M/F ratio (%) | Age (mean±SD) |
Control group | Tool characteristics 1. Name of the questionnaire 2. Number of items 3. Overall scoring of items |
Intervention type | Key results | JBI Score |
|---|---|---|---|---|---|---|---|---|---|
| Hoffman et al., 2001 (40) |
USA | 1. Quasi-experimental 2. 7 3. VR 4. N/A 5. N/A 6. 3 days |
85.71/14.29 | 21.90 | All participants served as their own control when had not received VR distraction. | 1. VAS 2. 100 3. 0 to 100 |
Immersive | The mean score of pain in participants was decreased during the intervention in the intervention group compared to the control group (P< 0.010). | Good |
| Das et al., 2005 (41) |
Australia |
|
N/A | 11.10 (SD=3.50) | All participants served as their own control when had not received VR. | 1. Face scale 2. 10 3. 0 to 10 |
Immersive | The mean score of pain in patients was decreased after the intervention in the intervention group compared to the control group (P<0.01). | Fair |
| Sharar et al., 2007 (42) |
USA | 1. RCT 2. 234 (88/146) 3. VR 4. N/A 5. 15 minutes 6. 0 |
82.91/17.09 | N/A | Participants in the control group had not received VR. | 1. GRS 2. 100 mm 3. 0 to 100 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| van Twillert et al., 2007 (43) |
Netherland | 1. RCT 2. 19 3. VR 4. 13 months 5. 19.2 minutes 6. 2 days |
63.16/36.84 | 30.00 | All participants served as their own control when had not received VR. | 1. VAT 2. 100 mm 3. 0 to 100 |
Immersive | The mean score of pain in participants was decreased during and a day after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| Hoffman et al., 2008 (44) |
USA |
5. 3 minutes 6. N/A |
100/0 | 27.00 | All participants served as their own control when had not received VR. | 1. GRS 2. 10 cm 3. 0 to 10 |
Immersive | The mean score of pain in patients was decreased during the intervention in the intervention group compared to the control group (P=0.015). | Fair |
| Mott et al., 2008 (45) |
Australia | 1. RCT 2. 42 (20/22) 3. AR 4. N/A 5. N/A 6. 0 |
69.05/30.95 | N/A | Participants in the control group had not received the AR. | 1. FLACC pain assessment tool 2. 5 items 3. 0 to 10 1. FPS-R 2. N/A 3. N/A 1. VAS 2. 5 cm 3. 0 to 5 |
Non-immersive | The mean score of pain in participants (long dressing times) was decreased during the intervention in the intervention group compared to the control group (P=0.006). | Good |
| Carrougher et al., 2009 (46) |
USA | 1. RCT (Crossover) 2. 39 3. VR 4. N/A 5. 10 minutes 6. 0 |
89.74/10.26 | 35.00 (SD=11.00) | Participants in the control group had not received VR. | 1. GRS 2.100 mm 3.0 to 100 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P=0.004). | Fair |
| Konstantatos et al., 2009 (32) |
Australia | 1. RCT 2. 86 (43/43) 3. VR 4. N/A 5. 18 minutes 6. 0 |
N/A | 38.60 (SD=15.95) | Participants in the control group had not received VR. | 1. BSAR 2.10 cm 3.0 to 10 |
Non-Immersive | The mean score of pain in participants was increased during and after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| Morris et al., 2010 (47) |
South Africa | 1. RCT (Crossover) 2. 11 3. VR 4. 4 months 5. 18 minutes 6. 0 |
N/A | N/A | All participants served as their own control when had not received VR. | 1.NPRS 2.N/A 3.N/A 1.BSPAS 2.100 mm 3.0 to 100 |
Non-immersive | There was no significant difference in pain scores during the intervention between the intervention and control groups (P=0.13). | Good |
| Maani et al., 2011 (48) |
USA | 1. RCT (Crossover) 2. 12 3. VR 4. N/A 5. 12 minutes 6. 0 |
100/0 | N/A | All participants served as their own control when had not received VR. | 1. GRS 2.100 mm 3.0 to 100 |
Immersive | The mean score of pain in participants was decreased during the intervention in the intervention group compared to the control group (P<0.05). | Fair |
| Schmitt et al., 2011 (49) |
USA | 1. RCT (Crossover) 2. 54 3. VR 4. N/A 5. 6.5 minutes 6. 0 |
81.48/18.52 | 12.00 (SD= 3.90) |
All participants served as their own control when had not received VR. | 1. GRS
|
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P< 0.05). | Fair |
| Kipping et al., 2012 (50) |
Australia | 1. RCT 2. 41 (20/21) 3. VR 4. 15 months 5. N/A 6. 0 |
68.29/31.71 | 13.05 (SD=1.55) | Participants in the control group had not received the VR. | 1. FLACC pain assessment tool 2.5 items 3. 0 to 10 1. VAS 2.10 cm 3. 0 to 10 |
Immersive | There was no significant difference between the intervention and the control group in pain score during dressing removal and application (P>0.05). | Good |
| Faber et al., 2013 (51) |
Netherlands | 1. Quasi-experimental 2. 36 3. VR 4. 40 months 5. N/A 6. 7 days |
83.33/16.67 | 27.70 (SD=15.20) | N/A | 1. VAT 2.10 cm 3.0 to 10 |
Immersive | The mean score of pain in participants was decreased during the intervention on days one, two, and three (P< 0.05). | Fair |
| Jeffs et al., 2014 (52) |
USA | 1. RCT 2. 28 (18/10) 3. VR 4. 22 months 5. 52.5 minutes 6. 0 |
32.14/67.86 | 13.50 (SD=2.30) | Participants in the control group had not received the VR. | 1.APPT 2.115 mm 3.0 to 115 |
Immersive | There was no significant difference in pain scores between the intervention and control groups during the intervention (P=0.32). | Good |
| Hua et al., 2015 (53) |
China | 1. RCT 2. 65 (33/32) 3. VR 4. 12 months 5. N/A 6. 0 |
47.69/52.31 | 8.72 (SD=3.38) | Participants in the control group had not perceived the VR. | 1. Faces picture scale 2.10 items 3.0 to 10 1. FLACC pain assessment tool 2.5 items 3. 0 to 10 1. VAS 2.10 cm 3. 0 to 10 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| Ebrahimi et al., 2017 (54) |
Iran | 1. RCT 2. 60 (40/20) 3. VR 4. N/A 5. N/A 6. 5 days |
56.67/43.33 | 35.00 (SD=10.00) | Participants in the control group had not received the VR. | 1. VAS 2.10 cm 3.0 to 10 |
Non-immersive | There was no significant difference in pain scores before and after the intervention between intervention and control groups from day one to five (P>0.05). | Good |
| Khadra et al., 2018 (55) |
Canada | 1. Quasi-experimental 2. 15 3. VR 4. 7 months 5. 18.4 minutes 6. 0 |
40.00/60.00 | 2.20 (SD=2.10) | N/A | 1. FLACC pain assessment tool 2.5 items 3. 0 to 10 |
Non-immersive | There was no significant difference in pain scores before and after the intervention in the intervention group (P>0.05). | Fair |
| McSherry et al., 2018 (56) |
USA | 1. RCT (Crossover) 2. 18 3. VR 4. 29 months 5. N/A 6. 0 |
72.22/27.78 | 38.40 (SD=15.50) | All participants served as their own control when had not received VR. | 1. VNS 2.10 cm 3.0 to 10 |
Immersive | There was no significant difference in pain intensity between intervention and control groups after intervention (P>0.05). | Fair |
| Soltani et al., 2018 (30) |
USA | 1. RCT (Crossover) 2. 39 3. VR 4. N/A 5. 6 minutes 6. 0 |
N/A | 36.00 | All participants served as their own control when performing ROM exercises without VR distraction. | 1. GRS
|
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P< 0.005). | Fair |
| Fatma & Ghada, 2019 (57) |
Egypt | 1. Quasi-experimental 2. 60 (30/30) 3. VR 4. N/A 5. N/A 6. 0 |
60.00/40.00 | N/A | Participants in the control group had not received VR. | 1. Faces picture scale 2.10 items 3.0 to 10 1. FLACC pain assessment tool 2.5 items 3. 0 to 10 1. VAS 2.10 cm 3. 0 to 10 |
Immersive | The mean score of pain in participants was decreased during and after the intervention in the intervention group compared to the control group (P<0.001). | Good |
| Hoffman et al., 2019 (25) |
USA | 1. RCT 2. 48 3. VR 4. 35 months 5. 5 minutes 6. N/A |
70.83/29.17 | 12.00 | All participants served as their own control when had not received VR. | 1. GRS 2.10 cm 3.0 to 10 |
Immersive | The mean score of pain in participants was decreased during the intervention in the intervention group compared to the control group (P<0.001). | Good |
| Phelan et al., 2019 (58) |
UK | 1. Quasi-experimental 2. 15 3. VR 4. N/A 5. 5 minutes 6. 0 |
66.67/33.33 | 25.00 | N/A | 1. VAS 2.100 3.0 to 100 |
Immersive and non-immersive |
|
Fair |
| Hoffman et al., 2020 (59) |
USA | 1. RCT 2. 50 3. VR 4. 29 months 5. N/A 6. 10 days |
84.00/16.00 | N/A | Participants in the control group had not received VR. | 1. GRS 2.10 cm 3. 0 to 10 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| Joo et al., 2020 (60) |
South Korea | 1. RCT 2. 57 (28/29) 3. VR 4. 4 months 5. 30 minutes 6. 0 |
94.74/5.26 | 44.88 (SD=11.09) | Participants in the control group had not received VR. | 1. MHQ 2. N/A 3.0 to 100 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P=0.002). | Good |
| Khadra et al., 2020 (28) |
Canada | 1. RCT 2. 38 3. VR 4. N/A 5. 25 minutes 6. 0 |
71.05/28.95 | 1.82 (SD=1.32) |
All participants served as their own control when had not received VR. | 1. FLACC
1. NRS-obs 2.N/A 3.N/A |
Non-immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| Kiani et al., 2020 (61) |
Iran | 1. Quasi-experimental 2. 45 (30/15) 3. VR 4. N/A 5. N/A 6. 0 |
N/A | 31.38 (SD=8.47) | Participants in the control group had not received VR. | 1. GRS 2.100 mm 3.0 to 100 1.BSPAS 2.100 mm 3.0 to 100 |
Immersive | There was no significant difference in pain intensity between intervention and control groups during the intervention (P>0.05). | Good |
| Phelan et al., 2021 (29) |
UK | 1. Quasi-experimental 2. 20 (15/5) 3. VR 4. N/A 5. 36.9 minutes 6. 0 |
60.00/40.00 | 48.20 (SD= 19.68) |
Participants in the control group had not received the VR. | 1. VAS 2.100 mm 3.0 to 100 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P= 0.007). | Good |
| Xiang et al., 2021 (62) |
USA | 1. RCT 2. 90 (61/29) 3. VR 4. 25 months 5. N/A 6. 0 |
50.00/50.00 | 11.30 | Participants in the control group had not received the VR. | 1. VAS3.0 to 100 1. FLACC
|
Immersive and non-immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.05). | Good |
| Ali et al., 2022 (63) |
Egypt | 1. RCT 2. 22 (11/11) 3. VR 4. N/A 5. 20 minutes 6. 0 |
59.09/40.91 | 13.18 (SD=1.73) | Participants in the control group had not received the VR. | 1. VAS 2.10 cm 3.0 to 10 |
Immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.001). | Good |
| Armstrong et al., 2022 (64) |
USA | 1. RCT 2. 24 (11/13) 3. VR 4. N/A 5. N/A 6. 7 days |
79.17/20.83 | 11.50 (SD=3.10) | Participants in the control group had not received the VR. | 1. VAS 2.10 cm 3.0 to 10 |
Non-immersive | The mean score of pain in participants was decreased after the intervention in the intervention group compared to the control group (P<0.05). | Good |
RCT: Randomized clinical trial; ANOVA: Analysis of variance; VAS: Visual analog scale; VR: Virtual reality; AR: Augmented reality; FLACC: Faces, legs, activity, cry and consolability; FPS-R: Faces pain scale-revised; GRS: Graph rating scale; VR-PAT: Virtual reality pain alleviation tool; BSAR: Burns specific anxiety rating; VNS: Verbal numeric scale; MHQ: Michigan hand outcomes questionnaire; BSPAS: Burn specific pain anxiety scale; APPT: Adolescent pediatric pain tool; NPRS: Numeric pain rating scale; VAT: Visual analog thermometer; NRS-obs: Numeric Rating Scale-observational; N/A: not applicable; SD: standard deviation; JBI: Joanna Briggs Institute; ROM: Range of motion.
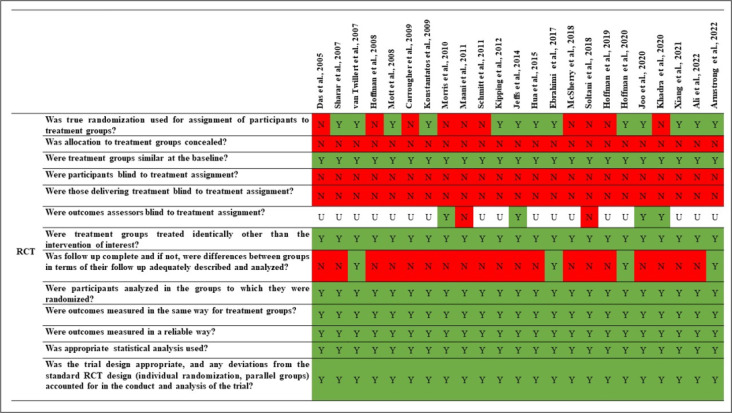
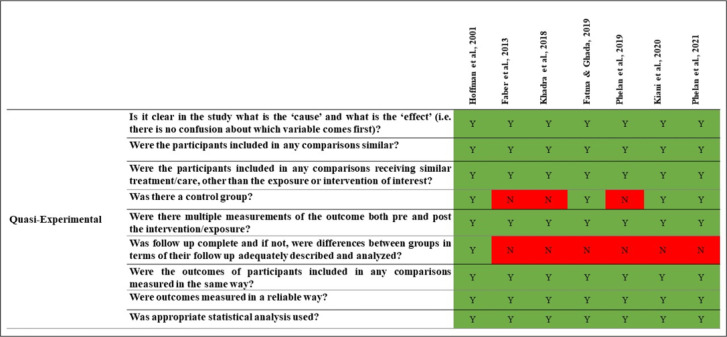
3.3. Methodological quality assessment of eligible studies
Of the thirty studies (25, 28-30, 32, 40-64), twenty (25, 28, 29, 32, 40, 42, 43, 45, 47, 50, 52-54, 57, 59-64) had good quality, while ten studies (30, 41, 44, 46, 48, 49, 51, 55, 56, 58) had fair quality (Figures 2 & 3).
Figure 2.
Methodological quality assessment of RCT studies using Joanna Briggs Institute (JBI) checklist
Figure 3.
Methodological quality assessment of quasi-experimental studies using Joanna Briggs Institute (JBI) checklist
3.4. Effect of VR methods on pain of burn patients during wound care
Thirty studies (25, 28-30, 32, 40-64) in the present systematic review examined the effect of different VR methods on reducing pain during wound care in burn patients. The characteristics of the interventions in the included studies are presented in Table 2. Overall, the results of twenty-two studies (25, 28-30, 40-46, 48, 49, 51, 53, 57-60, 62-64) showed that different VR methods reduced pain, while one study (32) showed that it increased pain when caring for burn wounds. However, the results of seven studies (47, 50, 52, 54-56, 61) showed that different VR methods did not affect patients' pain when caring for burn wounds.
Table 2.
Interventions of the studies included in the systematic review and meta-analysis
| First Author/year | Intervention Program | Description |
|---|---|---|
| Hoffman et al., 2001 (40) |
VR | Participants received VR distraction. The intervention was as follows: Patients underwent active-assisted physical therapy exercises with a VR helmet. A motion-sensing system was used with a VR helmet to measure the position of the participant's head. The first participant was placed in the virtual environment of the Spider World where she/he could move virtual objects with her/his cyber hands. Other participants were placed in the Snow World where they could move and throw snowballs. the pain was measured via VAS during the intervention. |
| Das et al., 2005 (41) |
VR | Participants received 10 to 45 minutes of VR. The intervention was as follows: Coin toss was used to sequence the analgesic test using medication or using medication and VR. The content in VR was a game based on the age group of the participants. Participants could shoot monsters using a pointer. The game was designed so that participants could play with minimal movement during dressing changes. The pain was measured via the face scale immediately after the intervention. |
| Sharar et al., 2007 (42) |
VR | Participants received immersive VR distraction for 15 minutes during physical therapy. The VR intervention was such that using a large screen above the patient's head with sound effects and moving explosions of blue, white, and green, the patient's communication with the environment was blocked. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via the GRS immediately after the intervention. |
| van Twillert et al., 2007 (43) |
VR | Participants received 19.2 minutes of VR during wound dressing change. VR intervention consisted of a pair of 3D glasses and an integrated audio system. The Snow World content included a snowy environment in which participants threw snowballs at snowmen, igloos, and penguins using the keys on the mouse and keyboard. There were special effects such as river and sky along with sound effects in this intervention. The pain was measured via the VAT one day before, during, and after wound dressing. |
| Hoffman et al., 2008 (44) |
VR | Participants received 3 minutes of VR distraction. The intervention was as follows: Patients underwent wound debridement for three minutes with a VR waterproof cap. In Immersive VR intervention, helmets, headphones, and joysticks were used to control the movement of snowballs and their launch. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via GRS during the intervention. |
| Mott et al., 2008 (45) |
AR | Participants received AR during dressing change. AR is a device that has several sculptures on top of it and is lifted by a camera, creating a three-dimensional character called Hospital Harry. A voice or the child's parents encouraged the child to continue and change the animation. By manipulating the camera, the child can visualize the existing character from different angles. The pain was measured via the FLACC pain assessment tool, the FPS-R, and the VAS before, during, and after the intervention. |
| Carrougher et al., 2009 (46) |
VR | Participants received VR during physical therapy for 10 minutes. VR intervention consisted of a pair of 3D glasses and an integrated audio system. The Snow World content included a snowy environment in which participants threw snowballs at snowmen, igloos, and penguins using the keys on the mouse and keyboard. There were special effects such as river and sky along with sound effects in this intervention. The pain was measured via GRS immediately after the intervention. |
| Konstantatos et al., 2009 (32) |
VR | Participants received VR relaxation with intravenous morphine patient-controlled analgesia during dressing change. VR relaxation intervention includes VR glasses, a headset, a DVD player, and a relaxing DVD. The content of the DVD includes the sequence "Snow World", which is based on the theory of hypnotherapy. The program includes videos of soothing scenery that end with a spiral, and participants are asked to focus on the spiral. The pain was measured via the BSAR before, during, and after the intervention. |
| Morris et al., 2010 (47) |
VR | Participants received a low-cost VR system with analgesia during physiotherapy for 18 minutes. The order of the meetings was determined using a coin toss. Low-cost VR system intervention used a VR display on the patient's head and contained a game called "Walt Disney's Chicken Little". The pain was measured via the BSPAS, and NPRS by a blinded assessor during physiotherapy. |
| Maani et al., 2011 (48) |
VR | Participants received robot-like arm-mounted VR goggles during wound care for 12 minutes. A random number generator was used to determine the order of intervention. The VR intervention consisted of a VR glass, a spectacle holding system, and a custom robot-like arm. The Snow World content included a snowy environment in which participants threw snowballs at snowmen, igloos, and penguins using the keys on the arm. There were special effects such as river and sky along with sound effects in this intervention. The pain was measured via the GRS during wound care. |
| Schmitt et al., 2011 (49) |
VR | Participants received 3-10 minutes of VR distraction during physical therapy. The intervention was as follows: Patients underwent post-burn physical therapy with a VR helmet. A motion-sensing system was used with a VR helmet to measure the position of the participant's head. The participants were placed in the virtual environment of the Snow World where they could move and throw snowballs. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via GRS immediately after the intervention. |
| Kipping et al., 2012 (50) |
VR | Participants received an Off-the-shelf VR system during dressing removal and application. The intervention was performed using a VR display on the head with a tracker and manual joystick control. The VR content displayed for patients was “Chicken Little” and “Need for Speed” games. The pain was measured via the FLACC pain assessment tool and the VAS before and during the intervention. |
| Faber et al., 2013 (51) |
VR | Participants received VR distraction in daily wound care. The intervention was as follows: Patients underwent wound care with a VR helmet. Motion-sensing system and integrated audio system were used with a VR helmet to place participants in the virtual environment of the Snow World where they could move and throw snowballs. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via VAT during and after interventions. |
| Jeffs et al., 2014 (52) |
VR | Participants received VR distraction during burn wound care. VR distraction intervention was performed using a VR helmet, a tripod with a hinged arm, headphones, and interaction with a trackball. The VR content of the game was Snow World. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via the VAS during the intervention. |
| Hua et al., 2015 (53) |
VR | Participants received VR distractions during dressing changes. VR distractions intervention was performed using a VR headset and headphones. The content of VR distraction was a third-person game called Ice Age 2: The Meltdown, in which participants control the game character in a snowy environment to reach the oak. The pain was measured via the FLACC pain assessment tool, the faces picture scale, and the VAS before, during, and after the intervention. |
| Ebrahimi et al., 2017 (54) |
VR | Participants received VR for five days during dressing changes. The VR intervention was performed with a VR goggle and headset through which audio and video were streamed. The pain was measured via the VAS. |
| Khadra et al., 2018 (55) |
VR | Participants received a VR dome environment during hydrotherapy for a mean of 18.4 minutes. The VR dome intervention consists of a curved plate located at the end of the hydrotherapy reservoir. The content of this intervention includes a game called bubbles in which there is a mouse and the child presses it to produce bubbles. Also, animals appear on the screen, which produce funny sounds and emoticons and the child is inside a wagon that passes between/through them. The pain was measured via the FLACC pain assessment tool, one hour before, immediately before, 10 minutes after onset, immediately after, and 30 minutes after hydrotherapy. |
| McSherry et al., 2018 (56) |
VR | Participants received immersive VR during dressing changes. The VR intervention was such that using a large screen above the patient's head with sound effects and moving explosions of blue, white, and green, the patient's communication with the environment was blocked. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via the VNS before and after the intervention. |
| Soltani et al., 2018 (30) |
VR | Participants received 3 minutes of VR distraction. The intervention was as follows: Patients underwent active physical therapy exercises with VR goggles. Participants were randomly divided into two groups with/without VR treatment orders. The participants were placed in the virtual environment of the Snow World where they could move and throw snowballs. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via GRS immediately after the intervention. |
| Fatma & Ghada, 2019 (57) |
VR | Participants received VR technology during dressing change. VR technology intervention involves a mobile phone with a 3D animation that sits on a device with 3D glasses on the head that also has headphones. The pain was measured via the FLACC pain assessment tool, the faces picture scale, and the VAS before, during, and after the intervention. |
| Hoffman et al., 2019 (25) |
VR | Participants received 5 minutes of VR distraction during wound cleaning. The intervention was as follows: Patients underwent wound care with waterproof VR goggles that were fixed near their eyes. Participants were randomly divided into two groups with/without VR treatment orders. The participants explored the virtual environment of the Snow World, with a mouse, where they could move and throw snowballs. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via GRS during the intervention. |
| Phelan et al., 2019 (58) |
VR | Participants received four different VR scenarios, each lasting an average of 5 minutes. The four VR scenarios were as follows:
The pain was measured via the VAS. |
| Hoffman et al., 2020 (59) |
VR | Participants received VR distraction during wound debridement. The intervention was as follows: Patients underwent wound care with waterproof VR goggles that were fixed near their eyes. The participants explored the virtual environment of the Snow World, with a mouse, where they could move and throw snowballs. The Snow World content was such that patients threw snowballs at snowmen, igloos, robots, and penguins at the push of a button. The pain was measured via GRS after the intervention. |
| Joo et al., 2020 (60) |
VR | Participants received VR-based rehabilitation for 30 minutes. The intervention involved using a system called RAPAEL Smart Glove, which was a combination of a glove and a VR system. This system collects the patient's active movements with gloves. The training program in using this glove included the following:
|
| Khadra et al., 2020 (28) |
VR | Participants received 10 minutes of VR distraction during hydrotherapy. The intervention was as follows: Patients underwent wound care in the hydrotherapy tank with projector-based hybrid VR. Participants were randomly divided into two groups with/without VR treatment orders. The participants played the Bubbles video game with a mouse or automatic mode. Patient pain was measured via FLACC scale and NRS at the following times: T1: before the intervention, T2: first 5 minutes of intervention, T3: end of the first phase of wound care session, T4: end of the second phase of wound care session, and T5: 30 minutes after end of wound care session. |
| Kiani et al., 2020 (61) |
VR | Participants received VR. The VR intervention consisted of VR glasses with a helmet that had two speakers inside the helmet to hear the sound, as well as gloves with a sensor. To detect the movement of the head, there was a tracker sensor inside the helmet that signaled the participants' movements to the computer. The content of this intervention included a game that had a cold and snowy atmosphere and the user threw snowballs at the snowmen to get points. The pain was measured via the GRS and BSPAS before and after the intervention. |
| Phelan et al., 2021 (29) |
Participants received four different VR scenarios. In this intervention, an Oculus Rift VR display system on the patient's head, a remote control, and a head tracker were used to monitor and detect movement. The four different VR scenarios were as follows:
|
|
| Xiang et al., 2021 (62) |
VR | Participants received two types of VR-PAT. The intervention was performed using an iPhone and headphones. Two types of VR-PAT were as follows:
|
| Ali et al., 2022 (63) |
VR | Participants received VR Oculus with physical therapy seasons, each season lasting for 20 minutes. VR oculus uses a VR goggle to restrict children's vision of the hospital environment. Children can choose their favorite video from the beginning of the intervention. In addition to VR glasses, headphones are also provided to play audio. The pain was measured via the VAS before and after the intervention. |
| Armstrong et al., 2022 (64) |
VR | Participants received VR-PAT for 7 days during the dressing change. The VR-PAT intervention includes a VR headset with a virtual river cruise game that runs on smartphones. The game involved guiding a boat to shore, with snow sculptures in the middle of the road where the participant could guide the boat by shaking its head and receiving the sculptures. The pain was measured via the APPT. |
VR: Virtual reality; VAS: Visual analog scale; GRS: Graph rating scale; VAT: Visual analog thermometer; Augmented reality; FLACC: Faces, legs, activity, cry and consolability; FPS-R: Faces pain scale-revised; BSAR: Burns specific anxiety rating; BSPAS: Burn specific pain anxiety scale; NPRS: Numeric pain rating scale; VNS: Verbal numeric scale; MHQ: Michigan hand outcomes questionnaire; NRS: Numeric Rating Scale; VR-PAT: Virtual reality pain alleviation tool; APPT: Adolescent pediatric pain tool.
3.5. A meta‑analysis of the effect of different VR methods on reducing pain during wound care in burn patients
The result of the meta-analysis demonstrated that the use of VR intervention, compared to the control group, led to a significant reduction in pain intensity (SMD: -0.70, 95%CI: -0.97 to -0.43, Z=5.05, P<0.001, I2:82.0%) (Figure 4).
Figure 4.
Sub-group analysis based on immersive and non-immersive VR intervention. SMD: standard mean difference; CI: confidence interval
The results of the subgroup analysis showed that immersive VR intervention significantly reduces pain intensity (SMD: -0.73, 95%CI: -0.97 to -0.49, Z=5.88, P<0.001, I2:69.3%). However, non-immersive VR intervention did not show a statistically significant effect on pain intensity (SMD: -0.62, 95%CI: -1.43 to 0.19, Z=1.51, P=0.132, I2:91.2%) (Figure 4).
The sub-group analyses showed that the included studies with different levels of bias (good and fair) significantly reduced pain intensity in the VR intervention groups. Other results from sub-group analysis showed that VR intervention had significant effects on pediatrics and both age groups (pediatrics and adults); however, it was not statically significant in the adults. Also, sub-group analysis indicated that VR intervention significantly reduced pain intensity in different burn procedures, such as dressing changes, wound debridement, and physical therapy. Studies with parallel and cross-over designs showed that VR significantly affected intervention groups (Table 3). Sensitivity analysis showed that the overall effect of VR on pain severity levels did not depend on a single study (95%CI: -1.03 to -0.35).
Table 3.
Sub-group analysis of included studies
| Sub-categories | Number* | Effect size** | 95%CI | Z | P | I 2 |
|---|---|---|---|---|---|---|
| Bias | ||||||
| Good | 19 | -0.69 | -1.03 to -0.35 | 3.97 | <0.001 | 85.4% |
| Fair | 6 | -0.74 | -1.06 to -0.43 | 4.59 | <0.001 | 37.5% |
| Age group | ||||||
| Pediatric | 14 | -0.81 | -1.22 to -0.39 | 3.83 | <0.001 | 82.9% |
| Adult | 7 | -0.45 | -1.01 to 0.10 | 1.59 | 0.11 | 84.0% |
| Both | 4 | -0.53 | -0.81 to -0.26 | 3.0 | 0.003 | 77.7% |
| Design | ||||||
| Parallel | 15 | -0.59 | -1.04 to -0.13 | 2.51 | 0.01 | 85.5% |
| Cross-over | 10 | -0.85 | -1.13 to -0.57 | 5.96 | <0.001 | 68.2% |
| Procedure | ||||||
| Dressing | 12 | -0.66 | -1.20 to -0.11 | 2.37 | 0.02 | 87.1% |
| Physical therapy | 8 | -0.63 | -0.95 to -0.31 | 3.84 | <0.001 | 72.2% |
| Debridement | 3 | -0.91 | -1.55 to -0.28 | 2.81 | 0.005 | 77.7% |
| Wound care | 0 | -0.35 | -1.29 to 0.59 | 0.73 | 0.46 | 0 |
*: number of studies, **: Standard mean difference. CI: confidence interval.
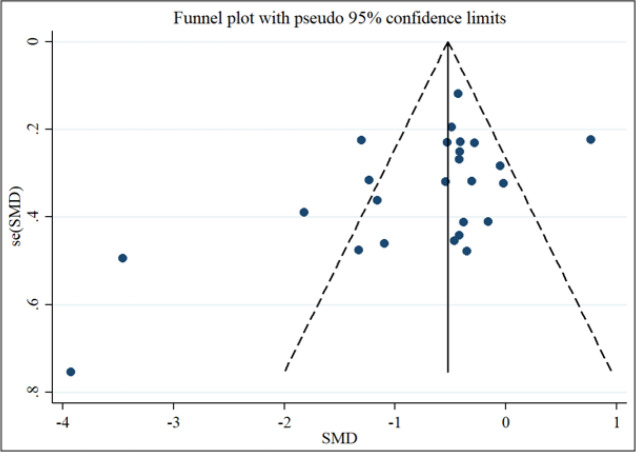
Based on the visual inspection of the funnel plot, we found an asymmetry (Figure 5). We did not observe any change in the overall effect size (SMD: -0.62, 95%CI: -0.88 to -36). Begg's (P=0.02) and Egger's regression tests (P=0.04) indicated a significant publication bias. Therefore, meta-trim with fill-and-trim method was used to correct probable publication bias.
Figure 5.
Funnel plot for asymmetry evaluation in included studies. SMD: standard mean difference
4. Discussion:
In the present systematic review, the effects of various VR methods were evaluated on patients’ pain when undergoing care for burn wounds. Findings delineated that twenty-two interventions reduced pain and one intervention increased pain. Meanwhile, seven interventions did not affect patients' pain. A meta-analysis was performed on 23 studies with parallel and cross-over RCT designs, which showed that VR intervention significantly reduced pain intensity.
One of the most important outcomes for burn patients is pain relief when caring for burn wounds. Pain in these patients is due to hypersensitivity of the pain pathways in the central and peripheral nervous systems (65). Lack of proper pain management can provoke a reaction and arousal in the later stages of burn wound care (66-78). Therefore, proper pain management is particularly important in these patients. In recent years, non-pharmacological approaches to relieving pain in burn patients have been considered. One of these approaches is VR, which has rare side effects (62).
In the present review, various VR methods were used in addition to conventional therapies to reduce pain during wound care in burn patients. A systematic review and meta-analysis was performed by Chan et al. on the clinical efficacy of VR in managing acute pain in various procedures. The Chan et al. study showed that VR could effectively relieve procedural pain, but its statistical analyses had issues with heterogeneity (79). Another review study examined the effect of VR interventions on procedural pain in paediatrics, which showed that VR interventions reduced pain in children more than standard care (80). A narrative review study examined the effect of VR on acute and chronic pain in adult patients. One of the topics studied in this study was the effect of VR on pain when changing dressings. This study showed that in 12 out of the eighteen studies reviewed, VR significantly reduced pain (81). Another review examined VR as a pain management tool and demonstrated that VR therapy could be suitable for distracting the patient while creating painful stimuli (82). Another systematic review and meta-analysis study examined the effect of VR on acute and chronic pain in adults. The results showed that VR effectively reduced acute pain in these patients. However, some studies have shown that VR can also reduces chronic pain, so more research is needed on the effect of VR on reducing chronic pain (83). Another systematic review also examined the effect of interactive VR on pain perception in patients, which showed that this intervention effectively reduced pain. However, more intervention studies are needed to confirm the effectiveness of VR intervention in reducing pain (84).
Results of a meta-analysis based on 23 studies with parallel and cross-over RCTs design showed that VR intervention significantly reduced pain intensity. The results of the present study were consistent with the results of previous meta-analyses. One meta-analysis (2022) was performed with six studies to evaluate the effects of VR on pain intensity and other outcomes. Sub-group analysis results of this particular study showed that immersive VR (4 studies) significantly decreased pain intensity, and non-immersive VR (2 studies) had no effect on patients’ pain perception (33). Based on the results of the current meta-analysis, immersive VR intervention (18 studies) significantly decreased pain intensity in the intervention group. However, non-immersive VR (7 studies) did not cause a statistically significant difference between intervention and control groups. In the non-immersive VR technique, the least interactive activities, such as interaction with the keyboards and mice without fully immersing into the environment, occurred. In immersive VR, the interaction is the highest and subjects are fully immersed in and interact with the VR environment (85). The current meta-analysis showed that VR intervention had a statistically significant effect on pediatric patients; however, it was ineffective among the adult age group. Various factors, such as different contextual factors in pain perception in each age group and measurement scales, can affect pain intensity. Also, one meta-analysis on paediatrics revealed that immersive VR significantly decreased pain intensity (34). Future studies should compare VR effects on adults and paediatrics.
The present systematic review results showed that out of thirty VR interventions, twenty-two interventions reduced patients' pain during burn wound care procedures. The meta-analysis found that VR can statistically decrease pain intensity in the intervention group compared to the control group. According to the results of previous studies and the present systematic review and meta-analysis, it is suggested that health policymakers and managers consider equipping burn wards/units with VR devices to provide the basis for this intervention when caring for burn patients. To compare the effects of VR intervention among different age groups and immersive vs non-immersive VR, it is recommended that future research be focused on this area.
4.1. Limitations
There are limitations in this study that are noteworthy. This systematic review and meta-analysis is based on the PRISMA checklist but is not listed in the international prospective register of systematic reviews database (PROSPERO). Although two researchers completed the search of electronic databases, all studies on this subject may not have been found. Finally, only studies in English and Persian have been included, and studies in other languages have not been included.
4.2. Implications for health managers and policymakers
Considering the importance of pain management when caring for burn patients using various interventions, including VR methods, and also considering the results of this systematic review and meta-analysis, it is suggested that health policymakers and managers equip burn wards with VR devices to provide the basis for this intervention when caring for the wounds of these patients, as well as develop policies and guidelines regarding the use and deployment of VR technology in the management of pain in burn patients.
4.3. Implications for future research
In the results of this meta-analysis study, studies that applied the immersive VR or performed on pediatric patients showed a more significant effect on the intervention than the control group. However, studies that applied non-immersive VR or included adults; demonstrated no significant difference between intervention and control groups. Therefore, it is suggested that future studies focus on comparing immersive and non-immersive VR interventions in paediatrics with adults.
5. Conclusion
In the present systematic review, the effects of various VR methods were evaluated on patients’ pain when undergoing care for burn wounds, which showed that immersive VR intervention significantly decreased pain intensity in the intervention group. Health policymakers and managers should equip burn wards with immersive VR devices to provide the basis for this intervention when caring for these patients' wounds.
6. Declarations:
6.1. Acknowledgement
None
6.2. Authors’ contributions
Study concept and design by all authors; Data acquisition by all authors; Data interpretation by all authors; drafting of the manuscript by all authors; Revision of the manuscript by all authors; the final version of the manuscript is approved by all authors.
6.3. Conflict of interest
The authors declare no conflict of interest.
6.4. Funding and support
None.
6.5. Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
- 1.WHO. Burns [Internet]. World Health Organization; 2018 [updated 2018 March 6. Available from: https://www.who.int/en/news-room/fact-sheets/detail/burns .
- 2.Scheffler M, Koranyi S, Meissner W, Strauss B, Rosendahl J. Efficacy of non-pharmacological interventions for procedural pain relief in adults undergoing burn wound care: A systematic review and meta-analysis of randomized controlled trials. Burns. 2018;44(7):1709–20. doi: 10.1016/j.burns.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Miri S, Mobayen M, Aboutaleb E, Ezzati K, Feizkhah A, Karkhah S. Exercise as a rehabilitation intervention for severe burn survivors: benefits & barriers. Burns. 2022;48(5):1269–70. doi: 10.1016/j.burns.2022.04.016. [DOI] [PubMed] [Google Scholar]
- 4.Akhoondian M, Zabihi MR, Yavari S, Karampoor M, Fouladpour A, Samadnia A, et al. Radiation burns and fertility: a negative correlation. Burns. 2022 doi: 10.1016/j.burns.2022.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Ghazanfari M, Mazloum S, Rahimzadeh N, Araste M, Vajargah P, Mollaei A, et al. Burns and pregnancy during the COVID-19 pandemic. Burns. 2022 doi: 10.1016/j.burns.2022.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feizkhah A, Mobayen M, Ghazanfari MJ, Toolaroud PB, Vajargah PG, Mollaei A, et al. Machine Learning for burned wound management. Burns. 2022;48(5):1261–2. doi: 10.1016/j.burns.2022.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Mobayen M, Feizkhah A, Ghazanfari MJ, Ezzati K, Mehrabian F, Toolaroud PB, et al. Sexual satisfaction among women with severe burns. Burns. 2022;48(6):1518–9. doi: 10.1016/j.burns.2022.05.024. [DOI] [PubMed] [Google Scholar]
- 8.Mobayen M, Ghazanfari MJ, Feizkhah A, Ezzati K, Mehrabian F, Aboutaleb E, et al. Parental adjustment after pediatric burn injury. Burns. 2022;48(6):1520–1. doi: 10.1016/j.burns.2022.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Bazzi A, Ghazanfari MJ, Norouzi M, Mobayen M, Jafaraghaee F, Zeydi AE, et al. Adherence to Referral Criteria for Burn Patients; a Systematic Review. Arch Acad Emerg Med. 2022;10(1):e43. doi: 10.22037/aaem.v10i1.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miri S, Mobayen M, Mazloum SMH, Rahimzadeh N, Mehrabi A, Abd Sonboli R, et al. The role of a structured rehabilitative exercise program as a safe and effective strategy for restoring the physiological function of burn survivors. Burns. 2022;48(6):1521–3. doi: 10.1016/j.burns.2022.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Mobayen M, Ghazanfari MJ, Feizkhah A, Zeydi AE, Karkhah S. Machine learning for burns clinical care: Opportunities & challenges. Burns. 2022;48(3):734–5. doi: 10.1016/j.burns.2022.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Mobayen M, Feizkhah A, Ghazanfari MJ, Toolaroud PB, Mobayen M, Osuji J, et al. Intraoperative three-dimensional bioprinting: A transformative technology for burn wound reconstruction. Burns. 2022;48(4):1023–4. doi: 10.1016/j.burns.2022.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Akhoondian M, Zabihi MR, Yavari S, Karampoor M, Fouladpour A, Fallahpour M, et al. Identification of TGF-β1 expression pathway in the improvement of burn wound healing. Burns. 2022 doi: 10.1016/j.burns.2022.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Akhoondian M, Zabihi MR, Yavari S, Karampoor M, Fouladpour A, Samadnia A, et al. Burns may be a risk factor for endometriosis. Burns. 2022 doi: 10.1016/j.burns.2022.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Asadi K, Aris A, Fouladpour A, Ghazanfari MJ, Karkhah S, Salari A. Is the assessment of sympathetic skin response valuable for bone damage management of severe electrical burns? Burns. 2022 doi: 10.1016/j.burns.2022.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Salari A, Fouladpour A, Aris A, Ghazanfari MJ, Karkhah S, Asadi K. Osteoporosis in electrical burn injuries. Burns. 2022 doi: 10.1016/j.burns.2022.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Takasi P, Falakdami A, Vajargah PG, Mollaei A, Mehrabi H, Ghazanfari MJ, et al. Dissatisfaction or slight satisfaction with life in burn patients: A rising cause for concern of the world's burn community. Burns. 2022 doi: 10.1016/j.burns.2022.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Zabihi MR, Akhoondian M, Tajik MH, Mastalizadeh A, Mobayen M, Karkhah S. Burns as a risk factor for glioblastoma. Burns. 2022 doi: 10.1016/j.burns.2022.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Provençal S-C, Bond S, Rizkallah E, El-Baalbaki G. Hypnosis for burn wound care pain and anxiety: A systematic review and meta-analysis. Burns. 2018;44(8):1870–81. doi: 10.1016/j.burns.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 20.Furness PJ, Phelan I, Babiker NT, Fehily O, Lindley SA, Thompson AR. Reducing pain during wound dressings in burn care using virtual reality: a study of perceived impact and usability with patients and nurses. J Burn Care Res. 2019;40(6):878–85. doi: 10.1093/jbcr/irz106. [DOI] [PubMed] [Google Scholar]
- 21.Richardson P, Mustard L. The management of pain in the burns unit. Burns. 2009;35(7):921–36. doi: 10.1016/j.burns.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Abid S, Hussain T, Nazir A, Zahir A, Khenoussi N. Acetaminophen loaded nanofibers as a potential contact layer for pain management in Burn wounds. Mater Res Express. 2018;5(8):085017. [Google Scholar]
- 23.Ford CG, Manegold EM, Randall CL, Aballay AM, Duncan CL. Assessing the feasibility of implementing low-cost virtual reality therapy during routine burn care. Burns. 2018;44(4):886–95. doi: 10.1016/j.burns.2017.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahrer NE, Gold JI. The use of virtual reality for pain control: A review. Curr Pain Headache Rep. 2009;13(2):100–9. doi: 10.1007/s11916-009-0019-8. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Peña R, Beck W, et al. Immersive virtual reality as an adjunctive non-opioid analgesic for pre-dominantly Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: a pilot study. Front Hum Neurosci. 2019;13 doi: 10.3389/fnhum.2019.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ang SP, Montuori M, Trimba Y, Maldari N, Patel D, Chen QC. Recent applications of virtual reality for the management of pain in burn and pediatric patients. Curr Pain Headache Rep. 2021;25(1):1–8. doi: 10.1007/s11916-020-00917-0. [DOI] [PubMed] [Google Scholar]
- 27.D’Alessandro LN, Corrales IL, Klein S, Kondo D, Stinson J. Using virtual reality distraction during wound management: A brief case report in a patient with epidermolysis bullosa. Pediatric Pain Letter. 2022;24(1):1–7. [Google Scholar]
- 28.Khadra C, Ballard A, Paquin D, Cotes-Turpin C, Hoffman HG, Perreault I, et al. Effects of a projector-based hybrid virtual reality on pain in young children with burn injuries during hydrotherapy sessions: A within-subject randomized crossover trial. Burns. 2020;46(7):1571–84. doi: 10.1016/j.burns.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Phelan I, Furness PJ, Matsangidou M, Babiker NT, Fehily O, Thompson A, et al. Designing effective virtual reality environments for pain management in burn-injured patients. Virtual Real. 2021:1–15. doi: 10.1007/s10055-021-00552-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soltani M, Drever SA, Hoffman HG, Sharar SR, Wiechman SA, Jensen MP, et al. Virtual reality analgesia for burn joint flexibility: A randomized controlled trial. Rehabil Psychol. 2018;63(4):487. doi: 10.1037/rep0000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carr JR. Effectiveness of Virtual Reality on Reducing Pain in Burn Patients. 2021 [Google Scholar]
- 32.Konstantatos A, Angliss M, Costello V, Cleland H, Stafrace S. Predicting the effectiveness of virtual reality relaxation on pain and anxiety when added to PCA morphine in patients having burns dressings changes. Burns. 2009;35(4):491–9. doi: 10.1016/j.burns.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 33.Czech O, Wrzeciono A, Batalík L, Szczepańska-Gieracha J, Malicka I, Rutkowski S. Virtual reality intervention as a support method during wound care and rehabilitation after burns: A systematic review and meta-analysis. Complement Ther Med. 2022;68:102837. doi: 10.1016/j.ctim.2022.102837. [DOI] [PubMed] [Google Scholar]
- 34.Lauwens Y, Rafaatpoor F, Corbeel K, Broekmans S, Toelen J, Allegaert K. Immersive Virtual Reality as Analgesia during Dressing Changes of Hospitalized Children and Adolescents with Burns: A Systematic Review with Meta-Analysis. Children (Basel). 2020;7(11) doi: 10.3390/children7110194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;10(1) doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Corlett RT. Trouble with the gray literature. Biotropica. 2011;43(1):3–5. [Google Scholar]
- 37.John JR, Jani H, Peters K, Agho K, Tannous WK. The effectiveness of patient-centred medical home-based models of care versus standard primary care in chronic disease management: A systematic review and meta-analysis of randomised and non-randomised controlled trials. Int J Environ Res Public Health. 2020;17(18):6886. doi: 10.3390/ijerph17186886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernández-Férez A, Ventura-Miranda MI, Camacho-Ávila M, Fernández-Caballero A, Granero-Molina J, Fernández-Medina IM, et al. Nursing Interventions to Facilitate the Grieving Process after Perinatal Death: A Systematic Review. Int J Environ Res Public Health. 2021;18(11):5587. doi: 10.3390/ijerph18115587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons: 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoffman HG, Patterson DR, Carrougher GJ, Sharar SR. Effectiveness of virtual reality–based pain control with multiple treatments. Clin J Pain. 2001;17(3):229–35. doi: 10.1097/00002508-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Das DA, Grimmer KA, Sparnon AL, McRae SE, Thomas BH. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial [ISRCTN87413556] BMC Pediatr. 2005;5(1):1–10. doi: 10.1186/1471-2431-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, Patterson DR. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Arch Phys Med Rehabil. 2007;88(12):S43–S9. doi: 10.1016/j.apmr.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 43.van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J Burn Care Res. 2007;28(5):694–702. doi: 10.1097/BCR.0B013E318148C96F. [DOI] [PubMed] [Google Scholar]
- 44.Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24(4):299–304. doi: 10.1097/AJP.0b013e318164d2cc. [DOI] [PubMed] [Google Scholar]
- 45.Mott J, Bucolo S, Cuttle L, Mill J, Hilder M, Miller K, et al. The efficacy of an augmented virtual reality system to alleviate pain in children undergoing burns dressing changes: a randomised controlled trial. Burns. 2008;34(6):803–8. doi: 10.1016/j.burns.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 46.Carrougher GJ, Hoffman HG, Nakamura D, Lezotte D, Soltani M, Leahy L, et al. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. 2009;30(5):785–91. doi: 10.1097/BCR.0b013e3181b485d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morris LD, Louw QA, Crous LC. Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. Burns. 2010;36(5):659–64. doi: 10.1016/j.burns.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 48.Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K, McGhee LL, et al. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J Trauma. 2011;71(10):S125. doi: 10.1097/TA.0b013e31822192e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, Soltani M, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011;37(1):61–8. doi: 10.1016/j.burns.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns. 2012;38(5):650–7. doi: 10.1016/j.burns.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 51.Faber AW, Patterson DR, Bremer M. Repeated use of immersive virtual reality therapy to control pain during wound dressing changes in pediatric and adult burn patients. J Burn Care Res. 2013;34(5):563–8. doi: 10.1097/BCR.0b013e3182777904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jeffs D, Dorman D, Brown S, Files A, Graves T, Kirk E, et al. Effect of virtual reality on adolescent pain during burn wound care. J Burn Care Res. 2014;35(5):395–408. doi: 10.1097/BCR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 53.Hua Y, Qiu R, Yao W-y, Zhang Q, Chen X-l. The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. Pain Manag Nurs. 2015;16(5):685–91. doi: 10.1016/j.pmn.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 54.Ebrahimi H, Namdar H, Ghahramanpour M, Ghafourifard M, Musavi S. Effect of virtual reality method and multimedia system on burn patients’ pain during dressing. J Clin Anal Med. 2017;8(suppl 5):485–9. [Google Scholar]
- 55.Khadra C, Ballard A, Déry J, Paquin D, Fortin J-S, Perreault I, et al. Projector-based virtual reality dome environment for procedural pain and anxiety in young children with burn injuries: a pilot study. J Pain Res. 2018;11:343–53. doi: 10.2147/JPR.S151084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McSherry T, Atterbury M, Gartner S, Helmold E, Searles DM, Schulman C. Randomized, crossover study of immersive virtual reality to decrease opioid use during painful wound care procedures in adults. J Burn Care Res. 2018;39(2):278–85. doi: 10.1097/BCR.0000000000000589. [DOI] [PubMed] [Google Scholar]
- 57.Fatma A, Ghada AH. Effect of virtual reality technology on pain during dressing change among children with burn injuries. J Nurs Healthc Res. 2019;8(6):37–46. [Google Scholar]
- 58.Phelan I, Furness PJ, Fehily O, Thompson AR, Babiker NT, Lamb MA, et al. A mixed-methods investigation into the acceptability, usability, and perceived effectiveness of active and passive virtual reality scenarios in managing pain under experimental conditions. J Burn Care Res. 2019;40(1):85–90. doi: 10.1093/jbcr/iry052. [DOI] [PubMed] [Google Scholar]
- 59.Hoffman HG, Patterson DR, Rodriguez RA, Peña R, Beck W, Meyer WJ. Virtual reality analgesia for children with large severe burn wounds during burn wound debridement. Front Virtual Real. 2020;1:32. doi: 10.3389/frvir.2020.602299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Joo SY, Cho YS, Lee SY, Seok H, Seo CH. Effects of virtual reality-based rehabilitation on burned hands: a prospective, randomized, single-blind study. J Clinical Med. 2020;9(3):731–42. doi: 10.3390/jcm9030731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kiani M, Manshaee G, Ghamarani A, Rasti H. Comparing the Effectiveness of Drug Therapy and Virtual Reality on Pain Anxiety and Pain Severity of Burn Patients. Iran J Psychiatric Nurs. 2020;8(2):45–56. [Google Scholar]
- 62.Xiang H, Shen J, Wheeler KK, Patterson J, Lever K, Armstrong M, et al. Efficacy of smartphone active and passive virtual reality distraction vs standard care on burn pain among pediatric patients: A randomized clinical trial. JAMA Netw Open. 2021;4(6):e2112082. doi: 10.1001/jamanetworkopen.2021.12082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ali RR, Selim AO, Ghafar MAA, Abdelraouf OR, Ali OI. Virtual reality as a pain distractor during physical rehabilitation in pediatric burns. Burns. 2022;48(2):303–8. doi: 10.1016/j.burns.2021.04.031. [DOI] [PubMed] [Google Scholar]
- 64.Armstrong M, Lun J, Groner JI, Thakkar RK, Fabia R, Noffsinger D, et al. Mobile Phone Virtual Reality Game for Pediatric Home Burn Dressing Pain Management, a Randomized Clinical Trial. Pilot Feasibility Stud. 2022;8:186. doi: 10.1186/s40814-022-01150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Baartmans M, De Jong A, Van Baar M, Beerthuizen G, Van Loey N, Tibboel D, et al. Early management in children with burns: Cooling, wound care and pain management. Burns. 2016;42(4):777–82. doi: 10.1016/j.burns.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 66.Van Der Heijden MJ, de Jong A, Rode H, Martinez R, van Dijk M. Assessing and addressing the problem of pain and distress during wound care procedures in paediatric patients with burns. Burns. 2018;44(1):175–82. doi: 10.1016/j.burns.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 67.Mobayen M, Feizkhah A, Mirmasoudi SS, Bejarpasi ZP, Bejarbane EJ, Habibiroudkenar P, et al. Nature efficient approach; Application of biomimetic nanocomposites in burn injuries. Burns. 2022;48(6):1525–6. doi: 10.1016/j.burns.2022.06.020. [DOI] [PubMed] [Google Scholar]
- 68.Jeddi FR, Mobayen M, Feizkhah A, Farrahi R, Heydari S, Toolaroud PB. Cost Analysis of the Treatment of Severe Burn Injuries in a Tertiary Burn Center in Northern Iran. Iran Red Crescent Med J. 2022;24(5):e1522. [Google Scholar]
- 69.Mobayen M, Sadeghi M. Prevalence and related factors of electrical burns in patients referred to Iranian medical centers: a systematic review and meta-analysis. World J Plast Surg. 2022;11(1):3. doi: 10.52547/wjps.11.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mobayen M, Zarei R, Masoumi S, Shahrousvand M, Mazloum SMH, Ghaed Z, et al. Epidemiology of Childhood Burn: A 5-Year Retrospective Study in the Referral Burn Center of Northern Iran Northern Iran. Casp J Health Res. 2021;6(3):101–8. [Google Scholar]
- 71.Haghdoost Z, Mobayen M, Omidi S. Predicting hope to be alive using spiritual experiences in burn patients. Ann Rom Soc Cell Biol. 2021;25(4):18957–62. [Google Scholar]
- 72.Mobayen M, Rimaz S, Malekshahi A. Evaluation of clinical and laboratory causes of burns in pre-school children. J Curr Biomed Rep. 2021;2(1):27–31. [Google Scholar]
- 73.Chukamei ZG, Mobayen M, Toolaroud PB, Ghalandari M, Delavari S. The length of stay and cost of burn patients and the affecting factors. Int J Burns Trauma. 2021;11(5):397. [PMC free article] [PubMed] [Google Scholar]
- 74.Khodayary R, Nikokar I, Mobayen MR, Afrasiabi F, Araghian A, Elmi A, et al. High incidence of type III secretion system associated virulence factors (exoenzymes) in Pseudomonas aeruginosa isolated from Iranian burn patients. BMC Res Notes. 2019;12(1):1–6. doi: 10.1186/s13104-019-4071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rimaz S, Moghadam AD, Mobayen M, Nasab MM, Rimaz S, Aghebati R, et al. Changes in serum phosphorus level in patients with severe burns: a prospective study. Burns. 2019;45(8):1864–70. doi: 10.1016/j.burns.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 76.Ghavami Y, Mobayen MR, Vaghardoost R. Electrical burn injury: a five-year survey of 682 patients. Trauma Mon. 2014;19(4):e18748. doi: 10.5812/traumamon.18748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Amir Alavi S, Mobayen MR, Tolouei M, Noursalehi I, Gholipour A, Gholamalipour N, et al. Epidemiology and outcome of burn injuries in burn patients in Guilan province, Iran. Qom Univ Med Sci J. 2013;7(5):35–41. [Google Scholar]
- 78.Alavi CE, Salehi SH, Tolouei M, Paydary K, Samidoust P, Mobayen M. Epidemiology of burn injuries at a newly established burn care center in rasht. Trauma Mon. 2012;17(3):341. doi: 10.5812/traumamon.6991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chan E, Foster S, Sambell R, Leong P. Clinical efficacy of virtual reality for acute procedural pain management: a systematic review and meta-analysis. PloS One. 2018;13(7):e0200987. doi: 10.1371/journal.pone.0200987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gold JI, Mahrer NE. Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol. 2018;43(3):266–75. doi: 10.1093/jpepsy/jsx129. [DOI] [PubMed] [Google Scholar]
- 81.Chuan A, Zhou J, Hou R, Stevens CJ, Bogdanovych A. Virtual reality for acute and chronic pain management in adult patients: a narrative review. Anaesthesia. 2021;76(5):695–704. doi: 10.1111/anae.15202. [DOI] [PubMed] [Google Scholar]
- 82.Pourmand A, Davis S, Marchak A, Whiteside T, Sikka N. Virtual reality as a clinical tool for pain management. Curr Pain Headache Rep. 2018;22(8):1–6. doi: 10.1007/s11916-018-0708-2. [DOI] [PubMed] [Google Scholar]
- 83.Mallari B, Spaeth EK, Goh H, Boyd BS. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019;12:2053. doi: 10.2147/JPR.S200498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wittkopf PG, Lloyd DM, Coe O, Yacoobali S, Billington J. The effect of interactive virtual reality on pain perception: a systematic review of clinical studies. Disabil Rehabil. 2020;42(26):3722–33. doi: 10.1080/09638288.2019.1610803. [DOI] [PubMed] [Google Scholar]
- 85.Shahrbanian S, Ma X, Aghaei N, N K-B, Simmonds M. Use of virtual reality (immersive v non immersive) for pain management in children and adults: A systematic review of evidence from randomized controlled trials. Euro J Exp Bio. 2012;2:1408–22. [Google Scholar]