Abstract
This research differentiated childhood unpredictability (i.e., perceptions of uncertainty or instability due to turbulent environmental changes) from other related constructs to identify its role in adult health. Study 1 (N = 441) showed that, beyond other childhood adversity variables (poverty and adverse childhood experiences or ACEs) and demographic characteristics, perceptions of unpredictability were associated with greater functional disability and worse health-related quality of life (assessed via the CDC’s HRQOL Healthy Days measure and the RAND SF-36). Study 2 (N = 564) replicated those findings in a more racially diverse sample and showed that associations with childhood unpredictability held while also controlling for the Big 5 personality traits. Findings suggest that effects of unpredictability were especially pronounced among Hispanic (in Study 1), and Black/African American and low-income participants (in Study 2). Experiencing childhood environments that are perceived to be uncertain, unstable, or uncontrollable may put children on a path toward poor health outcomes in adulthood. Findings advance theories of child adversity and health and identify childhood unpredictability as a potentially valuable target for intervention.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10865-022-00373-8.
Keywords: Development, Child adversity, Life history theory, Chronic disease, Evolution
Introduction
A range of health problems in adulthood have been linked with exposure to adverse experiences in childhood (Adler et al., 1993; Bradley & Corwyn, 2002; Chen et al., 2002; Ehrlich et al., 2016). Adults who experienced low-income, abusive, or traumatic childhoods are at substantially higher risk for experiencing chronic disease, physical and emotional disability, and low health-related quality of life (Boyce & Ellis, 2005; Chen & Miller, 2013; Miller et al., 2011). Despite the consistency of such findings, the field lacks a clear understanding of what psychological processes are responsible for translating adverse childhood experiences into negative adult health outcomes. Although many studies document the contribution of early life stress to adult health outcomes (e.g., Dube et al., 2001, 2003; Felliti et al., 1998), such research at times leaves uninvestigated the specific cognitive mechanisms that may explain effects of child adversity on adult health. Identifying those mechanisms provides key information about the psychological, behavioral, and neuroendocrine pathways through which childhood experiences affect adult health and offers insight into potentially valuable targets for intervention. The current study is the first to assess perceptions of childhood unpredictability—the extent to which childhood experiences are characterized by perceptions of uncertainty or instability due to turbulent changes in the environment—to evaluate their role in adult functional health status and health-related quality of life.
The role of perceived unpredictability
Theories of adaptive calibration (e.g., Del Giudice et al., 2011) such as life history theory (Belsky et al., 2012; Brumbach et al., 2009; Cabeza de Baca et al., 2016; Ellis et al., 2009; McDade, 2003) suggest that, early in childhood, psychological, behavioral, and neuroendocrine processes are calibrated to the perceived level of unpredictability in one’s environment (Del Giudice, 2009; Ellis & Del Giudice, 2019). Childhood unpredictability is characterized by the presence of uncertainty or instability due to turbulent changes in the environment. The core element of unpredictability involves the perception of social and physical threats that are inconsistent across time and situations and are, therefore, unpredictable. For example, perceptions of unpredictability can stem from inconsistency across time in the degree of support a child receives from their primary caregiver, uncertainty in a child’s ongoing interactions with teachers and peers, or variability in a child’s daily schedule or routines.
Perceived unpredictability may serve as a mechanism through which adverse childhood experiences (ACEs) affect health into adulthood. Many adverse childhood experiences, such as those involving trauma, abuse, and neglect (e.g., Dube et al., 2001; Felitti et al., 1998), as well as inconsistent caregiving and access to social support (e.g., Baram et al., 2012; Gee & Cohodes, 2021) are likely to contribute to perceptions of unpredictability. Such experiences can destabilize the social (or physical) environment and generate perceived threats that vary uncontrollably across time and situations. Some parental divorces, for example, can create home environments that are chaotic, hostile, or unsupportive (Kelly & Emery, 2003), and thus can contribute to feelings of unpredictability (Doom et al., 2016; Martinez et al., 2022).
Yet, the broader construct of unpredictability is not effectively captured by existing measures of ACEs, which focus narrowly on whether people were ever exposed to particular experiences during childhood, rather than on the degree to which they were exposed to those experiences or the extent to which those experiences were perceived to vary unpredictably across time and situations. For example, the quality of home environments for children whose parents divorce can range from routinized and predictable to chaotic and unsupportive (Kelly & Emery, 2003). Thus, simply assessing whether one’s parents divorced fails to capture the quality of the home experience or how predictable versus unpredictable it was perceived to be.
Perceptions of childhood unpredictability are also distinct from the experience of poverty. Poverty entails resource scarcity and often includes exposure to financial hardship, inadequate nutrition, poor physical living conditions, and lack of access to health care services (Chen & Miller, 2013). Effects of poverty are well-represented in models of allostatic load, toxic stress, and chronic deprivation, all of which encompass a focus on lack of access to resources (McEwen & Stellar, 1993; McLaughlin & Sheridan, 2016). However, whereas poverty often entails financial hardship experienced in a relatively consistent manner across time and situations, unpredictability entails the perception of social and physical threats that are highly variable and that often come from sources other than financial hardship (e.g., unstable relationships with caregivers). Thus, while poverty and unpredictability are correlated, they are conceptually and operationally distinct (see Maranges et al., 2022; Martinez et al., 2022).
Perceptions of childhood unpredictability and adult health
The current research is the first to pinpoint perceptions of childhood unpredictability as a potentially important contributor to adult health outcomes. This research addressed three overarching hypotheses. First, two studies tested the hypothesis that perceptions of unpredictability would be robustly associated with adult functional ability and health-related quality of life over and above poverty and ACEs, while controlling for demographic covariates (age, gender, racial and ethnic minority status, and current household income) and personality traits. Second, the studies used mediational analyses to test the hypothesis that perceptions of unpredictability might mediate associations between ACEs and adult health outcomes, i.e., that ACEs damage health in part because those experiences generate feelings of unpredictability. Third, the studies assessed whether effects of unpredictability are larger among populations who, by virtue of their race, ethnicity, or social class, may be characterized by high levels of stress due to prejudice, discrimination, or lack of financial resources. We reasoned that such populations may be especially vulnerable to experiencing cumulative effects of unpredictable environments. We thus assessed possible moderating effects of race, ethnicity, and current income.
This article reports findings from two studies. Study 1 provided preliminary tests of the three research questions above by including a relatively wide range of measures reflecting functional health status and health-related quality of life. Study 2 targeted a smaller number of outcome measures, included additional measures of personality traits to serve as covariates, and recruited a larger and more diverse sample. Thus, while Study 1 provided initial tests of the associations between childhood unpredictability and health outcomes, Study 2 replicated and extended Study 1 by allowing for a stronger assessment of whether those relationships depend on demographic group and whether they hold over and above basic aspects of personality.
Study 1
Method
Participants
An online community sample of 520 U.S. participants was recruited via CloudResearch. All adult participants were eligible to participate. Based on a priori criteria, 79 participants who failed one or more of three attention checks embedded in self-report items (e.g., “For this question please select strongly disagree”) were excluded from analyses. The final sample included 441 participants. Participants were compensated $0.50. See Table 1 for sample demographic characteristics. Data were collected in April–May, 2020. The study was approved by the Florida State University Institutional Review Board (IRB) and informed consent was obtained from all participants prior to participation. Data and data analytic syntax for both studies can be accessed here: https://osf.io/m69sq/?view_only=6a63862623d74ad2a23572e3d8fbdde7
Table 1.
Sample demographic characteristics
| Study 1 | Study 2 | |
|---|---|---|
| Variable | N (%) or M (SD) | N (%) or M (SD) |
| Age (years) |
M = 32.07, SD = 11.20 Range = 18–70 |
M = 38.00, SD = 12.47Range = 18–76 |
| Gender | 208 men, 232 women, 1 other | 201 men, 356 women, 3 nonbinary, 4 other |
| Race | ||
| American Indian | 8 (2%) | 4 (1%) |
| Asian | 51 (12%) | 31 (5%) |
| Native Hawaiian/Pacific | ||
| Islander | 2 (< 1%) | 1 (< 1%) |
| Black or African American | 36 (8%) | 201 (36%) |
| White | 311 (71%) | 303 (54%) |
| Multi-racial | 16 (4%) | 14 (2%) |
| Unknown/Did not report | 8 (2%) | 8 (1%) |
| Other | 9 (2%) | 2 (< 1%) |
| Hispanic or Latino | ||
| Yes | 90 (20%) | 46 (8%) |
| No | 332 (75%) | 507 (90%) |
| Unknown/Did not report | 19 (4%) | 11 (2%) |
| Current annual household | ||
| Income | ||
| $10,000 or less | 22 (5%) | 30 (5%) |
| $10,001–$19,999 | 28 (6%) | 34 (6%) |
| $20,000–$29,999 | 58 (13%) | 47 (8%) |
| $30,000–$39,999 | 52 (12%) | 75 (13%) |
| $40,000–$49,999 | 32 (7%) | 56 (10%) |
| $50,000–$59,999 | 42 (10%) | 64 (11%) |
| $60,000–$69,999 | 24 (5%) | 45 (8%) |
| $70,000–$79,999 | 43 (10%) | 50 (9%) |
| $80,000–$89,999 | 23 (5%) | 31 (5%) |
| $90,001–$99,999 | 25 (6%) | 21 (4%) |
| $100,000–$150,000 | 53 (12%) | 75 (13%) |
| $150,001 or more | 39 (9%) | 36 (6%) |
Percentages may not total 100% due to rounding error
Measures
Perceptions of Childhood Unpredictability. Fifteen items validated in previous work (Maranges et al., 2022) assessed perceived unpredictability during the first 10 years of childhood (e.g., “I never knew when my parents would be there to pick me up from school”, “I often did not know what to expect from other kids at school”, “When I left my house I was never quite certain what would happen in my neighborhood”) (1 = strongly disagree, 7 = strongly agree) (M = 3.13, SD = 1.53, range = 1.00 to 6.93, α = 0.95). The scale has been shown to demonstrate strong convergent, discriminant, and predictive validity (Maranges et al., 2022).
Perceptions of Childhood Poverty. Eleven items from previous work (Maranges et al., 2021, 2022) assessed perceptions of childhood poverty and financial hardship (e.g., “My family rarely had enough money to go out for a nice dinner”, “My family was strained financially”, “I felt relatively wealthy compared with other kids in my school”; reverse-scored). (1 = strongly disagree, 7 = strongly agree) (M = 3.83, SD = 1.42, range = 1.00 to 7.00, α = 0.91).
Adverse Child Experiences (ACEs; Dube et al., 2001). The ACEs scale was originally generated for the CDC-Kaiser Permanente Adverse Childhood Experiences study, a comprehensive study of childhood abuse and neglect (Felitti et al., 1998). The current study used the ACEs scale later adapted by Dube et al. (2001) to include a 10-item checklist assessing three forms of abuse (emotional, physical, sexual), two forms of neglect (emotional, physical), and five forms of household dysfunction including exposure to domestic violence, substance use, divorce, mental illness, and criminal activity (all experienced through age 18). Responses were summed to produce a total ACEs score (M = 2.89, SD = 2.67, scores ranged from 0 to 10).
CDC’s Health-Related Quality of Life (HRQOL; CDC, 1993). The HRQOL has been used extensively to assess health-related quality of life and is included in the Behavioral Risk Factor Surveillance System, the National Health and Nutrition Examination Survey, and the Medicare Health Outcomes Survey. The HRQOL consists of two separate modules. The core module prompts participants to report the number of days (out of the past 30) in which they experienced poor physical health and mental health. Based on CDC guidelines, those two items were averaged to provide a core measure of unhealthy days (M = 14.40, SD = 10.83, α = 0.70). The symptoms module includes five items to assess the number of days (out of the past 30 days) in which (1) pain caused participants to limit their activities, (2) they felt sad or depressed, (3) they felt anxious, (4) they did not get enough rest or sleep, and (5) they felt healthy and full of energy. Items were averaged after reverse-scoring the final item (M = 11.26, SD = 6.57, α = 0.78). Higher scores indicate worse health-related quality of life. The CDC HRQOL demonstrates strong psychometric properties in both community and clinical settings (Mielenz et al., 2006).
RAND SF-36 (RAND, 1995). The 36-item SF-36 assesses functional ability and includes eight subscales assessing Physical Functioning, Role Limitations due to Physical Health, Role Limitations due to Emotional Health, Energy/Fatigue, Emotional Well-Being, Social Functioning, Pain, and General Health. Subscale scores were calculated according to RAND’s guidelines. Scoring instructions can be found at https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html. Higher scores reflect better health-related functional ability. The SF-36 demonstrates strong psychometric properties, as well as predictive validity for both physical and mental health diagnostic outcomes (Elliott et al., 2003; Parshall et al., 2008).
Statistical approach
Preliminary analyses assessed correlations among all variables. Primary analyses first used multiple regression to assess independent associations between outcome variables (CDC HRQOL core and symptoms modules and SF-36 subscales), experiences of childhood unpredictability and poverty, and ACEs. We included age, gender, race, ethnicity, and current household income as demographic covariates. To differentiate racial/ethnic minority and majority participants, we focused on differences between participants identifying as Black/African American (vs non-Black) or Hispanic/Latino (vs non-Hispanic). Second, mediational analyses (using the Model 4 PROCESS macro in SPSS; Hayes, 2017) assessed whether perceived unpredictability might serve as a psychological mechanism explaining the link between ACEs and adult health outcomes. Third, regression analyses examined whether any effects of unpredictability might be moderated by participant race, ethnicity, or income. Because the SF-36 consists of eight subscales, for analyses of the SF-36 we used a conservative Bonferroni correction to reduce alpha inflation and avoid Type I error. The alpha level used to determine statistical significance was 0.05/8 = 0.00625. Study 2 provided a more targeted focus on two outcome variables (CDC’s HRQOL core module and the SF-36 Physical Functioning subscale). To facilitate comparison across the two studies, presentation of Study 1 results in the main text highlights those two outcome variables. There were no missing data in this study. To simplify statistical models, only participants self-identifying as male or female were included. Sensitivity analysis indicated that the study was well-powered (> 0.80) to detect effect sizes as small as r = 0.13 in both correlational analyses and regression analyses with 8 predictors.
Results
Correlations among variables are reported in Table 2, which includes all predictors and the two outcomes included in both studies (CDC HRQOL core module and SF-36 Physical Functioning scale). Correlations that include all 10 outcomes are in Supplemental Materials Table S1. Perceived childhood unpredictability, poverty, and ACEs were all moderately to strongly correlated, and all three were significantly correlated with all of the outcome measures.
Table 2.
Correlations among predictor variables and health-related outcome measures (studies 1 and 2)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. CDC HRQOL | – | − 0.47*** | 0.35*** | 0.19*** | 0.29*** | − 0.15*** | − 0.16*** | 0.02 | − 0.01 | − 0.06* |
| 2. Physical Functioning | − 0.41*** | – | − 0.32*** | − 0.18*** | − 0.23*** | 0.10* | − 0.19*** | − 0.01 | − 0.03 | 0.16*** |
| 3. Unpred ictability | 0.46*** | − 0.58*** | – | 0.49*** | 0.69*** | − 0.19*** | − 0.17*** | − 0.09* | 0.09* | − 0.17*** |
| 4. Poverty | 0.28*** | − 0.21*** | 0.54*** | – | 0.44*** | − 0.19*** | 0.04 | − 0.00 | 0.05 | − 0.06 |
| 5. ACEs | 0.44*** | − 0.36*** | 0.67*** | 0.41*** | – | − 0.16*** | − 0.08 | 0.08* | 0.10* | − 0.05 |
| 6. Annual Income | − 0.11* | 0.16** | − 0.21*** | − 0.20*** | − 0.24*** | – | 0.05 | 0.03 | − 0.19*** | 0.04 |
| 7. Age | 0.08 | − 0.29*** | 0.22*** | 0.11* | 0.23*** | 0.11* | – | 0.07 | − 0.11* | 0.08 |
| 8. Gender | 0.02 | 0.16** | − 0.17*** | − 0.05 | − 0.02 | − 0.05 | − 0.20*** | – | 0.03 | 0.07 |
| 9. Race | − 0.05 | 0.01 | − 0.02 | − 0.04 | − 0.01 | − 0.17*** | − 0.04 | 0.02 | – | 0.00 |
| 10. Ethnicity | 0.07 | − 0.18*** | 0.17*** | 0.12* | 0.12* | − 0.08 | − 0.02 | − 0.01 | − 0.05 | – |
Study 1 (N = 440) is below the diagonal; Study 2 (N = 557) is above the diagonal. Gender: 1 = Male, 2 = Female; Race: 0 = non-Black/African American, 1 = Black/African American, Ethnicity: 0 = non-Hispanic, 1 = Hispanic. Correlations with race, ethnicity, and gender reflect Pearson point biserial correlations. ***p < 0.001, **p < 0.01, *p < 0.05
Regression analyses for all outcomes are reported in Table 3. Once the overlap among predictors was taken into account, we observed significant associations between childhood unpredictability and nine out of ten outcome measures (the one exception was the energy/fatigue SF-36 subscale).
Table 3.
Study 1 Regression analyses: predictors of functional ability and health-related quality of life
| Beta | t | p | Partial r | |
|---|---|---|---|---|
| CDC HRQOL | ||||
| Core module | ||||
| Unpredictability | 0.31 | 4.92 | < 0.001 | 0.23 |
| Poverty | 0.03 | 0.56 | 0.58 | 0.03 |
| ACEs | 0.23 | 3.98 | < 0.001 | 0.19 |
| Age | − 0.04 | − 0.79 | 0.43 | − 0.04 |
| Gender | 0.07 | 1.62 | 0.11 | 0.08 |
| Current income | 0.01 | 0.31 | 0.76 | 0.02 |
| Black | − 0.04 | − 0.99 | 0.32 | − 0.05 |
| Hispanic | − 0.02 | − 0.44 | 0.66 | − 0.02 |
| Symptoms module | ||||
| Unpredictability | 0.23 | 3.62 | < 0.001 | 0.17 |
| Poverty | 0.07 | 1.37 | 0.17 | 0.07 |
| ACEs | 0.29 | 5.11 | < 0.001 | 0.24 |
| Age | − 0.02 | − 0.48 | 0.63 | − 0.02 |
| Gender | 0.13 | 3.00 | 0.003 | 0.14 |
| Current income | − 0.01 | − 0.21 | 0.84 | − 0.01 |
| Black | − 0.07 | − 1.69 | 0.09 | − 0.08 |
| Hispanic | − 0.03 | − 0.81 | 0.42 | − 0.04 |
| RAND SF-36 | ||||
| Physical functioning | ||||
| Unpredictability | − 0.63 | − 11.14 | < 0.001 | − 0.47 |
| Poverty | 0.15 | 3.25 | 0.001 | 0.16 |
| ACEs | 0.09 | 1.63 | 0.10 | 0.08 |
| Age | − 0.19 | − 4.78 | < 0.001 | − 0.22 |
| Gender | 0.03 | 0.72 | 0.47 | 0.04 |
| Current income | 0.09 | 2.18 | 0.03 | 0.11 |
| Black | 0.01 | 0.34 | 0.74 | 0.02 |
| Hispanic | − 0.10 | − 2.58 | 0.01 | − 0.12 |
| Role limitations-physical | ||||
| Unpredictability | − 0.47 | − 7.46 | < 0.001 | − 0.34 |
| Poverty | 0.05 | 0.97 | 0.34 | 0.05 |
| ACEs | − 0.01 | − 0.16 | 0.87 | − 0.01 |
| Age | − 0.06 | − 1.44 | 0.15 | − 0.07 |
| Gender | 0.00 | 0.03 | 0.98 | 0.00 |
| Current income | 0.10 | 2.16 | 0.03 | 0.10 |
| Black | − 0.02 | − 0.37 | 0.71 | − 0.02 |
| Hispanic | − 0.03 | − 0.79 | 0.43 | − 0.04 |
| Role limitations-emotional | ||||
| Unpredictability | − 0.25 | − 3.87 | < 0.001 | − 0.18 |
| Poverty | 0.02 | 0.29 | 0.78 | 0.01 |
| ACEs | − 0.22 | − 3.75 | < 0.001 | − 0.18 |
| Age | 0.11 | 2.45 | 0.02 | 0.12 |
| Gender | − 0.18 | − 3.98 | < 0.001 | − 0.19 |
| Current income | − 0.02 | − 0.34 | 0.74 | − 0.02 |
| Black | 0.10 | 2.26 | 0.03 | 0.11 |
| Hispanic | 0.08 | 1.89 | 0.06 | 0.09 |
| Energy/fatigue | ||||
| Unpredictability | − 0.06 | − 0.91 | 0.37 | − 0.04 |
| Poverty | − 0.10 | − 1.84 | 0.07 | − 0.09 |
| ACEs | − 0.21 | − 3.46 | 0.001 | − 0.16 |
| Age | 0.17 | 3.57 | < 0.001 | 0.17 |
| Gender | − 0.20 | − 4.38 | < 0.001 | − 0.21 |
| Current income | − 0.01 | − 0.14 | 0.89 | − 0.01 |
| Black | 0.03 | 0.61 | 0.54 | 0.03 |
| Hispanic | 0.16 | 3.51 | < 0.001 | 0.17 |
| Emotional well-being | ||||
| Unpredictability | − 0.20 | − 2.96 | 0.003 | − 0.14 |
| Poverty | − 0.07 | − 1.30 | 0.20 | − 0.06 |
| ACEs | − 0.22 | − 3.71 | < 0.001 | − 0.18 |
| Age | 0.11 | 2.27 | 0.02 | 0.11 |
| Gender | − 0.08 | − 1.86 | 0.06 | − 0.09 |
| Current income | 0.04 | 0.80 | 0.42 | 0.04 |
| Black | 0.06 | 1.23 | 0.22 | 0.06 |
| Hispanic | 0.11 | 2.53 | 0.01 | 0.12 |
| Social functioning | ||||
| Unpredictability | − 0.40 | − 6.33 | < 0.001 | − 0.29 |
| Poverty | − 0.00 | − 0.03 | 0.98 | − 0.00 |
| ACEs | − 0.13 | − 2.19 | 0.03 | − 0.11 |
| Age | 0.00 | 0.02 | 0.98 | 0.00 |
| Gender | − 0.15 | − 3.38 | 0.001 | − 0.16 |
| Current income | 0.06 | 1.30 | 0.19 | 0.06 |
| Black | 0.02 | 0.53 | 0.60 | 0.03 |
| Hispanic | − 0.01 | − 0.33 | 0.74 | − 0.02 |
| Pain | ||||
| Unpredictability | − 0.51 | − 8.33 | < 0.001 | − 0.37 |
| Poverty | 0.07 | 1.36 | 0.17 | 0.07 |
| ACEs | − 0.01 | − 0.20 | 0.85 | − 0.01 |
| Age | − 0.17 | − 3.95 | < 0.001 | − 0.19 |
| Gender | − 0.05 | − 1.18 | 0.24 | − 0.06 |
| Current income | 0.07 | 1.58 | 0.11 | 0.08 |
| Black | 0.04 | 1.04 | 0.30 | 0.05 |
| Hispanic | 0.01 | 0.28 | 0.78 | 0.01 |
| General health | ||||
| Unpredictability | − 0.24 | − 3.73 | < 0.001 | − 0.18 |
| Poverty | − 0.10 | − 1.99 | 0.05 | − 0.10 |
| ACEs | − 0.15 | − 2.57 | 0.01 | − 0.12 |
| Age | − 0.02 | − 0.37 | 0.71 | − 0.02 |
| Gender | − 0.17 | − 3.76 | < 0.001 | − 0.18 |
| Current income | 0.08 | 1.64 | 0.10 | 0.08 |
| Black | 0.00 | 0.01 | 10.00 | 0.00 |
| Hispanic | 0.06 | 1.28 | 0.20 | 0.06 |
N = 440. Gender: 1 = Male, 2 = Female. Race: 0 = non-Black/African American, 1 = Black/African American. Ethnicity: 0 = non-Hispanic, 1 = Hispanic. For the CDC HRQOL measures, higher scores indicate worse health-related quality of life. For the SF-36 measures, higher scores reflect higher health-related functional ability
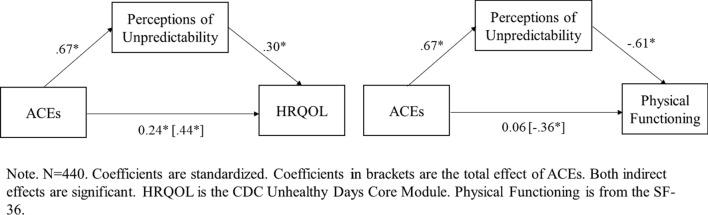
We next tested whether perceived unpredictability statistically mediated the association between ACEs and each outcome measure. The indirect effect was significant for all outcome variables except for the energy/fatigue subscale of the SF-36 (see Supplemental Materials Table S2). Figure 1 depicts the mediation model for the CDC HRQOL core module and the SF-36 Physical Functioning scale. Both standardized indirect effects were significant (HRQOL: Z = 0.20, SE = 0.04, CI [0.11, 0.28]; Physical Functioning: Z = − 0.41, SE = 0.04, CI [− 0.49, − 0.34]).
Fig. 1.
Study 1 Mediating effects of perceived childhood unpredictability
Moderation analyses assessed possible moderating effects of race, ethnicity, and income. To ensure that any moderated effects were independent of one another, we included centered interaction terms between unpredictability and race, ethnicity, and income simultaneously in the regression models. See Supplemental Materials Table S3 for full moderation results. For the CDC HRQOL symptoms module, we observed a significant interaction between childhood unpredictability and ethnicity, B = 0.11, t = 2.51, p = 0.01. Simple slopes analyses showed that unpredictability was more strongly tied to poor HRQOL in Hispanic, B = 0.43, t = 4.25, p < 0.001, relative to non-Hispanic, B = 0.16, t = 2.47, p = 0.01, participants. Although the moderated effect for the HRQOL core module only approached significance, B = 0.07, t = 1.68, p = 0.09, the pattern of simple slopes was similar to that for the symptoms module: Unpredictability was more strongly tied to poor HRQOL in Hispanic, B = 0.45, t = 4.37, p < 0.001, relative to non-Hispanic, B = 0.27, t = 3.98, p < 0.001, participants (see Supplemental Materials Fig. S1). No significant moderating effects were found for the SF-36 subscales; although some were significant at the 0.05 level, none were significant at the more conservative 0.00625 level (see Supplemental Materials Table S3).
Discussion
Study 1 provides preliminary evidence for robust connections between perceptions of childhood unpredictability and adult health-related quality of life and functional ability. Those connections were observed over and above ACEs, perceptions of resource scarcity, and a range of demographic variables. Indeed, reports of experiencing an unpredictable childhood were at least as consistent a predictor as having faced high levels of poverty or ACEs. Although tests of mediation are limited by the cross-sectional nature of the study, findings are consistent with the hypothesis that perceived unpredictability might explain the association between ACEs and adult HRQOL and functional disability. We saw some evidence for moderating effects of ethnicity, such that perceptions of unpredictability were tied to low HRQOL more strongly for Hispanic than non-Hispanic participants. This pattern provides preliminary evidence that effects of unpredictability may be pronounced among members of underrepresented groups at relatively high risk for experiencing stress associated with discrimination. No moderating effects of race were found. However, the lack of such moderating effects could be due to a lack of racial diversity within the sample, a problem we remedy in the second study.
Study 2
Study 2 provided an opportunity to replicate associations between perceptions of childhood unpredictability and adult functional ability and health-related quality of life. Three features of Study 2 enhanced the investigation. First, Study 2 recruited a larger and more racially diverse sample to increase statistical power to detect potential moderating effects. Second, Study 2 included a more targeted focus on two outcome variables: the CDC’s core HRQOL module and the SF-36 Physical Functioning measure. We chose the Physical Functioning measure because it is the most comprehensive (10 items) and reliable of the SF-36 subscales (RAND, 1995) and is the most differentiable from the CDC HRQOL core module (Barile et al., 2016). Third, reports of mental and physical health, as well as retrospective reports of childhood adversity, may be influenced by personality traits such as neuroticism (Baldwin et al., 2019). Therefore, to ensure that findings do not simply reflect shared associations with personality traits, we measured and controlled for the Big 5 personality traits (John & Srivastava, 1999).
Method
Participants
A sample of 564 community participants living in the U.S. was recruited via CloudResearch. Recruitment was open to all adult participants with the constraint that we aimed to recruit a minimum of 200 Black/African American participants. Similar to Study 1, participants who failed one or more of three attention checks embedded in self-report items were not permitted to complete the study and were excluded. Participants were compensated $2. See Table 1 for sample demographic characteristics. Data were collected in March–May, 2021. The study was approved by the Florida State University IRB and informed consent was obtained from all participants prior to participation.
Measures
Study 2 used the same measures of childhood unpredictability, poverty, and ACEs from Study 1. Study 2 included two of the outcome measures from Study 1: the CDC HRQOL core module and the 10-item SF-36 Physical Functioning scale.
To measure the Big 5 personality traits, we used the Ten-Item Personality Inventory (Gosling et al., 2003). The scale provided measures of Emotional Stability/Neuroticism, Conscientiousness, Agreeableness, Openness, and Extraversion.
Statistical approach
Preliminary analyses assessed correlations among variables. Primary analyses relied on hierarchical regression to assess independent associations between outcome measures (CDC HRQOL core module, SF-36 Physical Functioning) and measures of childhood adversity (unpredictability, poverty, and ACEs). The first step of the regression model replicated analyses from Study 1: outcomes were predicted from measures of childhood adversity and demographic covariates including participant age, gender, race (Black/African American vs. non-Black), ethnicity (Hispanic/Latino vs. non-Hispanic), and current income. In the second step of the regression model, we included the Big 5 personality traits as additional covariates. Moderation analyses built on this regression model to examine whether effects of unpredictability were moderated by race, ethnicity, or current income; all three centered interaction terms were included simultaneously to ensure that any moderated effects were independent of one another. Mediational analyses assessed whether perceived unpredictability might mediate effects of ACEs. There were no missing data. To simplify statistical models, only participants self-identifying as male or female were included. Sensitivity analysis indicated that the study was well-powered (> 0.80) to detect effect sizes as small as r = 0.12 in both correlational analyses and regression analyses with 13 predictors.
Results
Correlations are in Table 2. As in Study 1, all three measures of childhood adversity were correlated with one another, and all three were significantly correlated with the two outcome measures. Primary regression analyses accounted for the correlations among predictors and replicated findings from Study 1 (See Table 4). Childhood unpredictability was significantly associated with both outcome measures, while controlling for poverty, ACEs, and demographic covariates (step 1), as well as all Big 5 personality traits (step 2).
Table 4.
Study 2 regression analyses: predictors of functional disability and health-related quality of life
| Dependent variable | Predictor | Beta | t | p | Partial r |
|---|---|---|---|---|---|
| CDC HRQOL | |||||
| Step 1 | Unpredictability | 0.25 | 4.09 | < 0.001 | 0.17 |
| Poverty | 0.02 | 0.42 | 0.68 | 0.02 | |
| ACEs | 0.10 | 1.70 | 0.09 | 0.07 | |
| Age | − 0.12 | − 3.03 | 0.003 | − 0.13 | |
| Gender | 0.05 | 1.21 | 0.23 | 0.05 | |
| Current income | − 0.09 | − 2.20 | 0.03 | − 0.09 | |
| Black | − 0.07 | − 1.79 | 0.07 | − 0.08 | |
| Hispanic | − 0.00 | − 0.09 | 0.93 | − 0.00 | |
| Step 2 | Unpredictability | 0.13 | 2.36 | 0.02 | 0.10 |
| Poverty | 0.01 | 0.20 | 0.84 | 0.01 | |
| ACEs | 0.07 | 1.30 | 0.19 | 0.06 | |
| Age | − 0.01 | − 0.14 | 0.89 | − 0.01 | |
| Gender | − 0.02 | − 0.39 | 0.70 | − 0.02 | |
| Current income | − 0.01 | − 0.19 | 0.85 | − 0.01 | |
| Black | 0.04 | 1.02 | 0.31 | 0.04 | |
| Hispanic | 0.00 | − .05 | 0.96 | − 0.00 | |
| Extraversion | − 0.08 | − 2.12 | 0.03 | − 0.09 | |
| Agreeableness | − 0.02 | − 0.40 | 0.69 | − 0.02 | |
| Conscientiousness | − 0.12 | − 2.74 | 0.01 | − 0.12 | |
| Emotional stability | − 0.40 | − 9.02 | < 001 | − 0.36 | |
| Openness | − 0.01 | − 0.30 | 0.77 | − 0.01 | |
| Physical functioning | |||||
| Step 1 | Unpredictability | − 0.34 | − 5.68 | < 0.001 | − 0.24 |
| Poverty | 0.01 | 0.25 | 0.80 | 0.01 | |
| ACEs | − 0.00 | − 0.03 | 0.97 | − 0.00 | |
| Age | − 0.26 | − 6.44 | < 0.001 | − 0.27 | |
| Gender | − 0.03 | − 0.71 | 0.48 | − 0.03 | |
| Current income | 0.04 | 1.09 | 0.28 | 0.05 | |
| Black | − 0.02 | − 0.51 | 0.61 | − 0.02 | |
| Hispanic | 0.12 | 3.06 | 0.002 | 0.13 | |
| Step 2 | Unpredictability | − 0.28 | − 4.72 | < 0.001 | − 0.20 |
| Poverty | 0.01 | 0.31 | 0.75 | 0.01 | |
| ACEs | 0.01 | 0.21 | 0.84 | 0.01 | |
| Age | − 0.31 | − 7.45 | < 0.001 | − 0.31 | |
| Gender | − 0.01 | − 0.15 | 0.88 | − 0.01 | |
| Current income | 0.01 | 0.26 | 0.80 | 0.01 | |
| Black | − 0.07 | − 1.66 | 0.10 | − 0.07 | |
| Hispanic | 0.12 | 2.97 | 0.003 | 0.13 | |
| Extraversion | 0.02 | 0.58 | 0.56 | 0.03 | |
| Agreeableness | 0.02 | 0.46 | 0.64 | 0.02 | |
| Conscientiousness | 0.06 | 1.22 | 0.22 | 0.05 | |
| Emotional stability | 0.16 | 3.30 | 0.001 | 0.14 | |
| Openness | 0.00 | 0.09 | 0.93 | 0.00 | |
N = 557. Gender: 1 = Male, 2 = Female. Race: 0 = non-Black/African American, 1 = Black/African American. Ethnicity: 0 = non-Hispanic, 1 = Hispanic. For the CDC HRQOL measure, higher scores indicate worse health-related quality of life. For Physical Functioning, higher scores reflect better functional ability
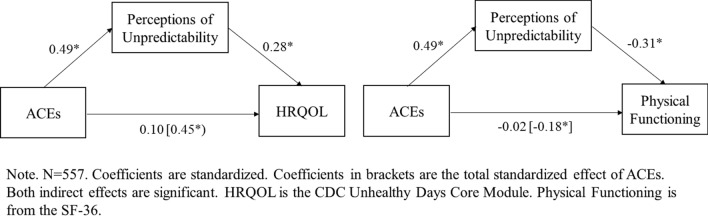
We tested whether perceived unpredictability mediated the association between ACEs and the two outcomes. Replicating Study 1, both standardized indirect effects were significant (Unhealthy Days: Z = 0.19, SE = 0.04, CI [0.11, 0.27]; Physical Functioning: Z = − 0.21, SE = 0.04, CI [− 0.30, − 0.13). See Fig. 2.
Fig. 2.
Study 2 mediating effects of perceived childhood unpredictability
Moderation analyses examined potential moderating effects of race, ethnicity, and income. We observed a significant (B = − 0.12, t = − 2.97, p = 0.003) moderating effect of race on Physical Functioning. Simple slopes analyses showed that there was a larger effect of unpredictability in Black (B = − 0.49, t = − 6.62, p < 0.001), compared with non-Black (B = − 0.32, t = − 5.38, p < 0.001) participants (see Supplemental Materials Fig. S2). The moderating effect of race on HRQOL was not significant (B = 0.06, t = 1.35, p = 0.18), but the pattern of simple effects was similar: a larger effect of unpredictability was seen in Black (B = 0.32, t = 4.24, p < 0.001), compared with non-Black (B = 0.24, t = 3.92, p < 0.001) participants (see Fig S2). No moderating effects of ethnicity were found on either measure (HRQOL: B = − 0.00, t = − 0.01, p = 1.00; Physical Functioning: B = 0.06, t = 1.47, p = 0.14). We also saw significant moderating effects of current income on both outcome measures (HRQOL: B = − 0.08, t = − 2.03, p = 0.04; Physical Functioning: B = 0.08, t = 2.04, p = 0.04). See Fig. S3. Simple slopes analyses showed that effects of unpredictability were considerably larger among those with lower incomes (1SD below the mean income: HRQOL: B = 0.33, t = 4.66, p < 0.001; Physical Functioning: B = − 0.42, t = − 6.14, p < 0.001), compared with higher incomes (1SD above the mean: HRQOL: B = 0.14, t = 1.75, p = 0.08; Physical Functioning: B = − 0.22, t = − 2.84, p = 0.005).
Discussion
Study 2 replicated evidence for robust associations between perceived childhood unpredictability and adult functional disability and health-related quality of life. Those associations were observed over and above other measures of childhood adversity, demographics, and Big 5 personality traits. As in Study 1, we saw evidence that effects of ACEs were statistically mediated by perceived unpredictability. We also observed evidence for independent moderating effects of race and income. Effects were relatively larger among Black (compared with non-Black) and lower income (compared with higher income) participants. No moderating effects of ethnicity were found, although this could be due to the relatively small number of Hispanic participants in this sample.
General discussion
Findings from two studies identify perceptions of childhood unpredictability as a key psychological factor potentially contributing to functional disability and low health-related quality of life in adulthood. The associations between perceived childhood unpredictability and health-related outcomes were observed while controlling for other measures of childhood adversity (poverty and ACEs), demographic variables (age, gender, racial/ethnic minority status, current household income), and personality (Big 5 traits). Although we replicated zero-order correlations between adult health-related outcomes and ACEs (and poverty), unpredictability emerged in regression analyses as an especially robust and independent predictor. That pattern, coupled with mediational analyses, is consistent with the possibility that perceptions of unpredictability partially explain associations between ACEs and poor adult health. (It is important to note, however, that tests of mediation are limited by the cross-sectional design of these studies and thus strong causal interpretations are not warranted.) Childhood experiences such as physical or emotional abuse or inconsistent caregiving can create a sense of instability and lack of control and certainty, as well as a psychological focus on short term (rather than long-term) rewards and goals. Over time, such processes may culminate in greater risk for poor health in adulthood. This work thus advances the literature by identifying perceptions of unpredictability as a potentially important factor underlying functional disability and poor health-related quality of life in adulthood.
The effects of childhood unpredictability on adult health may reflect psychological, behavioral, and neuroendocrine pathways. Psychological pathways reflect the fact that unpredictability entails a lack of stability, certainty, and control (Mittal & Griskevicius, 2014), and thus requires high levels of cognitive vigilance (Frankenhuis et al., 2016; Pepper & Nettle, 2017). Such vigilance is stressful and consumes valuable bioenergetic resources that could otherwise be devoted to creating supportive social relationships (Maranges et al., 2021) or to caring for one’s long-term health (Ellis et al., 2009; see also Schreier & Chen, 2010). Behavioral pathways reflect the fact that unpredictable childhood environments can promote a tendency to behave in impulsive and risky ways (Del Giudice, 2009; Martinez et al., 2022). Children who experience high levels of unpredictability learn to focus on short-term rather than long-term rewards (Frankenhuis & Nettle, 2020; Frankenhuis et al., 2016) and this focus can cause people who were exposed to unpredictable childhood environments to make impulsive decisions (Ellis et al., 2012; Hartman et al., 2018; Martinez et al., 2022), and to engage in health risk behaviors such as substance use (Doom et al., 2016; Simpson et al., 2012), risky sexual behavior (Ellis et al., 2012), and unhealthy dietary choices (Maner et al., 2017). Neuroendocrine pathways include influences on corticolimbic circuitry (Gee & Cohodes, 2021; Liu & Fisher, 2022) and the hypothalamic-pituitary adrenal axis (Zakreski & Pruessner, 2019), chronic alterations of which are associated with chronic disease risk, anxiety, and mortality (Schoorlemmer et al., 2009). Future work would benefit from assessing more directly the pathways through which childhood unpredictability may affect adult health outcomes.
Evidence for moderating effects was inconsistent across the two studies. Effects of unpredictability were heightened among Hispanic participants in Study 1, and among African American participants and those with relatively low income in Study 2. The presence of such moderating effects is consistent with the possibility that effects of perceived unpredictability may exacerbate the development of health problems among populations already at relatively high risk for experiencing stress associated with resource scarcity or discrimination. Compared with Study 1, which included 20% Hispanic participants, Study 2 included a higher proportion of African American participants (33% of the sample), but fewer Hispanic participants (8%). These differences in the demographic make-up of the samples may explain the inconsistent moderating effects of race and ethnicity. The two studies had similar variability in income levels, leaving open the question of whether effects are moderated by income.
Limitations of the current work provide valuable avenues for future research. One limitation involves the retrospective nature of the childhood adversity measures (see Baldwin et al., 2019). Future research would benefit from recruiting other data sources (e.g., parent report) to assess the unpredictability of childhood environments, to amass developmental data with children to assess prospectively whether childhood unpredictability underlies adult health outcomes, and to leverage existing longitudinal studies to capitalize on the prospective nature of those designs (Ehrlich, 2020). In addition, while we focused on self-reported functional ability and health-related quality of life, future studies should evaluate whether childhood unpredictability is associated with clinical indicators of disability and chronic disease risk and diagnosis. Finally, it is important to note that both studies were conducted during the COVID-19 pandemic, a time during which social isolation, anxiety, and depression were high among many individuals and this, coupled with decreases in routine medical visits, could have increased health problems, as well as perceptions of health problems.
Although the current work points to the importance of experiencing unpredictability in childhood, it fails to identify the specific age range in which unpredictability might exert its effects. Although some evidence suggests that such effects are especially strong in the first five to ten years of childhood (Mittal & Griskevicius, 2014; Simpson et al., 2012), ongoing debates center on the precise timing of this developmental calibration process. Future work would benefit from including repeated measurements and longitudinal designs to characterize more precisely the developmental trajectory arising from exposure to unpredictable childhood environments.
Despite these limitations, this work advances theories of child adversity and health. This work also provides valuable information for the development of child interventions targeting malleable environmental risk factors that influence health. Interventions that increase the predictability and certainty of childhood environments (e.g., by increasing the consistency of a child’s daily routines) may hold potential for improving health (Miller et al., 2014; Schreier & Chen, 2010). Such interventions are also feasible: creating a sense of certainty and stability by increasing the predictability of a child’s environment may provide a relatively cost-effective and implementable means of improving public health and well-being. The current work provides a useful springboard for examining the utility of such interventions and further investigating the role of childhood unpredictability in health across the lifespan.
Supplementary Information
Below is the link to the electronic supplementary material.
Authors contribution
All authors contributed substantially either to the design, conceptualization, execution, analysis, or write-up of this research.
Funding
Not applicable.
Data availability
All data and materials will be made available on OSF upon publication.
Code availability
All statistical code will be made available on OSF upon publication.
Declarations
Conflict of interest
The authors did not receive support from any organization for the submitted work and no funding was received to assist with the preparation of this manuscript. The authors have no competing interests to declare that are relevant to the content of this article.
Consent to participate
All participants provided consent prior to participation.
Consent for publication
Not applicable.
Ethical approval
This research was approved by the FSU IRB.
Human and animal rights and informed consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health: No easy solution. JAMA. 1993;269:3140–3145. doi: 10.1001/jama.1993.03500240084031. [DOI] [PubMed] [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, Danese A. Agreement between prospective and retrospective measures of childhood maltreatment: A systematic review and meta-analysis. JAMA Psychiatry. 2019;76:584–593. doi: 10.1001/jamapsychiatry.2019.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baram TZ, Davis EP, Obenaus A, Sandman CA, Small SL, Solodkin A, Stern H. Fragmentation and unpredictability of early-life experience in mental disorders. American Journal of Psychiatry. 2012;169(9):907–915. doi: 10.1176/appi.ajp.2012.11091347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barile JP, Horner-Johnson W, Krahn G, Zack M, Miranda D, et al. Measurement characteristics for two health-related quality of life measures in older adults: The SF-36 and the CDC Healthy Days items. Disability & Health Journal. 2016;9:567–574. doi: 10.1016/j.dhjo.2016.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Schlomer GL, Ellis BJ. Beyond cumulative risk: Distinguishing harshness and unpredictability as determinants of parenting and early life history strategy. Developmental Psychology. 2012;48:662–673. doi: 10.1037/a0024454. [DOI] [PubMed] [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: An evolutionary-developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;17:271–301. doi: 10.1017/S0954579405050145. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Brumbach BH, Figueredo AJ, Ellis BJ. Effects of harsh and unpredictable environments in adolescence on development of life history strategies: A longitudinal test of an evolutionary model. Human Nature. 2009;20:25–51. doi: 10.1007/s12110-009-9059-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabeza De Baca TC, Wahl RA, Barnett MA, Figueredo AJ, Ellis BJ. Adversity, adaptive calibration, and health: The case of disadvantaged families. Adaptive Human Behavior and Physiology. 2016;2:93–115. doi: 10.1007/s40750-016-0042-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (1993). Health related quality of life scale. (https://www.cdc.gov/hrqol/methods.htm).
- Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children’s health: How and why do these relationships change with age? Psych Bulletin. 2002;128:295–329. doi: 10.1037/0033-2909.128.2.295. [DOI] [PubMed] [Google Scholar]
- Chen E, Miller GE. Socioeconomic status and health: Mediating and moderating factors. Annual Review of Clinical Psychology. 2013;9:723–749. doi: 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- Del Giudice M. Sex, attachment, and the development of reproductive strategies. Behavioral and Brain Sciences. 2009;32:1–21. doi: 10.1017/S0140525X09000016. [DOI] [PubMed] [Google Scholar]
- Del Giudice M, Ellis BJ, Shirtcliff EA. The adaptive calibration model of stress responsivity. Neuroscience & Biobehavioral Reviews. 2011;35:1562–1592. doi: 10.1016/j.neubiorev.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doom JR, Vanzomeren-Dohm AA, Simpson JA. Early unpredictability predicts increased adolescent externalizing behaviors and substance use: A life history perspective. Development and Psychopathology. 2016;28:1505–1516. doi: 10.1017/S0954579415001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Croft JB, Edwards VJ, Giles WH. Growing up with parental alcohol abuse: Exposure to childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2001;25:1627–1640. doi: 10.1016/S0145-2134(01)00293-9. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Preventive Medicine. 2003;37:268–277. doi: 10.1016/S0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- Ehrlich KB. How does the social world shape health across the lifespan? Insights and new directions. American Psychologist. 2020;75:1231–1241. doi: 10.1037/amp0000757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlich KB, Miller GE, Chen E. Childhood adversity and adult physical health. Developmental Psychopathology. 2016;22:1–42. [Google Scholar]
- Elliott TE, Renier CM, Palcher JA. Chronic pain, depression, and quality of life: Correlations and predictive value of the SF-36. Pain Medicine. 2003;4:331–339. doi: 10.1111/j.1526-4637.2003.03040.x. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Del Giudice M. Developmental adaptation to stress: An evolutionary perspective. Annual Review of Psychology. 2019;70:111–139. doi: 10.1146/annurev-psych-122216-011732. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Del Giudice M, Dishion TJ, Figueredo AJ, Gray P, Griskevicius V, Hawley PH, et al. The evolutionary basis of risky adolescent behavior: Implications for science, policy, and practice. Developmental Psychology. 2012;48:598–627. doi: 10.1037/a0026220. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Figueredo AJ, Brumach BH, Schlomer GL. Fundamental dimensions of environmental risk: The impact of harsh versus unpredictable environments on the evolution and development of life history strategies. Human Nature. 2009;20:204–268. doi: 10.1007/s12110-009-9063-7. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14:245–328. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Frankenhuis WE, Nettle D. The strengths of people in poverty. Current Directions in Psychological Science. 2020;29:16–21. doi: 10.1177/0963721419881154. [DOI] [Google Scholar]
- Frankenhuis WE, Panchanathan K, Nettle D. Cognition in harsh and unpredictable environments. Current Opinion in Psychology. 2016;7:76–80. doi: 10.1016/j.copsyc.2015.08.011. [DOI] [Google Scholar]
- Gee DG, Cohodes EM. Influences of caregiving on development: A sensitive period for biological embedding of predictability and safety cues. Current Directions in Psychological Science. 2021;30(5):376–383. doi: 10.1177/09637214211015673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling SD, Rentfrow PJ, Swann WB., Jr A very brief measure of the big five personality domains. Journal of Research in Personality. 2003;37:504–528. doi: 10.1016/S0092-6566(03)00046-1. [DOI] [Google Scholar]
- Hartman S, Sung S, Simpson JA, Schlomer GL, Belsky J. Decomposing environmental unpredictability in forecasting adolescent and young adult development: A two-sample study. Developmental and Psychopathology. 2018;30:1321–1332. doi: 10.1017/S0954579417001729. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications; 2017. [Google Scholar]
- John OP, Srivastava S. The big-five trait taxonomy: History, measurement, and theoretical perspectives. In: Pervin LA, John OP, editors. Handbook of personality: Theory and research. Guilford Press; 1999. pp. 102–138. [Google Scholar]
- Kelly JB, Emery RE. Children's adjustment following divorce: Risk and resilience perspectives. Family Relations. 2003;52:352–362. doi: 10.1111/j.1741-3729.2003.00352.x. [DOI] [Google Scholar]
- Liu S, Fisher PA. Early experience unpredictability in child development as a model for understanding the impact of the COVID-19 pandemic: A translational neuroscience perspective. Developmental Cognitive Neuroscience. 2022;54:101091. doi: 10.1016/j.dcn.2022.101091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maner JK, Dittmann A, Meltzer AL, McNulty JK. Implications of life history strategies for obesity. Proceedings of the National Academy of Sciences. 2017;114:8517–8522. doi: 10.1073/pnas.1620482114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maranges H, Hasty C, Maner JK, Conway P. The behavioral ecology of moral dilemmas: Childhood unpredictability, but not harshness, predicts less deontological and utilitarian responding. Journal of Personality and Social Psychology. 2021;120:1696–1719. doi: 10.1037/pspp0000368. [DOI] [PubMed] [Google Scholar]
- Maranges HM, Hasty CR, Martinez JL, Maner JK. Adaptive calibration in early development. Brief measures of perceived harshness and unpredictability. Adaptive Human Behavior and Physiology. 2022;8(3):313–343. doi: 10.1007/s40750-022-00200-z. [DOI] [Google Scholar]
- Martinez JL, Hasty C, Morabito D, Maranges HM, Schmidt NB, Maner JK. Perceptions of childhood unpredictability, delay discounting, risk-taking, and adult externalizing behaviors: A life history approach. Development & Psychopathology. 2022;34:705–717. doi: 10.1017/S0954579421001607. [DOI] [PubMed] [Google Scholar]
- McDade TW. Life history theory and the immune system: Steps toward a human ecological immunity. American Journal of Physical Anthropology. 2003;122:100–125. doi: 10.1002/ajpa.10398. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Stellar E. Stress and the individual: Mechanisms leading to disease. Archives of Internal Medicine. 1993;153:2093–2101. doi: 10.1001/archinte.1993.00410180039004. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA. Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science. 2016;25:239–245. doi: 10.1177/0963721416655883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielenz T, Jackson E, Currey S, DeVellis R, Callahan LF. Psychometric properties of the Centers for Disease Control and Prevention health-related quality of life (CDC HRQOL) items in adults with arthritis. Health and Quality of Life Outcomes. 2006;4:66. doi: 10.1186/1477-7525-4-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Brody GH, Yu T, Chen E. A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proceedings of the National Academy of Sciences. 2014;111:11287–11292. doi: 10.1073/pnas.1406578111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic disease of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal C, Griskevicius V. Sense of control under uncertainty depends on people’s childhood environment: A life history theory approach. Journal of Personality and Social Psychology. 2014;107:621–637. doi: 10.1037/a0037398. [DOI] [PubMed] [Google Scholar]
- Parshall MB, Mapel DW, Rice L, Williams A, O’Reilly J. Predictive validity of short-form health survey [36 items] scales for chronic obstructive pulmonary disease exacerbation. Heart & Lung. 2008;37:356–365. doi: 10.1016/j.hrtlng.2007.09.007. [DOI] [PubMed] [Google Scholar]
- Pepper GV, Nettle D. The behavioural constellation of deprivation: Causes and consequences. Behavioral & Brain Sciences. 2017;40:e314. doi: 10.1017/S0140525X1600234X. [DOI] [PubMed] [Google Scholar]
- RAND Health Care. (1995). 36-item short form survey instrument (SF-36). https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/survey-instrument.html.
- Schoorlemmer R, Peeters G, van Schoor N, Lips P. Relationships between cortisol level, mortality, and chronic disease in older persons. Clinical Endocrinology. 2009;71:779–786. doi: 10.1111/j.1365-2265.2009.03552.x. [DOI] [PubMed] [Google Scholar]
- Schreier HM, Chen E. Longitudinal relationships between family routines and biological profiles among youth with asthma. Health Psychology. 2010;29:82–90. doi: 10.1037/a0018311. [DOI] [PubMed] [Google Scholar]
- Simpson JA, Griskevicius V, Kuo SI, Sung S, Collins WA. Evolution, stress, and sensitive periods: The influence of unpredictability in early versus late childhood on sex and risky behavior. Developmental Psychology. 2012;48:674–686. doi: 10.1037/a0027293. [DOI] [PubMed] [Google Scholar]
- Zakreski E, Pruessner JC. Effects of childhood trauma on the cortisol and testosterone stress response are mediated by life history strategy. Psychoneuroendocrinology. 2019;100:S21–S22. doi: 10.1016/j.psyneuen.2018.12.084. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data and materials will be made available on OSF upon publication.
All statistical code will be made available on OSF upon publication.