Abstract
Introduction
Socioeconomic disparities for breast cancer surgical care exist. Although the aetiology of the observed socioeconomic disparities is likely multifactorial, patient engagement during the surgical consult is critical. Shared decision-making may reduce health disparities by addressing barriers to patient engagement in decision-making that disproportionately impact socioeconomically disadvantaged patients. In this trial, we test the impact of a decision aid on increasing socioeconomically disadvantaged patients’ engagement in breast cancer surgery decision-making.
Methods and analysis
This multisite randomised trial is conducted through 10 surgical clinics within the National Cancer Institute Community Oncology Research Program (NCORP). We plan a stepped-wedge design with clinics randomised to the time of transition from usual care to the decision aid arm. Study participants are female patients, aged ≥18 years, with newly diagnosed stage 0–III breast cancer who are planning breast surgery. Data collection includes a baseline surgeon survey, baseline patient survey, audio-recording of the surgeon–patient consultation, a follow-up patient survey and medical record data review. Interviews and focus groups are conducted with a subset of patients, surgeons and clinic stakeholders. The effectiveness of the decision aid at increasing patient engagement (primary outcome) is evaluated using generalised linear mixed-effects models. The extent to which the effect of the decision aid intervention on patient engagement is mediated through the mitigation of barriers is tested in joint linear structural equation models. Qualitative interviews explore how barriers impact engagement, especially for socioeconomically disadvantaged women.
Ethics and dissemination
This protocol has been approved by the National Cancer Institute Central Institutional Review Board, and Certificate of Confidentiality has been obtained. We plan to disseminate the findings through journal publications and national meetings, including the NCORP network. Our findings will advance the science of medical decision-making with the potential to reduce socioeconomic health disparities.
Trial registration number
ClinicalTrials.gov Registry (NCT03766009).
Keywords: Breast surgery, Breast tumours, Protocols & guidelines
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The strategy for decision aid implementation used in this trial was developed with input from clinic and patient stakeholders.
Trial uses a national cancer research network to engage diverse clinical practices across the country.
The stepped-wedge study design allows all practices to experience the decision aid, allowing insight into implementation.
The COVID-19 pandemic negatively impacted accrual.
As the decision aid was only available in English, non-English speakers were excluded from the study.
Introduction
Socioeconomic disparities for breast cancer surgical care exist. Multiple clinical trials and registry studies demonstrate at least equivalent survival between breast-conserving therapy (BCT) and mastectomy (with or without reconstruction) for women diagnosed with early-stage breast cancer.1–6 However, patient-centred outcomes differ greatly, with some women experiencing a higher risk of local recurrence after BCT2 3 7–9 and a greater impact on body image with mastectomy.10–12 As many women are candidates for both procedures, patients’ preferences should drive decision-making.13–19 Despite this, population-based studies demonstrate that socioeconomically disadvantaged women—those being challenged by low income, limited education, and substandard living conditions for both herself and her neighbourhood20—are less likely to undergo BCT or receive post-mastectomy reconstruction.21–25 These disparities may lead to negative long-term outcomes such as treatment regret, poorer body image and reduced quality of life.26–31
Increased patient engagement in decision-making may mitigate existing socioeconomic disparities in breast cancer surgical care. Prior studies have demonstrated that socioeconomically disadvantaged women have less understanding of treatment options,32–34 are less likely to recall discussing a choice with their surgeon35 36 and participate less actively in decision-making.37 Although the aetiology of the observed socioeconomic disparities is likely multifactorial, patient engagement during the surgical consult is a critical component for this preference-sensitive choice.13–19
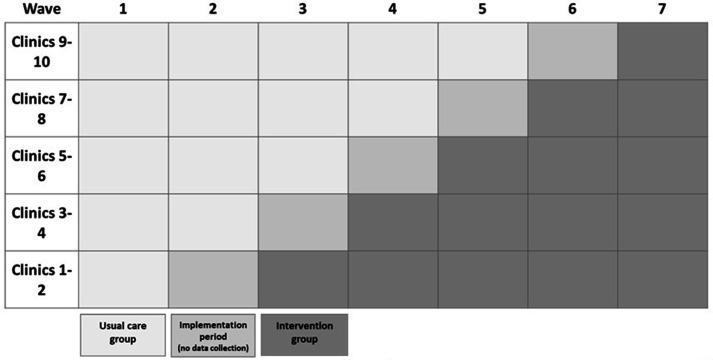
Shared decision-making (SDM) may reduce health disparities by addressing barriers to patient engagement in decision-making that disproportionately impact socioeconomically disadvantaged patients.38 39 SDM interventions (eg, decision aids) have the potential to increase patient involvement in decision-making, improve health outcomes and lower costs.40 To engage in SDM, patients must have both the power to influence decision-making and knowledge about the options. Decision aids increase patients’ knowledge about treatment options.39 41–43 Decision aids may also increase patients’ power in decision-making by preparing patients for the surgical consult by establishing expectations of their role during the consult, specifically that their input (ie, their values and preferences) is welcome and essential. By preparing patients for surgical consultation, decision aids may increase patients’ confidence in their ability to interact with their surgeon, empowering them to engage in SDM during the surgical consult (figure 1).38 However, barriers to patient engagement may exist even after receipt of a decision aid, including lack of awareness about treatment choices, patients’ perceptions that their personal input is not valued and doctor–patient power imbalances. These persistent barriers to engagement may be disproportionately experienced by socioeconomically disadvantaged patients.38 Combining routine delivery of a decision aid with the delivery of adjunct interventions targeting persistent barriers to engagement may therefore reduce disparities in care.
Figure 1.
Our conceptual model is based on the theory that in order to engage in SDM, patients must have both the power to influence decision-making and knowledge about the options. Pre-consultation review of a decision can address these key conditions by preparing patients for the surgical consultation and increasing their confidence in interacting with the surgeon. However, barriers to engagement may limit the effect of the decision aid. These barriers disproportionately impact socioeconomically disadvantaged patients. SDM, shared decision-making.
In this clinical trial, we test the impact of a decision aid on increasing socioeconomically disadvantaged patients’ engagement in breast cancer surgery decision-making. The aims of our study are as follows:
Aim 1: test the effectiveness of a breast cancer surgery decision aid in increasing patient engagement in decision-making in clinics serving a high proportion of socioeconomically disadvantaged patients.
Aim 2: test the extent to which the effect of a decision aid on patient engagement is mediated through the mitigation of barriers, and determine if persistent barriers are disproportionately experienced by socioeconomically disadvantaged patients.
Aim 3: characterise how persistent barriers influence patient engagement in decision-making in order to identify targets for adjunct interventions that could be implemented in clinics serving a high proportion of socioeconomically disadvantaged patients.
Methods and analysis
Setting
Ten surgical clinics within the National Cancer Institute Community Oncology Research Program (NCORP) agreed to participate in our study (table 1). NCORP is a community cancer research network created with the goal of improving cancer care outcomes, expanding access to cancer care and reducing cancer disparities.44 The Alliance for Clinical Trials in Oncology, a National Cancer Institute Clinical Trials Network group, serves as the research base for this trial and is responsible for protocol development, statistical and data management, and overall study operations.45 NCORP sites were selected that (1) annually provide surgical care for 120–300 patients with newly diagnosed breast cancer, and (2) serve a high proportion of socioeconomically disadvantaged patients. Sites were stratified into two groups, with the primary factor considered in the stratification being whether (group 2) or not (group 1) the site was a minority/underserved NCORP.
Table 1.
Participating NCORP sites and stratification grouping
| Clinic | City, state | NCORP |
| Group 1 | ||
| Marshfield Clinic | Marshfield, Wisconsin | Wisconsin NCORP |
| Carle Cancer Center | Urbana, Illinois | Carle Cancer Center NCORP |
| Bay Area Breast Surgeons | Emeryville, California | Bay Area Tumor Institute NCORP |
| Billings Clinic Cancer Center | Billings, Montana | Montana Cancer Consortium NCORP |
| Kapiolani Medical Center for Women and Children | Honolulu, Hawaii | Hawaii Minority Underserved NCORP |
| Group 2 | ||
| John H Stroger Hospital of Cook County | Chicago, Illinois | Stroger Hospital of Cook County Minority Underserved NCORP |
| Augusta University Medical Center | Augusta, Georgia | Georgia Cares Minority Underserved NCORP |
| New Mexico Cancer Center Alliance | Albuquerque, New Mexico | New Mexico Minority Underserved NCORP |
| Medical University of South Carolina | Charleston, South Carolina | Medical University of South Carolina Minority Underserved NCORP |
| Virginia Commonwealth University (VCU)/Massey Cancer Center | Richmond, Virginia | VCU Massey Cancer Center Minority Underserved NCORP |
NCORP, National Cancer Institute Community Oncology Research Program.
Patient and public involvement
The strategy for decision aid implementation used in this trial was developed with input from clinic and patient stakeholders at the University of Wisconsin Health (Madison, Wisconsin) and Baptist Medical Center (Nashville, Tennessee).46 47 Additional study design input was elicited from the Alliance for Clinical Trials in Oncology Patient Advocate and Community Oncology Committees to ensure the developed protocol would be feasible in diverse clinical settings and would meet the needs of the target population.45
Study design
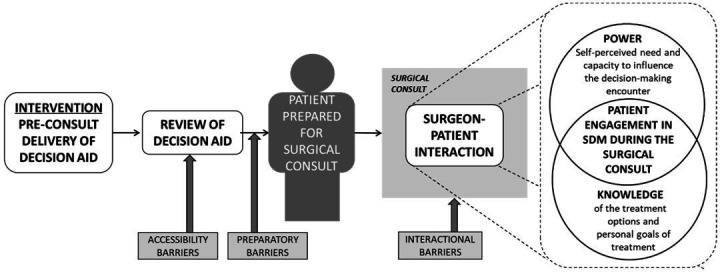
This study is a multisite cluster randomised trial using a stepped-wedge design with seven waves (figure 2). The stepped-wedge design was selected as it was not feasible to implement the decision aid simultaneously at all clinics. Further, this design ensured all clinics have the opportunity to experience the intervention.48 All clinics began in the usual care arm. The 10 clinics were randomised to the timing of crossover to the decision aid intervention, stratified by group so that each step included a clinic from each group. Every 10 weeks (length of one wave) and following a 10-week implementation period, two clinics crossed over into the intervention arm. To avoid anticipatory effects, clinics were blinded to crossover wave until the latest possible time. If the current accrual for a given site was <2/3 of the stated accrual goal for that site at the end of a wave, then the wave was extended one time by 3 weeks for that site (maximum wave length is 13 weeks). The effectiveness of the decision aid in increasing patient engagement in decision-making is assessed by comparing patients in the usual care arm with patients in the intervention arm.
Figure 2.
Stepped-wedge study design. The effect of the decision aid on patient engagement will be evaluated as a pre/post-comparison of usual care versus the decision aid intervention arms through the stepped-wedge design. The process of implementation of the decision aid will occur over a 10-week period during which the clinic does not collect patient-level data.
Intervention (decision aid)
The web-based decision aid was developed collaboratively by the Informed Medical Decisions Foundation49 and Health Dialog.50 We use the strategy developed in our pilot work to guide implementation.46 47 After crossover to the intervention arm, all new patients with breast cancer being cared for within a participating clinic are offered the web-based decision aid prior to the surgical consultation as a component of usual care in the clinic (regardless of whether they ultimately participate in the research study).
Participants
Patients who receive care at participating clinics were eligible if they were female, 18 years of age or older, newly diagnosed with stage 0–III breast cancer and planning breast surgery as a component of treatment. Patients were not eligible for the study if they have impaired decision-making capacity, have a hearing impairment or were a non-English speaker requiring the use of an interpreter. All surgeons at participating sites who perform breast surgery were eligible to participate in study activities. Clinic staff at participating clinics were also eligible.
Recruitment, consent and registration
Patients: each week, the research teams at each site pre-screen clinic schedules of enrolled surgeons to identify eligible patients. A research team member obtains written informed consent from interested eligible patients, and registers them into the Oncology Patient Enrollment Network system.
Clinic stakeholders: prior to initiation of patient accrual, all breast surgeons at a participating site received an email providing study information and an opportunity to opt out. Surgeons provided written informed consent for completion of the baseline survey and audio-recording of surgical consults. Surgeons were registered. Participating surgeons may also be recruited later for a focus group. Clinic staff at participating clinics may be recruited later for participation in a focus group.
Data collection
The overall schema for data collection for patients and clinic stakeholders is presented in figure 3. In the stepped-wedge design, patient quantitative data collection (baseline in-person patient survey, audio-recording of the consult, Qualtrics follow-up survey and chart review) within each clinic before and after implementation of the decision aid intervention is the same. A subset of patients in the decision aid intervention arm are eligible to participate in interviews, based on their survey responses. We interview a subset of patients who experience accessibility barriers, defined as patients who declined the decision aid, had difficulty accessing it or did not use it (~30 patients). We also interview a subset of patients who used the decision aid and experienced preparatory/interactional barriers and low engagement (lowest tertile) in decision-making (~50 patients). Finally, we conduct three patient focus groups at three separate clinics. We selected clinics with a relatively high prevalence of patients experiencing persistent barriers to engagement. All interviews and focus groups are audio-recorded and transcribed verbatim. We provide patients $10 for participation in the audio recording and baseline survey and $10 for completion of the post-consultation follow-up survey. We provide patients an additional incentive of $20 for interview and $20 for focus group participation.
Figure 3.
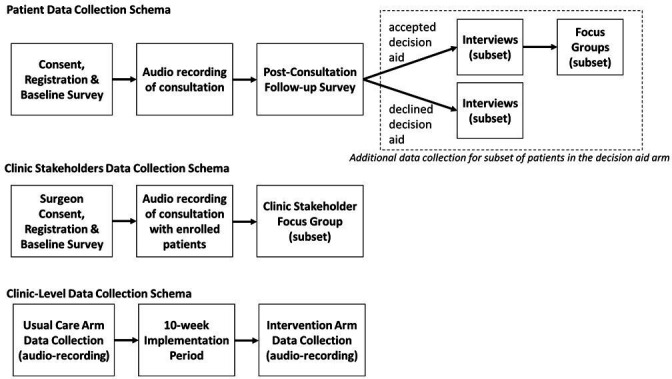
Overview of data collection scheme at patient, clinic stakeholder and clinic levels.
Surgeons completed a baseline survey at time of enrolment. We also plan to conduct two virtual focus groups with clinic stakeholders from our participating clinics, including both surgeons and nurses ($100 incentive). Focus groups are fully audio-recorded and transcribed.
Outcome variables: aims 1 and 2
Our study conceptualises engagement (figure 1) as being comprised of power (primary outcome) and knowledge (secondary outcome). We define power as ‘patients’ self-perceived need and capacity to influence the decision-making encounter’.38 We measure this in two ways, with the Patient’s Self-Efficacy in Patient-Physician Interactions (PEPPI-5)51 52 and active patient participation behaviours (table 2).53–55 PEPPI-5 is a survey-based measure assessed on the follow-up survey with a total score ranging from 5 to 25, where higher scores indicate increased self-efficacy. The active patient participation behaviour is assessed directly from the patient–surgeon consultation. It is a summary measure of patients’ active involvement in the interaction and represents a count of patients’ communicative behaviours, ranging from 0 to 100, where higher scores indicate increase active patient participation. The two measures provide complimentary but unique insight into the impact of the decision aid on engagement. Patients contribute data to the primary outcome analysis if they have audio-recorded consult or follow-up survey data. Secondary outcome includes knowledge.56
Table 2.
Outcomes and predictor variables
| Construct | Variable type | Specific measure | Source |
| Power | Primary outcome | Patient’s Self-Efficacy in Patient-Physician Interactions51 52 | Patient follow-up survey |
| Power | Primary outcome | Active patient participation behaviours53–55 | Audio-recording |
| Knowledge | Secondary outcome | Decision Quality Instrument-Breast Surgery56 | Patient follow-up survey |
| Intervention group | Predictor variable | Decision aid (yes/no) | Site randomisation |
| Socioeconomic disadvantage | Predictor variable | Area Deprivation Index57–60 | Medical record review |
Predictor variables: aims 1 and 2
The primary predictor variable for aims 1 and 2 is intervention group assignment (decision aid yes/no). Socioeconomic disadvantage is an additional predictor variable for aim 2. We define socioeconomic disadvantage to be those patients living in the 20% most disadvantaged neighbourhoods according to the Area Deprivation Index.57–60 We chose this measure of socioeconomic disadvantage based on the zipcode +4 as it allows early identification of disadvantaged patients by clinic staff without requiring a detailed patient assessment. This would allow early integration of any adjunct interventions targeting socioeconomically disadvantaged patients into clinical workflow. We collect measures related to barriers to engagement and patient, surgeon and clinic characteristics (table 3).
Table 3.
Measures related to barriers to engagement and participant characteristics
| Construct | Specific measure | Source |
| Accessibility barriers | ||
| Reach | Proportion of patients sent the decision aid/total number of eligible patients seen in clinic | Clinic logs and clinic characteristics |
| Acceptability of decision aid | Questions on email delivery, how the decision aid was used and the decision aid content | Patient baseline survey |
| Health literacy | Brief Health Literacy Screen75 | Patient baseline survey |
| Preparatory barriers | ||
| Patients’ expected role in the consult | Control Preferences Scale76 | Patient baseline survey |
| Preparation for shared decision-making (SDM) | Preparation for Decision Making Scale77 | Patient follow-up survey |
| Perceived level of knowledge | ‘How informed do you feel?’ | Baseline survey |
| Uncertainty in choosing options | SURE Decisional Conflict Scale78 | Patient follow-up survey |
| Interactional barriers | ||
| Surgeon facilitative behaviours | Coding system54 | Audio-recording |
| Patient self-autonomy | Health Care Climate Questionnaire79 | Patient follow-up survey |
| Family member presence during consult | Coding system54 | Audio-recording |
| Surgeon recommendation | Early timing within consult | Audio-recording |
| Provider attitude towards SDM | Practitioner Orientation Scale77 | Surgeon baseline survey |
| Patient, surgeon and clinic characteristics | ||
| Patient characteristics | Demographic (age, race, zipcode +4, payer), clinical (stage, receptor status) and treatment factors (surgery, radiation, systemic therapy) | Medical record review |
| Surgeon characteristics | Gender, race, ethnicity, fellowship training, % of practice comprised of breast, years in practice | Surgeon baseline survey |
| Clinic characteristics | Number of staff, presence of a navigator and annual breast cancer volume | Review of clinic resources |
Aim 3 data
In qualitative interviews with a subset of patients who experienced accessibility or preparatory/interactional barriers, we ask questions designed to increase our understanding of the patient’s experience with the decision aid and the process of decision-making. The accessibility barrier interviews elicit from patients their perspectives on how the decision aid was presented, reasons for not reviewing it and perceived value of the decision aid in supporting decision-making. The preparatory/interactional barrier interviews begin by exploring what patients had done to prepare for the consult and what they were expecting. The interviewer asks about the interactions with the surgeon, including how confident the patient felt talking with her surgeon and whether she felt the surgeon understood what was important to her. In both interviews, the interview probes on specific barriers to engagement patients reported in the survey.
We begin each focus group with a review of the persistent barriers to engagement identified through the quantitative and interview components of the study. We elicit participants’ perceptions of how these barriers impede engagement. We then present participants with potential adjunct interventions to target these barriers, identified through the existing literature. At the completion of the focus group, we use nominal group technique to identify three interventions perceived to have the greatest potential.61 62
Statistical considerations
Analysis plan for aims 1 and 2
Aim 1 analysis plan
The goal is to evaluate the effectiveness of a decision aid in increasing patient engagement in decision-making in clinics serving a high proportion of socioeconomically disadvantaged patients. We follow an intention-to-treat approach in that all patients recruited after a clinic transition to the decision aid arm are considered to be in the intervention arm, regardless of whether they were offered or accepted the decision aid. The data have a nested structure: patients nested within surgeons and surgeons nested within clinics, this last level being the formal level of intervention. Descriptive analyses will summarise patient, surgeon and clinic characteristics. We test intervention effects in the framework of generalised linear mixed-effects models (linear mixed-effects models for the approximately continuous and symmetrically distributed outcomes and logistic random-effects models for binary outcomes) with an ‘intervention versus usual care’ dummy variable (which varies over patients within clinic and surgeon), a surgeon random effect and a clinic random effect. Analysis models will include two additional parameters, for wave and wave-squared, respectively, to flexibly control for potential secular time effects and to allow for a non-linear relationship with outcome measures. We will also include a post-COVID-19 restart dichotomous variable that reflects whether a patient is enrolled during the post-COVID-19 restart time period for a given site (yes/no), as well as time (in units of wave) post-COVID-19 in all models. Before testing any treatment effects, we will develop ancillary features of the analysis model. First, in the event that the approximately continuous outcomes PEPPI-5 self-efficacy and active patient participation behaviours are not approximately symmetrically distributed, variable transformation will be considered (eg, square-root transformation). Further, we will fully test the variance–covariance structure of the model while blinded to any treatment effects. Models will be estimated and tested using SAS V.9.3 (PROC MIXED and PROC NLMIXED).63
Aim 2 analysis plan
The goals are to: (1) test the extent to which the effect of a decision aid on patient engagement is mediated through the mitigation of preparatory and interactional barriers, and (2) determine if persistent barriers are disproportionately experienced by socioeconomically disadvantaged patients. Because a decision aid can only be effective if patients are able to access/review it, we first assess accessibility barriers and then examine the impact of preparatory/interactional barriers.
Accessibility barriers: this is a largely descriptive analysis that guides sampling and interview content for aim 3. Reasons why patients declined the decision aid will be summarised. We will summarise other survey responses regarding decision aid accessibility and will perform exploratory analyses evaluating the association with socioeconomic disadvantage. Statistical tools will include standard Χ2 tests and ORs for categorical variables and analysis of variance mean differences for continuous variables, respectively.
Preparatory and interactional barriers: we will first perform analyses to test and quantify the extent to which the effect of the decision aid intervention on patient engagement endpoints is mediated through the mitigation of candidate preparatory and interactional barriers. We will quantify the indirect effect relative to the total effect of the decision aid in joint linear structural equation models (SEMs) for the endpoint and the candidate mediators, including random clinic and surgeon effects for each of the mediator and endpoint parts of the models. Each of the preparatory and interactional barriers will be represented by a continuous latent construct in the SEM. SEMs will be specified, estimated and tested using Mplus V.7.3.64 Standardised coefficient estimates from the SEM, representing total, direct and indirect effects, allow for the determination of whether the mechanism by which the decision aid leads to increased patient engagement is through the mitigation of preparatory and/or interactional barriers (see figure 4 for a simplified example). The coefficients X and Y will be tested together using the product null hypothesis XY=0. If either latent construct for preparatory or interactional barriers is significant, then each individual observed item will be tested, post hoc, as candidate barriers. Candidate barriers will be barriers for which the indirect effect is significant and/or barriers associated with lower levels of engagement (ie, coefficient Y). Barriers for either primary outcome (PEPPI-5 or active patient behaviours) will be prioritised for inclusion in the qualitative interviews (aim 3).
Figure 4.
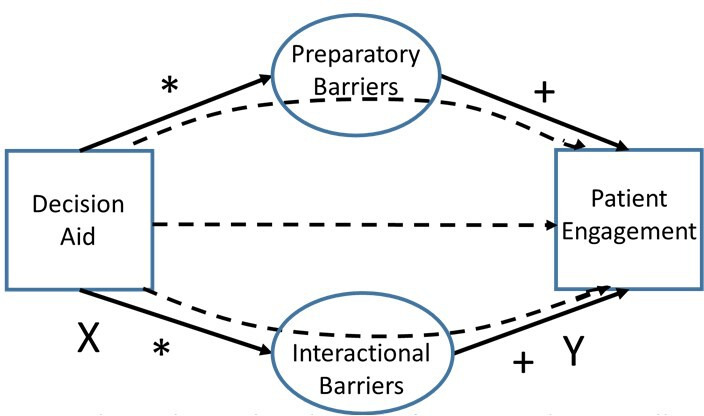
Schematic depicting the mediating role of preparatory and interactional barriers on engagement. The dashed lines represent the test for the overall effect of whether the decision aid improves engagement through that pathway. *Effect of decision aid on barriers; + Effect of barriers on engagement.
Persistent barriers to engagement experienced by socioeconomically disadvantaged patients: we will estimate logistic and Poisson regression models with socioeconomic deprivation as the explanatory variable, and each candidate persistent barrier as described above as the outcomes, in order to assess the extent to which persistent barriers to engagement are associated with socioeconomic disadvantage. Models will include surgeon and clinic random effects to account for patient clustering.
Sample size and power calculations for aims 1 and 2
Aim 1
We estimate a sample size of 563 patients and assume 23 surgeons. This was reduced from our original estimate of 1050 patients largely due to challenges associated with the COVID-19 pandemic. Aim 1 has two primary endpoints: PEPPI-5 self-efficacy and active patient participation behaviours (count). We desire a family-wise two-sided type I error rate of α=0.05; under a Bonferroni correction; tests will be conducted with nominal α=0.05/2=0.025. We consider half of an SD difference to be clinically relevant.65
Self-efficacy: assuming PEPPI-5 has an SD of 4.3 and both within-surgeon and within-site-between surgeon intraclass correlation coefficient (ICC) of 0.07,52 we will have 80% power to detect effects as small as 0.55×4.3=2.4 and 90% power to detect effects as small as 0.63×4.3=2.7 on a scale of 5–25.
Active patient participation behaviours: assuming the active patient participation behaviour count has an SD of 23.1 and a within-surgeon ICC of 0.01 and within-site-between surgeon ICC of 0.0001,55 we have 80% power to detect a difference of 0.50×23.1=11.6 and 90% power to detect a difference as small as 0.57×23.1=13.2 on a 0–150 scale.
Aim 2
MacKinnon et al have shown that one of the most accurate tests for mediation or indirect effect is the ‘asymmetric distribution of products’ test66 and have provided extensive simulation studies for estimating power for a variety of mediation tests.67 68 PowMedR software69 was developed based on that work, which we exploit here. We assume a sample size of 563 and then deduct 23 df for surgeon effects and 7 df for number of waves, yielding an effective sample size of 533. In addition, because we are testing two mediators, we set α=0.05/2=0.025 for these two tests. Suppose we have small mediation effects with R2=2% for the effect of the intervention on the latent barrier mediator (figure 4) and for the effect of the latent mediator on PEPPI-5 score or on active patient participation behaviour count. Suppose additionally that the three observed items have correlation of at least r=0.60. Then, the average of those three items will have reliability of λ=(r+(1/3)(1−r)), yielding net R2 values between the intervention and the observed mediator and between the observed mediator and PEPPI-5 score or active patient participation behaviour count of λR2=0.82×0.02=1.6%. Using the PowMedR software, we will have 60% power to detect mediation with small effect size and >99% power to detect mediation with medium effect size. Power will be higher with five items.
Once mediating barriers are detected, we use a model to test for an association of each barrier to a baseline indicator of socioeconomic disadvantage. We assume 30% of the sample will be disadvantaged, evenly distributed among clinics and surgeons. Assuming we will be testing up to four barriers, as we desire a family-wise two-sided type I error rate of α=0.05, under a Bonferroni correction, tests will be conducted with nominal α=0.05/4=0.0125. We will have 80% power to detect an effect size of 0.31 and 90% power to detect an effect size of 0.35.
Analysis plan for aim 3
Early interviews will be reviewed independently by at least three investigators to generate a preliminary list of conceptual codes that will be used to reduce the data. The identified coding schemes will be compared and discussed to reach consensus for a preliminary coding taxonomy, which will guide primary coding of subsequent interviews. If new concepts emerge during subsequent interviews, this coding taxonomy will undergo iterative revisions, and earlier interviews will be recoded to include the emerging constructs. We will use visual displays to broadly categorise the data and organise them into overarching themes, facilitating comparisons between our patient cohorts.70 We will use NVivo basic program (QSR International-Melbourne) to manage data and facilitate analysis.
We will take two approaches to data analysis. First, we will perform directed content analysis to identify and categorise barriers to engagement deductively.71 72 We will also perform inductive coding to identify previously unrecognised barriers and to characterise the mechanisms by which the identified barriers limited patient engagement despite a decision aid. We will also explore how patients were able to overcome, or not overcome, identified barriers. We will compare and contrast the experiences reported by patients based on their characteristics to elucidate the interaction between socioeconomic disadvantage and patient engagement.
Data integration
We use an explanatory mixed-methods approach to integrate the quantitative findings in order to identify potential targets for adjunct interventions (figure 5).73 The quantitative analysis will identify and prioritise persistent barriers to engagement that exist despite the decision aid. By understanding patients’ experiences with these barriers, we can obtain insight into potential ways to ameliorate them. From this integration, we will identify a list of potential targets for adjunct interventions, prioritised by the proportion of patients who experience the barrier and perceived impact of the barrier on engagement.
Figure 5.
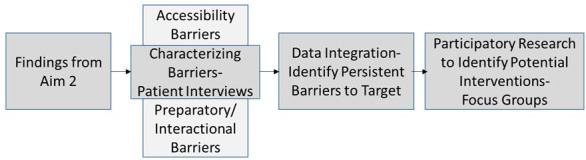
Overview of mixed methods.
Focus groups
We will perform directed content analysis to identify those components of the discussion directly relevant to our goal of identifying adjunct interventions to target identified barriers.61 62 The deliverable from the focus groups will be a list of potential adjunct interventions to target prioritised barriers.74
COVID-19 response
The COVID-19 pandemic necessitated a number of changes to our study protocol. First, trial accrual was halted on 24 March 2020, in response to the pandemic. Starting in August 2020, sites resumed recruitment when local conditions allowed (start times varied between August 2020 and January 2021). The impact of COVID-19 necessitated a minor redesign of the analytical plan to include post-COVID-19 indicators and time effects (described in this manuscript). Next, trial procedures were altered (eg, allowing remote consent, converting site visits to virtual, increasing flexibility in modality of interviews and focus groups). Finally, the pandemic led to slower accrual than expected. The stepped-wedge design made it difficult to adjust for COVID-19-related changes in accrual without introducing bias, as our sites were in both usual care and intervention arms at the time the pandemic started. Rather than disrupt the integrity of the stepped-wedge design, we accepted a smaller overall sample size for aim 1 (primary effectiveness analysis) than was originally planned. This manuscript presents the power for the updated projected sample size. We also revised the protocol to increase the sample of patients to be included in the analysis for aim 2 and the sampling pool for aim 3. We accomplished this by extending the period of enrolment beyond wave 7 (through 31 December 2021) for the sites that are still recruiting within the stepped-wedge design as of 30 August 2021.
Ethics and dissemination
Ethical review
This protocol has been approved by the National Cancer Institute Central Institutional Review Board. All participants provide written informed consent. Identifying information is redacted prior to analysis. A Certificate of Confidentiality has been issued to protect the privacy of subjects by limiting the disclosure of identifiable, sensitive information. We have regular review by the Data and Safety Monitoring Board of the Alliance for Clinical Trials in Oncology.
Relevance and dissemination
SDM has the potential to improve quality of care and reduce health disparities. To engage in SDM, patients must have both (1) knowledge of the treatment options, and (2) power—the self-perceived need and capacity—to influence decision-making. SDM interventions, for example, decision aids, consistently increase knowledge. However, barriers to patient empowerment hinder engagement. Importantly, socioeconomically disadvantaged patients disproportionately experience these barriers to engagement. Understanding how decision aids address these barriers to disadvantaged patients’ engagement in decision-making and identifying persistent barriers that can be targeted by adjunct interventions are critical steps toward reducing health disparities.
Our findings will advance the science of medical decision-making with the potential to reduce socioeconomic health disparities. By understanding barriers to engagement in SDM that persist despite receipt of a decision aid, we will identify targets for adjunct interventions. We propose a sustainable model of SDM that maximises clinics’ finite resources by combining the routine pre-consultation delivery of a decision aid with the tailored delivery of adjunct interventions, thereby addressing persistent barriers to engagement. If proven effective, this approach will have far-reaching implications across a variety of healthcare decisions.
Supplementary Material
Footnotes
Contributors: Conception and design of the protocol—JRS, DZ, SC, JT, RW, BMH, PJR, JLT and HBN. Drafting the article—JRS, JLT and HBN. Critical revisions of the article—JRS, DZ, SC, JT, RW, BMH, PJR, JLT and HBN. Final approval of the version to be published—JRS, DZ, SC, JT, RW, BMH, PJR, JLT and HBN.
Funding: This work was supported by the Agency for Healthcare Research and Quality (R01HS025194). There is also support for the Alliance for Clinical Trials in Oncology from U10CA180821, U10CA180882 and UG1CA189823.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Lagendijk M, van Maaren MC, Saadatmand S, et al. Breast conserving therapy and mastectomy revisited: breast cancer-specific survival and the influence of prognostic factors in 129,692 patients. Int J Cancer 2018;142:165–75. 10.1002/ijc.31034 [DOI] [PubMed] [Google Scholar]
- 2.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233–41. 10.1056/NEJMoa022152 [DOI] [PubMed] [Google Scholar]
- 3.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227–32. 10.1056/NEJMoa020989 [DOI] [PubMed] [Google Scholar]
- 4.van Maaren MC, de Munck L, de Bock GH, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol 2016;17:1158–70. 10.1016/S1470-2045(16)30067-5 [DOI] [PubMed] [Google Scholar]
- 5.Christiansen P, Carstensen SL, Ejlertsen B, et al. Breast conserving surgery versus mastectomy: overall and relative survival-a population based study by the Danish breast cancer Cooperative Group (DBCG). Acta Oncol 2018;57:19–25. 10.1080/0284186X.2017.1403042 [DOI] [PubMed] [Google Scholar]
- 6.de Boniface J, Szulkin R, Johansson ALV. Survival after breast conservation vs Mastectomy adjusted for comorbidity and socioeconomic status: a swedish national 6-year follow-up of 48 986 Women. JAMA Surg 2021;156:628–37. 10.1001/jamasurg.2021.1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Sangen MJC, van de Wiel FMM, Poortmans PMP, et al. Are breast conservation and mastectomy equally effective in the treatment of young women with early breast cancer? long-term results of a population-based cohort of 1,451 patients aged ≤ 40 years. Breast Cancer Res Treat 2011;127:207–15. 10.1007/s10549-010-1110-x [DOI] [PubMed] [Google Scholar]
- 8.Laurberg T, Lyngholm CD, Christiansen P, et al. Long-term age-dependent failure pattern after breast-conserving therapy or mastectomy among Danish lymph-node-negative breast cancer patients. Radiother Oncol 2016;120:98–106. 10.1016/j.radonc.2016.05.006 [DOI] [PubMed] [Google Scholar]
- 9.Nguyen DV, Kim S-W, Oh Y-T, et al. Local recurrence in young women with breast cancer: breast conserving therapy vs. mastectomy alone. Cancers 2021;13. 10.3390/cancers13092150. [Epub ahead of print: 29 04 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mundy LR, Rosenberger LH, Rushing CN, et al. The evolution of breast satisfaction and well-being after breast cancer: a Propensity-Matched comparison to the norm. Plast Reconstr Surg 2020;145:595–604. 10.1097/PRS.0000000000006535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kouwenberg CAE, de Ligt KM, Kranenburg LW, et al. Long-term health-related quality of life after four common surgical treatment options for breast cancer and the effect of complications: a retrospective patient-reported survey among 1871 patients. Plast Reconstr Surg 2020;146:1–13. 10.1097/PRS.0000000000006887 [DOI] [PubMed] [Google Scholar]
- 12.Pesce C, Jaffe J, Kuchta K, et al. Patient-reported outcomes among women with unilateral breast cancer undergoing breast conservation versus single or double mastectomy. Breast Cancer Res Treat 2021;185:359–69. 10.1007/s10549-020-05964-0 [DOI] [PubMed] [Google Scholar]
- 13.Frisell A, Lagergren J, de Boniface J. National study of the impact of patient information and involvement in decision-making on immediate breast reconstruction rates. Br J Surg 2016;103:1640–8. 10.1002/bjs.10286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martinez KA, Resnicow K, Williams GC, et al. Does physician communication style impact patient report of decision quality for breast cancer treatment? Patient Educ Couns 2016;99:1947–54. 10.1016/j.pec.2016.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mandelblatt J, Kreling B, Figeuriedo M, et al. What is the impact of shared decision making on treatment and outcomes for older women with breast cancer? J Clin Oncol 2006;24:4908–13. 10.1200/JCO.2006.07.1159 [DOI] [PubMed] [Google Scholar]
- 16.Frongillo M, Feibelmann S, Belkora J, et al. Is there shared decision making when the provider makes a recommendation? Patient Educ Couns 2013;90:69–73. 10.1016/j.pec.2012.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandelblatt JS, Berg CD, Meropol NJ, et al. Measuring and predicting surgeons??? practice styles for breast cancer treatment in older women. Med Care 2001;39:228–42. 10.1097/00005650-200103000-00004 [DOI] [PubMed] [Google Scholar]
- 18.Greenberg CC, Schneider EC, Lipsitz SR, et al. Do variations in provider discussions explain socioeconomic disparities in postmastectomy breast reconstruction? J Am Coll Surg 2008;206:605–15. 10.1016/j.jamcollsurg.2007.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morrow M, Jagsi R, Alderman AK, et al. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA 2009;302:1551–6. 10.1001/jama.2009.1450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kind AJH, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med 2014;161:765–74. 10.7326/M13-2946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christian CK, Niland J, Edge SB, et al. A multi-institutional analysis of the socioeconomic determinants of breast reconstruction: a study of the National comprehensive cancer network. Ann Surg 2006;243:241–9. 10.1097/01.sla.0000197738.63512.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobs LK, Kelley KA, Rosson GD, et al. Disparities in urban and rural mastectomy populations : the effects of patient- and county-level factors on likelihood of receipt of mastectomy. Ann Surg Oncol 2008;15): :2644–52. 10.1245/s10434-008-0053-5 [DOI] [PubMed] [Google Scholar]
- 23.Lautner M, Lin H, Shen Y, et al. Disparities in the use of breast-conserving therapy among patients with early-stage breast cancer. JAMA Surg 2015;150:778–86. 10.1001/jamasurg.2015.1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jagsi R, Jiang J, Momoh AO, et al. Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. J Clin Oncol 2014;32:919–26. 10.1200/JCO.2013.52.2284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sisco M, Du H, Warner JP, et al. Have we expanded the equitable delivery of postmastectomy breast reconstruction in the new millennium? Evidence from the National cancer data base. J Am Coll Surg 2012;215:discussion 666:658–66. 10.1016/j.jamcollsurg.2012.07.008 [DOI] [PubMed] [Google Scholar]
- 26.Moyer A. Psychosocial outcomes of breast-conserving surgery versus mastectomy: a meta-analytic review. Health Psychol 1997;16:284–98. 10.1037/0278-6133.16.3.284 [DOI] [PubMed] [Google Scholar]
- 27.Stevens LA, McGrath MH, Druss RG, et al. The psychological impact of immediate breast reconstruction for women with early breast cancer. Plast Reconstr Surg 1984;73:619–26. 10.1097/00006534-198404000-00018 [DOI] [PubMed] [Google Scholar]
- 28.Schain WS. Breast reconstruction. update of psychosocial and pragmatic concerns. Cancer 1991;68:1170–5. [DOI] [PubMed] [Google Scholar]
- 29.Elder EE, Brandberg Y, Björklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast 2005;14:201–8. 10.1016/j.breast.2004.10.008 [DOI] [PubMed] [Google Scholar]
- 30.Jagsi R, Li Y, Morrow M, et al. Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg 2015;261:1198–206. 10.1097/SLA.0000000000000908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Janz NK, Mujahid M, Lantz PM, et al. Population-based study of the relationship of treatment and sociodemographics on quality of life for early stage breast cancer. Qual Life Res 2005;14:1467–79. 10.1007/s11136-005-0288-6 [DOI] [PubMed] [Google Scholar]
- 32.Hawley ST, Fagerlin A, Janz NK, et al. Racial/ethnic disparities in knowledge about risks and benefits of breast cancer treatment: does it matter where you go? Health Serv Res 2008;43:1366–87. 10.1111/j.1475-6773.2008.00843.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freedman RA, Kouri EM, West DW, et al. Racial/ethnic disparities in knowledge about one's breast cancer characteristics. Cancer 2015;121:724–32. 10.1002/cncr.28977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Janz NK, Mujahid MS, Hawley ST, et al. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer 2008;113:1058–67. 10.1002/cncr.23660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katz SJ, Lantz PM, Janz NK, et al. Patient involvement in surgery treatment decisions for breast cancer. J Clin Oncol 2005;23:5526–33. 10.1200/JCO.2005.06.217 [DOI] [PubMed] [Google Scholar]
- 36.Polacek GNLJ, Ramos MC, Ferrer RL. Breast cancer disparities and decision-making among U.S. women. Patient Educ Couns 2007;65:158–65. 10.1016/j.pec.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 37.Maly RC, Stein JA, Umezawa Y, et al. Racial/ethnic differences in breast cancer outcomes among older patients: effects of physician communication and patient empowerment. Health Psychol 2008;27:728–36. 10.1037/0278-6133.27.6.728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 2014;94:291–309. 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- 39.Durand M-A, Carpenter L, Dolan H, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS One 2014;9:e94670. 10.1371/journal.pone.0094670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6–8. 10.1056/NEJMp1209500 [DOI] [PubMed] [Google Scholar]
- 41.Stacey D, et al. Decision AIDS for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014;1:CD001431. 10.1002/14651858.CD001431.pub4 [DOI] [PubMed] [Google Scholar]
- 42.Trikalinos TA, Wieland LS, Adam GP, et al. Decision AIDS for cancer screening and treatment. Rockville (MD), 2014. [PubMed] [Google Scholar]
- 43.Waljee JF, Rogers MAM, Alderman AK. Decision AIDS and breast cancer: do they influence choice for surgery and knowledge of treatment options? J Clin Oncol 2007;25:1067–73. 10.1200/JCO.2006.08.5472 [DOI] [PubMed] [Google Scholar]
- 44.National Cancer Institute Community Oncology Research Program . Available: http://ncorp.cancer.gov/ [Accessed 16 Oct 2015].
- 45.Alliance for Clinical Trials in Oncology . Available: https://www.allianceforclinicaltrialsinoncology.org/main/ [Accessed 10 Nov 2021].
- 46.Bruce JG, Tucholka JL, Steffens NM. Feasibility of providing web-based information to breast cancer patients prior to a surgical consult. J Cancer Educ 2017. 10.1007/s13187-017-1207-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tucholka JL, Yang D-Y, Bruce JG, et al. A randomized controlled trial evaluating the impact of web-based information on breast cancer patients' knowledge of surgical treatment options. J Am Coll Surg 2018;226:126–33. 10.1016/j.jamcollsurg.2017.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials 2007;28:182–91. 10.1016/j.cct.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 49.Informed Medical Decisions Foundation . Available: http://www.informedmedicaldecisions.org/ [Accessed 13 Oct 2015].
- 50.Dialog H. Available: http://www.healthdialog.com/ [Accessed 13 Oct 2015].
- 51.Maly RC, Frank JC, Marshall GN, et al. Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc 1998;46:889–94. 10.1111/j.1532-5415.1998.tb02725.x [DOI] [PubMed] [Google Scholar]
- 52.ten Klooster PM, Oostveen JCM, Zandbelt LC, et al. Further validation of the 5-item perceived efficacy in patient-physician interactions (PEPPI-5) scale in patients with osteoarthritis. Patient Educ Couns 2012;87:125–30. 10.1016/j.pec.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 53.Street RL, Voigt B, Geyer C, et al. Increasing patient involvement in choosing treatment for early breast cancer. Cancer 1995;76:2275–85. [DOI] [PubMed] [Google Scholar]
- 54.Street RL, Gordon HS, Ward MM, et al. Patient participation in medical consultations: why some patients are more involved than others. Med Care 2005;43:960–9. 10.1097/01.mlr.0000178172.40344.70 [DOI] [PubMed] [Google Scholar]
- 55.Gordon HS, Street RL. How physicians, patients, and observers compare on the use of qualitative and quantitative measures of physician-patient communication. Eval Health Prof 2016;39:496–511. 10.1177/0163278715625737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sepucha KR, Belkora JK, Chang Y, et al. Measuring decision quality: psychometric evaluation of a new instrument for breast cancer surgery. BMC Med Inform Decis Mak 2012;12:51. 10.1186/1472-6947-12-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Singh GK. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health 2003;93:1137–43. 10.2105/AJPH.93.7.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Singh GK, Miller BA, Hankey BF. Changing area socioeconomic patterns in U.S. cancer mortality, 1950-1998: Part II--Lung and colorectal cancers. J Natl Cancer Inst 2002;94:916–25. 10.1093/jnci/94.12.916 [DOI] [PubMed] [Google Scholar]
- 59.Singh GK, Miller BA, Hankey BF, et al. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975-2000. Cancer 2004;101:1051–7. 10.1002/cncr.20467 [DOI] [PubMed] [Google Scholar]
- 60.Singh GK, Miller BA, Hankey BF, et al. Changing area socioeconomic patterns in U.S. cancer mortality, 1950-1998: Part I--All cancers among men. J Natl Cancer Inst 2002;94:904–15. 10.1093/jnci/94.12.904 [DOI] [PubMed] [Google Scholar]
- 61.Delbecq AL, Van De Ven A. Group techniques for program planning: a guide to nominal groups and Delphi process. Glenview, IL: Scott Foresman Company, 1975. [Google Scholar]
- 62.Van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health 1972;62:337–42. 10.2105/AJPH.62.3.337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sheppard VB, Oppong BA, Hampton R, et al. Disparities in breast cancer surgery delay: the lingering effect of race. Ann Surg Oncol 2015;22:2902–11. 10.1245/s10434-015-4397-3 [DOI] [PubMed] [Google Scholar]
- 64.Muthén & Muthén . Mplus. Los Angeles, CA. [Google Scholar]
- 65.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582–92. 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- 66.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83–104. 10.1037/1082-989X.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci 2007;18:233–9. 10.1111/j.1467-9280.2007.01882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fritz MS, Taylor AB, Mackinnon DP. Explanation of two anomalous results in statistical mediation analysis. Multivariate Behav Res 2012;47:61–87. 10.1080/00273171.2012.640596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kenny DA. Mediation: PowMedR. Available: http://davidakenny.net/webinars/Mediation/PowMedR/PowMedR.html [Accessed 28 Feb 2017].
- 70.Miles MB, Huberman AM. An expanded Sourcebook: qualitative data analysis. 2nd ed. Thousand Oaks, California: SAGE Publications, Inc, 1994. [Google Scholar]
- 71.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 72.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 73.Creswell JW, Plano-Clark WL. Designing and conducting mixed methods research. 2nd ed. Thousand Oaks, California: SAGE Publications, 2011. [Google Scholar]
- 74.O'Connor AM, Cranney A. User Manual - Acceptability; 1996.
- 75.Wallston KA, Cawthon C, McNaughton CD, et al. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med 2014;29:119–26. 10.1007/s11606-013-2568-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Degner LF, Sloan JA, Venkatesh P. The control preferences scale. Can J Nurs Res 1997;29:21–43. [PubMed] [Google Scholar]
- 77.Bennett C, Graham ID, Kristjansson E, et al. Validation of a preparation for decision making scale. Patient Educ Couns 2010;78:130–3. 10.1016/j.pec.2009.05.012 [DOI] [PubMed] [Google Scholar]
- 78.Légaré F, Kearing S, Clay K, et al. Are you sure?: assessing patient decisional conflict with a 4-item screening test. Can Fam Physician 2010;56:e308–14. [PMC free article] [PubMed] [Google Scholar]
- 79.Williams GC, Grow VM, Freedman ZR, et al. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol 1996;70:115–26. 10.1037/0022-3514.70.1.115 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.