Abstract
Objectives
To identify and thematically analyse how healthcare professionals (HCPs) integrate patient values and preferences (‘values integration’) in primary care for adults with non-communicable diseases (NCDs).
Design
Systematic review and meta-aggregation methods were used for extraction, synthesis and analysis of qualitative evidence.
Data sources
Relevant records were sourced using keywords to search 12 databases (ASSIA, CINAHL, DARE, EMBASE, ERIC, Google Scholar, GreyLit, Ovid-MEDLINE, PsycINFO, PubMed-MEDLINE, Scopus and Web of Science).
Eligibility criteria
Records needed to be published between 2000 and 2020 and report qualitative methods and findings in English involving HCP participants regarding primary care for adult patients.
Data extraction and synthesis
Relevant data including participant quotations, authors’ observations, interpretations and conclusions were extracted, synthesised and analysed in a phased approach using a modified version of the Joanna Briggs Institute (JBI) Data Extraction Tool, as well as EPPI Reviewer and NVivo software. The JBI Critical Appraisal Checklist for Qualitative Research was used to assess methodological quality of included records.
Results
Thirty-one records involving >1032 HCP participants and 1823 HCP-patient encounters were reviewed. Findings included 143 approaches to values integration in clinical care, thematically analysed and synthesised into four themes: (1) approaches of concern; (2) approaches of competence; (3) approaches of communication and (4) approaches of congruence. Confidence in the quality of included records was deemed high.
Conclusions
HCPs incorporate patient values and preferences in healthcare through a variety of approaches including showing concern for the patient as a person, demonstrating competence at managing diseases, communicating with patients as partners and tailoring, adjusting and balancing overall care. Themes in this review provide a novel framework for understanding and addressing values integration in clinical care and provide useful insights for policymakers, educators and practitioners.
PROSPERO registration number
CRD42020166002.
Keywords: general medicine (see internal medicine), primary care, asthma, general diabetes, adult oncology, adult cardiology
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This is the first systematic review to identify and thematically analyse approaches to values integration in clinical care.
An extensive search strategy and well-defined study selection criteria were employed to find qualitative evidence related to this topic.
Systematic, transparent methods were used to appraise the quality of included records, extract and analyse data.
Thematic analysis can present limitations as it involves subjective interpretation of previously reported evidence.
Introduction
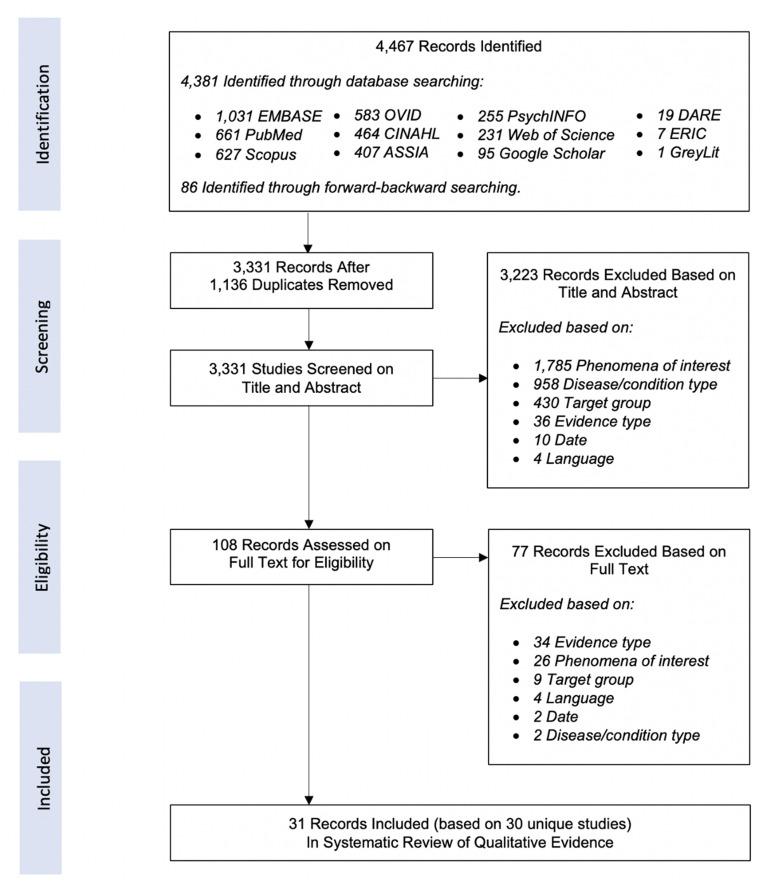
The practice of evidence-based medicine (EBM) calls for patient values and preferences to be considered and integrated by clinicians alongside the best available research and clinical expertise.1 These three forces comprise the EBM ‘triad’ (figure 1) and, when conscientiously and judiciously applied2 by healthcare professionals (HCPs), it is believed that optimal patient-centred care can be achieved.3
Figure 1.
The evidence-based medicine (EBM) triad.
Delivering patient-centred care relies on understanding the patient’s values and preferences at every stage,4 but acquiring this knowledge is challenging. Patients and their needs are heterogenous, difficult to predict, subject to change and dependent on many factors.5
Patient values and preferences are the unique understandings, preferences, concerns, expectations and life circumstances of each patient.6 Values are defined as a patient’s attitudes and perceptions about certain healthcare options, and preferences are their preferred choices after accounting for their values.7
A recent systematic review of qualitative studies identified a taxonomy of what patients say they value in healthcare including uniqueness, autonomy, compassion, professionalism, responsiveness, partnership and empowerment.8 While this is useful for understanding what patients value and prefer, the question remains: How do HCPs integrate values and preferences into clinical care for individual patients? Very little research has been done on this critical component of EBM.
Research evidence (especially quantitative research, randomised controlled trials in particular)9 has received most of the attention in EBM, with less systematic consideration given to values integration which has been ‘almost completely ignored’,10 resulting in a paucity of data on values integration in clinical decision-making.11
Research on patient values and preferences—and how HCPs approach values integration—tends to be reliant on qualitative evidence,8 a level of evidence that does not appear in the standard EBM hierarchy of evidence.12–14 Considerations for patient values and preferences are seldom encoded into clinical practice guidelines15 and there are no established methods for addressing values integration when developing guidelines.16
Non-communicable diseases (NCDs), also known as chronic diseases, are defined by WHO as conditions of long duration resulting from a number of physical, behavioural or environmental factors and account for 7-out-of-10 deaths worldwide.17 The four most common categories of NCDs include cancers, diabetes, cardiovascular (CV) diseases and chronic respiratory diseases. These are often managed in primary and secondary care settings18 and require ongoing therapeutic relationships involving more frequent HCP-patient interaction which makes values integration even more important.
Improvements in patient-centred care can lead to improved outcomes including lowering readmission rates, decreasing hospital length of stay, reducing mortality and better management of chronic diseases overall.17 Therefore, understanding how to better incorporate patient values and preferences in healthcare is an essential skill that can improve clinical outcomes19 and patient satisfaction20 to help reduce the burden of NCDs.
The primary objective of this review is to identify and thematically analyse how HCPs integrate patient values and preferences in primary care for adults with NCDs.
Methods
Methodology
This review used a meta-aggregation methodology.21 A protocol was prospectively published on the PROSPERO international register of systematic reviews, https://www.crd.york.ac.uk/prospero/ registration no. CRD42020166002 (online supplemental appendix A).
bmjopen-2022-067268supp001.pdf (912.9KB, pdf)
Participants and phenomena of interest
Participants included practising HCPs in primary and secondary care: professionals with experience in direct patient care in non-inpatient and non-emergency settings, including doctors, nurses and other clinicians.22 Phenomena of interest included HCP approaches, behaviours, attitudes, perceptions, experiences, perspectives, opinions and observations regarding values integration in clinical care.
Information sources and search strategy
Authors were interested in current relevant practice so this review’s preplanned search considered studies and other evidence published between January 2000 and August 2020 with full text available in English reporting data derived from HCP participants. Only studies using qualitative methods including, but not limited to, interviews, focus groups, direct observations, surveys, narrative reviews or content analysis were included.
Search terms were identified and adapted from an initial scoping of databases and an analysis of text from titles, abstracts and index terms, followed by a systematic literature search of 12 databases (ASSIA, CINAHL, DARE, EMBASE, ERIC, Google Scholar, GreyLit, Ovid-MEDLINE, PsycINFO, PubMed-MEDLINE, Scopus and Web of Science). The search was tailored to the unique formats, operators and conventions of each database using a variety of search terms related to participants, phenomena of interest, context, setting and qualitative methodologies and methods (online supplemental appendix B).
Study eligibility and selection
Two reviewers (MT and GS) participated in a four-stage screening and selection process using the EPPI Reviewer software23 including independent double-screening24 of 10% of initial abstracts and titles, single screening of remaining titles and abstracts, full-text screening of all records not yet excluded and forward-backward search and screening of additional citations. Conflicts among screeners were resolved by conference and mutual agreement or by a third reviewer. Inclusion/Exclusion criteria were predetermined by reviewers including:
Evidence type (excluded records that did not use any qualitative methods and did not report qualitative findings).
Date (excluded records published before the year 2000).
Language (excluded records for which full text was not available in the English language).
Phenomena of interest (excluded records that did not report findings related to incorporating patient values and preferences).
Target group (excluded records that did not involve HCP participants, or were not concerned with HCP interactions with adult patients).
Disease/Condition type (excluded records that did not refer to primary or secondary care or one of the top four most common NCD categories (oncology (cancers), CV, endocrine related (diabetes) and respiratory)).
Appraisal of quality
The objectivity of qualitative research can be strengthened through the use of quality methods.25 This review used the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Qualitative Research,21 26 27 a validated tool to help determine the methodological quality of included records in systematic reviews (online supplemental appendix C).
Extraction, synthesis and analysis
This review employed meta-aggregative methods for extraction, synthesis and analysis.21 Data including participant quotations, authors’ observations, interpretations and conclusions were extracted in a phased approach using a modified version of the JBI Data Extraction Tool27 (online supplemental appendix D). One author (MT) with experience in qualitative methods and coding conducted line-by-line coding using NVivo28 computer software allowing for simultaneous coding and an initial synthesis of the information.29
Using an inductive approach, extraction began with reading and re-reading records to become familiar with the content followed by hand-coding of all records. This enabled the development of a preliminary coding scheme for organising and managing data in NVivo, wherein the author continued to inductively and iteratively code the data. Codes were collated, analysed, grouped and categorised into a number of increasingly narrow sets of codes based on statements and ideas across data. Themes, developed from the codes, were further synthesised based on patterns and similarities in their meaning to arrive at a final set of primary themes that could be used as a basis for a meaningful summary and interpretation. Themes were only considered if there were two or more codes underlying the theme.
Excluded data
Some records reported mixed methods, but quantitative data and/or data not derived from HCP participants were excluded from this review.
Patient and public involvement
It was not appropriate or possible to involve patients or the public in the design, conduct, reporting or dissemination plans of this systematic review. However, a minority of the included records reported patient and public involvement in their methods.
Results
Included records
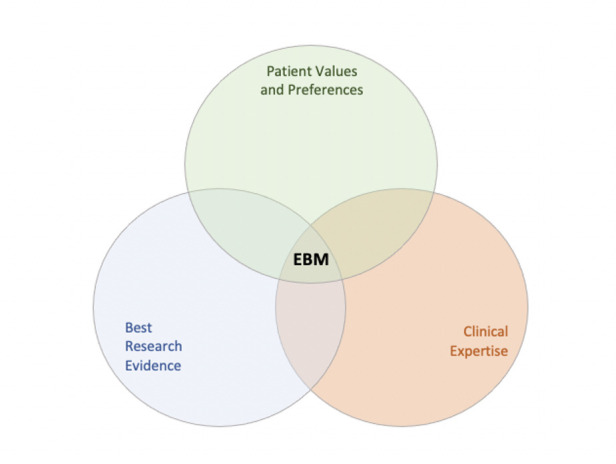
The initial search identified 3331 records and after full-text screening 31 records were included (figure 2).30 No systematic review regarding values integration was published between 2000 and 2020.
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Characteristics of included records
Most records were peer-reviewed published reports of original research, two are separate reports from the same study,31 32 and one was an unpublished dissertation33 (table 1). The most common methods of data collection were interviews (in-depth, semi-structured (in-person and telephone)) in 17 studies,31 32 34–48 observations (real-time, in-person or audio/video recordings) in 9 studies33 34 39 48–53 and focus groups in 6 studies.40 41 54–57 Other methods included surveys,45 55 58 Delphi technique,45 48 narrative description,34 narrative review,59 document analysis,36 evidence review,60 research work groups,11 chart audits,34 note taking34 and video reflexive ethnography (VRE).61 Nine studies employed more than one method.33 34 36 39–41 45 48 55
Table 1.
Characteristics of included records
| Study | Method(s) | Analytical approach | HCPs (n) | Practice setting(s) | HCP experience | Encounters observed | Location | Number of findings (online supplemental appendix E) |
| Aita V et al.34 (2005) | Chart audits, interviews, narrative descriptions, note taking, participatory observations | Coding, group analysis, themes | Physicians (44) | 18 Family practice clinics | Unspecified | 1500 | USA | 25 |
| Chhabra KR et al.49 (2013) | Observations of audio-recorded consultations | Theme-oriented discourse analysis | Oncologists (15) | 2 Cancer centres | Unspecified | 20 | USA | 27 |
| Davis K et al.35 (2017) | Semi-structured interviews | Coding, themes | Physicians (33) | Multiple clinics in 2 HMO territories | Mean 13–20 years | N/A | USA | 20 |
| Elwyn G et al.54 (2000) | Focus groups | Codes, themes | GPs (6) | 6 Service settings | Mean 12 years | N/A | UK | 40 |
| Feiring E et al.36 (2020) | Document analysis, in-depth interviews | Thematic analysis | Various (8) | 4 Specialist institutions | Unspecified | N/A | Norway | 16 |
| Ford S et al.*32 (2002) | Semi-structured interviews | Constant comparative analysis | Various (37) | Hospitals and clinics | Unspecified | N/A | UK | 17 |
| Ford S et al.*31 (2003) | Semi-structured interviews | Constant comparative analysis | Various (37) | Hospitals and clinics | Unspecified | N/A | UK | 54 |
| Ford S et al.50 (2006) | Observation of video-taped consultations | Thematic coding | GPs (13) | 12 GP surgeries | Unspecified | 149 | UK | 16 |
| Friedberg MW et al.37 (2013) | Semi-structured interviews | Codes, themes | Various (23) | 8 Primary care | Unspecified | N/A | USA | 23 |
| Golden SE et al.38 (2017) | Interviews | Directed content analysis | Various (20) | 7 Medical centres | Mean 12 years | N/A | USA | 30 |
| Gruß I et al.39 (2019) | Observations, semi-structured interviews | Codes, template analysis | Physicians (8) | 1 Cancer clinic | Unspecified | 8 | USA | 24 |
| Hall J et al.59 (2011) | Narrative review | Narrative review | Various (unspecified) | N/A | N/A | N/A | USA | 18 |
| Hart PL et al.58 (2014) | Mail survey | Thematic analysis | Nurses (374) | Hospital (43%) Non-hospital (57%) |
Mean 22.4 years | N/A | USA | 10 |
| Hisham R et al.40 (2016) | Focus groups, in-depth interviews | Thematic analysis | Physicians (18) | 2 Rural clinics | Mean 6.2 years | N/A | Malaysia | 7 |
| Jefford M et al.60 (2002) | Review | Review | Doctors (unspecified) | Unspecified | Unspecified | N/A | Australia | 27 |
| Kennedy BM et al.55 (2017) | Focus groups, survey | Thematic categorisation | Various (7) | 1 Rural clinic | Median 12 years | N/A | USA | 18 |
| Landmark AM et al.51 (2016) | Observations of video-recorded encounters | Conversation analysis | Physicians (17) | 1 University hospital | Unspecified | 17 | Norway | 34 |
| Lown B et al.11 (2009) | Research work groups | Constant comparative analysis and grounded theory | PCPs (41) | Hospital-based practices | ‘At least >3 years postresidency’ | N/A | USA | 49 |
| McLeod H33 (2017) | Observations of video-recorded encounters, VRE | Grounded theory | PCPs (17) | 1 Hospital-based clinic | Unspecified | 15 | USA | 89 |
| Murdoch J et al.52 (2020) | Observations of video-recorded consultations | Conversation analysis | GPs (5) | 3 General practices | Range <10 to >20 years | 22 | UK | 37 |
| Paiva D et al.56 (2019) | Focus groups | Grounded theory | Various (12) | 1 Institution | Range 1 to >10 years | N/A | Portugal | 36 |
| Pieterse AH et al.53 (2011) | Observations of video-recorded consultations | Coded and categorised observations | Radiation oncologists (10) | 1 Hospital | Median 7 years | 25 | The Netherlands | 35 |
| Salter C et al.41 (2019) | Focus group, interview, observations of video-recorded consultations | Thematic analysis | GPs (5) | 3 General practices | Range <10 to >20 years | 40 | UK | 40 |
| Schulman-Green DJ et al.57 (2006) | Focus groups | Content analysis | Various (11) | Hospital-affiliated practices | Unspecified | N/A | USA | 14 |
| Shepherd HL et al.42 (2011) | Telephone interviews | Framework analysis | Physicians (22) | Unspecified | Mean 24 years | N/A | Australia | 19 |
| Shortus T et al.43 (2011) | In-depth interviews | Grounded theory, constant comparison | Various (29) | ‘…a range of clinical settings…’ | ‘…a range of clinical experience…’ | N/A | Australia | 29 |
| Tracy CS et al.44 (2003) | Semi-structured interviews | Constant comparative method | FPs (15) | 15 Practices | Range 2–32 years | N/A | Canada | 18 |
| Van Humbeeck L et al.45 (2020) | Delphi, cognitive interviewing, survey | Thematic analysis | Various (174) | 2 Hospitals | Range <1 to >21 years | N/A | Belgium | 26 |
| Vermunt N et al.46 (2019) | Semi-structured interviews | Framework analysis | Physicians (33) | Hospitals and community clinics | Range 3–34 years | N/A | The Netherlands | 29 |
| Visser LNC et al.47 (2018) | Semi-structured interviews | Content analysis | Oncologists (13) | Academic and general hospitals | Range 4–41 years | N/A | The Netherlands | 31 |
| Zulman DM et al.48 (2020) | Delphi, interviews, observations | Evidence review | Physicians (18) | Primary care clinics at 1 academic medical centre, 1 VA hospital, 1 federally qualified health centre | Unspecified | 27 | USA | 47 |
HCP experience early career <11 years, mid-career 11–20 years, late career ≥21 years.88
*Ford 2002 and Ford 2003 are two reports from the same study.
CV, cardiovascular; DAS-O, decision analysis system for oncology; GP, general practitioner; HCP, healthcare professional; HMO, health maintenance organisation; N/A, not applicable; PCP, primary care physician; VA, veteran's administration; VRE, video reflexive ethnography.
At least 1032 HCP participants are represented in the included records, including 477 nurses/nurse practitioners, 417 physicians and 138 other HCP types including allied health professionals, pharmacists, clinical administrators, nutritionists, social workers and patient decision coaches. At least 1823 HCP-patient consultations, encounters or interactions (either observed or described) in various clinical settings are represented in the records.
Nearly half of the studies included were conducted in North America with 15 in the USA and 2 in Canada, followed by 5 in the UK, 3 in Australia, 3 in the Netherlands, 2 in Norway and 1 each in Belgium, Italy, Malaysia and Portugal.
Methodological quality of included records
Confidence in the quality of included records was deemed high. Most used appropriate qualitative methodologies, methods and analytical approaches, resulting in meaningful findings and conclusions. However, most records failed to provide adequate reflexive statements locating researchers theoretically or culturally, and also failed to address the researchers’ influence on the research and vice versa (online supplemental appendix C).
Findings
This review identified 143 approaches—specific behaviours, actions, practices or experiences of HCPs—to integrating patient values and preferences in clinical care. These were thematically analysed and synthesised into four primary themes—approaches of concern, competence, communication and congruence—and several subthemes (table 2). See online supplemental appendix E for a complete list of approaches.
Table 2.
Taxonomy of themes: approaches to values integration
| Concern | Competence | Communication | Congruence |
|
|
|
|
Approaches of concern
HCPs incorporate patient values and preferences when they demonstrate concern for the patient as a unique individual and as a partner in their own care, and show concern for diseases and their effects on the patient.
This includes advocating on a patient’s behalf,11 such as talking to HCP colleagues to get additional insights, making referrals to other specialist or advocating for second opinions on conditions and treatments.44
‘Advocates for the patient (includes willingness to circumvent or adapt the system) and Physicians’ advocacy within (or around) the health-care system helps patients implement jointly negotiated decisions.’11
HCPs use caring and connecting behaviours like acting in a sincere,45 relational11 and empathetic manner, making the patient feel comfortable and creating a safe space to talk, question and/or disagree,33 and using expressive touch.48 Treating the patient as unique45 and seeing the patient’s perspective48 are also approaches that demonstrate concern which can include HCPs sharing their own personal experiences, interests or feelings.11 HCPs also show compassion, empathy and basic human concern47 without being judgmental.45 Other such approaches include remaining present, mindful and ‘in the moment’48 while providing care for immediate concerns, and incorporating preventative care to demonstrate concern for the patient’s overall well-being.34
‘A physician participant highlighted the importance of the physician’s effort to act in a relational way by saying, ‘‘…Express caring in that interaction—this is what the physician can do. And the quality of that caring is what enhances the intrinsic motivation of the patient to take the responsibility’’.’11
HCPs also show concern by empowering the patient through approaches that value the individual, enable self-management and promote patient agency by recognising, confirming and validating patient autonomy11 and respecting privacy.45 Empowering also includes creating an environment of equality,54 establishing trust by sharing control,11 inviting the patient to lead41 or to set the pace31 in clinical encounters, letting the patient have the final say in decisions45 or providing opportunities to reconsider previous decisions.54
‘The patient is enabled to keep control of his or her own situation. The patient has authority in the decision-making process.’45
HCPs also show concern by inviting the involvement of others38 in clinical decision-making, such as asking loved ones, family or caregivers45 to help the patient make choices, or seeking input from colleagues, specialists and other HCPs for advice or second opinions.11
‘You have to have the team. You have to have the physician buy-in. And often I ask them to bring somebody with them so that there’s somebody else there who can hear the conversation….’38
HCPs show concern by partnering with the patient48 by investing time with them,41 cultivating mutual respect to form a ‘therapeutic alliance’33 and treating the patient as an equal partner.31 Understanding the patient is a key element of partnering52 as well as taking a long-term view of the patient’s care.
‘Partnership process—strategies to establish and maintain a partnership with the patient.’48
HCPs also show concern by sensing, that is, perceiving and acting in a sensitive manner, including interpersonal sensitivity,59 cultural sensitivity58 or showing respect and deference for religious beliefs.33 HCPs also may use intuition in the clinical encounter59 to sense patient moods and feelings.
‘There are two basic types of interpersonal sensitivity. The first type is simply to notice (and, relatedly, remember) the other person’s appearance, words, or nonverbal behavior. And The second, and most commonly investigated, kind of interpersonal sensitivity involves accuracy in interpreting cues.’59
Approaches of competence
HCPs incorporate patient values and preferences when they competently address diseases, share decision-making, understand and use research evidence and professionally manage patient care.
Competence includes many behaviours including decision making, when HCPs competently engage with the patient to support, direct and share decision-making. Shared decision-making (SDM) was one of the most frequently mentioned approaches to incorporating patient values and preferences in the records. It is its own discipline in the patient-centred care paradigm with many adherents and a large body of evidence regarding its use and effectiveness with several SDM methods and techniques. However, as its name implies, SDM addresses values integration when making treatment decisions and does not account for the predecision-making and postdecision-making values and preferences that are important to patients and HCPs in their overall long-term relationships.
‘The physician sharing decision making acknowledges that power is shared and integrates the patient’s preferences into a mutual decision.’11
SDM also involves HCP competence with research evidence54 as well as skills to help formulate the patient’s stance on issues and options,51 or to negotiate decisions.11 HCPs may also use decision aids or tools to assist the patient in making treatment decisions39 or use vivid descriptions,51 a technique to aid the patient in arriving at their own conclusions. SDM also includes directing behaviours that involve the HCP giving their own opinion or recommendation to the patient46 when asked or when the patient is unable to make a decision.33 It also involves listing, an action by HCPs to suggest or ‘draw out patients’ views about possible choices’.54
‘[If] you ask [patients] what they think is wrong with them, then they won’t tell you. But if you give them a list of things that are in your mind, then they will usually identify some of their concerns.’54
HCP competence also includes managing the patient care process to help achieve mutual goals without controlling the patient, including working on mutually setting an agenda41 and priorities.48 This also includes negotiating with patients to help them understand, assess, weigh and prioritise options,52 gaining clarity on agreements and disagreements11 and openly discussing the pros and cons of options.46 All of this is with the intent of eventually gaining agreement on issues, mutual roles, possible solutions and next steps.43 Managing also refers to managing patient emotions which includes efforts to reduce patient anxiety and distress,31 exploring and responding to emotions, allowing time for patients to process emotions as well as HCPs displaying their own emotions.47 Managing also involves planning and preparing behaviours such as action plans for treatment,37 agreeing on priorities,48 arranging follow-ups46 and collaborative goal setting.52 It also includes preparing for the clinical encounter to maximise the efficiency of time with the patient and readiness to elicit and incorporate values and preferences.52
Another competency is to manage the administrative processes that are needed to support values integration, such as having clear systematic processes for patient encounters and consultations,46 using electronic health records and other methods of record keeping to capture and encode patient values and preferences for future access,48 leaving time for questions in the encounter,38 having smooth continuity of care including a system for follow-up56 and collaborative action planning.41
‘This process involved a significant investment of time, negotiation, deliberation, and shared decision making about the steps towards goal attainment, as well as setting a nominal target.’41
Competent management also includes professionalism, that is, approaching the patient in a professional and honest manner. Honesty, transparency,38 responsiveness45 and a reality-based approach43 to the patient play an important role in patient-centred care and values integration, as well as being consistent with information, care and decisions.56
‘Professional responsiveness, Professionalism—Healthcare providers explain what is possible and what is not…Healthcare providers are honest with patients…Healthcare providers do not judge the patient’s situation…Healthcare providers respect the patient’s privacy.’45
Approaches of communication
HCPs incorporate patient values and preferences when they successfully communicate with the patient as a partner, share information and evidence and manage patient engagement.
This includes approaches like acknowledging the patient’s efforts to get and stay healthy or to adhere to treatment plans,48 as well as expressing support or reassurance for the patient’s preferences and validating their choices.53
‘The second component of the practice involves acknowledging specific patient efforts in a genuine and positive manner.’48
Values integration through communication also includes clarifying the patient’s stances by checking on the status of their choices, feelings, values and preferences,41 framing and reframing52 to help clarify their positions and repeating to reinforce patient preferences.56 It also includes revisiting patient decisions over time43 as patients may change their minds. Values clarification methods45 are also described in which HCPs actively engage with the patient to discuss positive and negative characteristics of options to clarify which are most important to the patient.
‘The mutual clarification of values can be a rewarding exercise, as it not only ensures the best possible decision but also demonstrates to patients a genuine interest in incorporating their views.’45
Another communication approach is encouraging the patient to be active in the process, to participate in the clinical encounter/conversation,49 encouraging patient questions31 and patient storytelling.33 One technique, motivational interviewing, ‘uses an empathic non-confrontational style to increase the motivation for behaviour change, engage patients with treatment and build therapeutic relationships’.56
‘By comparison, providers preferring ‘‘personalized care’’ described their approach as encouraging rather than persuasive, and they were more accepting of different priorities and preferences.’43
Values integration via communication also includes exchanging information including explaining or defining the clinical problem46 or sharing necessary biomedical information with the patient and informing them of the facts of the condition or diagnosis.39
‘Clinicians emphasized sharing medical information with patients. We observed a few instances during which clinicians also prompted discussion of patients’ goals and values. Clinicians reported a clear rationale in interviews as to why sharing biomedical information was central for them.’39
Information exchange also includes sharing and presenting research evidence,39 as well as a willingness to see more information and encouraging patients to seek more information.11
‘There was a general view that evidence-based information regarding diagnosis and treatment options must be shared with patients during a consultation.’31
Information exchange also includes patient education,60 coaching,48 tailoring information for the patient as well as using teaching aids, written materials60 or other educational interventions.55 Interviewing and eliciting approaches are other forms of information exchange and they were the most frequent behaviours described in the records. HCPs use various approaches to gain information from the patient, including directly eliciting patient values,49 preferences,35 goals57 and circumstances,31 sometimes referred to as patient-centred clinical interviewing.34 It also involves getting patients to appraise various preferences openly and to identify their favoured choices.53
‘…this meant providing current information, risks and benefits, eliciting questions and adjusting information to patients’ needs, being honest about the limits of the physician’s and scientific knowledge, and presenting an opinion.’11
Communication also includes exploring, asking open-ended questions to better assess patient values, preferences and expectations.34 Studies noted the importance of openly exploring alternatives with the patient and exploring the clues and cues—verbal and non-verbal—that patients often provide.31
‘Explore ideas, fears, and expectations of the problem and possible treatments. And, Informants stated that experienced practitioners are continually alert to signals that patients accept the level of involvement being required of them and adapt accordingly.’54
Values integration also occurs through language when HCPs use tones and techniques such as deferential, directive or inviting language,49 emotion-oriented speech47 or common language, terms or phrases with patients,38 all of which can support the patient’s values, preferences and autonomy.
‘‘‘Deferential’’ language…physicians did not evaluate each treatment on behalf of the patient. Instead, they used language that minimized their role in the patient’s decision and deferred to the patient’s autonomy.’49
HCPs also integrate values by listening, including active listening without interruption59 or simple silence as a response to certain patient emotions.47
‘The most frequently mentioned skill was the ability to listen. Listening to patients was seen as a basic skill to enable ‘‘assessment of the language that patients use in order to pitch information level’’ and to ‘‘encourage discussion by listening to patients’ views without interruption’’.’31
When HCPs summarise information, choices or next steps for patients, they are also integrating values. This can be done as written or audio summaries of clinical discussions60 or summaries of the encounter31 at the end of clinical visits to ensure that the HCP and patient depart with a mutual understanding of the decisions and next steps. This also allows patients to more easily share information with caregivers or other HCPs.
Approaches of congruence
HCPs incorporate patient values and preferences when they customise and harmonise care for each patient and balance their overall approach to care considering the patient’s values and preferences, the best available research evidence and their own clinical expertise.
Specifically, HCPs seek congruence by adjusting and tailoring care for each unique patient. HCPs adjust information based on a patient’s needs, values and preferences,11 as well as tailor options for the patient36 according the many factors that must be considered within the realm of the research evidence, the patient’s values and the HCP’s own expertise.
‘Identify preferred format and provide tailor-made information…This competence consists of making the correct range of options available and listing them in a logical sequence and in sufficient clarity so that patients perceive the opportunity to take part in the decision.’54
HCPs also seek congruence by maintaining balance and flexibility regarding patient needs, values, information, communication style, decision-making, clinical/treatment approaches and roles.50 This also refers to HCP efforts to balance multiple factors such as evidence, information, issues, mutual needs, shared power and responsibilities for and with the patient.56
‘The informants stressed the importance of maintaining flexibility: adherence to the ‘‘informed choice’’ approach was considered ‘‘another form of paternalism’’.’54
Discussion
Incorporating patient values and preferences in healthcare is critical for patient-centred care, but it is complex and requires medical knowledge as well as ‘soft skills’ such as social, psychological and communication proficiencies.62 The themes developed in this review provide a useful model for better understanding, exploring and teaching this topic. When plotted on the EBM triad (figure 3), these themes also provide a useful framework for operationalising values integration into evidence-based clinical practice.
Figure 3.
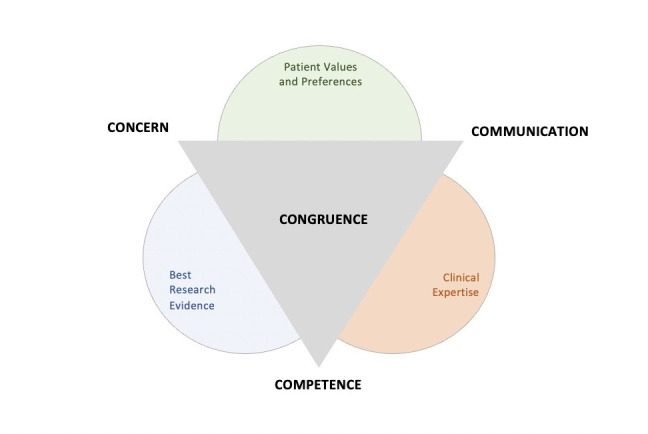
The EBM triad and primary themes of approaches to values integration.
Our findings fit well into the existing EBM discussion and contribute new evidence to this discussion by identifying and thematically analysing, for the first time, the specific behaviours and approaches that practising HCPs use to integrate patient values and preferences into everyday clinical care.
Previous studies have described the importance of approaches that show concern for patient autonomy,32 60 taking feelings seriously,33 seeing the patient as a person and showing concern about their problems, diseases, effects, treatments and research evidence,32 63–67 as well as advising HCPs to make ‘statements of concern, empathy and reassurance’.67
Previous studies have also described ‘the competences of involving patients in healthcare choices’.54 the competencies required for SDM,32 technical competencies for involving patients,50 ‘culturally competent care’.58 ‘competencies they (HCPs) can execute to involve patients in decision making’11 and the importance of medical competency for HCPs.8
Previous research has also emphasised ‘provider-patient communication as key to achieving patient-centred care’.65 patient-centred54 and physician-patient communication32 and the importance of skills to ‘communicate with patients about their treatment options’.37
Finally, other EBM literature encourages HCPs to ensure that ‘clinical goals are congruent’ with patient goals,34 to ‘achieve congruence in the consultation’.50 to strive for ‘congruency between (the patient’s) preferred and actual involvement in decision making’.64 to seek ‘congruence between (patient’s) options and their values’68 and to find ‘more balance between science, clinical expertise and patient values’.8
Strengths and limitations
This review used accepted, thorough and systematic methodologies and methods for qualitative synthesis, and included a wide range of databases in the search for records. Authors’ interpretations and participant quotes were included extensively throughout the review. There remains a possibility that evidence has been missed searching only records published from 2000 in English, however adherence to robust systematic review methods helped to minimise this limitation.
Although there is a paucity of qualitative studies explicitly on the topic of ‘integrating’ or ‘incorporating’ patient values and preferences, this review identified records on related topics such as ‘patient-centred care’, ‘implementing SDM’, ‘HCP-patient communications’, ‘eliciting goals’ or ‘managing patient involvement’ and similar. There were 17 previous reviews on related topics,8 63–78 which did not qualify for inclusion in this review. However, a forward-backward search of references in those reviews identified four records already selected for inclusion in this review44 49 54 57 strengthening confidence in the robustness of this review and saturation of the topic. The original record search period between January 2000 and August 2020 is now 2 years old and, while no other qualitative systematic review has been published on this topic between August 2020 and October 2022, it is possible that additional qualitative evidence has been published which is not included in this review.
Double screening is considered best practice for systematic reviews, with single screening recommended primarily as an ‘appropriate methodological short cut’79 for experienced researchers.24 We double-screened 10% of titles/abstracts and included reviewer discussions and debates to arrive at mutually agreed screening criteria, before single screening was conducted for the remaining records. One author conducted the initial coding and further developed themes in discussion with other authors. All authors contributed to the review, analysis and interpretation of findings.
Rigorous thematic analysis methods were used to synthesise the findings and identify key themes and ideas across all records. Thematic analysis involves interpretation of other researchers’ previous interpretations which can present limitations. To minimise this limitation, we extensively reported direct verbatims and transcripts from HCP participants and authors when describing concepts, themes and subthemes to prevent misinterpretation of the original evidence.
Implications for policy and practice
Integrating patient values and preferences in modern clinical practice is important and impacts health outcomes.80 Findings from this review could help improve health policy, HCP clinical performance or patient satisfaction and outcomes by describing specific and practical patient-centred approaches to values integration.
These findings can aid the inclusion of values integration in clinical guidelines which so far has been limited15 and for which there are few systematic standards.16 However, encoding values and preferences into a single guideline has challenges, so individual HCP skills to elicit and incorporate patient values and preferences will always be necessary.81
Medical education and training emphasises patient-centred care and values integration in theory, but HCPs receive inadequate instruction on the skills needed to deliver it.82 This review’s primary themes and descriptions of specific approaches provide a theoretical and practical framework for education and training on this topic.
Scope of practice varies for physicians, nurses, allied health professionals and others, but this review shows they each have a role in—and something important to contribute to—values integration. These findings can influence policymakers who should consider the entire continuum of care and provide training, tools, funding and support and encourage values integration at every level of care delivery. These findings also offer a structure to educate and assess HCPs and organisations as a whole on values integration beyond the consultation and ‘throughout the care delivery at every point’.83 HCPs and health systems need to consider patient values and preferences beyond just treatment decisions5 and this study underscores the need to be aware of, and skilled at, a number of approaches.
This review can inform clinical practice to improve HCP-patient encounters, develop patient-centred tools and improve patient outcomes19 and satisfaction.20 Advanced practice providers could benefit from better clinical communications skills84 and the approaches described in this review could provide a guide for improvement. Despite evidence that patient decision aids improve specific outcomes,85 many HCPs do not use them86 due to lack of awareness, availability, difficulty of use or inappropriate context. Findings from this review could be useful in guiding tool developers to make and disseminate more effective decision aids.
Future research
The broad themes described in this review provide multiple areas for future study. The primary themes of concern, competence, communication and congruence should be explored further. While shared decision-making and HCP-patient communication are already well-represented in the literature, more study is needed on other approaches such as caring and connecting, planning and preparing or goals setting, to name a few. Future research could consider whether the themes described in this review vary, or are more common, among specific NCD groups, HCP types or care settings.
There is significant research in the area of SDM between HCPs and patients, but very little in the area of values integration outside of the decision-making process. Future research should explore this gap. Future studies could also seek to quantify many of the qualitative findings from this review to collect evidence on what contributes to better outcomes. Many of the approaches described from the data and the resulting themes may be applicable to clinical care for other chronic diseases, but separate independent studies are encouraged.
Finally, the theme of congruence described in this review—how HCPs tailor, adjust, balance and harmonise approaches for each patient—needs more scientific consideration. It is under-represented in the published literature, yet it represents the essence of EBM: the ‘conscientious, explicit and judicious’87 integration of patient values and preferences with the best research evidence and clinical expertise.
Reflexivity statement
The principal investigator for this review was a part-time graduate student (MT) at the University of Oxford while residing and working full-time in the USA in the pharmaceutical industry. MT has experience in designing, executing and analysing qualitative methods involving focus groups, interviews, Delphi methods, surveys and literature/content analysis for health-related research. MT has authored or coauthored peer-reviewed and published articles, however, had not previously conducted a systematic review. MT is not a clinician but has worked with clinicians for >25 years in hospital administration, health education and communications, research, policy and advocacy.
Author GS, living in Canada, has a clinical background, and was also enrolled in the same Oxford graduate programme. Authors A-MB and CH live in the UK, are both faculty members from the University of Oxford’s MSc in evidence-based healthcare programme. Both have academic and/or clinical backgrounds that include researching, writing and teaching extensively on EBM and the role of patient values and preferences. They provided supervision throughout the review.
Conclusion
HCPs incorporate patient values and preferences in healthcare through a variety of approaches including: concern for the patient as a person as well as diseases and their effects; competence at skillfully addressing diseases, research evidence and managing patient care; communication with the patient as a partner, sharing information and evidence and productively managing patient encounters; and congruence to tailor, adjust and balance their approaches to overall care for each patient. Themes in this review provide a novel framework for understanding and addressing values integration in clinical care and provide useful insights for policymakers, educators and practitioners.
Supplementary Material
Footnotes
Twitter: @tringm
Contributors: As principal investigator, MT led the planning, conduct and reporting of the study, submitted the manuscript and is responsible for the overall content as guarantor. As research assistant, GS contributed to the conduct of the literature screening and review as well as provided review and editing of the manuscript. As research supervisors, A-MB and CH contributed to the planning, oversight and reporting, as well as provided review and editing of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: CH receives grant funding from the NIHR School of Primary Care Research. He has received financial remuneration from an asbestos case and given legal advice on mesh and hormone pregnancy tests cases. He has received expenses and fees for his media work, for teaching EBM and is also paid for his GP work in NHS out of hours. He has also received income from the publication of a series of toolkit books and for appraising treatment recommendations in non-NHS settings. He is Director of CEBM and former editor-in-chief of BMJ-EBM. No competing interests for other authors.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Guyatt GH, Haynes RB, Jaeschke RZ, et al. Users' guides to the medical literature: XXV. evidence-based medicine: principles for applying the users' guides to patient care. evidence-based medicine Working group. JAMA 2000;284:1290–6. 10.1001/jama.284.10.1290 [DOI] [PubMed] [Google Scholar]
- 2.Sackett DL, Rosenberg WMC, Gray JAM, et al. Evidence based medicine: what it is and what it isn't. BMJ 1996;312:71–2. 10.1136/bmj.312.7023.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mellis C. Evidence-Based medicine: what has happened in the past 50 years? J Paediatr Child Health 2015;51:65–8. 10.1111/jpc.12800 [DOI] [PubMed] [Google Scholar]
- 4.Gooberman-Hill R. Qualitative approaches to understanding patient preferences. Patient 2012;5:215–23. 10.1007/BF03262494 [DOI] [PubMed] [Google Scholar]
- 5.Lee YK, Low WY, Ng CJ. Exploring patient values in medical decision making: a qualitative study. PLoS One 2013;8:e80051. 10.1371/journal.pone.0080051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Straus SE, Pattani R, Veroniki AA. Evidence-based medicine : how to practice and teach EBM. Edinburgh: Elsevier, 2019. [Google Scholar]
- 7.Llewellyn-Thomas HA, Crump RT. Decision support for patients: values clarification and preference elicitation. Med Care Res Rev 2013;70:50S–79 http://ezproxy-prd.bodleian.ox.ac.uk:2094/ 10.1177/1077558712461182 [DOI] [PubMed] [Google Scholar]
- 8.Bastemeijer CM, Voogt L, van Ewijk JP, et al. What do patient values and preferences mean? A taxonomy based on a systematic review of qualitative papers. Patient Educ Couns 2017;100:871–81. 10.1016/j.pec.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 9.Fernandez A, Sturmberg J, Lukersmith S, et al. Evidence-Based medicine: is it a bridge too far? Health Res Policy Syst 2015;13:66. 10.1186/s12961-015-0057-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly MP, Heath I, Howick J, et al. The importance of values in evidence-based medicine. BMC Med Ethics 2015;16:69. 10.1186/s12910-015-0063-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lown BA, Clark WD, Hanson JL. Mutual influence in shared decision making: a collaborative study of patients and physicians. Health Expect 2009;12:160–74. 10.1111/j.1369-7625.2008.00525.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petrisor B, Bhandari M. The hierarchy of evidence: levels and grades of recommendation. Indian J Orthop 2007;41:11–15. 10.4103/0019-5413.30519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Porta M, Greenland S, Burón A. A dictionary of epidemiology. Oxford, England: Oxford University Press, 2014. [Google Scholar]
- 14.Ebm levels of evidence. Available: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 [Accessed Sep 2020].
- 15.van der Weijden T, Pieterse AH, Koelewijn-van Loon MS, et al. How can clinical practice guidelines be adapted to facilitate shared decision making? A qualitative key-informant study. BMJ Qual Saf 2013;22:855–63. 10.1136/bmjqs-2012-001502 [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Coello PA, Brożek J, et al. Using patient values and preferences to inform the importance of health outcomes in practice Guideline development following the grade approach. Health Qual Life Outcomes 2017;15:52. 10.1186/s12955-017-0621-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noncommunicable diseases. Available: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases [Accessed 20 Jan 2020].
- 18.Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? systematic review. Can Fam Physician 2018;64:832. [PMC free article] [PubMed] [Google Scholar]
- 19.Gluyas H. Patient-Centred care: improving healthcare outcomes. Nurs Stand 2015;30:50–9. 10.7748/ns.30.4.50.e10186 [DOI] [PubMed] [Google Scholar]
- 20.Wolf DM, Lehman L, Quinlin R, et al. Effect of patient-centered care on patient satisfaction and quality of care. J Nurs Care Qual 2008;23:316–21. 10.1097/01.NCQ.0000336672.02725.a5 [DOI] [PubMed] [Google Scholar]
- 21.Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc 2015;13:179–87. 10.1097/XEB.0000000000000062 [DOI] [PubMed] [Google Scholar]
- 22.Transforming and scaling up health professionals' education and training: World Health organization guidelines. Available: https://www.who.int/publications/i/item/transforming-and-scaling-up-health-professionals%E2%80%99-education-and-training [Accessed Jan 2020]. [PubMed]
- 23.EPPI reviewer 4 for systematic reviews. Available: http://eppi.ioe.ac.uk/cms/Default.aspx?alias=eppi.ioe.ac.uk/cms/er4 [Accessed Jan 2020].
- 24.Mahtani KR, Heneghan C, Aronson J. Single screening or double screening for study selection in systematic reviews? BMJ Evid Based Med 2020;25:149–50. 10.1136/bmjebm-2019-111269 [DOI] [PubMed] [Google Scholar]
- 25.Lincoln YS, Guba EG. Naturalistic inquiry. 11. Beverly Hills; London: SageChapter, 1985: 293. [Google Scholar]
- 26.Lockwood C, Porrit K, Munn Z, eds. JBI Reviewer’s Manual - Chapter 2: Systematic Review of Qualitative Evidence. Joanna Briggs Institute (JBI), 2017. [Google Scholar]
- 27.Aromataris E. Chapter 2. In: Munn Z, ed. Joanna Briggs Institute Reviewer’s Manual, 2017. [Google Scholar]
- 28.NVivo for qualitative research. Available: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home [Accessed Mar 2020].
- 29.Bryman A. Social research methods. Oxford: Oxford University Press, 2012. [Google Scholar]
- 30.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ford S, Schofield T, Hope T. What are the ingredients for a successful evidence-based patient choice consultation?: a qualitative study. Soc Sci Med 2003;56:589–602. 10.1016/S0277-9536(02)00056-4 [DOI] [PubMed] [Google Scholar]
- 32.Ford S, Schofield T, Hope T. Barriers to the evidence-based patient choice (EBPC) consultation. Patient Educ Couns 2002;47:179–85. 10.1016/S0738-3991(01)00198-7 [DOI] [PubMed] [Google Scholar]
- 33.McLeod H. Respect and shared decision making in the clinical encounter. A Video-Reflexive ethnography, 2017
- 34.Aita V, McIlvain H, Backer E, et al. Patient-Centered care and communication in primary care practice: what is involved? Patient Educ Couns 2005;58:296–304. 10.1016/j.pec.2004.12.008 [DOI] [PubMed] [Google Scholar]
- 35.Davis K, Bellini P, Hagerman C, et al. Physicians' perceptions of factors influencing the treatment decision-making process for men with low-risk prostate cancer. Urology 2017;107:86–95. 10.1016/j.urology.2017.02.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feiring E, Friis T. Facilitators and barriers to clinicians' use of COPD action plans in self-management support: a qualitative study. Patient Educ Couns 2020;103:693–701. 10.1016/j.pec.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 37.Friedberg MW, Van Busum K, Wexler R, et al. A demonstration of shared decision making in primary care highlights barriers to adoption and potential remedies. Health Aff 2013;32:268–75. 10.1377/hlthaff.2012.1084 [DOI] [PubMed] [Google Scholar]
- 38.Golden SE, Thomas CR, Moghanaki D, et al. Dumping the information bucket: a qualitative study of clinicians caring for patients with early stage non-small cell lung cancer. Patient Educ Couns 2017;100:861–70. 10.1016/j.pec.2016.12.023 [DOI] [PubMed] [Google Scholar]
- 39.Gruß I, McMullen CK. Barriers to eliciting patient goals and values in shared decision-making breast cancer surgery consultations: an ethnographic and interview study. Psychooncology 2019;28:2233–9 http://ezproxy-prd.bodleian.ox.ac.uk:2094/ 10.1002/pon.5212 [DOI] [PubMed] [Google Scholar]
- 40.Hisham R, Liew SM, Ng CJ, et al. Rural doctors' views on and experiences with evidence-based medicine: the freedom qualitative study. PLoS One 2016;11:e0152649. 10.1371/journal.pone.0152649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salter C, Shiner A, Lenaghan E, et al. Setting goals with patients living with multimorbidity: qualitative analysis of general practice consultations. Br J Gen Pract 2019;69:e479–88. 10.3399/bjgp19X704129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shepherd HL, Butow PN, Tattersall MHN. Factors which motivate cancer doctors to involve their patients in reaching treatment decisions. Patient Educ Couns 2011;84:229–35. 10.1016/j.pec.2010.10.018 [DOI] [PubMed] [Google Scholar]
- 43.Shortus T, Kemp L, McKenzie S, et al. 'Managing patient involvement': provider perspectives on diabetes decision-making. Health Expect 2013;16:189–98. 10.1111/j.1369-7625.2011.00700.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tracy CS, Dantas GC, Upshur REG. Evidence-Based medicine in primary care: qualitative study of family physicians. BMC Fam Pract 2003;4:6. 10.1186/1471-2296-4-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Humbeeck L, Malfait S, Holvoet E, et al. Value discrepancies between nurses and patients: a survey study. Nurs Ethics 2020;27:1044–55. 10.1177/0969733020906595 [DOI] [PubMed] [Google Scholar]
- 46.Vermunt N, Elwyn G, Westert G, et al. Goal setting is insufficiently recognised as an essential part of shared decision-making in the complex care of older patients: a framework analysis. BMC Fam Pract 2019;20:76. 10.1186/s12875-019-0966-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Visser LNC, Schepers S, Tollenaar MS, et al. Patients' and oncologists' views on how oncologists may best address patients' emotions during consultations: an interview study. Patient Educ Couns 2018;101:1223–31. 10.1016/j.pec.2018.02.012 [DOI] [PubMed] [Google Scholar]
- 48.Zulman DM, Haverfield MC, Shaw JG, et al. Practices to foster physician presence and connection with patients in the clinical encounter. JAMA 2020;323:70–81. 10.1001/jama.2019.19003 [DOI] [PubMed] [Google Scholar]
- 49.Chhabra KR, Pollak KI, Lee SJ, et al. Physician communication styles in initial consultations for hematological cancer. Patient Educ Couns 2013;93:573–8. 10.1016/j.pec.2013.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ford S, Schofield T, Hope T. Observing decision-making in the general practice consultation: who makes which decisions? Health Expect 2006;9:130–7. 10.1111/j.1369-7625.2006.00382.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Landmark AMD, Svennevig J, Gulbrandsen P. Negotiating treatment preferences: physicians' formulations of patients' stance. Soc Sci Med 2016;149:26–36. 10.1016/j.socscimed.2015.11.035 [DOI] [PubMed] [Google Scholar]
- 52.Murdoch J, Salter C, Ford J, et al. The "unknown territory" of goal-setting: Negotiating a novel interactional activity within primary care doctor-patient consultations for patients with multiple chronic conditions. Soc Sci Med 2020;256:113040. 10.1016/j.socscimed.2020.113040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pieterse AH, Henselmans I, de Haes HCJM, et al. Shared decision making: prostate cancer patients' appraisal of treatment alternatives and oncologists' eliciting and responding behavior, an explorative study. Patient Educ Couns 2011;85:e251–9. 10.1016/j.pec.2011.05.012 [DOI] [PubMed] [Google Scholar]
- 54.Elwyn G, Edwards A, Kinnersley P, et al. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract 2000;50:892. [PMC free article] [PubMed] [Google Scholar]
- 55.Kennedy BM, Rehman M, Johnson WD, et al. Healthcare providers versus patients' understanding of health beliefs and values. Patient Exp J 2017;4:29–37. 10.35680/2372-0247.1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paiva D, Abreu L, Azevedo A, et al. Patient-Centered communication in type 2 diabetes: the facilitating and constraining factors in clinical encounters. Health Serv Res 2019;54:623–35. 10.1111/1475-6773.13126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schulman-Green DJ, Naik AD, Bradley EH, et al. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Educ Couns 2006;63:145–51. 10.1016/j.pec.2005.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hart PL, Mareno N. Cultural challenges and barriers through the voices of nurses. J Clin Nurs 2014;23:2223–33. 10.1111/jocn.12500 [DOI] [PubMed] [Google Scholar]
- 59.Hall JA. Clinicians’ accuracy in perceiving patients: Its relevance for clinical practice and a narrative review of methods and correlates. Patient Educ Couns 2011;84:319–24. 10.1016/j.pec.2011.03.006 [DOI] [PubMed] [Google Scholar]
- 60.Jefford M, Tattersall MHN. Informing and involving cancer patients in their own care. Lancet Oncol 2002;3:629–37. 10.1016/S1470-2045(02)00877-X [DOI] [PubMed] [Google Scholar]
- 61.Iedema R, Carroll K, Collier A. Video-reflexive ethnography in health research and healthcare improvement : theory and application. Boca Raton: CRC Press, 2018. [Google Scholar]
- 62.Salloch S, Otte IC, Reinacher-Schick A, et al. [Physician perspectives on the impact of patient preferences and the role of next-of-kin of patients in evidence-based decision-making: A qualitative interview study from oncology]. Z Evid Fortbild Qual Gesundhwes 2018;131-132:46–52. 10.1016/j.zefq.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 63.Contreary K, Collins A, Rich EC. Barriers to evidence-based physician decision-making at the point of care: a narrative literature review. J Comp Eff Res 2017;6:51–63. 10.2217/cer-2016-0043 [DOI] [PubMed] [Google Scholar]
- 64.Covvey JR, Kamal KM, Gorse EE, et al. Barriers and facilitators to shared decision-making in oncology: a systematic review of the literature. Support Care Cancer 2019;27:1613–37. 10.1007/s00520-019-04675-7 [DOI] [PubMed] [Google Scholar]
- 65.Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12:CD003267. 10.1002/14651858.CD003267.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harrington J, Noble LM, Newman SP. Improving patients' communication with doctors: a systematic review of intervention studies. Patient Educ Couns 2004;52:7–16. 10.1016/S0738-3991(03)00017-X [DOI] [PubMed] [Google Scholar]
- 67.Lewin SA, Skea ZC, Entwistle V. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2001:CD003267. 10.1002/14651858.CD003267 [DOI] [PubMed] [Google Scholar]
- 68.Stacey D, Légaré F, Lewis K, et al. Decision AIDS for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4:CD001431. 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals' perceptions. Implement Sci 2006;1:16. 10.1186/1748-5908-1-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Harrison M, Milbers K, Hudson M, et al. Do patients and health care providers have discordant preferences about which aspects of treatments matter most? Evidence from a systematic review of discrete choice experiments. BMJ Open 2017;7:e014719. 10.1136/bmjopen-2016-014719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Johnson RA, Huntley A, Hughes RA, et al. Interventions to support shared decision making for hypertension: a systematic review of controlled studies. Health Expect 2018;21:1191–207 http://ezproxy-prd.bodleian.ox.ac.uk:2094/ 10.1111/hex.12826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Laidsaar-Powell RC, Butow PN, Bu S, et al. Physician-patient-companion communication and decision-making: a systematic review of triadic medical consultations. Patient Educ Couns 2013;91:3–13. 10.1016/j.pec.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 73.Légaré F, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals' perceptions. Patient Educ Couns 2008;73:526–35. 10.1016/j.pec.2008.07.018 [DOI] [PubMed] [Google Scholar]
- 74.Mangin D, Stephen G, Bismah V, et al. Making patient values visible in healthcare: a systematic review of tools to assess patient treatment priorities and preferences in the context of multimorbidity. BMJ Open 2016;6:e010903. 10.1136/bmjopen-2015-010903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Marsh K, Caro JJ, Hamed A, et al. Amplifying each patient's voice: a systematic review of Multi-criteria decision analyses involving patients. Appl Health Econ Health Policy 2017;15:155–62. 10.1007/s40258-016-0299-1 [DOI] [PubMed] [Google Scholar]
- 76.Truglio-Londrigan M, Slyer JT. Shared decision-making for nursing practice: an integrative review. Open Nurs J 2018;12:1–14. 10.2174/1874434601812010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Truglio-Londrigan M, Slyer JT, Singleton JK, et al. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Libr Syst Rev 2012;10:4633–46. 10.11124/jbisrir-2012-432 [DOI] [PubMed] [Google Scholar]
- 78.Zwolsman S, te Pas E, Hooft L, et al. Barriers to GPs' use of evidence-based medicine: a systematic review. Br J Gen Pract 2012;62:e511–21. 10.3399/bjgp12X652382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Waffenschmidt S, Knelangen M, Sieben W, et al. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Methodol 2019;19:132. 10.1186/s12874-019-0782-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570. 10.1136/bmjopen-2012-001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lewis DK, Robinson J, Wilkinson E. Factors involved in deciding to start preventive treatment: qualitative study of clinicians' and lay people's attitudes. BMJ 2003;327:841. 10.1136/bmj.327.7419.841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Henschen BL, Ryan ER, Evans DB, et al. Perceptions of patient-centered care among first-year medical students. Teach Learn Med 2019;31:26–33. 10.1080/10401334.2018.1468260 [DOI] [PubMed] [Google Scholar]
- 83.Armstrong MJ, Mullins CD. Value assessment at the point of care: incorporating patient values throughout care delivery and a draft taxonomy of patient values. Value Health 2017;20:292–5. 10.1016/j.jval.2016.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Back AL, Fromme EK, Meier DE. Training clinicians with communication skills needed to match medical treatments to patient values. J Am Geriatr Soc 2019;67:S435–41. 10.1111/jgs.15709 [DOI] [PubMed] [Google Scholar]
- 85.O'Connor A. Using patient decision AIDS to promote evidence-based decision making. ACP J Club 2001;135:100. [PubMed] [Google Scholar]
- 86.Brace C, Schmocker S, Huang H, et al. Physicians' awareness and attitudes toward decision AIDS for patients with cancer. J Clin Oncol 2010;28:2286–92. 10.1200/JCO.2009.25.2874 [DOI] [PubMed] [Google Scholar]
- 87.Sackett DL, Straus S, Richardson W. Evidence-based medicine : how to practice and teach EBM. Edinburgh: Churchill Livingstone, 2000. [Google Scholar]
- 88.Dyrbye LN, Varkey P, Boone SL, et al. Physician satisfaction and burnout at different career stages. Mayo Clin Proc 2013;88:1358–67. 10.1016/j.mayocp.2013.07.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-067268supp001.pdf (912.9KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.