Abstract
Objective
The aim of this study was to assess the prevalence of pregnancy and associated factors among adolescent girls in Nguenyyiel Refugee Camp.
Design
Cross-sectional study was employed to conduct this study.
Setting
A community-based cross-sectional study was done in Nguenyyiel Refugee Camp.
Participants
Four hundred and fourteen adolescent girls participated in this study. The systematic random sampling technique was used to select respondents. Data were collected using a well-structured and pretested questionnaire. Pregnancy test was done using the human chorionic gonadotropin test. Bivariate and multivariate logistic regression analysis was run to identify factors associated with adolescent pregnancy.
Results
The prevalence of pregnancy among adolescent girls in the Nguenyyiel Refugee Camp was 21.7% (95% CI: 17.6% to 25.6%). Factors associated with adolescent pregnancy were age (17–19 years) (AOR): 2.79; 95% CI: 1.55 to 5.05; educational status: primary education (AOR: 7.69; 95% CI: 3.55 to 16.68) and no formal education (AOR: 3.42; 95% CI: 1.59 to 7.36); and household living arrangement: living with none of the biological parents (AOR: 2.14; 95% CI: 1.02 to 4.49) and living with either of the biological parent (AOR: 3.71; 95% CI: 1.76 to 7.81).
Conclusions and recommendations
This study showed that there is a high prevalence of pregnancy among adolescent girls in the study setting. Age (17–19 years), educational status and household living arrangement (living with none of the biological parents and living with either of the biological parents) were among the factors significantly associated with adolescent pregnancy. Hence, health workers and other stakeholders in the camps should focus on strengthening adolescent sexual health education giving special attention to late adolescents, uneducated and living without biological family.
Keywords: Reproductive medicine, Public health, Maternal medicine
Strengths and limitations of this study.
Conducting community-based studies, using primary data including collecting urine samples directly from the study participants in humanitarian settings, is strength.
The human chorionic gonadotropin test cannot detect a pregnancy that is less than a week old.
Since adolescent pregnancy is a sensitive issue, respondents may commit social desirability bias.
Therefore, the prevalence of pregnancy among adolescent girls identified by this study among study participants might be higher than the one reported by this study.
Introduction
Each year, an estimated 21 million adolescent girls become pregnant every year and approximately 12 million of them give birth worldwide.1 At least 777 000 births occur to adolescent girls younger than 15 years in developing countries.1 Adolescent pregnancy is associated with higher risks of adverse birth outcomes such as preterm birth, low birth weight, intrauterine growth retardation, stillbirth, unsafe abortion, maternal and neonatal mortality and morbidity compared with women in their 20s.2–10 Complications from pregnancy and childbirth are the leading cause of death among adolescent girls.11 12 Moreover, adolescent pregnancy is associated with social and economic problems like school dropout, unemployment and limited future opportunities, risk of remaining poor and, and increased cost for healthcare.3 13
Many teenage pregnancies in Ethiopia occur within marriage.14 Similarly, other studies have showed that the prevalence of pregnancy among adolescent girls in humanitarian settings (refugee camps or settlements) is 30% higher than among their non-displaced counterparts.13 14 This is due to the fact that adolescents in humanitarian settings are extremely vulnerable to early sexual practice, violence and exploitation or abuse compared with their counterparts in general population.15–17 The experience of forced migration impacts refugee adolescent girls’ decision-making power related to their sexual relationships and reproductive life.10 Hence, adolescents may lack the autonomy to determine over their affairs including their sexual and reproductive health and rights.12 18 Adolescents are also the only age group for whom AIDS deaths are on the rise.11
According to the Ethiopian Demographic and Health Survey and many other studies, the study area, Gambella regional state of Ethiopia, has high unmet need for family planning (23%),14 high polygamy practice (21%)19 and highest HIV/sexually transmitted infections prevalence in the country due to multiple factors such as, low service coverage, high prevalence of male uncircumcision, early sexual initiation among adolescents related to traditional malpractice like ‘Tifo bet’20 and environmental factors like presence of gold mining workers21 and others.14 18 20 22–24 Besides, the majority of the refugee community including adolescents are those who lost one or both of their parents during the conflict. This leaves the adolescent girls helpless and enforce them to be engaged in risky sexual behaviours. However, there was no study conducted to determine the prevalence and factors associated with pregnancy among adolescent refugees in humanitarian settings. This study, therefore, aimed at assessing the prevalence of pregnancy among adolescent girls and associated factors in the Nguenyyiel Refugee Camp, Gambella region, Southwest Ethiopia.
Methods and materials
Study design and setting
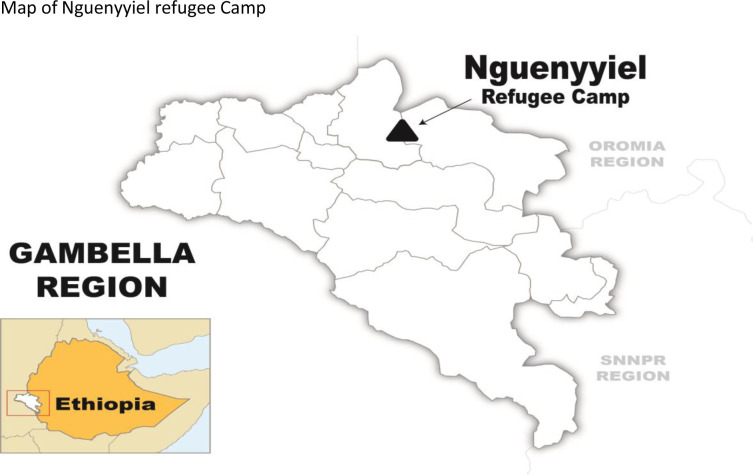
A community-based cross-sectional study was conducted in Nguenyyiel Refugee Camp, Gambella region, from 15 May 2021 to 15 June 2021. Gambella region of Ethiopia hosted a 337 081 refugee population from the bordering country of South Sudan in seven refugee camps (as of May 2021). The Nguenyyiel Refugee Camp is the newest and the largest camp in Ethiopia. It was opened to accommodate the new refugee influx from South Sudan following the escalation of the conflict in that country in July 2016. It is located in Itang special woreda (district). It is located about 769 km from the capital city, Finfinnee/Addis Ababa, and 55 km from the region’s capital city, Gambella25 (figure 1). It has 10 916 households and a total population of 90,506 that contains 43,759 men and 46,747 women. Adolescents constitute majority of the women in the reproductive age in the camp.
Figure 1.
Map of Nguenyyiel Refugee Camp, Gambella, Ethiopia. (Source: nguenyyiel refugee camp map - Bing)
Population
Source population
The source populations were all adolescent girls (10–19 years) in the Nguenyyiel Refugee Camp. The study populations were adolescent girls in the selected households who participated in this study.
Eligibility criteria
Inclusion criteria
All girls in the adolescence age interval10–19 who were residents in the Nguenyyiel Refugee Camp at least for the last 6 months before the data collection were considered eligible.
Sample size determination
The sample size was calculated for both objectives. For the first objective, sample size was calculated using a single population proportion formula with the assumptions of: Z=1.96 at 95% CI: d=margin of error assumed to be (0.05), p=prevalence of pregnancy in adolescent from previous studies2 and 10% non-response rate; n=Zα2p (1-p)/d2=421.
The sample size for the second objective was calculated by using the double population proportion formula using Epi Info V.3.0 statistical software by considering the following assumptions after reviewing previous literature: Zα/2: 1.96 at 95% confidence level, Zβ: power=statistical power of 80%, P1: the probability of outcome in the unexposed, P2: the probability of outcome in the exposed and r: ratio of unexposed to exposed (table 1).
Table 1.
Sample size calculation based on the significant factors of adolescent pregnancy; Nguenyyiel Refugee Camp, Gambella region, Southwest Ethiopia, 2021
| S/no. | Significant factors associated with adolescent pregnancy and citations | Power | 95% CI | The proportion of pregnancy among non-exposed adolescent girls (P1) | The proportion of pregnancy among exposed (P2) | Risk ratio (r) | Adjusted OR | n1 | n total |
| 1 | Educational status (no formal education vs secondary and above)42 | 80% | 1.96 | 31.0% | 7.4% | 0.24 | 3.83 | 164 | 181 |
| 2 | Modern contraceptive use (users vs non-users)38 | 80% | 1.96 | 64.6% | 19.2% | 0.29 | 10.62 | 131 | 144 |
| 3 | Marital status (married vs single (not-married))38 | 80% | 1.96 | 3.80% | 54.4% | 14.3 | 2.16 | 33 | 37 |
As shown in the above table, since the calculated sample sizes for the second objective are less than that of the first objective (n=421), the larger sample size (n=421) was taken and used for this study.
Sampling techniques and procedures
A pre-study survey was conducted in the Nguenyyiel Refugee Camp to generate a sampling frame (ie, to identify families with adolescent girls). Accordingly, around 4100 households with adolescent girls were identified and recorded during the pre-study survey. Then, the 421 respondents in the Nguenyyiel Refugee Camp were chosen using a systematic random sampling technique. The sampling interval was calculated by dividing the number of households with adolescent girls in the Nguenyyiel Refugee Camp (N=4100) by the sample size (n=421), resulting in K=4100/421=9. As a result, every ninth household with an adolescent was chosen. In cases where a household had two or more adolescents, the lottery technique was employed to choose one adolescent girl who was interviewed.
Operational definitions
Adolescent pregnancy
In this study, adolescent pregnancy is defined as a current conception (pregnancy) occurring in a girl aged 10–19 (ie, before the age of 20), regardless of marital status.26
Communication on sexual and reproductive health issues
An adolescent girl was considered to have parent–adolescent communication on sexual and reproductive health (SRH) issues if she discussed with either of her parents at least one of the SRH issues such as menstrual cycle and fertile period and how one can get pregnant.27
Knowledge of modern contraceptive methods
Knowledge of modern contraceptive methods among the adolescent girls was measured based on the score or correctness of response to the seven modern contraceptive knowledge-tracing questions.
Adolescent girls who responded ‘Yes’ to the questions were considered to have ‘comprehensive knowledge, good knowledge and poor knowledge about contraceptive methods if they scored ≥5, 3–4 and ≤2, respectively.27
Data collection tools and procedures
The data was gathered by eight trained diploma nurses and two supervisors with a BSc degree in public health. A well-structured questionnaire was used in a face-to-face interviewer-administered data collection method. The questionnaire was adapted from different literature and pretested at sites other than the study area before the commencement of the actual data collection.14 24 28 It contained socio-demographic, family and individual-level characteristics, including SRH knowledge, modern contraceptive knowledge and other pregnancy-related characteristics. Pregnancy in adolescent girls was determined using urine human chorionic gonadotropin (HCG) test kits. Each study participant was asked before collecting a urine sample if she was pregnant or if the pregnancy was visible to the data collectors at the time of data collection (interviews). Urine samples were then collected from all study participants except those whose pregnancies had been confirmed.
Data quality control and analysis
The questionnaire was first prepared in English and then translated into the local language (Nuer). Then, it was translated back into English by a different language expert to verify its consistency. Data collectors and supervisors were provided a 2-day training on the importance and objective of the study.
Data collection tools, sampling methods, interviewing techniques and important precautions and procedures were to be followed while conducting the HCG pregnancy test. The questionnaire was pretested on 5% of the sample size in places other than the study area. The completeness and consistency of the data were checked by the supervisors on a daily basis. After that, the data was entered into EpiData software V.3.1 and exported to SPSS V.22. Frequencies and cross-tabulations were used to check for missed values. Descriptive analysis was done on socio-demographic, individual-level and related characteristics and presented using tables and graphs.
Bivariate and multivariate logistic regression analysis was done to identify factors associated with the outcome variable. Accordingly, variables with a p value<0.25 on bivariable logistic regression were taken as candidates for multivariate analysis. The goodness of fit for the final regression model was checked by the Hosmer-Lemeshow goodness of fit test at a p value of >0.05. On multivariate logistic regression analysis, variables with a p value of <0.05 at a 95% confidence level were declared significant. The adjusted OR (AOR) is used to measure the strength of the association.
Patient and public involvement
No patient and public involvement.
Results
Socio-demographic characteristics of respondents
A total of 414 adolescent girls (10–19 years) participated in this study, making the response rate as 98.3%. The mean age of the respondents was 16.8 years with ±1.52 SD. The majority of the respondents, 241 (58.2%), were late-stage adolescents (17–19 years), and more than one-third of the respondents, 164 (39.6%), were middle-stage adolescents (14–16 years), while 9 (2.2%) were in the early adolescence stage (10–13 years). Nearly three-fourths of the respondents, 309 (74.6%), were Protestants, while 57 (13.8%) and 32 (7.7%) were Seventh-Day Adventist and Church of God, respectively. More than half of the respondents, 221 (53.4%), had primary education and nearly one-third of respondents, 129 (31.1%), had no formal education. Three-fourths of the adolescent girls, 313 (75.6%) were single (not married) and 101 (24.4%) were married or ever-married. The majority of the married adolescents, 85 (84.2%), got married while they are in their middle-stage adolescence age (14–16 years); and one-fifth of the marriages, 21 (20.8%), were arranged marriages (table 2).
Table 2.
Socio-demographic characteristics of respondents (adolescent girls, N=414) in Nguenyyiel Refugee Camp, Gambella region, Southwest Ethiopia, September 2021
| Variable | Category | Frequency | Per cent |
| Age category by adolescence stages | Early adolescence (10–13 years) | 9 | 2.20 |
| Middle adolescence (14–16 years) | 164 | 39.6 | |
| Late adolescence (17–19 years) | 241 | 58.2 | |
| Religion | Protestant | 309 | 74.6 |
| Seventh-Day Adventist | 57 | 13.8 | |
| Church of God | 32 | 7.70 | |
| Catholic | 16 | 3.90 | |
| Ethnicity | Nuer | 414 | 100 |
| Educational status | Secondary and above | 64 | 15.5 |
| Primary education (grade 1–8) | 221 | 53.4 | |
| No formal education | 129 | 31.1 | |
| Marital status | Single (not married) | 313 | 75.6 |
| Married and living together | 79 | 19.1 | |
| Married and separated | 14 | 3.40 | |
| Divorced | 8 | 1.90 | |
| Age at marriage by age groups | Married before 15 years | 18 | 17.8 |
| Married between 15 and 19 years | 83 | 82.2 | |
| Age at marriage by adolescence stage | Early adolescence (10–13 years) | 1 | 0.90 |
| Middle adolescence (14–16 years) | 85 | 84.2 | |
| Late adolescence (17–19 years) | 15 | 14.9 | |
| Marriage arranged by parents | Yes | 21 | 20.8 |
| No | 80 | 79.2 |
Family related-characteristics of respondents
Only 126 (30.4%) of the study participants had communication with their parents on SRH issues, while more than two-thirds of adolescent girls (288, 69.6%) had no communication with their parents on the issues. Nearly half of the adolescents, 194 (46.9%), living with either of their biological parents (single parent). One-fourth of the adolescents, 104 (25.4%), living with none of their biological parents and less than one-fifth of the adolescents, 75 (18.1%), living with both of their biological parents. The mean family size in households of the respondents was 6.32 people, with ±1.86 SD and a range of 2–13. The majority of the adolescent girls, 351 (84.8%), living in households with five or more people and three-fourths (75%) of them living in large families of seven or more people (table 3).
Table 3.
Familial-level characteristics of respondents in Nguenyyiel Refugee Camp Gambella region, Southwest Ethiopia, September 2021
| Variable | Category | Frequency | Per cent |
| Parent–adolescent communication on SRH issues | Yes | 126 | 30.4 |
| No | 288 | 69.6 | |
| Household living arrangement | Living with both biological parents | 75 | 18.1 |
| Living with either of the biological parents | 194 | 46.9 | |
| Living with none of the biological parent | 104 | 25.4 | |
| Married (living together with husband) | 40 | 9.60 | |
| Family size | Small family (four persons and below) | 63 | 15.2 |
| Large family (five and more persons) | 351 | 84.8 |
SRH, sexual and reproductive health.
Respondents knowledge about contraceptive methods among
More than one-third of the adolescent girls, 167 (40.3%), had poor knowledge of modern contraceptive methods; 118 (28.5%) and 129 (31.2%), respectively, had good and comprehensive knowledge of modern contraceptives. The majority of the respondents (326, 78.7%) knew or ever heard of condom, 305 (73.7%) knew or ever heard of oral contraceptive pills (OCP), more than half (218, 52.7%) knew or heard about injectables (Depo-Provera and Norethisterone enanthate (NET-EN)) and 154 (37.2%) heard about implants (table 4).
Table 4.
Knowledge of modern contraceptive methods among adolescent girls (N=414) in Nguenyyiel Refugee Camp, Gambella region, Southwest Ethiopia, September 2021
| Variable | Category | Frequency (N=414) | Per cent |
| Knew or ever heard of OCP | Yes | 305 | 73.7 |
| Knew or ever heard of injectable | Yes | 218 | 52.7 |
| Knew or ever heard of a condom | Yes | 326 | 78.7 |
| Knew or ever heard of implants | Yes | 154 | 37.2 |
| Knew or ever heard of SDM | Yes | 126 | 30.4 |
| Knew or ever heard of IUCD | Yes | 126 | 30.4 |
| Knew or ever heard of sterilisation | Yes | 51 | 12.3 |
| Overall knowledge about contraceptive methods | Comprehensive knowledge | 129 | 31.2 |
| Good knowledge | 118 | 28.5 | |
| Poor knowledge | 167 | 40.3 |
IUCD, intrauterine contraceptive device; OCP, oral contraceptive pills; SDM, Standard Day Method.
SRH characteristics (behaviours) of respondents
The mean age at menarche (first menstrual bleeding) was 12.5 years with ±1.99 SD. Menarche in almost all respondents, 403 (99.5%), occurred between 10 and 14 years of age. The mean age at first sexual intercourse among respondents was 14.03 years, with ±3.88 SD. Almost half of the adolescent girls, 193 (49.6%), were sexually active before 15 years; two-thirds of the respondents, 257 (66.0%), were sexually active in middle-stage adolescence (14–16 years); and 338 (86.9%) of the adolescents had sexual intercourse before 18 years. The contraceptive prevalence rate among adolescent girls was 27 (6.5%). Out of these, 23 (5.6%) of the adolescents had ever used injectables (Depo-Provera and/or NET-EN); 26 (6.3%) used condoms, and 27 (6.5%) of the respondents used OCPs (table 5).
Table 5.
Sexual behaviour (characteristics) of respondents (adolescent girls), (N=414) in Nguenyyiel Refugee Camp, Gambella region, Southwest Ethiopia, September 2021
| Variable | Category | Frequency | Per cent |
| Adolescent girl had menarche | Yes (menarche occurred) | 405 | 97.8 |
| No (menarche not occurred) | 9 | 2.20 | |
| Sexual practice (N=414) | Yes (ever had sexual intercourse) | 389 | 94.0 |
| No (has not ever had sex) | 25 | 6.00 | |
| Age at sexual practice by age groups (N=389) | Sexually active before 15 years | 193 | 49.6 |
| Sexually active at 15–19 years | 196 | 50.4 | |
| Age at sexual intercourse stages (N=389) | Early adolescence (10–13 years) | 64 | 16.5 |
| Middle adolescence (14–16 years) | 257 | 66.0 | |
| Late adolescence (17–19 years) | 68 | 17.5 | |
| Early sexual initiation (debut) (N=389) | Yes | 338 | 86.9 |
| No | 51 | 13.1 | |
| Knowledge about contraceptive methods | Comprehensive knowledge | 129 | 31.2 |
| Good knowledge | 118 | 28.5 | |
| Poor knowledge | 167 | 40.3 | |
| Total contraceptive use | 88 | 21.26 | |
| Modern contraceptive use (N=414) | 86 | 20.77 | |
| OCP (N=414) | 27 | 6.50 | |
| Injectable (N=414) | 23 | 5.60 | |
| Condom (N=414) | 26 | 6.30 | |
| Implant (N=414) | 3 | 0.70 | |
| SDM (N=414) | 2 | 0.50 | |
| IUCD (N=414) | 5 | 1.20 | |
IUCD, intra uterine contraceptive device; N, sample size (no of response); OCP, oral contraceptive pills; SDM, Standard Day Method.
Prevalence of adolescent pregnancy in Nguenyyiel Refugee Camp, Gambella region
The prevalence of pregnancy among adolescent girls in the Nguenyyiel Refugee Camp was 21.7% (95% CI: 17.6 to 25.6). More than half of the pregnant girls (51.1%) were middle-stage adolescents (14–16 years) and 48.9% were late-stage adolescents (17–19 years old).
Factors associated with pregnancy among adolescent
Age (17–19 years), educational status (no formal education and primary education) and family structure (living with either biological parent and living with neither biological parent) were statistically significantly associated with pregnancy among adolescent girls (10–19 years) in Nguenyyiel Refugee Camp.
The odds of pregnancy among late-stage adolescent girls (17–19 years) was 2.8 times higher compared with adolescents 10–16 years of age (AOR: 2.8; 95% CI: 1.6 to 5.1). Adolescent girls with primary education (grade 1–8) were 7.7 times more likely to become pregnant compared with those with secondary and above education (AOR: 7.7; 95% CI: 3.55 to 16.7). Similarly, the odds of pregnancy among adolescent girls with no formal education were 3.4 times higher compared with girls who attended secondary school and above (AOR: 3.4; 95% CI: 1.6 to 7.4).
Odds of pregnancy among adolescent girls living with none of their biological parents were two times more likely to be pregnant compared with adolescents living with both biological parents (AOR: 2.1; 95% CI: 1.02 to 4.5). Likewise, the odds of pregnancy among adolescent girls living with either of their biological parents was 3.7 times higher compared with girls living with both of their biological parents (AOR: 3.7; 95% CI: 1.8 to 7.8) (table 6).
Table 6.
Factors associated with pregnancy among adolescent girls (10–19 years) in Nguenyyiel Refugee Camp, Gambella region, Southwest Ethiopia, September 2021
| Variable | Categories | Pregnancy (status) | AOR (95% CI) | P value | |
| Yes (HCG positive) | No (HCG negative) | ||||
| N (%) | N (%) | ||||
| Age (stages of adolescence) | 10–16 years | 46 (51.1) | 127 (39.2) | 1 | |
| 17–19 years | 44 (48.9) | 197 (60.8) | 2.79 (1.55 to 5.05) | 0.001 | |
| Educational status | Secondary and above | 26 (28.9) | 38 (11.7) | 1 | |
| Primary education (grade 1–8) | 26 (28.9) | 195 (60.2) | 7.69 (3.55 to 16.68) | 0.001 | |
| No formal education | 38 (42.2) | 91 (28.1) | 3.42 (1.59 to 7.36) | 0.002 | |
| Sexual experience | Sexually active at 15–19 year-old | 54 (60.0) | 142 (47.5) | 1 | |
| Sexually active before 15 years of age | 36 (40.0) | 157 (52.5) | 1.39 (0.76 to 2.54) | 0.282 | |
| Knowledge about contraceptive | Comprehensive knowledge | 37 (41.1) | 92 (28.4) | 1 | |
| Good knowledge | 20 (22.2) | 98 (30.2) | 1.29 (0.62 to 2.69) | 0.496 | |
| Poor knowledge | 33 (36.7) | 134 (41.4) | 1.73 (0.90 to 3.32) | 0.100 | |
| Early sexual debut (before 18 years) |
No | 6 (11.8) | 84 (24.9) | 1 | |
| Yes | 45 (88.2) | 254 (75.1) | 0.41 (0.14 to 1.17) | 0.096 | |
| Parent–adolescent communication on (SRH) | Yes | 40 (44.4) | 86 (26.5) | 1 | |
| No | 50 (55.6) | 238 (73.5) | 1.37 (0.73 to 2.54) | 0.326 | |
| Household living arrangement | Living with both biological parents | 29 (32.2) | 46 (14.2) | 1 | |
| Living with either of biological parent | 23 (25.6) | 171 (52.8) | 3.71 (1.76 to 7.81) | 0.001 | |
| Living with none of biological parents | 25 (27.8) | 80 (24.7) | 2.14 (1.02 to 4.49) | 0.043 | |
| Married and living together with husband | 13 (14.4) | 27 (8.30) | 2.04 (0.81 to 5.14) | 0.132 | |
AOR, adjusted OR; HCG, human chorionic gonadotropin; SRH, sexually transmitted infections.
Discussions
This study showed that the prevalence of pregnancy among adolescent girls (10–19 years) in the Nguenyyiel Refugee Camp was high. This finding is consistent with findings of similar studies conducted among South Sudanese refugees (10–19 years) in the Bidibidi Refugee Settlement, northern Uganda (25%).4 Eritrean refugees in the northern Tigray region, Ethiopia (28.4%),29 Somalian refugees in Kobe refugee camp of Somali region, Ethiopia (26.3%)30 and among refugees in Thailand–Myanmar border settlement, Southeast Asia.31
The observed similarity could be due to similar socio-demographic and socioeconomic characteristics in humanitarian settings as well as similarity in the vulnerability of adolescent girls to SRH problems in humanitarian settings.
The findings of this study are higher than the findings of similar studies among adolescent girls in non-emergency (non-humanitarian) settings: in Africa (a pooled prevalence of 18.8%),32 Arba Minch town, Southern Ethiopia (7.7%),33 Gambella region of Ethiopia (16.2%) and India (10%).34
The possible reasons for the difference in the prevalence of adolescent pregnancy in humanitarian settings compared with non-emergency contexts could be due to differences in settings. That is, adolescents in humanitarian settings are more vulnerable to poor socioeconomic status following the disruption of family structure, loss of father or mother, or both, during conflict or disaster.
This in turn leads adolescents to hopelessness, being prone to gender-based violence and early marriage. In addition to that, basic reproductive healthcare services like family planning, including health information communication on reproductive issues, are less available in humanitarian settings than in non-humanitarian settings.
However, the finding of this study is lower than that of studies conducted in: Nigeria (45.4%),35 Eastern Ethiopia, (30.2%),32 East Africa (pooled prevalence of 54.6%),36 Uganda (35.8%)37 and Northeast Ethiopia (28.6%).38 The possible explanation for this discrepancy could be difference in socio-demographic, socioeconomic, larger sample size and inclusion terminated pregnancy in the case of East Africa pooled prevalence.
This study showed that pregnancy among refugee adolescents was associated with increasing age; the odds of pregnancy among late-stage adolescent girls (17–19 years) was higher than girls in the early and middle stages of adolescence (10–16 years). This is in line with studies conducted in Eastern Ethiopia, East Africa, Northeast Ethiopia and Kenya.32 36 38 39 This could be due to the fact that as age increases, teenagers will have more exposure to sex and their chance of getting married also increase.
Adolescent girls with primary education (grade 1–8) were more likely to become pregnant compared with their counterparts who attended secondary and above. Likewise, the odds of pregnancy among adolescents with no formal education was high compared with girls who attained secondary and above.
This is similar with finding of studies conducted in Eastern Ethiopia,32 South East Nigeria,35 a systematic review and meta-analysis in Africa,40 a multilevel analysis in five East African countries.41 The possible justification could be adolescent girls with lower educational attainment lack appropriate information regarding the consequence of unsafe sexual practice as well as the means to avoid unwanted pregnancy.
This study showed that household living arrangements (family structure) were associated with adolescent pregnancy: Adolescent girls living with none of their biological parents were more likely to be pregnant compared with adolescents living with both biological parents (ie, living in nuclear families). The odds of pregnancy among adolescent girls living with either of their biological parents (single parent families) higher compared with girls living with both of their biological parents. This is similar to the findings of studies conducted in Southern Ethiopia,33 Eastern Ethiopia32 and Northeast Ethiopia.38 This could be because adolescent girls who did not live with one or both of their biological parents lack parental support and guidance. Adolescent girls might have lost one or both of their biological parents during the conflict. Adolescents in this situation may feel helpless and hopeless and choose to get married or engage in unsafe sex to secure their survival.
Finally, even though the authors have tried to maximise the quality of this study, it is important to note that using HCG test to diagnose pregnancy might undermine the true figure of prevalence of adolescent pregnancy as the HCG test cannot detect a pregnancy that is less than a week old.
Similarly, since sexuality is a sensitive issue, respondents might not disclose their true behaviour. This results in social desirability bias. Therefore, the authors have forwarded the following recommendations for future researchers to overcome the limitations committed in this study.
Conclusions
This study showed a high prevalence of pregnancy among refugee adolescent girls (10–19 years) in the Nguenyyiel Refugee Camp, Gambella region, Ethiopia. The significant factors associated with adolescent pregnancy were: age (17–19 years), educational status (no formal education and primary education) and household living arrangement or family structure: living with none of the biological parents and living with either of the biological parents.
Recommendation
Healthcare provider
Health workers in the camps should work to strengthen targeted adolescent sexual health education and information, giving special attention to the uneducated, those living without biological family and late-stage adolescents.
Humanitarian organisations (MS, ARRA, UNHCR, etc)
Strengthen adolescent–youth-friendly services and adolescent girls’ empowerment in refugee camps.
Strengthen health education and schooling for refugee adolescent girls.
Strengthen comprehensive sexuality education programmes at schools in refugee camps.
Adolescent girls who have lost their parents should be given special attention.
Regional health bureaus, zonal and other health offices
Strengthening intervention programmes aimed at preventing pregnancy among refugee adolescents.
Prepare programmes and strategies (approaches) to support refugee adolescent girls living with none or either of their biological parents.
Researchers
Future researchers should focus on exploring the underlying sociocultural conditions through a mixed approach (qualitative and quantitative study).
Important points that are not addressed in this study, like the level of unmet need for family planning and the prevalence of unwanted pregnancy, are among the issues that seek the attention of future researchers.
Supplementary Material
Acknowledgments
We would like to acknowledge Mettu University for financial support. We are also grateful to the data collectors and respondents who took part in this study.
Footnotes
Twitter: @KoangBolLew, @AbdiioromoFree
Contributors: KNB: made a significant contribution to the conception, study design, execution and acquisition of data, analysis and interpretation and has agreed on the journal to which the article has been submitted. EN: took part in study design, execution, drafting, revising and critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted. AGG: contributed to the planning, acquisition of data, analysis and interpretation, revising and critically reviewing the article, writing the report and agreeing on the journal to which the article has been submitted. KNB is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographical or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All the data used or mentioned in this research are available.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and was approved by Research Ethical Committee of Mettu University, Ref: RPG/03/2013. Participants gave informed consent to participate in the study before taking part.
References
- 1.Adolescent pregnancy . Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy [Accessed 05 May 2022].
- 2.Kawakita T, Wilson K, Grantz KL, et al. Adverse maternal and neonatal outcomes in adolescent pregnancy. J Pediatr Adolesc Gynecol 2016;29:130–6. 10.1016/j.jpag.2015.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen PH, Sanghvi T, Tran LM, et al. The nutrition and health risks faced by pregnant adolescents: insights from a cross-sectional study in Bangladesh. PLoS One 2017;12:e0178878–13. 10.1371/journal.pone.0178878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakesiima R, Cleeve A, Larsson E, et al. Modern contraceptive use among female refugee adolescents in northern Uganda: prevalence and associated factors. Reprod Health 2020;17:1–9. 10.1186/s12978-020-00921-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nove A, Matthews Z, Neal S, et al. Maternal mortality in adolescents compared with women of other ages: evidence from 144 countries. Lancet Glob Health 2014;2:e155–64. 10.1016/S2214-109X(13)70179-7 [DOI] [PubMed] [Google Scholar]
- 6.Parker AL, Parker DM, Zan BN, et al. Trends and birth outcomes in adolescent refugees and migrants on the Thailand-Myanmar border, 1986-2016: an observational study. Wellcome Open Res 2018;3:62. 10.12688/wellcomeopenres.14613.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang T, Wang H, Wang X, et al. The adverse maternal and perinatal outcomes of adolescent pregnancy: a cross sectional study in Hebei, China. BMC Pregnancy Childbirth 2020;20:1–10. 10.1186/s12884-020-03022-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Regional Office for South-East Asia . Adolescent pregnancy situation in south-east Asia region. In: Media Cent, 2015: 1–194. [Google Scholar]
- 9.Johnson W, Moore SE. Adolescent pregnancy, nutrition, and health outcomes in low- and middle-income countries: what we know and what we don't know. BJOG 2016;123:1589–92. 10.1111/1471-0528.13782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Indarti J, Al Fattah AN, Dewi Z, et al. Teenage pregnancy: obstetric and perinatal outcome in a tertiary centre in Indonesia. Obstet Gynecol Int 2020;2020:2787602. 10.1155/2020/2787602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UNICEF . Adolescent health and well-being. Available: https://www.unicef.org/health/adolescent-health-and-well-being [Accessed 03 Jan 2022].
- 12.Adolescent pregnancy. Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy [Accessed 03 Jan 2022].
- 13.Mekonnen T, Dune T, Perz J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: a systematic scoping review. BMC Pregnancy Childbirth 2019;19:366. 10.1186/s12884-019-2501-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.EDHS 2016 Team . Ethiopian demographic and health survey. Report; 2016.
- 15.Morris JL, Rushwan H. Adolescent sexual and reproductive health: the global challenges. Int J Gynaecol Obstet 2015;131 Suppl 1:S40–2. 10.1016/j.ijgo.2015.02.006 [DOI] [PubMed] [Google Scholar]
- 16.Kerner B, Manohar S, Mazzacurati C, et al. Adolescent sexual and reproductive health in humanitarian settings. Forced Migration Review, 2012: 21–2. http://www.fmreview.org/young-and-out-of-place [Google Scholar]
- 17.Neal S, Mahendra S, Bose K, et al. The causes of maternal mortality in adolescents in low and middle income countries: a systematic review of the literature. BMC Pregnancy Childbirth 2016;16:1–18. 10.1186/s12884-016-1120-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United Nations Population Fund . Adolescent pregnancy. Available: https://www.unfpa.org/adolescent-pregnancy [Accessed 03 Jan 2022].
- 19.Tadesse A, Geda A. Why syphilis infection is high among pregnant women in refugee camps? A case in Ethiopia. Int J Womens Health 2022;14:481–9. 10.2147/IJWH.S354045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qanche Q, Wondimu W, Asefa A, et al. Factors contributing to high HIV prevalence in Majang zone, Southwest Ethiopia: what lies beneath the tip of the iceberg? J Multidiscip Healthc 2021;14:3273–83. 10.2147/JMDH.S331708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nigussie T, Mamo Y, Qanche Q, et al. HIV preventive behaviors and associated factors among gold mining workers in Dima district, Southwest Ethiopia, 2019: community-based cross-sectional study. Biomed Res Int 2021;2021:4797590. 10.1155/2021/4797590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kibret GD, Ferede A, Leshargie CT, et al. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty 2019;8:1–9. 10.1186/s40249-019-0594-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Central Statistical Agency Addis Ababa E. UNICEF Ethiopia . Ethiopia demographic and health survey. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016: 249. [Google Scholar]
- 24.Ethiopian Public Health Institute (EPHI), ICF . Ethiopia mini demographic and health survey 2019: final report; 2021: 1–207. https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf
- 25.UNHCR . Nguenyyiel refugee cAMP, 2020. Available: https://reliefweb.int/sites/reliefweb.int/files/resources/77009.pdf
- 26.Birhanu BE, Kebede DL, Kahsay AB, et al. Predictors of teenage pregnancy in Ethiopia: a multilevel analysis. BMC Public Health 2019;19:1–10. 10.1186/s12889-019-6845-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yimer AS, Modiba LM. Modern contraceptive methods knowledge and practice among blind and deaf women in Ethiopia. A cross-sectional survey. BMC Womens Health 2019;19:1–13. 10.1186/s12905-019-0850-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen PH, Sanghvi T, Tran LM, et al. The nutrition and health risks faced by pregnant adolescents: insights from a cross-sectional study in Bangladesh. PLoS One 2017;12:e0178878. 10.1371/journal.pone.0178878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gebrecherkos K, Gebremariam B, Gebeyehu A. Unmet need for modern contraception and associated factors among reproductive age group women in Eritrean refugee camps, Tigray, North Ethiopia: a cross-sectional study 11 medical and health sciences 1117 public health and health services 11 medical and H. BMC Res Notes 2018;11:1–6. 10.1186/s13104-018-3956-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elnakib S, Hunersen K, Metzler J, et al. Child marriage among Somali refugees in Ethiopia: a cross sectional survey of adolescent girls and adult women. BMC Public Health 2021;21:1–12. 10.1186/s12889-021-11080-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker AL, Parker DM, Zan BN, et al. Trends and birth outcomes in adolescent refugees and migrants on the Thailand-Myanmar border, 1986-2016: an observational study. Wellcome Open Res 2018;3:62. 10.12688/wellcomeopenres.14613.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mezmur H, Assefa N, Alemayehu T. Teenage pregnancy and its associated factors in eastern Ethiopia: a community-based study. Int J Womens Health 2021;13:267–78. 10.2147/IJWH.S287715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathewos S, Mekuria A. Teenage pregnancy and its associated factors among school adolescents of Arba Minch town, southern Ethiopia. Ethiop J Health Sci 2018;28:287–98. 10.4314/ejhs.v28i3.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahavarkar SH, Madhu CK, Mule VD. A comparative study of teenage pregnancy. J Obstet Gynaecol 2008;28:604–7. 10.1080/01443610802281831 [DOI] [PubMed] [Google Scholar]
- 35.Uwaezuoke AI, Uzochukwu BS, Nwagbo DF. Determinants of teenage pregnancy in rural communities of Abia state, South East Nigeria. Int J Med Heal Dev 2004;9:28–33. 10.4314/JCM.V9I1.10471 [DOI] [Google Scholar]
- 36.Worku MG, Tessema ZT, Teshale AB, et al. Prevalence and associated factors of adolescent pregnancy (15–19 years) in East Africa: a multilevel analysis. BMC Pregnancy Childbirth 2021;21:1–8. 10.1186/s12884-021-03713-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manzi F, Ogwang J, Akankwatsa A, et al. Factors associated with teenage pregnancy and its effects in Kibuku town Council, Kibuku district, eastern Uganda: a cross sectional study. Prim Health Care 2018;08. 10.4172/2167-1079.1000298 [DOI] [Google Scholar]
- 38.Ayanaw Habitu Y, Yalew A, Azale Bisetegn T. Prevalence and factors associated with teenage pregnancy, northeast Ethiopia, 2017: a cross-sectional study. J Pregnancy 2018;2018:1–7. 10.1155/2018/1714527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Omoro T, Gray SC, Otieno G, et al. Teen pregnancy in rural Western Kenya: a public health issue. Int J Adolesc Youth 2017;3:1–10. 10.1080/02673843.2017.1402794 [DOI] [Google Scholar]
- 40.Kassa GM, Arowojolu AO, Odukogbe AA, et al. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and meta-analysis. Reprod Health 2018;15:195. 10.1186/s12978-018-0640-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wado YD, Sully EA, Mumah JN. Pregnancy and early motherhood among adolescents in five East African countries: a multi-level analysis of risk and protective factors. BMC Pregnancy Childbirth 2019;19:1–11. 10.1186/s12884-019-2204-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kefale B, Yalew M, Damtie Y, et al. A multilevel analysis of factors associated with teenage pregnancy in Ethiopia. Int J Womens Health 2020;12:785–93. 10.2147/IJWH.S265201 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data used or mentioned in this research are available.