Abstract
OBJECTIVE
Vaccination is the primary way to mitigate the COVID-19 pandemic. Vaccine hesitancy and refusal are one of the most important challenges against to reach herd immunity. The aim of this study is to examine the reasons for not getting vaccinated and the attitudes toward vaccines by people in Turkiye, who were not vaccinated, even though a COVID-19 vaccine was available for them.
METHODS
This cross-sectional study is conducted in Eyupsultan district of Istanbul. The study population is 12,540. A questionnaire consisted of three sections as sociodemographic characteristics, attitudes toward COVID-19 vaccines, and Vaccination Attitudes Examination (VAX) scale was used. Among the sample size, participation rate is 69.4%.
RESULTS
About 50.2% of the participants (n=259) are male, 80.3% are married, 13.1% are university graduates, and 44.0% are working in a job. About 32.8% of the participants have COVID-19 history. About 34.4% of the participants stated that they would be vaccinated against COVID-19. Although those who define themselves as vaccine refuser are 5.4%, those who still refuse to be vaccinated for COVID-19 are 20.1%. In addition to this, those who are hesitant about COVID-19 vaccines are 45.6%. The most frequently preferred vaccine is comirnaty (41.7%). About 13.1% of the participants stated that “if we had a domestic COVID-19 vaccine, I would have it.” The most common sources of information about vaccines are television with 78.4%, and health workers are in the last place with 14.7%. “Concerns about side effects” are the most frequently cited (85.9%) reason for not vaccinating. The mean score of the VAX scale is 42.34±10.93, and the “mistrust of vaccine benefit” is higher among primary school graduates than other educational status groups (p=0.001).
CONCLUSION
Anti-vaccination attitudes have increased with the COVID-19 vaccines during pandemic. Our study is valuable in terms of examining the reasons of individuals who have not gotten vaccinated even though they had no access problems. Prominent concerns of the population should be approached seriously. Otherwise, vaccine hesitancy can be a decisive factor that would prevent the success of the struggle against pandemic.
Keywords: Anti-vaccination attitudes examination, COVID-19, herd immunity, vaccination attitudes examination scale, vaccine hesitancy
Highlight key points
Vaccine hesitancy and refusal, which has become widespread in recent years, has increased even more COVID-19 vaccines during the pandemic.
Even those who are considering getting vaccinated have many concerns, especially about the side effects of vaccines.
A significant amount of people living in regions where access to vaccines is fairly easy is not willing to get vaccinated against COVID-19. Given the fact that people from less developed parts of the world have been suffering from the inequalities that prevent their access to vaccines, those anti-vaccination attitudes should be examined delicately.
Vaccination is considered as one of the “10 great public health achievements” and the most effective protection method from infectious diseases [1]. The occurrence of several diseases with their adverse effects has been prevented by vaccines. Despite many successful results, hesitations against vaccines have also emerged since their discovery. Although vaccine hesitancy and refusal had an undulant course in the past, it has been rising in recent years [2]. Vaccine hesitancy is identified by the World Health Organization (WHO) as one of the 10 threats to global health [3].
It is well known that the herd immunity required to mitigate the COVID-19 pandemic can only be achieved with vaccines [4]. While the uncertainties about both the virus and the disease continue, vaccine development studies have swiftly started. Seven different vaccines were approved by the WHO Emergency Use Listing Procedure, and 22 vaccines were approved by at least one country, and in use as of August 20, 2021 [5]. It is observed that in countries where partial or full vaccination rates increased, incidence, hospitalization, and death rates of COVID-19 have decreased [6, 7]. However, some hesitations have arisen about COVID-19 vaccines as it was expected. Most important reasons of hesitancy were unfamiliarity about the messenger RNA vaccine technology that was used for the 1st time and the fact that vaccines were developed in a much shorter period than previous ones [8]. Besides the access problems to vaccines in many regions of the world, vaccine hesitancy seems to be a significant barrier in front of the global herd immunity. Even though the safety and efficacy of vaccines are demonstrated with new studies, the resistance of anti-VAX movements is still a critical problem in the fight against the pandemic [9–11].
Studies regarding attitudes toward COVID-19 vaccination show that vaccine hesitancy varies between 13.9% and 71.3%, depending on participants’ characteristics [12–16]. Side effects and inefficacy, need for multiple doses, distrust to industry, and the violation of body integrity are some of the prominent reasons of negative attitudes and hesitations about COVID-19 vaccines [17, 18].
In Turkiye, the scope of the COVID-19 vaccinations, which were first introduced for healthcare professionals in January 14, 2021, had rapidly expanded with the prioritization of risk groups [19]. At the beginning, only the CoronaVac was administered and in the following months, the comirnaty was also provided. As of August 19, 2021, 27.5% of the population over 18 years old have not yet been vaccinated despite being in the eligible group to be vaccinated [20].
The aim of this study is to examine the reasons for not getting vaccinated and the attitudes toward vaccines by people in Turkiye, who were not vaccinated, even though a COVID-19 vaccine was available for them.
MATERIALS AND METHODS
This cross-sectional study is conducted during June 21–28, 2021, in Eyupsultan district of Istanbul. The study population (n=12.540) is the people who meet the inclusion criteria as residing in Eyupsultan district, to be unvaccinated by any COVID-19 vaccine, having a registered phone number in the Public Health Management System, and being over age of 50 who was the latest group added to the vaccination by June 1, 2021. Sample size needed at 95% confidence level with 5% sampling error is calculated as 373. Considering the reasons such as refusal to participate, wrong phone number, and not answering the call, 505 people are selected from the population phone number list by simple random sampling.
The official permission for the study is obtained from Ministry of Health COVID-19 Scientific Research Commission. The study plan is approved by Non-Interventional Clinical Research Ethics Committee of Istanbul Medipol University (date: June 17, 2021, number: 674). The study was carried out in accordance with the Helsinki Declaration. Participation to the study was on a voluntary basis following the informed consent.
Data were collected during phone interviews by the researchers. A questionnaire consisted of three sections and 38 questions was used to collect the data. The first section included 14 questions regarding sociodemographic characteristics such as age, gender, and educational status. The second section had 12 questions about specific attitudes toward COVID-19 vaccines. In the third part, the Vaccination Attitudes Examination (VAX) scale was used to evaluate the general attitude toward vaccines. VAX scale was developed by Martin and Petrie [21] for adults. It is designed 6-point Likert scale consisting of 12 items and four subscales as mistrust of vaccine benefit (1–3), worries about unforeseen future effects (4–6), concerns about commercial profiteering (7–9), and preference for natural immunity (10–12). Total scores range between 12 and 72 and higher scores mean stronger anti-vaccination attitudes. Turkish version of the scale was prepared and found to be valid and reliable by Yildiz et al. [22].
Among the sample group of 505 individuals, 74 (14.6%) had a wrong registered phone number, 95 (18.8%) were called 3 times on separate days but could not be reached, 77 (15.2%) refused answer to questionnaire, and complete data were collected from 259 individuals (participation rate: 51.3%, Fig. 1).
Figure 1.
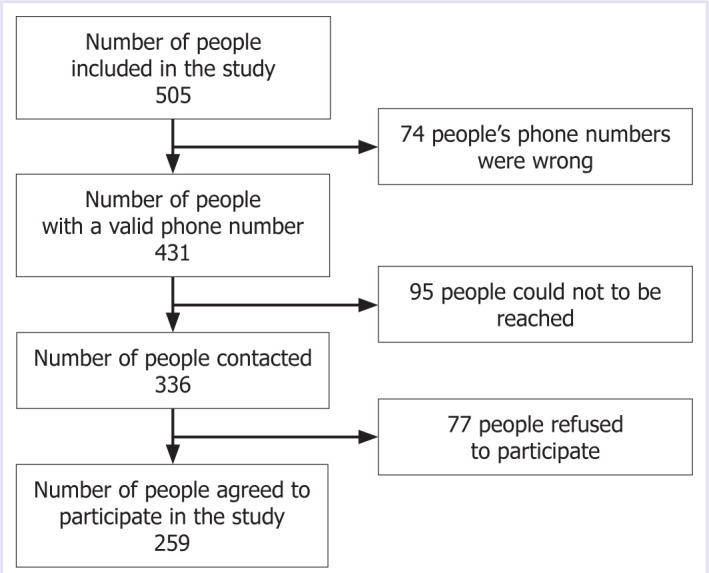
Flowchart of the study sampling method.
Statistical Analysis
Statistical analysis is performed using SPSS 23.0 (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). The descriptive statistics were summarized as number, frequency, percentage, mean, and standard deviation. ANOVA analysis was used for group comparisons. Statistically significant level was accepted as p<0.05.
RESULTS
The descriptive characteristics and vaccination preferences of the participants are given in Table 1. About 50.2% of the study group are male, 13.1% are university graduates, 80.3% are married, 92.3% have children, 56.0% are not working, 52.9% have at least one health problem, and 32.8% have COVID-19 history. The mean age is 56.16±5.24.
Table 1.
Descriptive characteristics, vaccination history, intentions, and preferences of participants
| % | |
|---|---|
| Gender | |
| Male | 49.8 |
| Female | 50.2 |
| Educational status | |
| Primary-secondary school | 59.1 |
| High school | 27.8 |
| University | 13.1 |
| Marital status | |
| Married | 80.3 |
| Others | 19.7 |
| Having a child | |
| Yes | 92.3 |
| No | 7.7 |
| Working status | |
| Working | 44.0 |
| Not working | 56.0 |
| Presence of a health problem | |
| Yes | 52.1 |
| No | 47.9 |
| COVID-19 history | |
| Yes | 32.8 |
| No | 62.2 |
| Not sure | 5.0 |
| Any vaccination history | |
| Yes | 78.0 |
| No | 12.7 |
| Not sure | 9.3 |
| Intention to vaccinate against COVID-19 | |
| Will vaccinate | 34.4 |
| Hesitant | 45.6 |
| Refuser | 20.1 |
| COVID-19 vaccine preferences | |
| Comirnaty | 41.7 |
| CoronaVac | 20.8 |
| Domestic vaccine | 13.1 |
| Does not matter | 4.2 |
| Vaccine refusal | |
| Yes | 5.4 |
| No | 76.1 |
| Not sure | 18.5 |
| Total | 100.0 |
| Information sources about vaccines* | |
| Television | 78.4 |
| Social media | 35.1 |
| Internet | 27.0 |
| Friends or relatives | 23.6 |
| Health care workers | 14.7 |
: Since more than 1 option can be chosen, the total exceeds 100.0%.
Answers given to the questions about past vaccination experience indicate that 78.0% of the study group have a vaccination history and 20.1% of them stated that they will not be vaccinated against COVID-19. Almost half of the group (45.6%) are hesitant about COVID-19 vaccination and only 5.4% are vaccine refusers. The most frequently preferred vaccine is comirnaty (41.7%). The most common information source about vaccines is television with 78.4%, while health care workers are in the last rank with 14.7%.
In Table 2, the reasons for not having intention for the COVID-19 vaccination are given for those who are hesitant or will not vaccinate. Concerns about side effects are the most frequent reason (85.9%) of hesitancy and refusal about COVID-19 vaccination. Shortness of vaccine production period is the second (45.3%) and waiting for others to be vaccinated (39.4%) is the third reason. This is followed by distrust of vaccine producer companies, absence of domestic vaccines, and wrong beliefs about vaccines.
Table 2.
Reasons of hesitancy or not vaccinating for COVID-19 (n=170)*
| %** | |
|---|---|
| Concerns about side effects of vaccines | 85.9 |
| Very short discovery period of vaccines | 45.3 |
| Preferring to have others vaccinated first | 39.4 |
| Distrust of companies producing vaccines | 37.6 |
| No domestic vaccine yet | 28.2 |
| Not to believe in vaccine protection | 26.5 |
| Believing that vaccines contain harmful ingredients | 25.9 |
| Preferring natural immunity instead of vaccines | 18.8 |
| Preferring to take other measures instead of vaccines | 18.2 |
| Not to believe COVID-19 as a serious illness | 11.8 |
| Having immunity due to getting COVID-19 | 10.0 |
| Possibility of COVID-19 infection transmission | |
| from the vaccine itself | 9.4 |
| History of adverse reactions to vaccines | 9.4 |
| Recommendations by people not to have the | |
| COVID-19 vaccine | 8.2 |
| Not to believe COVID-19 as a real disease | 5.9 |
| Needle phobia | 5.3 |
| Recommendation of health care workers not to | |
| have the vaccine | 1.2 |
| Total |
: Except those who will vaccinate; **: Since more than 1 option can be chosen, the total exceeds 100.0%.
Table 3 presents the distribution of participants’ attitudes toward COVID-19 vaccines according to their vaccination intentions. There is a statistically significant difference between the groups for all attitudes except A3 (p<0.001 in all comparisons). The proportion of “yes/not sure” answers of refusers is significantly higher than others for A1, A2, A4, A5, A8, A9, and A10 while proportion of “yes/not sure” answers is higher among hesitant individuals for A6, and “yes/not sure” answers of refusers is lower for A7.
Table 3.
Distribution of participants’ attitudes toward the COVID-19 vaccine in terms of vaccination intentions
| Intentions to vaccinate against COVID-19 | Will vaccinate (n=89) % | Hesitant (n=118) % | Refusers (n=52) % | p |
|---|---|---|---|---|
| A1. I do not believe that COVID-19 vaccines will protect me from the disease | <0.001 | |||
| Yes/not sure | 19.1 | 66.9 | 92.3 | |
| No | 80.9 | 33.1 | 7.7 | |
| A2. I do not believe that vaccines will be effective to mitigate the pandemic | <0.001 | |||
| Yes/not sure | 19.1 | 56.8 | 84.6 | |
| No | 80.9 | 43.2 | 15.4 | |
| A3. I do not think having COVID-19 as a risk, as the symptoms of the disease are mild | 0.251 | |||
| Yes/not sure | 30.3 | 35.6 | 44.2 | |
| No | 69.7 | 64.4 | 55.8 | |
| A4. I’d rather be immune by having COVID-19 than get vaccinated | <0.001 | |||
| Yes/not sure | 21.3 | 40.7 | 61.5 | |
| No | 78.7 | 59.3 | 38.5 | |
| A5. I am concerned about the side effects of the COVID-19 vaccines | <0.001 | |||
| Yes/not sure | 73.0 | 97.5 | 100.0 | |
| No | 27.0 | 2.5 | 0 (0.0) | |
| A6. Before I get the COVID-19 vaccine, I want to see the effects on other people first | <0.001 | |||
| Yes/not sure | 52.8 | 78.8 | 61.5 | |
| No | 47.2 | 21.2 | 38.5 | |
| A7. If we had a domestic COVID-19 vaccine, I would have it | 0.001 | |||
| Yes/not sure | 88.8 | 89.8 | 69.2 | |
| No | 11.2 | 10.2 | 30.8 | |
| A8. My friends do not think I should get the COVID-19 vaccine | <0.001 | |||
| Yes/not sure | 1.1 | 13.6 | 78.8 | |
| No | 98.9 | 86.4 | 21.2 | |
| A9. I think that COVID-19 vaccines are developed by manufacturers for different purposes | <0.001 | |||
| Yes/not sure | 4.5 | 28.0 | 48.1 | |
| No | 95.5 | 72.0 | 51.9 | |
| A10. I do not find it religiously appropriate to get the COVID-19 vaccine | <0.001 | |||
| Yes/not sure | 5.6 | 10.2 | 30.8 | |
| No | 94.4 | 89.8 | 69.2 |
In Tables 4 and 5, the VAX scale total and subscale scores are presented by descriptive characteristics of the study group. The mean of total VAX scale score is 42.34±10.93 (Min: 18 and max: 71). The mistrust of vaccine benefit scores of primary-secondary school graduates is (8.79±4.63) significantly higher than high school graduates (p=0.001).
Table 4.
Mean VAX scale scores by descriptive characteristics of participants
| Mistrust of vaccine benefit | Worries about unforeseen future effects | Concerns about commercial profiteering | Preference for natural immunity | Total | |
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | |
| Gender | |||||
| Male | 8.16±4.55 | 14.12±3.84 | 7.64±3.76 | 12.64±4.89 | 42.57±11.47 |
| Female | 8.72±4.39 | 14.43±3.29 | 7.48±3.30 | 11.48±4.66 | 42.10±10.40 |
| P-value | 0.320 | 0.491 | 0.705 | 0.051 | 0.728 |
| Educational status | |||||
| Primary-secondary school | 8.79±4.63 | 14.03±3.67 | 7.92±3.71 | 11.20±5.02 | 41.94±11.49 |
| High school | 7.74±4.17 | 14.68±3.30 | 6.99±3.18 | 13.68±4.24 | 43.08±10.08 |
| University | 8.35±4.26 | 14.59±3.68 | 7.15±3.25 | 12.47±4.05 | 42.53±10.24 |
| P-value | 0.001 | 0.254 | 0.391 | 0.137 | 0.762 |
| Marital status | |||||
| Married | 8.22±4.40 | 14.32±3.62 | 7.64±3.59 | 12.12±4.99 | 42.30±11.23 |
| Others | 9.33±4.66 | 14.10±3.41 | 7.23±3.30 | 11.80±3.98 | 42.47±9.67 |
| P-value | 0.111 | 0.689 | 0.465 | 0.631 | 0.922 |
| Having a child | |||||
| Yes | 8.46±4.45 | 14.32±3.55 | 7.54±3.52 | 12.06±4.88 | 42.38±11.00 |
| No | 8.25±4.74 | 13.75±3.85 | 7.80±3.75 | 12.053.83 | 41.85±10.21 |
| P-value | 0.843 | 0.493 | 0.752 | 0.993 | 0.836 |
| Working status | |||||
| Working | 8.54±4.47 | 14.35±3.61 | 7.53±3.69 | 12.60±4.76 | 43.01±10.63 |
| Not working | 8.37±4.48 | 14.22±3.55 | 7.59±3.41 | 11.63±4.81 | 41.81±11.16 |
| P-value | 0.762 | 0.772 | 0.892 | 0.110 | 0.381 |
| Presence of a health problem | |||||
| Yes | 8.10±4.36 | 14.23±3.46 | 7.55±3.44 | 11.91±4.74 | 41.79±10.50 |
| No | 8.81±4.57 | 14.33±3.71 | 7.57±3.64 | 12.21±4.89 | 42.93±11.39 |
| P-value | 0.207 | 0.821 | 0.956 | 0.609 | 0.405 |
SD: Standard deviation; VAX: Vaccination attitudes examination.
Table 5.
Mean VAX scale scores by COVID-19 history, any vaccination history, intentions-preferences, and refusal of the participants
| Mistrust of vaccine benefit | Worries about unforeseen future effects | Concerns about commercial profiteering | Preference for natural immunity | Total | |
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | |
| COVID-19 history | |||||
| Yes | 8.44±4.18 | 14.15±3.69 | 7.38±3.55 | 13.22±4.35 | 43.19±10.34 |
| No | 8.53±4.60 | 14.34±3.54 | 7.45±3.39 | 11.47±4.86 | 41.80±11.04 |
| Not sure | 7.38±4.82 | 14.31±3.45 | 10.08±4.37 | 11.69±5.91 | 42.34±10.93 |
| P-value | 0.676 | 0.925 | 0.030 | 0.023 | 0.593 |
| Any vaccination history | |||||
| Yes | 7.88±4.15 | 14.16±3.69 | 7.30±3.38 | 12.52±4.58 | 41.87±10.03 |
| No | 10.97±4.75 | 9.67±5.31 | 15.55±2.56 | 9.33±3.85 | 47.73±11.72 |
| Not sure | 9.67±5.31 | 13.54±3.48 | 7.29±3.78 | 8.38±4.97 | 38.88±14.61 |
| P-value | <0.001 | 0.067 | 0.008 | <0.001 | 0.004 |
| Intentions to vaccinate against COVID-19 | |||||
| Will vaccinate | 5.90±2.87 | 12.60±3.62 | 5.66±2.42 | 11.29±4.72 | 35.45±8.25 |
| Hesitant | 8.77±4.32 | 14.64±3.39 | 8.14±3.66 | 12.05±4.95 | 43.59±9.96 |
| Refusers | 12.04±4.39 | 16.35±2.43 | 9.50±3.36 | 13.38±4.41 | 51.27±9.55 |
| P-value | <0.001 | <0.001 | <0.001 | 0.044 | <0.001 |
| COVID-19 vaccine preferences | |||||
| Comirnaty | 6.98±3.79 | 13.20±3.52 | 6.72±3.47 | 12.45±4.61 | 39.36±9.36 |
| CoronaVac | 7.91±4.33 | 14.26±3.91 | 6.65±2.93 | 11.09±5.05 | 39.91±9.97 |
| Domestic vaccine | 8.85±4.10 | 14.91±2.72 | 9.15±3.25 | 11.26±4.88 | 44.18±10.27 |
| Does not matter | 7.09±3.65 | 13.18±4.87 | 6.18±3.54 | 9.09±5.30 | 35.55±14.05 |
| P-value | 0.097 | 0.063 | 0.001 | 0.074 | 0.037 |
| Vaccine refusal | |||||
| Yes | 15.86±3.03 | 17.21±1.25 | 11.50±3.13 | 12.14±3.98 | 56.71±7.40 |
| No | 7.26±3.80 | 13.85±3.61 | 6.92±3.16 | 11.76±4.92 | 39.79±9.84 |
| Not sure | 11.13±4.15 | 15.19±3.32 | 9.02±3.94 | 13.25±4.44 | 48.58±10.93 |
| P-value | <0.001 | <0.001 | <0.001 | 0.157 | <0.001 |
| All (n=259) | 8.44±4.47 | 14.28±3.57 | 7.56±3.53 | 12.06±4.81 | 42.34±10.93 |
SD: Standard deviation; VAX: Vaccination attitudes examination.
Two of the four VAX subscales have significantly different mean scores by COVID-19 history. The mean value of “preference for natural immunity” subscale score (13.22±4.35) is significantly higher in participants with positive COVID-19 history than the others (p=0.023). “Concerns about commercial profiteering” score are significantly higher among the individuals who are not sure about their COVID-19 history (p=0.030).
Participants who do not have any vaccination history have significantly the higher scores for the subscales of “mistrust of vaccine benefit,” “concerns about commercial profiteering,” and total VAX score (p<0.001, p=0.008, and p=0.004, respectively). The group with positive vaccination history has significantly the higher scores for “preference for natural immunity” subscale (p<0.001).
The group who has no intention for vaccination against COVID-19 has higher scores for all subscales than all other groups (p<0.05 for all comparisons). In terms of the vaccine preference, “concerns about commercial profiteering” subscale and the total VAX scores are higher among the participants who prefer the domestic vaccine and CoronaVac than the other groups (p=0.002 and p=0.037, respectively). Vaccine refusers have the highest total and subscale scores (p<0.001 for all comparisons) except for “preference for natural immunity.”
We performed multiple linear regression analysis to understand the predictors of total VAX scale scores. As it is shown from Table 6, “Presence of a health problem” (β=0.147, p=0.044), “COVID-19 history” (β=-0.161, p=0.021), “intentions to vaccinate against COVID-19” (β=0.551, p<0.001), and “vaccine refusal” (β=0.208, p=0.027) are significant predictors of the total VAX scale score (R2=0.484). While the presence of a health problem, COVID-19 history, and intentions to vaccinate against COVID-19 are negatively associated, vaccine refusal has a positive association with the VAX scale. “Intentions to vaccinate against COVID-19” is the strongest and most significant predictor of VAX scale and it is followed by “vaccine refusal” which is not surprising.
Table 6.
Multiple linear regression findings of VAX scale scores
| VAX scale score | B | SE | β | p |
|---|---|---|---|---|
| Constant | 77.223 | 12.891 | <0.001 | |
| Age | -0.159 | 0.176 | -0.072 | 0.367 |
| Gender | ||||
| 1: Female 2: Male | -1.221 | 2.011 | -0.055 | 0.545 |
| Educational status | ||||
| 1: Primary/secondary school | ||||
| 2: High school | -0.362 | 1.245 | -0.023 | 0.772 |
| 3: University | ||||
| Marital status | ||||
| 1: Married 2: Other | -0.952 | 2.436 | -0.033 | 0.697 |
| Having a child | ||||
| 1: Yes 2: No | -0.442 | 4.280 | -0.009 | 0.918 |
| Working status | ||||
| 1: Yes 2: No | -4.574 | 2.047 | -0.206 | 0.127 |
| Presence of a health problem | ||||
| 1: Yes 2: No | 2.995 | 1.474 | 0.147 | 0.044 |
| COVID-19 history | ||||
| 1: Yes 2: No | 3.440 | 1.476 | 0.161 | 0.021 |
| Any vaccination history | ||||
| 1: Yes 2: No | 0.452 | 2.531 | 0.015 | 0.859 |
| Vaccine refusal | ||||
| 1: Yes 2: Not sure 3:No | -5.559 | 2.486 | -0.208 | 0.027 |
| Intentions to vaccinate against COVID-19 | ||||
| 1: Yes 2: Hesitant 3: No | 12.812 | 2.026 | 0.551 | <0.001 |
VAX: Vaccination attitudes examination; B: The unstandardized beta; SE: The standard error for the unstandardized beta; β: The standardized beta; p: The probability value.
DISCUSSION
The degree of existing vaccine hesitancy has increased in recent years, reached its peak during the COVID-19 pandemic [23]. Many vaccines with different production technologies are currently in use and many others are going to be developed [24]. It is well known that to reach immunization levels that will ensure herd immunity, COVID-19 vaccines should be widely accepted and used by the community. Refusal of vaccination will provide opportunities for the emergence of new variants in addition to negative effects on herd immunity. Therefore, the increasing anti-vaccination attitudes and vaccine hesitancy are an important public health issue to be overwhelmed. Due to the complexity of the problem, it is not possible to plan a single intervention strategy. Although interventions should be made according to the specific characteristics of the groups, it is important to understand the attitudes and practices as the first step [25].
In our study group, the frequency of vaccine hesitancy is 18.5% and the proportion of refusers is 5.4%. In a guidelines on dealing with vaccine hesitancy and refusal, it is stated that hesitant group should be the primary target group for persuasion [26]. When the hesitant group in our study is handled with this approach, it can be ensured that the supporters of the vaccine can go up to 95%, and the refusers remain in a small group. However, when the attitudes specifically toward COVID-19 vaccines are considered both the hesitancy and refusal increases significantly (45.6% and 20.1%, respectively). In a study conducted in Israel, it was reported that the level of vaccine hesitancy in the community is higher for COVID-19 vaccines [27]. A systematic review findings indicate that the COVID-19 vaccine acceptance percentages vary in a wide range as 23.6–97.0% [23]. In a study conducted in Turkiye, proportion of hesitant group was 34.0% and refusers 3.0% for COVID-19 vaccines [28].
The first vaccines approved by the WHO, were comirnaty, Oxford-AstraZeneca, and Moderna [29]. Turkiye started vaccination program by China-based CoronaVac on January 14, 2021, and it was followed by comirnaty a few months later besides the development studies of a domestic vaccine [30]. More than 60% of our study participants stated that they would prefer comirnaty or CoronaVac, and only 13.1% stated to prefer a domestic vaccine. Contrary to popular belief, this finding shows that the preference for domestic vaccine is low. The high score of the mistrust of vaccine benefit and concerns about commercial profiteering subscale in those who prefer domestic vaccine indicates the reasons underlying the preference of them. Therefore, we can say that the presence of at least one domestic vaccine alternative may increase the vaccination percentage.
Studies show that individuals are most exposed to anti-vaccination propaganda through the news sources on the internet and the spread of gossip, myth, and false beliefs has risen parallel to the increased use of social media [31]. The participants in our study also stated TV, internet, and social media as primary information sources about vaccines. This finding shows that fighting against misinformation is as important as the fight against the pandemic. Social media users with an anti-vaccine view are being more active, even though they are less in number, which lead their voice to be heard louder and their claims without evidence to spread [32]. Access to accurate and reliable information resources should be one of the main topics of the struggle. It can be ensured with methods such as more extensive and visible statements from official institutions and experts, optimizing web search algorithms, and defining verified information sources [32–34]. To be successful, it is essential that all information about vaccines should be communicated to the public through an open and transparent manner [14].
While the reasons of anti-vaccination differ among communities underestimating the disease, the idea that vaccines are not a need, distrust against industry, and cultural-religious factors are listed as the main reasons [31, 32]. During the COVID-19 pandemic, new claims such as “vaccines are not capable of protecting against the disease,” “the virus did not actually exist,” “5G,” and “vaccines are used to put microchips into human body” have been added [18, 31, 32]. More than 80% of the participants of our study have expressed side effects as the most common reason of concern. When we consider factors such as the distrust against the industry, the belief that the vaccines do not provide protection, and that COVID-19 vaccines are produced relatively faster, the fundamental issue seems to be the lack of knowledge. Although several scientific publications helped to put forth many proof regarding the impropriety of these concerns, it is clear that not getting vaccinated because of such unreal arguments is still an important issue [10, 11].
It is known that there are various concerns among the people regarding COVID-19 vaccines, whether they intend to be vaccinated or not. This is supported by the fact that, despite stating that they will be vaccinated, 70% are afraid of the side effects and 20% have doubts about the protection of vaccines. It is expectable that these concerns are more common in those who are hesitant about vaccination or those who refuse vaccination. However, it is noteworthy that those who wait for the effects of the vaccine on others for a while and then consider getting vaccinated are at a considerable level. This finding shows that, as the safety of vaccines will become more understood, part of those who even have not gotten their first doses will get vaccinated.
Due to the statements about development of strong immune response following the disease and publications about the difficulty of achieving herd immunity through vaccination, ideas have emerged that advocate having the disease instead of getting vaccinated [18, 35–37]. In some infections, the immunity acquired by the disease is stronger and more permanent than the immunity by vaccination. However, considering the risks of the disease, the advantages of vaccination are indisputable [38, 39]. The fact that the subscale “preference to natural immunity” stands out on individuals who have had the disease, shows that this point of view in the community is one of the factors that affect the vaccination decision. Similarly, a study conducted in Qatar reported that natural exposure to viruses is perceived as the safest protection attitude [40]. It is interesting those who have chronic illnesses are low on anti-vaccination attitudes and reasons for it should be examined in other studies.
The negative attitudes toward vaccines in our study are moderate in every group and are similar to other study findings [27, 40, 41]. The presence of a trust problem in those with low educational status and opinions about natural immunity is also compatible findings with the literature. It is seen that low education level and mistrust toward the industry are most important factors associated with COVID-19 vaccine hesitancy.
Limitations
A cross-sectional design is the major limitation of our study findings since attitudes of the participants may change over time. Other limitations are related with selection and size of the study sample. Study results cannot be generalized because it is conduct of the study in a single district and exclusion of individuals who do not have a registered phone number disables the generalization of the findings. Possible recall biases due to data collection through phone call is another limitation.
Recommendations
In a period where the supply issue of the COVID-19 vaccine has decreased, the priority should be taking the necessary precautions against hesitations and anti-vaccine attitudes with a suitable risk communication plan. The reasons should be questioned and required improvements should be made through special communication channels for those who have not been vaccinated when a vaccine was available for them. It is important that the public commonly prefers receiving information from sources that include comments from competent experts. Finally, the development of domestic vaccine should be accelerated as it will increase the immunization percentage.
Conclusion
Rise of anti-vaccination attitudes and vaccine hesitancy that have increased with the COVID-19 vaccines seems to be significant barriers in front of the herd immunity. Our study is valuable in terms of examining the reasons of individuals who have not gotten vaccinated even though they had no access problems. It grabs attention that, while hesitant and refusers are usually around 24.0%, it rises to 65.0% for COVID-19 vaccines. There are important concerns, even among individuals who have decided on getting vaccinated, particularly on the side effects and distrust against the industry. These concerns should be taken seriously. Misinformation can be prevented by taking the required implementations to both spread correct information and prevent false ones. Otherwise, vaccine hesitancy can be a decisive factor that would prevent the success of the pandemic.
Footnotes
Cite this article as: Atac O, Elmaslar B, Yavuz EF, Yurdabak FE, Kaya F, Aktas S, et al. Attitudes and practices against COVID-19 vaccines in Turkiye. North Clin Istanb 2022;9(5):484–494.
Ethics Committee Approval
The Istanbul Medipol University on-Interventional Clinical Research Ethics Committee granted approval for this study (date: 17.06.2021, number: 674).
Conflict of Interest
No conflict of interest was declared by the authors.
Financial Disclosure
The authors declared that this study has received no financial support.
Authorship Contributions
Concept – OA, BE, EFY, FEY, FK, SA, MA, OH; Design – OA, BE, EFY, FEY, FK, SA, MA, OH; Supervision – OA, OH, MA; Fundings – OA, BE, EFY, FEY, FK, SA, MA; Materials – MA; Data collection and/or processing – BE, EFY, FEY, FK, SA, MA; Analysis and/or interpretation – OA, BE, EFY, FEY, FK, SA, OH; Literature review – OA, BE, EFY, FEY, FK, SA; Writing – OA, BE, EFY, FEY, FK, SA, OH; Critical review – OA, OH.
References
- 1.Centers for Disease Control and Prevention (CDC) Ten great public health achievements--worldwide, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60:814–8. [PubMed] [Google Scholar]
- 2.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9:1763–73. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Ten threats to global health in 2019. Available at: https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019 Accessed Sep 10, 2021.
- 4.Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. 2020;369:846–9. doi: 10.1126/science.abc6810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGill COVID19 Vaccine Tracker Team COVID19 Vaccine Tracker Dashboard [Internet] Available at: https://covid19.trackvaccines.org/ Accessed Sep 8 2022.
- 6.Christie A, Henley SJ, Mattocks L, Fernando R, Lansky A, Ahmad FB, et al. Decreases in COVID-19 cases, emergency department visits, hospital admissions, and deaths among older adults following the ıntroduction of COVID-19 vaccine-United States, September 6, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:858–64. doi: 10.15585/mmwr.mm7023e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina, et al. Coronavirus Pandemic (COVID-19) [Internet] Available at: https://ourworldindata.org/coronavirus Accessed Sep 8, 2022.
- 8.Dratva J, Wagner A, Zysset A, Volken T. To vaccinate or not to vaccinate-this ıs the question among Swiss university students. Int J Environ Res Public Health. 2021;18:9210. doi: 10.3390/ijerph18179210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranzani OT, Hitchings M, Nieto MD, D’Agostini TL, de Paula RC, de Paula OF, et al. Effectiveness of the CoronaVac vaccine in the elderly population during a P.1 variant-associated epidemic of COVID-19 in Brazil: A test-negative case-control study. BMJ. 2021;374:1–12. doi: 10.1136/bmj.n2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. C4591001 Clinical Trial Group Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–15. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doroftei B, Ciobica A, Ilie OD, Maftei R, Ilea C. Mini-review discussing the reliability and efficiency of COVID-19 vaccines. Diagnostics (Basel) 2021;11:579. doi: 10.3390/diagnostics11040579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis. 2020;14:e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu T, He Z, Huang J, Yan N, Chen Q, Huang F, et al. A comparison of vaccine hesitancy of COVID-19 vaccination in China and the United States. Vaccines (Basel) 2021;9:649. doi: 10.3390/vaccines9060649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–8. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657–63. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35:781–3. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines (Basel) 2020;9:16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Küçükali H, Ataç Ö, Palteki AS, Tokaç AZ, Hayran O. Vaccine hesitancy and anti-vaccination attitudes during the start of COVID-19 vaccination program: a content analysis on twitter data. Vaccines. 2022;10:161. doi: 10.3390/vaccines10020161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministry of Health Turkish national COVID-19 vaccine administration strategy. Available at: https://covid19asi.saglik.gov.tr/EN-78317/turkish-national-covid-19-vaccine-administration-strategy Accessed Sep 1, 2021.
- 20.Ministry of Health Republic of Turkey Ministry of Health COVID-19 vaccination information platform. Available at: https://covid19asi.saglik.gov.tr Accessed Sep 5, 2021.
- 21.Martin LR, Petrie KJ. Understanding the dimensions of anti-vaccination attitudes: the Vaccination Attitudes Examination (VAX) Scale. Ann Behav Med. 2017;51:652–60. doi: 10.1007/s12160-017-9888-y. [DOI] [PubMed] [Google Scholar]
- 22.Yildiz E, Gungormus Z, Dayapoglu N. Assessment of validity and reliability of the Turkish version of the Vaccination Attitudes Examination (VAX) Scale. Int J Caring Sci. 2021;14:261–8. [Google Scholar]
- 23.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization COVID-19 vaccine tracker and landscape. Available at: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines Accessed Jan 23 2021.
- 25.Eskola J, Duclos P, Schuster M, MacDonald NE, SAGE Working Group on Vaccine Hesitancy How to deal with vaccine hesitancy? Vaccine. 2015;33:4215–7. doi: 10.1016/j.vaccine.2015.04.043. [DOI] [PubMed] [Google Scholar]
- 26.Nowak GJ, Gellin BG, MacDonald NE, Butler R, SAGE Working Group on Vaccine Hesitancy Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine. 2015;33:4204–11. doi: 10.1016/j.vaccine.2015.04.039. [DOI] [PubMed] [Google Scholar]
- 27.Shacham M, Greenblatt-Kimron L, Hamama-Raz Y, Martin LR, Peleg O, Ben-Ezra M, et al. Increased COVID-19 vaccination hesitancy and health awareness amid COVID-19 vaccinations programs in Israel. Int J Environ Res Public Health. 2021;18:3804. doi: 10.3390/ijerph18073804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salali GD, Uysal MS. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med. 2020:1–3. doi: 10.1017/S0033291720004067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization Status of COVID-19 vaccines within WHO EUL/PQ evaluation process. Available at: https://extranet.who.int/pqweb/sites/default/files/documents/Status_COVID_VAX_11Nov2021.pdf Accessed Nov 15, 2021.
- 30.ClinicalTrials.gov Efficacy, immunogenicity, and safety of the inactivated COVID-19 vaccine (TURKOVAC) versus the CoronaVac Vaccine. Available at: https://clinicaltrials.gov/ct2/show/NCT04942405 Accessed Nov 1 2021.
- 31.Ullah I, Khan KS, Tahir MJ, Ahmed A, Harapan H. Myths and conspiracy theories on vaccines and COVID-19: Potential effect on global vaccine refusals. Vacunas. 2021;22:93–7. doi: 10.1016/j.vacun.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ortiz-Sánchez E, Velando-Soriano A, Pradas-Hernández L, Vargas-Román K, Gómez-Urquiza JL, Cañadas-De la Fuente GA, et al. Analysis of the anti-vaccine movement in social networks: a systematic review. Int J Environ Res Public Health. 2020;17:5394. doi: 10.3390/ijerph17155394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fadda M, Albanese E, Suggs LS. When a COVID-19 vaccine is ready, will we all be ready for it? Int J Public Health. 2020;65:711–2. doi: 10.1007/s00038-020-01404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Choe PG, Kim KH, Kang CK, Suh HJ, Kang E, Lee SY, et al. Antibody responses 8 months after asymptomatic or mild SARS-CoV-2 infection. Emerg Infect Dis. 2021;27:928–31. doi: 10.3201/eid2703.204543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature. 2021;591:520–2. doi: 10.1038/d41586-021-00728-2. [DOI] [PubMed] [Google Scholar]
- 37.Block J. Vaccinating people who have had covid-19: why doesn’t natural immunity count in the US? BMJ. 2021;374:n2101. doi: 10.1136/bmj.n2101. [DOI] [PubMed] [Google Scholar]
- 38.Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373:n1088. doi: 10.1136/bmj.n1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397:1819–29. doi: 10.1016/S0140-6736(21)00947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alabdulla M, Reagu SM, Al-Khal A, Elzain M, Jones RM. COVID-19 vaccine hesitancy and attitudes in Qatar: A national cross-sectional survey of a migrant-majority population. Influenza Other Respir Viruses. 2021;15:361–70. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Godasi GR, Donthu RK, Mohammed AS, Pasam RS, Tiruveedhula SL. Attitude towards COVID-19 vaccine among the general public in south India: A cross sectional study. Arch Ment Heal. 2021;22:28–35. [Google Scholar]


