Abstract
Background:
Performance measures such as strength, jump height/length, and change of direction (CoD) time during anterior cruciate ligament (ACL) rehabilitation have been used to determine readiness to return to play and identify those who may be at risk of rerupture. However, athletes may reach these criteria despite ongoing biomechanical deficits when performing these tests. Combining return-to-play criteria with an assessment of movement through 3-dimensional (3D) biomechanics in male field sports athletes to identify risk factors for ACL rerupture has not been explored previously.
Purpose:
To prospectively examine differences in strength, jump, and CoD performance and movement using 3D biomechanics in a cohort of male athletes playing level 1 sports (ie, multidirectional field sports that involve landing, pivoting, or CoD) between those who reinjured the reconstructed ACL (RI group) and those with no reinjury (NRI group) after 2 years of follow-up and to examine the ability of these differences to predict reinjury.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
After primary ACL reconstruction (ACLR), 1045 male athletes were recruited and underwent testing 9 months after surgery including isokinetic strength, jump, and CoD performance measures as well as patient-reported outcomes and 3D biomechanical analyses. Participants were followed up after 2 years regarding ACL reinjury status. Differences were determined between the RI and NRI groups in patient-reported outcomes, performance measures, and 3D biomechanics on the ACLR side and symmetry between limbs. The ability of these measures to predict ACL reinjury was determined through logistic regression.
Results:
No differences were identified in strength and performance measures on the ACLR side or in symmetry. Biomechanical analysis indicated differences on the ACLR side primarily in the sagittal plane for the double-leg drop jump (effect size, 0.59–0.64) and greater asymmetry primarily in the frontal plane during unplanned CoD (effect size, 0.61–0.69) in the RI group. While these biomechanical test results were different between groups, multivariate regression modeling demonstrated limited ability (area under the curve, 0.67 and 0.75, respectively) to prospectively predict ACL reinjury.
Conclusion:
Commonly reported return-to-play strength, jump, and timed CoD performance measures did not differ between the RI and NRI groups. Differences in movement based on biomechanical measures during double-leg drop jump and unplanned CoD were identified, although they had limited ability to predict reinjury. Targeting these variables during rehabilitation may reduce reinjury risk in male athletes returning to level 1 sports after ACLR.
Keywords: anterior cruciate ligament reconstruction, return to play, reinjury, biomechanics
Reducing the risk of anterior cruciate ligament (ACL) reinjury is probably the most important goal for a surgeon, athlete, and physical therapist after ACL reconstruction (ACLR) surgery.21,23 Return-to-play (RTP) criteria have been used to mitigate the risk of reinjury, and to monitor rehabilitation status before RTP. The criteria are commonly assessed using physical tests of lower limb strength, jump height/length, and timed change-of-direction (CoD) performance. Outcomes from these performance tests are combined with patient-reported outcome (PRO) questionnaires to identify factors that may influence ACL reinjury risk.9,11,21,26 Recovery of symmetry of these performance measures, reported as limb symmetry index (LSI), is suggested to influence the risk of any injury to the operated knee11 and reinjury of the reconstructed ACL.21 It has been recommended that success rates (percentage of group that achieves ≥90% LSI) should also be reported during group comparison.43 However, passing the RTP criteria has not always shown a significant association with second injury risk. Athletes have also been reported to achieve symmetrical performance during jump and CoD tests after ACLR but with asymmetrical joint mechanics.14,15 This suggests that assessing movement quality through biomechanical analysis may offer a more robust measure of physical recovery after ACLR when assessing reinjury risk than assessing it through commonly used performance test batteries alone.
To date, few studies have prospectively examined biomechanical variables related to ACL reinjury risk. Paterno et al35 identified several biomechanical factors predicting second ACL injury during double-leg drop jump testing including uninvolved limb hip rotation moment, asymmetry of knee extension moment at initial contact, and knee valgus range of motion during landing. However, reinjury and contralateral ACL injuries were combined during the analysis, so it is unclear if the risk factors were specific to injury to either limb or were different between limbs. Our understanding of the mechanisms that may result in reinjury may be complicated by inclusion of male and female patients.19,40 A potential limitation to our understanding of the reinjury mechanism is that the research is restricted to the double-leg drop jump, although up to 50% of ACL injuries occur during CoD maneuvers and single-leg landing.1 To assess the influence of PROs, performance measures, and biomechanics on ACL reinjury, studies must control for several nonphysical factors that may influence the risk of ACL reinjury and physical recovery, including time since surgery, age, level and type of sport, and graft type.11,21,29,35,41,46 Therefore, a combination of PRO, strength, and performance measures as well as 3-dimensional (3D) biomechanical analysis in jump and CoD tests in a homogeneous cohort of athletes may better identify those at increased risk of ACL reinjury.
The primary aim of this study was to examine differences in strength, jump, and timed CoD performance measures as well as PROs and 3D biomechanics during jump and CoD testing in a group of male athletes aged 18 to 35 years returning to level 1 sports (multidirectional field sports that involve landing, pivoting, or CoD) after primary ACLR between those with ACL reinjury and a matched cohort with no reinjury 2 years after surgery. The secondary aim was to assess the ability of these variables to predict who would experience ACL reinjury.
METHODS
Athletes were recruited for this prospective case-control study between January 1, 2014, and December 31, 2016, from the caseload of 2 orthopaedic surgeons (M.J., R.M.) at the Sports Surgery Clinic in Dublin. Participants were enrolled in the study if they received a diagnosis of ACL rupture, had a confirmed surgical date, and provided informed consent. Before surgery, participants completed a preoperative questionnaire outlining their sport, mechanism of injury, and level of desired return after surgery. Male participants aged 18 to 35 years who played multidirectional field sports and intended to return to the same level of sport were included in the study. All participants underwent primary ACLR using either a bone–patellar tendon–bone or hamstring (gracilis/semitendinosus) graft from the ipsilateral limb. Participants who were undergoing second or subsequent ACLR, did not intend to return to level 1 sports, or had meniscal/additional ligamentous repair at the time of surgery were excluded. The study was registered at ClinicalTrials.gov (NCT02771548) and received ethical approval from the Sports Surgery Clinic Hospital Ethics Committee (25-AFM-010).
Testing Protocol
After surgery, all participants underwent an accelerated rehabilitation protocol with weightbearing as tolerated on crutches for 2 weeks, followed by progressive blocks of strength and neuromuscular control, power and reactive strength development, and running and CoD mechanics as physical competency and knee symptoms allowed. Athletes underwent rehabilitation locally with their referring physiotherapist and were reviewed by their orthopaedic surgeons at 2 weeks, 3 months, and 6 to 9 months after surgery. As part of their final orthopaedic review, participants took part in a physical testing protocol at approximately 9 months after surgery. Before the testing session, all participants completed the following PRO measures: the International Knee Documentation Committee (IKDC),13 Marx Activity Scale,25 and ACL Return to Sport After Injury (ACL-RSI) questionnaire.45 The data collection protocol took place in a 3D biomechanics laboratory and included a double-leg drop jump from 30 cm, a single-leg drop jump from 20 cm, and 90° planned and unplanned CoD, as described elsewhere.14,15 In addition, single-leg countermovement jump height and single-leg hop for distance length were assessed to compare with previous literature.11,21,30 Participants undertook a standardized warm-up: 2-minute jog, 5 bodyweight squats, and 2 submaximal and 3 maximal double-leg countermovement jumps. Each participant underwent 2 submaximal practice trials of each movement before 3 valid test trial attempts were captured (maximal effort and full-foot contact on force plate), with the mean of 3 trials used for analysis. Participants took a 30-second recovery between trials. Laboratory testing was followed by concentric isokinetic testing of the quadriceps and hamstring muscle groups of both limbs at 60 deg/s through 0° to 100° of knee flexion. Peak torque/body mass was used to define the strength performance measures.44
Biomechanical Analysis
Joint kinematic data were collected using an 8-camera motion analysis system (Bonita-B10; Vicon) capturing at 200 Hz that was synchronized with 2 force platforms (BP400600; AMTI) sampling at 1000 Hz. Motion data from 24 reflective markers (14-mm diameter) were integrated with ground-reaction forces (Nexus 1.8.5; Vicon), which were low pass filtered using a fourth-order Butterworth filter (cutoff frequency, 15 Hz).18 Participants wore their own athletic footwear. Reflective markers were secured using tape at bony landmarks on the lower limbs, pelvis, and trunk per the adapted Plug-in-Gait marker set.24 A custom MATLAB program (MathWorks Inc) was used for processing and calculating the variables analyzed. The motion of the center of mass (COM) relative to the ankle and knee joints was assessed by quantifying the distance from the COM to the ankle and knee joints in all 3 planes.15 At the joint level, in addition to the ankle, knee, and hip 3D joint angles and moments, the trunk to pelvis angle in all 3 planes and the foot-pelvis angle in the transverse plane were quantified. All kinetic variables including ground-reaction force were normalized to body mass. Whole body stiffness when the body was accepting load was calculated as follows:
where vGRF denotes vertical ground-reaction force and delta for both variables is from impact (the point of initial ground contact) to the end of the eccentric phase, defined as the first instance at which COM vertical power was >0. Kinetic and kinematic analyses were performed for the stance phase of each jump and CoD test (defined by ground-reaction force >20 N). Curves were normalized to 101 frames and landmark registered37 to the end of the eccentric phase.28 This process aligned onset of the eccentric phase to 50% of the movement cycle across participants to ensure relevant comparison of neuromuscular characteristics between limbs and participants during continuous waveform analysis. Performance outcomes were determined for the jump and CoD tasks. Jump height for single-leg countermovement jump, double-leg drop jump, and single-leg drop jump was calculated from ground-reaction forces using the impulse-momentum theorem, and jump length for single-leg hop for distance was calculated as the distance from heel marker at start to landing. Time to complete the 90° CoD was recorded using speed gates (Smartspeed; Fusion Sport) with a trigger gate 2 m from the start line and an exit gate 2 m to the left and right of the force plates to indicate the end of the maneuver.14 LSI for strength and jump performance scores was calculated as follows: (ACLR side / non–ACLR side) × 100. Asymmetry in biomechanical variables was calculated as the ACLR side minus non–ACLR side.
Follow-up
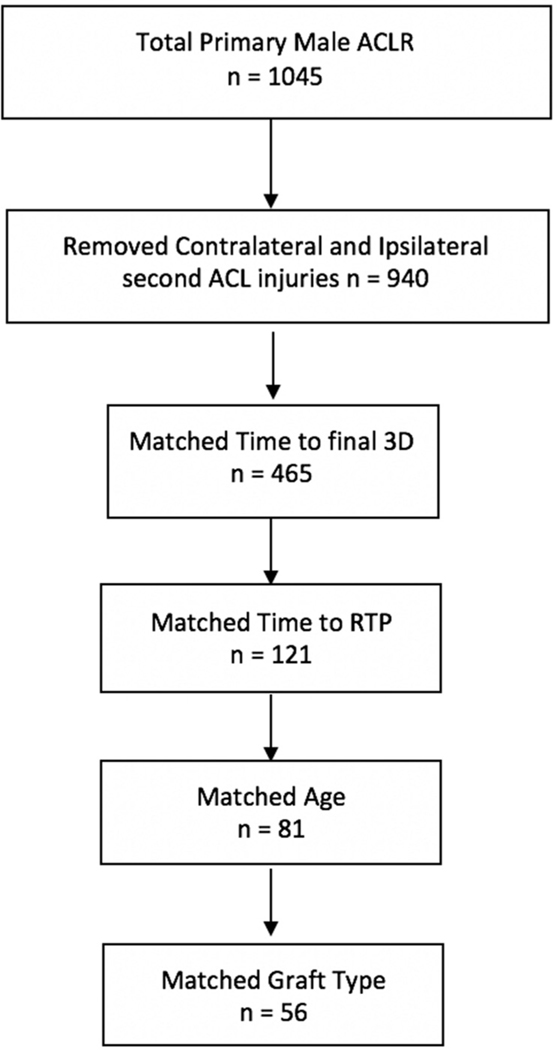
All participants were followed up via email at 1 and 2 years after surgery using a questionnaire recording RTP status (return to same level of sports, yes/no) and identifying those who sustained rerupture of the reconstructed ACL or rupture of the contralateral ACL. Reinjuries were also identified between these time points if participants returned to the surgeon with diagnosis of another ACL injury, with the same questionnaire regarding RTP and reinjury completed at this point. If participants did not reply to the email questionnaire or return to the surgeon, they received a follow-up telephone call to complete the questionnaires. For this study, all participants who reinjured the reconstructed ACL were included and placed in the ipsilateral reinjury group (RI group). From the remaining participants who returned to multidirectional field sports after ACLR and did not have ipsilateral reinjury or contralateral ACL injury (NRI group) at 2-year follow-up, a cohort was selected to match to the RI group based on the following: mean time from surgery to 3D biomechanical testing, time from surgery to RTP, age, and graft type (Figure 1). This ensured appropriate comparison and minimized the potential influence of other factors on ACL reinjury.
Figure 1.
Flow diagram of matching process between the reinjury and no-reinjury groups. 3D, 3-dimensional; ACL, anterior cruciate ligament; ACLR, ACL reconstruction; RTP, return to play.
Statistical Analysis
Differences in PROs, strength (normalized knee flexion, extension peak torque), and performance (single-leg countermovement jump, single-leg drop jump height, single-leg hop for distance length, CoD time) for the ACLR side were examined using Mann-Whitney U tests. Differences in LSI between the RI and NRI groups were examined using independent Student t tests (Table 1).33 Effect sizes for differences between groups were calculated and interpreted using Cohen d (0.20–0.49, small; 0.50–0.79, medium; 0.80, strong).7 Success rates (percentage of group that achieved the outcome) attaining ≥90% LSI for quadriceps and hamstring strength, single-leg countermovement jump and single-leg drop jump height, and single-leg hop for distance length were calculated for all groups,42 with differences examined using the chi-square test of homogeneity. Additionally, odds ratios were calculated for being in the NRI group as compared with the RI group when the LSI was ≥90% for quadriceps, hamstring strength, single-leg countermovement jump, single leg hop for distance, and single-leg drop jump height, as well as when the LSI was ≥90% for all 5 tests collectively.
TABLE 1.
Data Points and Statistical Analysisa
| Data Set | Analysis |
|---|---|
|
| |
| PRO data | Mann-Whitney U test Independent Student t test |
| Strength, jump, and CoD performance | Success rate ≥90% LSI |
| ACLR side and LSI | Odds ratio for NRI if ≥90% LSI Logistic regression |
| Biomechanics on ACLR side and ASYM | 1D SPM independent Student t test |
| Logistic regression | |
1D, 1-dimensional; ACLR, anterior cruciate ligament reconstruction; ASYM, asymmetry; CoD, change of direction; LSI, limb symmetry index; NRI, no reinjury group; PRO, patient-reported outcome; SPM, statistical parametric mapping.
Statistical parametric mapping (1 dimensional unpaired t test, parametric) was used to examine differences in lower limb biomechanics between the RI and NRI groups for the ACLR limb and differences in asymmetry between limbs between groups (ACLR minus non-ACLR limb) for each biomechanical variable for the double-leg drop jump, single-leg drop jump, and planned and unplanned 90° CoD during stance. Reported values are mean effect sizes across phases with significant differences (P <.05), excluding phases with Cohen d <0.50, to report differences of a medium effect size or larger. Graphs for biomechanical variables with differences are displayed in Appendix A (available in the online version of this article).
To assess the ability of the results to predict ACL reinjury, logistic regressions were performed using 3 predictor variables that were chosen per the effect of the identified differences for the magnitude and symmetry analysis. Only 3 features were chosen to achieve an input to observations ratio of 1:10 to 15 to generate a model that avoided overfitting the model to the data.2,36 If a feature was multicollinear (correlation >.70) with a higher-ranked feature, it was excluded, and an additional lower ranked feature was included. Predictor variables were the average value of the phases within a biomechanical waveform that differed between groups. Before the logistic regression was fitted, predictor variables were transformed into z scores, and cohorts were balanced so that the sample sizes of the RI and NRI groups were equal. To transform a predictor variable vector x (eg, contact time: n × m, n = 88 participants, m = 1 feature) into z scores, the following equation was used:
where is the mean and S the standard deviation of the sample within x. During the fitting, data were balanced (using the synthetic minority oversampling technique)6 so that the minority class contained the same number of observations as the majority class. To interpret predictive ability of the logistic regression, receiver operating characterstic curve and prediction accuracy were reported. The area under the curve (AUC) was used in the receiver operating characterstic curve to classify findings (n = 0.50; poor, >0.60; fair, >0.70; good, >0.80), while the accuracy measure was compared with expected accuracy (ie, accuracy that would have been obtained if the most frequent class had been guessed).
RESULTS
A total of 1045 male athletes underwent primary ACL reconstruction during the enrollment period. Reinjury of the reconstructed ACL was recorded in 38 participants. Of those reinjured (constituting the RI group), 3D biomechanical analysis and PRO data were recorded for 31 participants at orthopaedic follow-up; 7 participants did not attend the testing session 6 to 9 months after surgery. A matched cohort of 57 athletes with no ACL reinjury constituted the NRI group. Anthropometric data of both groups are reported in Table 2. The mean ± SD time to ACL reinjury was 19.8 ± 8.4 months after surgery and 9.7 ± 8.9 months after RTP.
TABLE 2.
Anthropometric Dataa
| Group, No. (%) or Mean ± SD |
||
|---|---|---|
| RI (n = 31) | NRI (n = 57) | |
|
| ||
| Graft type, BPTB:HT | 21.7 ± 4.9 | 22.9 ± 4.1 |
| Mass, kg | 82.4 ± 9.5 | 81.3 ± 11.8 |
| Height, cm | 180.3 ± 6.4 | 180.0 ± 6 |
| Gaelic football | 16 (52) | 23 (40) |
| Hurling | 6 (19) | 14 (25) |
| Soccer | 5 (16) | 11 (19) |
| Rugby | 4 (13) | 9 (16) |
| Surgery to, mo | ||
| RTP | 9.6 ± 3.2 | 9.9 ± 3.0 |
| Testing | 9.1 ± 3.1 | 9.3 ± 1.2 |
| Reinjury | 19.8 ± 8.4 | NA |
| RTP to reinjury, mo | 9.7 ± 8.9 | NA |
BPTB, bone–patellar tendon–bone; HT, hamstring tendon; NA, not applicable; NRI, no reinjury; RI, reinjury; RTP, return to play.
PRO Scores
No differences were detected in IKDC, ACL-RSI, or Marx Activity Scale scores between groups (Table 3).
TABLE 3.
Differences in Patient-Reported Outcome Measuresa
| Group, Mean ± SD |
||||
|---|---|---|---|---|
| Measure | RI | NRI | P Value | Effect Size |
|
| ||||
| IKDC | 79.3 ± 11.2 | 83.3 ± 9.9 | .12 | 0.31 |
| ACL-RSI | 71.2 ± 16.2 | 77.2 ± 15.0 | .09 | 0.37 |
| Marx | 11.3 ± 3.5 | 11.1 ± 3.5 | .25 | 0.17 |
| Activity Scale | ||||
ACL-RSI, Anterior Cruciate Ligament Return to Sport After Injury questionnaire; IKDC, International Knee Documentation Committee; NRI, no reinjury; RI, reinjury.
Strength and Performance Measures
Comparison of ACLR limbs, LSI, or ≥90% LSI success rates between the RI and NRI groups across all strength, jump, and CoD scores individually and combined revealed only 1 significant difference (Table 4): with hamstring strength, ≥90% LSI success rate was significantly lower for the RI group (45%) than the NRI group (69%; P = .02). Both groups had low success rates combined across all tests (4% RI, 2% NRI). The odds of being in the NRI group when ≥90% LSI was achieved for all tests was 0.49 (95% CI, 0.03–8.15). No difference between groups was observed for CoD performance time during planned CoD on the ACLR side (1.43 ± 0.15 vs 1.42 ± 0.11 seconds; P = .81) or in LSI (99.3% ± 5.0% vs 99.3% ± 4.8%; P = .95). Similarly, no difference between groups was detected in unplanned CoD performance time on the ACLR side (1.52 ± 0.12 vs 1.52 6 0.09 seconds; P = .93) or in LSI (98.7% ± 4.6% vs 98.7% ± 4.7%; P = .92).
TABLE 4.
Comparison of Strength and Jump Performance Measures and ≥90% LSI Successa
| Ipsilateral Injury |
Ipsilateral Matched |
|||||
|---|---|---|---|---|---|---|
| Test | Mean ± SD | 95% CI | Mean ± SD | 95% CI | P Value | Effect Size |
|
| ||||||
| Quadriceps, N/kg | 198 ± 43 | 180 to 213 | 200 ± 39 | 190 to 210 | .724 | 0.08 |
| LSI, % | 89.4 ± 11.9 | 85 to 94 | 88.1 ± 13.1 | 85 to 92 | .652 | 0.10 |
| >90% LSI success rate | 52 | 47 | .644 | |||
| Hamstring, N/kg | 122.6 ± 25.1 | 113 to 132 | 127.1 ± 28.6 | 120 to 134 | .488 | 0.16 |
| LSI, % | 93 ± 14.4 | 88 to 99 | 96.5 ± 13.9 | 93 to 100 | .2745 | 0.24 |
| >90% LSI success rate | 45 | 69 | .022b | |||
| SLCMJ, cm | 9.9 ± 2.8 | 8.9 to 10.9 | 9.9 ± 2.6 | 9.2 to 10.6 | .964 | 0.01 |
| LSI, % | 85.4 ± 16.2 | 79 to 91 | 86 ± 15.8 | 82 to 90 | .875 | 0.03 |
| >90% LSI success rate | 41 | 44 | .821 | |||
| SLDJ, cm | 9.73 ± 2.8 | 8.7 to 10.8 | 9.2 ± 2.7 | 8.5 to 9.9 | .445 | 0.19 |
| LSI, % | 80.1 ± 17.9 | 73.9 to 87.8 | 76.3 ± 15.5 | 72.2 to 80.3 | .224 | 0.28 |
| >90% LSI success rate | 25 | 16 | .287 | |||
| SLHD, cm | 148.8 ± 33.8 | 135 to 162 | 142.2 ± 23.3 | 137 to 149 | .388 | 0.21 |
| LSI, % | 95.6 ± 14.6 | 89.5 to 100 | 95.7 ± 13.7 | 92.1 to 99.4 | .961 | 0.01 |
| >90% LSI success rate | 83 | 68 | .162 | |||
| >90% LSI success rate for all 4 tests | 4 | 2 | .562 | |||
LSI, limb symmetry index; NRI, no reinjury; RI, reinjury; SLCMJ, single-leg countermovement jump; SLDJ, single-leg drop jump; SLHD, single-leg hop for distance.
P < .05.
Biomechanical Analysis
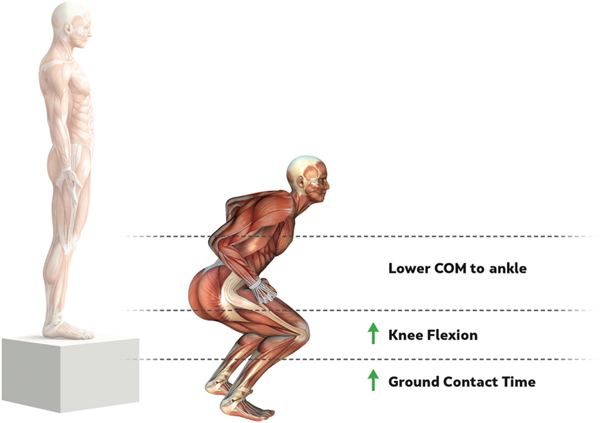
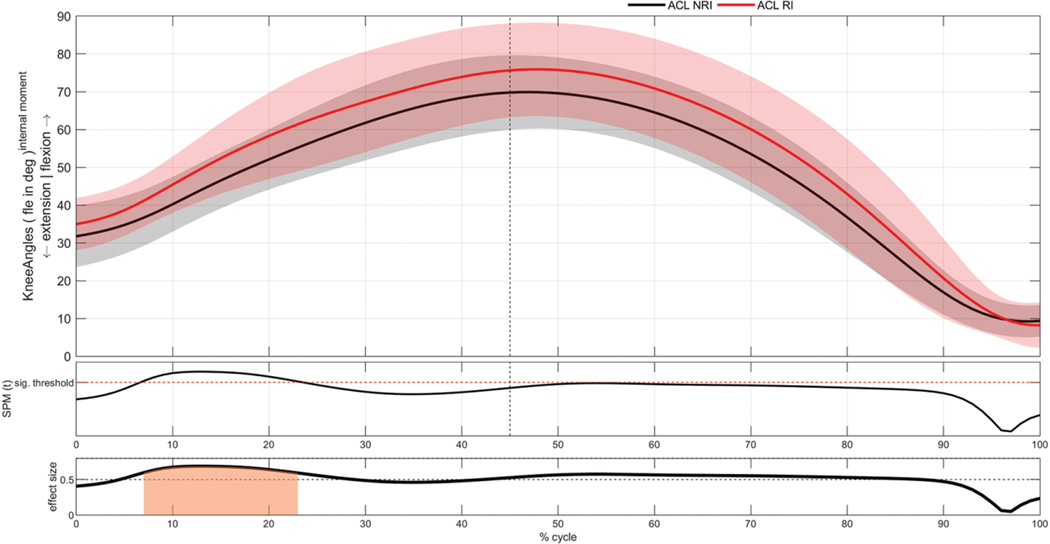
Biomechanical differences (percentage stance, effect size) on the ACLR side between the RI and NRI groups are reported in Table 5 and Figure 2. In the double-leg drop jump, there were medium effect size differences for knee flexion angle (9%−22%; effect size, 0.64) (Figure 3), vertical distance from COM to the ankle (9%−29%, d = 0.64; 49%−74%, d = 0.59), and ground contact time (d = 0.52) with more knee flexion, shorter vertical distance from COM to the ankle, and longer ground contact times in the RI group. Groups did not significantly differ for any variable within the single-leg drop jump. In the planned CoD, COM was less posterior to the knee in the RI group throughout stance (0%12%, d = 0.66; 26%−34%, d = 0.63; 54%−63%, d = 0.67; 82%−93%, d = 0.62). In the unplanned CoD, there was less anterior pelvic tilt in the RI group (42%−90%; d = 0.63). The prediction model for biomechanical variables for the double-leg drop jump selected vertical distance from COM to the ankle (9%−29%), knee flexion angle, and ground contact time for inclusion and could predict membership of the RI group with an accuracy of 61.3% (baseline, 62.5%), a sensitivity of 0.69, and a specificity of 0.47 (AUC, 0.67).
TABLE 5.
Biomechanical Differences on the ACLR Side Between the RI and NRI Groupsa
| RI Group |
NRI Group |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Start, % | End, % | Mean ± SD | 95% CI | Mean ± SD | 95% CI | P Value | Effect Size |
|
| ||||||||
| Double-leg drop jump | ||||||||
| Knee flexion angle, deg | 9 | 22 | 52.7 ± 9.7 | 49.0 to 56.4 | 47.2 ± 7.1 | 45.3 to 49.0 | .030 | 0.64 |
| COM to ankle vertical distance, mm/BH | 9 | 29 | 0.42 ± 0.02 | 0.41 to 0.43 | 0.43 ± 0.02 | 0.42 to 0.44 | .027 | 0.64 |
| 49 | 74 | 0.40 ± 0.03 | 0.39 to 0.41 | 0.42 ± 0.02 | 0.41 to 0.43 | .017 | 0.59 | |
| Ground contact time, s | 0.31 ± 0.09 | 0.27 to 0.34 | 0.26 ± 0.05 | 0.25 to 0.28 | .021 | 0.52 | ||
| Planned CoD | ||||||||
| COM to knee posterior, mm | 0 | 12 | −11.1 ± 60.3 | −34.1 to 11.8 | −60.1 ± 72.5 | −79.3 to −40.8 | .025 | 0.66 |
| 26 | 34 | 18.9 ± 56.9 | −2.7 to 40.5 | −23.3 ± 66.2 | −40.9 to −5.8 | .037 | 0.63 | |
| 54 | 63 | 66.1 ± 62.2 | 42.4 to 89.7 | 15.8 ± 74.1 | −3.8 to 35.5 | .033 | 0.67 | |
| 82 | 93 | 163 ± 68.4 | 137.1 to 189.1 | 112.6 ± 80.1 | 91.4 to 133.9 | .028 | 0.62 | |
| Unplanned CoD | ||||||||
| Anterior pelvic tilt, deg | 42 | 90 | 2.1 ± 7.0 | −0.7 to 4.8 | 7.0 ± 7.4 | 5.1 to 9.0 | .009 | 0.63 |
ACLR, anterior cruciate ligament reconstruction; BH, body height; CoD, change of direction; COM, center of mass; NRI, no reinjury; RI, reinjury.
Figure 2.
Biomechanical differences on the anterior cruciate ligament reconstruction side during the double-leg drop jump in the reinjury group as compared with the no-reinjury group illustrate longer ground contact times, greater knee flexion, and lower center of mass (COM) to the ankle.
Figure 3.
Difference in knee flexion angle on the anterior cruciate ligament (ACL) reconstruction side between the reinjury (RI) and no-reinjury (NRI) groups during the double-leg drop jump. Top panel illustrates mean and SD clouds for RI (red) and NRI (black) limbs. Middle panel illustrates SPM{t}, the t statistic as a function of time describing the difference between the groups. The dotted red line of the SPM curve indicates P < .05 and that a significant difference exists between groups. The bottom panel illustrates effect size as a function of time, describing magnitude of the effect. The dotted black line and shaded portion indicate an average Cohen d >.0.5, with orange indicating a medium effect size and a significant difference throughout that phase. There was less knee flexion in the RI group (9%−22%) with a medium effect size (0.64). fle, flexion; SPM, statistical parametric mapping.
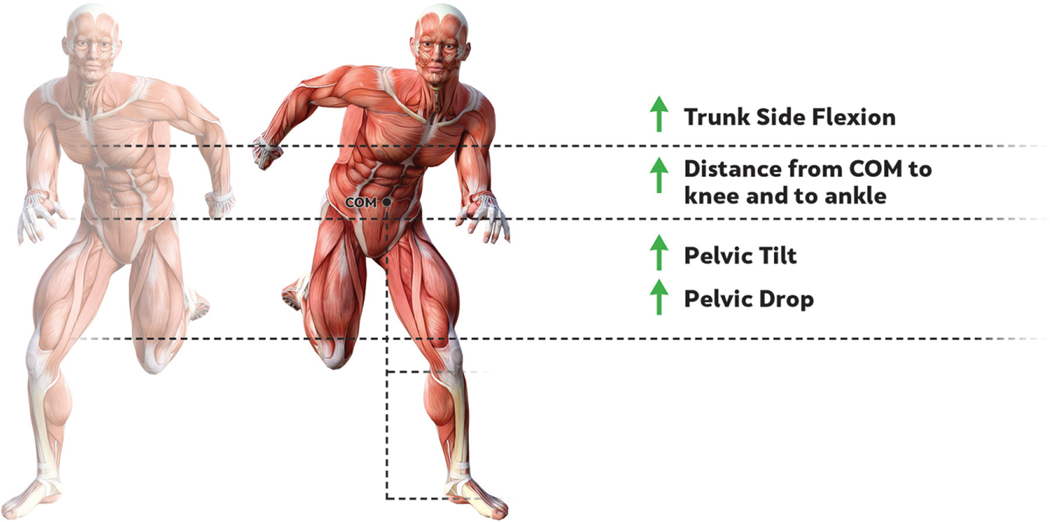
Differences in asymmetry between the groups are reported in Table 6 and Figure 4. No significant differences in asymmetry were detected in the double-leg drop jump, single-leg drop jump, and planned CoD. In the unplanned CoD, significant differences in asymmetry indicated that the RI group was more asymmetrical for COM to knee (76%−90%; d = 0.69) and ankle (12%−23%; d = 0.62), with the COM more contralateral (medial) to the knee on the ACLR side. The trunk to pelvis side flexion angle was more asymmetrical in the RI group (73%−100%; d = 0.68) toward the end of the stance phase. There also was greater asymmetry in anterior pelvic tilt in the RI group (28%−99%; d = 0.69), with less anterior pelvic tilt on the ACLR side, as well as greater asymmetry in pelvic drop (9%−36%; d = 0.61), with more pelvic drop during early stance on the ACLR side. The prediction model for symmetry of biomechanical variables during unplanned CoD selected COM to knee in the frontal plane, pelvic drop, and trunk pelvis side flexion for inclusion and could predict ACL reinjury with an accuracy of 67.7% (baseline, 59.7%), a sensitivity of 0.65, and a specificity of 0.72 (AUC, 0.75).
TABLE 6.
Biomechanical Differences Between Limbs Between the RI and NRI Groupsa
| RI |
NRI |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unplanned CoD | Start | End | Mean ± SD | 95% CI | Mean ± SD | 95% CI | P Value | Effect Size |
|
| ||||||||
| COM to knee in frontal plane, mm | 76 | 90 | 20.1 ± 42.8 | 3.2 to 37.1 | −6.9 ± 33.3 | −16.0 to 2.0 | .021 | 0.69 |
| Anterior pelvic tilt, deg | 28 | 99 | −4.9 ± 8.8 | −8.4 to −1.5 | 0.3 ± 5.6 | −1.2 to 1.8 | <.001 | 0.69 |
| Trunk to pelvis side flexion, deg | 73 | 100 | −4.9 ± 10.4 | −9.0 to −0.8 | 1.7 ± 8.7 | 1.4 to 2.1 | .029 | 0.68 |
| COM to ankle in frontal plane, mm | 12 | 23 | 38.8 ± 57.4 | 16.1 to 61.6 | 5.0 ± 49.9 | −8.5 to 18.5 | .043 | 0.62 |
| Contralateral pelvic drop, deg | 9 | 36 | 6.9 ± 7.5 | 4.0 to 9.9 | 2.6 ± 6.3 | 0.9 to 4.3 | .030 | 0.61 |
CoD, change of direction; COM, center of mass; NRI, no reinjury; RI, reinjury.
Figure 4.
Biomechanical variables with greater asymmetry during unplanned change of direction in the reinjury group as compared with the no-reinjury group illustrate greater asymmetry of trunk-side flexion, distance from center of mass (COM) to the knee and ankle in the frontal plane, pelvic tilt, and pelvic drop.
DISCUSSION
RTP criteria are used to determine rehabilitation status and reinjury risk after ACLR and frequently assess PRO, strength and jump/hop, and CoD performance measures, knee and ankle in the but movement (biomechanical) analysis is commonly absent. This study aimed to prospectively examine this combination of measures in a large cohort of male field sports athletes. This study identified differences in biomechanical measures between those who experienced reinjury and those who did not. These biomechanical differences were present in the absence of any differences between groups in commonly used and reported isokinetic strength, jump, and CoD timed performance measures, individually and combined. Biomechanical variables from individual jump and CoD tests demonstrated limited predictive ability but highlighted variables that could be targeted during rehabilitation and RTP decision making and considered in future injury prediction models.
Patient-Reported Outcomes
This study examined differences in PROs. There was no difference in IKDC, Marx Activity Scale, or ACL-RSI score between groups, suggesting that self-reported knee function, activity levels at the time of testing, and perceived readiness to RTP are not factors in reinjury risk. This is in agreement with previous research that found no difference in PROs between those who had a subsequent knee injury and those who did not after ACLR.11
Performance Measures
There was no difference between ACLR limbs or in LSI for isokinetic strength of the quadriceps or hamstrings, jump height/length, or CoD times individually or collectively between the RI and NRI groups. There was also no difference in >90% LSI success rates for all variables, with the exception of hamstring strength testing (P = .022). This difference was not evident in terms of group means, highlighting how potentially important results may be hidden in group averages.42 For the >90% LSI success rates of all tests combined, there was a lower odds of being in the NRI group (0.49), but the CI was wide (0.03–8.15). This differs from findings from Kyritsis et al,21 who reported a 4-fold increase in reinjury risk after ACLR in those not achieving >90% LSI across strength, jump, and CoD tests. The RI and NRI groups demonstrated ongoing deficits relating to <90% LSI threshold at the time of testing, consistent with previous studies demonstrating ongoing strength and jump deficits after ACLR at RTP.27,30,39,47 However, biomechanical deficits after ACLR have been demonstrated despite athletes passing >90% LSI criteria during jump and CoD tests.14,15 These results suggest that previously used performance measures of strength,21 jump, and CoD performance on the ACLR side or in measures of symmetry (LSI) may not be sufficient to identify physical deficits that may influence risk of ACL reinjury. Additional factors may need to be considered during RTP assessment or decision making.
Biomechanical Analysis
There were some biomechanical differences on the ACLR side and in symmetry between limbs between the RI and NRI groups. In the double-leg drop jump, there was increased knee flexion, shorter vertical distance from COM to the ankle, and longer ground contact times on the ACLR side for those who experienced ACL reinjury. This suggests that the RI group required longer time on the ground and more flexion/lowering of COM to absorb landing forces and then jump again during the double-leg task. This longer time to absorb load may influence knee loading on RTP, resulting in higher knee and ACL load during sports-specific activities and possibly in increased risk of ACL reinjury.5,22,39,47,48 Differences between groups in the biomechanics of planned and unplanned CoD on the ACLR side demonstrated that the COM was less posterior to the knee (planned) and had less anterior pelvic tilt (unplanned) in the RI group. A less posterior position of the COM relative to the knee has been suggested as a method to reduce the knee extension moment required during landing and deceleration31,32 and knee valgus moment during CoD.10 Combined with variables identified in the double-leg drop jump, it may reflect a difference in the ability to absorb load in the sagittal plane in those who reinjure the ACL. However, given the number of biomechanical variables analyzed in both CoD tests, the identification of a single variable of difference may hold little relevant information. Of note, external knee valgus moment (internal knee varus moment) and knee valgus angle were not different between groups in any test, despite this being reported as a risk factor in previous literature11,35 and a common mechanism of ACL injury.1,16 This difference in findings may be due to previous analyses being mostly in female athletes rather than male athletes, with female athletes more likely to demonstrate dynamic knee valgus during landing30,38 and during ACL injury.19 In addition, previous studies have often combined ipsilateral and contralateral injuries during analysis, which may have influenced outcomes.11,34,35
CoD tests revealed differences of symmetry in biomechanical measures between groups. In the unplanned CoD, there was greater between-limb difference for distance between the COM and the knee and ankle in the frontal plane in the RI group, with a greater distance (more medial) on the ACLR side. Greater step width has been suggested as a potential mechanism for ACL injury and increased knee loading, and asymmetry in strategy between limbs may increase reinjury risk in the RI group.8,17 However, it should be noted that there was large variation in asymmetry in these variables in both groups, which may be in part due to group differences but also may reflect the greater variation that may exist in a more open task, such as unplanned CoD. Additionally, there was greater asymmetry of ipsilateral trunk-pelvis lateral flexion and pelvic drop on the ACLR side in the RI group. Frontal plane control has been suggested as an important risk factor for ACL injury, and increased trunk sway during CoD has been demonstrated to increase knee loading and is a commonly reported mechanism during ACL injury.1,4,8
While previous research seeking to identify risk factors for ACL injury has focused on jumping mechanics,12,20,35 this study demonstrates that biomechanical analysis of jump and CoD movements can enhance assessment of rehabilitation status to reduce ACL reinjury risk on RTP after ACLR. Biomechanical differences between groups were found despite no differences in commonly used isokinetic peak torque strength, jump, and CoD performance measures, highlighting the potential importance of examining performance and biomechanical measures after ACLR.14,15 Biomechanical variables for the double-leg drop jump and unplanned CoD demonstrated poor predictive ability to identify those who would reinjure the ACL. Differences between those with and without reinjury were related to the ability to absorb load during the double-leg drop jump and frontal plane control during unplanned CoD. Targeting these variables during rehabilitation in male athletes returning from ACLR may reduce the incidence of reinjury but may not be able to currently predict who will go on to reinjury.3 The results of this study suggest that biomechanical variables during jump and CoD testing may play an important role in those who will experience ACL reinjury on return to high-demand multidirectional sports. These results may also offer more relevant information than the common strength and jump score tests previously used in isolation.
Limitations and Future Directions
Although ACL reinjury was tracked prospectively in a large number of participants, biomechanical data were not available for 7 of 38 patients (18%), which may have biased the results. As there is little research on prospective risk factors for ACL reinjury in male athletes, this study examined a large number of variables and tests. This increases the risk of type 1 error, although we offset this risk by setting a medium effect size threshold and reporting variables with sufficient magnitude differences. Furthermore, we included only male athletes, so future research should carry out similar analyses in female athletic populations to identify risk factors specific to that cohort and the potential differences in risk factors for male and female athletes for ACL reinjury after ACLR. In addition, those identified biomechanical variables demonstrated limited predictive ability and had large variability in some cases. Predictive accuracy may be improved by using nonlinear models, specifically exploring alternative biomechanical measures (eg, variability and coordination), and including data that are reported to influence ACL reinjury (eg, demographic, surgical, and radiological), to build a comprehensive model of factors influencing risk of second ACL injury.
CONCLUSION
This large prospective study examined differences in performance and biomechanical variables during jump and CoD testing to identify risk factors for ACL reinjury in male athletes. The RI group had no difference in IKDC, ACL-RSI, Marx Activity Scale, or commonly used strength and performance measures at 9-month follow-up compared with the NRI group. Findings demonstrated differences in biomechanical variables in the sagittal plane on the ACLR side during the double-leg drop jump and symmetry of frontal plane control during unplanned CoD with poor predictive ability. Targeting these variables during ACL rehabilitation may reduce the risk of reinjury. Future research should combine biomechanical, surgical, and demographic data to determine if these factors are involved in ACL reinjury.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Dr Neil Welch, Liz Kearns and Ciaran McFadden for their assistance in the recruitment and data collection of participants for this study. In addition, they thank Sports Surgery Clinic, Dublin, and the Gaelic Players Association for their roles in funding the study.
Footnotes
Registration: NCT02771548 (ClinicalTrials.gov identifier).
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
REFERENCES
- 1.Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contactanterior cruciate ligament injuries in soccer players, part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):705–729. [DOI] [PubMed] [Google Scholar]
- 2.Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66(3):411–421. [DOI] [PubMed] [Google Scholar]
- 3.Bahr R.Why screening tests to predict injury do not work—and probablynever will . . . : a critical review. Br J Sports Med. 2016;50(13):776–780. [DOI] [PubMed] [Google Scholar]
- 4.Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cerulli G, Benoit DL, Lamontagne M, Caraffa A, Liti A. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):307–311. [DOI] [PubMed] [Google Scholar]
- 6.Chawla N, Bowyer K, Hall L, Kegelmeyer W. SMOTE: synthetic minority over-sampling technique. J Artif Intell Res. 2002;16:321–357. [Google Scholar]
- 7.Cohen J.Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 8.Dempsey AR, Lloyd DG, Elliott BC, Steele JR, Munro BJ. Changing sidestep cutting technique reduces knee valgus loading. Am J Sports Med. 2009;37(11):2194–2200. [DOI] [PubMed] [Google Scholar]
- 9.Dingenen B, Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017;47(8):1487–1500. [DOI] [PubMed] [Google Scholar]
- 10.Donnelly CJ, Lloyd DG, Elliott BC, Reinbolt JA. Optimizing whole-body kinematics to minimize valgus knee loading during sidestepping: implications for ACL injury risk. J Biomech. 2012;45(8):1491–1497. [DOI] [PubMed] [Google Scholar]
- 11.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 13.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 14.King E, Richter C, Franklyn-Miller A, et al. Biomechanical but nottimed performance asymmetries persist between limbs 9 months after ACL reconstruction during planned and unplanned change of direction. J Biomech. 2018;81:93–103. [DOI] [PubMed] [Google Scholar]
- 15.King E, Richter C, Franklyn-Miller A, et al. Whole-body biomechanical differences between limbs exist 9 months after ACL reconstruction across jump/landing tasks. Scand J Med Sci Sports. 2018;28(12): 2567–2578. [DOI] [PubMed] [Google Scholar]
- 16.Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218–2225. [DOI] [PubMed] [Google Scholar]
- 17.Kristianslund E, Faul O, Bahr R, Myklebust G, Krosshaug T. Sidestep cutting technique and knee abduction loading: implications for ACL prevention exercises. Br J Sports Med. 2014;48(9):779–783. [DOI] [PubMed] [Google Scholar]
- 18.Kristianslund E, Krosshaug T, van den Bogert AJ. Effect of low pass filtering on joint moments from inverse dynamics: implications for injury prevention. J Biomech. 2012;45(4):666–671. [DOI] [PubMed] [Google Scholar]
- 19.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. [DOI] [PubMed] [Google Scholar]
- 20.Krosshaug T, Steffen K, Kristianslund E, et al. The vertical drop jump is a poor screening test for ACL injuries in female elite soccer and handball players: a prospective cohort study of 710 athletes. Am J Sports Med. 2016;44(4):874–883. [DOI] [PubMed] [Google Scholar]
- 21.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood ofACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 22.Lin CF, Gross M, Ji C, et al. A stochastic biomechanical model for risk and risk factors of non-contact anterior cruciate ligament injuries. J Biomech. 2009;42(4):418–423. [DOI] [PubMed] [Google Scholar]
- 23.Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining ‘‘successful outcome’’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49(5):335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marshall BM, Franklyn-Miller AD, King EA, Moran KA, Strike SC, Falvey EC. Biomechanical factors associated with time to complete a change of direction cutting maneuver. J Strength Cond Res. 2014;28(10):2845–2851. [DOI] [PubMed] [Google Scholar]
- 25.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 26.McPherson AL, Feller JA, Hewett TE, Webster KE. Smaller change inpsychological readiness to return to sport is associated with second anterior cruciate ligament injury among younger patients. Am J Sports Med. 2019;47(5):1209–1215. [DOI] [PubMed] [Google Scholar]
- 27.Mohammadi F, Salavati M, Akhbari B, Mazaheri M, Mohsen Mir S, Etemadi Y. Comparison of functional outcome measures after ACL reconstruction in competitive soccer players: a randomized trial. J Bone Joint Surg Am. 2013;95(14):1271–1277. [DOI] [PubMed] [Google Scholar]
- 28.Moudy S, Richter C, Strike S. Landmark registering waveform dataimproves the ability to predict performance measures. J Biomech. 2018;78:109–117. [DOI] [PubMed] [Google Scholar]
- 29.Narducci E, Waltz A, Gorski K, Leppla L, Donaldson M. The clinical utility of functional performance tests within one-year post-ACL reconstruction: a systematic review. Int J Sports Phys Ther. 2011;6(4):333–342. [PMC free article] [PubMed] [Google Scholar]
- 30.O’Malley E, Richter C, King E, et al. Countermovement jump and isokinetic dynamometry as measures of rehabilitation status after anterior cruciate ligament reconstruction. J Athl Train. 2018;53(7):687–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oberlander KD, Bruggemann GP, Hoher J, Karamanidis K. Reduced knee joint moment in ACL deficient patients at a cost of dynamic stability during landing. J Biomech. 2012;45(8):1387–1392. [DOI] [PubMed] [Google Scholar]
- 32.Oberlander KD, Bruggemann GP, Hoher J, Karamanidis K. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45(3):506–513. [DOI] [PubMed] [Google Scholar]
- 33.Pataky TC, Vanrenterghem J, Robinson MA. Zero- vs one-dimensional, parametric vs non-parametric, and confidence interval vs hypothesis testing procedures in one-dimensional biomechanical trajectory analysis. J Biomech. 2015;48(7):1277–1285. [DOI] [PubMed] [Google Scholar]
- 34.Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: preliminary development of a clinical decision algorithm. Orthop J Sports Med. 2017;5(12):2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. [DOI] [PubMed] [Google Scholar]
- 37.Ramsey JO. Functional Data Analysis. John Wiley & Sons; 2006. [Google Scholar]
- 38.Russell KA, Palmieri RM, Zinder SM, Ingersoll CD. Sex differences invalgus knee angle during a single-leg drop jump. J Athl Train. 2006;41(2):166–171. [PMC free article] [PubMed] [Google Scholar]
- 39.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sell TC, Ferris CM, Abt JP, et al. The effect of direction and reaction on the neuromuscular and biomechanical characteristics of the knee during tasks that simulate the noncontact anterior cruciate ligament injury mechanism. Am J Sports Med. 2006;34(1):43–54. [DOI] [PubMed] [Google Scholar]
- 41.Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):277–291. [DOI] [PubMed] [Google Scholar]
- 42.Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–1805. [DOI] [PubMed] [Google Scholar]
- 43.Thomeé R, Neeter C, Gustavsson A, et al. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):11431–151. [DOI] [PubMed] [Google Scholar]
- 44.Undheim MB, Cosgrave C, King E, et al. Isokinetic muscle strengthand readiness to return to sport following anterior cruciate ligament reconstruction: is there an association? A systematic review and a protocol recommendation. Br J Sports Med. 2015;49(20):1305–1310. [DOI] [PubMed] [Google Scholar]
- 45.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. [DOI] [PubMed] [Google Scholar]
- 46.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE,Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xergia SA, Pappas E, Zampeli F, Georgiou S, Georgoulis AD. Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2013;43(3): 154–162. [DOI] [PubMed] [Google Scholar]
- 48.Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41(suppl 1):i47–i51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.