Abstract
Objectives
Emergency ultrasound (EUS) is a critical component of emergency medicine (EM) resident education. Currently, there is no consensus list of competencies for EUS training, and graduating residents have varying levels of skill and comfort. The objective of this study was to define a widely accepted comprehensive list of EUS competencies for graduating EM residents through a modified Delphi method.
Methods
We developed a list of EUS applications through a comprehensive literature search, the American College of Emergency Physicians list of core EUS benchmarks, and the Council of Emergency Medicine Residency‐Academy of Emergency Ultrasound consensus document. We assembled a multi‐institutional expert panel including 15 faculty members from diverse practice environments and geographical regions. The panel voted on the list of competencies through two rounds of a modified Delphi process using a modified Likert scale (1 = not at all important, 5 = very important) to determine levels of agreement for each application—with revisions occurring between the two rounds. High agreement for consensus was set at >80%.
Results
Fifteen of 15 panelists completed the first‐round survey (100%) that included 359 topics related to EUS. After the first round, 195 applications achieved high agreement, four applications achieved medium agreement, and 164 applications achieved low agreement. After the discussion, we removed three questions and added 13 questions. Fifteen of 15 panelists completed the second round of the survey (100%) with 209 of the 369 applications achieving consensus.
Conclusion
Our final list represents expert opinion on EUS competencies for graduating EM residents. We hope to use this consensus list to implement a more consistent EUS curriculum for graduating EM residents and to standardize EUS training across EM residency programs.
Keywords: consensus, education, graduate medical education, point‐of‐care ultrasound, resident, ultrasound
INTRODUCTION
Emergency ultrasound (EUS) is a critical component of emergency medicine (EM) resident education. 1 , 2 Residents find EUS to be relevant to their future practice and therefore an important skill to develop in training. 3 Eighty‐eight percent of residency programs in the country have a dedicated EUS rotation. 4 Given its importance, multiple governing bodies have developed guidelines over the years to help structure how ultrasound training is implemented in graduate medical education (GME). 1 , 2 However, there is currently no unified consensus list of competencies for EUS training of residents. As EUS education and training is standardized at the fellow level through the development of the Emergency Ultrasound Fellowship Accreditation Council and the focused practice designation (FPD), it is equally important to develop a standardized process for training residents in EUS.
Multiple prior studies have evaluated methods to implement EUS education in residency programs and to assess competency. 5 , 6 , 7 In 2008, the American College of Emergency Physicians (ACEP) developed EUS policy statements to support the use of point‐of‐care ultrasound as a routine part of EM practice. 1 This was followed by the development of the Council of Emergency Medicine Residency‐Academy of Emergency Ultrasound (CORD‐AEUS) consensus guidelines for assessment and progression of EUS in 2012, coinciding with the inclusion of EUS in the Accredited Council for Graduate Medical Education (ACGME) milestones. 1 , 8 The milestones introduced minimum requirements for EUS completion, but equated the number of ultrasounds performed with competency. While the milestones recommended 150 minimum total focused EUS scans, Blehar et al. 7 determined that different types of scans required different numbers of minimums for residents to reach proficiency, ranging from 30 to 80 scans per type. Furthermore, as more programs began to implement EUS education into their curricula, the lack of standardization allowed for vast differences in the quality of training. Akhtar et al. 9 discussed the importance of implementing dedicated EUS training sessions so that residents can utilize EUS in their daily clinical practice, emphasizing that unsupervised image acquisition and interpretation alone is insufficient. Amini et al. 10 found that there is significant variation in the methods of competency assessment.
Despite the clear importance of EUS in resident education and the vast amount of literature discussing its implementation, there does not appear to be any curriculum standardization or consensus competencies. In 2021, The Milestones 2.0 Project replaced the original ACGME milestones—which eliminated the specific procedural competencies. 11 , 12 EUS, along with five other procedural milestones, were combined into one “general approach to procedures.” 11 , 12 This change gave programs autonomy in defining basic versus advanced procedures for their given context. 12 However, there is still no unifying consensus list of competencies for EUS training. Given this, graduating residents will have various degrees of exposure to EUS which could potentially lead to varying levels of skill and comfort.
The objective of this study was to define a widely accepted comprehensive list of EUS competencies for all graduating EM residents through a modified Delphi consisting of a diverse group of leaders in the ultrasound education community. We define competencies in the context of the competency‐based medical education (CBME) framework of Van Melle et al. 13 as “knowledge, attitudes, or observable behaviors which together account for the ability to deliver a specified professional service,” which originates from the landmark competency‐based curriculum development work of McGahie et al. 14
METHODS
Study design
We developed an extensive list of relevant topics within EUS using the ACEP list of ultrasound guidelines and CORD‐AEUS consensus recommendations and input from a group of educationally focused ultrasound faculty (including one program director, EUS fellowship director, and EUS director) and EUS fellows at a large academic EM residency in the central region of the United States. 3 , 8 After this, we conducted a comprehensive literature review of all clinical applications of ultrasound with the assistance of a librarian to develop a final comprehensive list of applications in Fall 2020. 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 The specific search terms are presented in Figure 1. The final list included topics such as physics and general principles as well as normal anatomy and pathology in the following categories: trauma, aorta, thoracic, cardiac, obstetrics and gynecology (OBGYN), testicular, ocular, neurology, venous, biliary, renal, soft tissue and musculoskeletal (MSK), head and neck, bowel, procedural guidance, and airway. This study was ruled exempt and not regulated by our institutional review board (HUM00197359).
FIGURE 1.
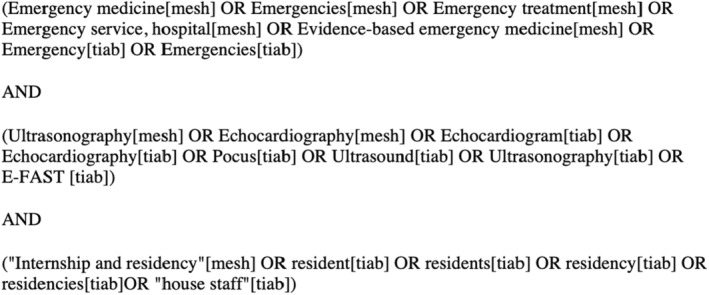
Literature search for comprehensive list of EUS competencies
Study setting and participants
We assembled a multi‐institutional expert panel of 15 faculty members from 15 programs across the country. We targeted ABEM‐certified and fellowship‐trained ultrasound experts with extensive experience in EUS education at the GME level from diverse practice environments and with varying years of experience. Panelists self‐described their practice type as community, county, academic, or a combination. Six programs had multiple designations. Our panel consisted of two former program directors, two former assistant program directors, seven current or former ultrasound directors, and nine current or former EUS fellowship directors. We used the Association of American Medical Colleges Residency Explorer tool to define each program's geographic region. Panelist demographics are described in Table 1. We used a modified Delphi technique, which was decided a priori, to rate each item in the list of EUS applications. The modified Delphi is a well‐established and theory‐driven method with validity evidence used to achieve expert opinion. 56 , 57 We created an online questionnaire of EUS applications using the Qualtrics online platform, which allowed us to send, receive, and track information from individual participants and confidentially store data. The questionnaire also allowed for experts to provide commentary regarding question clarification or general thoughts.
TABLE 1.
Panelist demographics
| Sex | |
| Female | 7 |
| Male | 8 |
| Years of experience, mean (range) | 10.63 (2–20) |
| Practice type | |
| Academic | 9 |
| Community hybrid | 1 |
| County hybrid | 5 |
| Geographic region | |
| Northeast | 5 |
| Central | 2 |
| Southern | 4 |
| Western | 4 |
Measurements and outcomes
During the first round, we asked panelists to rate how important each EUS application is for “EM residents to be able to competently perform at the time of graduation.” We utilized a 5‐point Likert scale to quantify this (1 = not very important, 2 = not important, 3 = kind of important, 4 = important, 5 = very important).
After the first round, we extracted the data from Qualtrics and generated detailed reports that we sent to the individual panelists. These reports included data for each individual EUS application such as individual panelist's response, the group mean, standard deviation (SD), and level of agreement. Levels of agreement as outlined by de Loe 58 were calculated and used to assess modified Delphi results and achieve consensus, which is a validated approach to interpret modified Delphi data. 59 Levels of agreement are broken down into high, medium, and low agreement. High agreement was defined as when >80% of responses fell on two continuous points on the 5‐point Likert scale. Medium agreement was defined as between 70% and 79.99%. Low agreement was defined as below 70%. Based on these guidelines, items qualified for inclusion in the consensus guidelines when >80% of responses were either a 4 or a 5.
After panelists received the results of the first round, we conducted two separate virtual meetings to ensure maximum participation from panelists. We also had a running online document available for meeting minutes so that those unable to attend the virtual meetings could still participate by providing commentary. Nine of 15 panelists and the three nonpanelist authors participated in the virtual meetings. The remaining six panelists were able to provide commentary on the online document asynchronously. During these meetings, panelists discussed the results of the first round of voting. They provided general opinions on the consensus list, discussed the results, and suggested changes to the survey. The discussions specifically focused on medium agreement topics, low agreement topics with high means, and high agreement topics with low means.
Data analysis
After these meetings, we revised the questionnaire to include changes from the discussion and included the group mean with each individual application. This second questionnaire was sent to panelists again using the Qualtrics online platform. After panelists completed the second questionnaire, the final results were analyzed using the above methods to assess mean, SD, and level of agreement. The applications that achieved high agreement after the second round constituted the final consensus list of applications. Medium agreement and low agreement items were eliminated from the final list.
RESULTS
The first questionnaire consisted of 359 applications of EUS. Fifteen of 15 (100%) panelists completed this initial questionnaire. A total of 195 applications achieved high agreement, four achieved medium agreement, and 160 achieved low agreement. The results are available in Data Supplement 1.
After the virtual meetings, we removed three questions and added 13 questions. We removed three questions from the pulmonary pathology section as they focused on specific medical diagnoses and replaced them with questions that focused on specific sonographic findings instead. We added questions to the following categories: pulmonary pathology, cardiac pathology, OBGYN normal anatomy, venous pathology, renal pathology, soft tissue pathology, intraoral pathology, and procedural guidance. New questions were added to broaden our scope to include additional pathologies or EUS applications.
The second questionnaire consisted of 369 applications of EUS and 100% of the panelists (15/15) completed this as well. A total of 209 applications achieved high agreement, nine achieved medium agreement, and 151 achieved low agreement. The results of the second round are available in Data Supplement 1. Our expert panel included a total of 209 EUS applications in the final consensus list of EUS applications for graduating EM residents, which are available in Table 2.
TABLE 2.
Final consensus list of EUS competencies
| General principles |
| Identifies need to accurately label images with patient information |
| Places patient in appropriate position |
| Explains the exam to be performed to the patient |
| Selects appropriate probe |
| Selects appropriate exam preset |
| Adjusts depth to adequately identify all relevant anatomy and pathology |
| Adjusts gain to appropriately identify all relevant structures and pathology |
| Assures proper cleaning of probe before and after use |
| Relays findings to patient care team |
| Appropriately documents all findings in the medical record |
| Physics |
| Identifies posterior acoustic enhancement |
| Identifies acoustic shadowing |
| Identifies mirror artifact |
| Trauma: normal anatomy |
| Identify liver |
| Identify kidney |
| Identify diaphragm |
| Identify spine |
| Identify Morison's pouch |
| Identify splenorenal space |
| Identify splenodiaphragmatic space |
| Identify paracolic gutter bilaterally |
| Identify pleural space bilaterally |
| Identify bladder in transverse and sagittal planes |
| Identify uterus in a female patient |
| Identify prostate in a male patient |
| Identify pouch of Douglas in a female patient |
| Identify rectovesicular space in a male patient |
| Identify ribs |
| Identify lung pleura |
| Identify lung sliding |
| Trauma: pathology |
| Intraabdominal hemorrhage |
| Identify the anechoic appearance of intraabdominal free fluid |
| Identify the hypoechoic/mixed echogenic appearance of clotting intraperitoneal blood |
| Identify potential spaces where intraabdominal blood can accumulate |
| Pneumothorax |
| Identify loss of lung sliding |
| Identify the appearance of the lung point |
| Pleural effusion/hemothorax |
| Identify the pleural space where pleural fluid will accumulate |
| Identify the appearance of anechoic pleural fluid |
| Identify the appearance of mixed‐echogenicity complex pleural fluid |
| Identify the spine sign |
| Aorta: normal anatomy |
| Identify aorta in transverse, sagittal, and coronal plane |
| Identify spine |
| Identify IVC |
| Identify celiac axis |
| Identify SMA |
| Identify aortic bifurcation |
| Aorta: pathology |
| Aortic aneurysm |
| Measure abdominal aorta in transverse in proximal, mid, and distal abdomen |
| Measure outer to outer wall in anterior to posterior plane |
| Measure outer to outer wall |
| Aortic dissection |
| Identify aortic dissection flap |
| Measure aortic root |
| Lung: normal anatomy |
| Identify the different zones of the lung (upper/mid/lower) |
| Identify A‐lines |
| Lung: pathology |
| Interstitial pulmonary fluid |
| Identify B‐lines |
| Identify differential for diffuse bilateral B‐line pattern |
| Identify differential for focal bilateral B‐line pattern |
| Pneumonia |
| Identify pneumonia pattern of focal B‐line appearance |
| Identify lung consolidation |
| Identify subpleural effusion |
| Cardiac: normal anatomy |
| Identify RA in apical four chamber and subxiphoid views |
| Identify RV in parasternal long, parasternal short, apical four chamber, and subxiphoid views |
| Identify LA in parasternal long, apical four chamber, and subxiphoid views |
| Identify LV in parasternal long, parasternal short, apical four chamber, and subxiphoid views |
| Identify aortic outflow tract in parasternal long and apical four chamber views |
| Identify descending thoracic aorta in parasternal long view |
| Identify mitral valve in parasternal long, parasternal short, apical four chamber, and subxiphoid views |
| Identify tricuspid valve in apical four chamber and subxiphoid views |
| Identify aortic valve in parasternal long, apical four chamber, and subxiphoid views |
| Identify papillary muscles |
| Identify pericardium |
| Identify IVC in long and short axis |
| Identify hepatic vein confluence with IVC |
| Cardiac: pathology |
| Cardiac arrest |
| Identify sonographic appearance of cardiac standstill |
| Identify sonographic appearance of ventricular fibrillation |
| Identify sonographic appearance of agonal cardiac activity |
| Decreased ejection fraction |
| Accurately characterize ejection fraction into hyperdynamic/normal/mildly depressed/moderately depressed/severely depressed using subjective interpretation of cardiac contraction |
| Cardiac tamponade |
| Identifies where pericardial fluid accumulates |
| Identifies right atrial collapse |
| Identifies right ventricular collapse |
| Identifies plethoric IVC |
| Valvular |
| Identifies vegetation on valve |
| Measures aortic root diameter |
| Volume assessment |
| Demonstrate evaluation of IVC collapsibility 2 cm inferior from the confluence of the hepatic veins |
| Identifies plethoric IVC |
| Identifies collapsed IVC |
| Elevated right heart pressure |
| Identifies the D sign |
| Identifies an increased RV:LV ratio |
| Myocardial infarction |
| Identifies the septal wall of the heart on parasternal short |
| Identifies the anterior wall of the heart on parasternal short |
| Identifies the lateral wall of the heart on parasternal short |
| Identifies the posterior wall of the heart on parasternal short |
| Identifies the inferior wall of the heart on parasternal short |
| OBGYN: normal anatomy |
| Identifies uterus in transverse axis using transabdominal approach |
| Identifies uterus in the sagittal axis using the transabdominal approach |
| Identifies uterus in the coronal axis using the transvaginal approach |
| Identifies uterus in the sagittal axis using the transvaginal approach |
| Identifies bladder |
| Identifies ovaries |
| Identifies right ovary |
| Identifies left ovary |
| Identifies pouch of Douglas |
| Identifies endometrial stripe |
| Identifies cervix |
| First‐trimester intrauterine pregnancy |
| Identifies gestational sac |
| Identifies yolk sac |
| Identifies fetal pole |
| Identifies fetal heart rate |
| Measure fetal heart rate using M‐mode |
| Performs crown–rump length measurement to estimate gestational age |
| OBGYN: pathology |
| Ovarian cyst |
| Identifies echogenic fluid in the cul‐de‐sac |
| Ectopic pregnancy |
| Identifies empty uterus in setting of positive pregnancy test |
| Identifies pseudo‐gestational sac in setting of positive pregnancy test |
| Identifies yolk sac/fetal pole in a nonuterine location |
| Identifies free fluid in the pouch of Douglas |
| Identifies free fluid in Morison's pouch |
| Testicular: normal anatomy |
| Identifies testicle |
| Ocular: normal anatomy |
| Identifies anterior chamber |
| Identifies posterior chamber |
| Identifies pupil |
| Identifies lens |
| Identifies optic nerve sheath |
| Ocular: pathology |
| Posterior chamber |
| Identifies vitreous hemorrhage |
| Identifies vitreous detachment |
| Identifies retinal detachment |
| Distinguishes vitreous from retinal detachment via visualization of optic nerve sheath |
| Demonstrates dynamic evaluation of the eye via patient eye movement |
| Other |
| Identifies globe rupture |
| Venous: normal anatomy |
| Identifies greater saphenous vein |
| Identifies common femoral vein |
| Identifies deep femoral vein |
| Identifies superficial femoral vein |
| Identifies popliteal vein |
| Identifies popliteal trifurcation (anterior tibial, posterior tibial, peroneal) |
| Venous: pathology |
| DVT |
| Identifies compressibility of a normal vessel |
| Identifies lack of compressibility in the setting of a DVT |
| Performs compression at areas of venous bifurcation |
| Identifies presence of DVT in lower extremity |
| Biliary: normal anatomy |
| Identifies liver |
| Identifies gallbladder in long axis |
| Identifies gallbladder in short axis |
| Identifies portal triad |
| Identifies portal vein |
| Identifies hepatic artery |
| Identifies common bile duct |
| Biliary: pathology |
| Gallstones |
| Identifies gallstones |
| Identifies gallstone characteristics of echogenicity, shadowing, and mobility |
| Identifies WES sign (wall–echo–shadow) |
| Identifies gallbladder sludge |
| Cholecystitis |
| Identifies pericholecystic fluid |
| Identifies increase size of gallbladder wall |
| Measures anterior gallbladder wall in short axis |
| Identifies sonographic Murphy's sign |
| Choledocholithiasis/cholangitis |
| Identifies enlarged common bile duct |
| Measures common bile duct |
| Renal: normal anatomy |
| Identifies renal cortex |
| Identifies renal medulla |
| Identifies renal pelvis |
| Identifies ureter |
| Identifies bladder |
| Renal: pathology |
| Identifies mild hydronephrosis |
| Identifies moderate hydronephrosis |
| Identifies severe hydronephrosis |
| Identifies mimics of hydronephrosis |
| Uses color to differentiate hydronephrosis from vasculature |
| MSK: normal anatomy |
| Identifies muscle appearance |
| Identifies tendon appearance |
| Identifies peripheral nerve appearance ‐ anisotropy |
| Identifies peripheral nerve apperance ‐ hyperechoic honeycomb |
| Identifies normal appearance of dermis |
| Identifies appearance of lymph node |
| Identifies bone as hyperechoic line in longitudinal and transverse planes |
| MSK: pathology |
| General |
| Identifies joint dislocation |
| Identifies joint effusion |
| Soft tissue |
| Identifies cobblestoning |
| Identifies other causes of cobblestoning—lymphedema/edema |
| Identifies appearance of abscess |
| Identifies air echoes as sign of necrotizing fasciitis |
| Identifies foreign objects in subcutaneous tissue |
| Shoulder |
| Identifies humeral head |
| Identifies glenoid |
| Knee |
| Identifies patella |
| Identifies femur |
| Identifies tibia |
| Identifies patellar tendon |
| Ankle |
| Identifies Achilles tendon |
| Identifies Achilles tendon rupture |
| Head and neck |
| Identifies appearance of peritonsillar abscess using endocavitary probe |
| Bowel: pathology |
| SBO |
| Identifies to and fro peristalsis as sign of SBO |
| Procedures |
| Needle guidance |
| Identifies and tracks needle in long axis |
| Identifies and tracks needle tip in short axis |
| Identifies important nearby structures |
| Confirms location of guidewire within vessel |
| Confirms location of catheter within vessel |
| Correctly identifies appropriate vessel |
| Correctly identifies size and location of vessel |
| Identifies back‐walling of needle or guidewire in vessel |
| Identifies needle going through and through vessel |
| Fluid drainage |
| Identifies anechoic or hypoechoic fluid pocket |
| Procedures |
| Can place internal jugular CVC under ultrasound guidance |
| Can place femoral vein CVC under ultrasound guidance |
| Can place radial arterial line under ultrasound guidance |
| Can cannulate vessel in short and long axis |
| Can place femoral arterial line under ultrasound guidance |
| Can perform thoracentesis under ultrasound guidance |
| Can perform paracentesis under ultrasound guidance |
| Can perform paracentesis with ultrasound assistance |
| Can perform arthrocentesis under ultrasound guidance |
| Can perform pericardiocentesis under ultrasound guidance |
| Can perform nerve blocks under ultrasound guidance |
| Can place peripheral venous line under ultrasound guidance |
Abbreviations: CVC, central venous catheter; DVT, deep venous thrombosis; IVC, inferior vena cava; LA, left atrium; LV, left ventricle; MSK, musculoskeletal; OBGYN, obstetrics and gynecology; RA, right atrium; RV, right ventricle; SBO, small bowel obstruction; SMA, superior mesenteric artery.
The topics included in the final list are general principles, physics, normal trauma anatomy and trauma pathology, normal aorta and aorta pathology, normal lung and lung pathology, normal cardiac and cardiac pathology, normal OBGYN and OBGYN pathology, normal testicular anatomy, normal ocular and ocular pathology, normal venous anatomy and venous pathology, normal biliary and biliary pathology, normal renal and renal pathology, normal MSK and MSK pathology, head and neck pathology, bowel pathology, and procedures. Organ systems with no elements in the final list were neurology, airway ultrasound, normal bowel anatomy, and testicular pathology.
DISCUSSION
Our comprehensive list includes elements of all the core EUS applications from both the ACEP EUS guidelines and the CORD‐AEUS consensus document. 1 , 8 Adjunct applications from the ACEP EUS guidelines that overlapped included advanced echo, small bowel obstruction (SBO), adnexal pathology, and testicular pathology. 1 Our list expanded on these core topics to include specific details outlining normal anatomy and pathology, with the aim of providing a more comprehensive list that better informs institutions on what topics to include in an EUS curriculum. It is not surprising that our list includes more EUS topics than the CORD‐AEUS consensus document from 2011. 8 While both projects aimed to define expectations for graduating EM residents, the footprint of ultrasound within EM has changed dramatically over the past decade. Every year, the EM workforce includes a higher percentage of working emergency physicians for whom EUS was a required part of their EM residency curriculum. Additionally, the field of EUS itself has changed—a decade ago EUS was relatively new to EM when compared to topics long included in the EM scope of practice. Today, EM physicians have a pathway to an ABEM FPD in advanced emergency ultrasonography. The increasing number of topics our study generated may be due to a natural maturation and expansion of EUS. As with many aspects of medicine, what was once cutting edge has become routine.
Conversely, it is not surprising that some elements included within the ACEP EUS guidelines and the CORD‐AEUS consensus document failed to make our consensus list, as the aim of our study is fundamentally different. The ACEP guidelines describe the potential scope of ultrasound use within the clinical practice of EM. Our goal was to define a minimum expected EUS competency for EM residents graduating from an ACGME‐accredited training program at time of graduation. Our exclusion of bowel ultrasound (other than SBO), transesophageal echo, contrast‐enhanced ultrasound, and transcranial Doppler is not a break from the ACEP guidelines, but rather a recognition that competency in these specific EUS applications may require additional focus and training within or after residency. Furthermore, the exclusion of these applications and other advanced skills from the CORD‐AEUS consensus document is consistent with the goal of our project to define a list of EUS competencies for all graduating EM residents—as competency in such advanced topics is likely to require participation in advanced tracks or additional training opportunities that may not be available to all EM residents.
Our panel did not include pediatric EM–trained physicians, which may explain why bowel pathologies outside of SBO did not meet consensus criteria for inclusion—as the use of ultrasound to diagnose intussusception, appendicitis, and pyloric stenosis is more prevalent in pediatric populations. This may also reflect the challenge of performing sufficient pediatric ultrasound studies to develop competency, which is a challenge faced even by pediatric EM fellows who spend their clinical time in the pediatric environment. 60
The organ systems included in our consensus list represent the most common types of exams completed in the emergency department. 61 A recurring theme during our discussion was the consistent expectation that residents should be able to recognize the absence of normal anatomy and function as opposed to specific pathologic diagnoses. Residents are expected to recognize basic anatomy so that they do not overcall normal variants or normal findings as pathology. Furthermore, the general consensus was that residents should not be expected to specifically identify all of these abnormalities but should instead recognize that an abnormality exists and appropriately follow up with further imaging, consultation, or additional workup. While our procedures section specifically listed individual procedures, we did not specifically mention individual regional nerve blocks and instead chose to include an all‐encompassing question because previous studies have already defined an ultrasound guided regional nerve block curriculum using a modified Delphi technique. 62
Our Delphi group had a robust discussion about the physics topics included in our questionnaire. Unsurprisingly, ultrasound experts considered understanding of common artifacts to be an important and clinically relevant skill for EM residents to avoid misdiagnosing artifacts as pathology and to also recognize normal anatomy accurately. There was significant discussion on whether the recognition of artifact alone was sufficient, compared to the true understanding of the physics behind it, with the group's opinion being split evenly on the matter. Side lobe artifact and aliasing both did not reach consensus, despite the panel agreeing they were important topics to be familiar with.
There was a lengthy discussion regarding the importance of teaching transvaginal ultrasound (TVUS) at the resident level. While the questionnaire did not specify image acquisition and interpretation via transabdominal or transvaginal approach, the panel agreed that it was important for residents to be able to recognize images obtained via TVUS, but not necessarily expected that residents would perform high volumes of TVUS during their residency. This led to the important conversation of utilizing simulation for rare sonographic findings or pathologies when clinical practice was not sufficient in providing these experiences. Where programs cannot support a robust simulation curriculum, they can instead utilize structured online courses and the vast number of free open‐access medical education resources such as podcasts, blog posts, instructional videos, etc. Another interesting finding was that residents were expected to identify the presence of lower extremity deep venous thrombosis (DVTs) but not upper‐extremity DVTs, potentially due to the complexity in diagnosing upper extremity DVTs, the controversial management, and the fact that they are less prevalent.
Topics that were excluded from the final list include testicular pathology, normal bowel anatomy, neurology, and airway ultrasound. While normal testicular anatomy was included, testicular pathology did not reach consensus. Our questions specifically asked if residents could identify hydroceles, varicoceles, epididymitis, orchitis, or hernias. If we instead phrased the questions as recognizing presence of fluid or inflammation, this may have led to higher agreement and possible inclusion into the consensus list. This is likely related to the recurring theme that recognition of absence of normal is more important than diagnosing specific abnormalities. In line with this theme, we likely did not include any normal bowel anatomy given that it is more important to recognize presence or absence of dilated loops of bowel than it is to be able to identify specific anatomic structures of normal bowel.
The neurology section specifically focused on spinal anatomy and lumbar punctures, and the consensus was that use of ultrasound for lumbar puncture was not essential. Finally, airway anatomy was not included, and discussion among panelists was that ultrasound use in airway management was not a resident‐level expectation but rather a fellow‐level skill. There was commentary that recognizing airway structures was important so that one recognizes what structures to avoid during needle insertion for central line access. Comments from the Round 2 survey mainly focused on question phrasing and rewording certain topics, but there were no significant additions or changes included.
Our consensus list serves as an initial benchmark for graduating residents. Future studies could explore both in theory and in practice how these competencies fit into the broader CBME framework. 13 The CBME framework includes five core components: outcome competencies, progressive sequencing of competencies, tailored learning experiences, competency‐focused teaching instruction, and programmatic assessment. 13 This study provides a list of outcome competencies satisfying the first of the five core components. Further work could be done to sequence these, develop and implement learning experiences for learners to achieve these competencies, develop teaching practices to promote the development of these competencies, and to develop a programmatic assessment piece to support and document the developmental acquisition of these competencies in resident learners. Future studies could also explore additional outcomes after implementation of a curriculum to teach to these competencies—such as changes in number of scans completed, scans billed, and number of confirmatory studies ordered after benchmark implementation. Patient‐centered outcomes such as changes in management could also be considered.
LIMITATIONS
Despite our comprehensive literature search with the help of a librarian, our consensus list may not have been exhaustive. By allowing panelists to provide suggestions during the survey and during our discussion, we attempted to maximize the number of topics included. Additionally, attempting to include an exhaustive and large list of items for our expert panel to address in each round may have contributed to survey fatigue and decreased attention to detail in responses compared to a smaller list of items.
There are inherent limitations to using Delphi panels due to the potential for bias. We attempted to mitigate this by including a diverse group of panelists from various geographic locations, practice environments, years of experience, and institutional roles. However, our panel of experts may not have been representative of all residency programs throughout the country. We did have representation from a mix of community, county, and academic programs. However, our panel predominantly came from academic programs, which may not fully represent the opinion on training at exclusively community or county sites. Given this, certain EUS applications that did not reach consensus may be more important to programs where ultrasound techs or consultants are not as readily available. Conversely, if our expert panel does not adequately represent the community or county consensus, there may be some items included in the final list that certain programs may not find as useful. Furthermore, our panel consisted mostly of programs that support an EUS fellowship, and since residents complete more scans when an EUS fellowship is present at their program, this introduces another bias toward the breadth of competencies selected. 63
While some of our ultrasound faculty are involved in program leadership, we did not include non–ultrasound‐trained program directors, department chairs, residents, or others who may have interest in resident ultrasound training as they were less likely to have predictable knowledge or experience developing an EUS curriculum for residents. Pediatric emergency medicine (PEM) faculty representation was also not included in this process. Future work could examine EUS items pertinent to PEM at the resident or fellow level.
While this study focused on developing a consensus list of EUS competencies, this consensus list requires further validation and feasibility testing. This can be accomplished by developing curricula using this list and obtaining learner and faculty feedback. There may be barriers to implementing and evaluating a curriculum based on this extensive set of competencies depending on resources available at an individual residency program. Potential barriers include limitations in dedicated time for EUS education, adequate number of machines to scan on shift, faculty with EUS training and comfort teaching the above topics, and the ability to supplement clinical learning with simulation for more rare pathologies or clinical presentations.
CONCLUSIONS
In summary, our final consensus list represents expert opinion on emergency ultrasound competencies for graduating emergency medicine residents. We hope to use this consensus list as a guide for programs to develop a more consistent and robust emergency ultrasound curriculum for future graduating emergency medicine residents and to standardize residency emergency ultrasound training across a diverse group of emergency medicine training programs.
AUTHOR CONTRIBUTIONS
David A. Haidar, William J. Peterson, and Rob D. Huang proposed goals and designed the study. William J. Peterson provided advice on study design and data analysis. David A. Haidar, Rob D. Huang, and Patrick G. Minges contributed to data collection. David A. Haidar and William J. Peterson obtained institutional review board approval and exemption. David A. Haidar, Rob D. Huang, and William J. Peterson developed survey. Patrick G. Minges, Jennifer Carnell, Jason T. Nomura, John Bailitz, Jeremy S. Boyd, Megan M. Leo, E. Liang Liu, Youyou Duanmu, Josie Acuña, Ross Kessler, Marco F. Elegante, Mathew Nelson, Rachel B. Liu, Resa E. Lewiss, and Arun Nagdev all completed surveys and participated in discussion and revision of survey along with David A. Haidar, Rob D. Huang, and William J. Peterson. David A. Haidar and William J. Peterson analyzed the data. David A. Haidar, William J. Peterson, and Rob D. Huang drafted manuscript and prepared the tables and figures. All listed authors contributed substantially to the editing of the manuscript and conduct of this study. David A. Haidar takes responsibility of corresponding author.
CONFLICT OF INTEREST
JC provides consulting services for Caption Health, Inc. JTN provides consulting services for Philips Healthcare and reports grant money from BMS to conduct research. JB reports grant money from Caption Health, Inc. to conduct research. RBL provides consulting services for Philips Healthcare, Caption Health, Inc., and Butterfly Network, Inc. REL provides consulting services for Echonous. The other authors declare no potential conflict of interest.
Supporting information
Appendix S1
ACKNOWLEDGMENTS
The authors acknowledge and thank the ultrasound faculty and fellows who helped develop the initial comprehensive list of ultrasound applications, including Nik Theyyunni, Ryan Tucker, Chris Fung, Helena Wang‐Flores, Nicole Klekowski, and Douglas Stayer. We also acknowledge and thank Tyler Nix, who assisted with the comprehensive literature search and development of the specific search terms.
Haidar DA, Peterson WJ, Minges PG, et al. A consensus list of ultrasound competencies for graduating emergency medicine residents. AEM Educ Train. 2022;6:e10817. doi: 10.1002/aet2.10817
Presented at the SAEM Western Regional Meeting, Palo Alto, CA, April 2022, and the Society for Academic Emergency Medicne Annual Meeting, New Orleans, LA, May 2022.
Supervising Editor: Dr. Sally Santen
REFERENCES
- 1. American College of Emergency Physicians . Emergency ultrasound guidelines. Ann Emerg Med. 2009;53(4):550‐570. [DOI] [PubMed] [Google Scholar]
- 2. Beeson MS, Ankel F, Bhat R, et al. The 2019 Model of the Clinical Practice of Emergency Medicine. J Emerg Med. 2020;59(1):96‐120. doi: 10.1016/j.jemermed.2020.03.018 [DOI] [PubMed] [Google Scholar]
- 3. Stolz LA, Stolz U, Fields JM, et al. Emergency medicine resident assessment of the emergency ultrasound milestones and current training recommendations. Acad Emerg Med. 2017;24(3):353‐361. doi: 10.1111/acem.13113 [DOI] [PubMed] [Google Scholar]
- 4. Gottlieb M, Arno K, Kuhns M, Chan TM. Distribution of clinical rotations among emergency medicine residency programs in the United States. AEM Educ Train. 2018;2(4):288‐292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alerhand S, Situ‐Lacasse E, Ramdin C, Gottlieb M. National survey of point‐of‐care ultrasound scholarly tracks in emergency medicine residency programs. West J Emerg Med. 2021;22(5):1095‐1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nelson M, Abdi A, Adhikari S, et al. Goal‐directed focused ultrasound milestones revised: a multiorganizational consensus. Acad Emerg Med. 2016;23(11):1274‐1279. doi: 10.1111/acem.13069 [DOI] [PubMed] [Google Scholar]
- 7. Blehar DJ, Barton B, Gaspari RJ. Learning curves in emergency ultrasound education. Acad Emerg Med. 2015;22(5):574‐582. doi: 10.1111/acem.12653 [DOI] [PubMed] [Google Scholar]
- 8. Lewiss RE, Pearl M, Nomura JT, et al. CORD‐AEUS: consensus document for the emergency ultrasound milestone project. Acad Emerg Med. 2013;20(7):740‐745. [DOI] [PubMed] [Google Scholar]
- 9. Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound: consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med. 2009;16(Suppl 2):S32‐S36. [DOI] [PubMed] [Google Scholar]
- 10. Amini R, Adhikari S, Fiorello A. Ultrasound competency assessment in emergency medicine residency programs. Acad Emerg Med. 2014;21(7):799‐801. doi: 10.1111/acem.12408 [DOI] [PubMed] [Google Scholar]
- 11. Beeson MS, Carter WA, Christopher TA, et al. Emergency medicine milestones. J Grad Med Educ. 2013;5(1 Suppl 1):5‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cooney RR, Murano T, Ring H, Starr R, Beeson MS, Edgar L. The Emergency Medicine Milestones 2.0: setting the stage for 2025 and beyond. AEM Educ Train. 2021;5(3):e10640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Van Melle E, Frank JR, Holmboe ES, et al. A core components framework for evaluating implementation of competency‐based medical education programs. Acad Med. 2019;94(7):1002‐1009. [DOI] [PubMed] [Google Scholar]
- 14. McGaghie WC, Miller GE, Sajid AW, Telder TV. Competency‐based curriculum development on medical education: an introduction. Public Health Pap. 1978;68:11‐91. [PubMed] [Google Scholar]
- 15. Murphy JT, Hall J, Provost D. Fascial ultrasound for evaluation of anterior abdominal stab wound injury. J Trauma. 2005;59(4):843‐846. [DOI] [PubMed] [Google Scholar]
- 16. Hatemi AC, Omay O, Baskurt M, Kücükoglu S, Öz B, Süzer K. Mobile atheromatous plaque of the aortic arch diagnosed by transthoracic echocardiography prior to coronary artery bypass surgery. Which one would you choose: scepticism or wishful thinking? Cardiovasc J Afr. 2012;23(4):e3‐e5. [DOI] [PubMed] [Google Scholar]
- 17. Chenkin J, Hockmann E, Jelic T. Simulator‐based training for learning resuscitative transesophageal echocardiography. CJEM. 2019;21(4):523‐526. doi: 10.1017/cem.2019.13 [DOI] [PubMed] [Google Scholar]
- 18. Colony MD, Edwards F, Kellogg D. Ultrasound assisted evaluation of chest pain in the emergency department. Am J Emerg Med. 2018;36(4):533‐539. doi: 10.1016/j.ajem.2017.09.003 [DOI] [PubMed] [Google Scholar]
- 19. Stolz LA, Mosier JM, Gross AM, Douglas MJ, Blaivas M, Adhikari S. Can emergency physicians perform common carotid Doppler flow measurements to assess volume responsiveness? West J Emerg Med. 2015;16(2):255‐259. doi: 10.5811/westjem.2015.1.24301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yin WH, Chen Y, Jin XD, et al. Measurement of peak velocity variation of common carotid artery with bedside ultrasound to estimate preload in surgery ICU. Sichuan Da Xue Xue Bao Yi Xue Ban. 2013;44(4):624‐628. Chinese. [PubMed] [Google Scholar]
- 21. Ehrman RR, Russell FM, Ansari AH, et al. Can emergency physicians diagnose and correctly classify diastolic dysfunction using bedside echocardiography? Am J Emerg Med. 2015;33(9):1178‐1183. doi: 10.1016/j.ajem.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 22. Mulvagh SL, Rakowski H, Vannan MA, et al. American Society of Echocardiography Consensus Statement on the Clinical Applications of Ultrasonic Contrast Agents in Echocardiography. J Am Soc Echocardiogr. 2008;21(11):1179‐1201. quiz 1281. [DOI] [PubMed] [Google Scholar]
- 23. Jang TB, Kaji AH. A 2‐week elective experience provides comparable training as longitudinal exposure during residency for pelvic sonography. J Ultrasound Med. 2015;34(2):221‐224. [DOI] [PubMed] [Google Scholar]
- 24. Levin DC, Parker L, Sunshine JH, Busheé G, Merritt CR. Role of emergency medicine physicians in US performed in patients in the emergency department: how substantial is their participation? Radiology. 2000;216(1):265‐268. [DOI] [PubMed] [Google Scholar]
- 25. Arnold MJ, Jonas CE, Carter RE. Point‐of‐care ultrasonography. Am Fam Physician. 2020;101(5):275‐285. [PubMed] [Google Scholar]
- 26. Dimassi K, Douik F, Ajroudi M, Triki A, Gara MF. Ultrasound fetal weight estimation: how accurate are we now under emergency conditions? Ultrasound Med Biol. 2015;41(10):2562‐2566. doi: 10.1016/j.ultrasmedbio.2015.05.020 [DOI] [PubMed] [Google Scholar]
- 27. Shah S, Adedipe A, Ruffatto B, et al. BE‐SAFE: bedside sonography for assessment of the fetus in emergencies: educational intervention for late‐pregnancy obstetric ultrasound. West J Emerg Med. 2014;15(6):636‐640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blaivas M, Sierzenski P, Lambert M. Emergency evaluation of patients presenting with acute scrotum using bedside ultrasonography. Acad Emerg Med. 2001;8(1):90‐93. [DOI] [PubMed] [Google Scholar]
- 29. Chandra A, Mastrovitch T, Ladner H, Ting V, Radeos MS, Samudre S. The utility of bedside ultrasound in the detection of a ruptured globe in a porcine model. West J Emerg Med. 2009;10(4):263‐266. [PMC free article] [PubMed] [Google Scholar]
- 30. Shafé M, Blaivas M, Hooker E, Straus L. Noninvasive intracranial cerebral flow velocity evaluation in the emergency department by emergency physicians. Acad Emerg Med. 2004;11(7):774‐777. [DOI] [PubMed] [Google Scholar]
- 31. Farahmand S, Safavi S, Shahriarian S, Arbab M, Basirghafoori H, Bagheri‐Hariri S. Preferred view and transducer in lumbar ultrasound in overweight and obese patients. Ultrasound. 2017;25(1):45‐52. doi: 10.1177/1742271X16689590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Halm BM. Diagnosis of an acute lobar nephronia in the emergency department using point‐of‐care ultrasound. J Emerg Med. 2019;57(2):227‐231. doi: 10.1016/j.jemermed.2019.04.030 [DOI] [PubMed] [Google Scholar]
- 33. Bozkurt O, Ersel M, Karbek Akarca F, Yalcinli S, Midik S, Kucuk L. The diagnostic accuracy of ultrasonography in determining the reduction success of distal radius fractures. Turk J Emerg Med. 2018;18(3):111‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rushton WF, Vakkalanka JP, Moak JH, Charlton NP. Negative predictive value of excluding an embedded snake foreign body by ultrasonography. Wilderness Environ Med. 2015;26(2):227‐231. doi: 10.1016/j.wem.2014.12.015 [DOI] [PubMed] [Google Scholar]
- 35. Hill R, Conron R, Greissinger P, Heller M. Ultrasound for the detection of foreign bodies in human tissue. Ann Emerg Med. 1997;29(3):353‐356. [DOI] [PubMed] [Google Scholar]
- 36. Boswell B, Farrow R, Rosselli M, et al. Emergency medicine resident‐driven point of care ultrasound for suspected shoulder dislocation. South Med J. 2019;112(12):605‐609. [DOI] [PubMed] [Google Scholar]
- 37. Lyon M, Blaivas M. Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. Acad Emerg Med. 2005;12(1):85‐88. [DOI] [PubMed] [Google Scholar]
- 38. Wyrick DL, Smith SD, Dassinger MS. Surgeon as educator: bedside ultrasound in hypertrophic pyloric stenosis. J Surg Educ. 2014;71(6):896‐898. doi: 10.1016/j.jsurg.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 39. Patiño AM, Cantillo‐Campos S, Kearney AS, Kivlehan SM, Maldonado A. Emergency medicine challenges in ecuador. West J Emerg Med. 2020;21(6):284‐290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rice J, Crichlow A, Baker M, et al. An assessment tool for the placement of ultrasound‐guided peripheral intravenous access. J Grad Med Educ. 2016;8(2):202‐207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chaudery M, Clark J, Morrison JJ, Wilson MH, Bew D, Darzi A. Can contrast‐enhanced ultrasonography improve Zone III REBOA placement for prehospital care? J Trauma Acute Care Surg. 2016;80(1):89‐94. [DOI] [PubMed] [Google Scholar]
- 42. Lavingia KS, Soult MC, Collins JN, Novosel TJ, Weireter LJ, Britt LD. Basic ultrasound training can replace chest radiography for safe tube thoracostomy removal. Am Surg. 2014;80(8):783‐786. [PubMed] [Google Scholar]
- 43. Anderson ES, Hodell E, Mantuani D, Fahimi J, Pampalone I, Nagdev A. Pilot study of ultrasound‐guided corticosteroid hip injections by emergency physicians. West J Emerg Med. 2014;15(7):919‐924. doi: 10.5811/westjem.2014.9.20575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim HM, So BH, Jeong WJ, Choi SM, Park KN. The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center. Scand J Trauma Resusc Emerg Med. 2012;12(20):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Taylor LA, Vitto MJ, Joyce M, Tozer J, Evans DP. Ultrasound‐guided thoracostomy site identification in healthy volunteers. Crit Ultrasound J. 2018;10(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Park S, Lee S, Do HH, Kim JS, Seo JS. Effectiveness of limited airway ultrasound education for medical students: a pilot study. Clin Exp Emerg Med. 2019;6(3):257‐263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Das D, Kapoor M, Brown C, Ndubuisi A, Gupta S. Current status of emergency department attending physician ultrasound credentialing and quality assurance in the United States. Crit Ultrasound J. 2016;8(1):6. doi: 10.1186/s13089-016-0042-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hossein‐Nejad H, Mehrjerdi MS, Abdollahi A, et al. Ultrasound for intubation confirmation: a randomized controlled study among emergency medicine residents. Ultrasound Med Biol. 2021;47(2):230‐235. doi: 10.1016/j.ultrasmedbio.2020.10.012 [DOI] [PubMed] [Google Scholar]
- 49. Lahham S, Baydoun J, Bailey J, et al. A prospective evaluation of transverse tracheal sonography during emergent intubation by emergency medicine resident physicians. J Ultrasound Med. 2017;36(10):2079‐2085. doi: 10.1002/jum.14231 [DOI] [PubMed] [Google Scholar]
- 50. Barbe N, Martin P, Pascal J, Heras C, Rouffiange P, Molliex S. Locating the cricothyroid membrane in learning phase: value of ultrasonography? Ann Fr Anesth Reanim. 2014;33(3):163‐166. doi: 10.1016/j.annfar.2014.01.006 [DOI] [PubMed] [Google Scholar]
- 51. Chenkin J, McCartney CJ, Jelic T, Romano M, Heslop C, Bandiera G. Defining the learning curve of point‐of‐care ultrasound for confirming endotracheal tube placement by emergency physicians. Crit Ultrasound J. 2015;7(1):14. doi: 10.1186/s13089-015-0031-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hosseini JS, Talebian MT, Ghafari MH, Eslami V. Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci. 2013;3(2):113‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gildea TH, Anderson KL, Niknam KR, et al. The utility of color doppler to confirm endotracheal tube placement: a pilot study. West J Emerg Med. 2020;21(4):871‐876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bothwell J, Skinner C, Della‐Giustina D, Kang C, Cookman L, Laselle B. Impact of decontamination therapy on ultrasound visualization of ingested pills. West J Emerg Med. 2014;15(2):176‐179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Buonsenso D, Chiaretti A, Curatola A, Morello R, Giacalone M, Parri N. Pediatrician performed point‐of‐care ultrasound for the detection of ingested foreign bodies: case series and review of the literature. J Ultrasound. 2021;24(1):107‐114. doi: 10.1007/s40477-020-00452-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hauer KE, Kohlwes J, Cornett P, et al. Identifying entrustable professional activities in internal medicine training. J Grad Med Educ. 2013;5(1):54‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wijnen‐Meijer M, van der Schaaf M, Nillesen K, Harendza S, Ten Cate O. Essential facets of competence that enable trust in graduates: a delphi study among physician educators in The Netherlands. J Grad Med Educ. 2013;5(1):46‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. de Loe RC. Exploring complex policy questions using the policy Delphi. Appl Geogr. 1995;15:53‐68. [Google Scholar]
- 59. van der Schaaf MF, Stokking KM. Construct validation of content standards for teaching. Scand J Educ Res. 2011;55:273‐289. [Google Scholar]
- 60. Gold D, Levine M, Hsu D, et al. Design of a point‐of‐care ultrasound curriculum for pediatric emergency medicine fellows: a Delphi study. AEM Educ Train. 2021;5(4):e10700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Michalke JA. An overview of emergency ultrasound in the United States. World J Emerg Med. 2012;3(2):85‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Tucker RV, Peterson WJ, Mink JT, et al. Defining an ultrasound‐guided regional anesthesia curriculum for emergency medicine. AEM Educ Train. 2020;5(3):e10557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Adhikari S, Raio C, Morrison D, et al. Do emergency ultrasound fellowship programs impact emergency medicine residents' ultrasound education? J Ultrasound Med. 2014;33(6):999‐1004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


