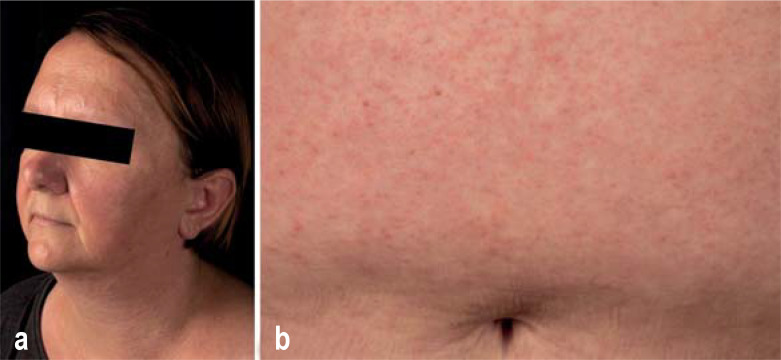
A 47-year-old woman presented with a 3-day history of maculopapular exanthema, facial edema, temperature spikes of up to 38.5 °C, fatigue, and right-sided upper abdominal pain (figure). Three weeks earlier she had started taking gradually increasing doses of sulfasalazine (most recently 2 g/day) to treat unclassified arthritis. Laboratory tests showed abnormal leukocytosis (26.49/nl), CRP (24.0 mg/l), eosinophilia (2.92/nl), and transaminases (GOT 134, GPT 166, GGT 237 U/l). Sonography revealed hepatosplenomegaly. We diagnosed sulfasalazine-induced DRESS syndrome (drug rash with eosinophilia and systemic symptoms), a rarely occurring severe systemic drug reaction associated with reactivation of human herpesviruses (75% of cases). HHV6 DNA was detected in the patient’s blood. The disease mostly becomes evident 2–8 weeks after the initiation of antiepileptics, allopurinol, antibacterial sulfonamides, minocycline, or vancomycin. Facial edema occurs in 70% of cases, and its presence in patients with drug-induced exanthema should prompt consideration of DRESS. The mortality is 2–10%. Danger was averted by immediate discontinuation of sulfasalazine and high-dose glucocorticoid treatment.
Figure.
a) Facial edema b) Maculopapular skin lesions on the abdomen
Cite this as: Ramcke T, Enk A, Hoffmann J: Facial edema as a sign of a rare severe drug reaction.
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement:
The authors declare that no conflict of interest exists.