Abstract
Patient: Female, 61-year-old
Final Diagnosis: Schwannoma
Symptoms: Low back pain with radiation • unsteady gait
Medication: —
Clinical Procedure: Laminectomy • thoracic magnetic resonance imaging
Specialty: Chiropractic • Neurosurgery
Objective:
Rare disease
Background:
Sciatica, which is pain radiating along the sciatic nerve distribution, is most often caused by degenerative conditions of the lower back and rarely results from lesions of the spinal cord. This case report illustrates a patient with suspected lumbar radiculopathy, ultimately diagnosed with a thoracic schwannoma after visiting a chiropractor.
Case Report:
A 61-year-old woman presented to a chiropractor with progressively worsening lower back pain radiating to the right lower extremity and unsteady gait. Her symptoms began 10 years previously and she had been diagnosed by an orthopedist with lumbar disc herniation causing radiculopathy via magnetic resonance imaging (MRI) and was treated with physical therapy and diclofenac. Upon examination by the chiropractor, the patient had bilateral lower-extremity neurologic deficits, hyperreflexia, and upgoing Babinski responses. The chiropractor ordered thoracic MRI, but the patient preferred to initiate a trial of care, which was unsuccessful. After a delay imposed by cardiac bypass surgery, the patient returned to the chiropractor with worsened symptoms and underwent thoracic MRI, revealing an intraspinal mass at T9. The patient underwent laminectomy and tumor removal, with histopathology confirming a diagnosis of schwannoma. The patient gradually improved after surgery with the help of rehabilitative exercises.
Conclusions:
Clinicians should suspect a spinal cord lesion as a cause of sciatic pain when patients fail to improve with treatment, have a broad sensorimotor distribution unexplained by lumbar imaging findings, hyperreflexia/pathological reflexes, or other atypical findings (eg, negative neural tension tests). In such cases, MRI of the cervical and thoracic spine may be indicated.
Keywords: Chiropractic, Low Back Pain, Neurilemmoma, Sciatica, Spinal Cord Diseases
Background
Sciatica is any pain along the course and distribution of the sciatic nerve, which runs along the posterior thigh and supplies sensation to much of the leg and foot [1]. Sciatica is most often caused by degenerative lumbar spine conditions such as disc herniation and stenosis, which affect 1 or more nerve roots, causing radiculopathy [2]. Rarely, sciatica is caused by conditions affecting the spinal cord (ie, myelopathy) [3,4]. Sciatic pain arising from the spinal cord presents a diagnostic challenge, as the clinical features can mimic those of common degenerative lumbar conditions [3,5].
Sciatica caused by myelopathy, sometimes referred to as cordonal sciatica [3,5], is extremely rare, accounting for less than 1% of all cases of sciatica. In a study of 252 patients referred to a spine surgery center for low back pain, only 2 patients (0.8%) were ultimately diagnosed with myelopathy [6]. In a study of 609 patients with low back and leg pain, only 1 patient had myelopathy (0.2%) [2]. Reviews on the topic of cordonal sciatica have found that most cases result from a neo-plastic etiology, followed by degenerative conditions such as disc herniation and degenerative cervical myelopathy [3,7,8]. In either event, sciatic symptoms are believed to arise due to compression of the spinothalamic tract or dorsal columns [3,8].
Sciatica arising from myelopathy is often misdiagnosed, with a diagnostic interval ranging from months to several years [3,9]. In some instances, patients undergo surgery for a degenerative lumbar spine finding that was presumed to explain their symptoms, and a neoplastic etiology is only identified later after the patient fails to improve [9]. Apart from a lack of response to lumbar surgery [9], clinical features of cordonal sciatica may include a sensory distribution that spans multiple dermatomes, negative (ie, painless) neural tension test results, or symptoms that are exacerbated at night [5].
According to a large study using United States (US) data, spinal cord tumors have an incidence of 0.59 cases per 100 000 people (95% CI: 0.58–0.61) [10]. The most common types of primary spinal cord tumors are schwannoma, meningioma, and ependymoma [11]. Such tumors are most often diagnosed after age 30 years, at a mean of 52 years of age [11].
Chiropractors have been described as primary spine care providers [12], considering they most often provide care for patients with low back and/or neck pain [13]. Importantly, spinal neoplasms are considered a contraindication or precaution to chiropractic spinal manipulative therapy, a treatment commonly utilized by these providers [14,15]. Although there is limited research on this subject, previous case reports have documented exacerbation of undiagnosed spinal neoplasms or spinal cord lesions with this treatment [16].
Considering that spinal cord tumors may cause pain resembling common degenerative lumbar spine conditions and prompt patients to seek chiropractic care, we present a case of a woman with chronic low back pain who was ultimately found to have a thoracic cord schwannoma after visiting a chiropractor.
Case Report
Patient Information
A 61-year-old woman with a history of hypertension, hyperlipidemia, hypothyroidism, osteoporosis, and gastroesophageal reflux disease presented with a 6-month history of progressively worsening lower back pain radiating to the right gluteal region, posterior and lateral thigh, anterolateral leg, and entire foot, and an unsteady gait. She reported her low back pain and stiffness were aggravated when waking up in the morning and rated her current pain severity a 7/10 on an 11-point numeric pain rating scale. Her World Health Organization Quality of Life (WHOQOL) score was 64%.
The patient was currently taking pantoprazole (40 milligrams [mg]), clopidogrel (75 mg), atorvastatin, aspirin 80 mg, metoprolol tartrate 50 mg, thyroxine (100 micrograms [mcg]), glyceryl trinitrate (500 mcg), and baclofen (10 mg), and received a denosumab injection (60 mg) every 6 months. She was a non-smoker, social drinker, and had no family history of cancer or spinal disorders. A review of systems was notable for fatigue and occasional angina, but she denied any neck pain or upper-extremity symptoms, bowel or bladder disturbances, recent weight loss, shortness of breath, or dizziness. The patient was a non-smoker, non-drinker, and had a family history of cardiovascular disease in both parents. She was a retired insurance manager.
The patient’s symptoms began insidiously 10 years prior to presenting to the chiropractor, causing her to visit an orthopedic surgeon, who ordered magnetic resonance imaging (MRI) of the lumbar region. The orthopedist diagnosed the patient with lumbar disc herniation and prescribed a nonsteroidal anti-inflammatory drug (diclofenac) and referred her for physical therapy. The patient also sought out acupuncture on her own. Each of these therapies provided temporary relief. However, at the time, her low back and lower-extremity symptoms were only mild to moderate in severity.
Three years prior to presenting to the chiropractor, the patient tripped, causing a fracture of her right tibia, which required open reduction and internal fixation. After the surgery, she had difficulty walking and required the use of a cane. She noted tightness, stiffness, and weakness of her lower extremities, mostly affecting the right lower extremity, and numbness of the right foot, which caused her to trip and stumble. She also noted progressive worsening of her posture.
Two weeks prior to presenting to the chiropractor, the patient returned to the orthopedist noting a 6-month history of worsening lower-extremity symptoms, gait difficulty, and severe low back pain. This provider ordered another lumbar MRI, which revealed a disc bulge at L4/5 and disc herniation at L5/S1, both left-sided and involving annular fissures (Figure 1). The orthopedist also ordered a cervical spine MRI, which revealed mild degenerative changes (Figure 2). The provider diagnosed the patient with lumbar disc herniation and degenerative cervical spondylosis, and again prescribed diclofenac and referred her to physiotherapy. The patient sought a chiropractor for another opinion.
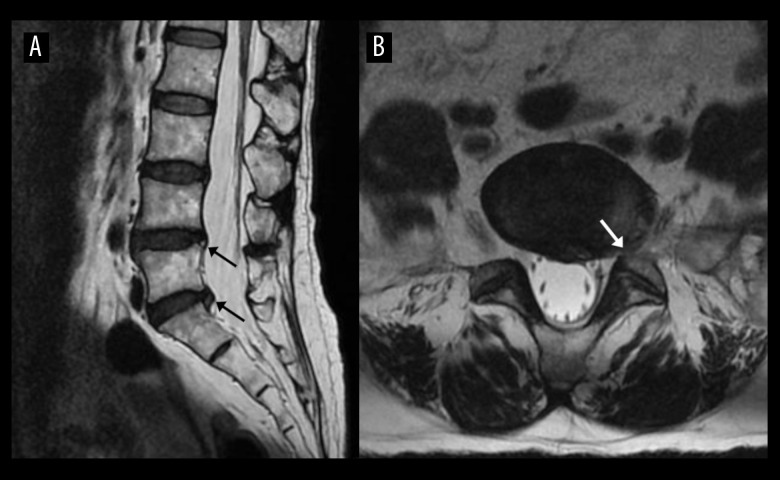
Figure 1.
Lumbar spine magnetic resonance imaging 2 weeks prior to the patient’s chiropractic visit. The sagittal (A) T2-weighted image shows disc displacements with radial fissures at L4/5 and L5/S1 (arrows). The axial T2-weighted image (B) highlight a disc displacement at L5–S1 (arrow). The L5/S1 disc displacement was interpreted by a board-certified medical radiologist as a broad-based disc protrusion from the posterocentral to left foraminal region and was noted to contain an abnormal T2 hyperintense annular signal consistent with annular fissure.
Figure 2.

Cervical spine magnetic resonance imaging showing mild degenerative changes. This mid-sagittal T2-weighted sequence shows mild disc protrusions at C4/5 and C5/6 (arrows) causing mild cervical canal stenosis without cervical cord compression.
Clinical Findings
Upon examination by the chiropractor, the patient walked with a cane and had a visibly unsteady gait. She was of an average build, slightly overweight, and had no obvious muscle atrophy in the torso or extremities. Her low back pain was exacerbated by active lumbar flexion, which was limited to 50 degrees (normal: 60). Palpation identified muscle hypertonicity and tenderness of the quadratus lumborum and lumbar paraspinal muscles bilaterally. Spinal motion palpation identified intersegmental restriction with tenderness at T3/4, T9/10, and L4/5. Supine and seated straight leg raising did not increase the patient’s symptoms. A neurological examination revealed diminished motor strength of hip flexion and knee extension bilaterally (grade 4/5, Medical Research Council scale), 4+ muscle stretch reflexes of the Achilles bilaterally with non-sustained clonus, bilateral upgoing plantar reflexes (Babinski response), and diminished sensation to pinwheel and cotton ball diffusely in the right leg and foot. The patient struggled to sit up from the supine position, suggesting a deficiency of abdominal muscle strength, but side plank and back extension endurance were not tested.
The chiropractor considered a diagnosis of myelopathy given the patient’s hyperreflexia, bilateral lower-extremity neurologic deficits, gait abnormality, and negative neural tension test results. Lumbar radiculopathy was also considered given the left-sided L4/5 and L5/S1 disc displacements, but the chiropractor recognized that the lumbar spine findings would be inconsistent with the patient’s lower-extremity symptoms, which were predominantly right-sided. Discogenic pain related to annular tears was also considered, but annular tears do not typically cause lower-extremity weakness [17]. The chiropractor recommended a thoracic MRI, but the patient refused, as she felt it was unnecessary given her extensive history of MRI and recent evaluation by an orthopedic surgeon. The patient instead requested to receive treatment, and the chiropractor and patient reached a mutual agreement to initiate a brief trial of care.
Chiropractic treatment began at a frequency of 3 visits per week for 3 weeks. Treatments included thermal ultrasound therapy to alleviate lumbar muscle hypertonicity, spinal manipulative therapy performed using a drop table, which is a mechanism allowing part of the cushioned table to quickly release to a lower position, allowing the chiropractor to provide an impulse, at the sacral base and pelvis to alleviate low back pain, and intermittent mechanical spinal traction (MID Series, WIZ Medical, Korea) applied to the lumbar region to decompress the L4/5 and L5/S1 disc displacements. Traction sessions lasted 20 minutes per visit and used a traction force of 50% of the patient’s body weight and ratio of hold to rest time of 2: 1. The patient noted transient relief from low back pain, which reduced to 4/10 in severity following treatments for a few hours. At a follow-up examination on the 9th visit, the patient’s neurological symptoms, examination findings, and walking ability were unchanged.
Given the lack of improvement and signs of upper motor neuron lesion, the chiropractor again recommended thoracic MRI, and the patient consented. However, the patient developed progressively worsening angina and visited her cardiologist, who recommended cardiac catheterization. This testing revealed significant coronary artery stenosis, and the patient underwent non-emergent cardiovascular bypass surgery. Accordingly, MRI for the spinal and lower-extremity concerns was delayed. After undergoing coronary bypass surgery, the patient required the use of a wheelchair for 3 months before transitioning to a cane.
The patient returned to the chiropractor 5 months after cardiac bypass surgery. Her WHOQOL score had worsened to 52%. On examination, there was a worsening of lower-extremity weakness, which now included grade 4/5 dorsiflexion and great toe extension bilaterally in addition to the deficits previously identified. The chiropractor again considered the possibility of myelopathy, ordered cervical and thoracic MRI, and urgently referred the patient to an orthopedic surgeon given the patient’s worsening status.
The patient’s cervical spine MRI was relatively unremarkable and re-demonstrated the mild canal stenosis that was shown previously. However, thoracic MRI identified a 1.2×0.9×3.4-centimeter (cm; transverse x anteroposterior x craniocaudal) intradural, extramedullary intraspinal mass extending from T9 to T10 with an associated mass effect displacing and compressing the spinal cord (Figure 3). Upon seeing these findings, the orthopedic surgeon referred the patient to a neurosurgeon.
Figure 3.
Thoracic spine magnetic resonance imaging showing an intraspinal mass. Sagittal T1-weighted (A) and T2-weighted (B) images show a mass extending from T9 to T10 with associated significant compression of the spinal cord. No extension to the neuroforamina or associated bony scalloping or bony erosion is seen.
Three weeks later, the neurosurgeon operated on the patient. The neurosurgeon performed a laminectomy at T9 and removed the schwannoma using microscopic magnification, with intra-operative somatosensory and motor evoked potential monitoring throughout the procedure. The neurosurgeon incised the dura mater and dissected the schwannoma from the surrounding structures, totally removing it in 2 pieces, the first piece measuring 2.7×1.0×1.0 cm and the second measuring 0.7×0.5×0.3 cm. Subsequently, the neurosurgeon discharged the patient to recover at home with postoperative pain medications (acetaminophen, tramadol).
The tumor specimen was sent for histological examination. Although high-quality pathology images were unavailable upon request, the report indicated that microscopically the specimen was consistent with a well-circumscribed schwannoma, featuring proliferation of bland short spindle or comma-shaped cells forming vague fascicles or palisades. Also noted were loosely dispersed spindle cells within the microcystic stroma. Within the tumor there were thick-walled blood vessels and scattered foamy histiocytes. The spindle cells showed scanty cytoplasm and bland darkly stained nuclei. There was no mitotic activity or necrosis, cellular dysplasia, or evidence of malignancy.
Within a week following surgery, the patient noted that her lower-extremity sensation began to return. The surgeon referred the patient for a 3-month course of post-surgical physiotherapy, which she supplemented with home rehabilitative exercises using exercise bands.
The patient returned to the chiropractor 6 months following surgery. At this time, her WHOQOL score had improved to 80%. She could now walk with a cane, but still reported lower-extremity weakness. On examination by the chiropractor, her hip extension, dorsiflexion, and great toe extension were graded 4/5 strength bilaterally, while her other motor deficits had normalized.
The chiropractor recommended continued care, focusing on rehabilitation, which the patient attended twice per week for a span of 3 months. Treatments included 30-minute sessions of focused electromagnetic field therapy (Emsculpt®, BTL, USA; [18]) to passively trigger muscle contractions in the rectus abdominis, internal and external obliques, and transversus abdominis. Core muscle function and endurance were also targeted using an apparatus in which the patient remained seated, while it slowly moved to different angles of inclination and rotation, with each session lasting 10 minutes (Allcore 360°, USA; [19]). The patient also exercised for 10-minute sessions, using a back extension machine and exercise bike (Biocircuit, Technogym, USA).
Nine months after surgery, upon re-examination by the chiropractor, the patient’s WHOQOL score had improved to 94%, she demonstrated improved gait and posture, no longer required the use of a cane, and her strength deficits had normalized. She noted ongoing residual mild thoracolumbar pain and occasional brief episodes of lower-extremity numbness and mild weakness, but these symptoms did not limit her activities of daily living. There were no treatment-related adverse events reported.
Discussion
This case report describes a woman with chronic low back pain and sciatica initially ascribed to degenerative lumbar findings, and ultimately diagnosed as thoracic schwannoma after visiting a chiropractor. In the current case, the diagnosis was made after the chiropractor ordered thoracic MRI after recognizing a discordance between the patient’s imaging findings and clinical features, which included neurological deficits of both lower extremities despite only unilateral lumbar disc displacements, and no imaging findings consistent with cervical myelopathy.
Similar cases of cordonal sciatica have been published, including cases resulting from benign cord tumors such as meningiomas and schwannomas [7,8]. In one such case, a 72-year-old man presented with acute low back pain radiating to the lower extremity after a fall, and underwent MRI, which showed a schwannoma at T9 [7]. In another case, a 37-year-old man presented with subacute lower-extremity sensorimotor concerns, which were initially ascribed to lumbar disc displacement, but additional thoracic MRI revealed a schwannoma at T7/8 [20].
Previous cases have also described that degenerative lumbar spine findings can lead clinicians to overlook underlying spinal neoplasms. In situations, as in the current case, patients may have symptoms for several months or over a year before receiving a diagnosis of spinal neoplasm [9]. The current case is unusual in that the correct diagnosis was only reached after visiting a chiropractor, rather than a medical physician. To the best of our knowledge, reports of chiropractors identifying intraspinal tumors have only rarely been reported in the literature [21–26].
Many variables can contribute to delayed diagnosis of cordonal sciatica. Degenerative changes in the lumbar spine are highly prevalent in the older population, yet these are not necessarily predictive of symptoms [27,28]. Dermatomal sensory patterns are not highly specific [29], and thus may be misleading. Further, clinicians may suspect that tandem stenosis (eg, combination of degenerative cervical and lumbar findings) [30] could explain symptoms rather than an isolated finding in the lumbar or cervical spine.
Imaging tests for sciatic pain typically begin with the lumbar spine, but such tests may fail to identify causes of cordonal sciatica, which typically occur in the cervical or thoracic region [7,8]. Accordingly, providers should consider imaging the cervical and/or thoracic spine for patients with sciatic symptoms unresponsive to care, upper motor neuron findings, or imaging findings that do not correlate with the patient’s symptoms or examination findings [5,7,8].
This case report has certain limitations. While the chiropractor in the current case utilized spinal manipulative therapy, the authors wish to emphasize that this treatment is potentially unsafe for those with spinal neoplasms [14–16]. Fortunately, spinal manipulations were provided away from the site of the thoracic schwannoma and the patient suffered no adverse events in relation to this treatment. Reaching an accurate diagnosis in this case was delayed by several years and further delayed after presenting to the chiropractor, in part due to a necessary cardiac surgery. However, the diagnosis of thoracic schwannoma may have been accelerated if the chiropractor further encouraged the patient to undergo early thoracic MRI or concluded the trial of care sooner.
Conclusions
This case report illustrates that providers should suspect a spinal cord lesion when patients with sciatica fail to respond to treatment, have widespread symptoms discordant with lumbar spine imaging findings, hyperreflexia, or other atypical features such as negative neural tension test results. In such patients, MRI of the thoracic and cervical spine may be warranted.
Footnotes
Department and Institution Where Work Was Done
New York Chiropractic and Physiotherapy Centre, EC Healthcare, Kowloon, Hong Kong.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Sweetman BJ. The words we use: Where did lumbago and sciatica come from? Int Musculoskelet Med. 2011;33(1):30–33. [Google Scholar]
- 2.Konstantinou K, Dunn KM, Ogollah R, et al. ATLAS Study Research Team Characteristics of patients with low back and leg pain seeking treatment in primary care: Baseline results from the ATLAS cohort study. BMC Musculoskelet Disord. 2015;16:332. doi: 10.1186/s12891-015-0787-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Florez G. [Sciatica and lumbosciatica of extradiscal origin.] Rev Esp Cir Ost. 1976;11:203–21. [in Spanish] [Google Scholar]
- 4.Kulcu DG, Naderi S. Differential diagnosis of intraspinal and extraspinal non-discogenic sciatica. J Clin Neurosci. 2008;15:1246–52. doi: 10.1016/j.jocn.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Postacchini F, Trasimeni G. Differential diagnosis I Organic diseases Lumbar Disc Herniation. Springer; 1999. pp. 293–318. [Google Scholar]
- 6.Tortolani PJ, Carbone JJ, Quartararo LG. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. Spine J. 2002;2:251–54. doi: 10.1016/s1529-9430(02)00198-5. [DOI] [PubMed] [Google Scholar]
- 7.Okimatsu S, Furuya T, Maki S, et al. Thoracic dumbbell-shaped spinal tumor with contralateral lower extremity pain: A case report. Chiba Med J. 2020;96:67–71. [Google Scholar]
- 8.Sasaoka R, Nakamura H, Yamano Y. Idiopathic spinal cord herniation in the thoracic spine as a cause of intractable leg pain: Case report and review of the literature. J Spinal Disord Tech. 2003;16:288–94. doi: 10.1097/00024720-200306000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Börm W, Gleixner M, Klasen J. Spinal tumors in coexisting degenerative spine disease – a differential diagnostic problem. Eur Spine J. 2004;13(7):633–38. doi: 10.1007/s00586-004-0678-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duong LM, McCarthy BJ, McLendon RE, et al. Descriptive epidemiology of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors, United States, 2004–2007. Cancer. Wiley Online Library. 2012;118:4220–17. doi: 10.1002/cncr.27390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirano K, Imagama S, Sato K, et al. Primary spinal cord tumors: Review of 678 surgically treated patients in Japan. A multicenter study. Eur Spine J. 2012;21:2019–26. doi: 10.1007/s00586-012-2345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy DR, Justice B, Bise CG, et al. The primary spine practitioner as a new role in healthcare systems in North America. Chiropr Man Ther. 2022;30:6. doi: 10.1186/s12998-022-00414-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beliveau PJH, Wong JJ, Sutton DA, et al. The chiropractic profession: A scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Ther. 2017;25:35. doi: 10.1186/s12998-017-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chu E. WHO guidelines on basic training and safety on chiropractic. Geneva: 2005. [Google Scholar]
- 15.Laoudikou MT, McCarthy PW. Patients with cancer. Is there a role for chiropractic? J Can Chiropr Assoc. 2020;64:32. [PMC free article] [PubMed] [Google Scholar]
- 16.Hebert JJ, Stomski NJ, French SD, Rubinstein SM. Serious adverse events and spinal manipulative therapy of the low back region: A systematic review of cases. J Manipulative Physiol Ther. 2015;38:677–91. doi: 10.1016/j.jmpt.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Peng B, Wu W, Li Z, et al. Chemical radiculitis. Pain. 2007;127:11–16. doi: 10.1016/j.pain.2006.06.034. [DOI] [PubMed] [Google Scholar]
- 18.Kinney BM, Lozanova P. High intensity focused electromagnetic therapy evaluated by magnetic resonance imaging: Safety and efficacy study of a dual tissue effect based non-invasive abdominal body shaping. Lasers Surg Med. 2019;51:40–46. doi: 10.1002/lsm.23024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palevo G, Walsh DJ, Park E, et al. Physiological responses to Allcore360 [degrees] core training system. J Exerc Physiol Online. 2021;24:67–74. [Google Scholar]
- 20.Ukaigwe A, Olugbodi A, Alweis RL. Taking it to the next level: Lumbar radiculopathy from thoracic nerve schwannoma. J Community Hosp Intern Med Perspect. 2015;5:25744. doi: 10.3402/jchimp.v5.25744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chu E, Trager R. Prevalence of serious pathology among adults with low back pain presenting for chiropractic care: A retrospective chart review of integrated clinics in Hong Kong. Med Sci Monit Int Med J Exp Clin Res. 2022;28:e938042. doi: 10.12659/MSM.938042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cox JM, Alter M. Schwannoma: Challenging diagnosis. J Manipulative Physiol Ther. 2001;24:526–28. doi: 10.1067/mmt.2001.118203. [DOI] [PubMed] [Google Scholar]
- 23.Cho JCS, Miller A, Kettner NW. Cervical ependymoma in a male adolescent with neck and back pain. J Manipulative Physiol Ther. 2009;32:695–700. doi: 10.1016/j.jmpt.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 24.Lensgraf AG, Young KJ. Ependymoma of the spinal cord presenting in a chiropractic practice: 2 case studies. J Manipulative Physiol Ther. 2006;29:676–81. doi: 10.1016/j.jmpt.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 25.O’Shaughnessy J, Bussières A. Subtle clinical signs of a spinal cord ependymoma at the cervicothoracic level in an adult: A case report. J Can Chiropr Assoc. 2006;50:244. [PMC free article] [PubMed] [Google Scholar]
- 26.Rodgers AM, Khauv KB. Thoracic schwannoma in an adult male presenting with thoracic pain: A case report. J Chiropr Med. 2017;16:242–45. doi: 10.1016/j.jcm.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brinjikji W, Diehn F, Jarvik J, et al. MRI findings of disc degeneration are more prevalent in adults with low back pain than in asymptomatic controls: A systematic review and meta-analysis. Am J Neuroradiol. 2015;36:2394–99. doi: 10.3174/ajnr.A4498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suri P, Boyko EJ, Goldberg J, et al. Longitudinal associations between incident lumbar spine MRI findings and chronic low back pain or radicular symptoms: retrospective analysis of data from the longitudinal assessment of imaging and disability of the back (LAIDBACK) BMC Musculoskelet Disord. 2014;15:1. doi: 10.1186/1471-2474-15-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tawa N, Rhoda A, Diener I. Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: A systematic literature review. BMC Musculoskelet Disord. 2017;18:93. doi: 10.1186/s12891-016-1383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Overley SC, Kim JS, Gogel BA, et al. Tandem spinal stenosis: A systematic review. JBJS Rev. 2017;5:e2. doi: 10.2106/JBJS.RVW.17.00007. [DOI] [PubMed] [Google Scholar]