Abstract
Rationale
The associations between the number of COVID-19 cases/deaths and subsequent uptake of protective behaviors may reflect cognitive and behavioral responses to threat-relevant information.
Objective
Applying protection motivation theory (PMT), this study explored whether the number of total COVID-19 cases/deaths and general anxiety were associated with cross-situational handwashing adherence and whether these associations were mediated by PMT-specific self-regulatory cognitions (threat appraisal: perceived vulnerability, perceived illness severity; coping appraisal: self-efficacy, response efficacy, response costs).
Method
The study (#NCT04367337) was conducted in March–September 2020 among 1256 adults residing in 14 countries. Self-reports on baseline general anxiety levels, handwashing adherence across 12 situations, and PMT-related constructs were collected using an online survey at two points in time, four weeks apart. Values of COVID-19 cases and deaths were retrieved twice for each country (one week prior to the individual data collection).
Results
Across countries and time, levels of adherence to handwashing guidelines were high. Path analysis indicated that smaller numbers of COVID-19 cases/deaths (Time 0; T0) were related to stronger self-efficacy (T1), which in turn was associated with higher handwashing adherence (T3). Lower general anxiety (T1) was related to better adherence (T3), with this effect mediated by higher response efficacy (T1, T3) and lower response cost (T3). However, higher general anxiety (T1) was related to better adherence via higher illness severity (T1, T3). General anxiety was unrelated to COVID-19 indicators.
Conclusions
We found a complex pattern of associations between the numbers of COVID-19 cases/deaths, general anxiety, PMT variables, and handwashing adherence at the early stages of the pandemic. Higher general anxiety may enable threat appraisal (perceived illness severity), but it may hinder coping appraisal (response efficacy and response costs). The indicators of the trajectory of the pandemic (i.e., the smaller number of COVID-19 cases) may be indirectly associated with higher handwashing adherence via stronger self-efficacy.
Keywords: Handwashing, COVID-19, Anxiety, Protection motivation theory
1. Introduction
1.1. Background
Hand hygiene has been promoted as a cornerstone of infection control during the COVID-19 pandemic (Beale et al., 2020), with fluctuations in COVID-19 morbidity/mortality levels related to changes in hand hygiene adherence. Our 14-country, cross-sectional study of 6064 adults conducted from March to July 2020 indicated that self-reported adherence to the World Health Organization's handwashing guidelines (2020) was negatively related to the accumulation of cases and deaths due to COVID-19 (Szczuka et al., 2021). Longitudinal research using data from automated hand hygiene monitoring systems in hospitals showed an increase in the level of adherence during the first months of the pandemic, followed by a reduction in adherence as the pandemic continued and the total number of COVID-19 cases was increasing (Makhni et al., 2021). Longitudinal data showed an overall decline in COVID-19 protective behaviors as the total number of cases was increasing across 2020 (Petherick et al., 2021). The associations between protective behaviors and COVID-19 morbidity/mortality levels may reflect cognitive and behavioral responses to threat-relevant information such that awareness of the number of national cases or deaths from COVID-19 could reduce (or raise) self-protective behaviors via changes in threat-related cognitions (Petherick et al., 2021).
Health behavior theories, such as protection motivation theory (PMT; Norman et al., 2015; Rogers, 1975), suggest that to prevent an illness, people change their behavior as a result of threat appraisal and coping appraisal, both of which contribute to behavioral intention (i.e., the proximal determinant of an action). Threat appraisal combines (1) perceived illness severity (i.e., the magnitude of noxiousness/severity of an illness) and (2) perceived vulnerability to being infected (i.e., the likelihood that the illness will occur if no protective behavior is adopted; Norman et al., 2015; Rogers, 1975). Fear related to threat appraisal also contributes to behavioral intentions. Coping appraisal includes: (1) response costs (e.g., expectancies that adhering to handwashing guidelines will result in some negative experiences/outcomes), (2) response efficacy (e.g., beliefs that handwashing will be effective in reducing threat of COVID-19), and (3) self-efficacy (e.g., beliefs about one's ability to adhere to the respective handwashing guidelines, even if some barriers may arise) (Norman et al., 2015; Rogers, 1975).
These PMT-based cognitions have already been investigated as cross-sectional correlates of COVID-19 preventive behaviors (Scholz and Freund, 2021). For example, a study explaining a combination of COVID-19 protective behaviors (mask wearing, social distancing, handwashing) indicated that the PMT cognitions were interconnected in line with the tenets of the theory (Ezati Rad et al., 2021). A study on COVID-19 vaccine uptake intentions partially supported PMT, showing associations between the following PMT cognitions and intention to vaccinate: perceived severity, response efficacy, and self-efficacy (Wang et al., 2021). Perceived vulnerability and response costs were unrelated to vaccination intentions (Wang et al., 2021).
Associations between the accumulation of COVID-19 cases/deaths and COVID-19 protective behaviors are likely to be mediated by theory-based cognitions, such as those related to threat appraisal. For example, longitudinal research confirmed that the number of accumulating COVID-19 cases was positively associated with perceived risk of being infected, which is an indicator of threat appraisal (Schneider et al., 2021). Stricter COVID-19 health and containment policies were negatively associated with self-efficacy and self-monitoring, which in turn were related to lower adherence to WHO handwashing guidelines (Luszczynska et al., 2021). These findings suggest that changes in threat appraisal and coping appraisal, and the associations between these appraisals and protective behaviors, may be shaped by the trajectory of the COVID-19 pandemic.
PMT suggests that cognitive processes operate jointly with affective processes, such as fear and anxiety-related arousal (Norman et al., 2015; Ruiter et al., 2001; Witte, 1992). Fear arousal may precede or follow threat appraisal (Norman et al., 2015). In the case of the former, fear arousal refers to unspecific anxiousness or fearfulness (see Ruiter et al., 2001) that is likely to enhance cognitive processing of threat-related information (e.g., “If I feel anxious, then I start to think about potential consequences of COVID-19”). In the latter case, fear arousal becomes a specific affective response to a specific cognitive response to threat (e.g., “I thought about severity of COVID-19 and then became anxious”). Fear arousal that precedes cognitive processing of threat is determined by individual characteristics, such as levels of general anxiety (Ruiter et al., 2001). Accordingly, it may be assumed that levels of general anxiety predict PMT cognitive processes, such as threat appraisal and coping appraisal.
The COVID-19 pandemic was associated with a 25.6% worldwide increase in cases of anxiety disorders and an overall increase in anxiety symptoms in the general population (Santomauro et al., 2021). Fear-related arousal is the cornerstone of anxiety disorder symptoms, with overgeneralization of conditioned fear as the key mechanism in the development of anxiety and anxiety disorder symptoms (Stegmann et al., 2019). The increase in anxiety symptoms in the general population may represent a preconscious response to the exposure to a threat (Ruiter et al., 2001), such as information on the accumulation of COVID-19 cases or deaths. Elevated symptoms of general anxiety and fear were found to be associated with higher levels of COVID-19 protective behaviors (Apisarnthanarak et al., 2020) and higher levels of risk perception, but lower levels of self-efficacy (Zhou et al., 2021). A better understanding of the indirect associations between general anxiety symptoms, PMT cognitions, and protective behaviors is needed to further clarify the complex processes through which general anxiety, PMT cognitions, and COVID-19 protective behaviors are interconnected.
1.2. Study aims
This longitudinal study investigates correlates of cross-situational adherence to handwashing guidelines (issued by the WHO [2020] and CDC [2020]) during the COVID-19 pandemic (March–September 2020) in 14 countries within Europe, Asia, North America, Africa, and Australia. We examined whether the level of general anxiety symptoms and the total number of COVID-19 cases and deaths accumulating in the country since the beginning of the pandemic would be indirectly related to handwashing adherence at follow-up, with PMT cognitions operating as mediators. In line with PMT's predictions, the putative mediators include: perceived illness severity, perceived vulnerability, response costs, response efficacy, self-efficacy, and behavioral intention.
2. Methods
2.1. Procedure
Data collected in this prospective study (see Clinical Trials.Gov, #NCT 04367337) included (1) total cases and total deaths due to COVID-19 (accumulated since the beginning of the pandemic) and (2) individual-level cognitions and behavior. Data at these two levels were assessed at two time points, resulting in four data collection points across the study. Time 0 (T0) involved collection of data on total cases and total deaths due to COVID-19 (since the beginning of the pandemic), as registered in the respective country and on the day of data collection. Time 1 (T1; 1–7 days after T0) involved data collection of PMT-related cognitions and cross-situational handwashing adherence. Time 2 (T2; 1 month after T0) involved collecting data on the total cases and total deaths due to COVID-19. At Time 3 (T3; 1–7 days after T2), data were again collected on the PMT-specified cognitions and cross-situational handwashing adherence.
The study was conducted in 14 countries: Australia, Canada, China, France, the Gambia, Germany, Israel, Italy, Malaysia, Poland, Portugal, Romania, Singapore, and Switzerland. The included countries had different trajectories of the COVID-19 pandemic (e.g., low vs. high numbers of total cases of COVID-19- during the data collection period, as reported by the WHO Coronavirus Disease Situation Reports [World Health Organization, 2021]). The countries also differed in the level of Human Development Index (HDI), varying from high and moderate values of HDI (i.e., between 0.800 and 0.550) to low values (i.e., <0.550), as defined by United Nations (United Nations Development Programme, 2021). The study was conducted between March and September 2020, after obtaining ethics clearance (following the institutional regulations in each study country). First, the approval was obtained from the Ethics Committee at SWPS University of Social Sciences and Humanities, Wroclaw, Poland. For details of ethics clearance in the remaining study countries, see the information provided at Open Science Framework, https://osf.io/vmn2q/.
Individual-level data (PMT, cross-situational handwashing adherence, sociodemographic) were obtained at T1 and T3 using a web-based survey delivered via the Qualtrics platform. The survey took approximately 15 min to complete. Snowball sampling was adopted as the main recruitment strategy. Links to the survey and study information (aims and design) were posted on university and social media websites. Before starting the survey, participants were provided with information regarding the handwashing guidelines, as proposed by the World Health Organization (2020). The only inclusion criterion was being ≥18 years old. All participants provided informed consent. There was no compensation for participation.
After completing the T1 survey, participants were informed that the next wave of data collection would take place in one month and they were invited to provide an email address that could be used to send the respective invitation. Consent was provided by 6397 respondents, with 6064 providing at least some PMT data at T1, and 2399 providing an email address for T3 data collection. An invitation to complete the T3 survey was sent via email from the Qualtrics platform, followed by two weekly reminders.
The study protocol and data collection procedures, all materials used in the study, data files, and outputs from main analyses (testing the hypothesized model) are available at Open Science Framework, https://osf.io/vmn2q/.
2.2. Participants
Data from 1256 participants was available at T1 and T3. The sample size per country ranged from n = 13 to n = 210 (M = 89.70, SD = 58.89). Sociodemographic characteristics for the total sample and the national subsamples are presented in Table 1 .
Table 1.
Sociodemographic sample characteristics for 14 countries.
| AUS | CAN | CHIN | FRA | GAM | GER | ISR | ITA | MALA | POL | POR | ROM | SGP | SWI | TOTAL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of participants | 195 | 66 | 127 | 107 | 23 | 210 | 89 | 63 | 36 | 65 | 56 | 78 | 13 | 128 | 1254 |
| Mean Age (SD) | 45.5 (13.6) | 40.7 (18.4) | 23.1 (3.1) | 37.8 (14.6) | 36.0 (11.1) | 36.2 (17.1) | 48.4 (16.0) | 32.8 (15.9) | 33.9 (14.5) | 33.5 (12.0) | 38.7 (13.2) | 34.0 (12.2) | 42.9 (15.0) | 35.2 (15.1) | 37.1 (15.7) |
| Gender (%) | |||||||||||||||
| Male | 5.6 | 24.2 | 26.8 | 14.0 | 65.2 | 21.4 | 20.2 | 25.4 | 19.4 | 15.4 | 25.0 | 15.4 | 15.4 | 19.5 | 19.1 |
| Female | 92.3 | 75.8 | 73.2 | 85.1 | 34.8 | 77.6 | 79.8 | 73.0 | 77.8 | 84.6 | 75.0 | 84.6 | 84.6 | 80.5 | 80.2 |
| Other | 2.1 | 0.00 | 0.00 | 0.9 | 0.0 | 1.0 | 0.0 | 1.6 | 2.8 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.7 |
| Education (%) | |||||||||||||||
| Primary education | 0.0 | 0.0 | 0.0 | 0.0 | 4.3 | 1.9 | 0.0 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.6 | 0.6 |
| High school | 12.3 | 6.1 | 4.7 | 15.0 | 4.4 | 7.6 | 5.6 | 17.5 | 5.6 | 23.1 | 5.4 | 10.3 | 15.4 | 10.2 | 10.0 |
| Vocational/post-secondary | 1.5 | 0.0 | 0.0 | 0.0 | 0.0 | 48.6 | 0.0 | 0.0 | 2.8 | 0.0 | 0.0 | 0.0 | 0.0 | 29.7 | 11.5 |
| University degree | 86.2 | 93.9 | 95.3 | 85.0 | 91.3 | 41.9 | 94.4 | 81.0 | 91.7 | 76.9 | 94.6 | 89.7 | 84.6 | 58.6 | 77.9 |
| Economic status (%) | |||||||||||||||
| Below average | 14.4 | 4.5 | 25.2 | 19.6 | 21.7 | 7.1 | 29.2 | 14.3 | 8.3 | 6.2 | 1.8 | 2.6 | 7.7 | 7.8 | 12.7 |
| Average for family in a country | 39.4 | 45.5 | 53.5 | 40.2 | 56.6 | 44.3 | 18.0 | 57.1 | 44.5 | 32.3 | 53.6 | 55.1 | 38.5 | 47.7 | 44.0 |
| Above average | 46.2 | 50.0 | 21.3 | 40.2 | 21.7 | 48.6 | 52.8 | 28.6 | 47.2 | 61.5 | 44.6 | 42.3 | 53.8 | 44.5 | 43.3 |
| Marital status | |||||||||||||||
| Single/Divorced/Widowed | 26.7 | 59.1 | 85.0 | 45.8 | 30.4 | 47.8 | 23.6 | 68.3 | 63.9 | 27.5 | 37.5 | 37.2 | 46.2 | 60.2 | 48.1 |
| Living with a partner | 73.3 | 40.9 | 15.0 | 54.2 | 69.6 | 52.2 | 76.4 | 31.7 | 36.1 | 72.5 | 62.5 | 62.8 | 53.8 | 39.8 | 51.9 |
| Employment | |||||||||||||||
| Unemployed/student/pensioner/retired | 31.3 | 37.9 | 80.3 | 34.6 | 13.0 | 56.7 | 27.0 | 69.4 | 58.3 | 32.1 | 19.6 | 32.1 | 23.1 | 39.1 | 43.5 |
| Full-/part-time employment | 68.7 | 62.1 | 19.7 | 65.4 | 87.0 | 43.3 | 73.0 | 30.6 | 41.7 | 67.9 | 80.4 | 67.9 | 76.9 | 60.9 | 56.5 |
| Healthcare professional | |||||||||||||||
| Health care | 9.7 | 16.3 | 6.2 | 24.4 | 36.4 | 6.7 | 5.6 | 9.5 | 35.0 | 6.2 | 21.6 | 11.9 | 18.2 | 18.7 | 12.5 |
| Other | 90.3 | 83.7 | 93.8 | 75.6 | 63.6 | 93.3 | 94.4 | 90.5 | 65.0 | 93.8 | 78.4 | 88.1 | 81.8 | 81.3 | 87.5 |
| Total cases (T0) | 6881.7 | 85694.8 | 83040.9 | 132184.2 | 44.2 | 126571.8 | 10631.9 | 126022.5 | 5186.0 | 3793.3 | 13256.5 | 20158.6 | 32155.2 | 24412.9 | 58475.6 |
| Total deaths (T0) | 94.6 | 6886.6 | 3532.6 | 25181.5 | 1.9 | 4067.2 | 100.8 | 15524.1 | 84.2 | 142.3 | 431.4 | 1237.8 | 22.1 | 881.7 | 4540.8 |
| Total cases (T2) | 7447.3 | 105103.8 | 84504.9 | 152472.5 | 39019.8 | 176430.6 | 16693.9 | 215638.3 | 7645.3 | 17200.8 | 29784.1 | 38683.8 | 44212.9 | 39763.4 | 79775.2 |
| Total deaths (T2) | 103.3 | 8367.8 | 4644.2 | 29210.6 | 5361.3 | 7961.2 | 254.7 | 30042.3 | 115.3 | 784.2 | 1213.2 | 1953.4 | 25.9 | 2147.7 | 6806.5 |
| General anxiety symptoms (T1) | 5.8 (4.8) | 5.3 (5.3) | 5.4 (3.7) | 6.3 (5.5) | 5.6 (6.3) | 5.3 (4.0) | 5.5 (4.4) | 6.4 (4.5) | 7.5 (5.6) | 8.9 (5.9) | 6.2 (4.7) | 5.6 (4.7) | 5.8 (3.6) | 4.5 (3.5) | 5.8 (4.7) |
| Handwashing (T1) | 3.4 (0.5) | 3.3 (0.5) | 3.3 (0.5) | 3.4 (0.5) | 3.3 (0.7) | 3.4 (0.5) | 3.2 (0.6) | 3.5 (0.4) | 3.4 (0.4) | 3.3 (0.6) | 3.6 (0.4) | 3.7 (0.4) | 3.4 (0.6) | 3.4 (0.5) | 3.4 (0.5) |
| Handwashing (T3) | 3.4 (0.5) | 3.3 (0.5) | 3.2 (0.5) | 3.4 (0.5) | 3.4 (0.7) | 3.4 (0.5) | 3.1 (0.6) | 3.5 (0.5) | 3.6 (0.4) | 3.3 (0.6) | 3.6 (0.4) | 3.7 (0.3) | 3.2 (0.8) | 3.4 (0.5) | 3.4 (0.5) |
Note. AUS = Australia; CAN = Canada; CHIN = China; FRA = France; GAM = Gambia; GER = Germany; ISR = Israel; ITA = Italy; MALA = Malaysia; POL = Poland; POR = Portugal; ROM = Romania; SGP = Singapore; SWI = Switzerland; Total = all countries combined; Handwashing = Adherence to the handwashing guidelines; Total cases/deaths = the number of total COVID-19 cases/deaths from the beginning of pandemic per country per date; Marital status: Living with a partner includes being married, civil partnership, and other romantic relationship.
2.3. Materials
The English language version of the questionnaire was prepared by the lead team (ZS, AL, and MS). The PMT measures were developed based on items that were used across cultures in research on handwashing and/or in the context of preventing infectious diseases (Park et al., 2010; Reyes Fernández et al., 2016) and following the guidelines to assess PMT variables (Norman et al., 2015). Two researchers from each of the involved countries (excluding Singapore, where one researcher was involved) tested the survey to assess whether the items (1) fit the context and culture of their country and (2) captured PMT measures appropriately. The lead team collated the feedback from all researchers, applied corrections, and developed the final English language version of the survey. Next, language/country versions were developed by two researchers in the respective countries. Australia, Canada, the Gambia, Malaysia, and Singapore applied the English language version. If a validated country language version of the general anxiety measure existed, this version was used in the survey.
2.3.1. T1 and T3 handwashing adherence to the CDC guidelines (the main study outcome)
Based on previous assessment tools (Lima-Costa et al., 2020; Nivette et al., 2021), the World Health Organization (2020) guidelines, and the Centers for Disease Control and Prevention (2020) guidelines, we developed a 12-item measure assessing handwashing that captured adherence across situations. The stem ‘During the previous week, I've usually washed my hands (for at least 20 s, all surfaces of the hands)’ was followed by eight situational contexts specified in the World Health Organization (2020) guidelines and four additional situational contexts specified in the Centers for Disease Control and Prevention (2020) guidelines: ‘Before, during, and after preparing food’, ‘Before eating food’, ‘Before and after caring for someone at home who is sick with vomiting or diarrhea’, ‘Before and after treating a cut or wound’, ‘After using the toilet’, ‘After changing diapers or cleaning up a child who has used the toilet’, ‘After blowing my nose, coughing, or sneezing’, ‘After touching an animal, animal feed, or animal waste’, ‘After handling pet food or pet treats’, ‘After touching garbage’, ‘After visiting public spaces’, and ‘When my hands were visibly dirty’. In the case of situations referring to caring for children, sick persons, animals, or treating a cut, participants were asked if they had encountered each of these situations in the previous week. If they indicated that they did not, these items were removed from the mean item score value for the participant. Responses were provided on a scale ranging from 1 (Strongly disagree) to 4 (Strongly agree). The internal consistency of scores was adequate (T1: α = 0.86; T3: α = 0.77). Descriptive statistics are presented in Table 1.
2.3.2. Total COVID-19 cases and deaths (country-and-day-specific data; T0 and T2)
An index of COVID-19 total morbidity and mortality was extracted from Coronavirus Disease Situation Reports, published daily by the World Health Organization (2021) for the period of data collection (March–September 2020) in the 14 included countries. The following data were extracted: (1) number of total COVID-19 cases since the beginning of pandemic, per country, and per specific date of data collection; and (2) number of COVID-19 deaths since the beginning of pandemic, per country, and per specific date of data collection (see Table 1 for descriptive information).
2.3.3. General anxiety symptoms (T1)
General anxiety was assessed with the Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006). Responses were provided on a 4-point scale ranging from 0 (Not at all) to 3 (Nearly every day). The scale had good reliability (T1: α = 0.89). Mean sum score was M = 5.79 (SD = 4.68), with 14.6% of participants reporting values above the cut-off point of ≥10, indicating a possible diagnosis of generalized anxiety disorder (Spitzer et al., 2006).
2.3.4. Constructs included in protection motivation theory (T1 and T3)
Perceived illness severity was assessed with one item, ‘If you were infected with coronavirus, how great of a burden would that be on your daily life?’ (Park et al., 2010). A 4-point response scale ranging from 1 (Mild symptoms like common cold) to 4 (May die from it) was used (T1: M = 2.26, SD = 0.98; T3: M = 2.22, SD = 0.94).
Perceived vulnerability was assessed with two items (e.g., ‘How possible do you believe it is for you to become infected with coronavirus SARS-CoV-2?‘) adapted from Park et al. (2010). A 5-point response scale ranging from 1 (Very low) to 5 (Very high) was used (T1: M = 2.70, SD = 0.78, r T1 = 0.50, p < .001; T3: M = 2.59, SD = 0.78, r T2 = 0.50, p < .001).
Response costs were assessed with one item, ‘If I wash my hands frequently every day in accordance with the WHO recommendations, then it would take too much of my time’ (Reyes Fernández et al., 2016). A 4-point response scale ranging from 1 (Strongly disagree) to 4 (Strongly agree) was used (T1: M = 1.82, SD = 0.74, T3: M = 1.95, M = 0.75).
Response efficacy was measured with one item, ‘Do you consider hand washing to be an effective means of preventing coronavirus SARS-CoV-2 infection?’ (Park et al., 2010). A 5-point response scale ranging from 1 (It is almost non-effective) to 5 (It is very effective) was used (T1: M = 4.02, SD = 0.78; T3: M = 3.96, SD = 0.80).
Self-efficacy was assessed with four items (as per Reyes Fernández et al., 2016), for example, ‘I am confident I can wash my hands in accordance with the WHO recommendations, even when I am in a hurry.’ A 4-point response scale (1 = Strongly disagree to 4 = Strongly agree) was used (T1: M = 3.31, SD = 0.58, α = 0.85; T3: M = 3.16, SD = 0.62, α = 0.87).
Intention (T1) was measured with two items (as per Reyes Fernández et al., 2016), for example, ‘Today and for the next 2 weeks I intend to properly wash my hands (for at least 20 s, all surfaces of the hands) with soap and water or alcohol-based hand rub in various situations identified by the WHO (e.g., before, during, and after preparing food.'A 4-point response scale ranging from 1 (Strongly disagree) to 4 (Strongly agree) was used (T1: M = 3.03, SD = 0.70, r = 0.40, p < .001; T3: M = 2.94, SD = 0.73, r = 0.50, p < .001).
2.3.5. Control variables (T1)
Individual-level data on country of residence, age, gender, education, perceived economic status, and marital status were assessed at T1. Participants indicated their education with responses representing the following four levels: primary school, vocational education/completed high school, up to three years of higher education, four or more years of higher education. Perceived economic status was measured with one item, ‘Compared to the average situation of a family in your country, what is the economic situation of your family?‘, with responses ranging from 1 (Much above the average) to 5 (Much below the average). Descriptive statistics are presented in Table 1.
2.4. Data analysis
The G*Power calculator simulating a multiple regression model was used to determine the sample size. As previous research yielded small direct effects of COVID-19 morbidity and mortality on handwashing (Szczuka et al., 2021), as well as very small indirect effects linking anxiety/mental health problems and the PMT variables (Zhou et al., 2021), we assumed small direct and indirect effect sizes f 2 = 0.02, power of .95, and Type I error rate of 0.05. The sample size was estimated using the approach suggested by O'Rourke and Hatcher (2013) and was based on the number of predictor and covariate variables in the path model and requirements for regression. The estimated sample size was 1300 respondents. Path analyses were conducted with the maximum likelihood estimation procedure, using SPSS and IBM AMOS versions 26. Indirect effects were evaluated with the user-defined estimands function and reported as unstandardized effect coefficients, calculated with 10,000 bootstraps and two-sided 95% bias-corrected confidence intervals (CI). Besides reporting p-values, we rely on two-tailed 95% CI for direct and indirect effect coefficients when interpreting the findings (Lin et al., 2013). The values of indirect effects coefficients do not allow for a valid quantitative indication of the effect value (Hafeman, 2009), whereas their two-tailed 95% bias-corrected CI can be used to assess whether indirect effects exist (Hafeman, 2009).
When evaluating the model fit, a cut-off point of ≤ .08 was applied for the root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR), and a cut-off point ≥.95 was used for the comparative fit index (CFI) and the normed fit index (NFI) (Byrne, 2010). Missing data were accounted for by using a full information maximum likelihood procedure (FIML; Byrne, 2010). The values of Little's MCAR test were not significant (χ 2 (31) = 42.44, p = .083), suggesting random missing data patterns. Mardia's coefficient of multivariate normality indicated substantial non-normality (284.79). To reduce non-normality, logarithmic transformations were applied to indicators of general anxiety (T1).
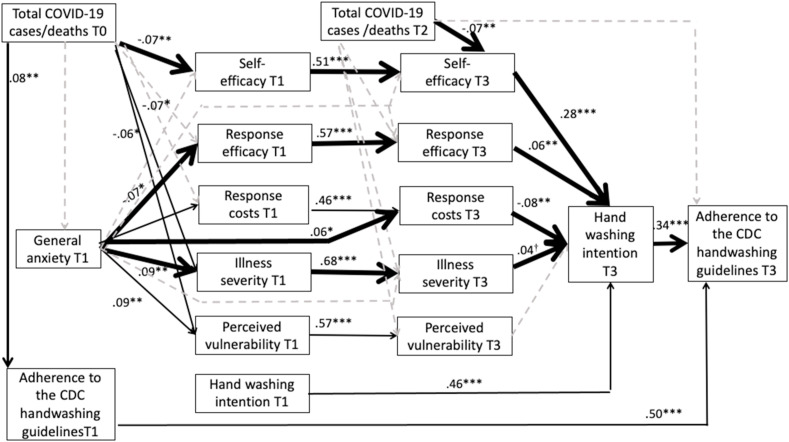
The hypothesized mediation model (Fig. 1) was tested using the half-longitudinal design (Byrne, 2010). The indirect effects were obtained by controlling the effects of the mediator at T1 on the mediator at T3 and the effects of the dependent variable at T1 on the dependent variable at T3. The model assumed that the total number of COVID-19 cases (T0) and general anxiety at T1 would be related to all T1 PMT variables (perceived illness severity, perceived vulnerability, response costs, response efficacy, self-efficacy, and intention) and cross-situational handwashing adherence at T1. Total number of COVID-19 cases at T2 was assumed to be related to the T3 PMT variables and adherence to handwashing at T3. T0 total number of COVID-19 cases was associated with T1 general anxiety and with the total number of COVID-19 cases at T2. Cross-situational handwashing adherence indicators at T1 and T3 were assumed to be related. Residuals of the PMT variables at T1 and handwashing adherence at T1 were assumed to covary with each other (unless the two variables were linked with a regression path). The residuals of the PMT variables at T3 were also assumed to covary.
Fig. 1.
Results of Path Analysis for the Mediation Model: Associations Between the Independent Variables (Including COVID-19 Cases at T0 and T2, and General Anxiety Symptoms at T1), the Protection Motivation Theory-based Mediators (T1 and T3), and the Dependent Variable, Adherence to Handwashing (T3) Across the Situations
Note: Dashed lines represent non-significant paths. Solid lines represent significant paths. Bold solid lines represent significant indirect effects. For clarity, the covariances between the variables measured at the same time point are not displayed.
*p < .05, **, p < .01, ***, p < .001.
Overall, 35 indirect effects were tested. Ten sequential mediating effects linked the total number of COVID-19 cases (T0 or T2) with the PMT variable (the mediator, T1 or T3, respectively), which in turn was associated with intention at T3, which was associated with handwashing adherence (the dependent variable, T3). Ten sequential mediating effects linked the total number of COVID-19 cases (T0) with general anxiety at T1, which was related to the PMT variable (the mediator, T1 or T3, respectively), which in turn was associated with intention at T3, which was associated with handwashing adherence (the dependent variable, T3). Ten sequential mediating effects linked general anxiety at T1 to the PMT variable (the mediator, T1 or T3, respectively), which in turn was associated with intention at T3, which was associated with handwashing adherence (the dependent variable, T3). Five sequential mediating effects linked the PMT variable at T1 (the dependent variable) and the respective T3 PMT variable T3 (the first mediator) with intention at T3 (the second mediator), which in turn was associated with handwashing adherence (the dependent variable, T3).
Sensitivity analyses (Thabane et al., 2013) were conducted to assess the robustness of the findings. First, analyses tested if the pattern of associations is similar when controlling for age, gender, and socioeconomic status. Second, analyses were repeated with data obtained from both dropouts and completers to test if the exclusion of dropouts affected the findings. The third sensitivity analysis was conducted with total COVID-19 cases replaced with another indicator of COVID-19 pandemic, namely total COVID-19 deaths.
Participants’ data were nested in k = 14 countries. Consequently, the intraclass correlation coefficient (ICC) was calculated to evaluate the potential presence of significant clustering effects across the study variables.
3. Results
3.1. Preliminary analyses
We compared those who responded at T1 but not T3 (n = 1143) with those who responded at both T1 and T3 (n = 1256). Those who completed the T1 survey only and those who completed both T1 and T3 surveys did not differ in the T1 PMT variables of perceived vulnerability, response efficacy, self-efficacy, and intention. Those who dropped out did, however, report higher response costs (p = .009) and higher perceived illness severity (p = .007). There were no differences in general anxiety and total deaths related to COVID-19, but the number of COVID-19 cases (T0) among dropouts was lower (p < .001). Finally, those who only completed the T1 survey were younger, reported higher levels of economic status, and were more likely to be men (all ps < .001). For details of the dropout analyses see Supplemental Materials.
In the total analyzed sample (N = 1256), the average adherence to handwashing across 12 situations was high (T1: M = 3.39, SD = 0.50; T3: M = 3.38, SD = 0.52) and did not change between T1 and T3, F (1, 1255), p < .01, p = .759. Between T0 and T2 there was a significant increase in the total number of COVID-19 cases, F (1, 1255) = 259.75, p < .001 (T0: M = 58,476, SD = 56,407 vs. T2: M = 79,775 SD = 79,333) and the total number of COVID-19 deaths, F (1, 1255) = 279.48, p < .001 (T0: M = 4,541, SD = 7615 vs. T2: M = 6,806, SD = 9927).
Across the PMT variables and handwashing adherence, participants with GAD-7 scores above the cut-off point for the potential diagnosis of the generalized anxiety disorder (14.6% of the total sample) did not differ from those with GAD-7 scores below this threshold, all Fs < 2.83, ps > .092. The only exception was perceived vulnerability (T1 and T3), which was higher among participants whose scores indicated a possibility of generalized anxiety disorders compared to those below the cut-off point, F (1, 1225) = 12.50, p < .001 at T1 and F (1, 1225) = 9.21, p = .002 at T3.
Intraclass correlation coefficients evaluating country-related clustering effects were not significant for total COVID-19 cases and deaths, the PMT variables, handwashing, and sociodemographic variables (see Supplementary Table 1, Supplemental Materials). The two exceptions were low but significant ICCs for generalized anxiety and age. Correlation coefficients for the total sample are presented in Supplementary Table 2, Supplemental Materials.
3.2. Indirect associations between COVID-19 cases/deaths, general anxiety symptoms, PMT variables, and handwashing
The model had an acceptable fit, with χ 2 (68) = 341.20, p < .001, χ 2/df = 5.02, NFI = 0.95, CFI = 0.96, RMSEA = 0.06 (90% CI: 0.05, 0.06), SRMR = 0.04. Direct associations between the independent variables (COVID-19 cases at T0 and T2; general anxiety at T1), PMT mediators (T1 and T3) and the dependent variable, (i.e., cross-situational adherence to handwashing (T3), are presented in Fig. 1 and Table 2 . The variables in the model explained 41.11% of the variance in intention and 52.81% of the variance in handwashing adherence.
Table 2.
Direct effects for the hypothesized model (N = 1256).
| Variables and hypothesized associations | β | 95% lower CI for β | 95% upper CI for β | p |
|---|---|---|---|---|
| Handwashing (T1) → Handwashing (T3) | .499 | .439 | .556 | <.001 |
| Total COVID-19 cases (T0) → Handwashing (T1) | .075 | .028 | .121 | .002 |
| Total COVID19 cases (T0) → General anxiety symptoms (T1) | −.003 | −.057 | .050 | .915 |
| Total COVID-19 cases (T0) → Perceived illness severity (T1) | −.065 | −.121 | −.011 | .020 |
| Total COVID-19 cases (T0) → Perceived vulnerability (T1) | −.060 | −.115 | −.007 | .029 |
| Total COVID-19 cases (T0) → Response costs (T1) | −.005 | −.056 | .052 | .887 |
| Total COVID-19 cases (T0) → Response efficacy (T1) | .049 | −.007 | .105 | .083 |
| Total COVID-19 cases (T0) → Self-efficacy (T1) | −.065 | −.115 | −.016 | .007 |
| General anxiety symptoms (T1)→ Handwashing (T1) | .000 | −.047 | .046 | .996 |
| General anxiety symptoms (T1) → Perceived illness severity (T1) | .094 | .038 | .149 | .001 |
| General anxiety symptoms (T1) → Perceived vulnerability (T1) | .088 | .029 | .145 | .003 |
| General anxiety symptoms (T1) → Response costs (T1) | .020 | −.031 | .074 | .463 |
| General anxiety symptoms (T1) → Response efficacy (T1) | −.068 | −.122 | −.012 | .018 |
| General anxiety symptoms (T1) → Self-efficacy (T1) | −.004 | −.052 | .043 | .859 |
| General anxiety symptoms (T1) → Perceived illness severity (T3) | .013 | −.028 | .054 | .540 |
| General anxiety symptoms (T1) → Perceived vulnerability (T3) | .050 | .000 | .097 | .052 |
| General anxiety symptoms (T1) → Response costs (T3) | .058 | .008 | .108 | .022 |
| General anxiety symptoms (T1) → Response efficacy (T3) | −.012 | −.058 | .033 | .617 |
| General anxiety symptoms (T1) → Self-efficacy (T3) | .010 | −.041 | .060 | .703 |
| Perceived illness severity (T1) → Perceived illness severity (T3) | .681 | .644 | .715 | <.001 |
| Perceived vulnerability (T1) → Perceived vulnerability (T3) | .566 | .519 | .609 | <.001 |
| Response costs (T1) → Response costs (T3) | .458 | .403 | .509 | <.001 |
| Response efficacy (T1) → Response efficacy (T3) | .574 | .529 | .618 | <.001 |
| Self-efficacy (T1) → Self-efficacy (T3) | .506 | .451 | .558 | <.001 |
| Intention (T1) → Intention (T3) | .459 | .407 | .512 | <.001 |
| Total COVID-19 cases (T2) → Perceived illness severity (T3) | .017 | −.023 | .056 | .392 |
| Total COVID-19 cases (T2) → Perceived vulnerability (T3) | −.011 | −.053 | .030 | .600 |
| Total COVID-19 cases (T2) → Response costs (T3) | .044 | −.024 | .130 | .228 |
| Total COVID-19 cases (T2) → Response efficacy (T3) | .015 | −.028 | .056 | .473 |
| Total COVID-19 cases (T2) → Self-efficacy (T3) | −.070 | −.123 | −.020 | .006 |
| Perceived illness severity (T3) → Intention (T3) | .039 | −.002 | .080 | .063 |
| Perceived vulnerability (T3) → Intention (T3) | .028 | −.014 | .069 | .203 |
| Response costs (T3) → Intention (T3) | −.080 | −.132 | −.027 | .002 |
| Response efficacy (T3) → Intention (T3) | .063 | .019 | .106 | .006 |
| Self-efficacy (T3) → Intention (T3) | .284 | .224 | .345 | <.001 |
| Intention (T3) → Handwashing (T3) | .343 | .293 | .394 | <.001 |
Note. 95% CI – values of 95% two-tailed bias corrected confidence intervals. Direct effect estimates presented in bold have values of two-tailed bias corrected confidence intervals that do not include zero. T0 = Time 0; T1 = Time 1 (1–7 days later); T2 = Time 2 (one month after T1), T3 = Time 3 (1–7 days after T2); Handwashing = Handwashing Adherence Index (based on the CDC Guidelines); Total COVID-19 Cases = the number of total COVID-19 cases/deaths from the beginning of pandemic per country per date. Data were collected in 14 countries (Australia, Canada, China, France, Gambia, Germany, Israel, Italy, Malaysia, Poland, Portugal, Romania, Singapore, and Switzerland) between March 25, 2020 and September 20, 2020, during the COVID-19 pandemic.
The observed pattern of associations provided support for PMT (see Fig. 1, see 95% CI in Table 2). Higher self-efficacy (T3), higher response efficacy (T3), and lower response costs (T3) were related to stronger intention (T3), which in turn was associated with higher handwashing adherence (T3). The values of covariance coefficients are presented in Supplementary Table 4, Supplemental Materials. Small size associations were found between higher general anxiety (T1) and lower self-efficacy (T1), higher perceived illness severity (T1), higher perceived vulnerability (T1, T3), and higher response costs (T3). Higher number of total COVID-19 cases (T0) was related to lower self-efficacy (T1), lower perceived illness severity (T1), lower perceived vulnerability (T1), and higher cross-situational handwashing adherence (T1). The higher number of COVID-19 cases at T2 was associated with lower self-efficacy (T3). The number of COVID-19 cases (T0) and general anxiety (T1) were unrelated. Respective coefficients and their 95% CI are presented in Table 2.
Next, 35 indirect effects analyses were performed (see Table 3 ), indicating nine significant indirect associations. For the indirect effects with total COVID-19 cases (T0 or T2) operating as the independent variable, three indirect associations were significant: lower COVID 19 cases (T0) → higher self-efficacy (T1) → higher self-efficacy (T3) → higher intention (T3) → higher handwashing adherence (T3); lower COVID 19 cases (T2) → higher self-efficacy (T3) → higher intention (T3) → higher handwashing (T3); lower COVID 19 cases (T0) → higher illness severity (T1) → higher illness severity (T3) → higher intention (T3) → higher handwashing (T3).
Table 3.
Significant simple indirect effects in the hypothesized model (N = 1256).
| Simple indirect effects | Estimate | SE | 95%BCI |
||
|---|---|---|---|---|---|
| Lower | Higher | p | |||
| Total COVID-19 cases (T0)→ Perceived illness severity (T1)→ Perceived illness severity (T3)→Handwashing adherence (T3) | <0.001 | <0.001 | <0.001 | <0.001 | .042 |
| Total COVID-19 cases (T0)→ Response efficacy (T1)→Response efficacy (T3)→Handwashing adherence (T3) | >-0.001 | <0.001 | >-0.001 | >-0.001 | .049 |
| Total COVID-19 cases (T0)→ Self-efficacy (T1)→ Self-efficacy (T3)→Handwashing adherence (T3) | >-0.001 | <0.001 | >-0.001 | >-0.001 | .005 |
| General anxiety symptoms (T1)→ Perceived illness severity (T1)→ Perceived illness severity (T3)→Handwashing adherence (T3) | 0.001 | 0.001 | <0.001 | 0.003 | .037 |
| General anxiety symptoms (T1)→Response efficacy (T1)→Response efficacy (T3)→Handwashing adherence (T3) | −0.001 | 0.001 | −0.003 | >-0.001 | .011 |
| General anxiety symptoms (T1)→Response costs (T3)→Handwashing adherence (T3) | −0.002 | 0.001 | −0.005 | >-0.001 | .012 |
| Response costs (T1)→Response costs (T3)→Handwashing adherence (T3) | −0.009 | 0.003 | −0.016 | −0.003 | .002 |
| Response efficacy (T1)→Response efficacy (T3)→Handwashing adherence (T3) | 0.008 | 0.003 | 0.003 | 0.014 | .005 |
| Self-efficacy (T1)→ Self-efficacy (T3)→Handwashing adherence (T3) | 0.044 | 0.007 | 0.032 | 0.059 | <.001 |
| Total COVID-19 cases (T2)→ Self-efficacy (T3)→Handwashing adherence (T3) | >-0.001 | <0.001 | >-0.001 | >-0.001 | .005 |
Note. Significant effects are presented only. All tested indirect effects (including not significant) are reports in Supplementary Table 3, Supplemental Materials. The values of the majority of indirect effect estimates were either larger than −0.001 (i.e., −0.0002) or smaller than 0.001 (i.e., 0.0002). T0 = Time 0; T1 = Time 1 (1–7 days later); T2 = Time 2 (one month after T1), T3 = Time 3 (1–7 days after T2); Handwashing = Handwashing adherence (based on the CDC Guidelines); Total COVID-19 Cases = the number of total COVID-19 cases from the beginning of pandemic per country per date. Data were collected in 14 countries between March 25, 2020 and September 20, 2020, during the COVID-19 pandemic.
Regarding the indirect effects with general anxiety (T1) operating as the independent variable, three indirect associations were significant: lower general anxiety (T1) → higher response efficacy (T1) → higher response efficacy (T3) → higher intention (T3) → higher handwashing adherence (T3); higher general anxiety (T1) → higher illness severity (T1) → higher illness severity (T3) → higher intention (T3) → higher handwashing adherence (T3); lower general anxiety (T1) → lower response costs (T3) → higher intention (T3) → higher handwashing adherence (T3). Table 3 presents 95% CI indicating significance of the indirect effects.
Finally, three indirect effects were found for the associations between the PMT variables and handwashing adherence: higher illness severity (T1) → higher illness severity (T3) → higher intention (T3) → higher handwashing adherence (T3); higher self-efficacy (T1) → higher self-efficacy (T3) → higher intention (T3) → higher handwashing adherence (T3); lower response costs (T1) → lower response costs (T3) → higher intention (T3) → higher handwashing adherence (T3). Respective coefficients and their 95% CI are reported in Table 3.
3.3. Sensitivity analyses
The first sensitivity analysis included sociodemographic variables (age, gender, and socioeconomic status) as predictors of handwashing adherence at T3 and correlates of all T1 variables (except for COVID-19 indicators). The model accounting for sociodemographic covariates had an acceptable fit, with χ 2 (94) = 480.27, p > .001, χ 2/df = 5.11, NFI = 0.94, CFI = 0.95, RMSEA = 0.06 (90% CI [0.05, 0.06]), SRMR = 0.04. The pattern of the 8 indirect effects was the same as in the hypothesized model without respective covariates (see Supplementary Tables 5–7, Supplemental Materials). The exception was one indirect effect (linking the independent variable, COVID-19 cases, with the mediator, perceived illness severity at T1) which was not significant.
The second sensitivity analysis tested if the missing data treatment strategy, namely the deletion of non-completers, affected the patterns of observed associations (see Supplementary Tables 8-10, Supplemental Materials). The path analysis was conducted in a sample of N = 2339 participants, including both completers and dropouts. The model had an acceptable fit, with χ 2 (68) = 444.03, p > .001, χ 2/df = 6.53, NFI = 0.98, CFI = 0.98, RMSEA = 0.05 (90% CI [ 0.04, 0.05]), SRMR = 0.04. The same eight indirect effects emerged, as found for the hypothesized model calculated for completers only (N = 1256). As in the case of the first sensitivity analysis, the exception was one indirect effect (linking the independent variable, COVID-19 cases, with the mediator, perceived illness severity at T1) which did not become significant.
The third additional analysis was conducted with the total number of COVID-19 cases at T0 and T2 replaced by the total number of COVID-19 deaths (T0 and T2, respectively). The analyses were again conducted for the sample including the dropouts. The model had an acceptable fit, with χ 2 (68) = 444.03, p > .001, χ 2/df = 5.09, NFI = 0.98, CFI = 0.99, RMSEA = 0.04 (90% CI [0.03, 0.05]), SRMR = 0.03. The same eight indirect effects emerged, as found for the hypothesized model, the first and second sensitivity analysis (see Supplementary Tables 11-13, Supplemental Materials). In line with previous sensitivity analyses, the exception referred to one insignificant indirect effect (linking the independent variable, COVID-19 cases, with the mediator, perceived illness severity at T1).
4. Discussion
The findings of this prospective 14-country study provide novel evidence for the associations between the indicators of the trajectory of the COVID-19 pandemic, general anxiety, PMT cognitions, and handwashing adherence across situations. Our findings suggest that the number of total cases and deaths due to COVID-19 was indirectly associated with adherence to handwashing guidelines. Self-efficacy and intention sequentially mediated this association. General anxiety was associated with three other PMT mediators, namely, response efficacy, response costs, and perceived illness severity. These three PMT mediators were linked to intention, and, sequentially, to handwashing adherence.
The tenets of PMT were supported, with higher levels of perceived illness severity, response efficacy and self-efficacy, and lower levels of response costs being associated with higher levels of intention and, in turn, higher adherence to handwashing across the situations indicated in the CDC guidelines (CDC, 2020). Path analysis indicated that perceived vulnerability was the only PMT predictor that was not associated with handwashing intention; however, bivariate associations of perceived vulnerability with intention and behavior were positive and significant, yet weak (rs between 0.08 and 0.10). This is in line with previous research indicating a “low key” role of perceived vulnerability or risk perception, operationalized as weak or not significant associations with COVID-19 protective behaviors (Ezati Rad et al., 2021; Hamilton et al., 2020; Scholz and Freund, 2021; Schüz et al., 2021; Wang et al., 2021).
The findings provide support for Ruiter et al.’s (2001) conceptualization of the links between fear, PMT cognitions, and protective behavior. We found indirect associations between higher general anxiety and higher handwashing adherence, mediated by perceptions of higher perceived severity of COVID-19 and intention. This is in line with the proposal formulated by Ruiter et al.’s (2001) that fear-related processes may bolster threat appraisal (e.g., perceived severity), which in turn is associated with stronger intentions and higher adherence to protective behaviors. The positive associations between general anxiety (or fear arousal) and perceived illness severity are consistent with (1) the assumptions of the extended parallel process model, which integrates PMT cognitions and affective processes (Witte, 1992), and (2) previous cross-sectional research, which found that general anxiety is positively related to perceived severity of, and vulnerability to, COVID-19 (Zhang et al., 2022).
We found that lower generalized anxiety was indirectly related with better adherence with two parallel mediators, higher response efficacy and lower response costs, followed by higher intention. These findings are consistent with the proposal by Ruiter et al. (2001) suggesting that negative emotions may activate other processes (such as avoidance or suppression) that may compete with or distract precautions motivation processes and, subsequently, disrupt adoption of protective behavior. Our findings are also consistent with research that found a negative association between general anxiety levels and COVID-19 response efficacy (measured as beliefs about the efficacy of governmental responses to curb the COVID-19 pandemic; Zhang et al., 2022). We did not find direct associations between general anxiety symptoms and self-efficacy, which is again in line with Ruiter et al.’s (2001) proposal that these associations are indirect (via the threat appraisal processes). Alternatively, self-efficacy may be bolstered by fear but at the same time hindered by competing fear-related processes such as avoidance or suppression (Ruiter et al., 2001), so these fear-related processes may counteract each other and result in a negligible link between negative emotions and self-efficacy.
We found an indirect association between the accumulating numbers of COVID-19 cases/deaths and handwashing adherence, with self-efficacy mediating this association. The lower number of COVID-19 cases/deaths was associated with higher self-efficacy beliefs. It is possible that lower numbers of COVID-19 cases/deaths were related to less strict containment policies (i.e., lower restriction of movement) and thus (relatively) more social contacts and more encounters of high-risk of infection situations during everyday life. This may have increased mastery of handwashing adherence resulting in higher self-efficacy (Bandura, 1997) and, consequently, higher handwashing adherence. As the number of COVID-19 cases and deaths was accumulating over time of the pandemic, ‘pandemic fatigue’ (Reicher and Drury, 2021) occurred, defined as a decline in motivation to engage in protective behaviors over time. Lower self-efficacy, following the accumulation of COVID-19 cases, may represent a decline in such motivation processes.
The associations confirmed in our study (specifically, the indirect effects of general anxiety levels and the number of COVID-19 cases/deaths on handwashing adherence via the PMT variables) may have some theoretical implications. First, following the developments of dual process models (Hagger, 2016), the models focusing on cognitive determinants of behavior change (such as PMT) may need to evolve and clarify the roles played by affective processes (such as general anxiety symptoms). Furthermore, following developments in social-ecological models and their applications (Jang, 2022), cognitive processes-oriented health behavior change models may need to account for the role of environmental factors (such as the trajectory of the COVID-19 pandemic) and the dynamic way they operate.
Our findings indicate weak associations between general anxiety, the number of COVID-19 cases, and PMT variables. Similarly, the associations between PMT predictors and intention were weak, whereas the association between intention and handwashing adherence was weak-to-moderate. The observed effect sizes were likely to be small-to-moderate as they were obtained in a heterogeneous sample, controlling for the baseline effects of the mediators and the outcome variable (handwashing adherence), and in a sample that had a high level of handwashing adherence at baseline and follow-up. The small effect sizes warrant replications before any conclusions for clinical practice can be drawn.
The present study has several limitations. First, due to the correlational nature of the results, causal inferences are not possible. Second, although the sensitivity analyses were conducted to control for the effects of sociodemographic variables, it must be acknowledged that the sample included mostly women, and the majority of respondents had at least some university education and perceived their economic status as being average or above average in their respective country. This reduces the generalizability of findings to the wider population. A large dropout rate further limits generalizability, although this limitation was mitigated by a replication of the analysis with missing data accounted for using the full information maximum procedure. Third, handwashing adherence was self-reported, but there is no recommended objective assessment of cross-situational handwashing and hand sanitizing (in contrast to an assessment conducted in a medical care setting, which may be done through automated monitoring of entries and the use of hand sanitizers; Makhni et al., 2021).
Fourth, data used in this study are clustered, with individuals nested in countries. This may have introduced non-independence in the sense that individuals living in the same country and being subject to similar policies at similar time points may be more similar than individuals across countries. However, because this study comprised too few clusters (i.e., countries, N = 14), a multi-level approach was not feasible. Fifth, applied measures of the PMT variables and handwashing adherence were not thoroughly validated across the cultures. Given that the COVID-19 cases and deaths data were country-specific and included in the analyses, this might have accounted partially for the violation of the non-independence requirement. Finally, sample sizes differed across the included countries and cultural factors were not controlled. Any conclusions drawn should take these limitations into account. Future research should investigate if the associations observed in this study may be similar in later stages of the COVID-19 pandemic and for other protective behaviors, such as social distancing or the uptake of vaccination against COVID-19.
Despite these limitations, the current study has several strengths. These include the use of a previously validated theoretical model of behavior change, and the assessment of indicators of the trajectory of COVID-19 that were varying across the time span of the study and across the studied countries. Overall, this study provides a novel insight into complex interrelations between the indicators of the COVID-19 pandemic trajectory, general anxiety symptoms, PMT cognitions, and adherence to handwashing guidelines. Importantly, the study confirms the enduring relevance of the PMT framework in understanding health-protective behavior patterns across threats. Replication of these results in other contexts (e.g., during the later phases of the COVID-19 pandemic) is warranted.
Credit author statement
Zofia Szczuka: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing - original draft, Writing - review & editing, Maria Siwa: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing - original draft, Writing - review & editing, Charles Abraham: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Adriana Baban: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Sydney Brooks: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Sabrina Cipolletta: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, brima Danso: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Stephan U. Dombrowski: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Yiqun Gan: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Tania Gaspar: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Margarida Gaspar de Matos: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Konstadina Griva: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Michelle Jongenelis: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Jan Keller: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Nina Knoll: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Jinjin Ma: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Mohammad Abdul Awal Miah: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Karen Morgan: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, William Peraud: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Bruno Quintard: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Vishna Shah: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Konstantin Schenkel: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Urte Scholz: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Ralf Schwarzer: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Diana Taut: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Silvia C. M. Tomaino: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Noa Vilchinsky: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Hodaya Wolf: Data curation, Investigation, Project administration, Resources, Visualization, Writing - review & editing, Aleksandra Luszczynska: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Writing - original draft, Writing - review & editing.
Funding source
The study was supported by grant number 2020/01/0/HS6/00059 from the National Science Centre, Poland, awarded to Aleksandra Luszczynska (study design; collection; analysis and interpretation of data; writing of the article).
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.115569.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
Data related to this paper as well as original study materials, outputs are available at https://osf.io/vmn2q/ except data for Germany, Malaysia, and Australia; based on decisions of the respective IRBs.
References
- Apisarnthanarak A., Apisarnthanarak P., Siripraparat C., Saengaram P., Leeprechanon N., Weber D.J. Impact of anxiety and fear for COVID-19 toward infection control practices among Thai healthcare workers. Infect. Control Hosp. Epidemiol. 2020;41(9):1093–1094. doi: 10.1017/ice.2020.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. W. H. Freeman/Times; 1997. Self-efficacy: the Exercise of Control. [Google Scholar]
- Beale S., Johnson A.M., Zambon M., Hayward A.C., Fragaszy E.B. Hand hygiene practices and the risk of human Coronavirus infections in a UK community cohort. Wellcome Open Research. 2020;5:98. doi: 10.12688/wellcomeopenres.15796.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne B.M. Routledge; 2010. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. [Google Scholar]
- Centers for Disease Control and Prevention . 2020. When and How to Wash Your Hands.https://www.cdc.gov/handwashing/when-how-handwashing.html [Google Scholar]
- Ezati Rad R., Mohseni S., Kamalzadeh Takhti H., Hassani Azad M., Shahabi N., Aghamolaei T., Norozian F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: a cross-sectional study. BMC Publ. Health. 2021;21(1):466. doi: 10.1186/s12889-021-10500-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafeman D.M. Proportion explained’: a causal interpretation for standard measures of indirect effect? Am. J. Epidemiol. 2009;170(11):1443–1448. doi: 10.1093/aje/kwp283. [DOI] [PubMed] [Google Scholar]
- Hagger M.S. Non-conscious processes and dual-process theories in health psychology. Health Psychol. Rev. 2016;10(4):375–380. doi: 10.1080/17437199.2016.1244647. [DOI] [PubMed] [Google Scholar]
- Hamilton K., Smith S.R., Keech J.J., Moyers S.A., Hagger M.S. Application of the health action process approach to social distancing behavior during COVID-19. Appl. Psychol. Health Well-Being. 2020;12(4):1244–1269. doi: 10.1111/aphw.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang S.H. Social-ecological factors related to preventive behaviors during the COVID-19 pandemic in South Korea. PLoS One. 2022;17(3) doi: 10.1371/journal.pone.0266264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima-Costa M.F., Mambrini J.V. de M., Andrade F. B. de, Peixoto S.W.V., Macinko J. Social distancing, use of face masks and hand washing among participants in the Brazilian Longitudinal Study of Aging: the ELSI-COVID-19 initiative. Cad. Saúde Pública. 2020;36(Suppl. 3) doi: 10.1590/0102-311X00193920. [DOI] [PubMed] [Google Scholar]
- Lin M., Lucas H.C., Jr., Shmueli G. Too big to fail: large samples and the p-value problem. Inf. Syst. Res. 2013;24(4):906–917. doi: 10.1287/isre.2013.0480. [DOI] [Google Scholar]
- Luszczynska A., Szczuka Z., Abraham C., Baban A., Brooks S., Cipolletta S., Danso E., Dombrowski S.U., Gan Y., Gaspar T., de Matos M.G., Griva K., Jongenelis M.I., Keller J., Knoll N., Ma J., Miah M.A.A., Morgan K., Peraud W., et al. The interplay between strictness of policies and individuals' self-regulatory efforts: associations with handwashing during the COVID-19 Pandemic. Ann. Behav. Med. 2021 doi: 10.1093/abm/kaab102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makhni S., Umscheid C.A., Soo J., Chu V., Bartlett A., Landon E., Marrs R. Hand hygiene compliance rate during the COVID-19 pandemic. Journal of the American Medical Associaiton Internal Medicine. 2021;181(7):1006–1008. doi: 10.1001/jamainternmed.2021.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nivette A., Ribeaud D., Murray A., Steinhoff A., Bechtiger L., Hepp U., Shanahan L., Eisner M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc. Sci. Med. 2021;268 doi: 10.1016/j.socscimed.2020.113370. 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman P., Boer H., Seydel E.R., Mullan B. In: Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models. third ed. Conner M., Norman P., editors. Open University Press; 2015. Protection motivation theory; pp. 81–126. [Google Scholar]
- O'Rourke N., Hatcher L. second ed. SAS Institute Inc; Cary, NC: 2013. A Step-by-step Approach to Using SAS for Factor Analysis and Structural Equation Modeling. [Google Scholar]
- Park J.H., Cheong H.K., Son D.Y., Kim S.U., Ha C.M. Perceptions and behaviors related to hand hygiene for the prevention of H1N1 influenza transmission among Korean university students during the peak pandemic period. BMC Infect. Dis. 2010;10:222. doi: 10.1186/1471-2334-10-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petherick A., Goldszmidt R., Andrade E.B., Furst R., Hale T., Pott A., Wood A. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Human Behav. 2021;5(9):1145–1160. doi: 10.1038/s41562-021-01181-x. [DOI] [PubMed] [Google Scholar]
- Reyes Fernández B., Knoll N., Hamilton K., Schwarzer R. Social-cognitive antecedents of hand washing: Action control bridges the planning-behaviour gap. Psychol. Health. 2016;31(8):993–1004. doi: 10.1080/08870446.2016.1174236. [DOI] [PubMed] [Google Scholar]
- Reicher S., Drury J. Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. Br. Med. J. 2021;372 doi: 10.1136/bmj.n137. [DOI] [PubMed] [Google Scholar]
- Rogers R.W. A protection motivation theory of fear appeals and Attitude Change 1. J. Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Ruiter R.A.C., Abraham C., Kok G. Scary warnings and rational precautions: a review of the psychology of fear appeals. Psychol. Health. 2001;16(6):613–630. doi: 10.1080/08870440108405863. [DOI] [Google Scholar]
- Santomauro D.F., Mantilla Herrera A.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Abbafati C., Adolph C., Amlag J.O., Aravkin A.Y., Bang-Jensen B.L., Bertolacci G.J., Bloom S.S., Castellano R., Castro E., Chakrabarti S., Chattopadhyay J., Cogen R.M., Collins J.K., et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholz U., Freund A.M. Determinants of protective behaviours during a nationwide lockdown in the wake of the COVID-19 pandemic. Br. J. Health Psychol. 2021;26(3):935–957. doi: 10.1111/bjhp.12513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider C.R., Dryhurst S., Kerr J., Freeman A.L.J., Recchia G., Spiegelhalter D., van der Linden S. COVID-19 risk perception: a longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. J. Risk Res. 2021;24(3–4):294–313. doi: 10.1080/13669877.2021.1890637. [DOI] [Google Scholar]
- Schüz B., Conner M., Wilding S., Alhawtan R., Prestwich A., Norman P. Do socio-structural factors moderate the effects of health cognitions on COVID-19 protection behaviours? Soc. Sci. Med. 2021 doi: 10.1016/j.socscimed.2021.114261. 1982), 285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stegmann Y., Schiele M.A., Schümann D., Lonsdorf T.B., Zwanzger P., Romanos M., Reif A., Domschke K., Deckert J., Gamer M., Pauli P. Individual differences in human fear generalization-pattern identification and implications for anxiety disorders. Transl. Psychiatry. 2019;9(1):307. doi: 10.1038/s41398-019-0646-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szczuka Z., Abraham C., Baban A., Brooks S., Cipolletta S., Danso E., Dombrowski S.U., Gan Y., Gaspar T., de Matos M.G., Griva K., Jongenelis M., Keller J., Knoll N., Ma J., Miah M., Morgan K., Peraud W., Quintard B., Shah V., et al. The trajectory of COVID-19 pandemic and handwashing adherence: findings from 14 countries. BMC Publ. Health. 2021;21(1):1791. doi: 10.1186/s12889-021-11822-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thabane L., Mbuagbaw L., Zhang S., Samaan Z., Marcucci M., Ye C., Thabane M., Giangregorio L., Dennis B., Kosa D., Borg Debono V., Dillenburg R., Fruci V., Bawor M., Lee J., Wells G., Goldsmith C.H. A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC Med. Res. Methodol. 2013;13:92. doi: 10.1186/1471-2288-13-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Development Programme . Human Development Data Center; 2021. Human Development Reports.http://www.hdr.undp.org/en/data [Google Scholar]
- Wang P.W., Ahorsu D.K., Lin C.Y., Chen I.H., Yen C.F., Kuo Y.J., Griffiths M.D., Pakpour A.H. Motivation to have COVID-19 vaccination explained using an extended Protection Motivation Theory among university students in China: the role of information sources. Vaccines. 2021;9(4):380. doi: 10.3390/vaccines9040380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun. Monogr. 1992;59(4):329–349. doi: 10.1080/03637759209376276. [DOI] [Google Scholar]
- World Health Organization WHO save lives: clean your hands in the context of COVID-19. 2020. https://www.who.int/infection-prevention/campaigns/clean-hands/WHO_HH-Community-Campaign_finalv3.pdf Available at:
- World Health Organization . 2021. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ [Google Scholar]
- Zhang W., Xiong S., Zheng Y., Wu J. Response efficacy and self-efficacy mediated the relationship between perceived threat and psychic anxiety among college students in the early stage of the COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2022;19(5):2832. doi: 10.3390/ijerph19052832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C., Yue X.D., Zhang X., Shangguan F., Zhang X.Y. Self-efficacy and mental health problems during COVID-19 pandemic: a multiple mediation model based on the Health Belief Model. Pers. Indiv. Differ. 2021;179 doi: 10.1016/j.paid.2021.110893. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data related to this paper as well as original study materials, outputs are available at https://osf.io/vmn2q/ except data for Germany, Malaysia, and Australia; based on decisions of the respective IRBs.