Abstract
BACKGROUND/OBJECTIVES:
To describe the caregiving experiences and physical and emotional needs of family members and friends who provide care to veterans with mental, physical, and cognitive comorbidities.
DESIGN:
Cross-sectional study.
SETTING:
National telephone surveys administered from 2017 to 2019.
PARTICIPANTS:
Family caregivers of veterans enrolled in the Veterans Affairs (VA) Program of General Caregiver Support Services between October 2016 and July 2018 who responded to a telephone survey (N = 1,509; response rate = 39%).
MEASUREMENTS:
We examined caregiver burden, depressive symptoms, financial strain, satisfaction with care, amount and duration of caregiving, life chaos, loneliness, and integration of caregiver with the healthcare team using validated instruments. We also collected caregiver demographic and socioeconomic characteristics and asked caregivers to identify the veteran’s condition(s) and provide an assessment of the veteran’s functioning.
RESULTS:
Average caregiver age was 62.2 (standard deviation [SD] = 13.7) and 69.8 (SD = 15.6) for veterans. Among caregivers, 76.7% identified at White, and 79.9% were married to the veteran. Caregivers reported having provided care for an average of 6.4 years and spending on average 9.6 hours per day and 6.6 days per week providing care. Average Zarit Subjective Burden score was 21.8 (SD = 9.4; range = 0–47), which is well above the cutoff for clinically significant burden (>16). Caregivers reported high levels of depressive symptoms; the sample average Center for Epidemiologic Studies Depression 10-item Scale score was 11.5 (SD = 7.1; range = 0–30). Caregivers also reported high levels of loneliness and financial strain.
CONCLUSION:
Caregivers who care for veterans with trauma-based comorbidities reported intensive caregiving and significant levels of distress, depressive symptoms, and other negative consequences. These caregivers require comprehensive support services including access to health care, financial assistance, and enhanced respite care. Planned expansion of VA caregiver support has the potential to provide positive benefits for this population and serve as a model for caregiver support programs outside the VA health care system.
Keywords: family caregiver, veteran, caregiver support, caregiver, informal caregiver
Family caregivers provide most long-term care for Americans in need of these services; care recipients are primarily older adults. In the United States, more than 17 million family members and friends provide assistance to a loved one aged 65 and older.1 Moreover, approximately 5.5 million individuals care for veterans or current military personnel; of these, 4.4 million provide care for veterans who served before September 11, 2001.2,3 Family caregiving has important benefits for patients and health systems because it reduces nursing home stays, inpatient visits, and formal home care use.4
Studies of mostly civilian family caregivers of older adults show caregivers experience wide-ranging negative effects such as physical stress, emotional distress, social isolation, and financial instability.1,5–8 Therefore, providing adequate support for family caregivers is critical, particularly because these support services improve caregiver well-being.1,9,10 Most programs that support family caregivers are managed at the state level, leading to considerable variability in assistance based on state of residence. As of June 2019, all 50 states provided assistance to older adults for community-based care, such as personal care services, through various mechanisms such as Medicaid waivers.11 However, the types of services offered and who can be compensated to provide home-based care differs by state; although most family caregivers are married to the care recipient, only 15 states allow spouses to be paid as caregivers.12 The National Family Caregiver Support Program (NFCSP) also funds states to assist family caregivers; support includes information on community-based services, training, and support groups. Although this support may improve caregiver outcomes,10,13 NFCSP programs are not uniformly available due to funding constraints.
Multiple programs have been implemented to specifically address the needs of caregivers of veterans. In 2010, the U.S. Congress mandated (PL 111–163) that the Department of Veterans Affairs roll out the most comprehensive set of support services for family caregivers in the country. This law established two programs: the Program of General Caregiver Support Services (PGCSS) and the Program of Comprehensive Assistance for Family Caregivers (PCAFC). PGCSS provides training and other supports for eligible caregivers of veterans of all service eras including respite care, support groups, and peer support mentoring.14 PCAFC includes services offered under PGCSS plus a stipend, enhanced respite care, health insurance, mental health care, and lodging/travel to accompany the veteran to VA medical appointments.15 Currently, PCAFC is only available for caregivers of eligible veterans who served in the U.S. military since September 11, 2001, and have a qualifying service-related injury.16 In 2018, Congress passed the VA Mission Act of 2018 (PL 115–182) that mandates the expansion of PCAFC services, albeit with staggered enrollment, to (1) include financial counseling, and (2) extend program eligibility to caregivers of qualified veterans from other service eras. This policy expansion has major implications for caregivers of veterans who are not currently eligible. For caregivers who qualify, participating in PCAFC may help caregivers access training and other supports. For caregivers who do not qualify, the expanded staffing and supports accompanying the mandate are intended to further bolster PGCSS features including psychological support and peer mentoring programs.14
As veterans age, we are beginning to observe how aging interacts with physical, mental, and cognitive comorbidities related to traumatic injuries. Yet our understanding of how these factors impact caregiver well-being and their need for supportive services is limited. This article describes the caregiving experiences and the physical and emotional needs of this caregiver population who may be eligible for PCAFC upon its expansion. Thus the study focuses on current PGCSS caregivers who may be likely to apply to PCAFC upon its expansion, rather than current PCAFC caregivers. The VA Caregiver Support Program (CSP) office requires information about the experiences of prospective applicants to PCAFC to target programmatic inputs that address caregiver challenges. Simultaneously, the VA is beginning to outsource care for veterans to community-based health providers; therefore, civilian health systems will need to understand how to support these caregivers. The experiences of military caregivers likely mirror experiences of nonmilitary caregivers who are also caring for loved ones with functional impairment and/or multiple chronic conditions including trauma-based illness.
DESIGN AND METHODS
Study Sample
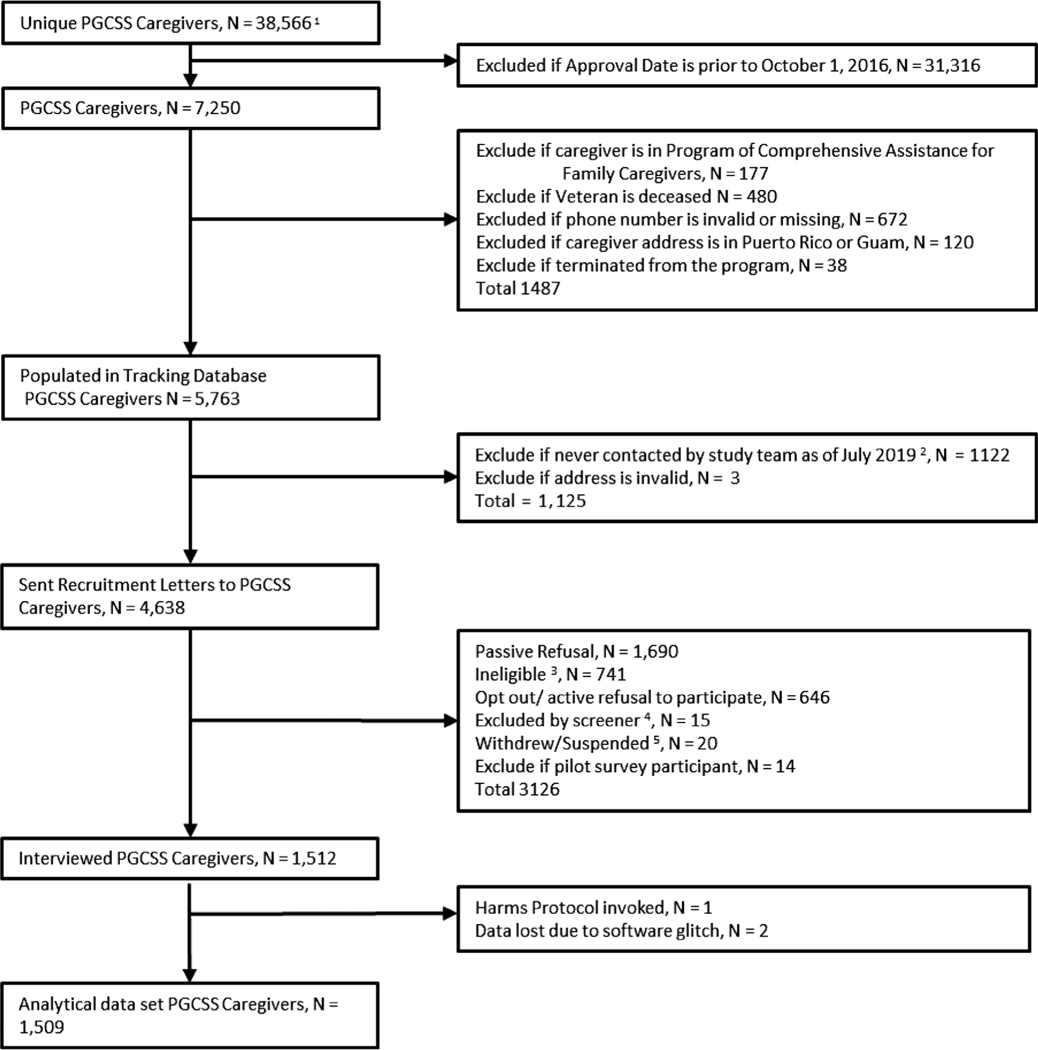
The analysis uses data collected through a national survey of caregivers of veterans before the expansion of the VA Mission Act. We recruited caregivers from a VA administrative list, the Caregiver Application Tracker (CAT), of caregivers enrolled in the PGCSS between October 2016 and July 2018 (Figure 1). To qualify for PGCSS, caregivers must be caring for a veteran with a demonstrated need for support with activities of daily living (ADLs) or instrumental activities of daily living (IADLs) for at least 6 months. Because PGCSS is a national program, we sampled caregivers from each VA Medical Center. All prospective caregivers were mailed a recruitment letter with a number to call to opt out if preferred. If caregivers did not opt out, they were contacted by phone and invited to participate. Data collection occurred through a survey administered over the phone by a team of research assistants and was stored using survey software, DatStat Illume and REDCap. A harms protocol was implemented to support highly distressed respondents and address any spontaneous disclosures of abuse or homicidal/suicidal ideation. The final analytic cohort was n = 1,509. The survey had a 39% response rate (Figure 1).
Figure 1.
Study flow. 1Based on the 2017 and 2018 raw Caregiver Application Tracker data pulls. 2Once initial recruitment goals of 1,500 were met, study team ceased recruitment. 3Ineligible reasons include if recruitment letter was returned with no forwarding address and no valid phone number available, veteran or caregiver deceased after data pull, caregiver no longer providing care. 4Exclusion reason: baseline never completed. 5Withdrew/suspended includes if the caregiver declined to continuing to participate in the survey after beginning the survey (eg, changed mind about participating, confidentiality/data concern, or too busy/no time). PGCSS, Program of General Caregiver Support Services.
Measures
We measured the following caregiver health and well-being outcomes using validated instruments commonly accepted in the caregiver literature: caregiver burden, depressive symptoms, financial strain, satisfaction with care, amount and duration of caregiving, life chaos, loneliness, and integration of caregiver with the healthcare team. We used an organizational framework to inform our choice of outcome measures; this framework shows how caregiver support services impact caregiver skills (eg, clinical nursing tasks, health system navigation, psychological coping) that influences the quality and intensity of care and impacts caregiver and patient outcomes (eg, general well-being, psychological and physical health, financial strain, and integration into the healthcare team).17,18 For all questions, caregivers may state “prefer not to answer.”
Caregiver Subjective Burden
We measured caregiver subjective burden using the Zarit Caregiver Burden instrument, a 12-item scale indicating frequency of level of stress experienced related to caregiving.19 Respondents are asked to indicate “Never,” “Rarely,” “Sometimes,” “Quite frequently,” or “Nearly always.” Questions cover health, psychological well-being, finances, social life, and the relationship between the caregiver and care recipient. Scores range from 0 to 48; higher scores indicate higher burden, and “a score >16 suggests clinically significant caregiver burden.”19–21
Depressive Symptoms
We used the Center for Epidemiologic Studies Depression 10-item Scale (CES-D-10) to measure caregivers’ symptoms of depression.22 Respondents can choose “Rarely or none of the time,” “Some or a little of the time,” “Occasionally or a moderate amount of the time,” or “Most or all of the time” regarding statements of frequency of depressive symptoms experienced in the past 7 days. The lowest possible score is 0 and the highest is 30, with higher scores signifying more depressive symptoms. A CES-D score of 8 or above or 10 or above is often used to indicate a positive screen of depressive symptoms and probable depression, respectively.22
Caregiver-Perceived Financial Strain
We measured perceived financial strain through the three-item Impact on Finances subscale from the Caregiver Reaction Assessment.23 This scale assesses whether caregivers feel that they have adequate resources to pay for needs related to caregiving, whether it is difficult to pay for things that the care recipient needs, and whether caregiving puts a financial strain on the caregivers. For each question, respondents can select “Strongly disagree,” “Disagree,” “Neither agree nor disagree,” “Agree,” or “Strongly agree” to indicate the degree of financial strain experienced. Scores range from 3 to 15; higher scores signify higher strain.23
Intensity of Caregiving
We measured intensity of caregiving using reported time spent caregiving (ie, average hours per day and average days per week). Additionally, we collected how long the caregiver has been serving as a family caregiver, estimated in months or years.
Life Chaos
Life chaos addresses constructs including daily routine and ability to plan. We measured life chaos using the six-item survey validated by Wong et al.24 Responses include “Strongly agree,” “Agree,” “Unsure,” “Disagree,” or “Strongly disagree.” In our sample, scores ranged from 6 to 36; a higher score indicates greater chaos.24
Loneliness
We measured loneliness using the three-item survey validated by Hughes et al.25 Responses include “Hardly ever,” “Some of the time,” and “Often” to questions about whether the individual perceives feeling left out, feeling isolated from others, and lacking companionship. This scale has been validated for phone-administered surveys. Scores range from 3 to 9; a higher score indicates a higher degree of loneliness.25
Caregiver Perceptions about Communication with Clinical Team Members
We measured caregiver perceptions of communication with the healthcare team using the instrument Caregiver Perceptions about Communication with Clinical Team Members (CAPACITY).26,27 It captures these domains: communication and the extent to which caregivers believe the patient’s health care team considers their capacity and preferences in medical decision making for the patient. Response options include “Always,” “Usually,” “Sometimes,” and “Never” for questions 1 and 3 to 12, and “Very well,” “Somewhat,” “A little bit,” and “Not at all well” for question 2.26 Scores range from 1 to 4 for the overall score and for each subscale; a higher score indicates improved level of perceived communication and capacity.26
Caregivers’ Global Satisfaction with Veterans Health Administration Care for Veterans
To measure caregivers’ satisfaction with veterans’ VHA care over the last 3 months, we used a single item from the Consumer Assessment of Healthcare Providers and Systems 2013 Health Plan survey.28 The scale measured from 0 to 10, with 0 indicating the worst health care possible and 10 indicating the best health care possible.28
We collected caregiver demographic and socioeconomic characteristics of age, sex, relationship to veteran, marital status, living distance from veteran, highest level of education, race/ethnicity, whether the caregiver is a veteran, self-reported health status, and health insurance coverage. We measured caregivers’ self-reported health status using one item from the 36-item short-form health survey (SF-36)29: “How would you rate your current health?” Possible responses include “Poor,” “Fair,” “Good,” “Very good,” and “Excellent.” Additionally, we measured caregivers’ current work status and work status before becoming a caregiver. Finally, we asked caregivers to identify the veteran’s condition(s) that required the need for caregiving and an assessment of veteran functioning using the Older Americans Resources and Services Activities of Daily Living and Instrumental Activities of Daily Living.30 We calculated veteran age using birthdate in CAT and survey date.
Statistical Analyses
We calculated descriptive statistics for the sociodemographic characteristics and well-being outcomes of caregivers. All analyses were conducted with SAS v.9.4 (SAS Institute, Inc, Cary, NC).
Ethical Considerations
This nonresearch evaluation was conducted under the authority of the CSP and Quality Enhancement Research Initiative (QUERI) and thus is classified as quality improvement. VHA Handbook 1058_05 (Veterans Health Administration 2011) provides guidance about authorization of manuscripts that have been developed through nonresearch activities (ie, without institutional review board approval under the authority of VHA operations). All VHA authors of this article attest that the activities that resulted in producing this manuscript were conducted as part of the nonresearch evaluation conducted under the authority of the CSP and QUERI. Caregiver responses were kept confidential to the researchers and anonymous to the operational partners in the VA CSP.
RESULTS
Sample Characteristics
Table 1 displays the demographic and socioeconomic characteristics of the 1,509 sample respondents reporting characteristics of a single veteran care recipient. The average age of caregivers was 62.2 (standard deviation [SD] = 13.7), with 30.6% aged 70 and older. The average age of veterans was 69.8 (SD = 15.6) with 60.3% aged 70 and older. When allowed to choose multiple race categories (ie, categories are not mutually exclusive), 76.7% caregivers marked White, 15.5% marked Black or African American, and 4.6% identified as American Indian or Alaska Native. Of respondents, 85.8% were married/living with a partner, and 79.9% were the spouse or significant other of the veteran. At the time of the survey, 12.1% reported working full time and 10.9% working part time, 46.1% reported being retired, 22.1% reported not working and not searching for paid work, and 5.8% reported being disabled. Before becoming a caregiver, 59.3% reported working full time, 15.2% reported working part time, and 15.4% reported being retired. Table 2 displays the self-reported health and well-being of the caregiver and health characteristics of the veteran. The average number of conditions a veteran had that necessitated the need for a caregiver was 3.9 (SD = 1.9). Of the conditions requiring a caregiver, the most frequently identified were depression (58.8%), physical injury or illness (53.4%), anxiety (49.6%), posttraumatic stress disorder (PTSD) (44.9%), Alzheimer’s or dementia (44.9%), and heart problems/heart disease (30.9%). Approximately 72.6% of caregivers reported the veteran’s health status as fair or poor. Nearly 30% of the veteran care recipients had no or missing service-connected disability; 13.2% had a 10% to 50% service connection; 21.8% had a 60% to 90% service connection, and 36.4% had a 100% service connection. Finally, 64.5% of caregivers reported that the veteran required assistance with 8 or more ADLs/IADLs.31
Table 1.
Caregiver and Veteran Demographics
| % | n | |
|---|---|---|
|
| ||
| Caregiver age, y, mean (SD), (n) | 62.2 (13.7) | 1,484 |
| Caregiver age, y, categories, % (n) | ||
| 20–29 | 1.9 | 28 |
| 30–39 | 5.8 | 87 |
| 40–49 | 10.0 | 151 |
| 50–59 | 18.0 | 272 |
| 60–69 | 32.0 | 483 |
| 70–79 | 21.9 | 331 |
| ≥80 | 8.7 | 132 |
| Missing/Prefer not to answer | 1.7 | 25 |
| Veteran age, y, mean (SD) (n) | 69.8 (15.6) | 1,509 |
| Veteran age, y, categories, % (n) | ||
| 20–29 | 1.2 | 18 |
| 30–39 | 5.7 | 86 |
| 40–49 | 6.2 | 94 |
| 50–59 | 8.2 | 123 |
| 60–69 | 18.4 | 278 |
| 70–79 | 33.3 | 502 |
| 80+ | 27.0 | 408 |
| Caregiver race: Mark all that apply | 4.6 | 70 |
| American Indian or Alaska Native | ||
| Asian | 1.9 | 28 |
| Black or African American | 15.5 | 234 |
| Native Hawaiian or Pacific Islander | .8 | 12 |
| White | 76.7 | 1,157 |
| Other | 4.8 | 73 |
| Missing/Prefer not to answer | 1.5 | 22 |
| Caregiver marital status, % (n) | ||
| Married or in a committed relationship/Living together | 85.8 | 1,295 |
| Not married or partnered | 13.9 | 210 |
| Missing/Prefer not to answer | .3 | 4 |
| Caregiver relationship to the veteran, % (n) | ||
| Spouse/Significant other | 79.9 | 1,205 |
| Parent | 2.1 | 31 |
| Child | 11.4 | 172 |
| Sibling | 2.3 | 34 |
| Other | 4.4 | 67 |
| Caregiver current work status, % (n) | ||
| Working full time (≥36 h/wk) | 12.1 | 183 |
| Working part time (≤35 h/wk) | 10.9 | 164 |
| Not working; searching for paid work |
1.8 | 27 |
| Not working; not searching for paid work |
22.1 | 333 |
| Retired | 46.1 | 696 |
| Disabled | 5.8 | 87 |
| Student | 1.1 | 17 |
| Missing/Prefer not to answer | .1 | 2 |
| Caregiver work status before caregiving, % (n) | ||
| Working full time (≥36 h/wk) | 59.3 | 895 |
| Working part time (≤35 h/wk) | 15.2 | 229 |
| Not working; searching for paid work |
.7 | 11 |
| Not working; not searching for paid work |
4.7 | 71 |
| Retired | 15.4 | 233 |
| Disabled | 3.2 | 48 |
| Student | 1.4 | 21 |
| Missing/Prefer not to answer | .1 | 1 |
| Veteran military separation date, % (n) | ||
| Before 9/11 | 85.9 | 1,296 |
| On or after 9/11 | 13.4 | 202 |
| Missing | .7 | 11 |
Abbreviation: SD, standard deviation.
Table 2.
Caregiver and Veteran Health and Well-being Characteristics
| % | n | Cronbach’s α | |
|---|---|---|---|
|
| |||
| Conditions requiring a caregiver, % a | NA | ||
| Depression | 58.8 | 887 | |
| Anxiety | 49.6 | 748 | |
| Posttraumatic stress disorder | 44.9 | 677 | |
| Headache | 24.9 | 375 | |
| Traumatic brain injury | 13.1 | 198 | |
| Bipolar disorder | 8.6 | 130 | |
| Other mental health illness | 7.3 | 110 | |
| Substance abuse | 6.2 | 94 | |
| Other physical illness or injury | 53.4 | 806 | |
| Alzheimer’s or dementia | 44.9 | 677 | |
| Heart problems/Heart disease | 30.9 | 466 | |
| Progressive neurological condition | 25.2 | 380 | |
| Cancer | 13.4 | 202 | |
| Spinal cord injury | 6.8 | 102 | |
| Amputation | 2.7 | 41 | |
| Veteran’s health status, % | NA | ||
| Veteran’s health status is poor or fair | 72.6 | 1,095 | |
| Veteran’s health status is good or better | 27.1 | 409 | |
| Missing/Prefer not to answer | .3 | 5 | |
| Mean number of IADLs/ADLs marked as unable or needs help (range = 0–13), mean (SD) | 8.7 (3.4) | 1,509 | NA |
| ADL/IADL problems categorized (13 ADLs/IADLs), % | .9 | ||
| Total IADL/ADL problems: Unable/Needs Help 8–13 ADLs/IADLs | 64.5 | 973 | |
| Severe IADL/ADL Problems: Unable/Needs Help 6–7 ADLs/IADLs | 16.3 | 246 | |
| Moderate IADL/ADL problems: Unable/Needs Help 4–5 ADLs/IADLs | 9.9 | 150 | |
| Mild IADL/ADL problems: Unable/Needs help 1–3 ADLs/IADLs | 8.1 | 122 | |
| No IADL/ADL problems | 1.2 | 18 | |
| Missing/Prefer not to answer | 0 | 0 | |
| Intensity of caregiving, mean (SD) | NA | ||
| Average hours per day | 9.6 (6.5) | 1,481 | |
| Average days per week | 6.6 (1.1) | 1,496 | |
| Years of caregiving | 6.4 (6.9) | 1,496 | |
| Caregiver subjective burden: Zarit Burden score mean (SD) | 21.8 (9.4) | 1,434 | .9 |
| Caregiver depressive symptoms: CES-D-10 score, mean (SD) | 11.5 (7.1) | 1,485 | .9 |
| Caregiver perceived financial strain, mean (SD) | 9.2 (3.7) | 1,464 | .8 |
| Caregiver life chaos, mean (SD) | 16.9 (4.9) | 1,464 | .7 |
| Caregiver loneliness, mean (SD) | 6.1 (2.1) | 1,449 | .8 |
| CAPACITY, mean (SD) | .9 | ||
| Communication subscale | 2.9 (.8) | 1,240 | |
| Caregiver Capacity subscale | 1.7 (.8) | 1,163 | |
| Caregiver global rating of satisfaction with VA care, mean (SD) | 8.1 (2.3) | 1,378 | NA |
| Caregiver’s health status, % | NA | ||
| Caregiver’s health status is poor or fair | 34.1 | 514 | |
| Caregiver’s health status is good or better | 65.1 | 983 | |
| Missing/Prefer not to answer | .8 | 12 | |
Abbreviations: ADL, activities of daily living; CAPACITY, Caregiver Perceptions about Community with Clinical Team Members; CES-D-10, Center for Epidemiologic Studies Depression 10-item Scale; IADL, instrumental activities of daily living; NA, not applicable; SD, standard deviation.
Categories are not mutually exclusive.
Respondents reported providing care for an average of 6.4 years and spending, on average, 9.6 hours per day and 6.6 days per week caring for the veteran. Caregivers also reported high levels of subjective caregiver burden with an average Zarit Subjective Burden score of 21.8 (SD = 9.4), well above the cutoff of clinically significant levels of burden (>16).19–21 Additionally, the average CES-D-10 score, 11.5 (SD = 7.1), was above the established threshold indicating probable depression.22 Caregivers also reported high levels of overall loneliness; mean score was 6.1 (SD = 2.1) on a scale of 3 to 9.25 Mean total score of perceived financial strain related to caregiving was 9.2 (SD = 3.7); the maximum score is 15, suggesting that, on average, caregivers reported experiencing fairly high levels of financial strain.23 Caregiver-reported average life chaos score was 16.9 (SD = 4.9).
Caregivers reported a mean score on the CAPACITY Communication subdomain of 2.9 (SD = .8) and Caregiver Capacity subdomain of 1.7 (SD = .8).8 These scores suggest that perceived communication with the healthcare team about the care recipient was higher than caregiver perception of the healthcare team assessing the caregivers’ own needs related to caregiving. The number of missing observations for this scale was substantially higher than other items largely because 16% of respondents were forced to skip this scale because the caregiver did not attend an appointment with the veteran or the veteran did not have an appointment in the last 6 months. Caregivers reported a high level of satisfaction with care that the veteran received at the VA; mean score was 8.1 (SD = 2.3) (Table 2). The Cronbach’s α for each validated subscale is listed in Table 2.
DISCUSSION
Among a sample of 1,509 caregivers enrolled in PGCSS, veteran care recipients required care for multiple conditions, most commonly for mental health conditions (eg, depression, anxiety, and PTSD), dementia, physical injuries or illnesses, and heart disease. Caregiving intensity was high; on average, caregivers provided care all days of the week and for most of the day. Distress and burden were well above clinical thresholds.19–22 Also, levels of self-reported loneliness and perceived financial strain were high.23,25
Caregivers in this sample provide care for veterans with traumatic stress and other injuries. Traumatic stress is associated with higher rates of disability and other negative health outcomes for veterans.32 PTSD and other mental health conditions may augment aging-related diseases such as dementia and heart disease.32–34 Although these conditions are challenging for caregivers to manage in isolation, their co-occurrence substantially complicates care.
The challenges associated with caring for patients with comorbid mental, physical, and cognitive conditions may drive higher rates of physical burden and distress among caregivers. For instance, PTSD-dementia caregivers were at higher risk for negative physical health outcomes.35 Another study found that caregivers of older adults with mental illness experienced feelings of isolation, concerns about stigma, high emotional distress, and poor self-reported health.36
Despite these challenges, health system support for caregivers can improve caregiver and patient outcomes. Caregivers also report that emotional support from peer mentors and VA staff through the CSP was beneficial.14 REACH VA, an education and skills training program targeting caregivers of veterans with dementia, may decrease caregiver burden and depression and reduce dementia-related problem behaviors in patients.37 This training program will be offered to all caregivers under the enhanced PGCSS.
Our findings also demonstrated financial distress among respondents. Expanded financial assistance should have positive effects. The Cash and Counseling Demonstration Project, a consumer-directed program that gave care recipients cash benefits to pay for long-term care needs, had positive effects on patient quality of life and caregiver physical health and emotional and financial distress.38 Within the VA, research on caregivers of post-9/11 veterans with comorbid physical and mental health conditions demonstrates the benefits of comprehensive support. Caregivers in PCAFC reported feeling more confident in their caregiving skills and more aware of VA resources.39 Veterans whose caregivers received financial support through PCAFC had higher rates of outpatient mental and physical health services.40,41
Strengths and Limitations
Our article is the first to report the characteristics and caregiving experiences of a large sample of caregivers of veterans with complex comorbid physical, mental, and cognitive health conditions who are not participating in PCAFC. Strengths of this study are that we identified a large national sample of family caregivers through the VA CSP administrative data and our standardized recruitment process. The limitations of this study are that we did not recruit caregivers who had not interacted with PGCSS. Also, it is possible that survey participants were either (1) less distressed than caregivers who declined to participate because of the overwhelming daily tasks of caregiving, or (2) more distressed and hope that by completing the survey they will receive assistance. Finally, although we measured satisfaction with VA care, we did not measure caregiver satisfaction with PGCSS that would have been helpful for targeted program improvement.
Implications and Conclusions
Caregivers in our sample have a high need for emotional support, respite care services, engagement with other caregivers, and training in disease education and clinical skills to provide care. Despite these needs, caregivers report some level of communication with VA health providers and high levels of satisfaction with VA care. Based on prior research about comprehensive caregiver support,38,40,42 it is likely that these caregivers would benefit substantially from financial assistance, access to health care, and enhanced respite care. VA is a promising setting to test a comprehensive caregiver support model for caregivers of older adults with trauma-based and other comorbidities. Potential benefits of comprehensive caregiver support include decreased stress, decreased financial burden, and improved mental and physical health.43
VA offers the most comprehensive support program for caregivers available in the United States. In the absence of other widely available programs, the results of our study begin to build an evidence base that could be applied to similar CSPs for civilian populations. Given that these caregivers report feeling lonely and disconnected from support services, it would be beneficial to conduct outreach activities to build awareness and to solicit applications from those who are less engaged in the healthcare system or live in rural communities.14 Another way to identify caregivers who might benefit is to encourage providers to recognize the dual role that caregivers play as a loved one of the patient and a member of the healthcare team. Because caregivers report that the patients’ providers often do not assess the caregiver’s own needs, health systems could consider instituting routinized screening for distress and referral mechanisms to caregiver support services. For example, the Elizabeth Dole Foundation’s Campaign for Inclusive Care has implemented a VA-wide program to train providers to integrate caregivers into the veteran’s healthcare team. Moreover, with the move to the Cerner electronic health record, VA will now identify caregivers as nonmedical providers, thereby explicitly linking caregivers to the care recipient in the medical record. When healthcare providers open a veteran’s record, they will be able to see whether or not they have a caregiver and, if so, the caregiver’s contact information.
In sum, PCAFC has already proven to be impactful policy initiative for caregivers and veterans. Expansion of the program through the Mission Act will likely confer similar benefits on a population in high need of additional support. For caregivers who do not qualify for PCAFC, CSP is also enhancing PGCSS services such that caregivers have access to multiple programs of supports (eg, skills education for caring for older adults with PTSD and dementia and suicide prevention training). An area for future research is to evaluate the impact of PGCSS on caregiver outcomes. Moreover, the VA’s ability to demonstrate the positive impact of comprehensive support for family caregivers has the potential to initiate a sector-wide culture shift around how health systems can and should support caregivers.
ACKNOWLEDGMENTS
We gratefully acknowledge the survey respondents for their time and for sharing their experiences as caregivers for veterans. We also gratefully acknowledge excellent research assistance from Laurie Marbrey, Neerali Patel, and Kaileigh Gray.
Financial Disclosure:
The analysis was funded by the VA Caregiver Support Program, Health Services Research and Development, and the Quality Enhancement Research Initiative (PEC 14-272), and it was supported by the Center of Innovation to Accelerate Discovery and Practice Transformation at the Durham VA Health Care System (Grant No. CIN 13-410).
Sponsor’s Role:
None.
Footnotes
Disclaimer
This work is classified as quality improvement and not research. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the U.S. government, Duke University, or the University of North Carolina.
Conflict of Interest: The authors have declared no conflicts of interest for this article.
REFERENCES
- 1.Committee on Family Caregiving for Older Adults; Board on Health Care Services; Health and Medicine Division; National Academies of Sciences, Engineering and Medicine. Families Caring for an Aging America. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 2.Family Caregiver Alliance. Caregiver statistics: demographics. 2019. https://www.caregiver.org/caregiver-statistics-demographics. Accessed March 15, 2020.
- 3.Ramchand R, Tanielian T, Fisher MP, et al. Hidden Heroes: America’s Military Caregivers. Santa Monica, CA: RAND Corporation; 2014. [PMC free article] [PubMed] [Google Scholar]
- 4.Van Houtven CH, Norton EC. Informal care and health care use of older adults. J Health Econ. 2004;23:1159–1180. [DOI] [PubMed] [Google Scholar]
- 5.AARP Public Policy Institute; National Alliance for Caregiving. Caregiving in the U.S. 2015. https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf. Accessed September 10, 2017.
- 6.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176:372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ornstein KA, Wolff JL, Bollens-Lund E, Rahman OK, Kelley AS. Spousal caregivers are caregiving alone in the last years of life. Health Aff. 2019;38: 964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bremault-Phillips S, Parmar J, Johnson M, et al. The voices of family caregivers of seniors with chronic conditions: a window into their experience using a qualitative design. Springerplus. 2016;5:620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lorig K, Ritter PL, Laurent DD, Yank V. Building better caregivers: a pragmatic 12-month trial of a community-based workshop for caregivers of cognitively impaired adults. J Appl Gerontol. 2019;38:1228–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCurry SM, Logsdon RG, Pike KC, LaFazia DM, Teri L. Training area agencies on aging case managers to improve physical function, mood, and behavior in persons with dementia and caregivers: examples from the RDAD-northwest study. J Gerontol Soc Work. 2018;61:45–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paying for Senior Care. Medicaid’s Home Care Benefits: Eligibility, Waivers & Application Information. 2019. https://www.payingforseniorcare.com/medicaid-waivers/home-care. Accessed October 10, 2019.
- 12.Paying for Senior Care. Paying Spouses to Care for their Elderly or Disabled Partners—Medicare, Medicaid, VA & Other Options. 2019. https://www.payingforseniorcare.com/paying-spousal-caregivers. Accessed February 3, 2020.
- 13.Avison C, Brock D, Campione J, et al. Outcome Evaluation of the National Family Caregiver Support Program. Rockville, MD: Westat; 2018. [Google Scholar]
- 14.Bruening R, Sperber N, Miller K, et al. Connecting caregivers to support: lessons learned from the VA caregiver support program. J Appl Gerontol. 2020;39(4):368–376. [DOI] [PubMed] [Google Scholar]
- 15.Miller KM, Kabat M, Henius J, Harold C, Van Houtven H. Engaging, supporting, and sustaining the invisible partners in care: young caregivers of veterans from the post-9/11 era. N C Med J. 2015;76:320–322. [DOI] [PubMed] [Google Scholar]
- 16.Caregivers and Veterans Omnibus Health Services Act of 2010. Washington, DC: United States of America: 111th Congress; 2010:1129. [Google Scholar]
- 17.Van Houtven CH, Voils CI, Weinberger M. An organizing framework for informal caregiver interventions: detailing caregiving activities and caregiver and care recipient outcomes to optimize evaluation efforts. BMC Geriatr. 2011;11:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith VA, Lindquist J, Miller KEM, et al. Comprehensive family caregiver support and caregiver well-being: preliminary evidence from a pre-post-survey study with a non-equivalent control group. Front Public Health. 2019;7:122–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bedard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M. The Zarit burden interview: a new short version and screening version. Gerontologist. 2001;41:652–657. [DOI] [PubMed] [Google Scholar]
- 20.O’Rourke N, Tuokko HA. Psychometric properties of an abridged version of the Zarit burden interview within a representative Canadian caregiver sample. Gerontologist. 2003;43:121–127. [DOI] [PubMed] [Google Scholar]
- 21.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649–655. [DOI] [PubMed] [Google Scholar]
- 22.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 23.Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15:271–283. [DOI] [PubMed] [Google Scholar]
- 24.Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007;22:1286–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Houtven CHV, Miller KEM, O’Brien EC, et al. Development and initial validation of the caregiver perceptions about communication with clinical team members (CAPACITY) measure. Med Care Res Rev. 2017;76:784–806. [DOI] [PubMed] [Google Scholar]
- 27.Van Houtven CH, Lippmann S, Belanger E, et al. Quality of communication with the health care team for care partners of persons with congitive impairment. Innov Aging. 2019;3:S206–S207. [Google Scholar]
- 28.Hargraves JL, Hays RD, Cleary PD. Psychometric properties of the consumer assessment of health plans study (CAHPS) 2.0 adult core survey. Health Serv Res. 2003;38:1509–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 30.George LK, Fillenbaum GG. OARS methodology. A decade of experience in geriatric assessment. J Am Geriatr Soc. 1985;33:607–615. [DOI] [PubMed] [Google Scholar]
- 31.Doble SE, Fisher AG. The dimensionality and validity of the Older Americans Resources and Services (OARS) Activities of Daily Living (ADL) scale. J Outcome Meas. 1998;2:4–24. [PubMed] [Google Scholar]
- 32.Byers AL, Covinsky KE, Neylan TC, Yaffe K. Chronicity of posttraumatic stress disorder and risk of disability in older persons. JAMA Psychiatry. 2014;71:540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67: 608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qureshi SU, Kimbrell T, Pyne JM, et al. Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. J Am Geriatr Soc. 2010;58:1627–1633. [DOI] [PubMed] [Google Scholar]
- 35.Pinciotti CM, Bass DM, McCarthy CA, et al. Negative consequences of family caregiving for veterans with PTSD and dementia. J Nerv Ment Dis. 2017; 205:106–111. [DOI] [PubMed] [Google Scholar]
- 36.National Alliance for Caregiving, Mental Health America, National Alliance on Mental Illness. On Pins and Needles: Caregivers of Adults with Mental Illness. Bethesda, MD: National Alliance for Caregiving; 2016. [Google Scholar]
- 37.Nichols LO, Martindale-Adams J, Burns R, Graney MJ, Zuber J. Translation of a dementia caregiver support program in a health care system–REACH VA. Arch Intern Med. 2011;171:353–359. [DOI] [PubMed] [Google Scholar]
- 38.Doty P, Mahoney KJ, Simon-Rusinowitz L. Designing the cash and counseling demonstration and evaluation. Health Serv Res. 2007;42:378–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sperber NR, Boucher NA, Delgado R, et al. Including family caregivers in seriously ill veterans’ care: a mixed-methods study. Health Aff (Millwood). 2019;38:957–963. [DOI] [PubMed] [Google Scholar]
- 40.Van Houtven CH, Smith VA, Stechuchak KM, et al. Comprehensive support for family caregivers: impact on veteran health care utilization and costs. Med Care Res Rev. 2019;76:89–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shepherd-Banigan M, Smith VA, Maciejewski ML, et al. The effect of support and training for family members on access to outpatient services for veterans with posttraumatic stress disorder (PTSD). Adm Policy Ment Health. 2018;45:550–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coe NB, Guo J, Konetzka RT, Van Houtven CH. What is the marginal benefit of payment-induced family care? Impact on Medicaid spending and health of care recipients. Health Econ. 2019;28:678–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith VA, Lindquist JL, Miller KEM, et al. Comprehensive family caregiver support and caregiver well-being: preliminary evidence from a pre-post survey study with a non-equivalent control group. Front Public Health. 2019;22:7–122. [DOI] [PMC free article] [PubMed] [Google Scholar]