Abstract
Video Abstract
CONTEXT
Adverse childhood experiences (ACEs) are associated with increased risk of poor mental health outcomes. Although there is interest in screening for ACEs for early identification and intervention, it is not known whether screening improves outcomes for children.
OBJECTIVE
To systematically review whether screening for ACEs in children leads to an increase in (1) identification of ACEs, (2) referrals to services, (3) increased uptake of services, and (4) improved mental health outcomes for children and parents.
DATA SOURCES
Ovid Medline, PsycINFO, CINAHL, and Center for Clinical and Translational Research electronic databases were searched between 2009 and 2021.
STUDY SELECTION
Studies were included if researchers screened for current ACEs in children aged 0 to 12 years and they had a control comparison.
DATA EXTRACTION
Information was extracted, including study characteristics, sample demographics, screening tool characteristics, referral rates to services, uptake rates, and mental health outcomes.
RESULTS
A total of 5816 articles were screened, with 4 articles meeting inclusion criteria. Screening for ACEs increases identification of adversity and may increase referrals to services. There are limited data about whether this leads to an increase in referral uptake by families. There are no reported data addressing mental health outcomes.
LIMITATIONS
There are few published control trials of moderate quality.
CONCLUSIONS
There is limited evidence that screening for ACEs improves identification of childhood adversity and may improve referrals. If we are to realize the hypothesized benefits of ACEs screening on child and parent mental health, it is essential to understand the barriers for families taking up referrals.
Adverse childhood experiences (ACEs) are defined as stressful or potentially traumatic events that occur before age 18 years and have a negative lasting effect on health and well-being. ACEs include physical, emotional, and sexual abuse and household dysfunction, such as parental mental illness, intimate partner violence (IPV), parental drug abuse, and parental separation. The seminal ACEs study from Kaiser Permanente, San Diego,1 revealed a link between exposure to ACEs and poor adult health outcomes, including ischemic heart disease, lung disease, and cancer. It showed a dose response, with exposure to a higher number of ACEs associated with an increased risk of poor health outcomes.1 Subsequent research has shown a link between ACEs and poor developmental and mental health outcomes in adolescents, including developmental and educational delays, poor school engagement, anxiety, and depression.2–4 Exposure to adversity does not only impact future adult health and well-being; impacts on health outcomes are evident in young children, and poorer developmental outcomes are seen in the first 3 years of life.5,6 In addition, other adversities, such as being a victim of bullying, exposure to community violence, and food scarcity, have been demonstrated to have a similar effect on long-term health outcomes as the original ACEs, leading to a call to expand the definition of ACEs.7,8
Screening for ACEs has been suggested as a public health measure by various health organizations in the United Kingdom and United States9–14 as a way to improve long-term health outcomes for children and their families. California has become the first state to start screening all children aged <18 years after a 160 million dollar initiative for children on Medi-Cal, California’s insurance for low-income people.15 The UK government made a commitment in 2015 to explore the implementation of routine ACEs screening for adolescents and adults.16 The American Academy of Pediatrics recommended in 2012 that pediatricians ask about both parent and child ACEs. However, in a national survey of pediatricians, 61% did not ask about any ACEs, and only 2% rated that they were familiar with the ACEs study.3,17,18
There are a number of controversies surrounding routine screening for ACEs, including debate about which ACEs to screen for,8 the ethics of screening when there are no clear evidence-based interventions for ACEs, and whether screening for ACEs is cost-effective given the time, effort, and training required to implement routine screening.13,19 There are no clear guidelines on what thresholds to use for referral after screening, which may lead to overburdening the social sector.19 ACEs screening may be harmful because some patients find it intrusive and retraumatizing,9,20–23 and it may disrupt the trust in the relationship with the health professional.19 In addition, screening for ACEs could trigger mandatory reporting to child protection services, which may be harmful or create stigma in families and result in reduced engagement.13,24 Physicians are often reluctant to screen for ACEs because of lack of time, reimbursement, or a lack of confidence to discuss trauma.25,26
Decisions about when and how to screen populations remain challenging. Wilson and Jungner’s27 principles of screening remain an important tool in decision-making and have formed the backbone of modern screening principles. Wilson and Jungner state that to screen for a condition there needs to be a suitable and acceptable screening test (ie, sensitive and specific), as well as accepted treatment, which is available and economically viable. In addition, there needs to be evidence of effectiveness and cost effectiveness, as demonstrated by randomized controlled studies. Wilson and Junger’s principles for screening have been updated to include a focus on operational and implementational issues, in addition to disease and test and/or intervention principles.28 In these updated principles, the overall benefit of the screening program needs to outweigh the potential harms, and there needs to be adequate infrastructure, coordination, and integration of the screening program within the broader health system.28 In applying these principles to screening for ACEs, challenges remain in regard to an acceptable and robust universal screening test, interventions that are readily available and will modify the natural history of childhood adversity, and operational challenges related to implementing screening within the broader health system.
In addition, before any population screening is undertaken, there needs to be a thorough review of the evidence supporting screening for ACEs, as has been done for other screening programs by the US Preventive Services Task Force.29 For example, screening for depression in the perinatal period has been demonstrated to be efficacious and is thus recommended by the US Preventive Services Task Force.30,31
Accurate identification of children living with adversity is paramount to be able to intervene through parenting support and education, mental health counseling, customized health care according to the needs of the family, connection to community-based services, and care coordination. These interventions have been shown to improve outcomes for children exposed to ACEs.32,33 However, the degree to which they are occurring in health and community services is often unknown. Connection to community-based services would be expected to lead to improved short-term outcomes, whereas improved long-term outcomes would likely need a multipronged approach to intervention.
Previous reviews of routine screening of adults for ACEs have revealed that screening is feasible and acceptable in primary health care settings.34 There has been no systematic synthesis of the available evidence to determine if screening for a comprehensive range of ACEs improves outcomes for children; the ultimate goal of screening. Given the strong association between ACEs and poor mental health outcomes, in this systematic review, we sought to determine if routine screening for ACEs in children leads to (1) better detection of adversity, (2) improved rates of referrals to services to address adversity or its childhood impacts, (3) improved uptake of referrals by families, and (4) improved mental health outcomes for children or parents.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.35 The study protocol was registered with the International Prospective Register of Systematic Reviews (registration number CRD42020196442) on August 2, 2020.
Literature Search
A systematic literature search was performed with the input of a professional research librarian by using the Ovid Medline, PsycINFO, CINAHL, and Cochrane Controlled Register of Trials electronic databases. The search included relevant peer-reviewed articles published between January 1, 2009, and January 31, 2021. Articles were restricted to those published in English. Key words included “adverse childhood experiences screening” OR “child adversity screening” OR “benefits child adversity screening” OR “harm child adversity screening” OR “benefits child ACEs screening” OR “harm child ACEs screening.” The full list of search terms is found in the Supplemental Information.
Studies were included if they met the following criteria: (1) children aged 0 to 12 years who are screened for current adversity; (2) randomized clinical trials or quasi-experimental designs with a control group; (3) screening for ACEs and/or screening for broader social determinants of health (SDOH), such as poverty, food insecurity, housing instability or community violence; and (4) screening was conducted by a practitioner using either a questionnaire or interview with a standard set of questions. Exclusion criteria included studies that (1) focused on screening of adolescents (age >12 years) or adults, (2) screened for only 1 ACE, (3) were set in a low- or middle-income country, or (4) screened for adversity as part of inclusion criteria for an intervention and provided no outcome measures of screening.
Study Selection
Studies were independently double screened by 3 authors (S.L., K.P., L.C.) for inclusion by using Covidence software (v2431).36 Any conflicts about inclusion were resolved through discussion with the primary author. Screening was followed by full-text review by 2 authors (S.L. and T.H.) to assess eligibility against the inclusion and/or exclusion criteria. All articles in full-text review were double screened. Disagreement was resolved through discussion between the 2 authors (S.L. and T.H.) or by referral to a third author (H.H.). The interrater agreement was >95%.
Data Extraction
Two authors (S.L. and T.H.) independently extracted data from all included studies using a standard data extraction template in Covidence software. Data extracted included the following information: (1) study characteristics, including country location, research design, year of publication, number of participants; (2) participant characteristics, including age, sex, education level, race, age of child, and financial support and/or Medicaid (public health insurance); (3) screening tool and measurement of ACE or adversity; and (4) outcomes, including referral rates, uptake of referrals, community service engagement, mental health service involvement, and child and parent mental health. The extraction forms were compared, and consensus was reached with discussion between 2 authors (S.L. and T.H.).
Quality Assessment
Two authors (S.L. and T.H.) independently assessed the quality of the included studies using the ROBINS-I (risk of bias in nonrandomized studies of interventions)37 tool for assessing the risk of bias in nonrandomized studies and the Cochrane risk-of-bias tool for randomized studies38 in Covidence software. Discrepancies were resolved with discussion between 2 authors (S.L. and T.H.).
Results
Studies Selected
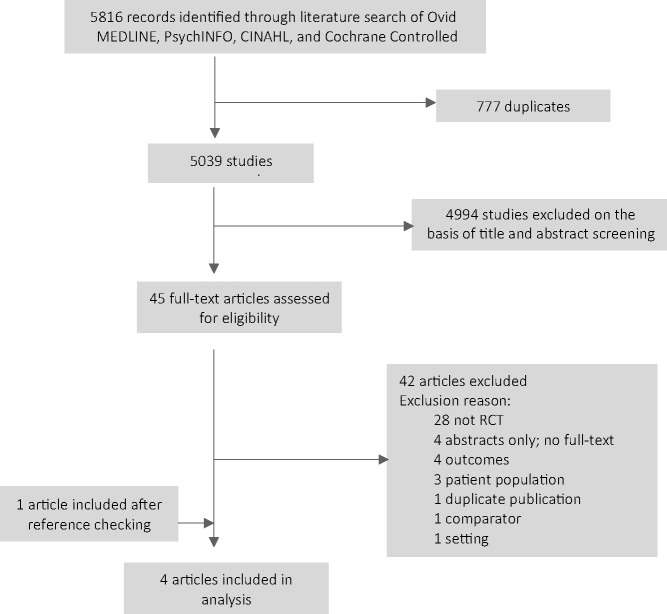
The PRISMA flow diagram (Fig 1) outlines the search strategy and results. The initial search identified 5816 articles. After removal of duplicates, 5039 articles were screened by title and abstract, and 45 articles were identified for full-text review. Three articles met the inclusion criteria after full-text review and were included in the analysis. By hand-searching references, we identified one additional article that met inclusion criteria.
FIGURE 1.
PRISMA flow diagram.
Study Characteristics
A summary of the studies included in this systematic review is presented in Table 1. All 4 studies took place in a health setting in the United States, with 3 studies based in a primary care pediatric clinic and the remaining study based in a nurse home-visiting program. In all studies, screening for ACEs occurred as part of routine well-child care. Screening for ACEs was not undertaken opportunistically when families presented for other health-related care and only occurred at specific well-child appointments.
TABLE 1.
Trial Summary Characteristics
| Source (Year, Location) | Design | Setting | Total Participant, N | Mean Maternal Age, y | Mean Child Age, mo | Medicaid, % | Ethnicity, % | Screening Test | ACE(s) Screened | Outcome Measures |
|---|---|---|---|---|---|---|---|---|---|---|
| Dubowitz (2009, United States) | RCT | Well-child assessments at primary pediatric clinics | 558 | 25.3 | 6a | 93 | Black, 93; White, NR; Hispanic, NR | PSQ | Parental depression, parental substance abuse, harsh punishment, major parental stress, IPV, and food insecurity | Reduction in childhood maltreatment as per reports to child protection, review of child chart, and CTSPC |
| Dubowitz (2012, United States) | RCT | Well-child assessments at primary pediatric clinics | 1119 | 28.3 | 25a | 12 | Black, 4; White, 86; Hispanic, 1 | PSQ | Parental depression, parental substance abuse, harsh punishment, major parental stress, IPV, and food insecurity | Reduction in childhood maltreatment as per reports to child protection, review of child chart, and CTSPC |
| Garg (2015, United States) | Cluster RCT | Well-child assessments at primary pediatric clinics | 336 | 28.5 | 2.5 | 81 | Black, 44; White, 24; Hispanic, 23 | PHQDS, Children’s HealthWatch survey | Child care, food security, household heat, housing, parent education and employment, and maternal depression | New enrollment in community-based resource; referral to community services |
| Dauber (2019, United States) | Quasi-experimental | Home-visiting program | 1165 | 26.35 | NR | 85 | Black, 37; White, 42; Other, 15 | EPDS, UNCOPE, and Relationship Assessment Tool | Postnatal depression, substance use, and IPV | Risk identification, risk discussion, and referral to community services |
EPDS, Edinburgh Postnatal Depression Scale; NR, not reported; PHQDS, Personal Health Questionnaire Depression Scale; UNCOPE, Used, Neglected, Cut Down, Objected Preoccupied, Emotional Discomfort.
Intervention group.
All 4 studies enrolled families with children aged <5 years, with mean ages between 2.5 and 25 months.39–41 There were 3178 children enrolled across the 4 studies (range 336–1149). The study populations differed in ethnicity and enrollment in Medicaid (public health insurance program). Three studies had either mixed or majority Black populations and high rates (>80%) of Medicaid enrollment39,41,42 compared with 1 study that had a predominately White population with only 12% of families enrolled in Medicaid.40
Screening
There were a range of ACEs screened across the studies. Two studies40,41 used the parent screening questionnaire (PSQ), which screens for a range of childhood adversities, including parental depression, parental substance abuse, harsh punishment, major parental stress, IPV, and food insecurity. One study39 used 12 questions from the Children’s HealthWatch survey to screen for child care needs, food security, household heat, housing, parent education, and employment and used the Personal Health Questionnaire Depression Scale to screen for maternal depression. One study42 used specific tools to screen for maternal depression (Edinburgh Postnatal Depression Scale), substance use (UNCOPE [Used, Neglected, Cut Down, Objected Preoccupied, Emotional Discomfort]), and IPV (Relationship Assessment Tool). Screening for ACEs was followed-up with motivational interviewing techniques by the practitioner who undertook the screening and planned referral to community-based services in all 4 studies.
Risk of Bias
There was moderate risk of bias in all studies on quality assessment (Tables 2 and 3), with significant missing data and low fidelity to study intervention,42 lack of blinding by outcome assessors and baseline differences,40,41 and unclear random assignment and allocation bias.39
TABLE 2.
Risk-of-Bias Assessment: Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomized Trials
| Study | Sequence Generation | Allocation Concealment | Blinding of Participants | Blinding of Outcome Assessors | Incomplete Data | Selective Reporting | Other Bias |
|---|---|---|---|---|---|---|---|
| Dubowitz 2009 | Low | High | High | High | Low | Low | High |
| Dubowitz 2012 | Low | High | High | High | Low | Low | High |
| Garg 2015 | Unclear | Unclear | High | Low | Low | Low | Low |
TABLE 3.
Risk-of-Bias Assessment: Robins-I Tool (Risk of Bias in Nonrandomized Studies of Interventions)
| Study | Confounding | Selection of Participants | Classification of Interventions | Deviation From Intended Interventions | Measurement of Outcomes | Incomplete Data | Selective Reporting |
|---|---|---|---|---|---|---|---|
| Dauber 2019 | High | Low | Low | High | Low | High | Low |
Outcomes
Meta-analysis was not possible because of the small number of studies and the significant heterogeneity in terms of interventions and outcomes reported. Therefore, a narrative description of outcomes is presented.
Screening for ACEs improved detection of some adversities in children in all studies compared with controls. Only 2 studies reported an improvement in screening rates. Dubowitz at al41 reported that screening for adversity improved by between 20% and 25%, whereas Dauber et al42 reported an improvement between 4% and 12% overall. Although home visitors reported that they were more likely to discuss substance use, IPV, and maternal depression with families, there was no statistically significant improvement in risk identification for substance use or IPV.42
Two studies reported the effect of screening for ACEs on referral rates. Garg et al39 reported that screening resulted in improved referrals to community-based health and social services, with mothers in the intervention group receiving significantly more referrals than those in the control group (70% vs 8%; adjusted odds ratio [OR] = 29.6; 95% confidence interval [CI] 14.7–59.6). At follow-up (at 12 months), more mothers in the intervention group were enrolled in community services than mothers in the control group (39% vs 24%; adjusted OR = 2.1; 95% CI 1.2–3.7).39 This contrasted with a study by Dauber et al42 in which there was minimal impact on referrals to community services (maternal depression referral OR 1.11, 95% CI 0.72–1.72; substance use referral OR 16.79, 95% CI 2.04–138.21; and IPV referral OR 2.49, 95% CI 1.27–4.91). However, there was low fidelity to the study protocol, so even when risks were identified through screening, only 32% of families received any case management including referrals.42
Two studies by Dubowitz et al40,41 reported on rates of referral to child protection services. Screening for ACEs in a low-socioeconomic population resulted in a decrease in referral to child protection services for the intervention group (OR 1.5; 95% CI not reported).41 However, use of the same screening tool in a middle and/or high socioeconomic population had no effect on referrals to child protection services.40
None of the studies reported mental health outcomes for children or parents. Most of the studies had limited follow-up between 642 and 12 months,39,40 with one study reporting no defined length of follow-up.41 None of the studies measured harms of screening for ACEs.
Discussion
This systematic review sought to identify whether screening for ACEs improves identification of adversity, referral to services, uptake of services, and better mental health outcomes for children and their parents. There is some evidence that screening for ACEs improves identification of adversity and limited evidence that screening may improve connection to community-based services and uptake of these services. There were no reported measures of mental health outcomes after screening for children or parents. This systematic review did not establish clear evidence that screening for ACEs improves any of our outcomes of interest. The evidence is limited because there were only 4 studies identified in our time period of interest, all of which were conducted in the United States and were of moderate quality.
From the studies in this systematic review, there was limited evidence that screening for ACEs improves identification of adversity, aligning with evidence from previous literature examining screening for ACEs or SDOH in children and parents.43–47 However, it is difficult to compare screening studies because all the studies in our review screened for different ACEs, using different tools, and one study screened for SDOH in addition to screening for one ACE.39 This is in part due to the lack of a universal definition of ACEs and a lack of agreement about which ACEs or other adversities for which to screen.7 In addition, increased rates of identification do not necessarily equate to better detection of adversity, which can be conceptualized as accurate identification of families living with adversity who would benefit from interventions. Moreover, although ACEs have been clearly demonstrated to be linked to poor health outcomes at a population level, ACEs cannot be used to predict an individual’s risk for chronic illness or mental health difficulties. Screening for ACEs in adults and children has limited ability to inform individual risk of poor health outcomes.48
This systematic review revealed mixed findings for the effect of screening for ACEs on connection to community-based services. Although screening for ACEs or SDOH can lead to increased referral rates to community-based services,43,44,49,50 referral and uptake of community services after a positive screen is dependent on health professional, parent, and systems factors. There are few current practice data on rates of referral to community services. Garg et al51 conducted a survey of pediatricians in the United States and found that 85% reported referring at least 1 family to community services in the past year; however, referrals for housing services and food support were low. From the 2 studies in this systematic review that reported on referral rates, the baseline referral rates to community services were low, between 2% and 8%.39,42 There are a number of barriers for providers in undertaking and responding to screening. Primary care providers, in the United States, report that they have incomplete knowledge about services and, thus, are less likely to make referrals.52 Primary care providers may also be ambivalent about screening for ACEs in part because of the lack of clarity about what referrals to make and concerns about lack of community resources.19,53,54 Pediatricians are less likely to refer to services with long waiting times.55 Uncontrolled studies have demonstrated low referral rates after positive ACEs or SDOH screening, with <30% of families having external referrals made in clinic-based or home visiting–based screening.45,52,56,57 Other studies have shown a variable acceptance of referrals by parents. Of parents who screened positive for ACEs in uncontrolled studies, between 53% and 77% consent for community services,52,53,58 with one study reporting rates as low as 14% of parents taking up referrals to community services.52 In qualitative studies of parental engagement, researchers have identified a number of barriers, including a lack of time, stigma, and a lack of perceived benefit from the referral.59
Referrals to child protection services is also a factor when considering ACEs screening. Dubowitz et al40,41 reported lower rates of child protection notifications in their studies included in this review, which was reported as a positive finding. However, one could also expect that ACE screening may lead to increased reporting to child protection. This could impact on the veracity of the screening tests because parents are less likely to report adversity if they feel that child protection may be notified.60
None of the studies identified in this systematic review reported on child or parent mental health outcomes. Early exposure to ACEs is associated with poor emotional regulation and aggression in the first 3 years of life,61 yet none of the studies assessed socioemotional health of the children enrolled. Dubowitz et al40,41 assessed harsh parenting in both studies included in this review and reported an improvement in the Conflict Tactics Scale, Parent-Child (CTSPC), in the intervention group compared with the control group. This is an interesting finding because there are a number of parenting factors that are associated with poor child mental health, namely, abusive parenting, aversiveness, and interparental conflict.62 In the studies by Dubowitz et al,40,41 the improvement in parent-child relationship may be a proxy for an improvement in parental mental health.
An important consideration when screening for a disease or condition is to assess the harm of the screening test. All screening tests do harm; however, it is important to balance whether the harm is offset by the effectiveness of the screening.63 Other research has indicated that there may be harms associated with just asking about ACEs. Although not explicitly an aim of this review, none of the included studies reported any assessment of harm. This contrasts with the consistent trend that ∼3% to 5% of parents report that ACEs screening is uncomfortable or harmful.9,20,23,64 This reported harm from screening is not negligible and may outweigh the potential benefits from ACEs screening. The focus on adversities may lead to stigmatization of the family and families may be less willing to engage.13 This is particularly relevant for families who are from an ethnic minority group who tend to have a high burden of ACEs.65 Labeling a child as high risk for a mental health disorder may lead to negative psychological effects and confirmation bias.24
This is the first review, to our knowledge, that has examined the impacts of ACEs screening on identification, referrals made, uptake of referrals, and child and parent mental health. We conducted a rigorous systematic search across 4 databases and hand searched the references of included articles. We followed a rigorous process to select studies (with a high interrater agreement), and 2 authors independently assessed for bias. There are some limitations of this review. As with all systematic reviews, there is a potential publication bias with only studies with positive results being published. In this review, we intentionally limited studies to randomized controlled trials (RCTs) or controlled trials in which researchers assessed the effect of screening for ACEs. This was to limit bias so that the outcome of screening for ACEs could more accurately be assessed. However, this limited the number of studies that were identified because there are few controlled trials published. All included studies were conducted in the United States, which limits the generalizability of these results to other health systems and populations. We included only English-language articles; however, given we found no ACEs screening trials implemented outside of the United States, we believe that there is unlikely to be similar trials conducted and published in languages other than English.
This systematic review has implications for health policy and health service delivery. A number of jurisdictions across the United Kingdom, United States, and Australia are implementing population-based ACEs screening, whether through universal platforms (eg, well-child care) or more targeted platforms (eg, pediatricians).9–13 From this systematic review, there is evidence that screening can improve detection of adversity and may improve referrals to community services, but there are no data on whether ACE screening improves child or parent mental health outcomes. All of the studies in this review were conducted within the health sector and undertaken during routine well-child assessments. This has implications for other health services that do not have funded yearly well-child assessments outside of infancy. This also has implications about generalizability of the results to population screening. None of the available evidence has demonstrated the efficacy, safety, and cost effectiveness of screening for ACEs at a population level. Furthermore, there is no current evidence about how ACE screening could be integrated into the current health system. This is a case in which health policy has outpaced evidence and caution needs to be employed. Further robust research, comprising rigorous, adequately powered RCTs is needed to determine if screening for ACEs can lead to improved outcomes, or unintentional harms, before widespread screening is advisable.
Conclusions
There is limited evidence, all arising from the United States, that screening for ACEs improves identification of childhood adversity and referrals to community services but no evidence for improvements in mental health outcomes for children or parents. Further RCTs are needed, in settings outside the United States, that measure both harms and benefits of screening. The relative merits of screening for ACEs, with and without screening for SDOH, should also be established through robust trials. More research is needed to examine the impact of screening for ACEs on parent-child relationships and mental health. Finally, understanding the barriers to referrals and how best to support families to take up referrals to community services once ACEs are identified is paramount if we are to realize the hypothesized benefits of ACEs screening on child and parent mental health.
Supplementary Material
Glossary
- ACE
adverse childhood experience
- CI
confidence interval
- CTSPC
Conflict Tactics Scale, Parent-Child
- IPV
intimate partner violence
- OR
odds ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PSQ
parent screening questionnaire
- RCT
randomized controlled trial
- SDOH
social determinants of health
Footnotes
Dr Loveday conceptualized and designed the study, collected data, conducted the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Hall, Ms Constable, and Ms Paton collected data, conducted the initial analyses, and reviewed and revised the manuscript; Drs Hiscock, Sanci, and Goldfeld conceptualized and designed the study, reviewed and revised the manuscript, and critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This trial has been registered at International Prospective Register of Systematic Reviews (identifier CRD42020196442).
FUNDING: No external funding.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2021-054624.
References
- 1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258 [DOI] [PubMed] [Google Scholar]
- 2. Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8): e356–e366 [DOI] [PubMed] [Google Scholar]
- 3. Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e232 [DOI] [PubMed] [Google Scholar]
- 4. Schilling EA, Aseltine RH Jr, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Flaherty EG, Thompson R, Litrownik AJ, et al. Effect of early childhood adversity on child health. Arch Pediatr Adolesc Med. 2006;160(12):1232–1238 [DOI] [PubMed] [Google Scholar]
- 6. Oh DL, Jerman P, Silvério Marques S, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatr. 2013;167(1):70–75 [DOI] [PubMed] [Google Scholar]
- 8. Karatekin C, Hill M. Expanding the original definition of adverse childhood experiences (ACEs). J Child Adolesc Trauma. 2018;12(3):289–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hardcastle K, Bellis MA. Asking about adverse childhood experiences (ACEs) in general practice: evaluation findings from a pilot study in Anglesey, North Wales. 2019. Available at: https://www.wales.nhs.uk/sitesplus/documents/888/Asking about ACEs in General Practice.pdf. Accessed October 20, 2020
- 10. Marsicek SM, Morrison JM, Manikonda N, O’Halleran M, Spoehr-Labutta Z, Brinn M. Implementing standardized screening for adverse childhood experiences in a pediatric resident continuity clinic. Pediatr Qual Saf. 2019;4(2):e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hetherington K. Ending Childhood Adversity: A Public Health Approach. Edinburgh, Scotland: Public Health Scotland; 2020 [Google Scholar]
- 12. Amor S, Campbell S, Collard B, et al. Adverse Childhood Experiences, Resilience and Trauma Informed Care: A Public Health Approach to Understanding and Responding to Adversity. Inverness, Scotland: NHS Highland; 2018 [Google Scholar]
- 13. Asmussen K, Fischer F, Drayton E, McBride T. Adverse Childhood Experiences: What We Know, What We Don’t Know, and What Should Happen Next. Westminster, London; Early Intervention Foundation; 2020 [Google Scholar]
- 14. Center for Disease Control and Prevention . Preventing Adverse Childhood Experiences (ACEs): Leveraging the Best Available Evidence. Atlanta, GA: Centers for Disease Control and Prevention; 2019 [Google Scholar]
- 15. Underwood E. California has begun screening for early childhood trauma, but critics urge caution. 2020. Science. Available at: https://www.science.org/content/article/california-has-begun- screening-early-childhood-trauma- critics-urge-caution. Accessed April 15, 2021
- 16. Quigg Z, Butler N, Wallis S. Routine Enquiry About Adverse Childhood Experiences: Implementation Pack Pilot Evaluation (Final Report). Liverpool, England: Public Health Institute of Liverpool John Moores University; 2018 [Google Scholar]
- 17. Szilagyi M, Kerker BD, Storfer-Isser A, et al. Factors associated with whether pediatricians inquire about parents’ adverse childhood experiences. Acad Pediatr. 2016;16(7):668–675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Appendix S4: the case for routine mental health screening. Pediatrics. 2010;125(Supplement 3). Available at: www.pediatrics.org/cgi/content/full/125/Supplement_3/S133 [Google Scholar]
- 19. Finkelhor D. Screening for adverse childhood experiences (ACEs): cautions and suggestions. Child Abuse Negl. 2018;85:174–179 [DOI] [PubMed] [Google Scholar]
- 20. Mersky JP, Lee CP, Gilbert RM. Client and provider discomfort with an adverse childhood experiences survey. Am J Prev Med. 2019;57(2):e51–e58 [DOI] [PubMed] [Google Scholar]
- 21. Koita K, Long D, Hessler D, et al. Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: a pilot study. PLoS One. 2018;13(12):e0208088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conn AM, Szilagyi MA, Jee SH, Manly JT, Briggs R, Szilagyi PG. Parental perspectives of screening for adverse childhood experiences in pediatric primary care. Fam Syst Health. 2018;36(1):62–72 [DOI] [PubMed] [Google Scholar]
- 23. Bodendorfer V, Koball AM, Rasmussen C, Klevan J, Ramirez L, Olson-Dorff D. Implementation of the adverse childhood experiences conversation in primary care. Fam Pract. 2020;37(3):355–359 [DOI] [PubMed] [Google Scholar]
- 24. Campbell TL. Screening for adverse childhood experiences (ACEs) in primary care: a cautionary note. JAMA. 2020;323(23):2379–2380 [DOI] [PubMed] [Google Scholar]
- 25. Jacob G, van den Heuvel M, Jama N, Moore AM, Ford-Jones L, Wong PD. Adverse childhood experiences: basics for the paediatrician. Paediatr Child Health. 2019;24(1):30–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Flynn AB, Fothergill KE, Wilcox HC, et al. Primary care interventions to prevent or treat traumatic stress in childhood: a systematic review. Acad Pediatr. 2015;15(5):480–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wilson J, Jungner G. [Principles and practice of screening for disease]. Bol Oficina Sanit Panam. 1968;(4):281–393 [PubMed] [Google Scholar]
- 28. Dobrow MJ, Hagens V, Chafe R, Sullivan T, Rabeneck L. Consolidated principles for screening based on a systematic review and consensus process. CMAJ. 2018;190(14):E422–E429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Anda RF, Porter LE, Brown DW. Inside the adverse childhood experience score: strengths, limitations, and misapplications. Am J Prev Med. 2020;59(2):293–295 [DOI] [PubMed] [Google Scholar]
- 30. van der Zee-van den Berg AI, Boere- Boonekamp MM, IJzerman MJ, Haasnoot-Smallegange RME, Reijneveld SA. Screening for postpartum depression in well-baby care settings: a systematic review. Matern Child Health J. 2017;21(1):9–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(4):388–406 [DOI] [PubMed] [Google Scholar]
- 32. Marie-Mitchell A, Kostolansky R. A systematic review of trials to improve child outcomes associated with adverse childhood experiences. Am J Prev Med. 2019;56(5):756–764 [DOI] [PubMed] [Google Scholar]
- 33. Traub F, Boynton-Jarrett R. Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics. 2017;139(5):e20162569. [DOI] [PubMed] [Google Scholar]
- 34. Ford K, Hughes K, Hardcastle K, et al. The evidence base for routine enquiry into adverse childhood experiences: a scoping review. Child Abuse Negl. 2019;91:131–146 [DOI] [PubMed] [Google Scholar]
- 35. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Veritas Health Innovation . Covidence systematic review software. Available at: https://www.covidence.org/?_gl=1%2A3mo8bn%2A_ga%2AMTQ4MjA1NjI1NS4xNjMxMTY5OTAy%2A_ga_HXKEQPTFLR%2AMTYzOTcwMTUxNS45Ny 4xLjE2Mzk3MDE1NDUuMzA. Accessed April 14, 2020
- 37. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 39. Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–e304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dubowitz H, Lane WG, Semiatin JN, Magder LS. The SEEK model of pediatric primary care: can child maltreatment be prevented in a low-risk population? Acad Pediatr. 2012;12(4):259–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dubowitz H, Feigelman S, Lane W, Kim J. Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) model. Pediatrics. 2009;123(3):858–864 [DOI] [PubMed] [Google Scholar]
- 42. Dauber S, Hogue A, Henderson CE, Nugent J, Hernandez G. Addressing maternal depression, substance use, and intimate partner violence in home visiting: a quasi-experimental pilot test of a screen-and-refer approach. Prev Sci. 2019;20(8):1233–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547–558 [DOI] [PubMed] [Google Scholar]
- 44. Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53(5):719–729 [DOI] [PubMed] [Google Scholar]
- 45. Fiori KP, Rehm CD, Sanderson D, et al. Integrating social needs screening and community health workers in primary care: the community linkage to care program. Clin Pediatr (Phila). 2020;59(6):547–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Colvin JD, Bettenhausen JL, Anderson-Carpenter KD, et al. Multiple behavior change intervention to improve detection of unmet social needs and resulting resource referrals. Acad Pediatr. 2016;16(2):168–174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Selvaraj K, Ruiz MJ, Aschkenasy J, et al. Screening for toxic stress risk factors at well-child visits: the addressing social key questions for health study. J Pediatr. 2019;205:244–249.e4 [DOI] [PubMed] [Google Scholar]
- 48. Baldwin JR, Caspi A, Meehan AJ, et al. Population vs individual prediction of poor health from results of adverse childhood experiences screening. JAMA Pediatr. 2021;175(4):385–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521. [DOI] [PubMed] [Google Scholar]
- 50. Valado T, Tracey J, Goldfinger J, Briggs R. HealthySteps: transforming the promise of pediatric care. Future Child. 2019;29(1):99–122 [Google Scholar]
- 51. Garg A, Cull W, Olson L, et al. Screening and referral for low-income families’ social determinants of health by US pediatricians. Acad Pediatr. 2019;19(8):875–883 [DOI] [PubMed] [Google Scholar]
- 52. Eismann EA, Theuerling J, Maguire S, Hente EA, Shapiro RA. Integration of the Safe Environment for Every Kid (SEEK) model across primary care settings. Clin Pediatr (Phila). 2019;58(2):166–176 [DOI] [PubMed] [Google Scholar]
- 53. Kia-Keating M, Barnett ML, Liu SR, Sims GM, Ruth AB. Trauma-responsive care in a pediatric setting: feasibility and acceptability of screening for adverse childhood experiences. Am J Community Psychol. 2019;64(3-4):286–297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Forkey H, Conn AM. Childhood trauma management in primary care. Adv Pediatr. 2018;65(1):143–158 [DOI] [PubMed] [Google Scholar]
- 55. Keating D, Syrmis M, Hamilton L, McMahon S. Paediatricians: referral rates and speech pathology waiting lists. J Paediatr Child Health. 1998;34(5):451–455 [DOI] [PubMed] [Google Scholar]
- 56. Fritz CQ, Thomas J, Brittan MS, Mazzio E, Pitkin J, Suh C. Referral and resource utilization among food insecure families identified in a pediatric medical setting. Acad Pediatr. 2021;21(3):446–454 [DOI] [PubMed] [Google Scholar]
- 57. Tandon SD, Parillo KM, Jenkins C, Duggan AK. Formative evaluation of home visitors’ role in addressing poor mental health, domestic violence, and substance abuse among low-income pregnant and parenting women. Matern Child Health J. 2005;9(3):273–283 [DOI] [PubMed] [Google Scholar]
- 58. Zielinski S, Paradis HA, Herendeen P, Barbel P. The identification of psychosocial risk factors associated with child neglect using the WE-CARE screening tool in a high-risk population. J Pediatr Health Care. 2017;31(4):470–475 [DOI] [PubMed] [Google Scholar]
- 59. Marie-Mitchell A, Studer KR, O’Connor TG. How knowledge of adverse childhood experiences can help pediatricians prevent mental health problems. Fam Syst Health. 2016;34(2):128–135 [DOI] [PubMed] [Google Scholar]
- 60. McTavish JR, Kimber M, Devries K, et al. Children’s and caregivers’ perspectives about mandatory reporting of child maltreatment: a meta-synthesis of qualitative studies. BMJ Open. 2019;9(4):e025741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. McKelvey LM, Selig JP, Whiteside-Mansell L. Foundations for screening adverse childhood experiences: Exploring patterns of exposure through infancy and toddlerhood. Child Abuse Negl. 2017;70:112–121 [DOI] [PubMed] [Google Scholar]
- 62. Yap MBH, Jorm AF. Parental factors associated with childhood anxiety, depression, and internalizing problems: a systematic review and meta-analysis. J Affect Disord. 2015;175:424–440 [DOI] [PubMed] [Google Scholar]
- 63. Gray JA, Patnick J, Blanks RG. Maximising benefit and minimising harm of screening. BMJ. 2008;336(7642):480–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Flanagan T, Alabaster A, McCaw B, Stoller N, Watson C, Young-Wolff KC. Feasibility and acceptability of screening for adverse childhood experiences in prenatal care. J Womens Health (Larchmt). 2018;27(7):903–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Sawrikar P. Child protection, domestic violence, and ethnic minorities: narrative results from a mixed methods study in Australia. PLoS One. 2019;14(12): e0226031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.