Abstract
Antimicrobial resistance against shigellosis is increasingly alarming. However, evidence-based knowledge gaps regarding the changing trends of shigellosis in Bangladesh exist due to the scarcity of longitudinal data on antimicrobial resistance. Our study evaluated the last 20 years antimicrobial resistance patterns against shigellosis among under-5 children in the urban and rural sites of Bangladesh. Data were extracted from the Diarrheal Disease Surveillance System (DDSS) of Dhaka Hospital (urban site) and Matlab Hospital (rural site) of the International Centre for Diarrheal Disease Research, Bangladesh (icddr,b) between January 2001 and December 2020. We studied culture-confirmed shigellosis cases from urban Dhaka Hospital (n = 883) and rural Matlab Hospital (n = 1263). Since 2001, a declining percentage of shigellosis in children observed in urban and rural sites. Moreover, higher isolation rates of Shigella were found in the rural site [1263/15684 (8.1%)] compared to the urban site [883/26804 (3.3%)] in the last 20 years. In both areas, S. flexneri was the predominant species. The upward trend of S. sonnei in both the study sites was statistically significant after adjusting for age and sex. WHO-recommended 1st line antibiotic ciprofloxacin resistance gradually reached more than 70% in both the urban and rural site by 2020. In multiple logistic regression after adjusting for age and sex, ciprofloxacin, azithromycin, mecillinam, ceftriaxone, and multidrug resistance (resistance to any two of these four drugs) among under-5 children were found to be increasing significantly (p<0.01) in the last 20 years in both sites. The study results underscore the importance of therapeutic interventions for shigellosis by appropriate drugs based on their current antibiogram for under-5 children. These observations may help policymakers in formulating better case management strategies for shigellosis.
Introduction
Shigella is the most common cause of invasive diarrhea. It remains accountable for increased morbidity and mortality rates in under-5 children in low- and middle-income countries [1]. The choice of an appropriate antibiotic for the treatment of shigellosis depends on the routine detection and monitoring of resistance patterns [2]. Clinical management, mostly of antimicrobial-resistant cases of shigellosis, is difficult without prior knowledge of the drug susceptibility patterns. Lack of such knowledge and inappropriate use of antimicrobials may lead to the onset of complications, requiring a prolonged hospital stay, and may ultimately result in fatal outcomes [3]. Globally, challenges for clinical management of shigellosis are emerging fast, more commonly in developing countries [4]. Multiple factors are involved in the emergence of antibiotic resistance, most often due to injudicious use of antibiotics resulting in resistant strains [5]. Drug resistance to Shigella infection develops by extrusion of drugs by active efflux pumps, decrease in cellular permeability, and over expression of drug-modifying and inactivating enzymes or target modification by mutation [6–8]. In addition to selective pressure and horizontal resistance-gene transmission, these different natures of antibiotic-resistance mechanisms contribute to an increase in the number of multidrug-resistant strains and cause conventional antibiotics to be highly incompetent against shigellosis within the shortest period [9]. Globally, it has been hypothesized that if necessary measure are not adopted to reduce the intensity of the rapidly expanding antimicrobial resistance, one person will die every three seconds by 2050 [10].
According to the WHO pocketbook, 1st line of antibiotics for shigellosis in children is ciprofloxacin and 2nd line of drugs is mecillinam /ceftriaxone [11, 12]. In this guideline, azithromycin was considered as 2nd line drug for adults only. International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) is monitoring the susceptibility pattern of Shigella isolates routinely as reported by the ongoing diarrheal disease surveillance system (DDSS) since its inception in treating shigellosis cases, seeking care from both urban (1979) and rural (1999) facilities. Alarming rates of resistance to ciprofloxacin were previously reported among the detected Shigella isolates [13], so azithromycin has currently been listed as a first [14] or second-line therapy [15] in some international guidelines for treating shigellosis in children. Consequently, cefixime has demonstrated effectiveness in treating shigellosis in both adult and pediatric patients [16, 17]. These different antibiotics are prescribed for the treatment of shigellosis, and enteric fever in children and it is an upsetting public health concern that resistance against this antimicrobial is also increasing over the period. Henceforth, we aimed to observe the changing pattern of resistance in the case of WHO-recommended 1st and 2nd line antibiotics used for shigellosis in children in Bangladesh.
Materials and methods
Ethical statement
For this study, data were extracted from the electronic database of hospital-based DDSS of both urban Dhaka Hospital and rural Matlab Hospital of icddr,b. DDSS is routine ongoing surveillance in hospitals of icddr,b located in Dhaka and Matlab, Bangladesh. The DDSS has the approval from the institutional review board of icddr,b (Research Review Committee and Ethical Review Committee) for data collection, analysis, and dissemination of the findings. At the time of enrolment into DDSS, verbal consent was obtained from the parents or the attending caregivers of each child, following hospital policy. Verbal consent was assured by showing the mark in the questionnaire to parents or caregivers. At the time of consenting, parents or caregivers were assured of ‘any risk being no more than minimal’, ‘their participation is voluntary’, ‘their rights to discontinue participation from the study’, and ‘the maintenance of strict confidentiality of disclosed information’. They were also informed about the use of anonymous data for analysis and using the results for improving patient management, conducting researches, and also for publication in leading peer-reviewed journals without disclosing the name or identity of their children.
Study population and study site
Dhaka hospital and Matlab hospital of icddr,b provides care and free treatment to around 200,000 diarrheal disease patients each year and about 62% of them are children less than five years of age. In Dhaka hospital, the DDSS systematically (from every 50th patient according to their hospital ID number) collected information, including age, sex, socio-demographic characteristics, clinical features, and common bacterial and viral etiology of diarrhea. For the Matlab hospital, patients from the Matlab HDSS (Health and Demographic Surveillance System) area were included in the study and stool samples were collected from each patient from this area attending in Matlab hospital. Parents or caregivers were interviewed by research assistants who collect demographic, socioeconomic, and clinical data. A physician documented the clinical findings including dehydration status. The stool sample was collected and submitted to the laboratory for microbiological evaluation. All relevant information was recorded into the electronic database as soon as possible. The present study’s analysis was limited to under-five children who were Shigella positive and enrolled in the DDSS from January 2001 to December 2020.
Laboratory methods
A single, fresh stool specimen was collected from all enrolled patients and submitted immediately to the clinical microbiology laboratory in Dhaka/ Matlab. All stool samples were routinely screened for common enteric pathogens, including Enterotoxigenic Escherichia coli, V. cholerae, Salmonella Shigella spp., and rotavirus following standard laboratory procedures [18]. For Shigella identification, stools were inoculated onto MacConkey (MAC) and Salmonella–Shigella (SS) agar media plates. Shigella spp. were isolated and identified using standard laboratory methods [19] and grouped serologically by slide agglutination with specific antisera (Denka Seiken, Tokyo, Japan). Antimicrobial susceptibility of the isolated strains wasdetermined by the disc diffusion method as recommended by the Clinical Laboratory and Standard Institute, CLSI [formerly the National Committee for Clinical Laboratory Standards (NCCLS)] and already described in detail elsewhere [20]. The antibiotic discs used in this study (Oxoid, UK) included ciprofloxacin (5mg), mecillinam (25mg), Ceftriaxone (30mg). Before 2019 there was no information for Azithromycin in the CLSI guideline. For Zone size interpretive standards for disks, we used the WHO manual for the ‘Laboratory identification and Antimicrobial susceptibility testing of Bacterial Pathogens of Public health importance in the developing World’. For interpretation of test with 15 μg azithromycin disk, susceptibility zone ≥19 mm and resistance ≤15mm were considered (intermediate not noted). E. coli ATCC 25922 was used as the control for susceptibility studies [21].
Definition
Multidrug resistance was defined by any of the two drugs out of ciprofloxacin, azithromycin, mecillinam, and ceftriaxone that were resistant to Shigella isolates.
Data analysis
Data were analyzed using STATA version 15.0 IC (College Station, Texas). Statistical analyses included descriptive methods, including percentages of detection, species distribution, and resistance to ciprofloxacin, azithromycin, mecillinam, and ceftriaxone (WHO recommended 1st and 2nd line drug). Percentage of each species at each year were calculated from total number of Shigella positive isolates to assess the trend of each species with the 20 years period. For the strength of association (odds ratio) between Shigella positive isolates and change of the time (in year), multiple logistic regression was performed where each of the species was outcome variables and the time period in years was treated as exposure variable after adjusting for the age and sex.
The percentage of each species was documented in graphs separately for rural and urban sites. In the graphical presentation, 5 years prevalence of antimicrobial resistance to each drug was placed against every 5 years period for all Shigella species, S. flexneri, and S. sonnei. We did not include antimicrobial resistance of S. boydii and S. dysenteriae, as their percentage were low in both the sites. To assess the strength of association of resistance of antibiotics with time in years, adjusted odd-ratios (aORs) were calculated using multiple logistic regression where outcomes were ciprofloxacin resistance, azithromycin resistance, mecillinam resistance, ceftriaxone resistance, multidrug resistance (resistance to any of the two drugs) and independent variable was year, adjusted for age in months and sex of children.
Results
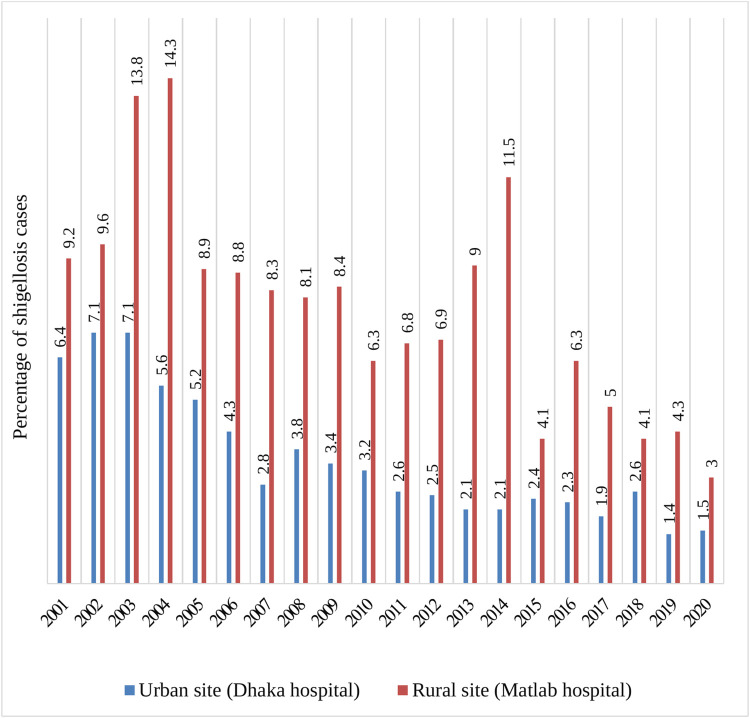
From 2001 to 2020, 26,804 and 15,684 under-5 children were included in Dhaka hospital and Matlab hospital surveillance systems, respectively. Of these, 883 and 1263 Shigella positive cases were enrolled in the urban and rural sites, respectively. Fig 1 shows the percentage of Shigella isolates in the last 20 years among under five children. Isolation rates of Shigella in the previous 20 years was 8.1% in the rural site and 3.3% in the urban site.
Fig 1. Percentage of shigellosis among under 5 children in last 20 years (2001–2020).
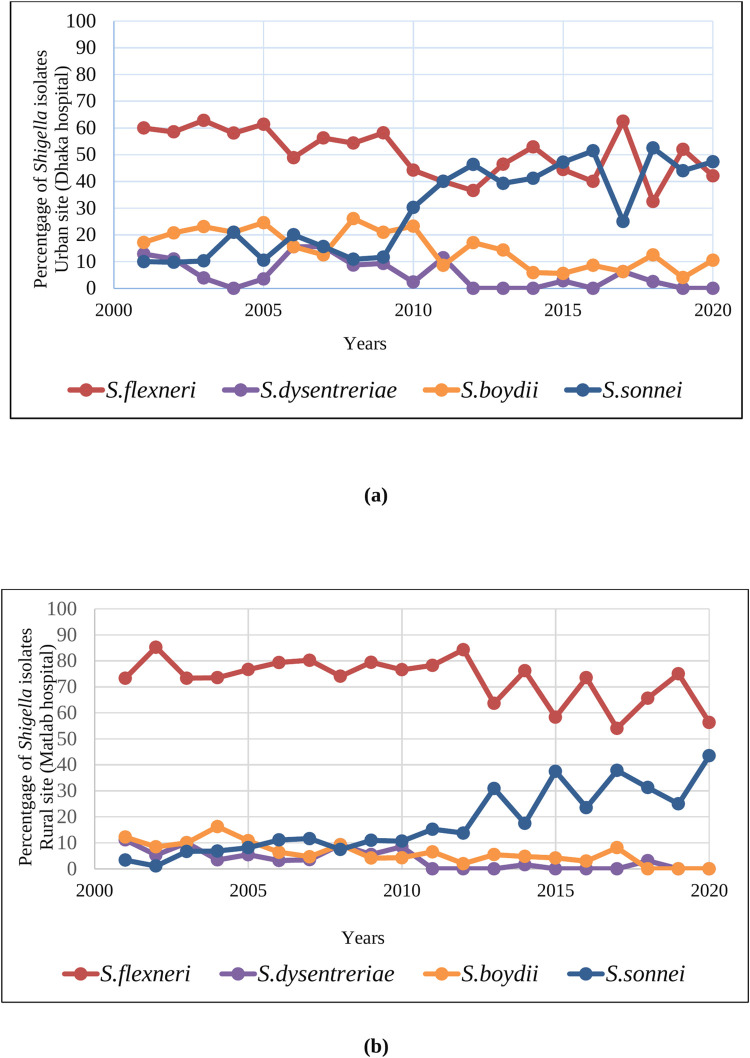
Fig 2(A) and 2(B) show the percentage of all species reported in the urban and rural sites in the last 20 years. In urban site S. flexneri was the predominant species in the early study period (up to 2010), whereas in the later periods (after 2010), detection of S. sonnei gradually increased. In rural site, S. flexneri was the predominant species during the entire study period, whereas in the later period, a gradual upward trend in the detection of S. sonnei was noted. But throughout the 20 years, there was a gradual decrease in the detection trend of S. boydii and S. dysenteriae.
Fig 2. Percentage of different Shigella species in under 5 children in the urban site and rural site in last 20 years.
In Table 1, multiple logistic regression shows a significant increase in the trend of detection of S. sonnei (aOR 1.13, 95% CI: 1.10–1.16; P <0.01) over 20 years period. Other Shigella species also show downward trend of isolation over the 20 years period after for adjusting age and sex.
Table 1. Trend of different Shigella species over the last 20 years in urban and rural sites.
| Urban site (Dhaka hospital) | Rural site (Matlab hospital) | |||||
|---|---|---|---|---|---|---|
| Total isolates (n = 883) (%) | aOR (95% CI) | p-value | Total isolates (n = 1263) (%) | aOR (95% CI) | p-value | |
| S. flexneri | 463 (52.43) | 0.96 (0.93–0.98) | <0.01 | 945 (74.82) | 0.97 (0.94–0.99) | <0.01 |
| S. dysentreriae | 52 (5.89) | 0.91 (0.86–0.96) | <0.01 | 60 (4.75) | 0.87 (0.81–0.92) | <0.01 |
| S. boydii | 147 (16.65) | 0.94 (0.91–0.97) | <0.01 | 96 (7.60) | 0.91 (0.87–0.96) | <0.01 |
| S. sonnei | 221 (25.03) | 1.13 (1.10–1.16) | <0.01 | 162 (12.83) | 1.16 (1.12–1.20) | <0.01 |
aOR: adjusted odds ratio, adjusted for age and sex
Table 2 shows the percentage of isolates tested for all the recommended antibiotics for shigellosis in under-5 children. Throughout the 20 years, it was not possible to test all the antibiotics for all the Shigella isolates due to the availability of different antibiotic discs. It has been documented that 96.04% and 92.98% of samples were tested for ciprofloxacin and mecillinam respectively in the urban site. However, a lower number of samples were tested for azithromycin (38.96%) and ceftriaxone (40.32%). Similarly, from rural site, 95.01% and 94.14% samples were tested for ciprofloxacin and mecillinam, whereas around 20% samples were tested for azithromycin and ceftriaxone.
Table 2. Percentage of isolates tested for recommended antibiotics for shigellosis.
| Urban site (Dhaka Hospital) | Rural site (Matlab Hospital) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total Shigella positive sample | Total Shigella positive sample | |||||||||
| n (%) | n (%) | |||||||||
| Percentage of samples tested for antibiotics (N = 883) | Percentage of samples tested for antibiotics (N = 1263) | |||||||||
| Total Shigella | S. flexneri | S. dysentreriae | S. boydii | S. sonnei | Total Shigella | S. flexneri | S. dysentreriae | S. boydii | S. sonnei | |
| Ciprofloxacin | 848 (96.04) | 452 (53.3) | 52 (2.62) | 146 (17.22) | 198 (23.35) | 1200 (95.01) | 911 (75.92) | 58 (4.83) | 93 (7.75) | 138 (11.50) |
| Mecillinam | 821 (92.98) | 433 (52.74) | 47 (5.72) | 132 (16.08) | 209 (25.46) | 1189 (94.14) | 893 (75.11) | 57 (4.79) | 92 (7.74) | 147 (12.36) |
| Azithromycin | 344 (38.96) | 155 (45.06) | 9 (2.62) | 38 (11.05) | 142 (41.28) | 259 (20.51) | 174 (67.18) | 1 (0.39) | 8 (3.14) | 76 (29.34) |
| Ceftriaxone | 356 (40.32) | 165 (46.35) | 9 (2.53) | 38 (10.67) | 144 (40.45) | 255 (20.19) | 169 (66.27) | 2 (0.78) | 8 (7.74) | 76 (29.80) |
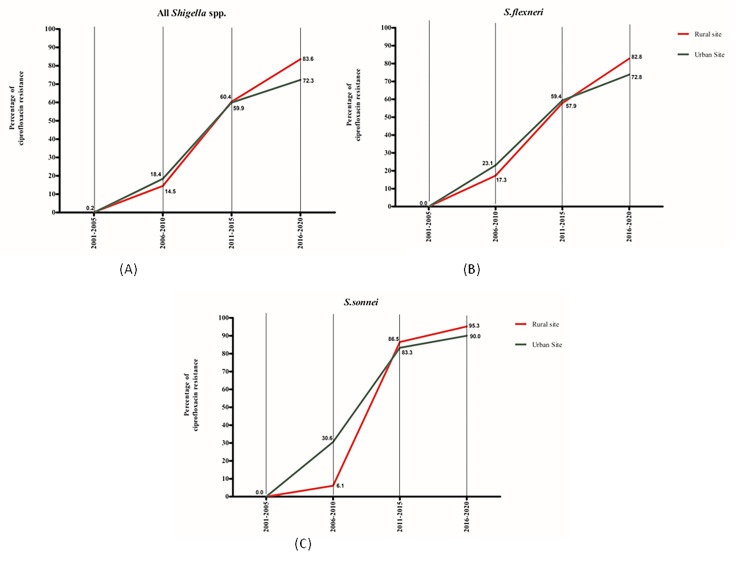
The percentage of 1st line antibiotic ciprofloxacin resistance for shigellosis in under-5 children. It was observed that, although ciprofloxacin resistance started in the early decades, the resistance gradually increased to more than 70% in both the rural and urban site by 2020 (Fig 3).
Fig 3. Percentage of ciprofloxacin resistance in shigellosis, 2001–2020.
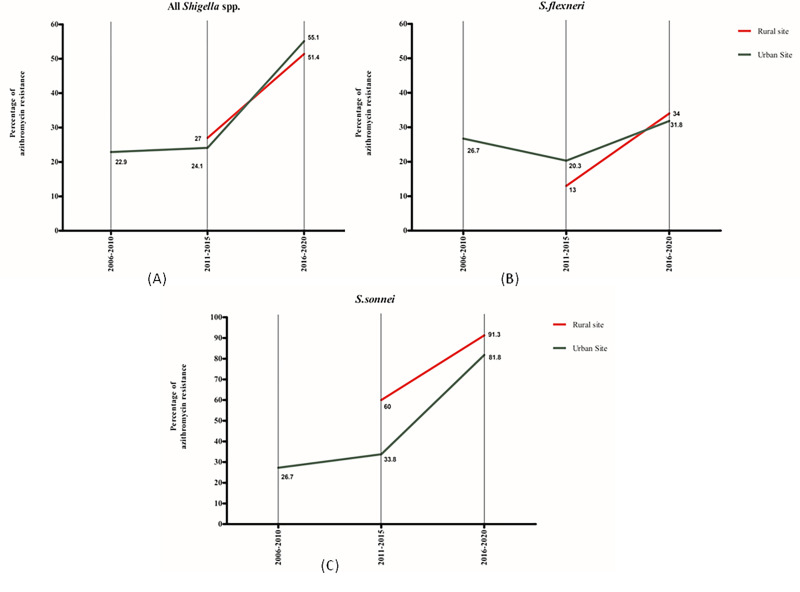
The percentage of resistance of azithromycin (2nd line antibiotics) in under-5 children increased to more than 50%, both in the urban and rural sites. A comparatively higher percentage of resistance for azithromycin was observed in the case of S. sonnei compared to that of S. flexneri (Fig 4).
Fig 4. Percentage of azithromycin resistance in shigellosis, 2001–2020.
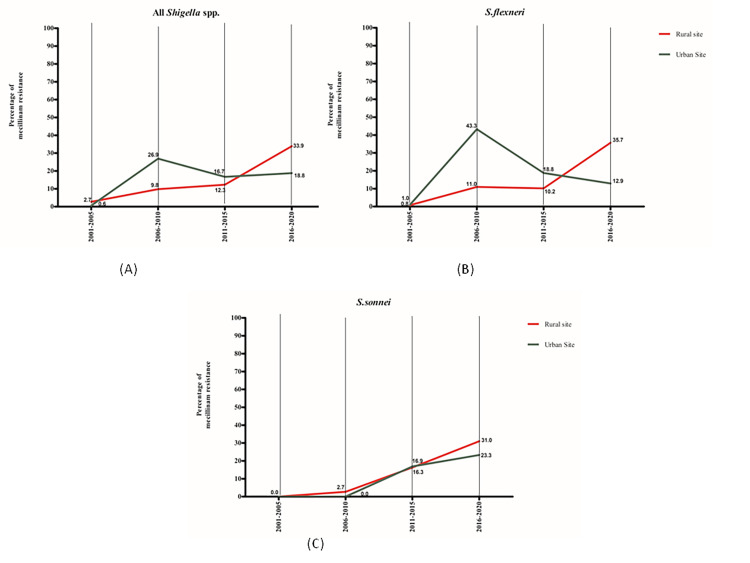
A diverse resistance pattern over the last 20 years was observed for mecillinam in the two study sites. Compared to the urban site, the rural site had a higher resistance in 2016–2020 (33.9% vs 18. 28%) against all Shigella isolates (Fig 5).
Fig 5. Percentage of mecillinam resistance in shigellosis, 2001–2020.
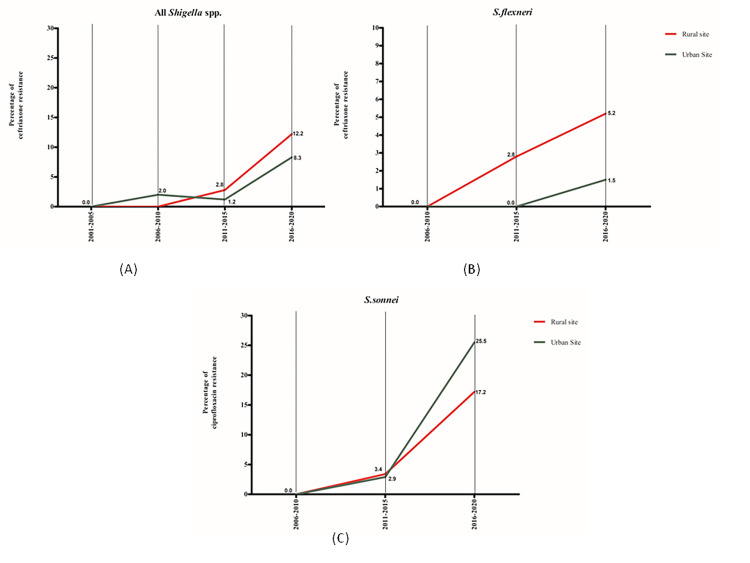
The ceftriaxone resistance started in the last decade (2011–2020) and gradually increased to more than 10% in the rural area, whereas in an urban area, it was 7.6% by 2020. Although only a few samples were tested for ceftriaxone, a comparatively higher percentage of resistance was observed for S. sonnei (Fig 6).
Fig 6. Percentage of ceftriaxone resistance in shigellosis, 2001–2020.
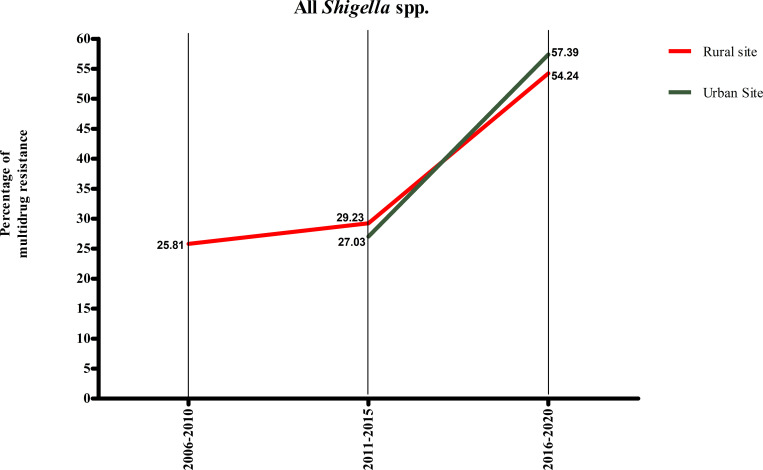
After the early decade (2001–2010), a persistent rise in multidrug resistance in the case of shigellosis was observed in both the study sites (Fig 7). In the supplementary table (S1 Table), we have included the percentage of three and four drug resistance in urban and rural settings.
Fig 7. Percentage of multidrug resistance in shigellosis, 2001–2020.
Tables 3 and 4 show the strength of association of antibiotic resistance in shigellosis among under-5 children in both urban and rural sites with the changes of time. After adjusting for age and sex, ciprofloxacin, azithromycin, mecillinam, ceftriaxone, and multidrug resistance increased significantly over time.
Table 3. Percentage of antibiotic resistance and association with year among under 5 children with shigellosis from 2001–2020 in urban site (Dhaka hospital).
| Year | Ciprofloxacin resistance (%) | Azithromycin resistance (%) | Mecillinam resistance (%) | Ceftriaxone resistance (%) | Multidrug resistance (%) |
|---|---|---|---|---|---|
| 2001 | 0.0 | Test not done | 1.49 | Test not done | |
| 2002 | 0.0 | Test not done | 0.0 | Test not done | |
| 2003 | 0.0 | Test not done | 1.35 | Test not done | |
| 2004 | 0.0 | Test not done | 0.0 | Test not done | |
| 2005 | 0.0 | Test not done | 0.0 | Test not done | |
| 2006 | 2.2 | Test not done | 0.0 | 0.0 | |
| 2007 | 6.2 | Test not done | 6.25 | Test not done | |
| 2008 | 27.7 | Test not done | 37.21 | 0.0 | |
| 2009 | 14.0 | Test not done | 48.78 | 0.0 | |
| 2010 | 47.50 | 22.86 | 37.50 | 2.63 | 25.81 |
| 2011 | 56.67 | 11.76 | 26.47 | 0.0 | 21.43 |
| 2012 | 45.45 | 25.0 | 9.76 | 0.0 | 21.88 |
| 2013 | 54.17 | 18.52 | 19.23 | 0.0 | 27.27 |
| 2014 | 64.52 | 27.59 | 13.33 | 3.33 | 43.48 |
| 2015 | 76.47 | 37.50 | 16.13 | 3.03 | 36.0 |
| 2016 | 80.0 | 57.14 | 14.71 | 3.13 | 61.29 |
| 2017 | 74.19 | 43.33 | 0.0 | 0.0 | 36.0 |
| 2018 | 65.71 | 56.0 | 32.26 | 13.51 | 52.0 |
| 2019 | 71.43 | 56.0 | 33.33 | 16.0 | 65.0 |
| 2020 | 68.4 | 66.67 | 11.11 | 10.53 | 58.82 |
| aOR (95% CI) | 1.41 (1.35–1.48)* | 1.27 (1.17–1.37)* | 1.13 (1.09–1.17)* | 1.45 (1.16–1.81)* | 1.21 (1.11–1.31)* |
*p value <0.01
aORs were calculated using multiple logistic regression where outcomes were ciprofloxacin resistance, azithromycin resistance, mecillinam resistance, ceftriaxone resistance, multidrug resistance (resistance to any of the two drugs) and independent variable was year, adjusted for age in months and sex of children.
Table 4. Percentage of antibiotic resistance and association with year among under 5 children with shigellosis from 2001–2020 in rural site (Matlab hospital).
| Year | Ciprofloxacin resistance (%) | Azithromycin resistance (%) | Mecillinam resistance (%) | Ceftriaxone resistance (%) | Multidrug resistance (%) |
|---|---|---|---|---|---|
| 2001 | 0 | Test not done | 10.11 | Test not done | |
| 2002 | 0 | Test not done | 1.06 | 0/1 | |
| 2003 | 0.85 | Test not done | 0.85 | Test not done | |
| 2004 | 0 | Test not done | 0.88 | Test not done | |
| 2005 | 0.0 | Test not done | 1.39 | Test not done | |
| 2006 | 0.0 | Test not done | 6.35 | Test not done | |
| 2007 | 4.76 | Test not done | 6.98 | Test not done | |
| 2008 | 14.14 | Test not done | 9.80 | Test not done | |
| 2009 | 23.19 | Test not done | 16.42 | Test not done | |
| 2010 | 40.91 | Test not done | 6.52 | Test not done | |
| 2011 | 41.46 | 0.0 | 4.76 | 0.0 | |
| 2012 | 53.19 | Test not done | 8.89 | Test not done | |
| 2013 | 67.44 | 26.29 | 22 | 4.17 | 40.0 |
| 2014 | 68.42 | 23.33 | 11.54 | 3.39 | 20.93 |
| 2015 | 78.95 | 37.50 | 13.04 | 0.0 | 31.25 |
| 2016 | 76.47 | 55.88 | 36.36 | 2.94 | 60.61 |
| 2017 | 71.43 | 55.88 | 53.85 | 14.29 | 59.09 |
| 2018 | 92.86 | 50.0 | 44.44 | 16.1 | 73.91 |
| 2019 | 93.55 | 0.63 | 6.9 | 12.5 | 39.29 |
| 2020 | 91.67 | 56.25 | 25.0 | 18.75 | 55.56 |
| aOR (95% CI) | 1.59 | 1.21 | 1.91 | 1.40 | 1.21 |
| (1.51–1.68)* | (1.08–1.36)* | (1.15–1.24)* | (1.11–1.77)* | (1.05–1.40)* |
*p value <0.01
aORs were calculated using multiple logistic regression where outcomes were ciprofloxacin resistance, azithromycin resistance, mecillinam resistance, ceftriaxone resistance, multidrug resistance (resistance to any of the two drugs) and independent variable was year, adjusted for age in months and sex of children.
Discussion
Our observation from the DDSS on the detection of Shigella isolates among under-5 children warrants greater clinical vigilance regarding the use of appropriate therapeutic strategy, owing to the gradual antimicrobial resistance among the Shigella isolates. The most important observations involve a twofold higher detection rate of Shigella cases in rural site compared to urban site and an alarming rise of antimicrobial resistance in both sites over the last 20 years.
Different studies, including the Global Enteric Multicenter Study (GEMS) reported that in the rural study site, poor hygiene practices, not covering the water container, not use of handwashing substances, and children from low-income families are vulnerable to childhood shigellosis [22, 23]. Tube-well is the primary drinking water source for Bangladesh’s rural population [24]. A shallow tube well is likely to be contaminated with adjacent polluted water sources due to its shallowness [24]. Moreover, deep tube-well water users are susceptible to S. sonnei infection due to decreased water contamination with Plesiomonas Shigelloides, which shares similar antigenic characteristics to S. sonnei [23]. Probably these are the factors associated with a higher percentage of isolation of Shigella cases in the rural site.
In our study, S. flexneri was the predominant species in both urban and rural sites among all Shigella cases. However, S. sonnei demonstrated an increasing trend that was statistically significant. We did not detect any S. dysenteriae isolates in 2019–2020. Increasing detection of S. sonnei has also been reported in many countries, including Bangladesh [23]. It is observed from different studies that developed nations have a predominance of S. sonnei [25–27] whereas in recent years, an increased trend of S. sonnei has been observed in developing countries [28]. P. shigelloides is a gram-negative bacterium surviving in surface water that shares antigens with S. sonnei [29], and exposure to P. shigelloides, through contaminated drinking water, may immunize people to S. sonnei in developing countries despite exposure to contaminated drinking water [30]. The upward trend of S. sonnei infections can be explained by the reduced exposure of individuals from developing countries, including Bangladesh, to Plesiomonas Shigelloides (P. shigelloides) from drinking water in recent years [31]. The gross economic improvement in Bangladesh may be linked to an increase in the use of relatively safe deep tube-well water (DTW) and bottled water [32], and thereby the present study observed an enhancing trend of higher S. sonnei cases. Climate and environmental changes over time, as well as changes in innate characteristics of different serogroups and serotypes of Shigella, are additional explanation for this change [33].
Our study, covering the years 2001–2020, demonstrated the increasing antimicrobial resistance of Shigella isolates among under-5 children in both urban and rural diarrheal disease hospitals in Bangladesh. The resistance to antimicrobial agents that are commonly used to treat shigellosis in young children, namely: mecillinam, azithromycin, ciprofloxacin, ceftriaxone as well as multidrug resistance reached 33.9% vs. 18.8%, 55.1% vs. 51.4%, 83.6% vs. 72.3%, 12.2% vs. 8.3% and 47.7% vs. 43.1% in the rural and urban setups, respectively in last 5-year period. Previous studies have shown that the resistance rate observed in a hospital-based microbiology laboratory was similar to all Shigella-positive cases compared to community-based microbiology laboratories [2, 34]. This was expected almost all cases were community-acquired as the cultures were obtained on the admission samples. This suggests that the resistance rates found in the present study are typical of the scenario in the community.
Antimicrobial treatment is suggested for shigellosis to prevent further complications, shorten the duration of fever, reduce diarrheal output, and limit post-symptomatic fecal shedding, particularly in malnourished children living in low- and middle-income countries [35]. Unfortunately, resistance to antimicrobials appears to arise rather effortlessly in the case of Shigella. It may result from an unrestricted barrier for horizontal gene transfer between Shigella in urban and rural settings.
The current recommended first-line treatment for shigellosis is fluoroquinolones, such as ciprofloxacin, although, these also rapidly became the mainstay prescription for acute diarrhea in endemic regions [36]. The trend of resistance to ciprofloxacin is rising, probably due to its over-the-counter availability and common use. Asia is a reservoir for the rise and spread of resistant bacteria [37]. Specifically, ciprofloxacin-resistance among isolates of S. sonnei has risen as a single clone, especially in South Asia, before applying globally to Southeast Asia and Europe [38]. Such resistance depends on the gradual accretion of the triple mutations in chromosomal gyrA and parC. Moreover, horizontally transferred elements could help to establish emerging resistant clones [39].
A study conducted in Bangladesh reported that the rate of mecillinam resistance was significantly lower in Bangladesh [16]. We have also observed similar findings that showed comparatively lower resistance than other 2nd line antibiotics for shigellosis, although yearly resistance to mecillinam showed fluctuation. The absence of pediatric formulation for mecillinam and poor compliance to recommended multiple doses with a bitter taste may have made mecillinam less susceptible to drug overuse, mostly in children. In addition, fluctuation in this drug’s steady supply might contribute to the change of resistance pattern.
Azithromycin has been considered to be the last oral choice for the treatment of bacillary dysentery. Decreased susceptibility to azithromycin was reported in recent years worldwide. Analyzing our antibiotic resistance data, we observed that azithromycin resistance increased almost four times from 2011 to 2020. A study from public health surveillance in Australia showed resistance to azithromycin is mediated by the plasmid pKSR100, which was recently revealed to be acquired in separate S. sonnei and S. flexneri 2a isolates [40]. Probably in Bangladesh, the selective pressure from azithromycin administration due to diarrhea-related symptoms might have contributed to the emergence of resistance in this organism.
Among hospitalized children with shigellosis, parenteral ceftriaxone is effective and usually recommended. Shigella was highly susceptible to ceftriaxone (>98%), which was introduced during the early decade (2001–2010) of the study period as a result of increasing resistance to mecillinam and ciprofloxacin [41]. In our study, among all Shigella cases, resistance to ceftriaxone increased over the period in both the study sites. However, we could not draw any conclusive remark on it because of the low number of samples tested. Very recently published research on shigellosis also observed increasing resistance to ceftriaxone [42, 43].
Multidrug resistance of shigellosis is commonly reported all over the world. The Centre for Disease Control (CDC) has categorized Shigella infections as a serious threat because of the increasing trend of drug resistance [44]. Resistance to ciprofloxacin, β-lactam antibiotics, or plasmid-mediated azithromycin resistance is of high concern [45, 46]. Our study observed that over the 20 years, multidrug resistance shigellosis has been increasing in both urban and rural settings, and the rate of this increase is more significant in the urban site.
In the last five years, there was a sharp rise of mono-drug and multidrug-resistant shigellosis in the rural site. Antibiotic resistance in urban and rural Bangladesh exhibited a trend of rising and falling in a simultaneous and synchronized manner [41]. A very recent article published on using data collected from 2017–2019 reported that the perception of a rural community on the use of antibiotics and AMR and it also showed the care-seeking changes in community-level [47]. A survey report from Bangladesh demonstrated irrational use of antibiotic among rural community [48]. Probably these explains the changes of antibiotic resistance pattern of rural site in the recent five years.
Our study has a few limitations warranting a careful interpretation of the results. We were able to evaluate only a limited number of antimicrobial susceptibility patterns of shigellosis due to the lack of availability of laboratory data which were extracted from the electronic database of hospital-based DDSS of Dhaka hospital and Matlab hospital. Moreover, the study was conducted in a diarrheal disease hospital setting in Bangladesh, so the results may not be generalizable for the more extensive and diverse population. Moreover, the issue of sub-clinical infections by Shigella, as reported in studies conducted in similar settings [49], was not considered for this study. To revise treatment guideline, antimicrobial susceptibility needs to be evaluated from community level.
In conclusion, our study findings identified changing pattern of Shigella species, and emerging resistance in Shigella isolates to WHO recommended 1st and 2nd line antimicrobial agents in the last 20 years in Bangladesh. Multidrug-resistant shigellosis is also gradually increasing both in urban and rural settings. physicians should be aware of the high rates of antimicrobial resistance to Shigella spp. in Bangladesh. Undoubtedly, the treatment of shigellosis among under-5 children demands careful and judicial use of antimicrobials to avoid rapid emergence and spread of resistance. At the same time, our study results underscore the need for continued monitoring and evidence-based alternative antibiotic regimens for multidrug-resistant Shigella infections.
Supporting information
(DOCX)
Acknowledgments
This research was funded by core donors who provide unrestricted support to icddr,b for its operations and research. Current donors providing unrestricted support include the Governments of Bangladesh, Canada, Sweden and the UK. We gratefully acknowledge our core donors for their support and commitment to icddr,b’s research efforts. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Data Availability
This data set contains some personal information of the study patients (such as name, admission date, month, area of residence). Our IRB has required that the personal information of the participants is not disclosed. Thus, the policy of our centre (icddr,b) is that we should not make the availability of whole data set in the manuscript, the supplemental files, or a public repository. However, data related to this manuscript are available upon request and for researchers who meet the criteria for access to confidential data may contact with Armana Ahmed (armana@icddrb.org) to the Research Administration of icddr,b (http://www.icddrb.org/).
Funding Statement
This study was funded by International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b; grant no Gr-00233) and its donors. This manuscript is partially supported by funding from the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health (NIH) under Award Number R01AI153399. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Puzari M, Sharma M, Chetia P. Emergence of antibiotic resistant Shigella species: A matter of concern. Journal of infection and public health. 2018;11(4):451–4. doi: 10.1016/j.jiph.2017.09.025 [DOI] [PubMed] [Google Scholar]
- 2.Ashkenazi S, Levy I, Kazaronovski V, Samra Z. Growing antimicrobial resistance of Shigella isolates. Journal of Antimicrobial Chemotherapy. 2003;51(2):427–9. doi: 10.1093/jac/dkg080 [DOI] [PubMed] [Google Scholar]
- 3.Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathogens and global health. 2015;109(7):309–18. doi: 10.1179/2047773215Y.0000000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mokomane M, Kasvosve I, Melo Ed, Pernica JM, Goldfarb DM. The global problem of childhood diarrhoeal diseases: emerging strategies in prevention and management. Therapeutic advances in infectious disease. 2018;5(1):29–43. doi: 10.1177/2049936117744429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sack DA, Lyke C, McLaughlin C, Suwanvanichkij V, Organization WH. Antimicrobial resistance in shigellosis, cholera and campylobacteriosis. World Health Organization, 2001. [Google Scholar]
- 6.Raja SB, Murali MR, Devaraj SN. Differential expression of ompC and ompF in multidrug-resistant Shigella dysenteriae and Shigella flexneri by aqueous extract of Aegle marmelos, altering its susceptibility toward β-lactam antibiotics. Diagnostic microbiology and infectious disease. 2008;61(3):321–8. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharya D, Bhattacharya H, Thamizhmani R, Sayi D, Reesu R, Anwesh M, et al. Shigellosis in Bay of Bengal Islands, India: clinical and seasonal patterns, surveillance of antibiotic susceptibility patterns, and molecular characterization of multidrug-resistant Shigella strains isolated during a 6-year period from 2006 to 2011. European journal of clinical microbiology & infectious diseases. 2014;33(2):157–70. [DOI] [PubMed] [Google Scholar]
- 8.Kar AK, Ghosh AS, Chauhan K, Ahamed J, Basu J, Chakrabarti P, et al. Involvement of a 43-kilodalton outer membrane protein in beta-lactam resistance of Shigella dysenteriae. Antimicrobial agents and chemotherapy. 1997;41(10):2302–4. doi: 10.1128/AAC.41.10.2302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranjbar R, Farahani A. Shigella: antibiotic-resistance mechanisms and new horizons for treatment. Infection and drug resistance. 2019;12:3137. doi: 10.2147/IDR.S219755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hussen S, Mulatu G, Kassa ZY. Prevalence of Shigella species and its drug resistance pattern in Ethiopia: a systematic review and meta-analysis. Annals of clinical microbiology and antimicrobials. 2019;18(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Organization WH. Pocket book of hospital care for children: guidelines for the management of common childhood illnesses: World Health Organization 2013. https://apps.who.int/iris/handle/10665/81170. [PubMed] [Google Scholar]
- 12.Li MY, Kelly J, Subhi R, Were W, Duke T. Global use of the WHO pocket book of hospital care for children. Paediatrics and international child health. 2013;33(1):4–11. doi: 10.1179/2046905512Y.0000000017 [DOI] [PubMed] [Google Scholar]
- 13.Khatun F, Faruque A, Koeck J, Olliaro P, Millet P, Paris N, et al. Changing species distribution and antimicrobial susceptibility pattern of Shigella over a 29-year period (1980–2008). Epidemiology & Infection. 2011;139(3):446–52. [DOI] [PubMed] [Google Scholar]
- 14.Pickering LK, Baker CJ, Kimberlin DW. Red Book, (2012): Report of the Committee on Infectious Diseases: Am Acad Pediatrics; 2012. [Google Scholar]
- 15.Williams PC, Berkley JA. Guidelines for the treatment of dysentery (shigellosis): a systematic review of the evidence. Paediatrics and international child health. 2018;38(sup1):S50–S65. doi: 10.1080/20469047.2017.1409454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahbubur R, Shoma S, Rashid H, El Arifeen S, Baqui AH, Siddique A, et al. Increasing spectrum in antimicrobial resistance of Shigella isolates in Bangladesh: resistance to azithromycin and ceftriaxone and decreased susceptibility to ciprofloxacin. Journal of health, population, and nutrition. 2007;25(2):158. [PMC free article] [PubMed] [Google Scholar]
- 17.Basualdo W, Arbo A. Randomized comparison of azithromycin versus cefixime for treatment of shigellosis in children. The Pediatric infectious disease journal. 2003;22(4):374–7. [PubMed] [Google Scholar]
- 18.Rahman M, Sultana R, Ahmed G, Nahar S, Hassan ZM, Saiada F, et al. Prevalence of G2P [4] and G12P [6] rotavirus, Bangladesh. Emerging infectious diseases. 2007;13(1):18. doi: 10.3201/eid1301.060910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edwards PR, Ewing WH. Identification of enterobacteriaceae. Identification of Enterobacteriaceae. 1972;(Third edition). [Google Scholar]
- 20.Parvin I, Shahid ASMSB, Das S, Shahrin L, Ackhter MM, Alam T, et al. Vibrio cholerae O139 persists in Dhaka, Bangladesh since 1993. PLoS neglected tropical diseases. 2021;15(9):e0009721. doi: 10.1371/journal.pntd.0009721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barry A, Thornsberry C, Gavan T. Quality control parameters and interpretive criteria for in vitro susceptibility tests with the macrolide azithromycin. European Journal of Clinical Microbiology and Infectious Diseases. 1989;8(6):544–9. [DOI] [PubMed] [Google Scholar]
- 22.Ferdous F, Ahmed S, Farzana F, Das J, Malek M, Das S, et al. Aetiologies of diarrhoea in adults from urban and rural treatment facilities in Bangladesh. Epidemiology & Infection. 2015;143(7):1377–87. doi: 10.1017/S0950268814002283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jahan Y, Moriyama M, Hossain S, Rahman MM, Ferdous F, Ahmed S, et al. Relation of childhood diarrheal morbidity with the type of tube well used and associated factors of Shigella sonnei diarrhea in rural Bangladesh site of the Global Enteric Multicenter Study. Tropical medicine and health. 2019;47(1):1–10. doi: 10.1186/s41182-019-0158-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam M, Siddika A, Khan M, Goldar M, Sadique MA, Kabir A, et al. Microbiological analysis of tube-well water in a rural area of Bangladesh. Applied and Environmental microbiology. 2001;67(7):3328–30. doi: 10.1128/AEM.67.7.3328-3330.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bardsley M, Jenkins C, Mitchell HD, Mikhail AF, Baker KS, Foster K, et al. Persistent transmission of shigellosis in England is associated with a recently emerged multidrug-resistant strain of Shigella sonnei. Journal of clinical microbiology. 2020;58(4):e01692–19. doi: 10.1128/JCM.01692-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ingle DJ, Andersson P, Valcanis M, Barnden J, da Silva AG, Horan KA, et al. Prolonged outbreak of multidrug-resistant Shigella sonnei harboring bla CTX-M-27 in victoria, Australia. Antimicrobial Agents and Chemotherapy. 2020;64(12):e01518–20. doi: 10.1128/AAC.01518-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kozyreva VK, Jospin G, Greninger AL, Watt JP, Eisen JA, Chaturvedi V. Recent outbreaks of shigellosis in California caused by two distinct populations of Shigella sonnei with either increased virulence or fluoroquinolone resistance. Msphere. 2016;1(6):e00344–16. doi: 10.1128/mSphere.00344-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson M, Sansonetti PJ, Marteyn BS. Shigella diversity and changing landscape: insights for the twenty-first century. Frontiers in cellular and infection microbiology. 2016;6:45. doi: 10.3389/fcimb.2016.00045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sack DA, Hoque S, Etheridge M, Huq A. Is protection against shigellosis induced by natural infection with Plesiomonas shigelloides? The Lancet. 1994;343(8910):1413–5. doi: 10.1016/s0140-6736(94)92531-3 [DOI] [PubMed] [Google Scholar]
- 30.Holt KE, Baker S, Weill F-X, Holmes EC, Kitchen A, Yu J, et al. Shigella sonnei genome sequencing and phylogenetic analysis indicate recent global dissemination from Europe. Nature genetics. 2012;44(9):1056–9. doi: 10.1038/ng.2369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Von Seidlein L, Kim DR, Ali M, Lee H, Wang X, Thiem VD, et al. A multicentre study of Shigella diarrhoea in six Asian countries: disease burden, clinical manifestations, and microbiology. PLoS medicine. 2006;3(9):e353. doi: 10.1371/journal.pmed.0030353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keusch GT, Bennish ML. Shigellosis: recent progress, persisting problems and research issues. The Pediatric infectious disease journal. 1989;8(10):713–9. [PubMed] [Google Scholar]
- 33.Basnet B, Niroula D, Acharya J, Basnyat S. Antibiotic Susceptibility Pattern of Shigella spp. Isolated from Patients Suspected of Acute Gastroenteritis. Journal of Institute of Science and Technology. 2021;26(2):1–7. [Google Scholar]
- 34.Ashkenazi S, May-Zahav M, Sulkes J, Zilberberg R, Samra Z. Increasing antimicrobial resistance of Shigella isolates in Israel during the period 1984 to 1992. Antimicrobial agents and chemotherapy. 1995;39(4):819–23. doi: 10.1128/AAC.39.4.819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vinh H, Wain J, Chinh MT, Tam CT, Trang PTT, Nga D, et al. Treatment of bacillary dysentery in Vietnamese children: two doses of ofloxacin versus 5-days nalidixic acid. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2000;94(3):323–6. doi: 10.1016/s0035-9203(00)90343-2 [DOI] [PubMed] [Google Scholar]
- 36.Organization WH. Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type 1. 2005. [Google Scholar]
- 37.Niyogi S. Increasing antimicrobial resistance—an emerging problem in the treatment of shigellosis. Elsevier; 2007. [DOI] [PubMed] [Google Scholar]
- 38.Baker KS, Dallman TJ, Ashton PM, Day M, Hughes G, Crook PD, et al. Intercontinental dissemination of azithromycin-resistant shigellosis through sexual transmission: a cross-sectional study. The Lancet infectious diseases. 2015;15(8):913–21. doi: 10.1016/S1473-3099(15)00002-X [DOI] [PubMed] [Google Scholar]
- 39.Baker KS, Dallman TJ, Field N, Childs T, Mitchell H, Day M, et al. Horizontal antimicrobial resistance transfer drives epidemics of multiple Shigella species. Nature communications. 2018;9(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guglielmino CJ, Kakkanat A, Forde BM, Rubenach S, Merone L, Stafford R, et al. Outbreak of multi-drug-resistant (MDR) Shigella flexneri in northern Australia due to an endemic regional clone acquiring an IncFII plasmid. European Journal of Clinical Microbiology & Infectious Diseases. 2021;40(2):279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klontz EH, Das SK, Ahmed D, Ahmed S, Chisti MJ, Malek MA, et al. Long-term comparison of antibiotic resistance in Vibrio cholerae O1 and Shigella species between urban and rural Bangladesh. Clinical Infectious Diseases. 2014;58(9):e133–e6. doi: 10.1093/cid/ciu040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Farsiani H, Sasan MS. High rate of resistance to ceftriaxone and azithromycin among Shigella spp. isolates at three children’s referral hospitals in Northeast Iran. Journal of Infection and Chemotherapy. 2020;26(9):955–8. [DOI] [PubMed] [Google Scholar]
- 43.Saeed DK, Farooqi J, Shakoor S, Hasan R. Antimicrobial resistance among GLASS priority pathogens from Pakistan: 2006–2018. BMC infectious diseases. 2021;21(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Control CfD Prevention. Antibiotic resistance threats in the United States, 2019. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. 2019. [Google Scholar]
- 45.Nüesch-Inderbinen M, Heini N, Zurfluh K, Althaus D, Hächler H, Stephan R. Shigella antimicrobial drug resistance mechanisms, 2004–2014. Emerg Infect Dis. 2016;22(6):1083. doi: 10.3201/eid2206.152088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Worley JN, Javkar K, Hoffmann M, Hysell K, Garcia-Williams A, Tagg K, et al. Genomic drivers of multidrug-resistant shigella affecting vulnerable patient populations in the United States and abroad. Mbio. 2021;12(1):e03188–20. doi: 10.1128/mBio.03188-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chowdhury M, Stewart Williams J, Wertheim H, Khan WA, Matin A, Kinsman J. Rural community perceptions of antibiotic access and understanding of antimicrobial resistance: qualitative evidence from the Health and Demographic Surveillance System site in Matlab, Bangladesh. Global Health Action. 2019;12(sup1):1824383. doi: 10.1080/16549716.2020.1824383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sutradhar KB, Saha A, Huda NH, Uddin R. Irrational use of antibiotics and antibiotic resistance in southern rural Bangladesh: perspectives from both the physicians and patients. Annual Research & Review in Biology. 2014:1421–30. [Google Scholar]
- 49.Rogawski ET, Liu J, Platts-Mills JA, Kabir F, Lertsethtakarn P, Siguas M, et al. Use of quantitative molecular diagnostic methods to investigate the effect of enteropathogen infections on linear growth in children in low-resource settings: longitudinal analysis of results from the MAL-ED cohort study. The Lancet Global Health. 2018;6(12):e1319–e28. doi: 10.1016/S2214-109X(18)30351-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
This data set contains some personal information of the study patients (such as name, admission date, month, area of residence). Our IRB has required that the personal information of the participants is not disclosed. Thus, the policy of our centre (icddr,b) is that we should not make the availability of whole data set in the manuscript, the supplemental files, or a public repository. However, data related to this manuscript are available upon request and for researchers who meet the criteria for access to confidential data may contact with Armana Ahmed (armana@icddrb.org) to the Research Administration of icddr,b (http://www.icddrb.org/).