Background:
Some patients develop long-term symptoms after Corona virus disease 2019 (COVID-19), and chronic fatigue syndrome (CFS) is one of the main symptoms. CFS is characterized by fatigue lasting for more than 6 months accompanied by sleep disorders, anxiety, and depression, which causes a certain degree of harm to both physiological and psychological aspects of the individual. Traditional Chinese exercises (TCEs) are an ancient Chinese therapy and has recently been reported to be effective for CFS. Therefore, we will conduct a systematic review and meta-analysis aiming to accurately evaluate the efficacy of TCEs on post-COVID-19 CFS and provide an alternative treatment for post-COVID-19 CFS.
Methods:
Seven databases (PubMed, Ovid Embase, Cochrane Library, Web of Science, Chinese National Knowledge Infrastructure (CNKI), China Biology Medicine (CBM), and Wanfang) will be searched from establishment to August 2022, and we will only include randomized controlled trials of TCEs for post-COVID-19 CFS. Two reviews will independently include the research according to the inclusion and exclusion criteria. Review Manager 5.2 software will be used to analyze the accepted literature, and the relative risk ratio (RR) and 95% confidence interval (CI) will be used as effect indicators for the outcome indicator dichotomous variables. For continuous variables, weighted mean difference (MD) and 95% CI will be used as effect indicators. The heterogeneity test will be assessed using the I2 statistic and Q statistic. The PEDro scale was used to evaluate the methodological quality of the included studies. Subgroup analysis was performed according to different TCEs, age, gender, and duration of CFS.
Results:
This systematic review and meta-analysis will evaluate the efficacy of TCEs in post-COVID-19 CFS.
Conclusion:
The results of this study will provide reliable evidence for the effects of TCEs for post-COVID-19 CFS on patients’ fatigue, anxiety, depression, sleep, and quality of life.
Keywords: anxiety, chronic fatigue syndrome, depression, post-COVID-19, traditional Chinese exercises
1. Introduction
The novel Corona virus disease 2019 (COVID-19) pandemic has been lasting for nearly three years, a proportion of patients with mild to moderate COVID-19 develop long-term symptoms, and chronic fatigue syndrome (CFS) is one of the main symptoms.[1–3] CFS, also known as myalgic encephalomyelitis, is a complicated chronic disease characterized by chronic fatigue lasting for more than 6 months. It is also accompanied by severe fatigue symptoms, depression, anxiety, and sleep disturbances, which seriously affects the quality of life of patients. what’s more, though the disease is not life-threatening, it may cause disability as well as rheumatoid arthritis and systemic lupus erythematosus.[4–6] The prevalence of CFS is estimated to be between 1% and 2% globally, causing a serious burden on the work and life of patients.[7,8] It is reported that at least 1 million people in the United States have CFS and that it is three to four times more common in women than in men, with the highest prevalence in people aged 40 to 50 years, but children and adolescents are also at risk.[9] And it has a huge impact on the American economy, costing approximately $9 to 37 billion in lost productivity and $9 to 14 billion in direct medical costs annually.[10,11] CFS is defined as a complex multisystem disease, and the pathogenesis of CFS is still unclear.[12] In addition, due to the lack of biological disease markers, approximately 20 diagnostic criteria are available for CFS, and the symptoms of CFS can be easily confused with diseases such as the flu has led to a tendency to underdiagnose patients with CFS, which is a great test for consultation rates and patient compliance.[13–15] Unfortunately, no specific medication is available to treat CFS, and only symptom relief is available. Considering the drug dependence and poor stability, more patients are turning to alternative therapies to relieve fatigue and improve quality of life.[16]
In China, Traditional Chinese exercises (TCEs) are widely used in the treatment of CFS. The exercises include Tai Chi, BaduanjJin, Yijinjing, Qigong, and Five-animal exercises, which play a major role in preventing and treating CFS.[17] They can be used to unify the mind and body, eliminate fatigue and improve sleep quality through a wonderful combination of movements.[18,19] They can also regulate the mood of CFS patients and provide better relief from anxiety and depression.[20] Some studies have reported that TCEs have a positive effect on a patient’s physical function and mind, and the mechanism may be an increase in telomerase activity.[21,22] Compared to common exercise therapy, TCEs may have similar health effects, but they are less intense and experience lower energy metabolism, which makes them more suitable for administration in patients with post-COVID-19 CFS.[23] However, previous studies have only systematically reviewed partial TCEs for CFS, and insufficient evidence exists to support the effects of TCEs in improving fatigue, emotion, sleep, and quality of life in individuals with post-COVID-19 CFS.[24,25] The evidence is still insufficient for TCEs in post-covid-19 CFS.
Therefore, the current study aimed to obtain a convincing conclusion as to whether TCEs contribute to a positive effect on fatigue, sleep, anxiety, depression, and quality of life in patients with CFS.
2. Methods
2.1. Study registration
This protocol of this systematic review strictly follows the PRISMA-P guidelines with a registration number (CRD42022361265) registered on the PROSPERO, and if necessary, we will keep our protocol constantly updated.[26]
2.2. Eligibility criteria
2.2.1. Types of studies.
Only randomized controlled trials of TCEs for post-COVID-19 CFS will be included in this systematic review, and only randomized controlled trials in Chinese and English will be included.
2.2.2. Types of participants.
First of all, the patients must have been previously infected with SARS-CoV-2 with typical symptoms and positive polymerase chain reaction test or antibodies without vaccination.[27] And then, we will include the post-COVID-19 CFS patients who met either of the following diagnostic criteria: the Fukuda or Centers for Disease Control and Prevention criteria (CDC, 1994), Canadian Consensus Criteria (CCC, 2003), and the International Consensus Criteria (ICC, 2011).[28–31]
2.2.3. Types of interventions and comparisons.
Post-COVID-19 CFS patients were treated by TCEs as the intervention group. The comparison groups involve other treatments, such as Common exercise, acupuncture, physiotherapy, and other therapies.
2.3. Types of outcome measures
2.3.1. Primary outcomes.
The primary outcome was assessed by the recognized fatigue, anxiety, and depression scales: Fatigue Scale-14 (FS-14), Multidimensional Fatigue Inventory-20 (MFI-20), Hospital Anxiety and Depression Scale (HADS), Self-rating Depression Scale (SDS), and Self-Rating Anxiety Scale (SAS).
2.3.2. Secondary outcomes.
The secondary outcomes will include quality of life, sleep, and anxiety. These items will also be assessed using following scales and neuropeptide substances: Neuropeptide Y (NPY), Calcitonin gene-related peptide (CGRP), the MOS item short form-36 health survey (SF-36), Pittsburgh Sleep Quality Index (PSQI).
2.4. Data sources
Seven databases (PubMed, Ovid Embase, Cochrane Library, Web of Science, Chinese National Knowledge Infrastructure (CNKI), China Biology Medicine (CBM), and Wanfang) will be searched from the beginning to August 2022 to choose RCTs that meet the requirements above. Table 1 shows the search strategy for the PubMed.
Table 1.
Search strategy for PubMed database.
| No. | Search items |
|---|---|
| #1 | “Fatigue Syndrome, Chronic”[Mesh] |
| #2 | “Chronic Fatigue Syndromes”[Title/Abstract] OR “Chronic Fatigue Syndromes”[Title/Abstract] OR “Chronic Fatigue Disorder”[Title/Abstract] OR “Fatigue Disorders, Chronic”[Title/Abstract] OR “fatigue”[Title/Abstract] |
| #3 | #1 OR #2 |
| #4 | “post-acute COVID-19 syndrome” [Supplementary Concept]” OR “long-COVID”[Title/Abstract] OR “post-acute COVID syndrome”[Title/Abstract] OR “long COVID”[Title/Abstract] OR “chronic COVID syndrome”[Title/Abstract] |
| #5 | #3 AND #4 |
| #6 | “traditional Chinese exercises”[Title/Abstract] OR “Tai Ji”[Mesh] OR “ Tai Chi”[Title/Abstract] OR “Tai Chi Chuan”[Title/Abstract] OR “Qigong”[Mesh] OR “Qi Gong”[Title/Abstract] OR “Baduanjin”[Title/Abstract] OR “Yijinjing”[Title/Abstract] OR “Five-animal exercises”[Title/Abstract] OR “Wuqinxi”[Title/Abstract] |
| #7 | “randomized controlled trial”[Publication Type] OR “randomized”[Title/Abstract] OR “placebo”[Title/Abstract |
| #8 | #3 AND #5 AND #7 |
2.5. Search strategy
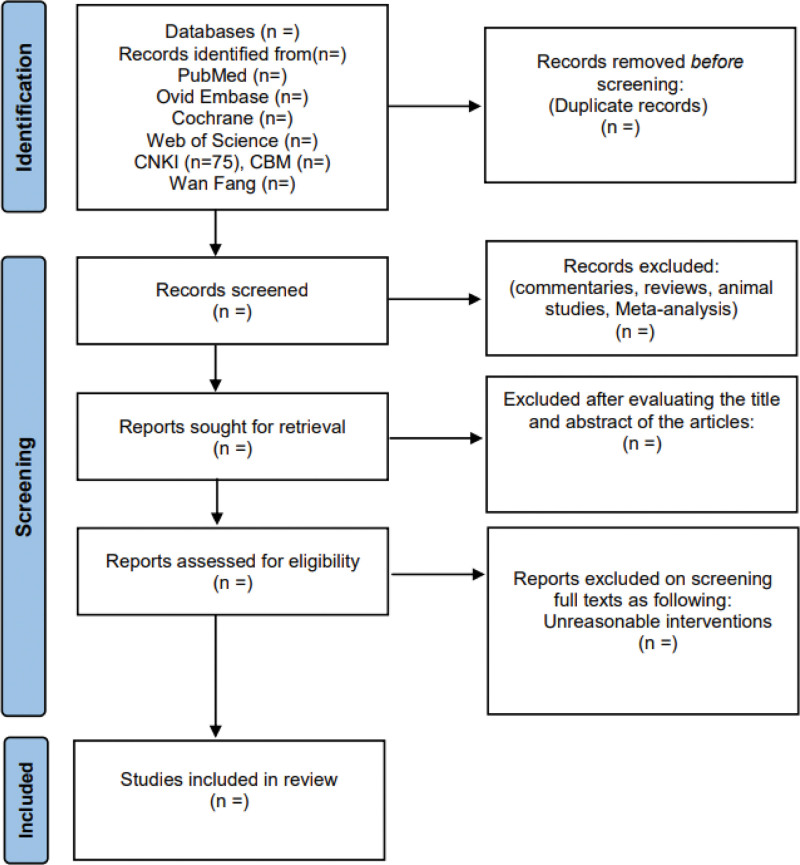
2.5.1. Study selection.
After eliminating duplicates from the retrieved research, two researchers will independently review the titles, abstracts, and eventually the full text according to the eligibility criteria. We will conduct a Cross-checking with each other after the screening was completed, and disagreements will be arbitrated by a third investigator. Figure 1 shows the process of the entire research selection.
Figure 1.
Flow chart for the review.
2.5.2. Data extraction.
Two reviewers (LZ, SJ) will jointly complete the data extraction. The following extracted data will be included: random assignment protocol, authors’ names, year of literature publication, number of included cases, age, interventions, control measures, treatment period, outcome indicators, diagnostic criteria, and dropouts. After checking, we fill in the data transformation into Review Manager 5.2, and disagreements will be arbitrated by a third investigator.
2.6. Quality evaluation
The quality of the RCTs will be assessed and scored by two reviewers using the Cochrane Risk of Bias Tool and the PEDro Scale. Biases in selection, performance, detection, attrition, reporting, and other aspects will be evaluated and classified as “low risk,” “high risk,” or “unclear,” the above are six items for the Cochrane bias risk tool. And the PEDro scale is composed of the following 11 items: predetermined research eligibility criteria, random patient assignment, allocation concealment, baseline data on between-group similarities, subject blinding, physical therapist blinding, assessor blinding, less than 15% dropouts, intention-to-treat analysis, comparison of between-group statistics, point measurement and variability data. Items 2 through 11 of the PEDro were assessed, resulting in a final score of 10 (item 1 was not scored).
2.7. Data synthesis
Review Manager 5.2 will be used to evaluate the selected research. We will use the relative risk ratio and 95% confidence interval (CI) to evaluate dichotomous data, and the standardized mean difference (MD) and 95% CI will be used to analyze continuous data. The heterogeneity test used I2 value and Q test as an effect indicator.[32]
2.7.1. Subgroup analysis.
If high heterogeneity exists, we will perform subgroup analysis for sex, age, duration of exercise, duration of CFS, and different TCEs.
2.7.2. Sensitivity analysis.
If the studies that will be included are of low quality or numerically far from other studies, we will conduct sensitivity analysis. Besides, we will iteratively remove one study at a time from Review Manager 5.2 to finish the analysis.
2.8. Ethics and dissemination
Systematic reviews don’t need ethics approval. Additionally, peer-reviewed publications will publish the current review’s findings.
3. Discussion
It is reported that COVID-19 pandemic contributes to an increase in CFS patients.[33] Since viral infections are frequently the cause of CFS, also since about 30% of individuals who don’t fully recover from the acute phase of COVID-19 suffer from the condition known as the post-COVID-19 syndrome, which is characterized by fatigue intolerance, persistent fatigue, insomnia and anxiety.[34–36] TCEs are painless therapies inherited from China and have high safety. It has been proven in a randomized controlled trial that TCEs can relieve fatigue and insomnia in CFS, but no systematic review of TCEs for post-COVID-19 CFS is currently available.[20] Therefore, the present systematic review and meta-analysis will evaluate the evidence of fatigue, anxiety, depression, sleep, and quality of life in TCEs for post-COVID-19 CFS. The results of the study will provide patients with the option of pain-free treatment for post-COVID-19 CFS. Importantly, the financial burden on patients will be greatly alleviated.
Author contributions
Conceptualization: Zhen Liu.
Data curation: Jiao Shi, Huazhi Huang, Shuangwei Hong, Zhen Liu, Zhizhen Lv.
Formal analysis: Zhen Liu, Zhizhen Lv.
Funding acquisition: Lijiang Lv.
Investigation: Lijiang Lv, Zhizhen Lv.
Methodology: Jiao Shi, Xingchen Zhou, Zhen Liu.
Supervision: Lijiang Lv.
Writing – original draft: Zhen Liu.
Writing – review & editing: Zhen Liu, Zhizhen Lv.
Abbreviations:
- CFS =
- chronic fatigue syndrome
- CI =
- confidence interval
- COVID-19 =
- Corona virus disease 2019
- TCEs =
- Traditional Chinese Exercises
The datasets generated during and/or analyzed during the current study are publicly available. All data generated or analyzed during this study are included in this published article [and its supplementary information files].
This study is supported by the Key Discipline of Chinese Medicine (Tui Na), State Administration of Traditional Chinese Medicine (No. GJXK-2022-02-01), and the National Key Clinical Specialties Construction Project (No. GWYF-2013-42).
The authors have no conflicts of interest to disclose.
How to cite this article: Liu Z, Lv Z, Zhou X, Shi J, Hong S, Huang H, Lv L. Efficacy of traditional Chinese exercises in patients with post-COVID-19 chronic fatigue syndrome: A protocol for systematic review and meta-analysis. Medicine 2022;101:46(e31450).
Contributor Information
Zhen Liu, Email: Alexliu049@163.com.
Zhizhen Lv, Email: 731577158@qq.com.
Xingchen Zhou, Email: zhouxingchen0210@163.com.
Jiao Shi, Email: 1458815678@qq.com.
Shuangwei Hong, Email: 919632329@qq.com.
Huazhi Huang, Email: 610213561@qq.com.
References
- [1].Kachaner A, Lemogne C, Dave J, et al. Somatic symptom disorder in patients with post-COVID-19 neurological symptoms: a preliminary report from the somatic study (Somatic Symptom Disorder Triggered by COVID-19). J Neurol Neurosurg Psychiatry. 2022. [DOI] [PubMed] [Google Scholar]
- [2].Kedor C, Freitag H, Meyer-Arndt L, et al. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat Commun. 2022;13:5104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Maes M, Al-Rubaye HT, Almulla AF, et al. Lowered quality of life in long COVID is predicted by affective symptoms, chronic fatigue syndrome, inflammation and neuroimmunotoxic pathways. Int J Environ Res Public Health. 2022;19:10362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Froehlich L, Hattesohl DB, Cotler J, et al. Causal attributions and perceived stigma for myalgic encephalomyelitis/chronic fatigue syndrome. J Health Psychol. 2022;27:2291–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sandler CX, Lloyd AR. Chronic fatigue syndrome: progress and possibilities. Med J Aust. 2020;212:428–33. [DOI] [PubMed] [Google Scholar]
- [6].Falk Hvidberg M, Brinth LS, Olesen AV, et al. The health-related quality of life for patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). PLoS One. 2015;10:e0132421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zhao S, Chi A, Wan B, et al. Differential metabolites and metabolic pathways involved in aerobic exercise improvement of chronic fatigue symptoms in adolescents based on gas chromatography-mass spectrometry. Int J Environ Res Public Health. 2022;19:2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rowe KS. Long term follow up of young people with chronic fatigue syndrome attending a pediatric outpatient service. Front Pediatr. 2019;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Unger ER, Lin JS, Brimmer DJ, et al. CDC grand rounds: chronic fatigue syndrome – advancing research and clinical education. MMWR Morb Mortal Wkly Rep. 2016;65:1434–8. [DOI] [PubMed] [Google Scholar]
- [10].Lin JS, Resch SC, Brimmer DJ, et al. The economic impact of chronic fatigue syndrome in Georgia: direct and indirect costs. Cost Effectiveness Res Allocation. 2011;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Reynolds KJ, Vernon SD, Bouchery E, et al. The economic impact of chronic fatigue syndrome. Cost Effectiveness Res Allocation. 2004;2:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].O’Neal AJ, Hanson MR. The enterovirus theory of disease etiology in myalgic encephalomyelitis/chronic fatigue syndrome: a critical review. Front Med. 2021;8:688486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jonsjö MA, Olsson GL, Wicksell RK, et al. The role of low-grade inflammation in ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) – associations with symptoms. Psychoneuroendocrinology. 2020;113:104578. [DOI] [PubMed] [Google Scholar]
- [14].Brurberg KG, Fønhus MS, Larun L, et al. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open. 2014;4:e003973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lim EJ, Son CG. Review of case definitions for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med. 2020;18:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Collatz A, Johnston SC, Staines DR, et al. A systematic review of drug therapies for chronic fatigue syndrome/myalgic encephalomyelitis. Clin Ther. 2016;38:1263–1271.e9. [DOI] [PubMed] [Google Scholar]
- [17].Wu YH, He WB, Gao YY, et al. Effects of traditional Chinese exercises and general aerobic exercises on older adults with sleep disorders: a systematic review and meta-analysis. J Integr Med. 2021;19:493–502. [DOI] [PubMed] [Google Scholar]
- [18].Lan C, Chen SY, Lai JS, et al. Tai chi chuan in medicine and health promotion. Evid Based Complement Alternat Med. 2013;2013:502131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Fan B, Song W, Zhang J, et al. The efficacy of mind-body (Baduanjin) exercise on self-reported sleep quality and quality of life in elderly subjects with sleep disturbances: a randomized controlled trial. Sleep Breathing. 2020;24:695–701. [DOI] [PubMed] [Google Scholar]
- [20].Xie F, You Y, Guan C, et al. The qigong of prolong life with nine turn method relieve fatigue, sleep, anxiety and depression in patients with chronic fatigue syndrome: a randomized controlled clinical study. Front Med. 2022;9:828414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ho RT, Chan JS, Wang CW, et al. A randomized controlled trial of qigong exercise on fatigue symptoms, functioning, and telomerase activity in persons with chronic fatigue or chronic fatigue syndrome. Annal Behav Med. 2012;44:160–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chen S, Zhang Y, Wang YT, et al. Traditional Chinese mind and body exercises for promoting balance ability of old adults: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2016;2016:7137362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kong L, Ren J, Fang S, et al. Traditional Chinese exercises on pain and disability in middle-aged and elderly patients with neck pain: a systematic review and meta-analysis of randomized controlled trials. Front Aging Neurosci. 2022;14:912945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang R, Huang X, Wu Y, et al. Efficacy of qigong exercise for treatment of fatigue: a systematic review and meta-analysis. Front Med. 2021;8:684058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Fang J, Zhang L, Wu F, et al. The safety of baduanjin exercise: a systematic review. Evid Based Complement Alternat Med. 2021;2021:8867098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed.). 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [27].Hejbøl EK, Harbo T, Agergaard J, et al. Myopathy as a cause of fatigue in long-term post-COVID-19 symptoms: evidence of skeletal muscle histopathology. Eur J Neurol. 2022;29:2832–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International chronic fatigue syndrome study group. Ann Intern Med. 1994;121:953–9. [DOI] [PubMed] [Google Scholar]
- [29].Carruthers BM, van de Sande MI, De Meirleir KL, et al. Myalgic encephalomyelitis: international consensus criteria. J Intern Med. 2011;270:327–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Sasso EM, Muraki K, Eaton-Fitch N, et al. Transient receptor potential melastatin 3 dysfunction in post COVID-19 condition and myalgic encephalomyelitis/chronic fatigue syndrome patients. Mol Med (Cambridge, Mass). 2022;28:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Carruthers BM, Jain AK, De Meirleir KL, et al. Myalgic encephalomyelitis/chronic fatigue syndrome: clinical working case definition, diagnostic and treatment protocols. J Chron Fatigue Syndrome. 2003;11:7–115. [Google Scholar]
- [32].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [33].Araja D, Berkis U, Lunga A, et al. Shadow burden of undiagnosed myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) on society: retrospective and prospective-in light of COVID-19. J Clin Med. 2021;10:3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Sotzny F, Blanco J, Capelli E, et al. Myalgic encephalomyelitis/chronic fatigue syndrome - evidence for an autoimmune disease. Autoimmun Rev. 2018;17:601–9. [DOI] [PubMed] [Google Scholar]
- [35].Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. 2021;4:e210830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Flaskamp L, Roubal C, Uddin S, et al. Serum of post-COVID-19 syndrome patients with or without ME/CFS differentially affects endothelial cell function in vitro. Cells. 2022;11:2376. [DOI] [PMC free article] [PubMed] [Google Scholar]