Abstract
The incidence and mortality rates of stroke in China are higher than the world average, seriously endangering the public’s health and quality of life. It is important to predict the incidence of stroke, identify the high-risk factors in the region, and raise the risk awareness of high-risk groups. This study sought to investigate and analyze the distribution of stroke population and the main risk factors for stroke occurrence in a Chinese population, and to predict the probability of stroke occurrence in high-risk groups with risk factors, so as to provide a scientific basis for the comprehensive prevention and treatment of stroke. A whole-group sampling method was used to investigate 1009 participants in Jingzhou city in central China, and a uniform questionnaire survey and related medical examinations were conducted. The risk factors for stroke in the area were analyzed by univariate analysis, and a multifactorial logistic regression prediction model was established based on the results of univariate analysis. The results of univariate and multifactorial logistic regression analyses suggested that gender, age, family history of stroke, hypertension, atrial fibrillation, diabetes, and sedentary lifestyle were significantly associated with an increased risk of stroke in the local population (all P < .05). The top 5 risk factors for stroke were atrial fibrillation (odds ratio [OR] = 5.225, 95% confidence interval [CI]: 2.826–9.663), sedentary lifestyle (OR = 2.701, 95% CI: 1.667–4.376), age (≥65 years) (OR = 2.593, 95% CI: 1.680–4.004), hypertension (OR = 2.106, 95% CI: 1.380–3.216), and gender (male) (OR = 2.099, 95% CI: 1.270–3.471). This study effectively identifies the high risk factors for stroke and provides scientific insights for risk assessment, intervention of risk factors, and decision making of health management departments in the central region of China. The modifable risk factors for stroke such as smoking, hypertension, atrial fibrillation, diabetes mellitus, and sedentary lifestyle were also observed. Our findings further highlight the significant of the primary and secondary prevention for stroke and reveal the potential targets to reduce the heavy stroke burden in China around the world.
Keywords: high-risk population, logistic regression, risk factors, stroke
1. Introduction
The global burden of stroke substantially increased from 1990 to 2019, especially in the developing countries.[1] Globally, stroke was described as the second leading cause of death, and the third most common reason for disability combined in 2019.[1,2] The incidence and mortality rates of stroke in China are higher than the world average due to various factors such as differences in living environment, genetics, lifestyle habits, dietary structure, and the aging of the population, etc.[3] The burden of stroke on Chinese population is particularly heavy, especially from ischemic stroke.[4] The MONICA study of the World Health Organization showed that the incidence of stroke in China was increasing at an annual rate of 8.7%, and about 30% of those who developed stroke died and 70% of those who survived suffered from disabilities such as hemiplegia and aphasia,[5] seriously endangering the public’s health and quality of life. In addition, the incidence of stroke is showing a younger trend and the recurrence rate is becoming higher, which also brings a heavy economic burden to society and families.
The overwhelming incidence and mortality rates of stroke in China make it essential to evaluate the predisposing risk factors for stroke in Chinese population. In 2009, the Ministry of Health in China launched the Stroke Screening and Prevention Project to promote stroke prevention, strengthen public education, formulate guidelines for stroke prevention and treatment, and carry out stroke screening and interventions nationwide.[6] In recent years, we have actively carried out screening works for stroke risk factors in outpatients, inpatients, and people in the community and townships, thereby establishing health records for the screened high-risk groups, further taking layer management measures and targeted interventions for them. This work is an effective means of preventing cerebrovascular lesions and stroke. Since the causes and risk factors of stroke remain unknown and vary by ethnicity and geographical area in the world, knowledge of potential stroke risk factors is essential for population-specific risk assessment for stroke. In this study, we investigated and analyzed the distribution of stroke population, and evaluated the main risk factors for stroke occurrence in 1009 participants from Jingzhou city in central China, so as to provide a scientific basis for early comprehensive prevention and treatment of stroke.
2. Methods
2.1. Study population
A whole-group sampling method was used to conduct this cross-sectional study. The study included 1009 participants in Jingzhou city in central China from November 2014 to November 2021, and a uniform questionnaire survey and related medical examinations were conducted by the research team. The data were completely collected and systematically analyzed. The recruiting criteria for the subjects of the study population was as follows: permanent residents who had lived in this region for more than 6 months, age ≥ 40 years old, the clinical data was complete, meeting all of the above criteria. Patients who suffered from mental disorders, Alzheimer’s disease, intellectual disability and others who could not cooperate were excluded. This study was approved by the Hospital’s Medical Ethics Committee, according to the Declaration of Helsinki.
2.2. Data collection
All participants were managed at the specialist neurologists’ discretion in accordance with the hospital’s stroke management protocols. The stroke high-risk population questionnaire was designed according to the guidelines of the Management Measures for Stroke Screening and Intervention for High-Risk Populations. The process of the questionnaire survey was as follows: at the first station, a professionally trained neurologist assisted the subjects to complete the clinical information through face-to-face communication, including general information (gender, age and socioeconomic details), stroke or transient ischemia attack (TIA) history, family history of stroke, history of atrial fibrillation or cardiovascular diseases, hypertension, diabetes mellitus, dyslipidemia, smoking, and physical exercise. The second station was carried out by the specialist nurses to measure blood pressure, height and weight for the participants. Also the blood drawing project for the participants was completed, and the laboratory tests included blood glucose, blood lipids, homocysteine and glycated hemoglobin. To ensure the consistency of criteria for physical examination, the specialist nurses were professionally trained and using the same set of gauges which were calibrated twice a month. Meanwhile, all participants were examined on an empty stomach. Further reports of carotid ultrasonography, electrocardiogram, and the brain CT/MRI confirming the diagnosis were collected at the third station. The fourth station was conducted by the chief neurologists for a comprehensive evaluation. At last, all questionnaires and reports were collected at the end of the screening process, and all relevant data were systematically recorded, then the risk factors of each participant were determined according to the data results.
2.3. Definitions of major risk factors
Definitions of major risk factors were as follows: diabetes (fasting plasma glucose ≥ 7.0 mmol/L, history, or those who were receiving antidiabetic medication), hypertension (blood pressure ≥ 140/90 mm Hg, history, or those who were receiving antihypertensive medication), atrial fibrillation (history or electrocardiographic evidence), hyperlipidemia (total cholesterol ≥ 6.22 mmol/L, low-density lipoprotein cholesterol ≥ 4.14 mmol/L, triglyceride ≥ 2.26 mmol/L or high-density lipoprotein cholesterol < 1.04 mmol/L, meeting any of the above criteria, history, or those who were receiving antihyperlipidemic medication), hyperhomocysteinemia (plasma homocysteine ≥ 15 μmol/L), obvious overweight (BMI ≥ 26 kg/m2), obesity (BMI ≥ 28 kg/m2), Sedentary lifestyle (those who were sitting for more than 8 to 12 hours a day). History of stroke, TIA, and previous and current smoking were also systematically recorded.
2.4. Statistical analysis
Data processing and analysis were performed using IBM SPSS 21.0 statistical software. Continuous variables were expressed as mean ± standard deviation, while categorical variables were statistically described using rate and composition ratio. Chi-squared χ2 test or Fisher’s exact test was used for statistical analysis when appropriate. A multi-factor logistic regression prediction model was established based on the results of single-factor analysis. Logistic regression analysis was performed using stroke occurrence as dependent variable (Y) and other risk factors as independent variables (X). For each risk factor, an odds ratio (OR) with 95% confidence interval (CI) was then estimated through the R language package. The difference was considered statistically significant at a P value < 0.05.
3. Results
3.1. Baseline characteristics
A total of 1009 Chinese Han participants were enrolled in this study, of which 327 participants (32.4%) were males and 682 participants (67.6%) were females. The mean age was(60.9 ± 8.9)years old, and 350 participants (34.7%) were over 65 years old. In addition, a total of 94 patients had suffered from stroke, with a prevalence rate of 9.3% on average, and the prevalence rate was significantly higher in men (15%) than in women (6.6%) (P < .05), as shown in Table 1.
Table 1.
Univariate analysis of risk factors for stroke.
| Variables | N (%) | Stroke | Non-Stroke | Stroke (%) | χ2 | P value | |
|---|---|---|---|---|---|---|---|
| Sex | 18.401 | .000 | |||||
| Male | 327 | 32.4 | 49 | 278 | 15.0 | ||
| Female | 682 | 67.6 | 45 | 637 | 6.6 | ||
| Age | 17.519 | .000 | |||||
| 40~65 years | 659 | 65.3 | 43 | 616 | 6.5 | ||
| ≥65 years | 350 | 34.7 | 51 | 299 | 14.6 | ||
| Occupation | 1.754 | .185 | |||||
| Peasantry | 450 | 44.6 | 48 | 402 | 10.7 | ||
| Non-peasantry | 559 | 55.4 | 46 | 513 | 8.2 | ||
| Hypertension | 14.818 | .000 | |||||
| Yes | 596 | 59.1 | 73 | 523 | 12.2 | ||
| No | 413 | 40.9 | 21 | 392 | 5.1 | ||
| Diabetes | 8.219 | .004 | |||||
| Yes | 114 | 11.3 | 19 | 95 | 16.7 | ||
| No | 895 | 88.7 | 75 | 820 | 8.4 | ||
| Hyperlipidemia | 5.486 | .019 | |||||
| Yes | 351 | 34.8 | 43 | 308 | 12.3 | ||
| No | 658 | 65.2 | 51 | 607 | 7.8 | ||
| Atrial fibrillation | 26.640 | .000 | |||||
| Yes | 50 | 5.0 | 15 | 35 | 30 | ||
| No | 959 | 95.0 | 79 | 880 | 8.2 | ||
| TIA | 5.174 | .023 | |||||
| Yes | 87 | 8.6 | 14 | 73 | 16.1 | ||
| No | 922 | 91.4 | 80 | 842 | 8.7 | ||
| BMI | 0.065 | .799 | |||||
| ≥26 | 247 | 24.5 | 22 | 225 | 8.9 | ||
| <26 ≥ 18 | 762 | 75.5 | 72 | 690 | 9.4 | ||
| Sedentary | 20.264 | .000 | |||||
| Yes | 137 | 13.6 | 27 | 110 | 19.7 | ||
| No | 872 | 86.4 | 67 | 805 | 7.7 | ||
| Smoking | 17.895 | .000 | |||||
| Yes | 151 | 15.0 | 28 | 123 | 18.5 | ||
| No | 858 | 85.0 | 66 | 792 | 7.7 | ||
| Family history of stroke | 6.053 | .014 | |||||
| Yes | 167 | 16.6 | 24 | 143 | 14.4 | ||
| No | 842 | 83.4 | 70 | 772 | 8.3 | ||
| Homocysteine | |||||||
| Undetected | 420 | 41.6 | 31 | 389 | 7.4 | ||
| ≥15 | 198 | 19.6 | 25 | 173 | 12.6 | 1.163 | .281 |
| Normal | 391 | 38.8 | 38 | 353 | 9.7 | ||
BMI = body mass index, TIA = transient ischemia attack. P value < .05 indicates statistical significance.
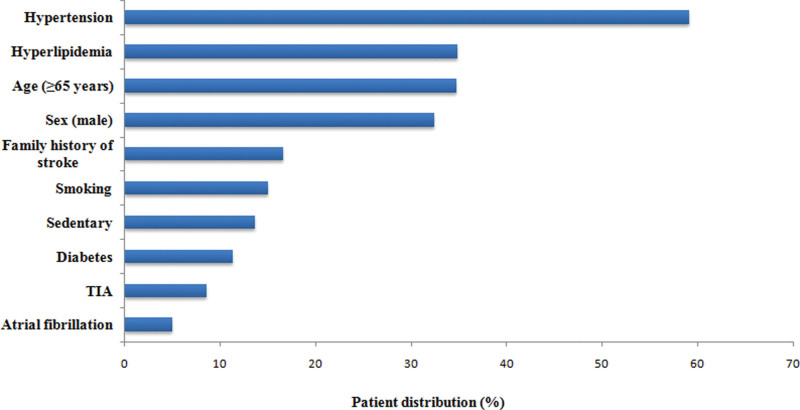
3.2. Univariate analysis of risk factors for stroke
The results of univariate analysis of risk factors for stroke in this study showed that there were statistically significant differences in the prevalence of stroke among residents with different age, sex, family history of stroke, hyperlipidemia, smoking, sedentary lifestyle, TIA, atrial fibrillation, diabetes and hypertension (all P < .05), as shown in Table 1. Among all risk factors, the highest exposure rate was hypertension (59.1%), then followed by hyperlipidemia (34.8%), age (≥65 years) (34.7%), sex (male) (32.4%), family history of stroke (16.6%), smoking (15%), sedentary (13.6%), diabetes (11.3%), TIA (8.6%), and atrial fibrillation (5%), as shown in Figure 1.
Figure 1.
The exposure rate of the main risk factors for stroke in the whole-group. TIA = transient ischemia attack.
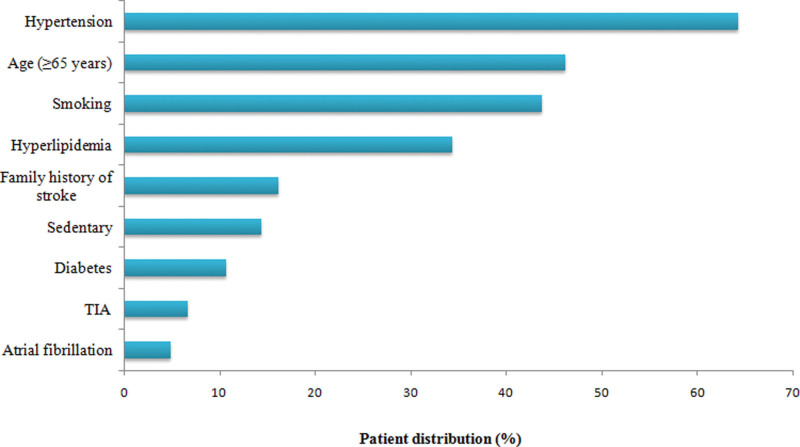
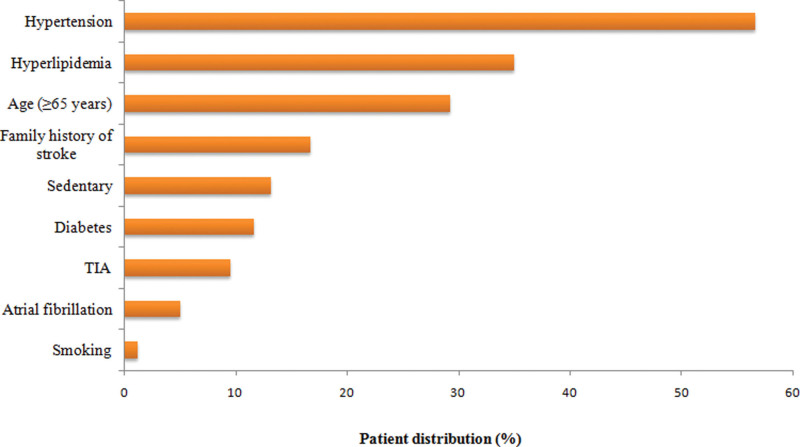
3.3. Comparison of risk factors for stroke in different genders
Among all risk factors, the top 3 exposure rates in males were hypertension (64.2%), age (≥65 years) (46.2%), and smoking (43.7%), while the top 3 exposure rates in females were hypertension (56.6%), hyperlipidemia (35%), and age (≥65 years) (29.2%), as shown in Figures 2 and 3. In the gender distribution, the exposure rates of hypertension, age (≥65 years), smoking, and sedentaty lifestyle in males were higher, while the exposure rates of diabetes, hyperlipidemia, atrial fibrillation, TIA, and family history of stroke in males were lower, as compared with females. Among them, there were statistically significant differences in hypertension, age (≥65 years), and smoking between males and females (all P < .05), as shown in Table 2.
Figure 2.
The exposure rate of the main risk factors for stroke in males. TIA = transient ischemia attack.
Figure 3.
The exposure rate of the main risk factors for stroke in females. TIA = transient ischemia attack.
Table 2.
Comparison of risk factors for stroke in different genders [n (%)].
| Risk factors | Male | Female | χ2 | P value |
|---|---|---|---|---|
| Age (≥65 years) | 151 (46.2) | 199 (29.2) | 28.190 | .000 |
| Hypertension | 210 (64.2) | 386 (56.6) | 5.311 | .021 |
| Diabetes | 35 (10.7) | 79 (11.6) | 0.171 | .679 |
| Hyperlipidemia | 112 (34.3) | 239 (35.0) | 0.061 | .804 |
| Atrial fibrillation | 16 (4.9) | 34 (5.0) | 0.004 | .950 |
| TIA | 22 (6.7) | 65 (9.5) | 2.204 | .138 |
| Sedentary | 47 (14.4) | 90 (13.2) | 0.261 | .610 |
| Smoking | 143 (43.7) | 8 (1.2) | 314.571 | .000 |
| Family history of stroke | 53 (16.2) | 114 (16.7) | 0.041 | .839 |
TIA = transient ischemia attack. P value < .05 indicates statistical significance.
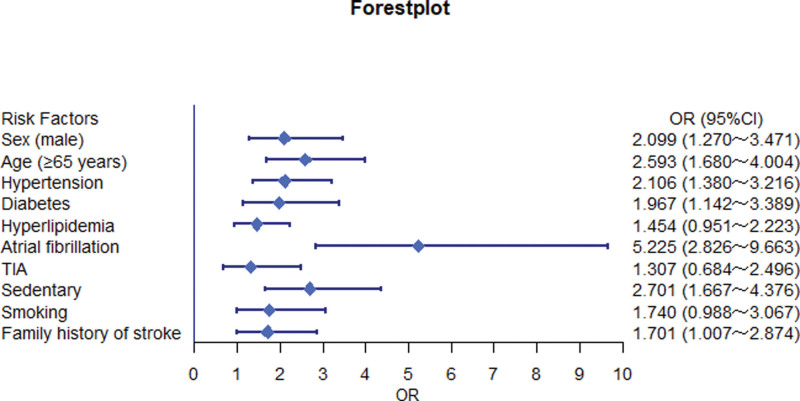
3.4. Results of logistic regression analysis of risk factors for stroke
According to the results of univariate analysis, risk factors with statistically significant differences were selected as independent variables, and whether stroke occurred was selected as dependent variable, and then further logistic regression analysis was performed. The final risk factors entered into the logistic regression model were gender, age, hypertension, diabetes, hyperlipidemia, presence of atrial fibrillation, TIA, sedentary lifestyle, smoking and family history of stroke (all P < .05, Table 1). The results of multifactorial logistic regression analysis showed that gender, age, family history of stroke, hypertension, atrial fibrillation, diabetes, and sedentary were significantly associated with an increased risk of stroke in the local population (all P < .05, Table 3). The top 5 risk factors for stroke were atrial fibrillation (OR = 5.225, 95% CI: 2.826–9.663), sedentary lifestyle (OR = 2.701, 95% CI: 1.667–4.376), age (≥65 years) (OR = 2.593, 95% CI: 1.680–4.004), hypertension (OR = 2.106, 95%CI: 1.380-3.216), and gender (male) (OR = 2.099, 95% CI: 1.270–3.471), as shown in Table 3 and Figure 4.
Table 3.
Logistic regression analysis of risk factors for stroke.
| Risk factors | B | SE | Wald | P value | OR (95% CI) |
|---|---|---|---|---|---|
| Sex (male) | 0.742 | 0.256 | 8.359 | .004 | 2.099 (1.270–3.471) |
| Age (≥65 years) | 0.953 | 0.222 | 18.498 | .000 | 2.593 (1.680–4.004) |
| Hypertension | 0.745 | 0.216 | 11.913 | .001 | 2.106 (1.380–3.216) |
| Diabetes | 0.677 | 0.277 | 5.953 | .015 | 1.967 (1.142–3.389) |
| Hyperlipidemia | 0.374 | 0.217 | 2.986 | .084 | 1.454 (0.951–2.223) |
| Atrial fibrillation | 1.654 | 0.314 | 27.793 | .000 | 5.225 (2.826–9.663) |
| TIA | 0.267 | 0.330 | 0.656 | .418 | 1.307 (0.684–2.496) |
| Sedentary | 0.994 | 0.246 | 16.284 | .000 | 2.701 (1.667–4.376) |
| Smoking | 0.554 | 0.289 | 3.676 | .055 | 1.740 (0.988–3.067) |
| Family history of stroke | 0.531 | 0.268 | 3.940 | .047 | 1.701 (1.007–2.874) |
CI = confidence interval, OR =odds ratio, TIA = transient ischemia attack. P value < .05 indicates statistical significance.
Figure 4.
Forestplot of risk factor analyses for stroke conducted by the R language package. Diamonds represent ORs. Horizontal lines indicate 95% CIs. CI = confidence interval, OR = odds ratio, TIA = transient ischemia attack.
4. Discussion
It is of great importance to identify high-risk factors that may lead to stroke and raise the risk awareness of high-risk groups.[7] Currently, there are some methods related to stroke screening or prediction of recurrence applied in clinical application,[8,9] however, the method of stroke risk prediction based on geographical characteristics has not been fully elucidated. According to the Chinese Center of Disease Control and Prevention, the prevalence and mortality rates of stroke in China varied by geographic region, and the results showed that the central region had higher incidence and mortality rates of stroke. We used a whole-group sampling method to conduct this cross-sectional study with a uniform questionnaire and related physical examinations of 1009 permanent residents in the Jingzhou City in central China, and the sample was representative. In this study, 94 stroke cases were screened, with a prevalence rate of 9.3% on average, and it was significantly higher in men (15%) than in women (6.6%) (P < .05). On the other hand, the prevalence of the disease became higher with the increasing of age, and it was significantly higher in patients aged over 65 years than those aged 45 years (P < .05). As for the causes, it may be attributed to men’s social pressure, long-term smoking, and other unhealthy lifestyles. On the other hand, it may be related to the protective effects of endogenous estrogen on women’s cardiovascular and cerebrovascular. At this point, it is suggested that more attention should be paid to stroke education especially for the male population to strengthen their health awareness and improve their life behaviors in the future. Also, people aged over 65 years should be considered as key group for the intervention of stroke and its risk factors, and both screening and prevention efforts of stroke in this age group should be strengthened.
Increasing evidence suggests that hypertension is the first risk factor for the development of stroke, and long-term hypertension predisposes the body to intimal damage leading to the development of atherosclerosis, which in turn causes the onset of stroke.[10,11] Based on the results from the present study, multi-factor logistic regression analysis suggested that gender, age, hypertension, diabetes, hyperlipidemia, presence of atrial fibrillation, TIA, sedentary, smoking and family history of stroke were associated risk factors for stroke in the local population (all P < .05), which is generally consistent with the results of previous studies.[12–14] The top 5 risk factors for stroke were atrial fibrillation (OR = 5.225, 95% CI: 2.826–9.663), sedentary lifestyle (OR = 2.701, 95% CI: 1.667–4.376), age (≥65 years) (OR = 2.593, 95% CI: 1.680–4.004), hypertension (OR = 2.106, 95% CI: 1.380–3.216), and gender (male) (OR = 2.099, 95% CI: 1.270–3.471). Two risk factors, age and hypertension, increase the risk of atherosclerotic lesions in patients, and this study further found that atrial fibrillation was a high risk factor for stroke occurrence in this region, which may be related to the reason that long-term atrial fibrillation tends to cause blood clots to dislodge from the heart and thus block cerebral vessels along the blood flow, which in turn causes stroke,[15,16] suggesting that on the basis of strengthening the prevention of hypertension and diabetes mellitus, effective measures should be actively taken to control and manage those patients with atrial fibrillation, thus delaying or reducing the occurrence of stroke. The poor lifestyle habits such as smoking and sedentary lifestyle further increase the risk of stroke in the population. The high-risk factors are closely related to the lifestyle habits of the regional population.[17,18] To some extent, the weak awareness of prevention and control among the population contributes to the high incidence of stroke, and if these high-risk individuals are not managed seriously, they will become stroke patients in 10 years.[19] Therefore, smoking cessation education should be strengthened especially for the male population, and smoking cessation should be made a priority in stroke prevention and control in the central area. At the same time, the population in this central area should be encouraged to engage in more appropriate physical exercises such as slow walking and hiking.
Stroke is mainly caused by the long-term accumulation of multiple complex factors, which can be categorized into 2 types: modifiable and non-modifiable risk factors, and the key prevention of stroke is mainly to minimize the modifiable risk factors,[20,21] including smoking, hypertension, atrial fibrillation, diabetes mellitus and sedentary lifestyle in this study. Hence, providing targeted intervention strategies and scientific guidance for those people with modifiable risk factors is of great public health significance to reduce the incidence and mortality of stroke. On the other hand, there may be some limitations. Some data of risk factors were collected in part from medical records from patients and their families, while recall bias associated with history of diseases in a few participants who had no specific data could not completely excluded. Additionally, some possible risk factors such as homocysteine levels were not fully investigated and detected. In spite of this, we made meticulous efforts to reduce these differences or bias in the descriptive data and tried to expand the sample size in this study. Further investigations are warranted to focus on the specific mechanisms and individual measures for different groups with different risk factors of stroke in the future study.
In conclusion, this study effectively identifies the high risk factors for stroke and provides scientific insights for risk assessment, intervention of risk factors, and decision making of health management departments in the central region of China. The modifable risk factors for stroke such as smoking, hypertension, atrial fibrillation, diabetes mellitus, and sedentary lifestyle were also observed. Our findings further highlight the significant of the primary and secondary prevention for stroke and reveal the potential targets to reduce the heavy stroke burden in China around the world.
Author contributions
Data curation: Mingcan Wu, Qingfen Tu.
Formal analysis: Mingcan Wu.
Investigation: Honglian Wang.
Project administration: Honglian Wang, Qingfen Tu.
Software: Qingfen Tu.
Writing – original draft: Honglian Wang.
Writing – review & editing: Maokun Li.
Abbreviations:
- CI =
- confidence interval
- OR =
- odds ratio
- TIA =
- transient ischemia attack
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The authors have no conflicts of interest.
How to cite this article: Wang H, Wu M, Tu Q, Li M. Risk factors for stroke in a population of central China: A cross-sectional study. Medicine 2022;101:46(e31946).
Contributor Information
Honglian Wang, Email: 282911852@qq.com.
Mingcan Wu, Email: Letitia777@sina.cn.
References
- [1].GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Feigin LF, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120:439–48. [DOI] [PubMed] [Google Scholar]
- [3].Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention and management. Lancet Neurol. 2019;18:394–405. [DOI] [PubMed] [Google Scholar]
- [4].Wang W, Jiang B, Sun H, et al. Prevalence, incidence and mortality of stroke in China: results from a Nationwide Population-Based Survey of 480687 Adults. Circulation. 2017;135:759–71. [DOI] [PubMed] [Google Scholar]
- [5].Jiang NN, Luo HY, Liu JH. Evaluation of screening and clinical intervention effects in high-risk groups for stroke. China Med Innov. 2017;14:22–5. [Google Scholar]
- [6].Zhang X. Evaluation of screening and clinical intervention effects in high-risk groups for stroke. Clin Res. 2019;27:77–8. [Google Scholar]
- [7].Wang J, Wen X, Li W, et al. Risk factors for stroke in the Chinese population: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2017;26:509–17. [DOI] [PubMed] [Google Scholar]
- [8].Wang R, Bian D, Wang SQ, et al. Application of decision tree algorithm in stroke risk classification prediction. Chin Convalesc Med. 2019;28:233–6. [Google Scholar]
- [9].van Alebeek ME, Arntz RM, Ekker MS, et al. Risk factors and mechanisms of stroke in young adults: the FUTURE study. J Cereb Blood Flow Metab. 2018;38:1631–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Buonacera A, Stancanelli B, Malatino L. Stroke and hypertension: an appraisal from pathophysiology to clinical practice. Curr Vasc Pharmacol. 2019;17:72–84. [DOI] [PubMed] [Google Scholar]
- [11].Sun P, Chen M, Guo X, et al. Combined effect of hypertension and hyperuricemia on ischemic stroke in a rural Chinese population. BMC Public Health. 2021;21:776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Liu Y, Li J, Dou Y, et al. Impacts of type 2 diabetes mellitus and hypertension on the incidence of cardiovascular diseases and stroke in China real-world setting: a retrospective cohort study. BMJ Open. 2021;11:e053698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Joundi RA, Patten SB, Williams JVA, et al. Association between excess leisure sedentary time and risk of stroke in young individuals. Stroke. 2021;52:3562–8. [DOI] [PubMed] [Google Scholar]
- [14].Ram CVS, Kumar S, Renjen PN, et al. Risk factors predisposing to acute stroke in India: a prospective study. J Hypertens. 2021;39:2183–9. [DOI] [PubMed] [Google Scholar]
- [15].Migdady I, Russman A, Buletko AB. Atrial fibrillation and ischemic stroke: a clinical review. Semin Neurol. 2021;41:348–64. [DOI] [PubMed] [Google Scholar]
- [16].Healey JS, Amit G, Field TS. Atrial fibrillation and stroke: how much atrial fibrillation is enough to cause a stroke? Curr Opin Neurol. 2020;33:17–23. [DOI] [PubMed] [Google Scholar]
- [17].Ingeman A, Andersen G, Thomsen RW, et al. Lifestyle factors and early clinical outcome in patients with acute stroke: a population-based study. Stroke. 2017;48:611–7. [DOI] [PubMed] [Google Scholar]
- [18].Sarikaya H, Ferro J, Arnold M. Stroke prevention--medical and lifestyle measures. Eur Neurol. 2015;73:150–7. [DOI] [PubMed] [Google Scholar]
- [19].Yang MZ, Fang F, Chen L. Stroke risk screening and risk factor analysis in high-risk groups. J Nurs. 2014;29:15–7. [Google Scholar]
- [20].Hankey GS. Stroke. Lancet. 2017;389:641–54. [DOI] [PubMed] [Google Scholar]
- [21].Harshfield EL, Georgakis MK, Malik R, et al. Modifiable lifestyle factors and risk of stroke: a mendelian randomization analysis. Stroke. 2021;52:931–6. [DOI] [PMC free article] [PubMed] [Google Scholar]